Management of Retinal detachment Dr Vincent YauWing Lee


- Slides: 51
Management of Retinal detachment Dr. Vincent Yau-Wing Lee Asia-Pacific Vitreo-retina Society
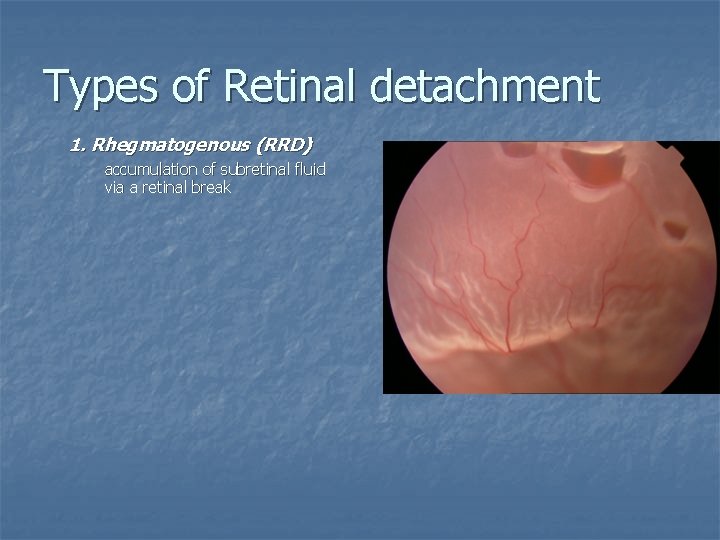
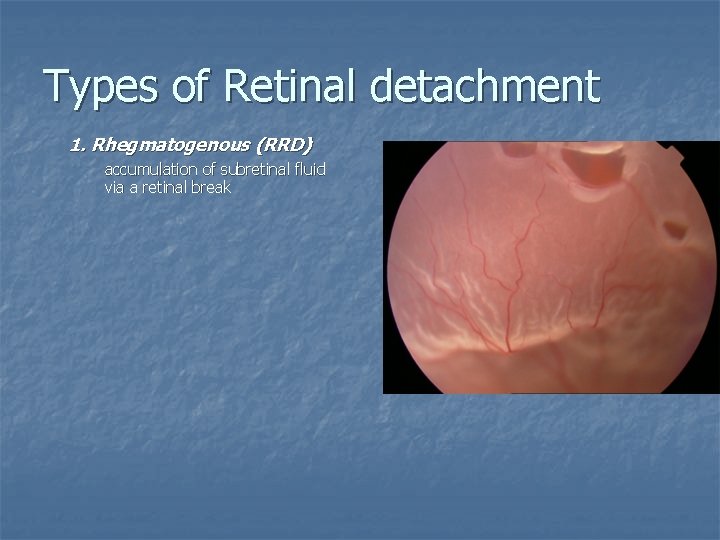
Types of Retinal detachment 1. Rhegmatogenous (RRD) accumulation of subretinal fluid via a retinal break
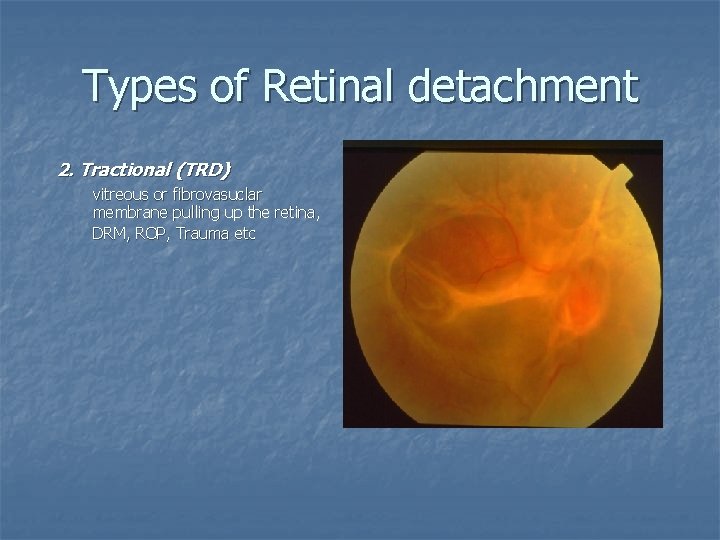
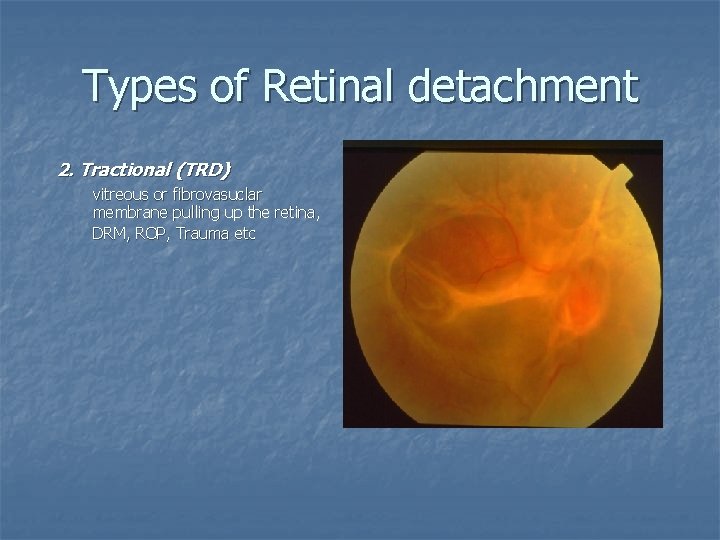
Types of Retinal detachment 2. Tractional (TRD) vitreous or fibrovasuclar membrane pulling up the retina, DRM, ROP, Trauma etc
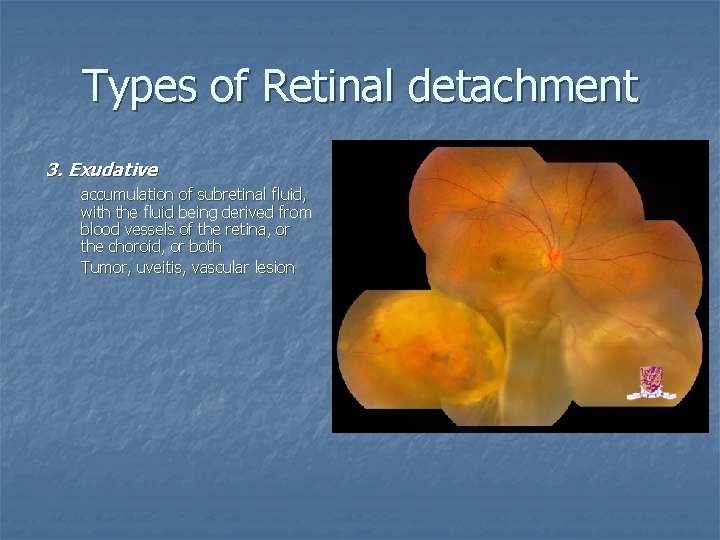
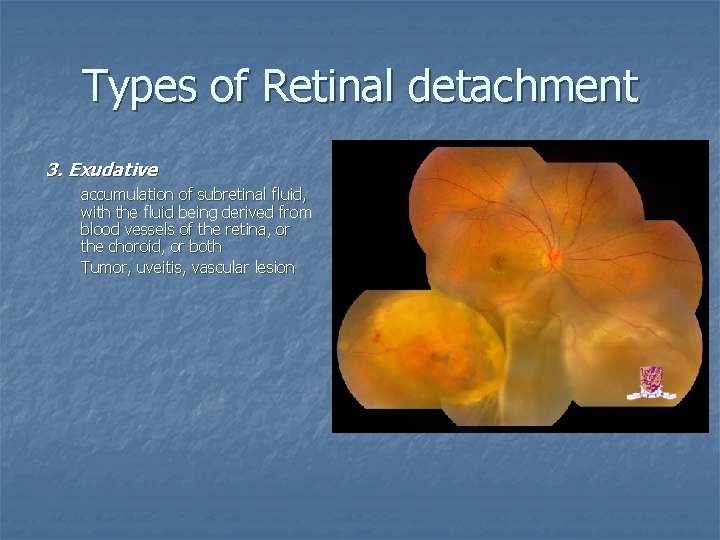
Types of Retinal detachment 3. Exudative accumulation of subretinal fluid, with the fluid being derived from blood vessels of the retina, or the choroid, or both Tumor, uveitis, vascular lesion

Rhegmatogenous Retinal detachment (RRD)
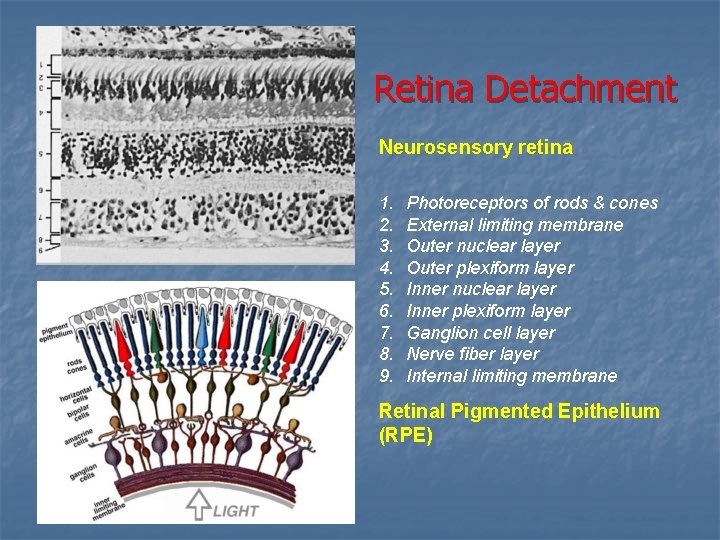
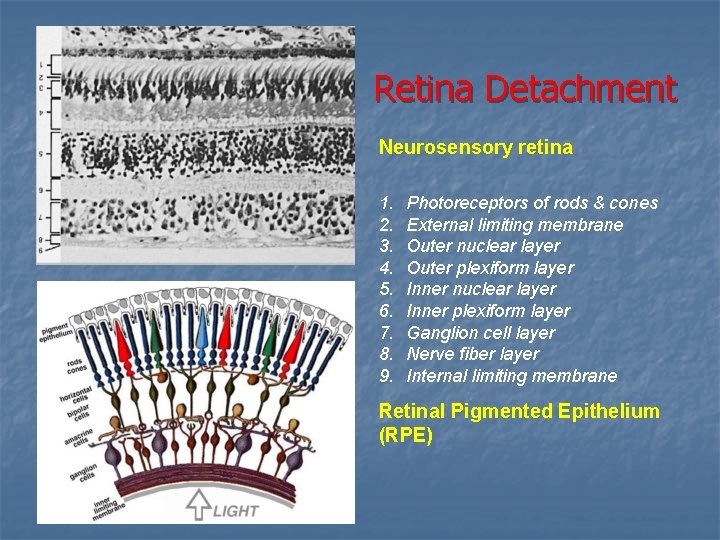
Retina Detachment Neurosensory retina 1. 2. 3. 4. 5. 6. 7. 8. 9. Photoreceptors of rods & cones External limiting membrane Outer nuclear layer Outer plexiform layer Inner nuclear layer Inner plexiform layer Ganglion cell layer Nerve fiber layer Internal limiting membrane Retinal Pigmented Epithelium (RPE)
n Rhegmatogenous retinal detachment from the Greek word rhegma, which means “a rent”
How does RRD happen? n n n Understand the normal force keep the retina attached. Understand the relationship between PVD and RD Causes of RD other than PVD
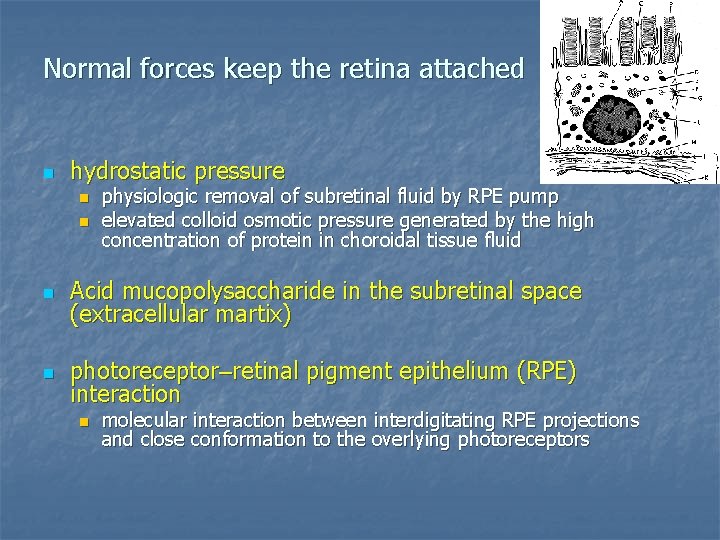
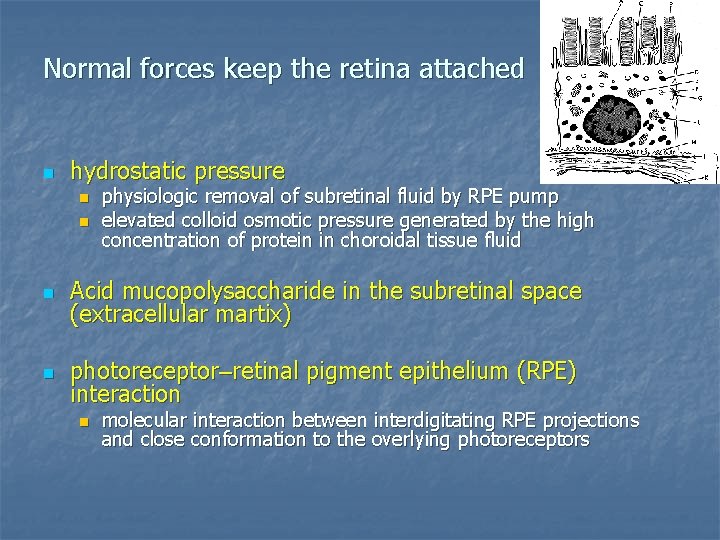
Normal forces keep the retina attached n hydrostatic pressure n n physiologic removal of subretinal fluid by RPE pump elevated colloid osmotic pressure generated by the high concentration of protein in choroidal tissue fluid n Acid mucopolysaccharide in the subretinal space (extracellular martix) n photoreceptor–retinal pigment epithelium (RPE) interaction n molecular interaction between interdigitating RPE projections and close conformation to the overlying photoreceptors
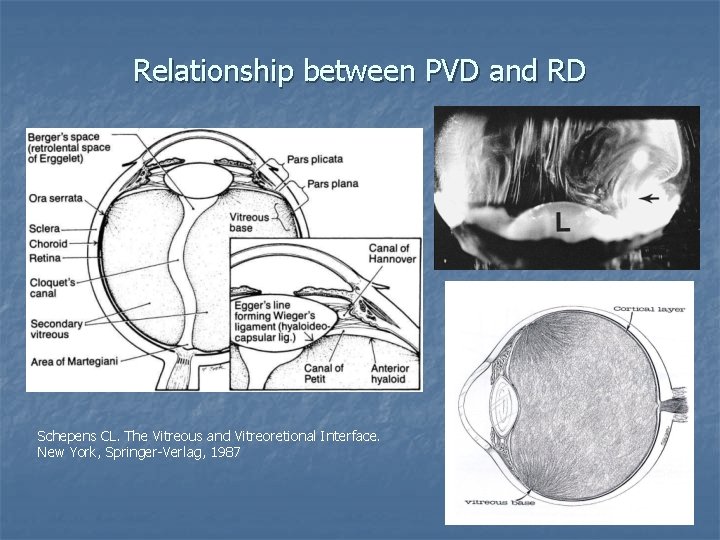
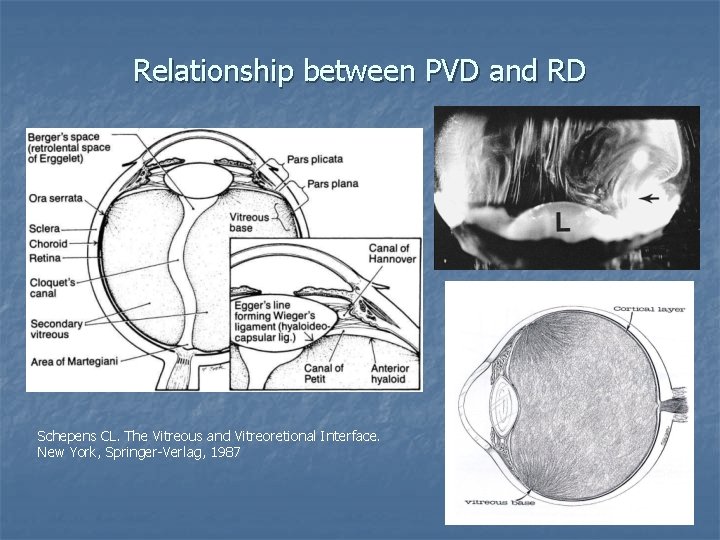
Relationship between PVD and RD Schepens CL. The Vitreous and Vitreoretional Interface. New York, Springer-Verlag, 1987
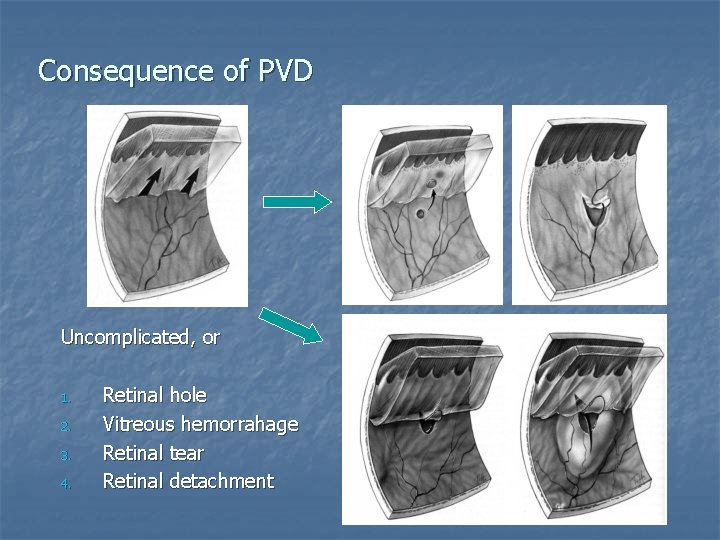
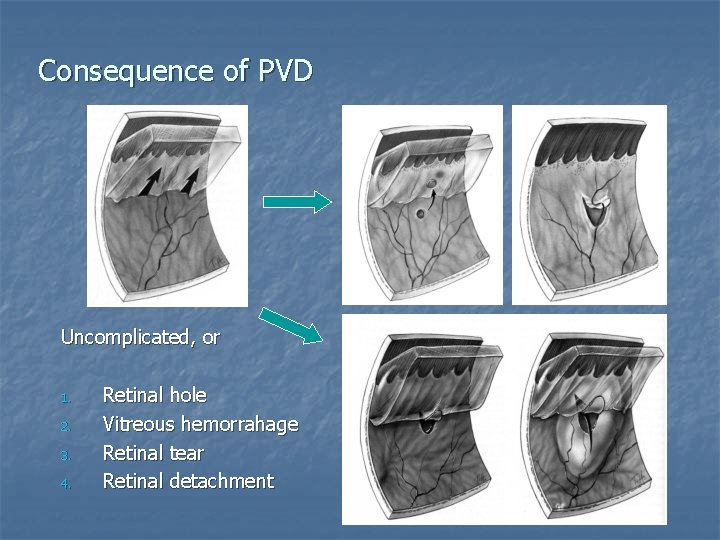
Consequence of PVD 1 2 Uncomplicated, or 1. 2. 3. 4. Retinal hole Vitreous hemorrahage Retinal tear Retinal detachment 3 4
Rhegmatogenous RD (RRD) Causes n n n n Posterior vitreous detachment Peripheral fundus lesion Myopia Ocular surgery – cataract extraction Trauma Intraocular inflammation / infection Syndromes n n n Wagner-Jansen-Stickler Syndrome Goldmann Favre Syndrome Marfan’s Syndrome Homocystinuria Ehlers-Danlos Syndrome
Management of RRD
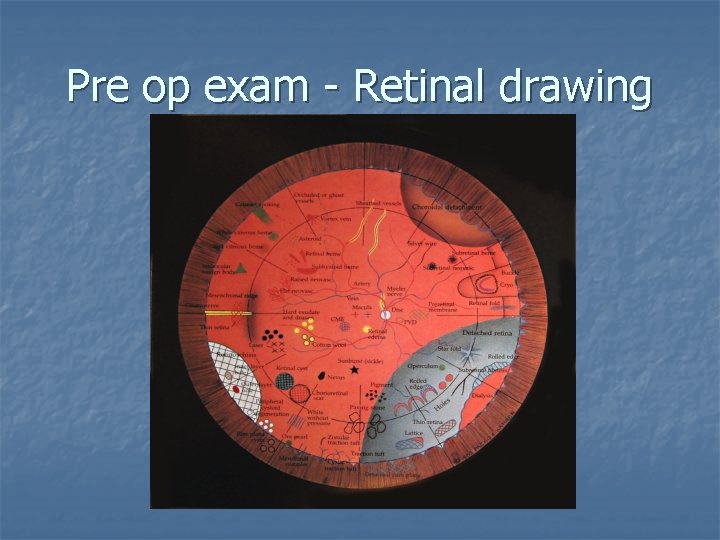
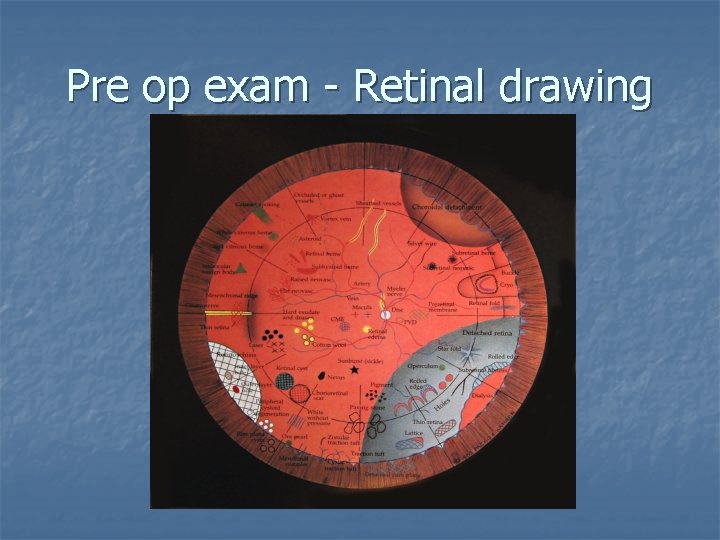
Pre op exam - Retinal drawing
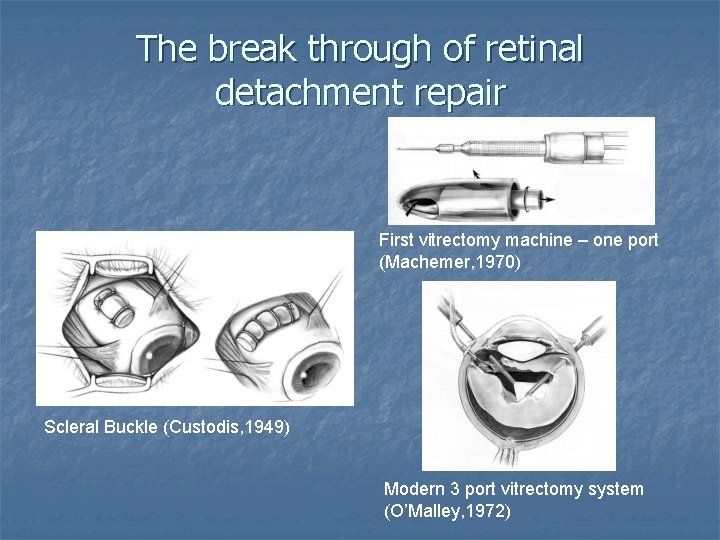
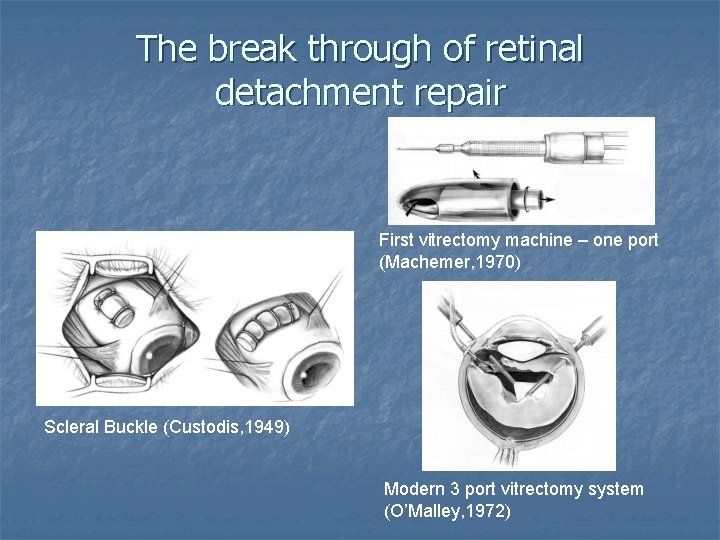
The break through of retinal detachment repair First vitrectomy machine – one port (Machemer, 1970) Scleral Buckle (Custodis, 1949) Modern 3 port vitrectomy system (O’Malley, 1972)
Goals of treatment for Retinal Detachment n n Preservation of vision. In particular the central vision Relief of inward traction on the retina Closure of all retinal breaks Elimination of subretinal fluid
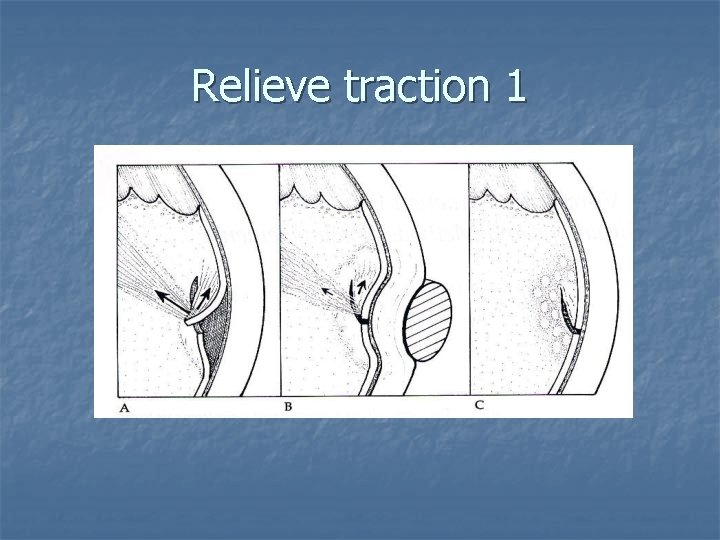
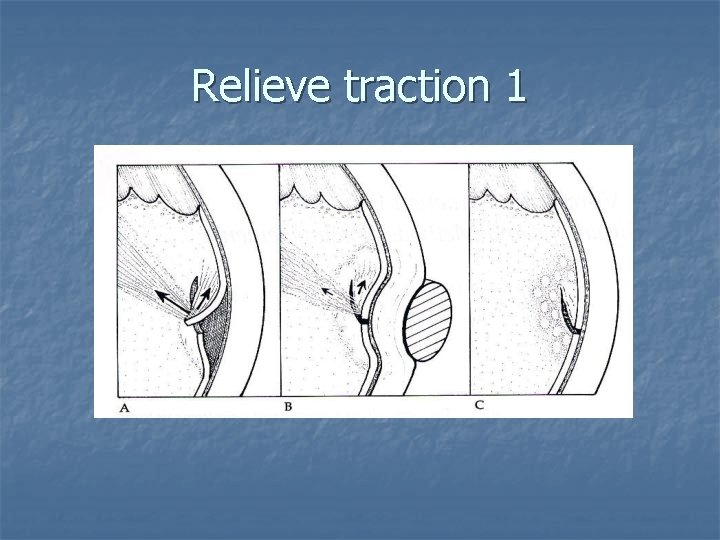
Relieve traction 1
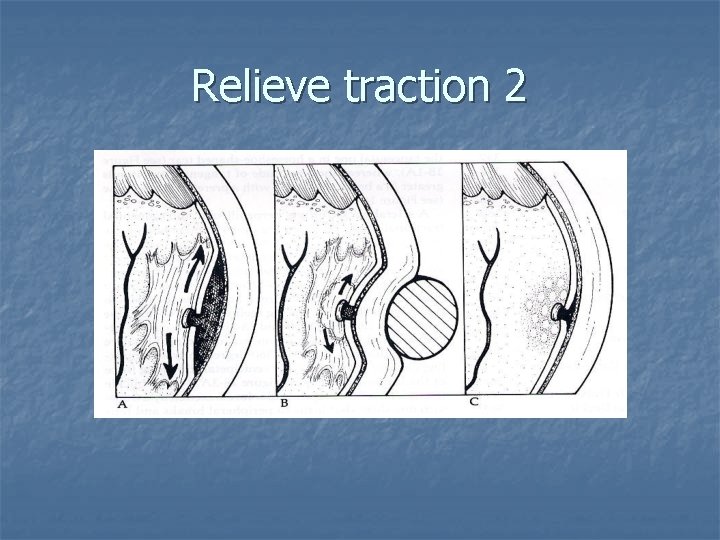
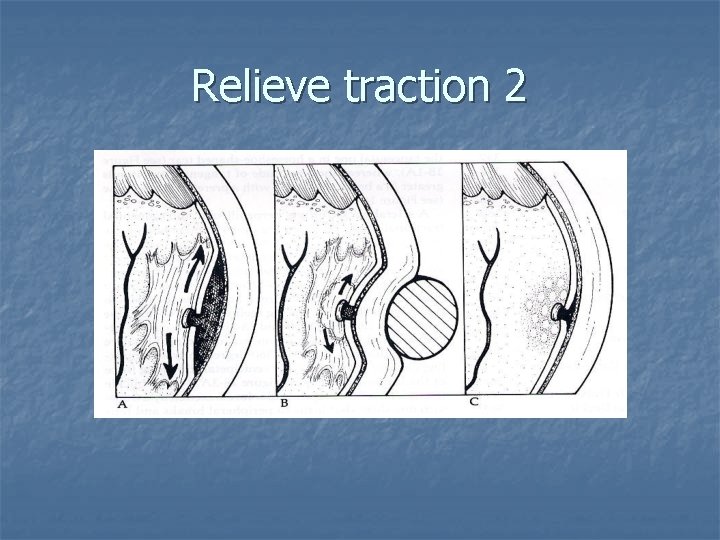
Relieve traction 2
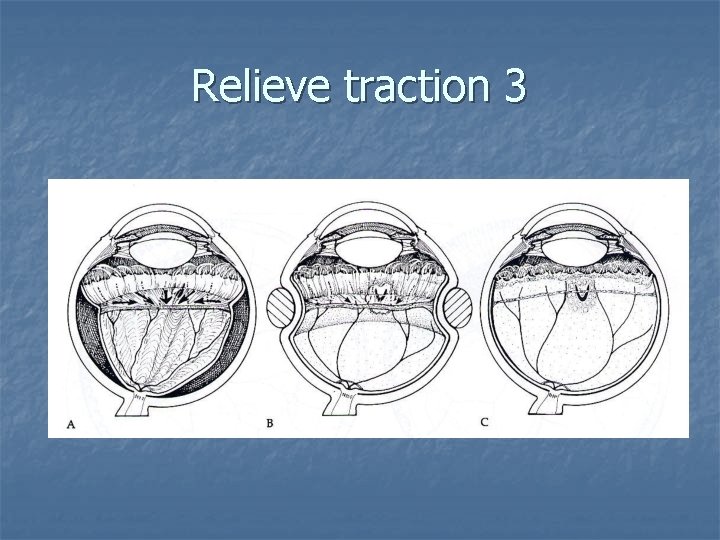
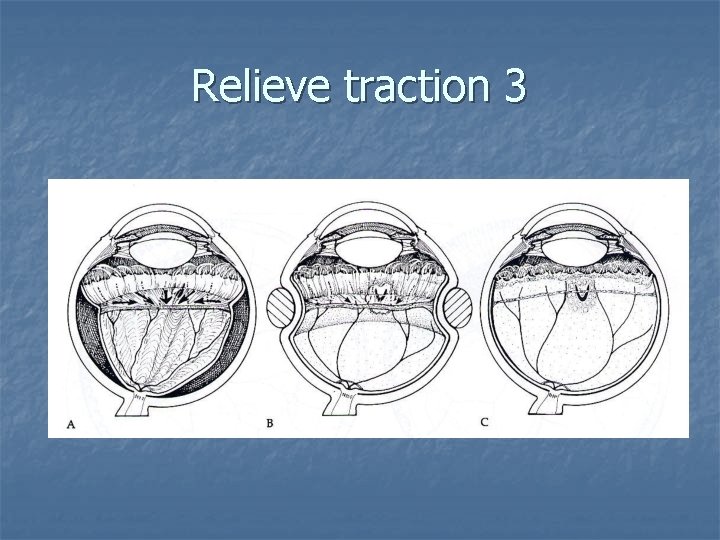
Relieve traction 3
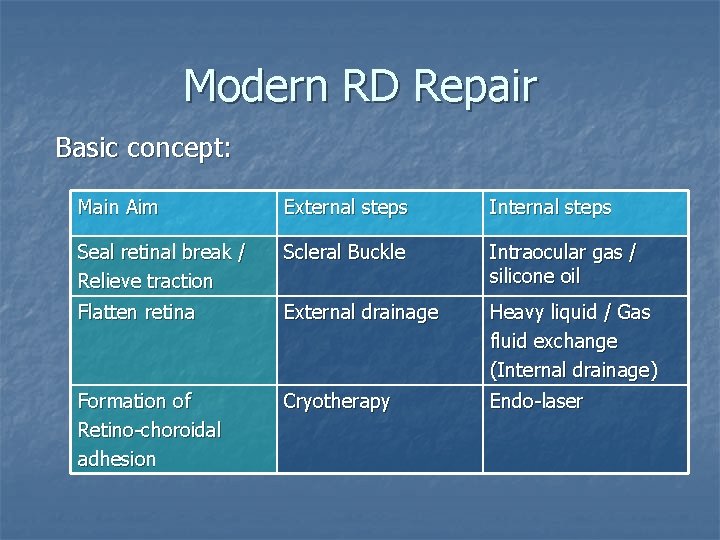
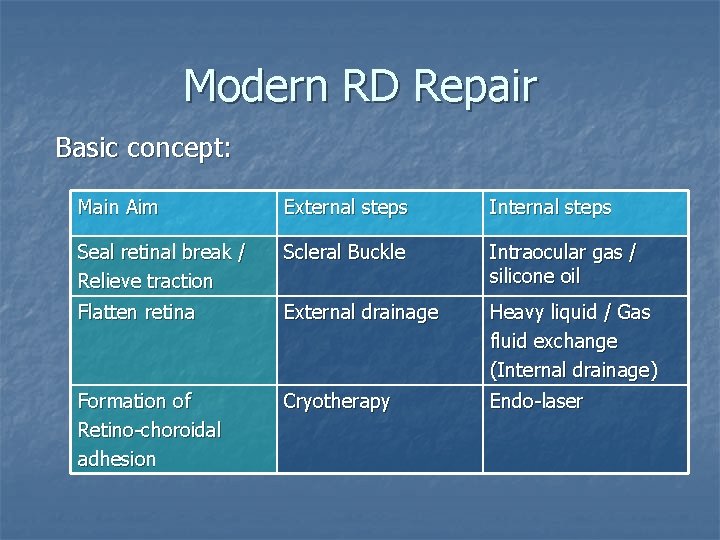
Modern RD Repair Basic concept: Main Aim External steps Internal steps Seal retinal break / Relieve traction Scleral Buckle Intraocular gas / silicone oil Flatten retina External drainage Heavy liquid / Gas fluid exchange (Internal drainage) Formation of Retino-choroidal adhesion Cryotherapy Endo-laser
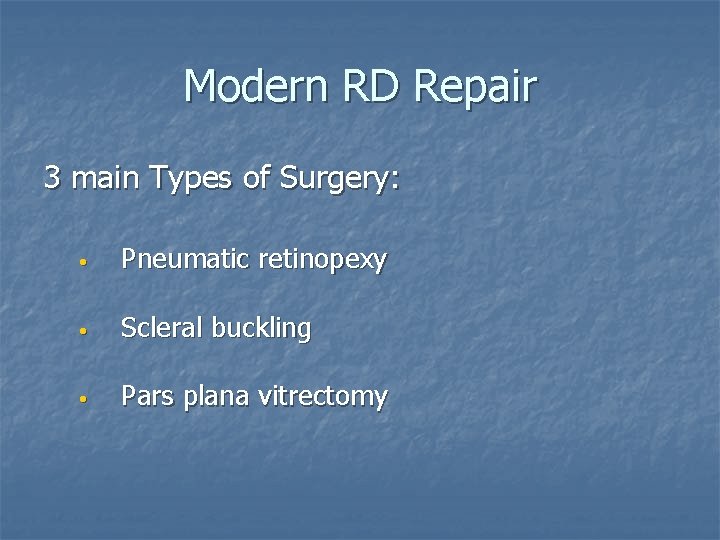
Modern RD Repair 3 main Types of Surgery: • Pneumatic retinopexy • Scleral buckling • Pars plana vitrectomy
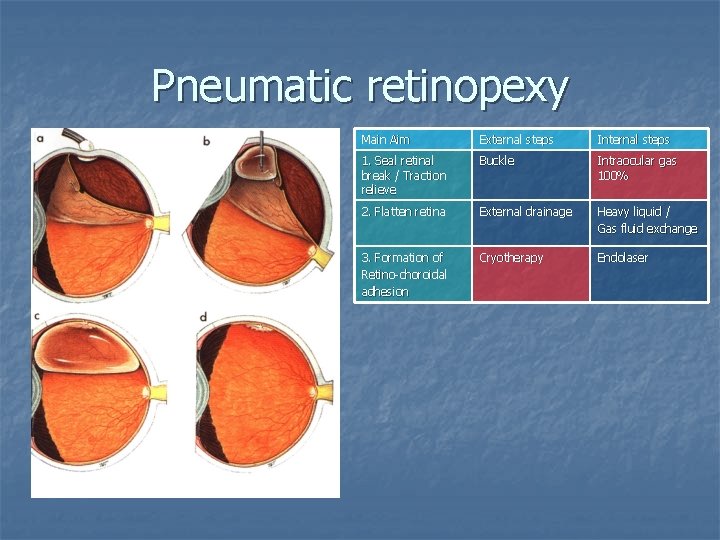
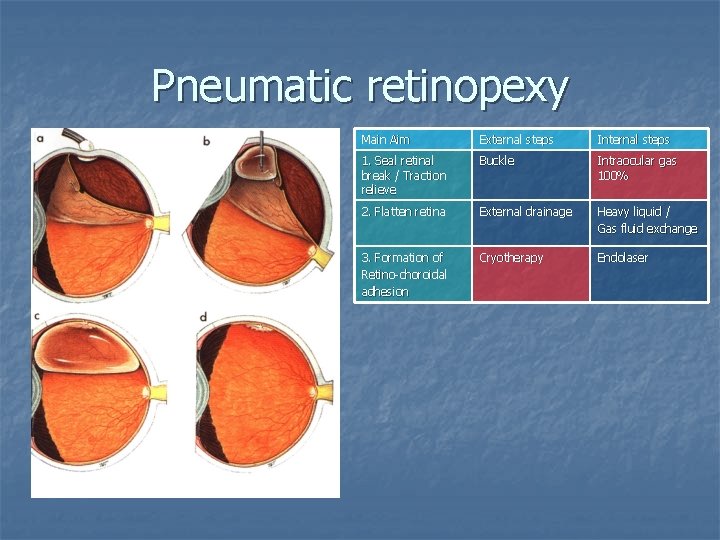
Pneumatic retinopexy Main Aim External steps Internal steps 1. Seal retinal break / Traction relieve Buckle Intraocular gas 100% 2. Flatten retina External drainage Heavy liquid / Gas fluid exchange 3. Formation of Retino-choroidal adhesion Cryotherapy Endolaser
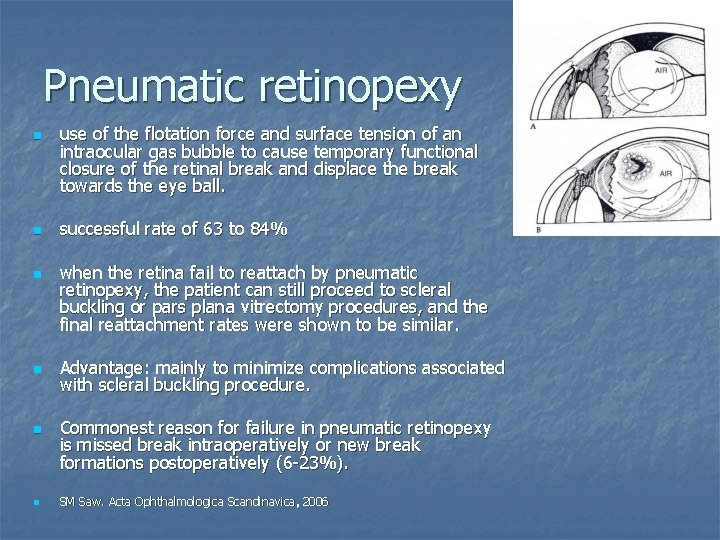
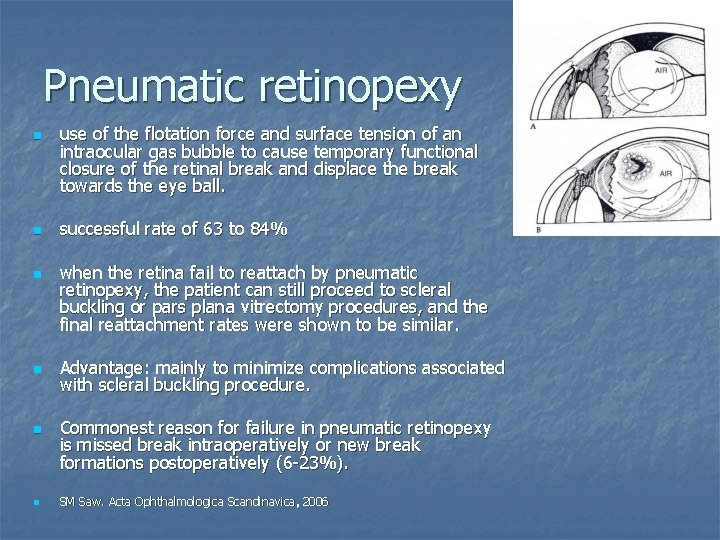
Pneumatic retinopexy n n n use of the flotation force and surface tension of an intraocular gas bubble to cause temporary functional closure of the retinal break and displace the break towards the eye ball. successful rate of 63 to 84% when the retina fail to reattach by pneumatic retinopexy, the patient can still proceed to scleral buckling or pars plana vitrectomy procedures, and the final reattachment rates were shown to be similar. Advantage: mainly to minimize complications associated with scleral buckling procedure. Commonest reason for failure in pneumatic retinopexy is missed break intraoperatively or new break formations postoperatively (6 -23%). SM Saw. Acta Ophthalmologica Scandinavica, 2006
Pneumatic retinopexy n Indication n Contraindication n retinal break equal to / smaller than 1 clock hours’ size located within the superior 8 clock hours of the peripheral retina with proliferative retinopathy grade C or above Aphakic / pseudophakic eye (relative contraindication only) The Retina Detachment Study Group: Pneumatic retinopexy: A multicenter random ized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1989
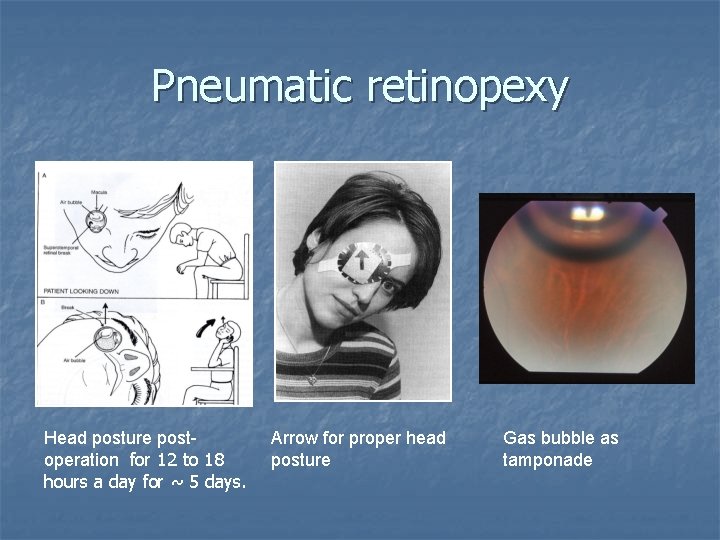
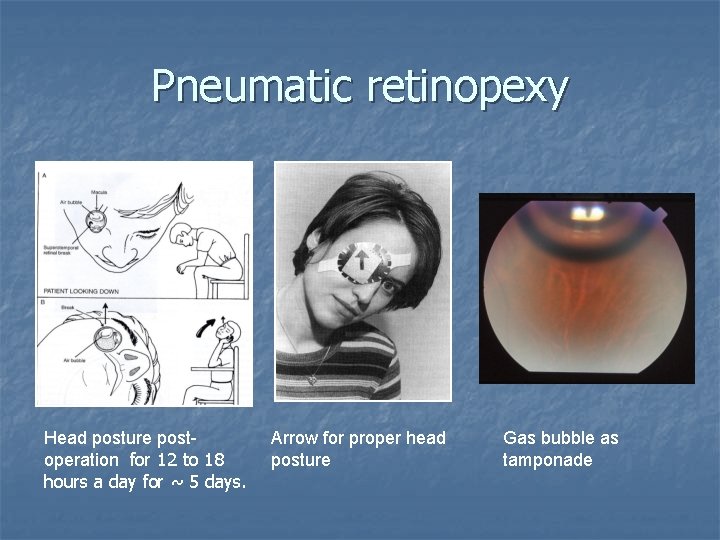
Pneumatic retinopexy Head posture post operation for 12 to 18 hours a day for ~ 5 days. Arrow for proper head posture Gas bubble as tamponade
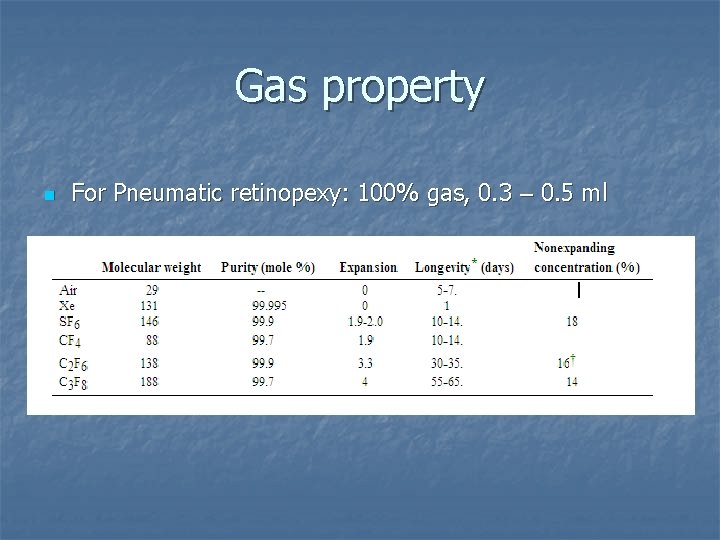
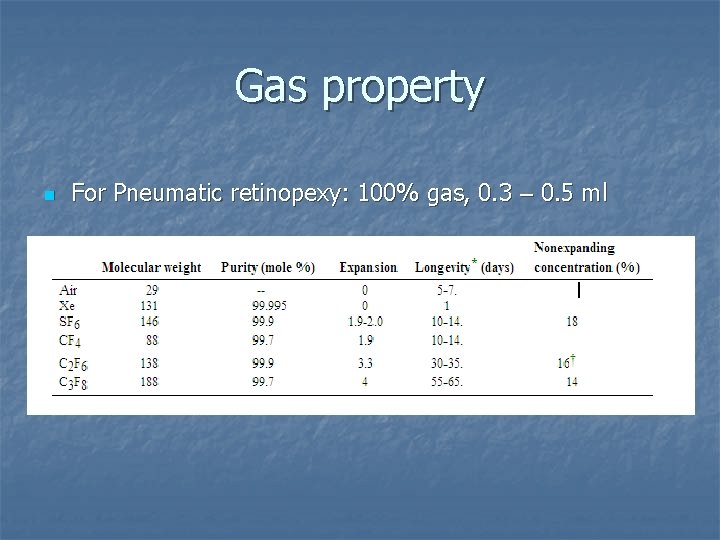
Gas property n For Pneumatic retinopexy: 100% gas, 0. 3 – 0. 5 ml
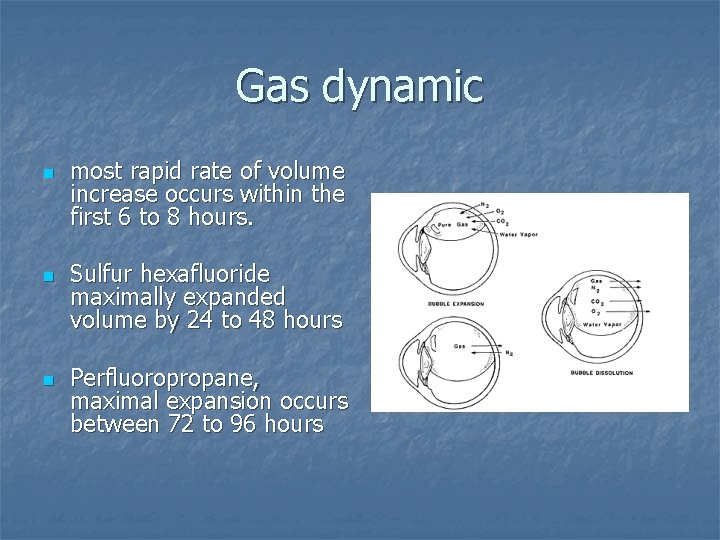
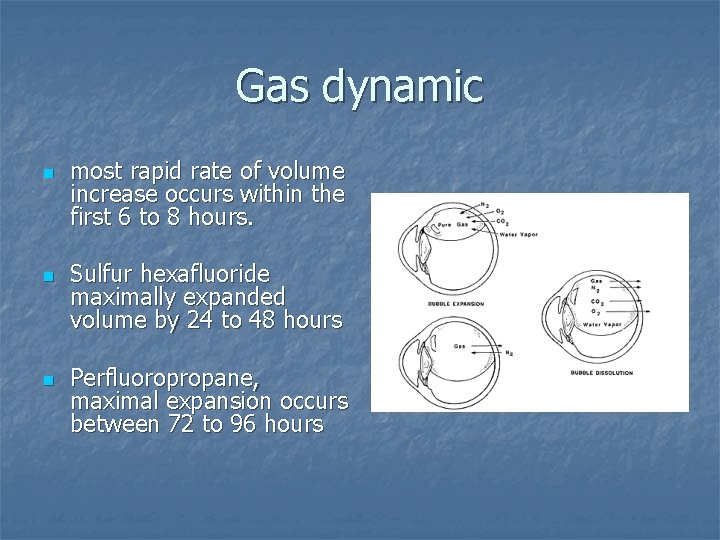
Gas dynamic n n n most rapid rate of volume increase occurs within the first 6 to 8 hours. Sulfur hexafluoride maximally expanded volume by 24 to 48 hours Perfluoropropane, maximal expansion occurs between 72 to 96 hours
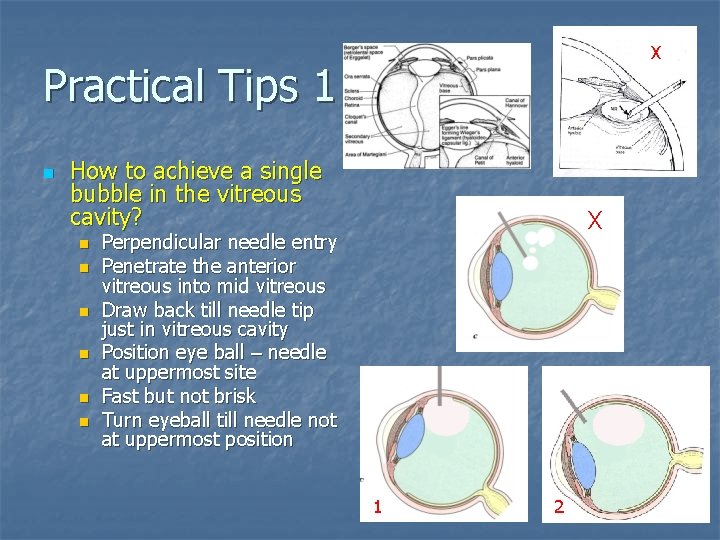
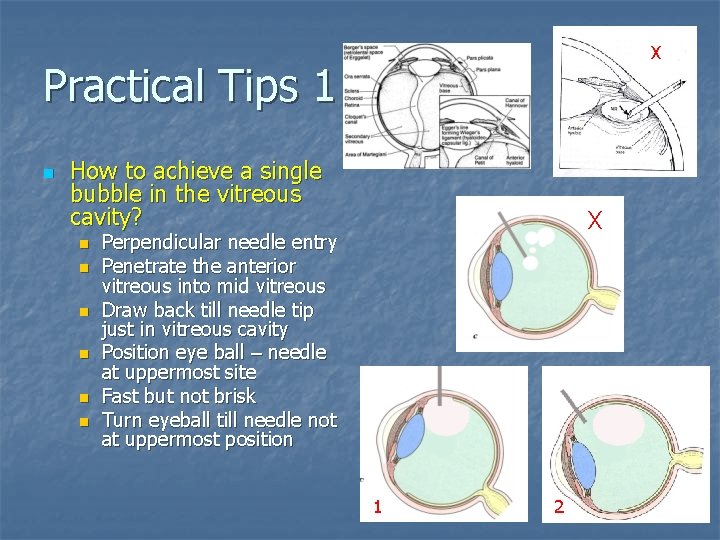
X Practical Tips 1 n How to achieve a single bubble in the vitreous cavity? n n n X Perpendicular needle entry Penetrate the anterior vitreous into mid vitreous Draw back till needle tip just in vitreous cavity Position eye ball – needle at uppermost site Fast but not brisk Turn eyeball till needle not at uppermost position 1 2
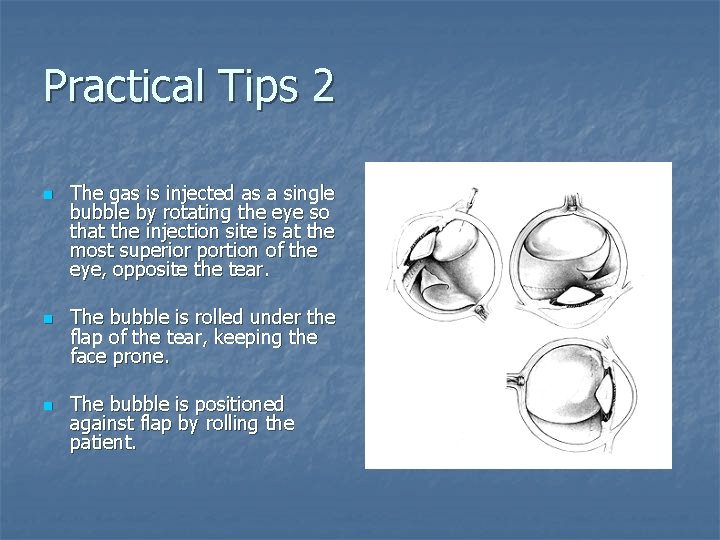
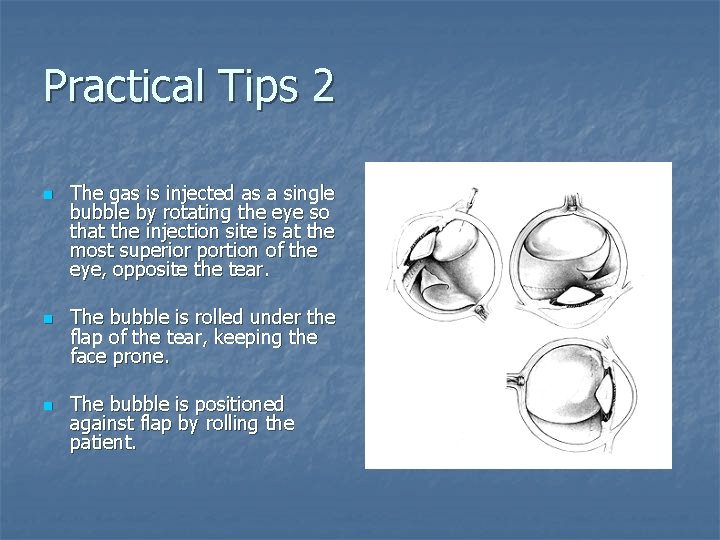
Practical Tips 2 n n n The gas is injected as a single bubble by rotating the eye so that the injection site is at the most superior portion of the eye, opposite the tear. The bubble is rolled under the flap of the tear, keeping the face prone. The bubble is positioned against flap by rolling the patient.
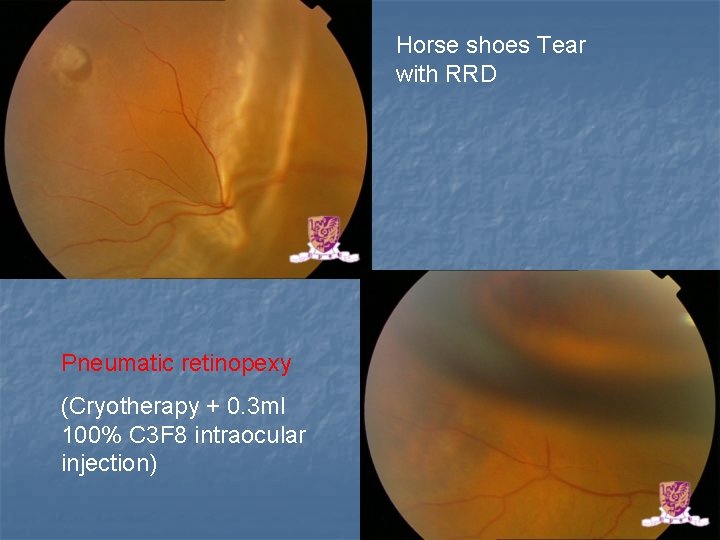
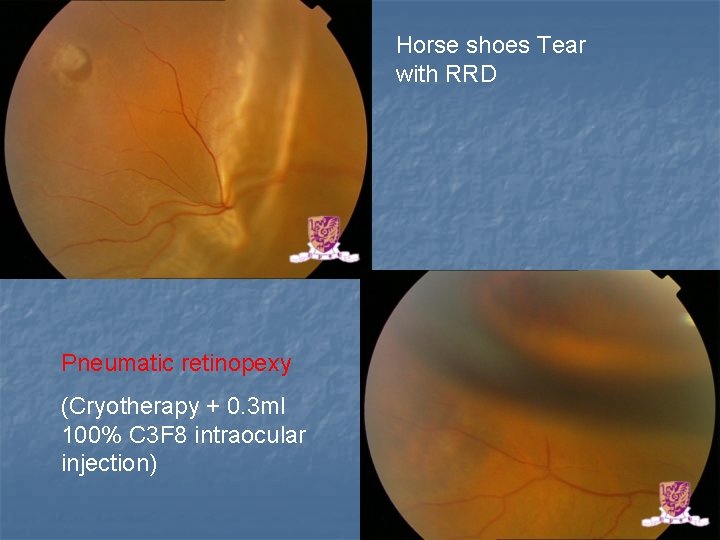
Horse shoes Tear with RRD Pneumatic retinopexy (Cryotherapy + 0. 3 ml 100% C 3 F 8 intraocular injection)
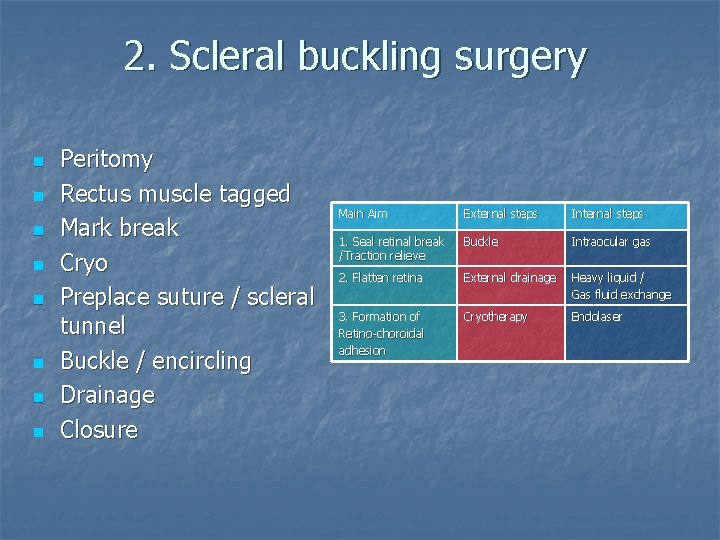
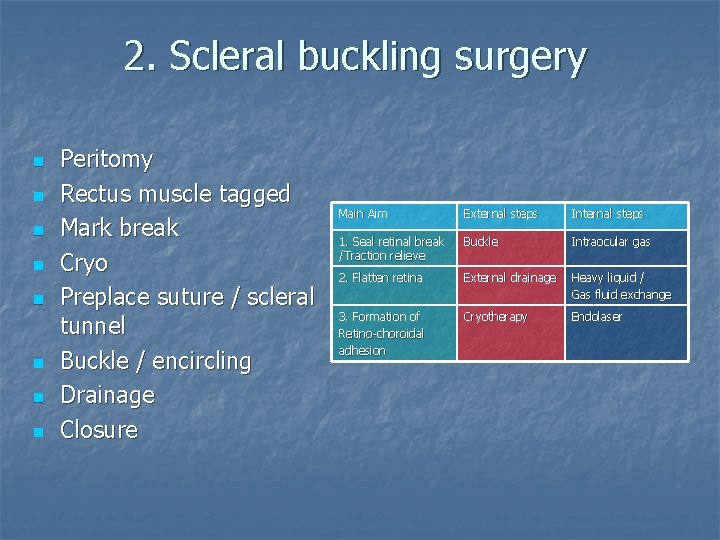
2. Scleral buckling surgery n n n n Peritomy Rectus muscle tagged Mark break Cryo Preplace suture / scleral tunnel Buckle / encircling Drainage Closure Main Aim External steps Internal steps 1. Seal retinal break /Traction relieve Buckle Intraocular gas 2. Flatten retina External drainage Heavy liquid / Gas fluid exchange 3. Formation of Retino-choroidal adhesion Cryotherapy Endolaser
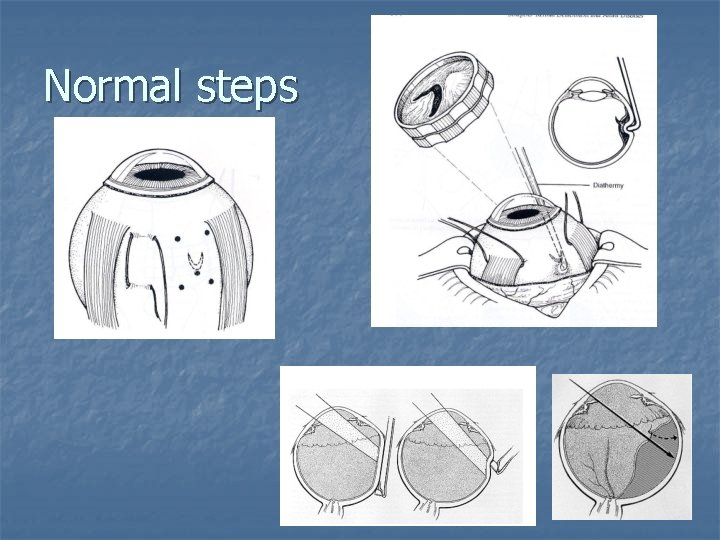
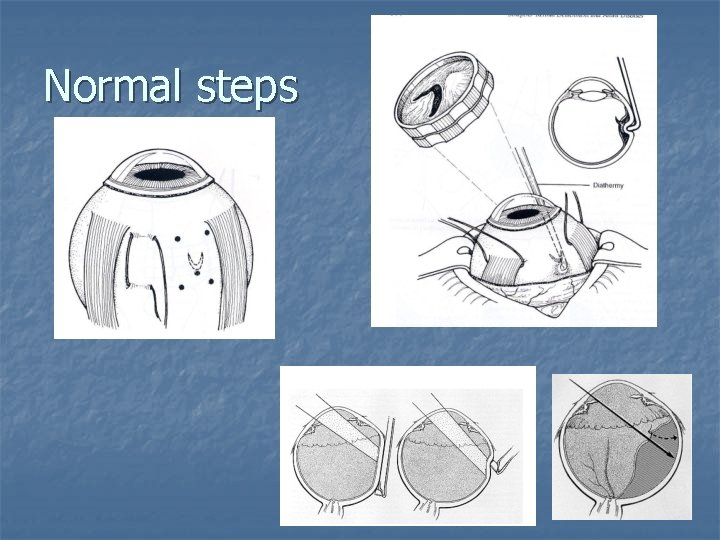
Normal steps
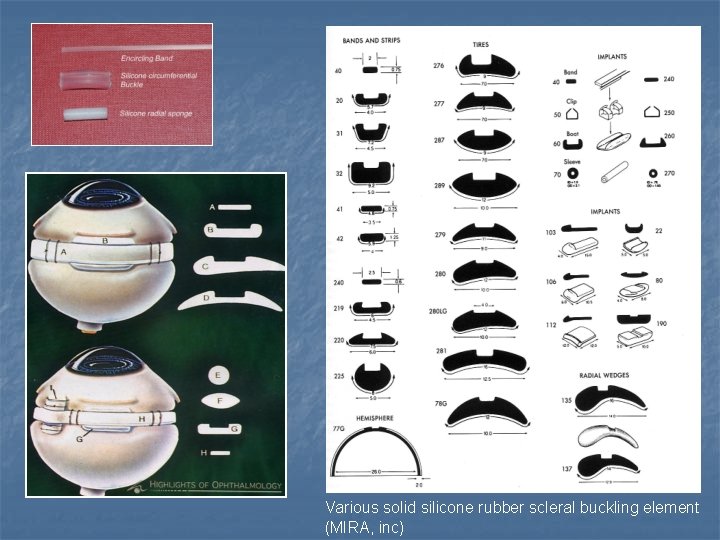
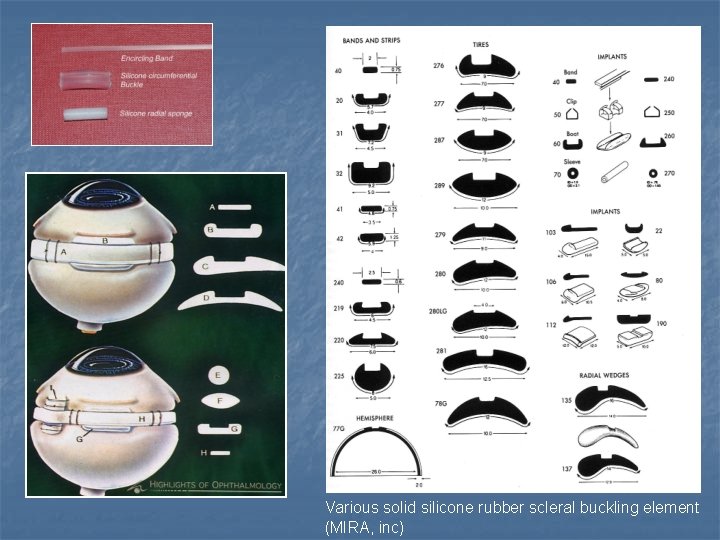
Various solid silicone rubber scleral buckling element (MIRA, inc)
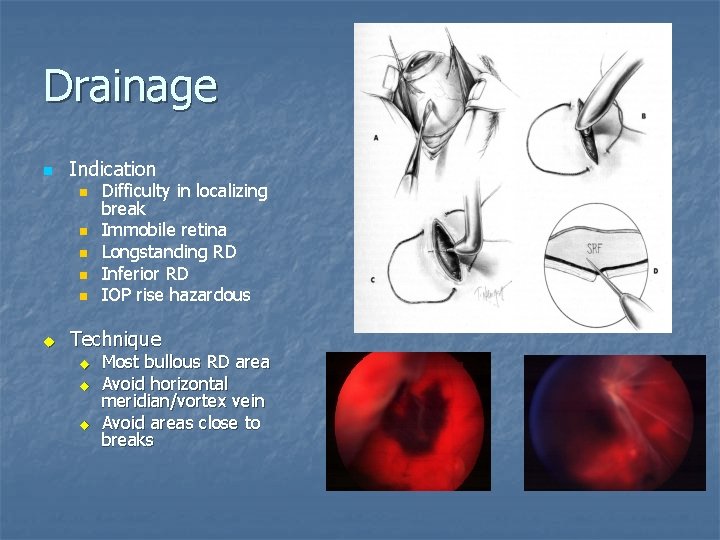
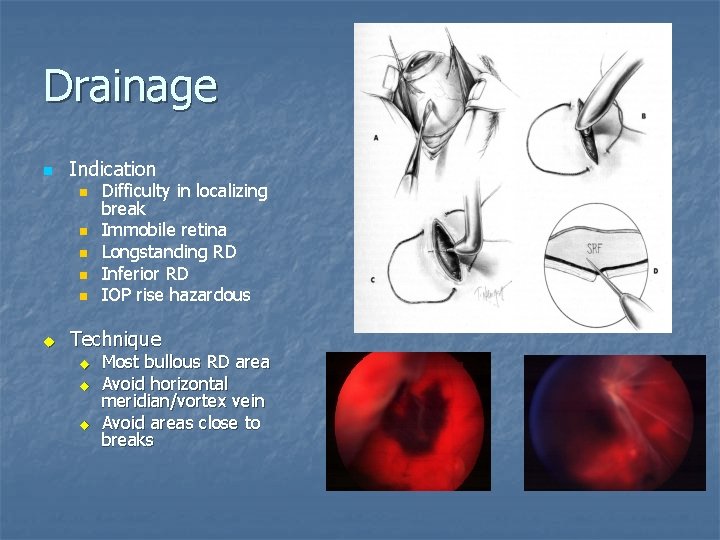
Drainage n Indication n n u Difficulty in localizing break Immobile retina Longstanding RD Inferior RD IOP rise hazardous Technique u u u Most bullous RD area Avoid horizontal meridian/vortex vein Avoid areas close to breaks
Special technique n “DACE” for very bullous RD Drainage n Air injection n Cryo n Explant n
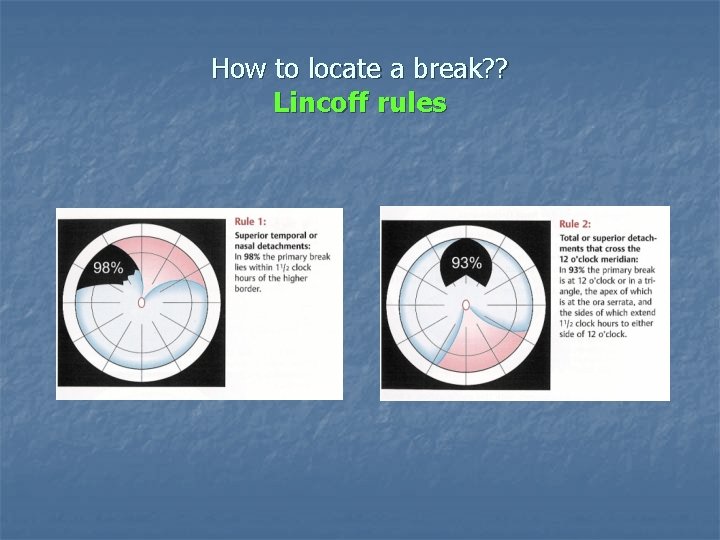
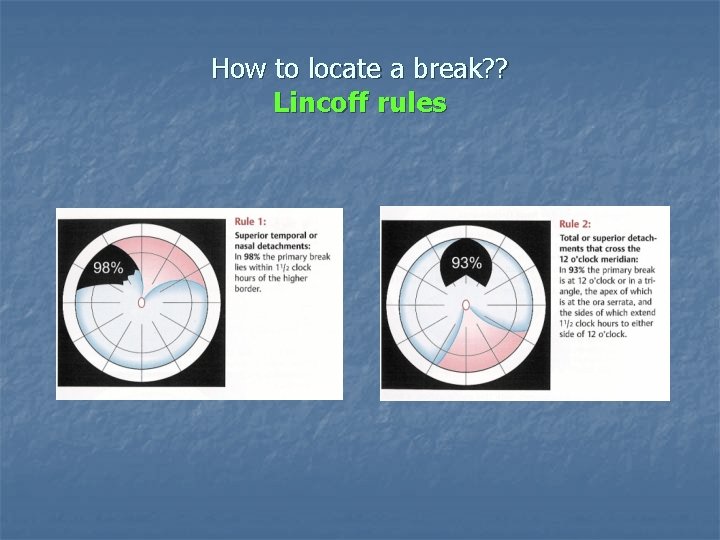
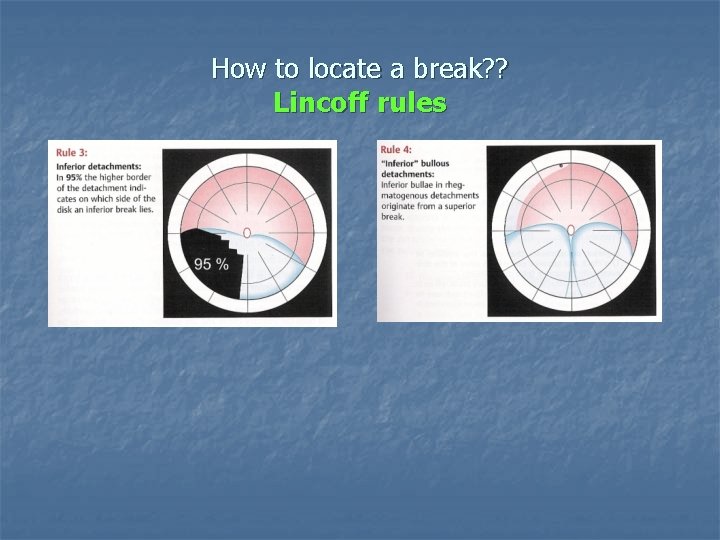
How to locate a break? ? Lincoff rules
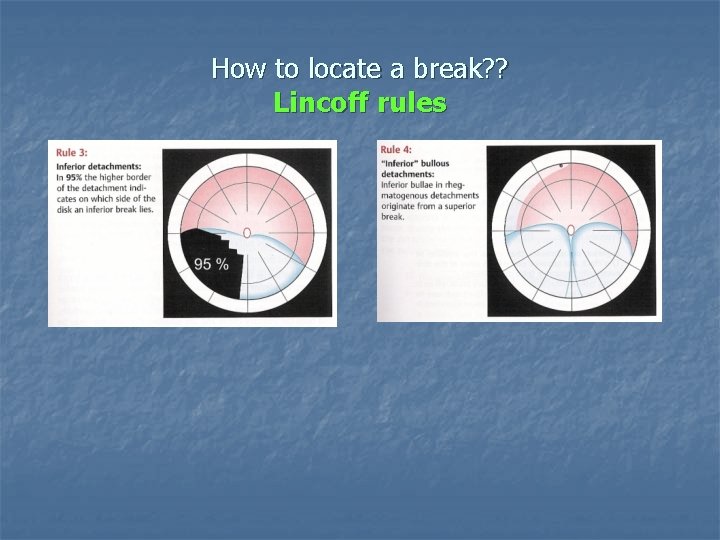
How to locate a break? ? Lincoff rules
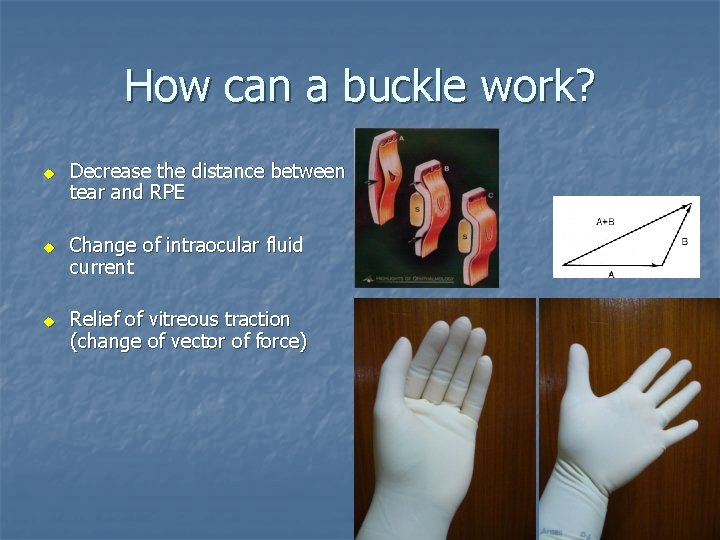
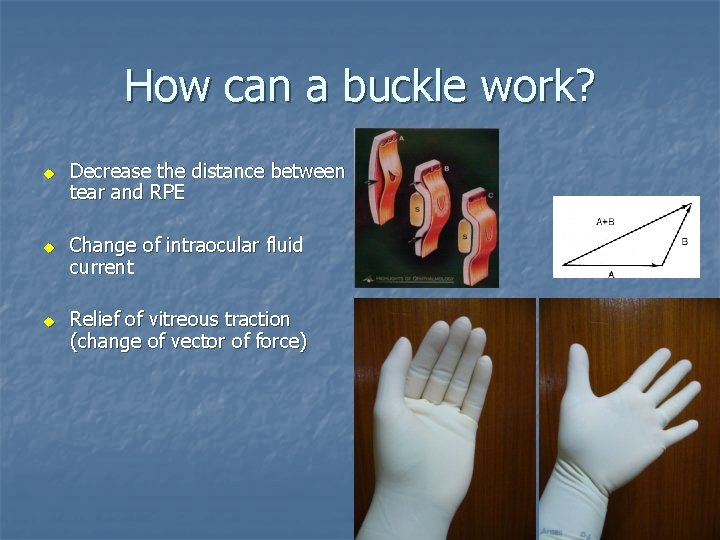
How can a buckle work? u u u Decrease the distance between tear and RPE Change of intraocular fluid current Relief of vitreous traction (change of vector of force)
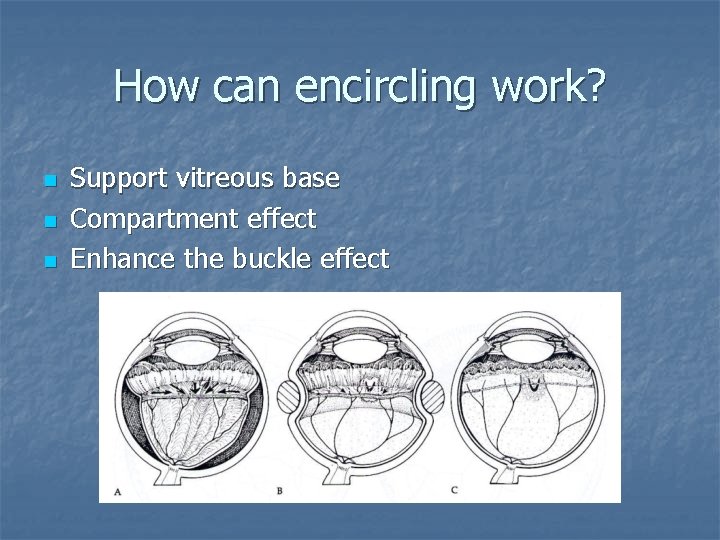
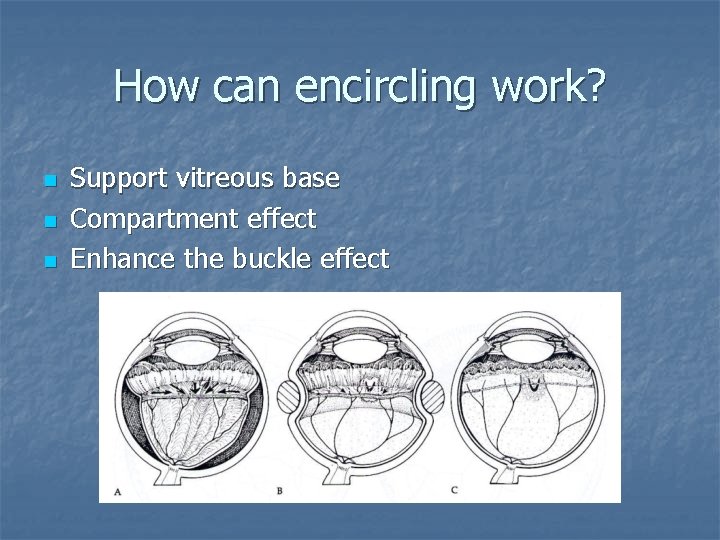
How can encircling work? n n n Support vitreous base Compartment effect Enhance the buckle effect
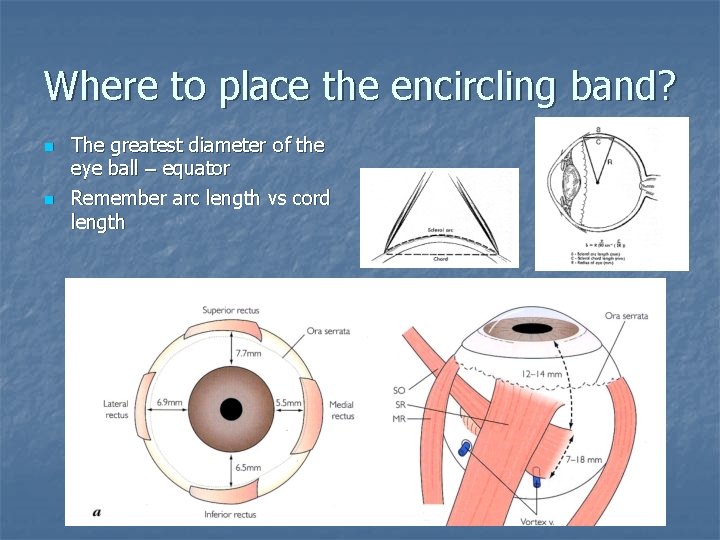
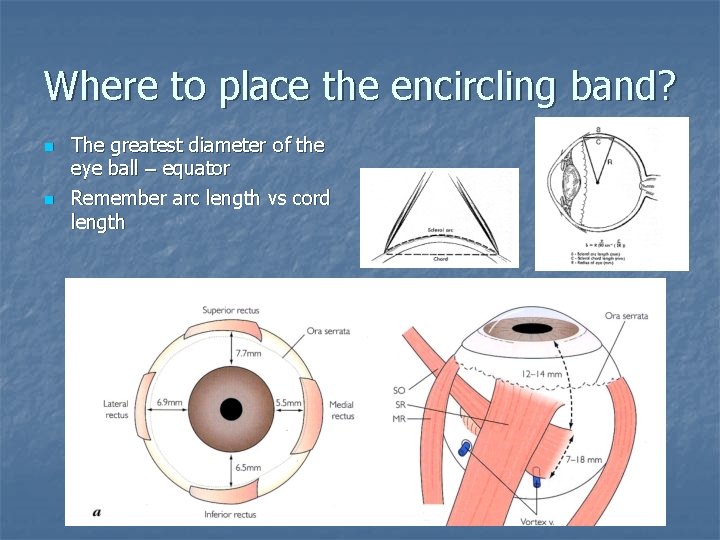
Where to place the encircling band? n n The greatest diameter of the eye ball – equator Remember arc length vs cord length
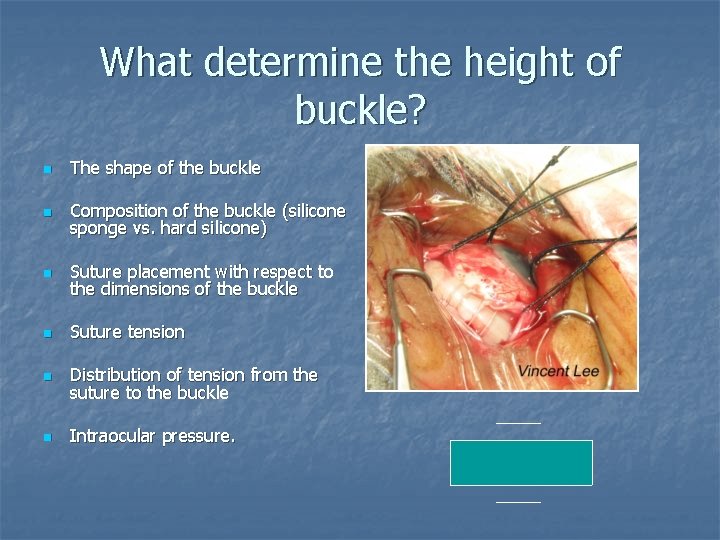
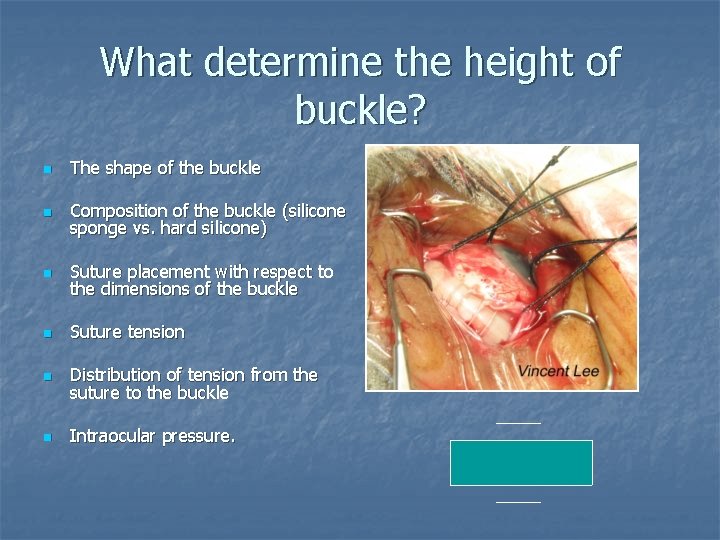
What determine the height of buckle? n The shape of the buckle n Composition of the buckle (silicone sponge vs. hard silicone) n Suture placement with respect to the dimensions of the buckle n Suture tension n Distribution of tension from the suture to the buckle n Intraocular pressure.
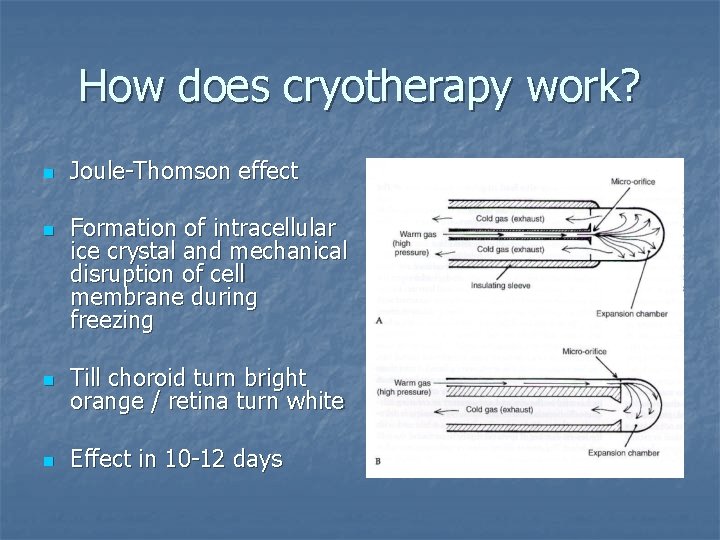
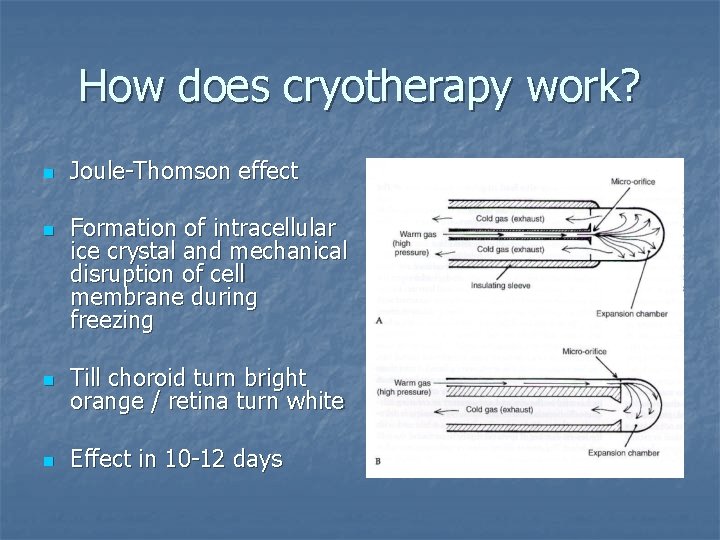
How does cryotherapy work? n n Joule-Thomson effect Formation of intracellular ice crystal and mechanical disruption of cell membrane during freezing n Till choroid turn bright orange / retina turn white n Effect in 10 -12 days

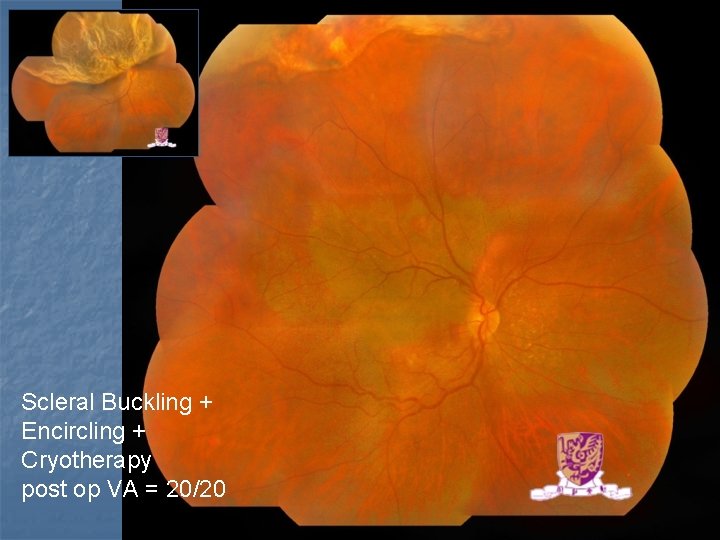
Macula on RRD pre op
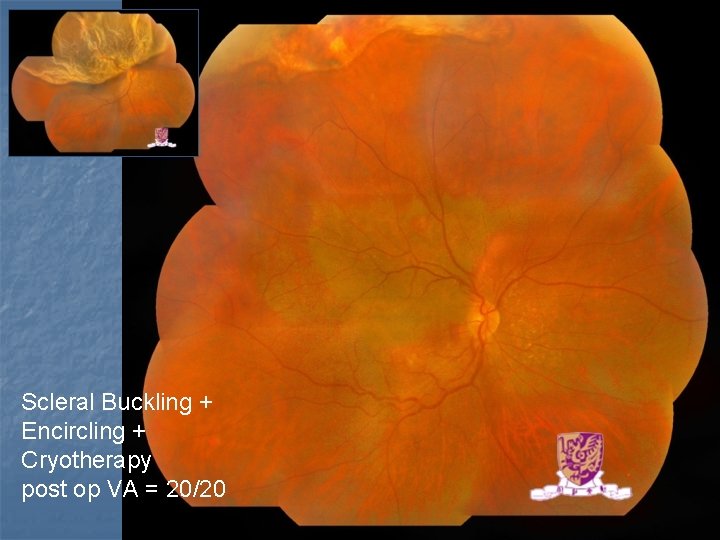
Scleral Buckling + Encircling + Cryotherapy post op VA = 20/20
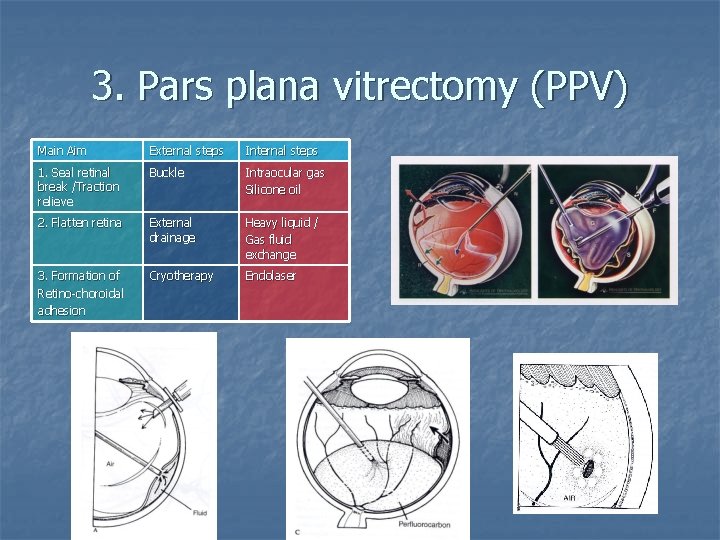
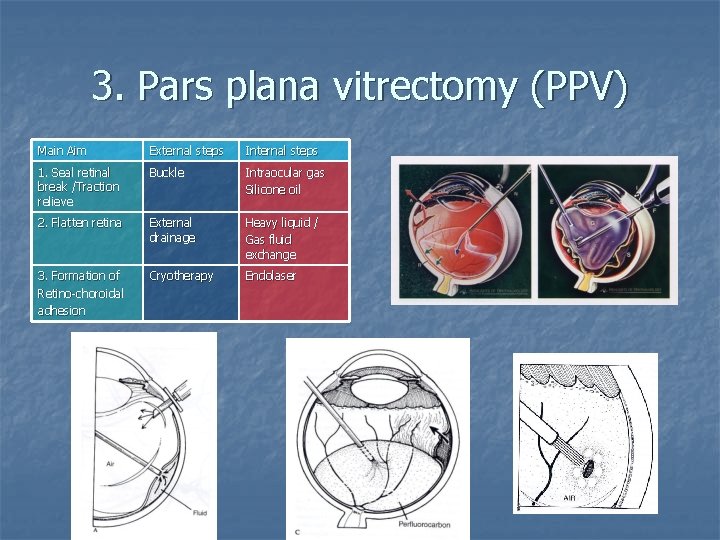
3. Pars plana vitrectomy (PPV) Main Aim External steps Internal steps 1. Seal retinal break /Traction relieve Buckle Intraocular gas Silicone oil 2. Flatten retina External drainage Heavy liquid / Gas fluid exchange 3. Formation of Retino-choroidal adhesion Cryotherapy Endolaser
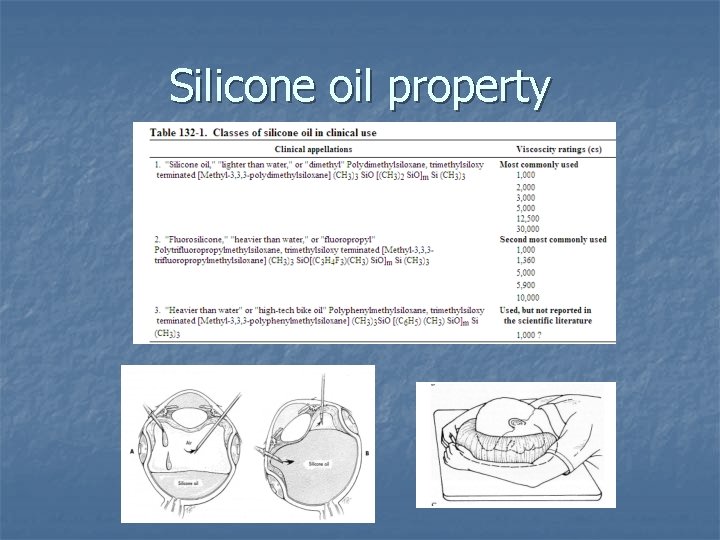
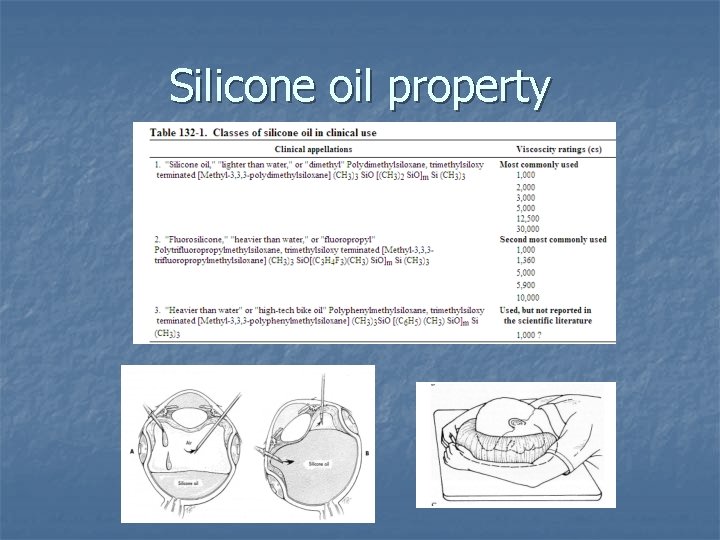
Silicone oil property
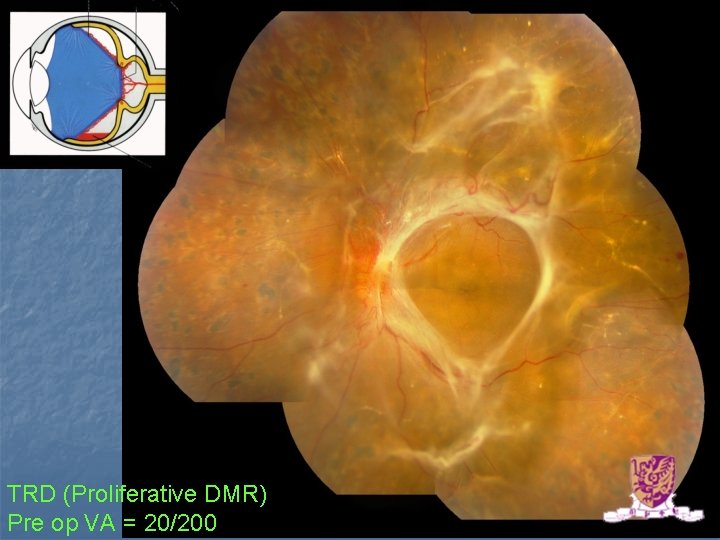
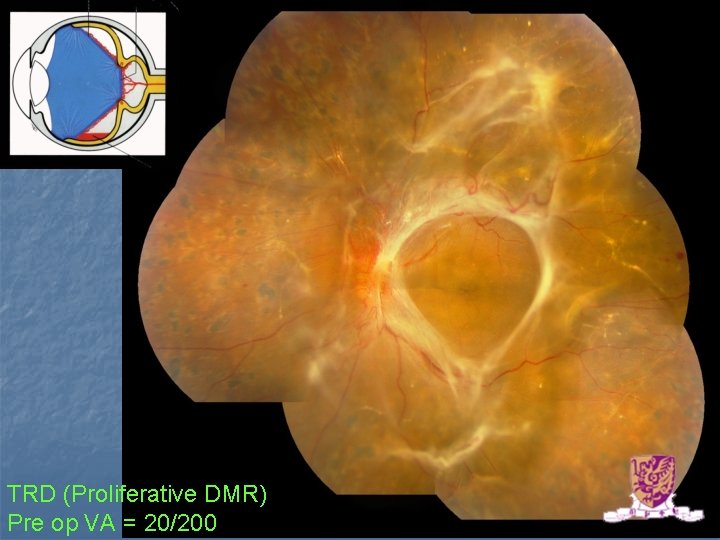
TRD (Proliferative DMR) Pre op VA = 20/200
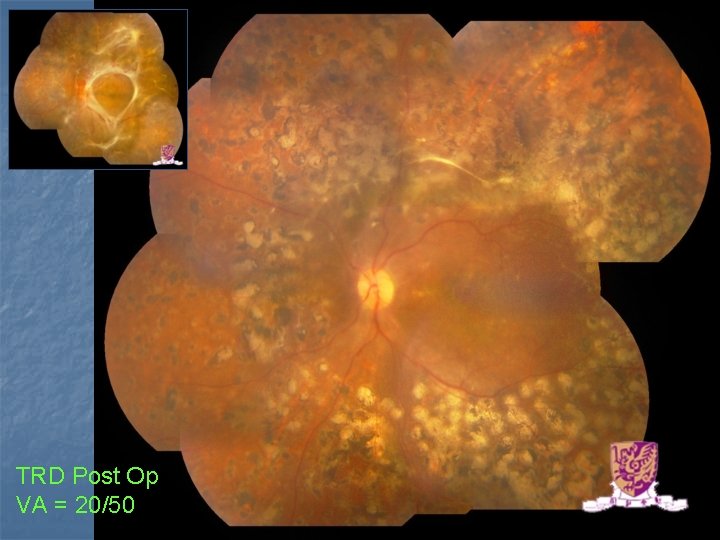
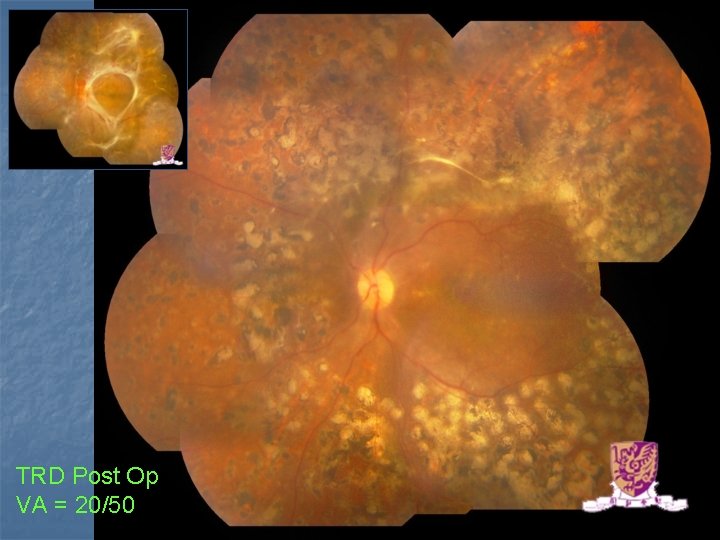
TRD Post Op VA = 20/50
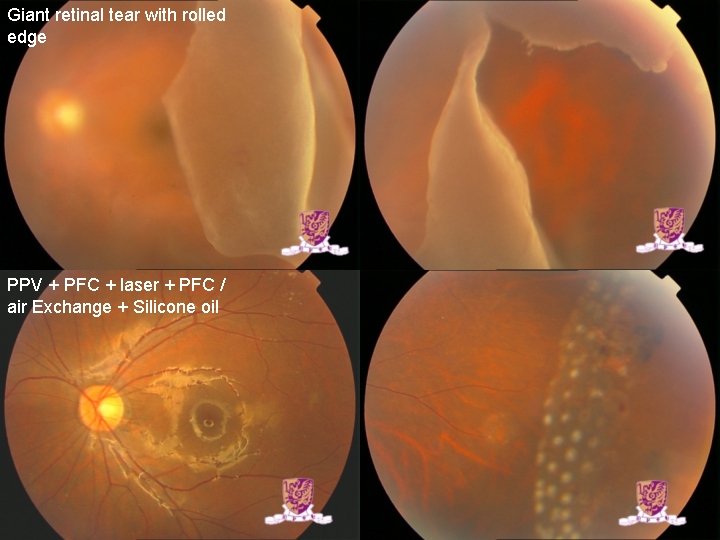
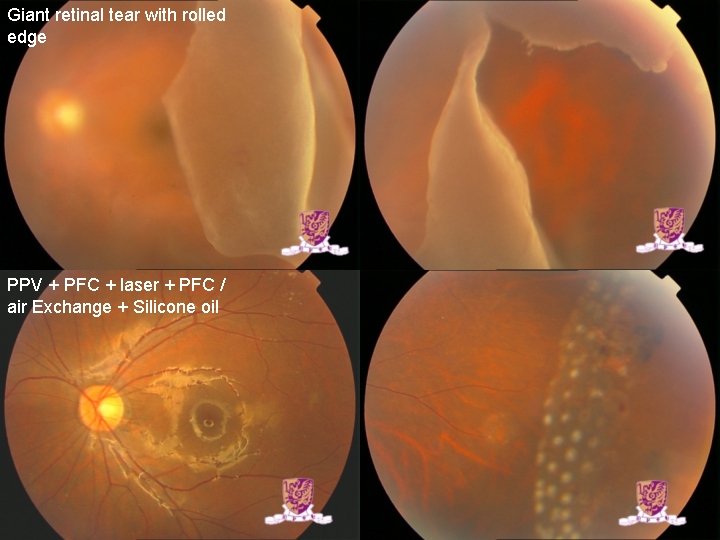
Giant retinal tear with rolled edge PPV + PFC + laser + PFC / air Exchange + Silicone oil