MANAGEMENT OF PERIAMPULLARY TUMOR WHAT ARE THE OPTIONS
- Slides: 32
MANAGEMENT OF PERIAMPULLARY TUMOR WHAT ARE THE OPTIONS FOR AMPULLARY ADENOMA? Joint Hospital Surgical Grand Round (July 2017) Presented by Dr. Sin Kar Yan, PMH
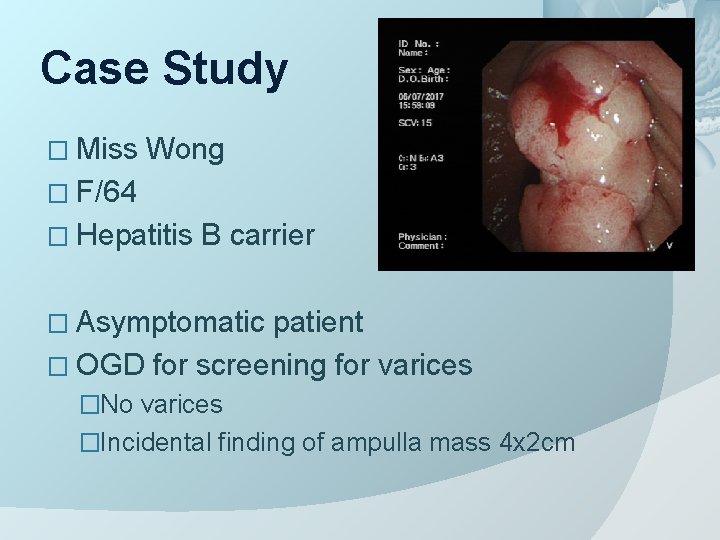
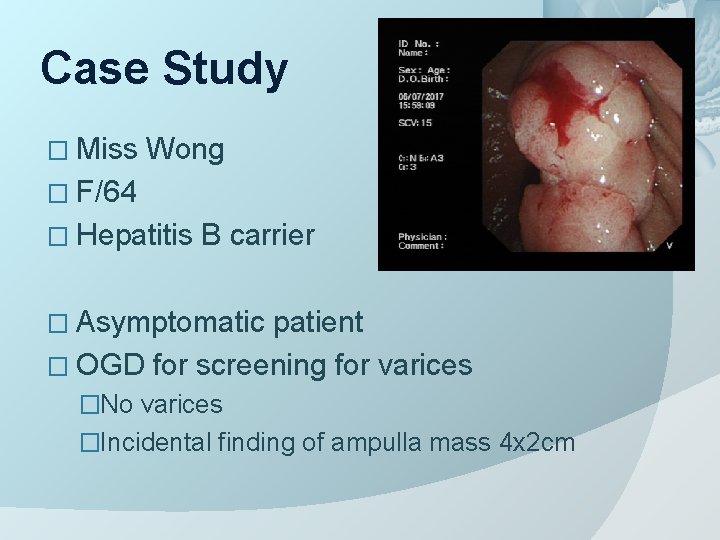
Case Study � Miss Wong � F/64 � Hepatitis B carrier � Asymptomatic patient � OGD for screening for varices �No varices �Incidental finding of ampulla mass 4 x 2 cm
Case Study Biopsy: Tubular adenoma � Hb normal � LFT normal � Referral to surgery What to do next?
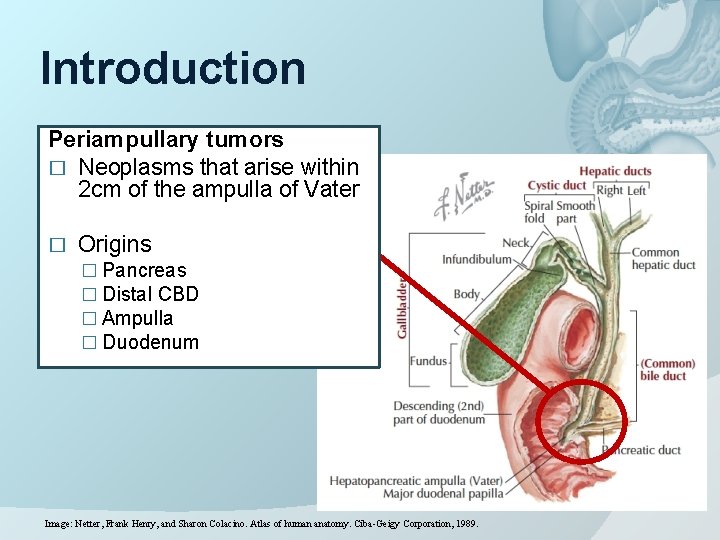
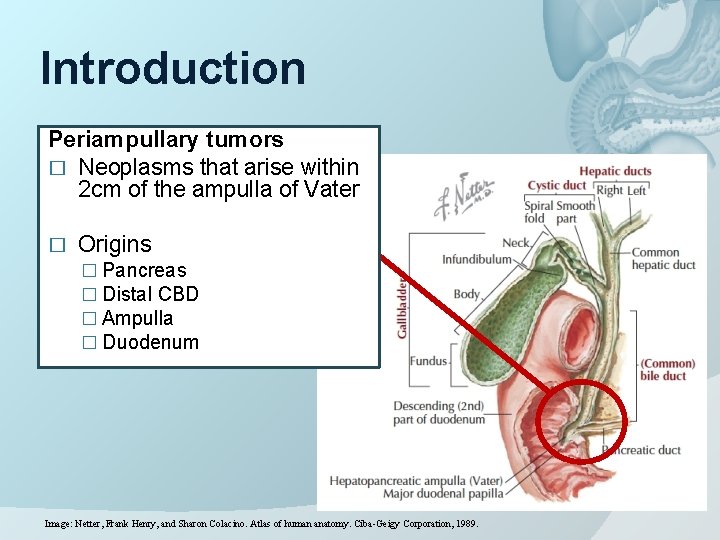
Introduction Periampullary tumors � Neoplasms that arise within 2 cm of the ampulla of Vater � Origins � Pancreas � Distal CBD � Ampulla � Duodenum Image: Netter, Frank Henry, and Sharon Colacino. Atlas of human anatomy. Ciba-Geigy Corporation, 1989.
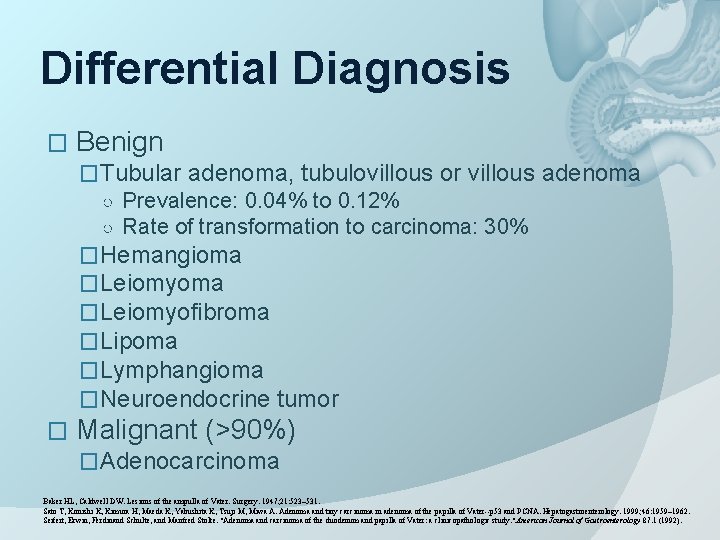
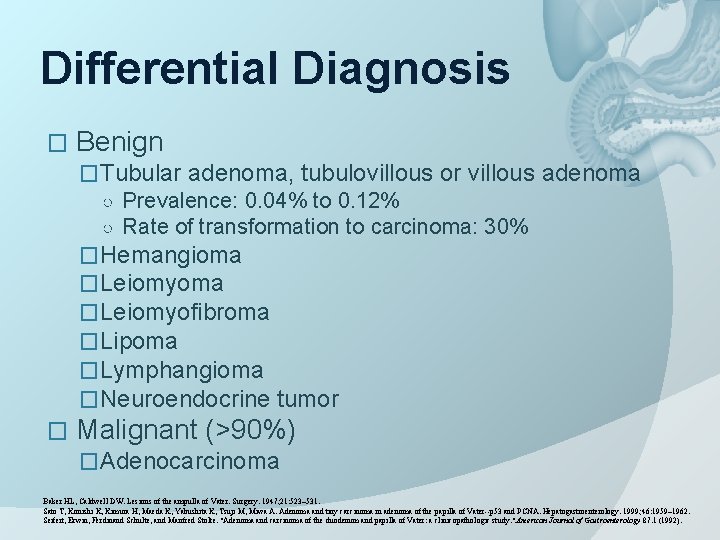
Differential Diagnosis � Benign �Tubular adenoma, tubulovillous or villous adenoma ○ Prevalence: 0. 04% to 0. 12% ○ Rate of transformation to carcinoma: 30% �Hemangioma �Leiomyofibroma �Lipoma �Lymphangioma �Neuroendocrine tumor � Malignant (>90%) �Adenocarcinoma Baker HL, Caldwell DW. Lesions of the ampulla of Vater. Surgery. 1947; 21: 523– 531. Sato T, Konishi K, Kimura H, Maeda K, Yabushita K, Tsuji M, Miwa A. Adenoma and tiny carcinoma in adenoma of the papilla of Vater--p 53 and PCNA. Hepatogastroenterology. 1999; 46: 1959– 1962. Seifert, Erwin, Ferdinand Schulte, and Manfred Stolte. "Adenoma and carcinoma of the duodenum and papilla of Vater: a clinicopathologic study. " American Journal of Gastroenterology 87. 1 (1992).
Presentations of Periampullary Tumors � Asymptomatic as incidental finding � Symptomatic �Jaundice �Abdominal pain �Palpable gallbladder �Acute pancreatitis �UGIB / obstruction
Investigations � Blood investigations �Complete blood count �Liver function test �CA 19. 9 � Imaging and endoscopy �Ultrasound �CT �MRCP �Duodenoscopy �ERCP �EUS
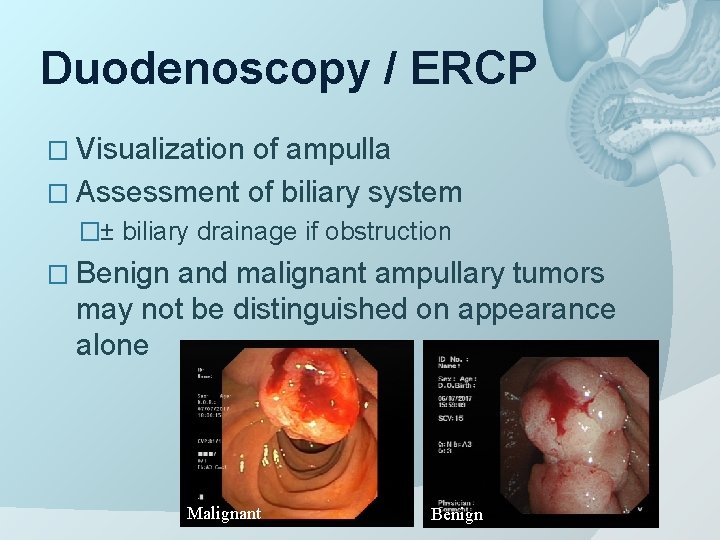
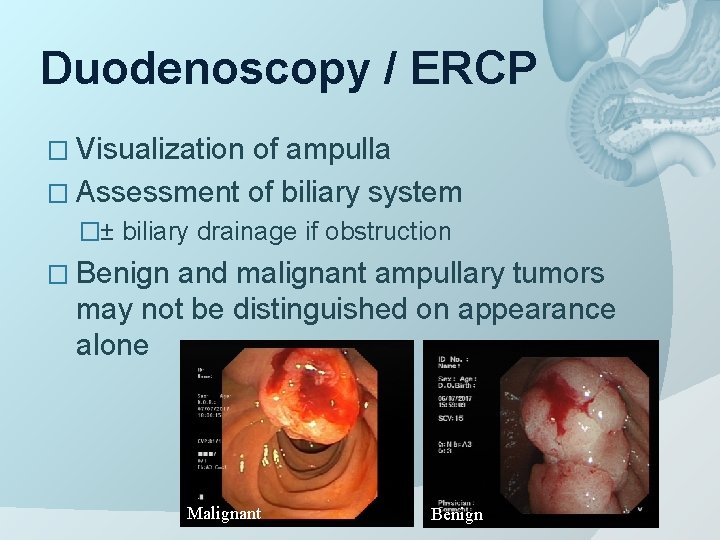
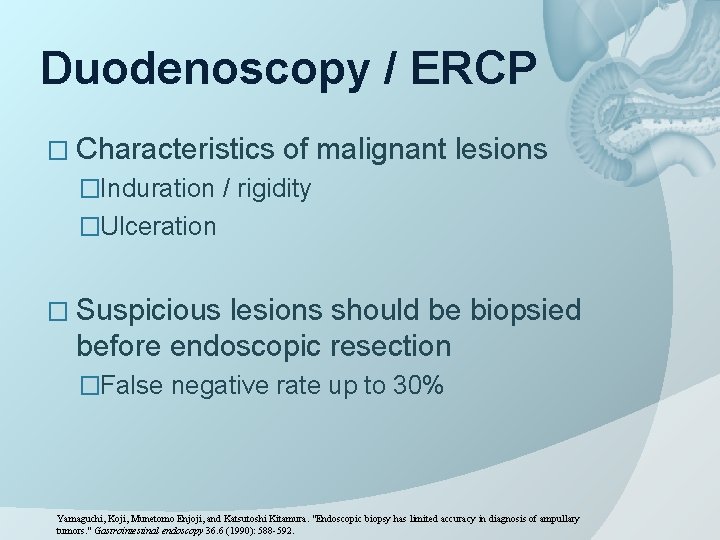
Duodenoscopy / ERCP � Visualization of ampulla � Assessment of biliary system �± biliary drainage if obstruction � Benign and malignant ampullary tumors may not be distinguished on appearance alone Malignant Benign
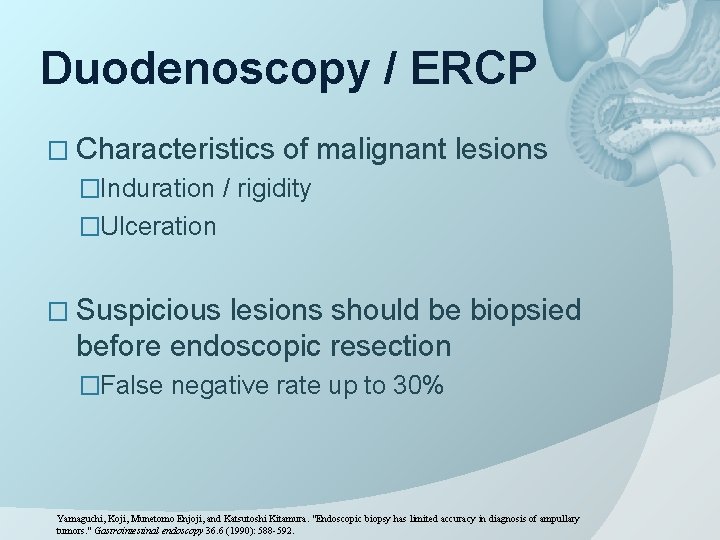
Duodenoscopy / ERCP � Characteristics of malignant lesions �Induration / rigidity �Ulceration � Suspicious lesions should be biopsied before endoscopic resection �False negative rate up to 30% Yamaguchi, Koji, Munetomo Enjoji, and Katsutoshi Kitamura. "Endoscopic biopsy has limited accuracy in diagnosis of ampullary tumors. " Gastrointestinal endoscopy 36. 6 (1990): 588 -592.
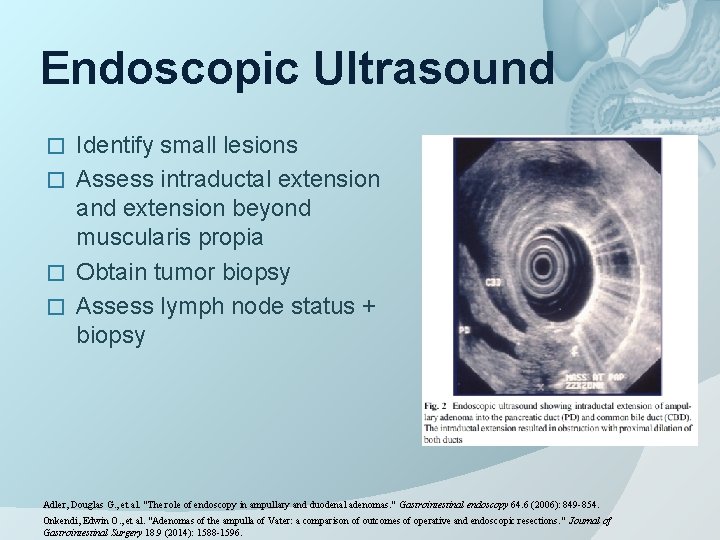
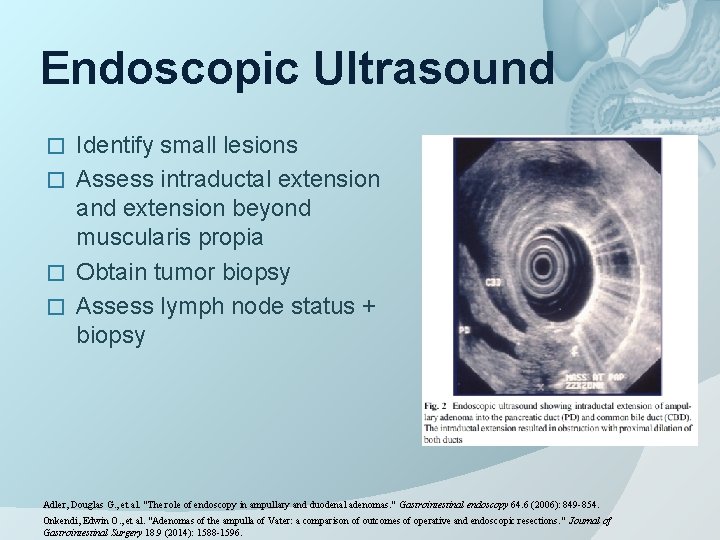
Endoscopic Ultrasound Identify small lesions � Assess intraductal extension and extension beyond muscularis propia � Obtain tumor biopsy � Assess lymph node status + biopsy � Adler, Douglas G. , et al. "The role of endoscopy in ampullary and duodenal adenomas. " Gastrointestinal endoscopy 64. 6 (2006): 849 -854. Onkendi, Edwin O. , et al. "Adenomas of the ampulla of Vater: a comparison of outcomes of operative and endoscopic resections. " Journal of Gastrointestinal Surgery 18. 9 (2014): 1588 -1596.
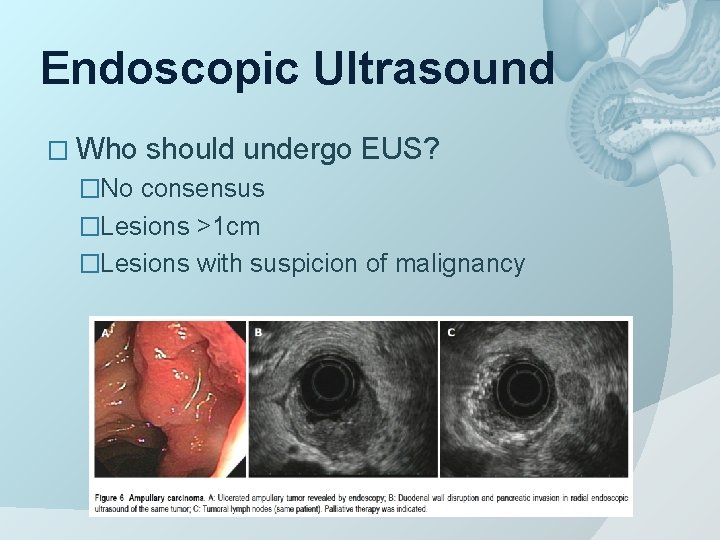
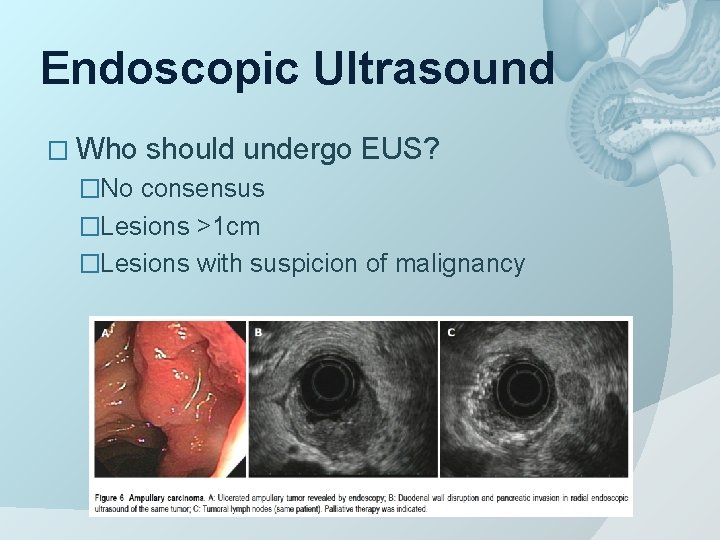
Endoscopic Ultrasound � Who should undergo EUS? �No consensus �Lesions >1 cm �Lesions with suspicion of malignancy
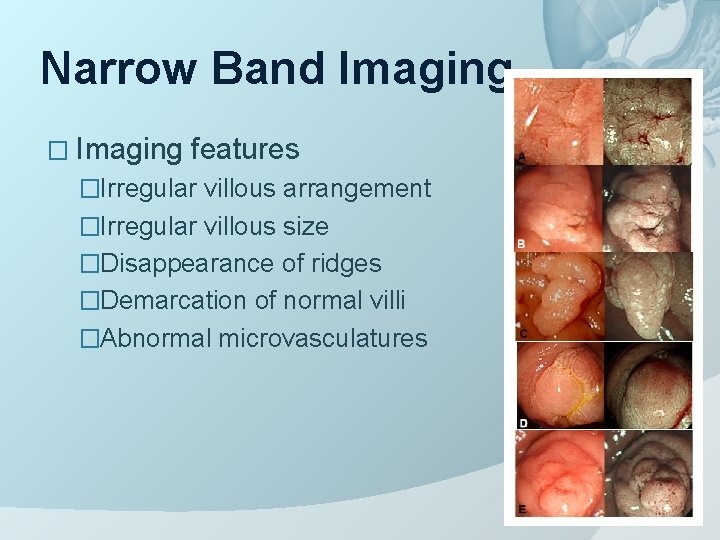
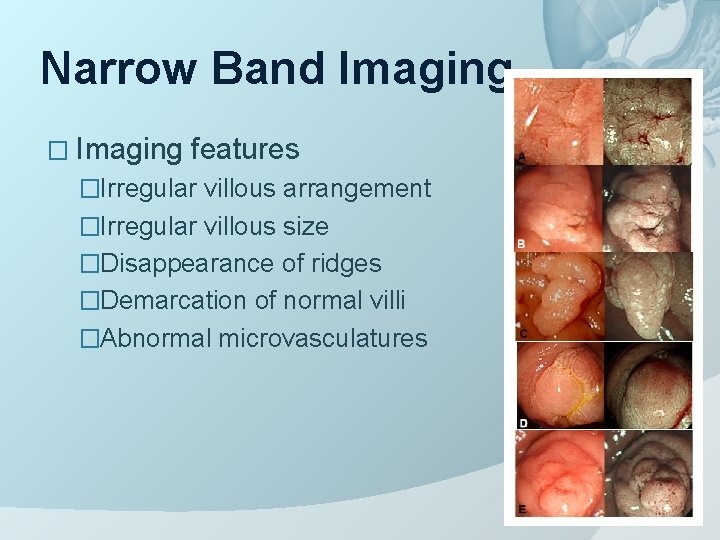
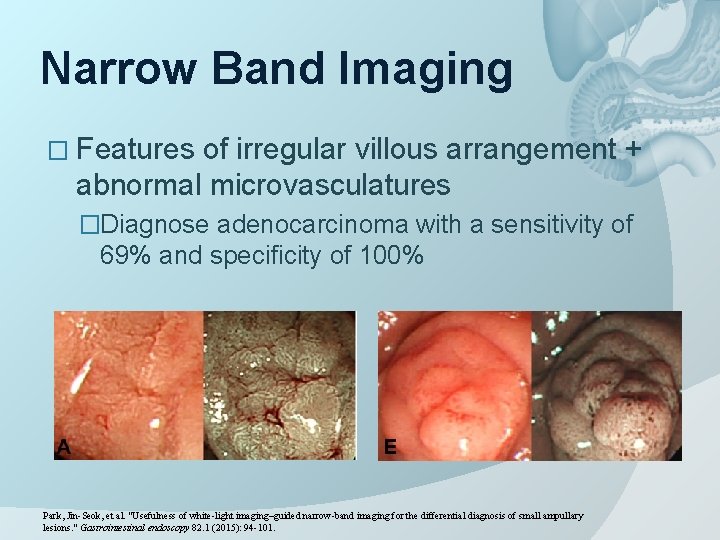
Narrow Band Imaging � Imaging features �Irregular villous arrangement �Irregular villous size �Disappearance of ridges �Demarcation of normal villi �Abnormal microvasculatures
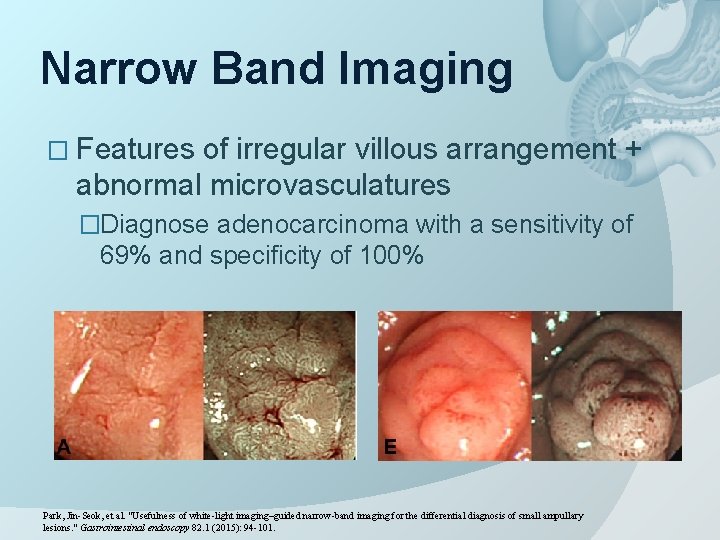
Narrow Band Imaging � Features of irregular villous arrangement + abnormal microvasculatures �Diagnose adenocarcinoma with a sensitivity of 69% and specificity of 100% Park, Jin-Seok, et al. "Usefulness of white-light imaging–guided narrow-band imaging for the differential diagnosis of small ampullary lesions. " Gastrointestinal endoscopy 82. 1 (2015): 94 -101.
Narrow Band Imaging � Guide � Not target biopsy site suitable as a screening tool due to the low sensitivity � Role of NBI is still being investigated � Large scale prospective study is required
Treatment: Ampullectomy
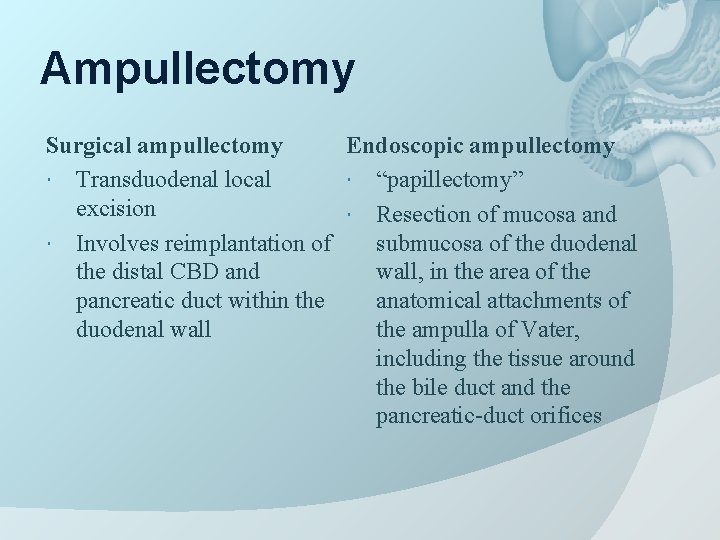
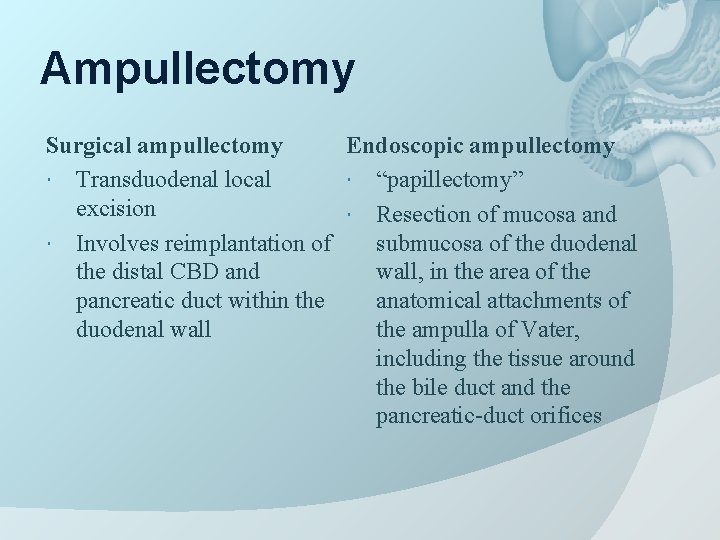
Ampullectomy Surgical ampullectomy Endoscopic ampullectomy Transduodenal local “papillectomy” excision Resection of mucosa and Involves reimplantation of submucosa of the duodenal the distal CBD and wall, in the area of the pancreatic duct within the anatomical attachments of duodenal wall the ampulla of Vater, including the tissue around the bile duct and the pancreatic-duct orifices
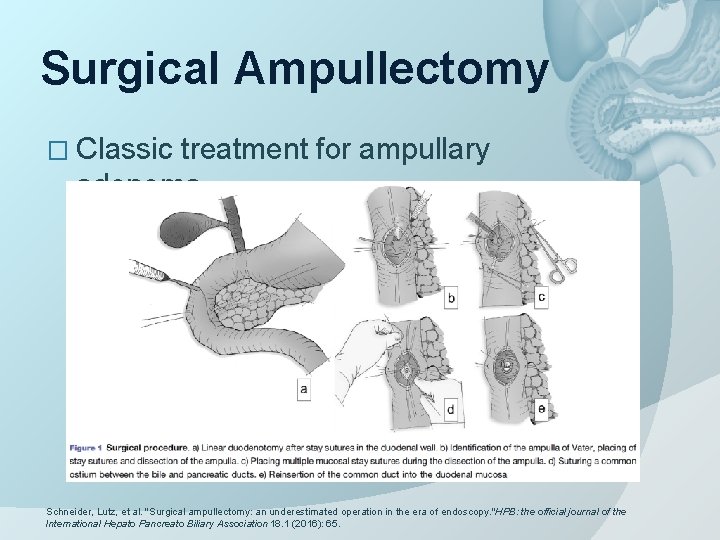
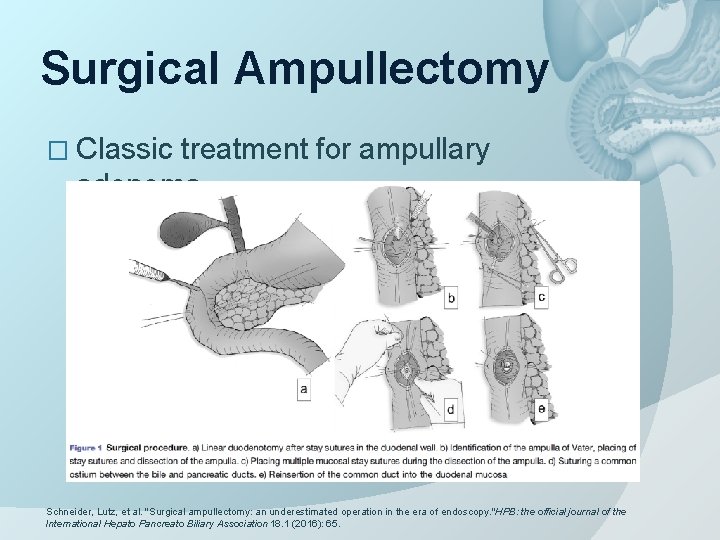
Surgical Ampullectomy � Classic treatment for ampullary adenoma Schneider, Lutz, et al. "Surgical ampullectomy: an underestimated operation in the era of endoscopy. "HPB: the official journal of the International Hepato Pancreato Biliary Association 18. 1 (2016): 65.
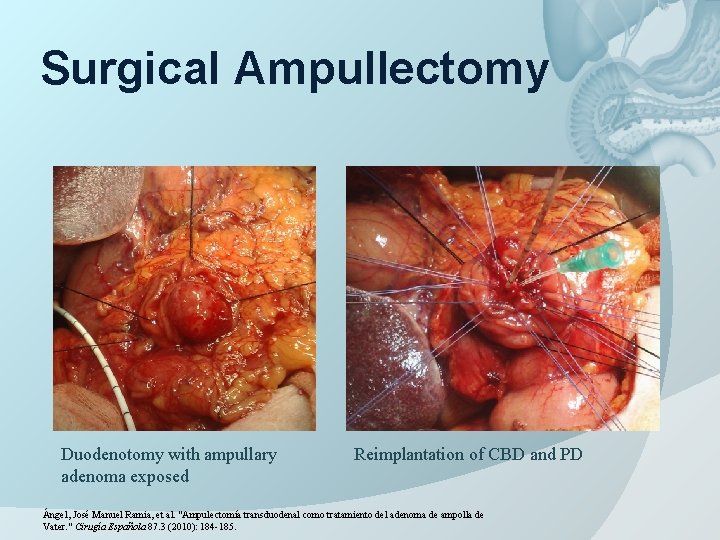
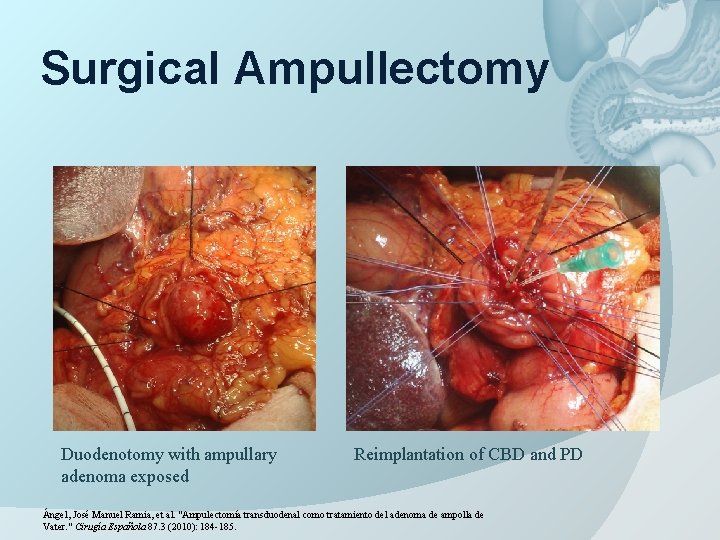
Surgical Ampullectomy Duodenotomy with ampullary adenoma exposed Reimplantation of CBD and PD Ángel, José Manuel Ramia, et al. "Ampulectomía transduodenal como tratamiento del adenoma de ampolla de Vater. " Cirugía Española 87. 3 (2010): 184 -185.
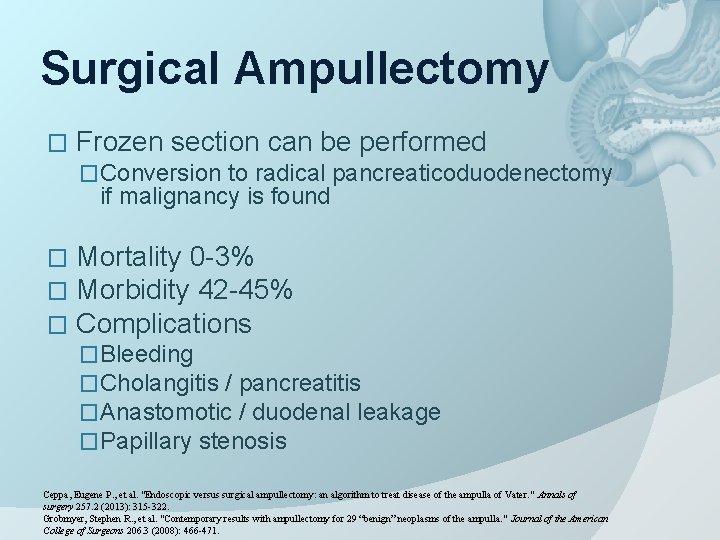
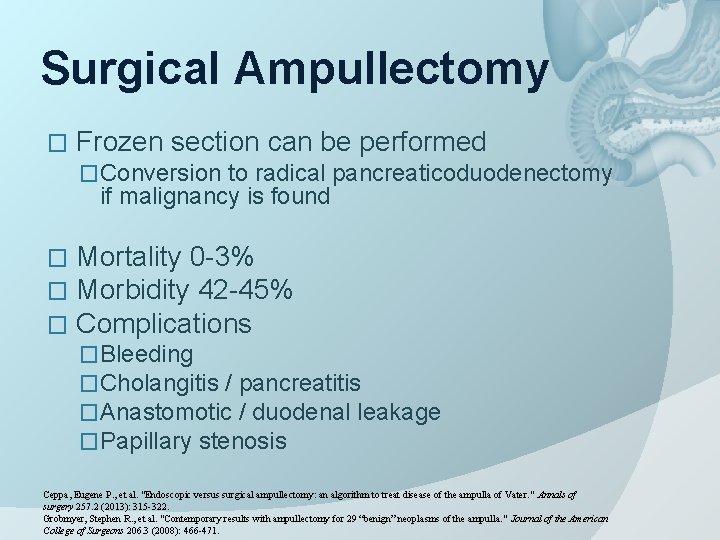
Surgical Ampullectomy � Frozen section can be performed �Conversion to radical pancreaticoduodenectomy if malignancy is found � � � Mortality 0 -3% Morbidity 42 -45% Complications �Bleeding �Cholangitis / pancreatitis �Anastomotic / duodenal leakage �Papillary stenosis Ceppa, Eugene P. , et al. "Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. " Annals of surgery 257. 2 (2013): 315 -322. Grobmyer, Stephen R. , et al. "Contemporary results with ampullectomy for 29 “benign” neoplasms of the ampulla. " Journal of the American College of Surgeons 206. 3 (2008): 466 -471.
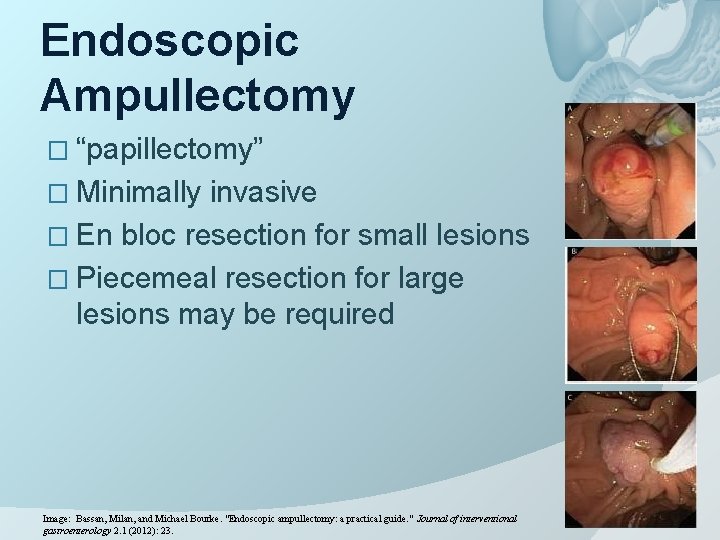
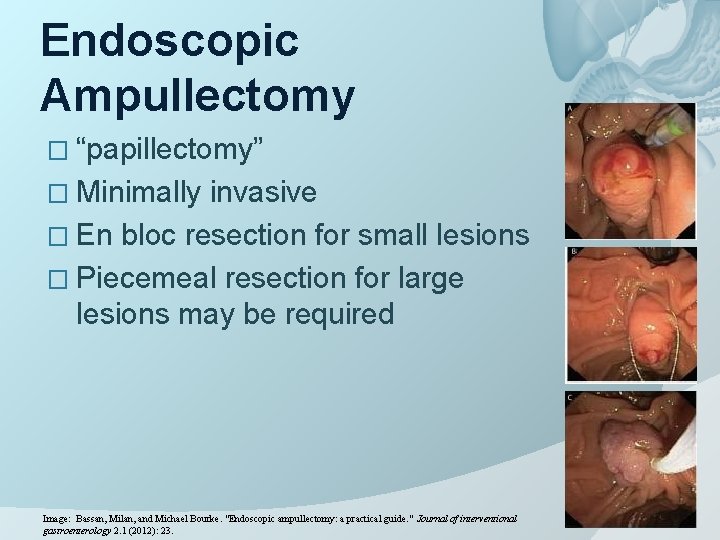
Endoscopic Ampullectomy � “papillectomy” � Minimally invasive � En bloc resection for small lesions � Piecemeal resection for large lesions may be required Image: Bassan, Milan, and Michael Bourke. "Endoscopic ampullectomy: a practical guide. " Journal of interventional gastroenterology 2. 1 (2012): 23.
Endoscopic Ampullectomy � Patient selection �Lesion <4 -5 cm �Histology ○ Benign ○ High grade dysplasia is not a contraindication �EUS criteria ○ No invasion of duodenal muscularis propia ○ No tumor growth beyond 1 cm inside CBD / pancreatic duct �Positive lifting sign
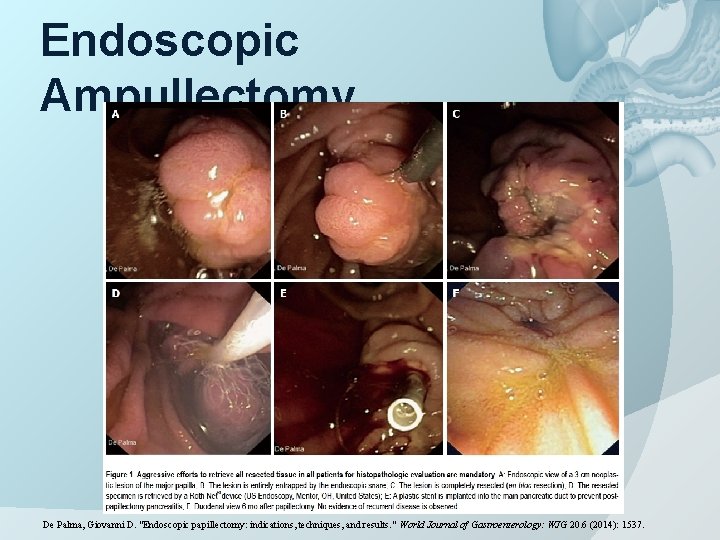
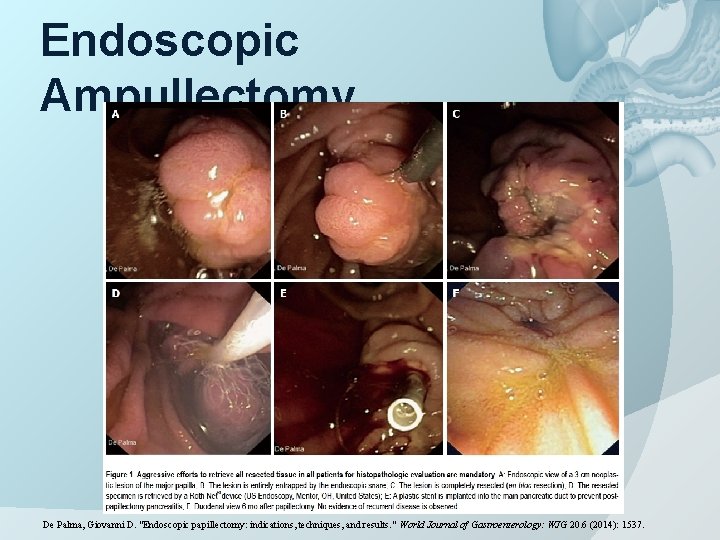
Endoscopic Ampullectomy De Palma, Giovanni D. "Endoscopic papillectomy: indications, techniques, and results. " World Journal of Gastroenterology: WJG 20. 6 (2014): 1537.
Endoscopic Ampullectomy � Techniques � Submucosal injection ○ Lift sign � Endoscopic snare and electrocautery � En bloc resection for small lesions � Piecemeal resection or multiple procedures may be required for larger lesions ○ Electrocautery injuries to tissue fragments can affect pathological analysis � Ablation (Argon plasma coagulation) if any residual lesion � Sphincterotomy ○ Helps pancreaticobiliary drainage after papillectomy � Stent placement ○ Not routine ○ Aim to prevent iatrogenic pancreatitis
Endoscopic Ampullectomy � Multiple sessions may be required Mortality 0% � Morbidity 18% � Complications � � Early: Pancreatitis, cholangitis, bleeding, perforation � Late: Papillary stenosis � Post-ampullectomy surveillance endoscopy required � 3 -12 months for at least 2 years � More frequently in case of high grade dysplasia Ceppa, Eugene P. , et al. "Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. " Annals of surgery 257. 2 (2013): 315 -322.
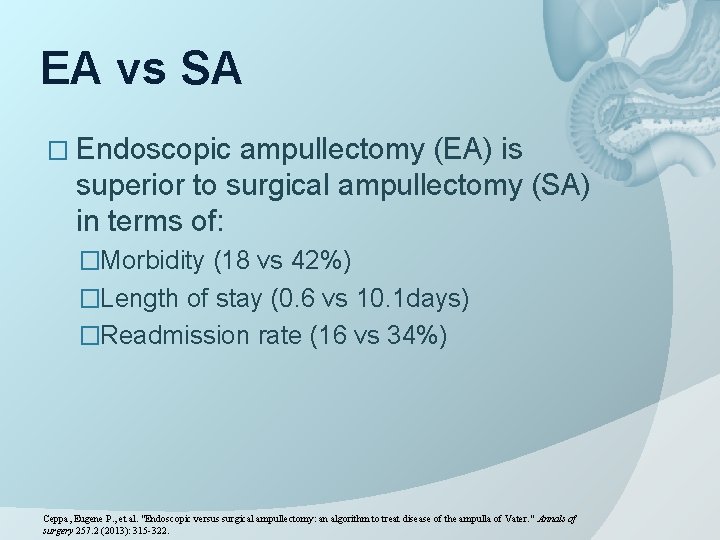
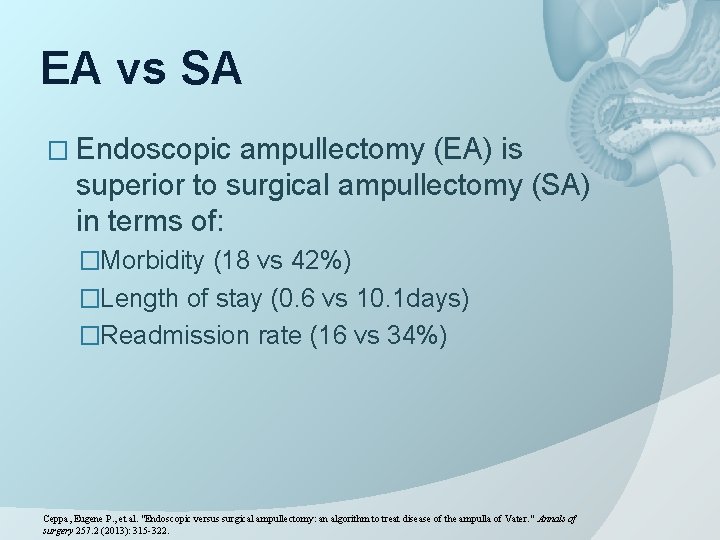
EA vs SA � Endoscopic ampullectomy (EA) is superior to surgical ampullectomy (SA) in terms of: �Morbidity (18 vs 42%) �Length of stay (0. 6 vs 10. 1 days) �Readmission rate (16 vs 34%) Ceppa, Eugene P. , et al. "Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. " Annals of surgery 257. 2 (2013): 315 -322.
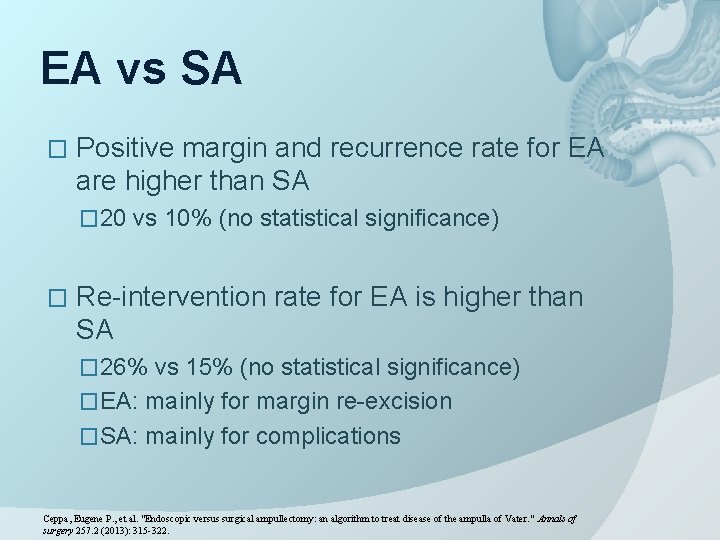
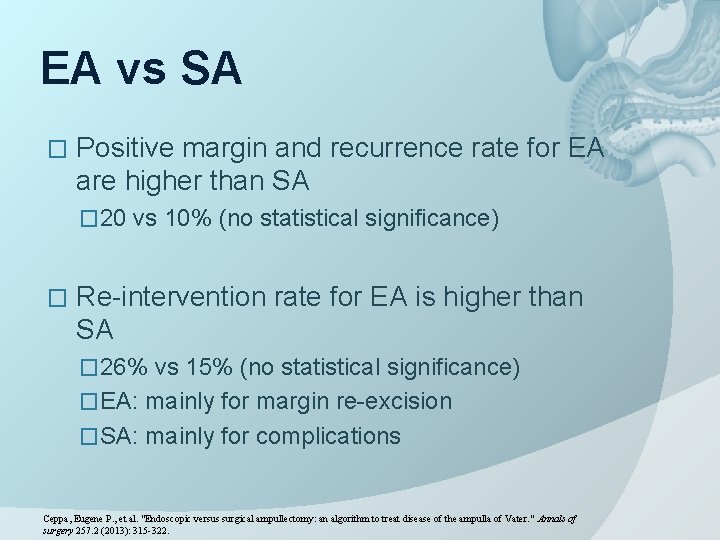
EA vs SA � Positive margin and recurrence rate for EA are higher than SA � 20 vs 10% (no statistical significance) � Re-intervention rate for EA is higher than SA � 26% vs 15% (no statistical significance) �EA: mainly for margin re-excision �SA: mainly for complications Ceppa, Eugene P. , et al. "Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. " Annals of surgery 257. 2 (2013): 315 -322.
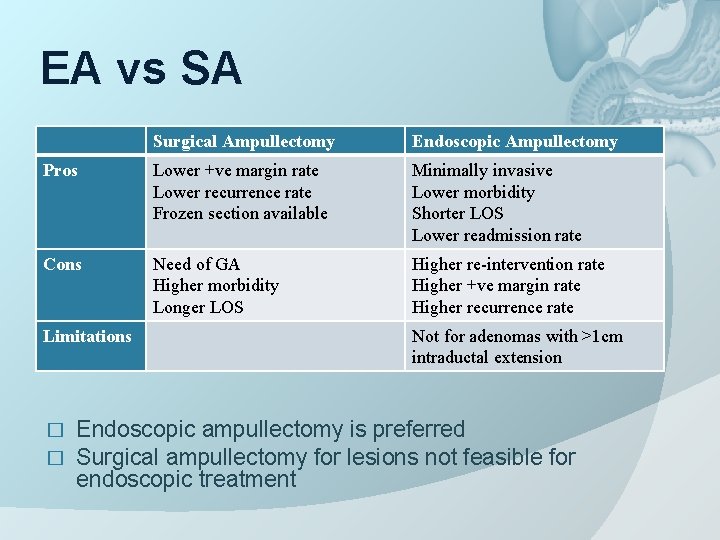
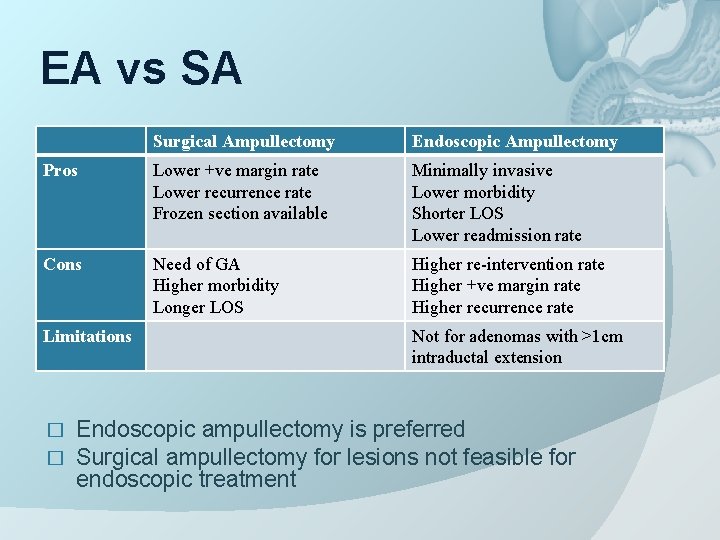
EA vs SA Surgical Ampullectomy Endoscopic Ampullectomy Pros Lower +ve margin rate Lower recurrence rate Frozen section available Minimally invasive Lower morbidity Shorter LOS Lower readmission rate Cons Need of GA Higher morbidity Longer LOS Higher re-intervention rate Higher +ve margin rate Higher recurrence rate Limitations � � Not for adenomas with >1 cm intraductal extension Endoscopic ampullectomy is preferred Surgical ampullectomy for lesions not feasible for endoscopic treatment
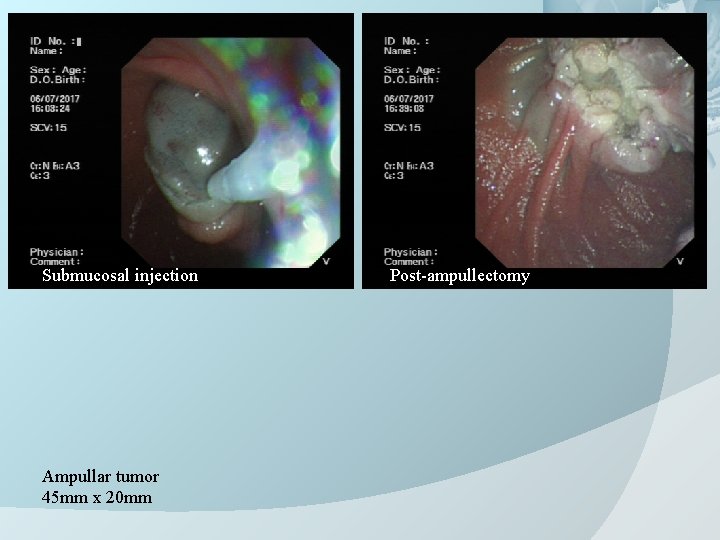
Back to our patient… � EUS + endoscopic ampullectomy done � 4. 5 cm lateral spreading ampulla tumor ○ No intraductal extension � Ampullectomy performed � CBD stent and pancreatic ductal stent inserted
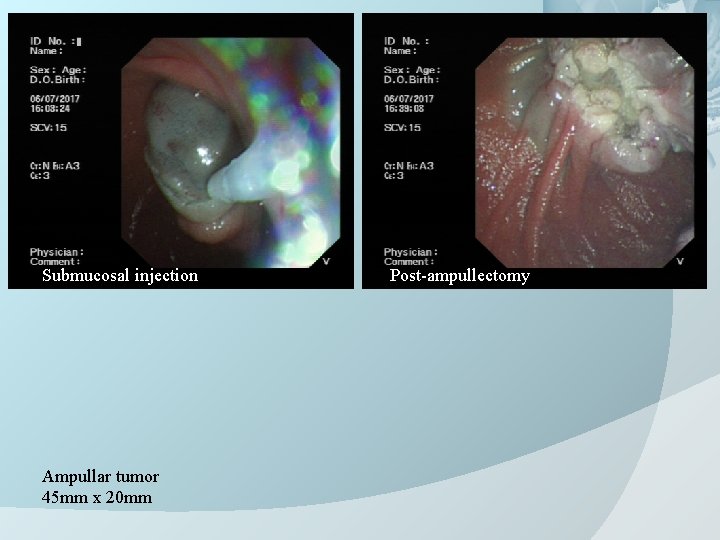
Submucosal injection Ampullar tumor 45 mm x 20 mm Post-ampullectomy
Back to our patient… � Post-operative course was uneventful � Diet was resumed on the next day � No fever � LFT normal � Discharge home on day 4 � Pathology: � Tubulovillous adenoma with low grade dysplasia � Lateral margin clear � Plan for surveillance endoscopy 3 months later
Conclusions Ampullary adenomas are rare EUS has an important role in management decision � NBI may help improve diagnostic accuracy � � � More study would be needed to assess its efficacy � Endoscopic ampullectomy is a more favorable option than surgical ampullectomy � Minimally invasive, avoid GA � Lower morbidity � But the positive margin and recurrence rates are higher � Surgical ampullectomy � Treatment choice when EA is not feasible
The End