Management of Overactive Bladder Judith ten Hof Consultant
Management of Overactive Bladder Judith ten Hof Consultant Obstetrician and Gynaecologist Nottingham University Hospitals
Management of Overactive bladder Can we do better?
Contents �Definition �Incidence and etiology �Risk factors �History and examination �Management �Referral pathway
Definitions Lower Urinary Tract Symptoms (LUTS) Storage symptoms Voiding symptoms �Urinary incontinence: complaint of any involuntary loss of urine causing social and hygienic problems �UUI: accompanied by or immediately preceded by urgency �SUI: on effort, exertion, sneezing or coughing �MUI: combination of both �Overactive bladder: urgency with or without UI usually associated with frequency & nocturia (ICS)
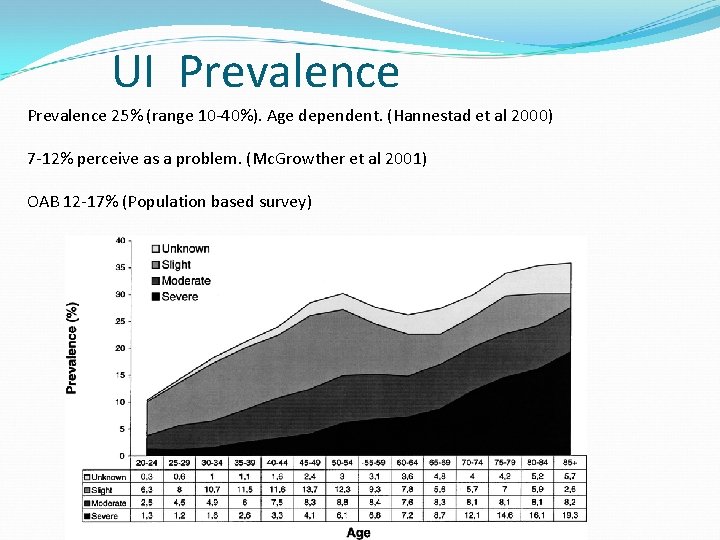
UI Prevalence 25% (range 10 -40%). Age dependent. (Hannestad et al 2000) 7 -12% perceive as a problem. (Mc. Growther et al 2001) OAB 12 -17% (Population based survey)
Impact of UI �Quality of life �associated with depression and anxiety, work impairment, and social isolation �Sexual dysfunction � 30% (fear of) coital incontinence �Morbidity �perineal infections �falls and fractures �Caregiver burden � 6 -10% of nursing home admissions
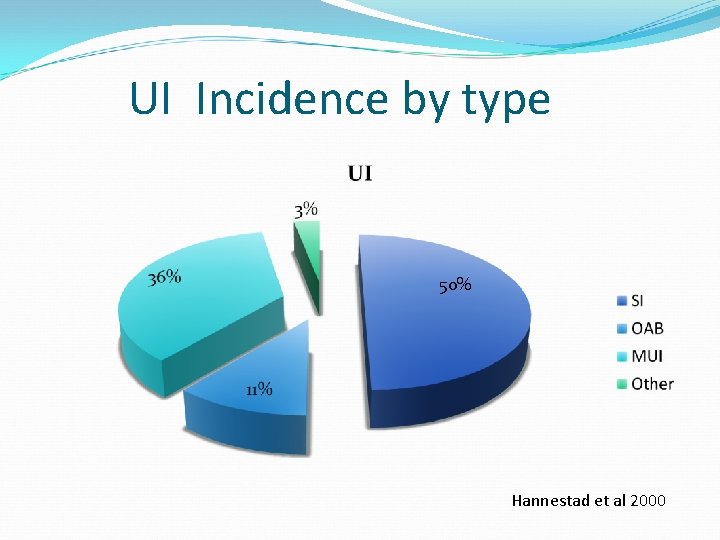
UI Incidence by type 50% Hannestad et al 2000
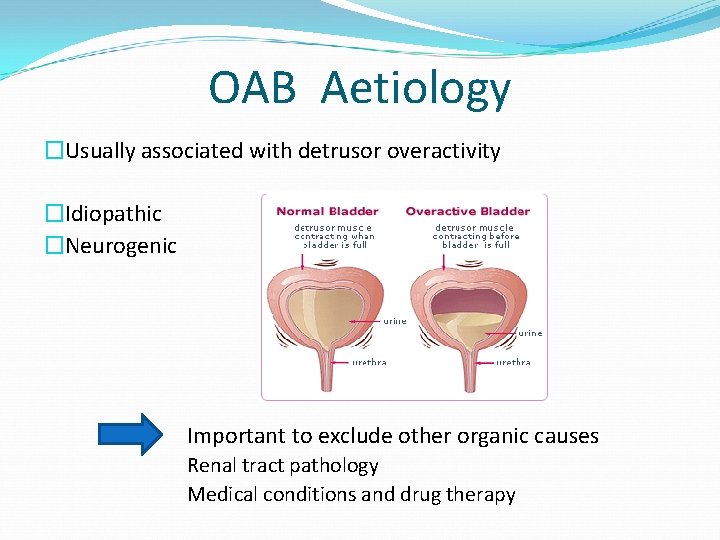
OAB Aetiology �Usually associated with detrusor overactivity �Idiopathic �Neurogenic Important to exclude other organic causes Renal tract pathology Medical conditions and drug therapy
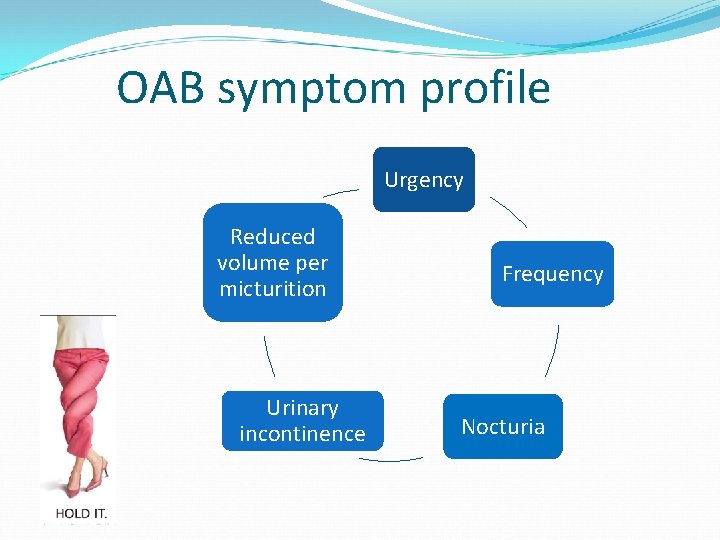
OAB symptom profile Urgency Reduced volume per micturition Urinary incontinence Frequency Nocturia
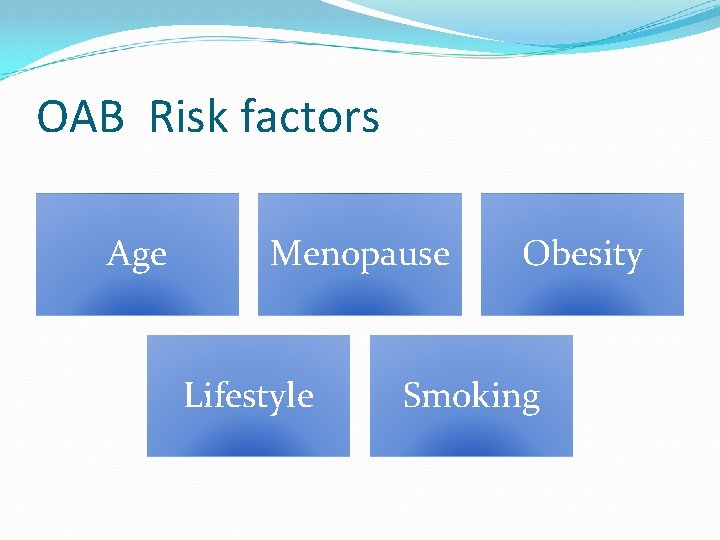
OAB Risk factors Age Menopause Lifestyle Obesity Smoking
Case history 55 year old lady presents with symptoms of Frequency Urge incontinence Occasional stress incontinence No voiding dysfunction No infection
Patient journey Primary Care/ continence advisors
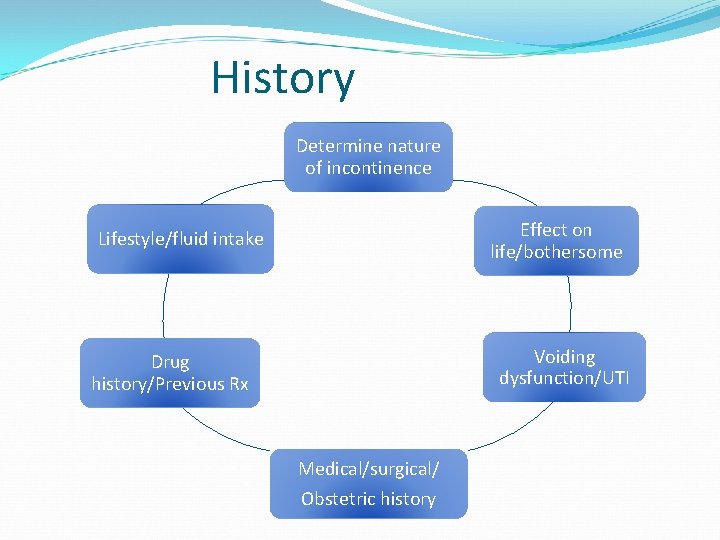
History Determine nature of incontinence Effect on life/bothersome Lifestyle/fluid intake Voiding dysfunction/UTI Drug history/Previous Rx Medical/surgical/ Obstetric history
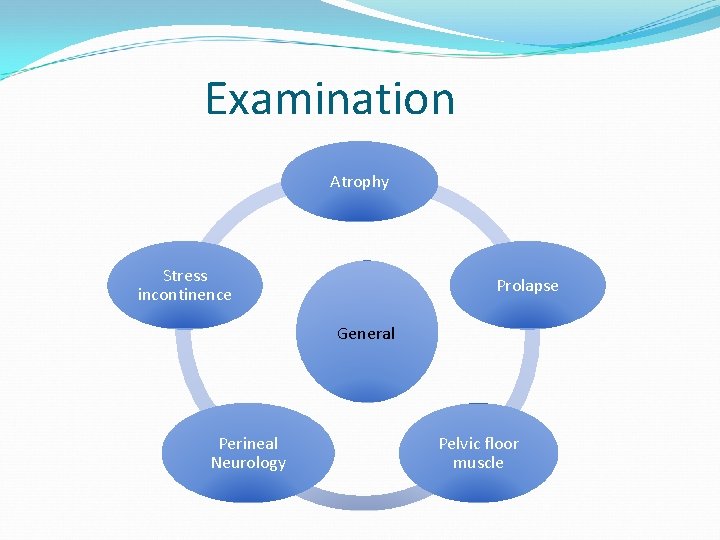
Examination Atrophy Stress incontinence Prolapse General Perineal Neurology Pelvic floor muscle
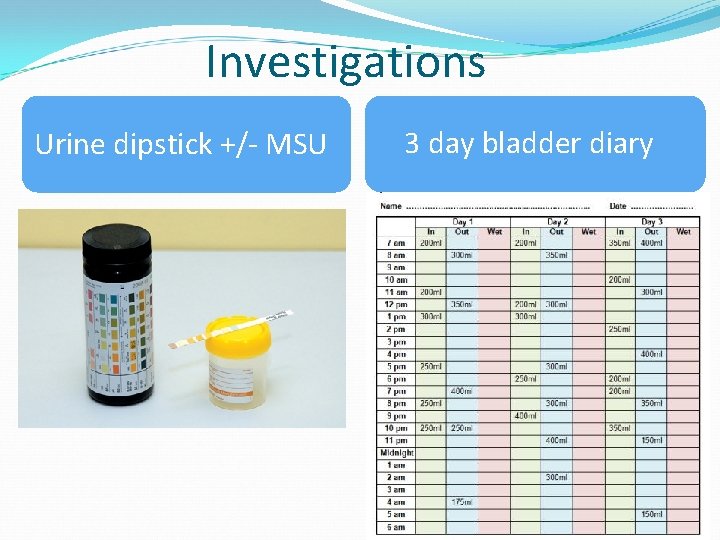
Investigations Urine dipstick +/- MSU 3 day bladder diary
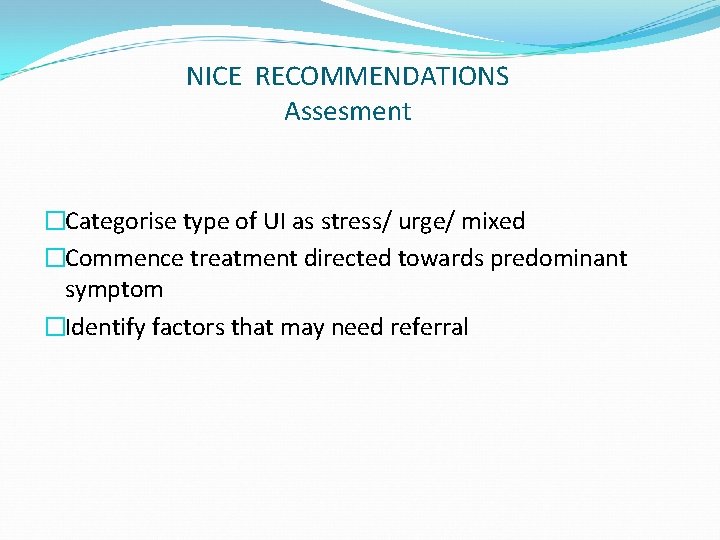
NICE RECOMMENDATIONS Assesment �Categorise type of UI as stress/ urge/ mixed �Commence treatment directed towards predominant symptom �Identify factors that may need referral
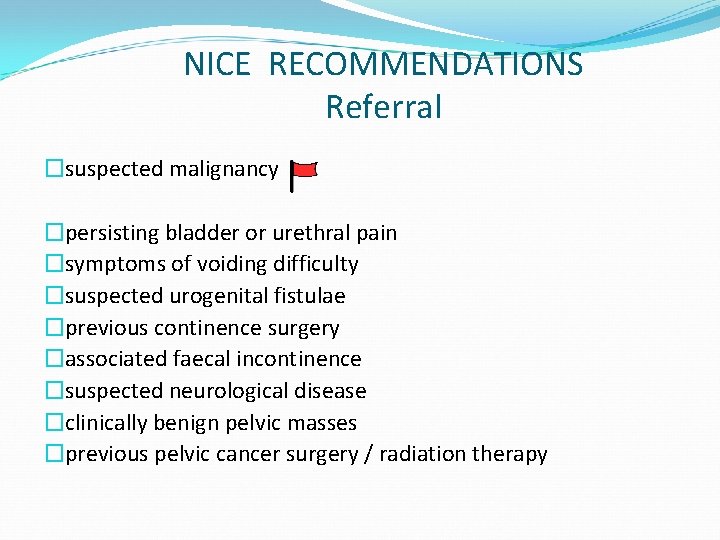
NICE RECOMMENDATIONS Referral �suspected malignancy �persisting bladder or urethral pain �symptoms of voiding difficulty �suspected urogenital fistulae �previous continence surgery �associated faecal incontinence �suspected neurological disease �clinically benign pelvic masses �previous pelvic cancer surgery / radiation therapy
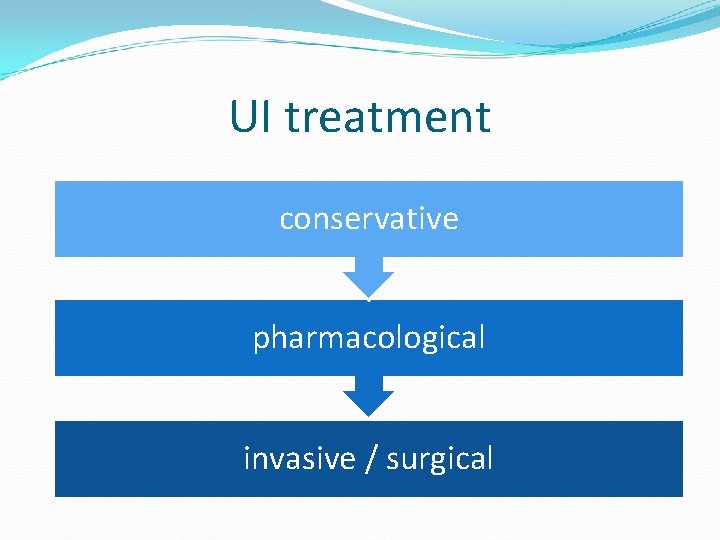
UI treatment conservative pharmacological invasive / surgical

Behavioural modification Weight loss Pads/ catheters OAB Conservative Management Fluid management and caffeine reduction Pelvic Floor exercises Bladder retraining 6 weeks Adjusting medication Vaginal Estrogen
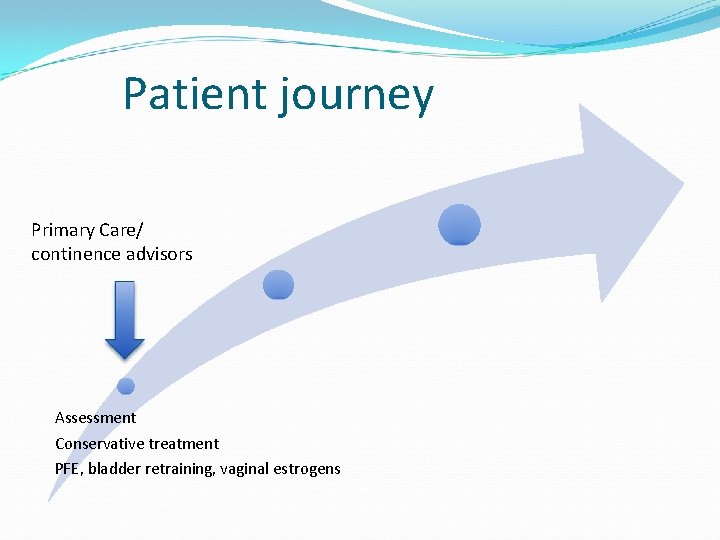
Patient journey Primary Care/ continence advisors Assessment Conservative treatment PFE, bladder retraining, vaginal estrogens
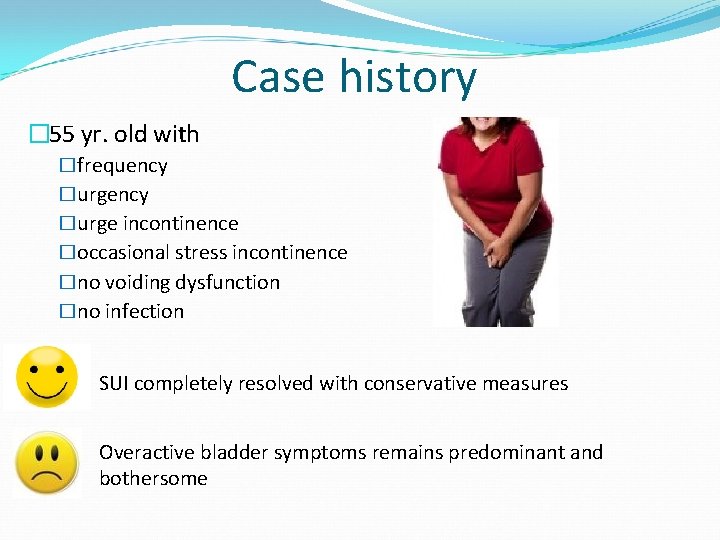
Case history � 55 yr. old with �frequency �urge incontinence �occasional stress incontinence �no voiding dysfunction �no infection SUI completely resolved with conservative measures Overactive bladder symptoms remains predominant and bothersome
Pharmacological OAB treatment Anticholinergics Beta 3 adrenoceptor agonist
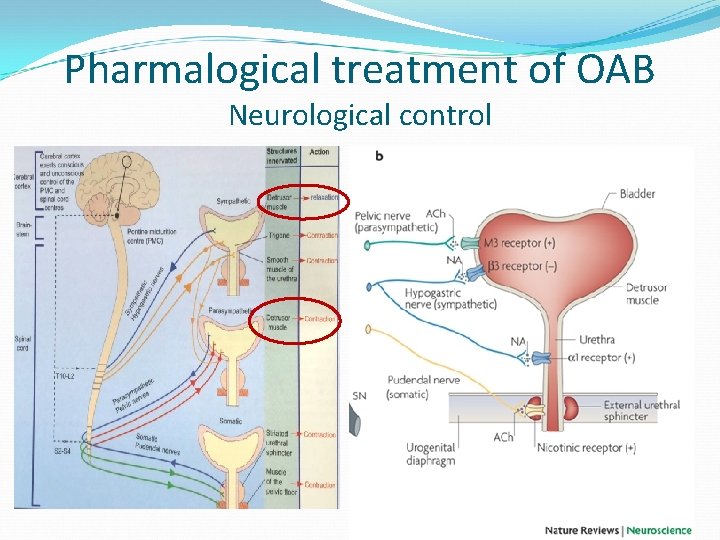
Pharmalogical treatment of OAB Neurological control
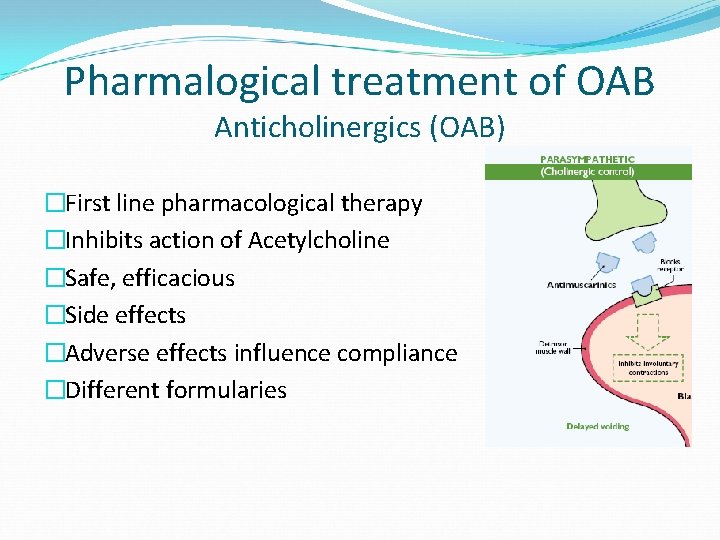
Pharmalogical treatment of OAB Anticholinergics (OAB) �First line pharmacological therapy �Inhibits action of Acetylcholine �Safe, efficacious �Side effects �Adverse effects influence compliance �Different formularies
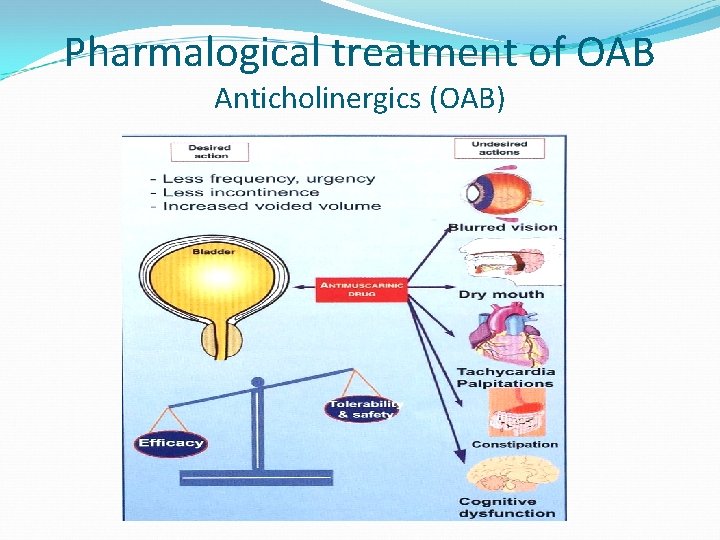
Pharmalogical treatment of OAB Anticholinergics (OAB)
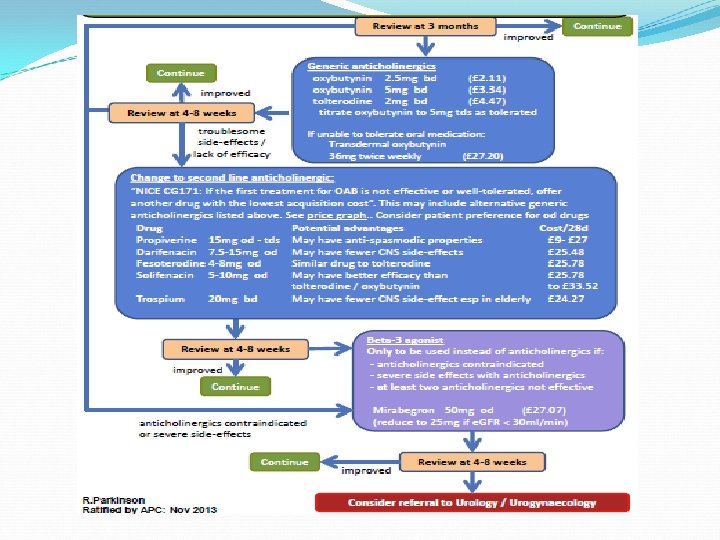
NICE RECOMMENDATIONS First Line Anticholinergics for OAB �oxybutynin (immediate release), or � not to frail older women �tolterodine (immediate release), or �darifenacin (once daily preparation) [new 2013] Review in 4 weeks � If not effective or well‑tolerated, offer another drug with the lowest acquisition cost [new 2013] � Offer transdermal to women unable to tolerate oral medication [new 2013] � Do not use flavoxate, propantheline and imipramine
NICE RECOMMENDATIONS Anticholinergics for OAB Always take account of �coexisting conditions (for example, poor bladder emptying) �use of other existing medication affecting the total anticholinergic load �risk of adverse effects [new 2013]
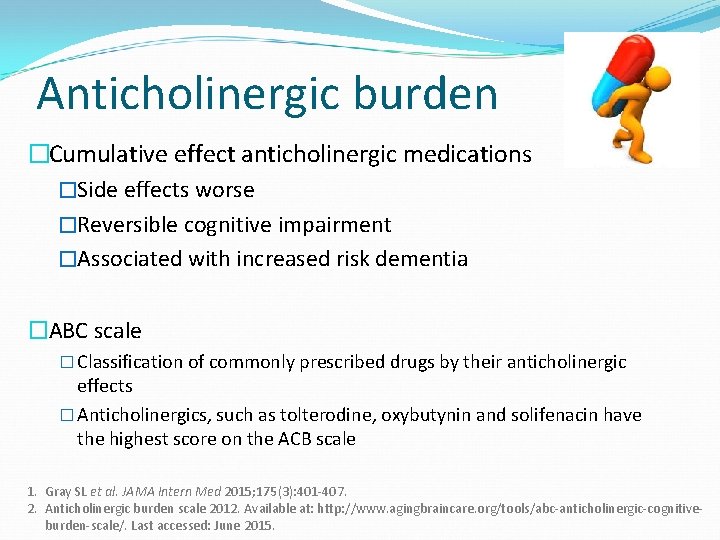
Anticholinergic burden �Cumulative effect anticholinergic medications �Side effects worse �Reversible cognitive impairment �Associated with increased risk dementia �ABC scale � Classification of commonly prescribed drugs by their anticholinergic effects � Anticholinergics, such as tolterodine, oxybutynin and solifenacin have the highest score on the ACB scale 1. Gray SL et al. JAMA Intern Med 2015; 175(3): 401 -407. 2. Anticholinergic burden scale 2012. Available at: http: //www. agingbraincare. org/tools/abc-anticholinergic-cognitiveburden-scale/. Last accessed: June 2015.
NICE RECOMMENDATIONS Anticholinergics for OAB Discuss � likelihood of success and associated common adverse effects �frequency and route of administration �some adverse effects such as dry mouth and constipation may indicate that treatment is starting to have an effect, and �that they may not see the full benefits until they have been taking the treatment for 4 weeks. [new 2013]
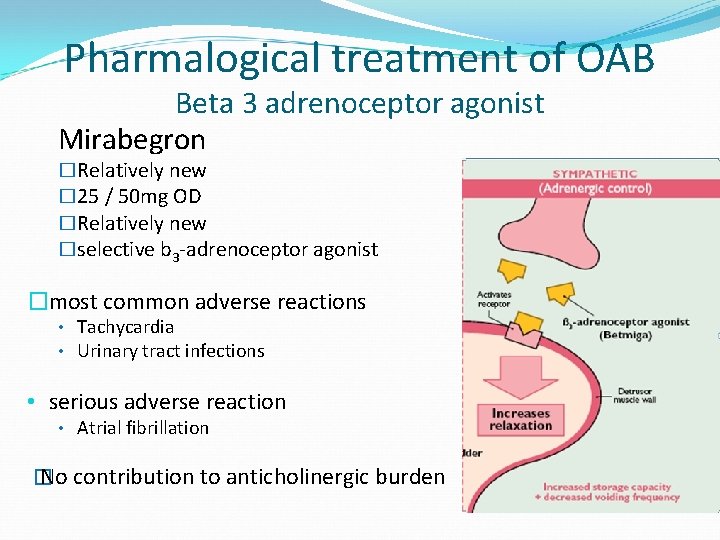
Pharmalogical treatment of OAB Beta 3 adrenoceptor agonist Mirabegron �Relatively new � 25 / 50 mg OD �Relatively new �selective b 3 -adrenoceptor agonist �most common adverse reactions • Tachycardia • Urinary tract infections • serious adverse reaction • Atrial fibrillation � No contribution to anticholinergic burden
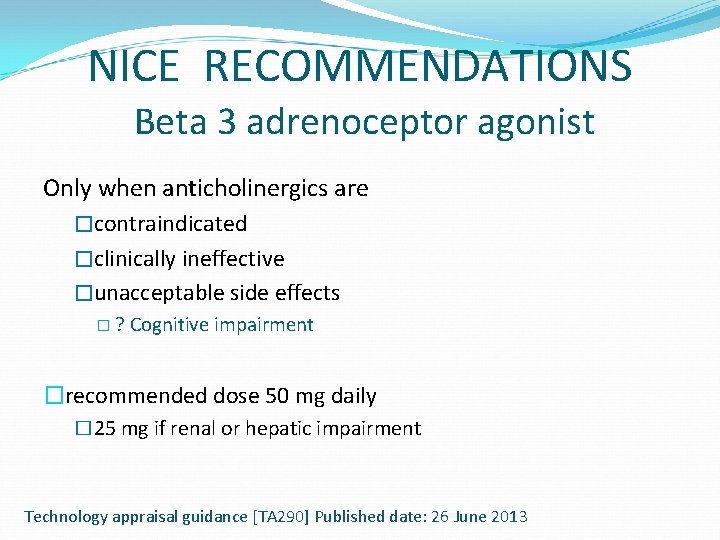
NICE RECOMMENDATIONS Beta 3 adrenoceptor agonist Only when anticholinergics are �contraindicated �clinically ineffective �unacceptable side effects � ? Cognitive impairment �recommended dose 50 mg daily � 25 mg if renal or hepatic impairment Technology appraisal guidance [TA 290] Published date: 26 June 2013
Case history � 55 yr. old with �frequency �urge incontinence �occasional stress incontinence �no voiding dysfunction �no infection SUI completely resolved with conservative measures Marginal improvement of overactive symptoms with 1/2 different anticholinergics. Symptoms still bothersome
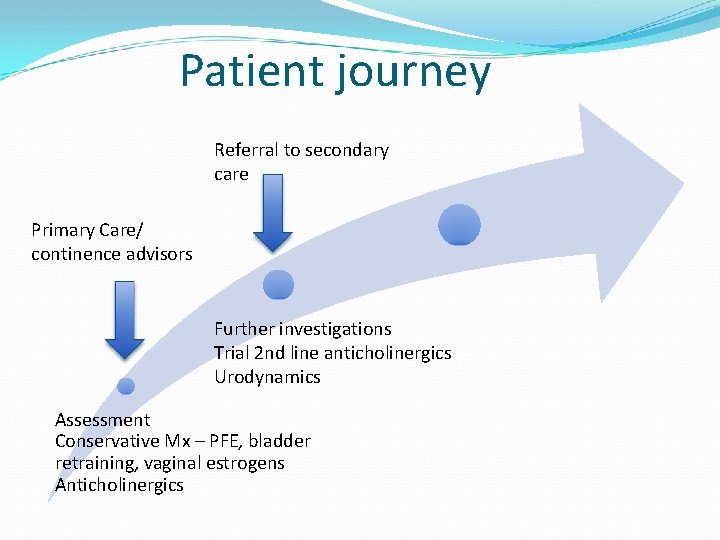
Patient journey Referral to secondary care Primary Care/ continence advisors Further investigations Trial 2 nd line anticholinergics Urodynamics Assessment Conservative Mx – PFE, bladder retraining, vaginal estrogens Anticholinergics
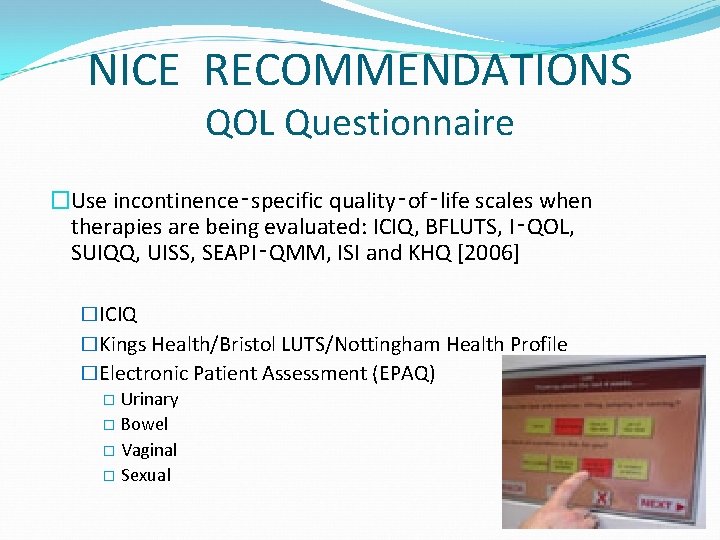
NICE RECOMMENDATIONS QOL Questionnaire �Use incontinence‑specific quality‑of‑life scales when therapies are being evaluated: ICIQ, BFLUTS, I‑QOL, SUIQQ, UISS, SEAPI‑QMM, ISI and KHQ [2006] �ICIQ �Kings Health/Bristol LUTS/Nottingham Health Profile �Electronic Patient Assessment (EPAQ) � Urinary � Bowel � Vaginal � Sexual
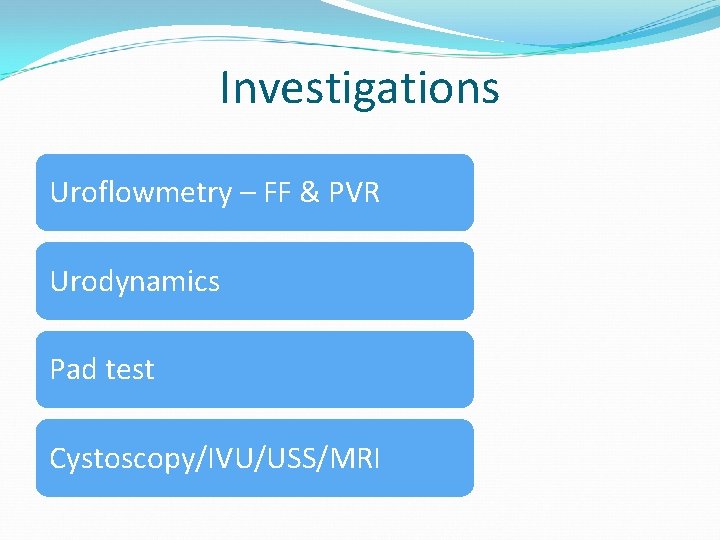
Investigations Uroflowmetry – FF & PVR Urodynamics Pad test Cystoscopy/IVU/USS/MRI
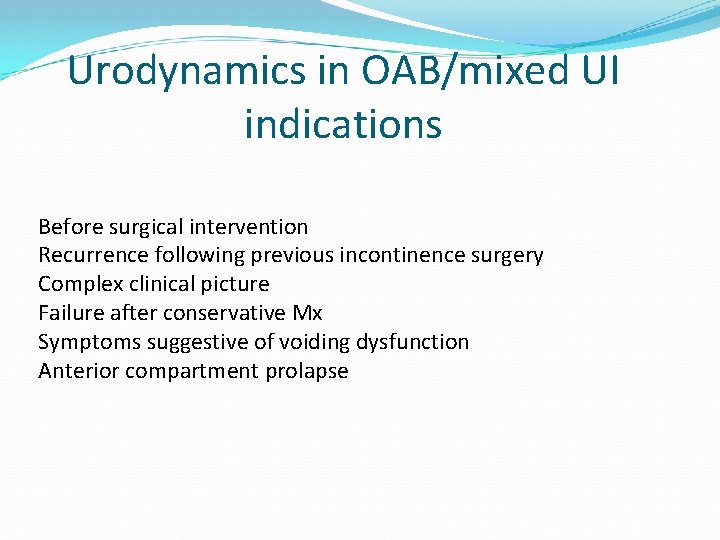
Urodynamics in OAB/mixed UI indications Before surgical intervention Recurrence following previous incontinence surgery Complex clinical picture Failure after conservative Mx Symptoms suggestive of voiding dysfunction Anterior compartment prolapse
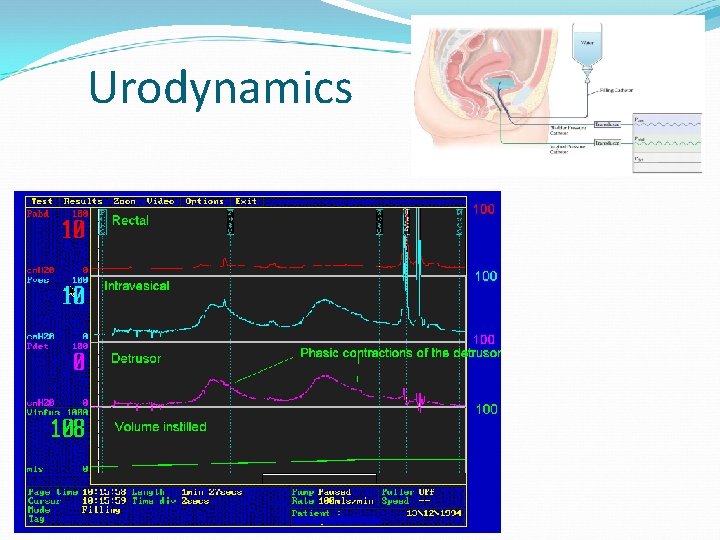
Urodynamics
Urodynamic diagnosis Detrusor Overactivity (DOA) Mixed Urinary Incontinence
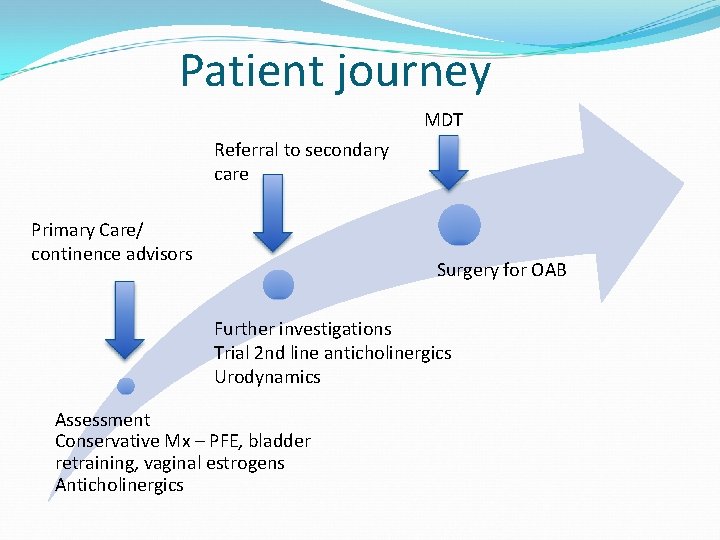
Patient journey MDT Referral to secondary care Primary Care/ continence advisors Surgery for OAB Further investigations Trial 2 nd line anticholinergics Urodynamics Assessment Conservative Mx – PFE, bladder retraining, vaginal estrogens Anticholinergics
Invasive / surgical Botulinum Toxin injections Sacral neuromodulation / Tibial nerve stimulation Augmentation cystoplasty / Urinary diversion
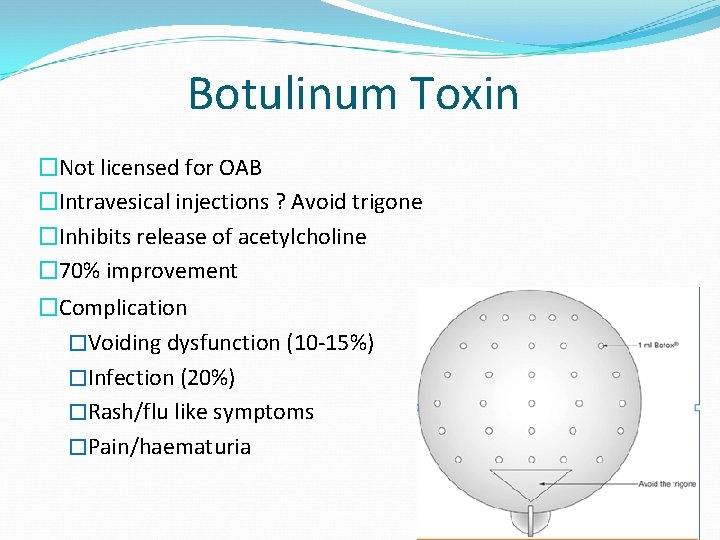
Botulinum Toxin �Not licensed for OAB �Intravesical injections ? Avoid trigone �Inhibits release of acetylcholine � 70% improvement �Complication �Voiding dysfunction (10 -15%) �Infection (20%) �Rash/flu like symptoms �Pain/haematuria
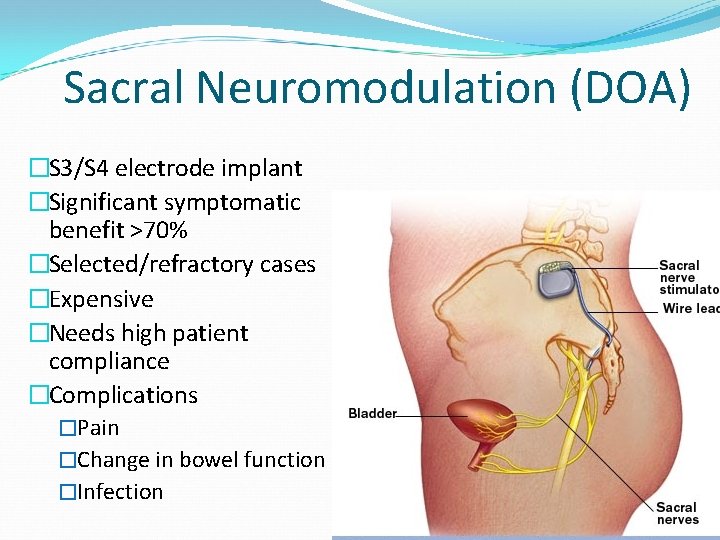
Sacral Neuromodulation (DOA) �S 3/S 4 electrode implant �Significant symptomatic benefit >70% �Selected/refractory cases �Expensive �Needs high patient compliance �Complications �Pain �Change in bowel function �Infection
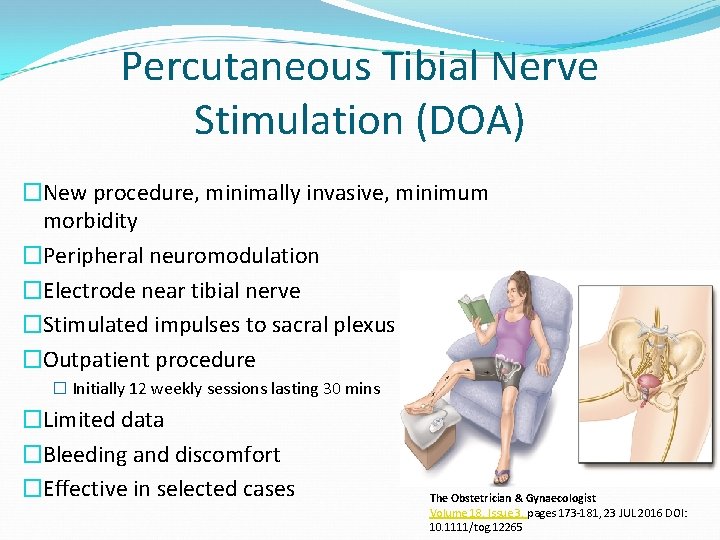
Percutaneous Tibial Nerve Stimulation (DOA) �New procedure, minimally invasive, minimum morbidity �Peripheral neuromodulation �Electrode near tibial nerve �Stimulated impulses to sacral plexus �Outpatient procedure � Initially 12 weekly sessions lasting 30 mins �Limited data �Bleeding and discomfort �Effective in selected cases The Obstetrician & Gynaecologist Volume 18, Issue 3, pages 173 -181, 23 JUL 2016 DOI: 10. 1111/tog. 12265
Augmentation cystoplasty / Urinary diversion Augmentation cystoplasty • Implanting ileum into bladder • Significant morbidity Urinary diversion • Ileal conduit • Total cystectomy may be indicated with this • Complications
Key issues �Patience and commitment �Conservative and medical treatments are effective, but there is poor long-term compliance with medication, and many patients seek alternative treatments �Need favourable balance between efficacy & tolerability �Patient satisfaction & appropriate counselling �Safety in elderly patients with co-morbidities
Patient care pathway �Common condition �Can be diagnosed and treated in primary care �Inappropriate referral may occur �Cost implications �Implications to patient
Management of Overactive bladder Can we do better? Yes we can!!
Questions?
- Slides: 49