Management of Patients with Cerebrovascular Disorders Cerebrovascular Disorders
Management of Patients with Cerebrovascular Disorders
Cerebrovascular Disorders • Functional abnormality of the CNS that occurs when the blood supply is disrupted • Stroke is the primary cerebrovascular disorder and the third leading cause of death in the U. S. • Stroke is the leading cause of serious longterm disability in the U. S.
Prevention • Nonmodifiable risk factors – Age (over 55), male gender, African-American race • Modifiable risk factors – Hypertension is the primary risk factor – Cardiovascular disease – Elevated cholesterol or elevated hematocrit – Obesity – Diabetes – Oral contraceptive use – Smoking and drug and alcohol abuse
Stroke • “Brain attack” • Sudden loss of function resulting from a disruption of the blood supply to a part of the brain • Types of stroke – Ischemic (80– 85%) – Hemorrhagic (15– 20%)
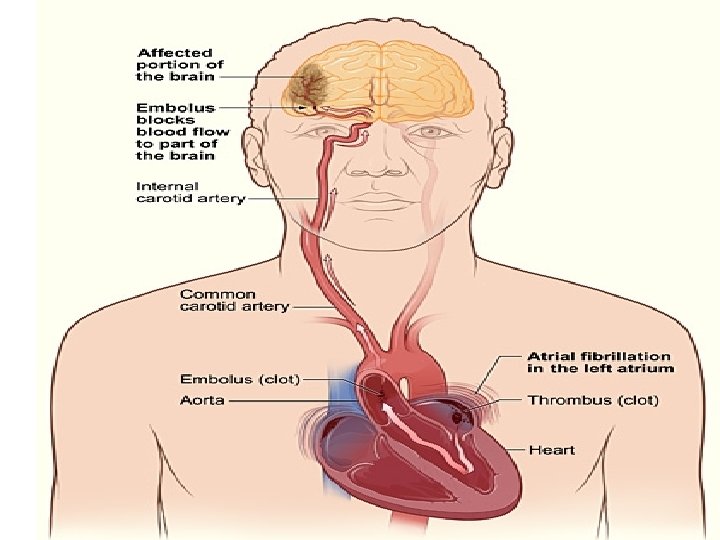
Ischemic Stroke • Disruption of the blood supply due to an obstruction, usually a thrombus or embolism, that causes infarction of brain tissue • Types – Large artery thrombosis – Small penetrating artery thrombosis – Cardiogenic embolism – Cryptogenic – Other
Other causes of ischemic stroke • Cerebral arterial spasm- caused by irritation decreased bld flow to brain • Hypercoagulable state- -- thrombosis & ischemic stroke • Compression of cerebral vessels-from tumor, large clot, brain abscess
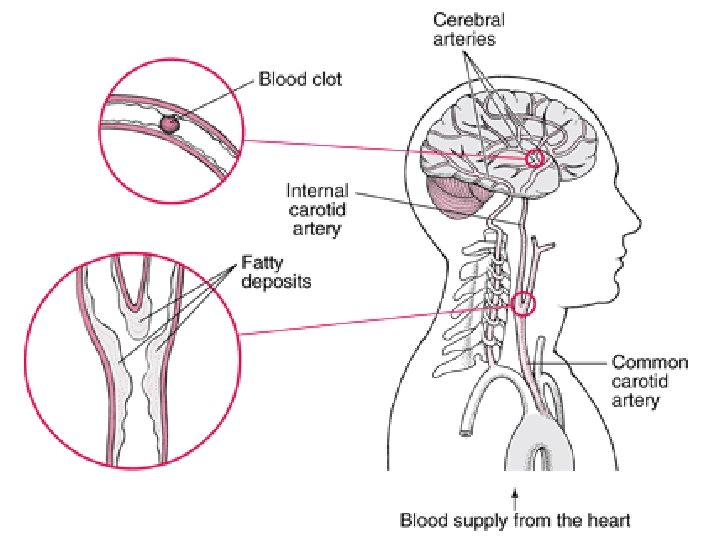
Pathophysiology p. 1897 Brunner , . . • Refer to fig. 62 -1
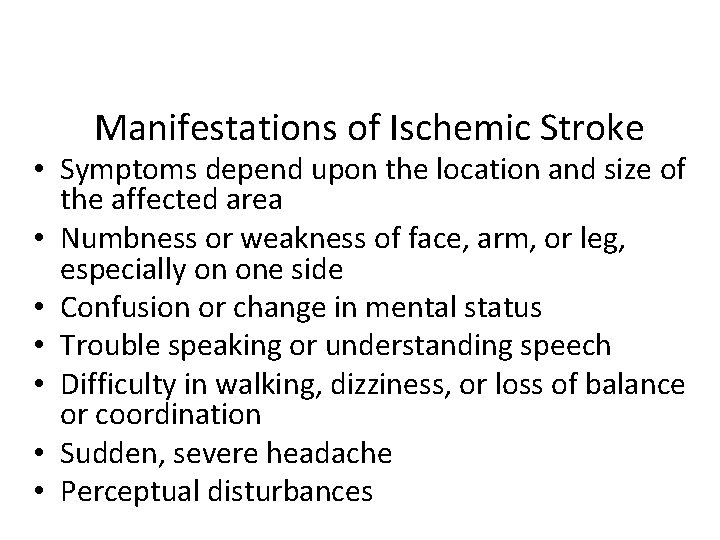
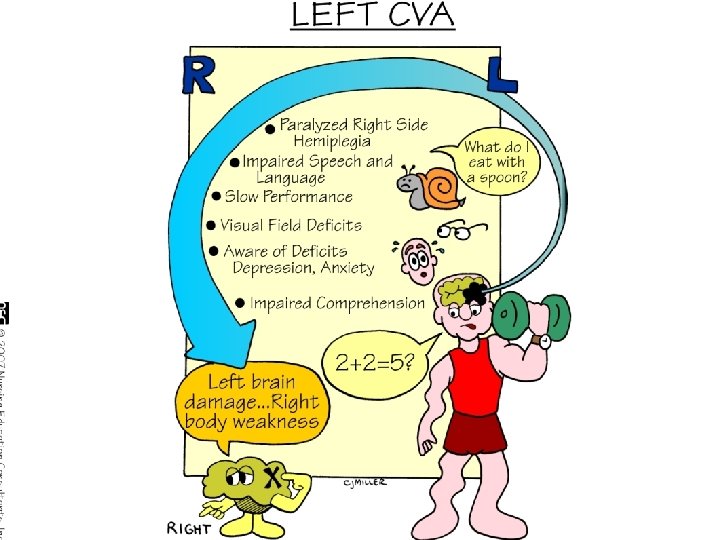
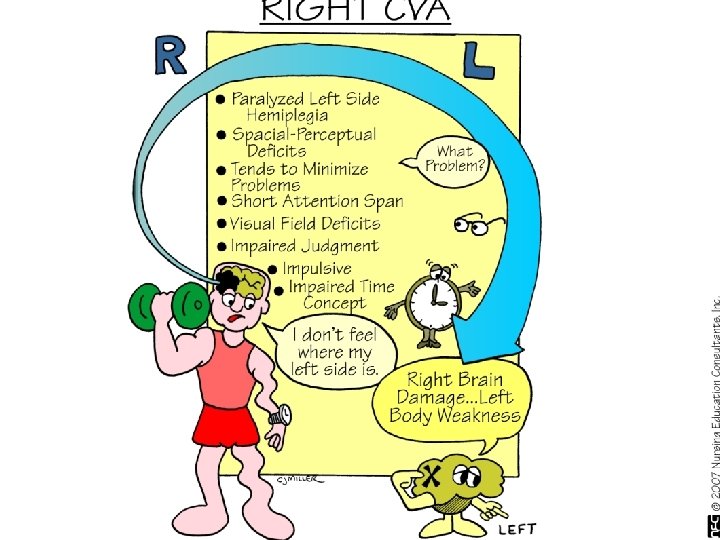
Manifestations of Ischemic Stroke • Symptoms depend upon the location and size of the affected area • Numbness or weakness of face, arm, or leg, especially on one side • Confusion or change in mental status • Trouble speaking or understanding speech • Difficulty in walking, dizziness, or loss of balance or coordination • Sudden, severe headache • Perceptual disturbances
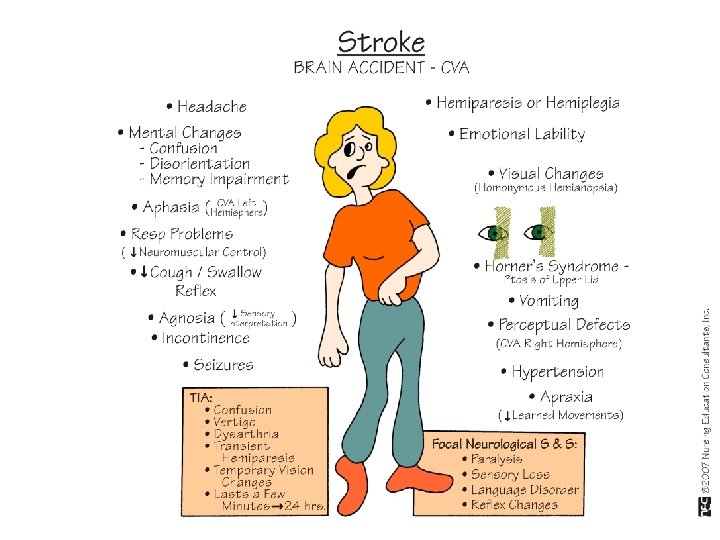
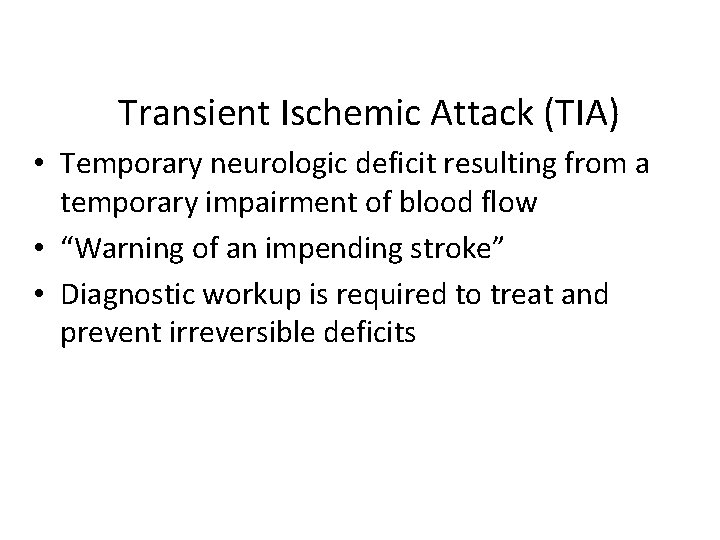
Transient Ischemic Attack (TIA) • Temporary neurologic deficit resulting from a temporary impairment of blood flow • “Warning of an impending stroke” • Diagnostic workup is required to treat and prevent irreversible deficits
Preventive Treatment and Secondary Prevention • Health maintenance measures including a healthy diet, exercise, and the prevention and treatment of periodontal disease • Carotid endarterectomy • Anticoagulant therapy • Antiplatelet therapy: aspirin, dipyridamole (Persantine), clopidogrel (Plavix), ticlopidine (Ticlid) • “Statins” – simvastatin ( Zocor) • Antihypertensive medications – ACEI , thiazide-
DASH Diet • Dietary Approaches to Stop Hypertension – High in fruits, vegetables, moderate in low fat diary products, low in animal protein
Prevent complications-Stroke recurrence • Heparin – to prev stroke at risk for cardiogenic emboli • Unfractionated heparin – then warfarin po. – Activated partial thromboplastin time ( a. PTT) - 1. 5 - 2. 5 times control for anticoagulation – PO is given even while on Heparin. Takes 24 - 48 hrs for therapeutic response – – INR- 2. 0 - 3. 0 INR – International Normalized ratio for prophylaxis against cardiogenic emboli – Monitor for S. E
• Antiplatelet agents- Aspirin, ticlopidine extended release dipyridamole + aspirin, clopidogrel
Drug Therapy aims to improve & restore circulation to the brain • 1. Diuretics - to <cerebral edema. Edema reaches maximum levels 3 -5 days after cerebral infarction • 2. Anticoagulants-to prevent further development or propagation of the thrombosis or embolization elsewhere in the cardiovascular system • 3. Antiplatelets-platelets play a major role in thrombus formation and embolization • 4. Antihypertensives-reduce pressure on cerebral blood vessels. Must use caution not to decrease BP too quickly or too low
cont. -Medical Management • 5. Steroids- Prednisone up to 100 mg/day or dexamethasone- to reduce vasogenic cerebral edema • 6. Barbiturates- decrease neuronal metabolism & energy requirements
Medical Management—Acute Phase of Stroke • Prompt diagnosis and treatment • Assessment of stroke: NIHSS assessment tool • Thrombolytic therapy – Criteria for t. PA – IV dosage and administration – Patient monitoring – Side effects—potential bleeding • Elevate HOB unless contraindicated • Maintain airway and ventilation • Continuous hemodynamic monitoring and neurologic assessment

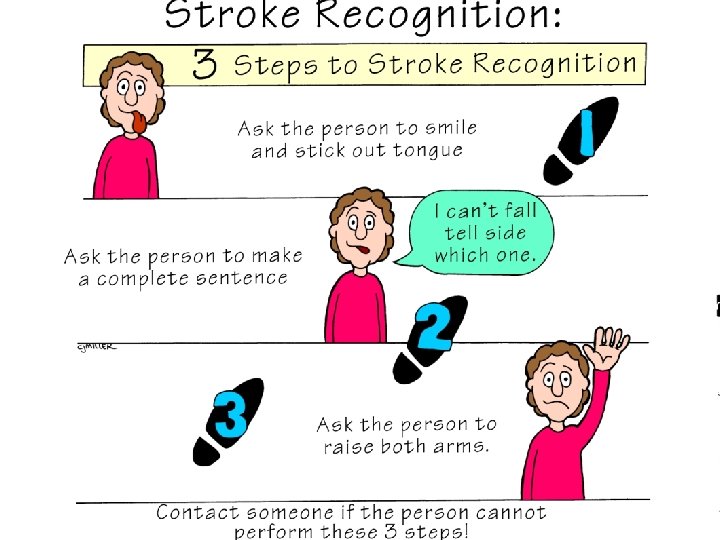
Management • Identify stroke early- – Use of Acute Stroke Quick Screen & the National Institutes of Health Stroke Scale ( NIHSS) • To identify who can benefit from thrombolytic therapy ( adm within 3 hrs of onset of s/s) • Initial assessment include LOC , response to light, visual fields, movement of extremities, sensation, reflexes, speech, sensation, vital signs Data recorded on Glascow Coma Scale ( GCS)
Restore cerebral blood flow • R/O intracebral hemorrhage before rt-PA CT no evidence of intracranial hemorrhage – Recannalization of the occluded vessels & reperfusion of ischemic brain tissue • Recombinant tissue plasminogen (rt-PA) within 3 hrs of onset of stroke – 0. 9 mg/kg IV over 1 hr. Ten percent of the total dose is IV push over 1 minute as bolus then IV – Pt admitted to ICU
rt-PA • Recombinant tissue plasminogen activators – dissolve thrombus or embolus blocking cerebral blood flow – Contraindications-: • Recent hemorrhage, increased risk of hemorrhage ( treatment w/ anticoagulants), systolic BP above 185 or diastolic BP above 110 mm Hg.
Bleeding Prevent complications – Watch for bleeding– Monitor blood work – Monitor systemic bleeding- change in LOC, tachycardia, hypotension, cool clammy skin, pale skin – Stop thrombolytic therapy if sign of bleeding
CVA Treatments Maintain airway & cerebral perfusion, Prevent cerebral edema , Regulate temp • Remove cause, prevent complications, and maintain function, rehabilitation to restore function • Meds – – – Antihypertensives Steroids Anticoagulants Anticonvulsants, Stool softeners Diuretics
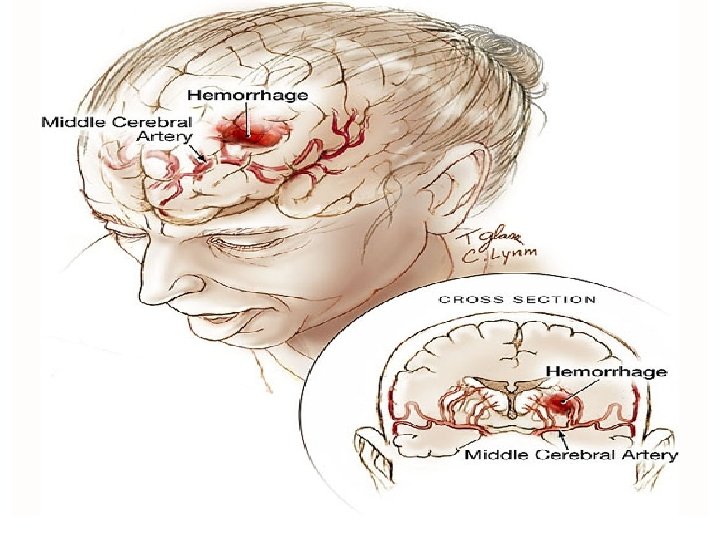
Hemorrhagic Stroke • Bleeding -brain tissue, ventricles, or subarachnoid space. • Rupture ofsmall vessels(hypertension); subarachnoid hemorrhage (ruptured aneurysm); arterial venous malformations (AVMs), intracranial aneurysms, medications(anticoagulants) • Brain metabolism -disrupted by exposure to bld • ICP increases -bld in the subarachnoid space. • Compression or secondary ischemia due to reduced perfusion & vasoconstriction injury to brain tissue.
Manifestations • • Similar to ischemic stroke Severe headache Early and sudden changes in LOC Vomiting
Medical Management • Prevention: control of hypertension • Diagnosis: CT scan, cerebral angiography, lumbar puncture if CT is negative and ICP is not elevated to confirm subarachnoid hemorrhage • Care is primarily supportive • Bed rest with sedation • Oxygen • Treatment of vasospasm, increased ICP, hypertension, potential seizures, and prevention of further bleeding
Nursing Process: The Patient Recovering from an Ischemic Stroke—Assessment • Acute phase – Monitor all systems –VS. Neuro assessment—LOC, motor symptoms, speech, eye symptoms – Monitor for complications-musculoskeletal problems, swallowing difficulties, respiratory problems, increased ICP & meningeal irritation • After the stroke is complete – Focus on patient function; self-care ability, coping, and teaching needs to facilitate rehabilitation
Nursing Process: The Patient Recovering from an Ischemic Stroke—Diagnoses • • • Impaired physical mobility Acute pain Self-care deficits Disturbed sensory perception Impaired swallowing Urinary incontinence Disturbed thought processes Impaired verbal communication Risk for impaired skin integrity Interrupted family processes Sexual dysfunction
Collaborative Problems/Potential Complications • Decreased cerebral blood flow • Inadequate oxygen delivery to brain • Pneumonia
Nursing Process: The Patient Recovering from an Ischemic Stroke—Planning • Major goals may include: – Improved mobility – Avoidance of shoulder pain – Achievement of self-care – Relief of sensory and perceptual deprivation – Prevention of aspiration – Continence of bowel and bladder – Improved thought processes – Achieving a form of communication – Maintaining skin integrity – Restored family functioning – Improved sexual function – Absence of complications
Interventions • Focus on the whole person • Provide interventions to prevent complications and to promote rehabilitation • Provide support and encouragement • Listen to the patient
Improving Mobility and Preventing Joint Deformities • Turn and position in correct alignment every 2 hours • Use of splints • Passive or active ROM 4– 5 times day • Positioning of hands and fingers • Prevention of flexion contractures • Prevention of shoulder abduction • Do not lift by flaccid shoulder
Improving Mobility and Preventing Joint Deformities Passive or active ROM 4– 5 times day Encourage patient to exercise unaffected side Establish regular exercise routine Quadriceps setting and gluteal exercises Assist patient out of bed as soon as possibleassess and help patient achieve balance, move slowly • Ambulation training • • •
Interventions • Enhancing self-care – Set realistic goals with the patient – Encourage personal hygiene – Assure that patient does not neglect the affected side – Use of assistive devices and modification of clothing • Support and encouragement • Strategies to enhance communication • Encourage patient to turn head, look to side with visual field loss
• Nutrition Interventions – Consult with speech therapy or nutritional services – Have patient sit upright, preferably OOB, to eat – Chin tuck or swallowing method – Use of thickened liquids or pureed diet • Bowel and bladder control – Assessment of voiding and scheduled voiding – Measures to prevent constipation—fiber, fluid, toileting schedule – Bowel and bladder retraining
Nursing Process: The Patient with a Hemorrhagic Stroke—Assessment • Complete and ongoing neurologic assessment • • • —use neurologic flow chart Monitor respiratory status and oxygenation Monitoring of ICP Patients with intracerebral or subarachnoid hemorrhage should be monitored in the ICU Monitor for potential complications Monitor fluid balance and laboratory data All changes must be reported immediately
Nursing Process: The Patient with a Hemorrhagic Stroke—Diagnoses • Ineffective tissue perfusion (cerebral) • Disturbed sensory perception • Anxiety
Collaborative Problems/Potential Complications • • • Vasospasm Seizures Hydrocephalus Rebleeding Hyponatremia
Nursing Process: The Patient with a Hemorrhagic Stroke—Planning • Goals may include: – Improved cerebral tissue perfusion – Relief of sensory and perceptual deprivation – Relief of anxiety – The absence of complications
Home Care and Teaching for the Patient Recovering from a Stroke • Prevention of subsequent strokes, health promotion, and follow-up care • Prevention of and signs and symptoms of complications • Medication teaching • Safety measures • Adaptive strategies and use of assistive devices for ADLs • Nutrition—diet, swallowing techniques, tube feeding administration • Elimination—bowel and bladder programs, catheter use • Exercise and activities, recreation and diversion • Socialization, support groups, and community resources
Transient Ischemic Attacks -TIA • Referred to as “Mini Stroke” It is not a stroke at all & doesn’t typically cause permanent brain damage. It is a warning sign that a stroke may occur in the future • Altered cerebral tissue perfusion related to a temporary neurologic disturbance • Manifested by sudden loss of motor or sensory function • Lasts for a few minutes average-10 mins • Must resolve within 24 hours. TIA that last longer than 1 hr is – small infarcts. • Caused by temporarily diminished blood supply to an area of the brain
Transient Ischemic Attack • African-Americans affected more frequently as a result of high frequency of diabetes and HTN in this group. • Prevalence – Estimated million stroke survivors in U. S. • The number of strokes occurring in the younger population is increasing as a result of IV drug abuse. • .
• Those using crack cocaine experience increased incidence of stroke due to changes in clotting mechanism caused by the drugs or sudden increase in systolic BP
Pathophysiology • Similar to stroke but of short duration and no permanent deficits
• Based on symptoms – Diagnosis – Also + bruit • Dx tests: – CT to R/O stroke or other disorder – Doppler , Computed tomographic angiography (CTA) , magnetic resonance angiography ( MRA) of the carotid arteries – Cerebral angiogram – ECG – Transthoracic or transesophageal echocardiography- to r/o mural thrombosis & valvular disorder ( TTE & TEE)
TIA Treatment • • Control hypertension Low sodium diet Possible anticoagulant therapy Stop smoking
Treatment of Ischemic Stroke Treatment of a TIA Warning - treat to prevent stroke Antiplatelet drugs - ex aspirin Anticoagulant drugs - ex warfarin avoid dehydration, hypotension Endarterectomy for carotid plaque Emphasis on saving brain tissue by use of thrombolytic agents (<disability) Ex-streptokinase • Use CT scan to exclude hemorrhagic stroke (also anticoagulant drugs, >BP) • Begin therapy within 3 hr of onset of symptoms • • •
Surgical management • For asx carotid artery dis- with 60 % or more stenosis • Symptomatic- with 70 % stenosis or > Preop-ASA to prev embolism at surgical site Stop anticoagulant
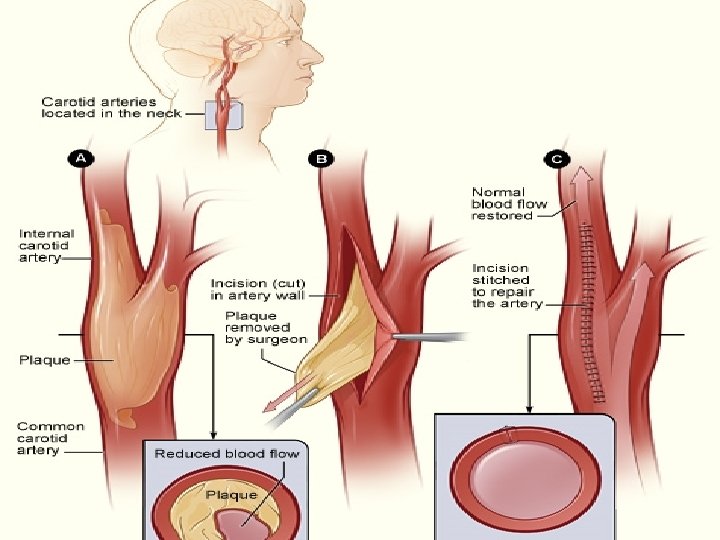
Endarterectomy • Opening of carotid artery. Plaque is removed. Incision is made in sternocleidomastoid muscle • Post –op – Monitor neuro – Doppler after 6 mos to 1 yr to assess patency of artery
Other techniques • Carotid angioplasty- balloon catheter is threaded thru femoral artery- to area of carotid stenosis. It is inflated to dilate the lesions. • Stent catheter is also used to open the area
Post op care • Neuro assessment • Assess facial ( VII) Vagus (X), spinal accessory ( XI) & hypoglossal ( XII) – Common damage- vocal cord paralysis, difficulty managing saliva, tongue deviation – Head be aligned – Antiplatelet
- Slides: 58