Management of Neurologic Dysfunction 1 Copyright 2008 Lippincott
- Slides: 66
Management of Neurologic Dysfunction 1 Copyright © 2008 Lippincott Williams & Wilkins.
The Neurologic System • Central nervous system controls the body’s vital functions • Relies on structural integrity for support and homeostasis – Structural disruptions (eg, stroke, tumor) • Relies on the body’s ability to maintain a homeostatic environment – Homeostatic disruptions (eg, toxins, lyte imbalance) 2 Copyright © 2008 Lippincott Williams & Wilkins.
Altered Level of Consciousness (LOC) • Level of responsiveness and consciousness is the most important indicator of the patient's condition • LOC is a continuum from normal alertness and full cognition (consciousness) to coma • Altered LOC is not the disorder but the result of a pathology – Cause may be neurologic, toxicologic or metabolic – Initial changes may be subtle 3 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Assessment of the • Patient With Altered LOC Verbal response and orientation • • Alertness Motor responses Respiratory status and pattern Eye signs Reflexes Postures Glasgow Coma Scale – Eye opening, verbal and motor response 4 Copyright © 2008 Lippincott Williams & Wilkins.
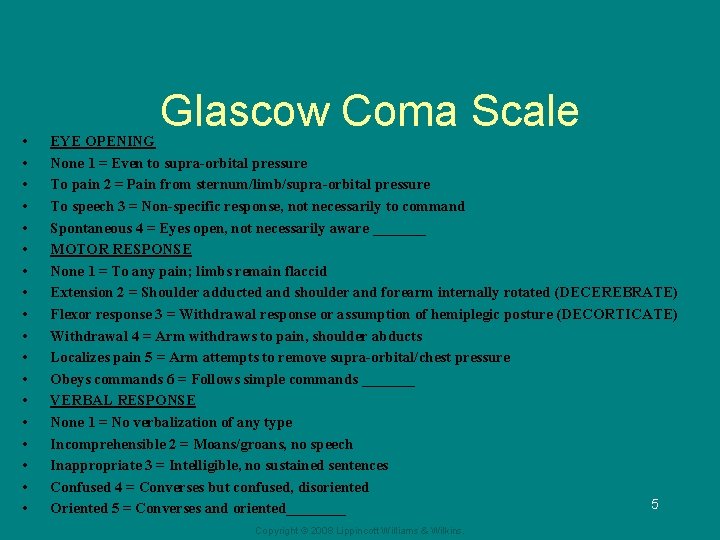
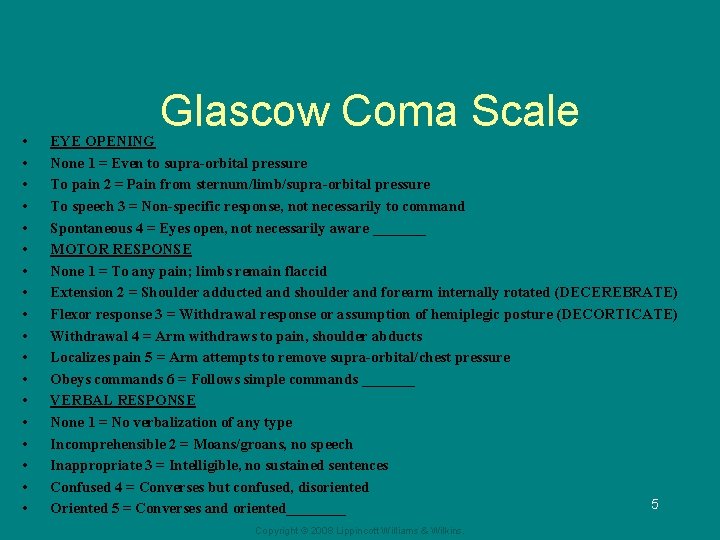
• • • • • Glascow Coma Scale EYE OPENING None 1 = Even to supra-orbital pressure To pain 2 = Pain from sternum/limb/supra-orbital pressure To speech 3 = Non-specific response, not necessarily to command Spontaneous 4 = Eyes open, not necessarily aware _______ MOTOR RESPONSE None 1 = To any pain; limbs remain flaccid Extension 2 = Shoulder adducted and shoulder and forearm internally rotated (DECEREBRATE) Flexor response 3 = Withdrawal response or assumption of hemiplegic posture (DECORTICATE) Withdrawal 4 = Arm withdraws to pain, shoulder abducts Localizes pain 5 = Arm attempts to remove supra-orbital/chest pressure Obeys commands 6 = Follows simple commands _______ VERBAL RESPONSE None 1 = No verbalization of any type Incomprehensible 2 = Moans/groans, no speech Inappropriate 3 = Intelligible, no sustained sentences Confused 4 = Converses but confused, disoriented 5 Oriented 5 = Converses and oriented____ Copyright © 2008 Lippincott Williams & Wilkins.
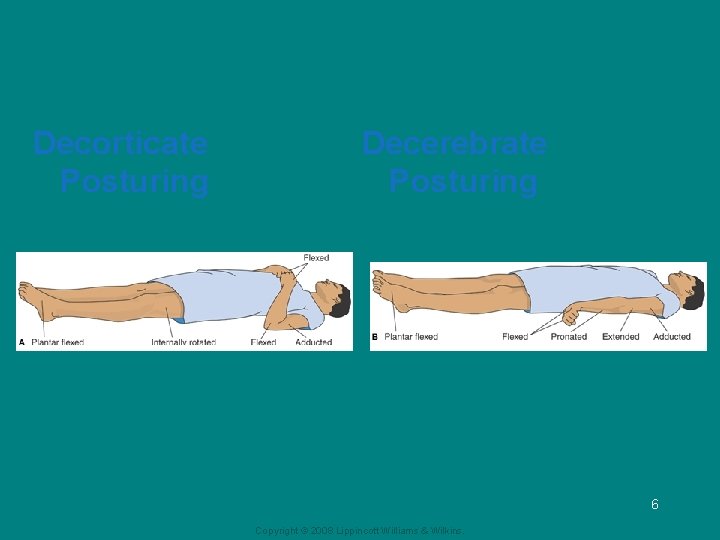
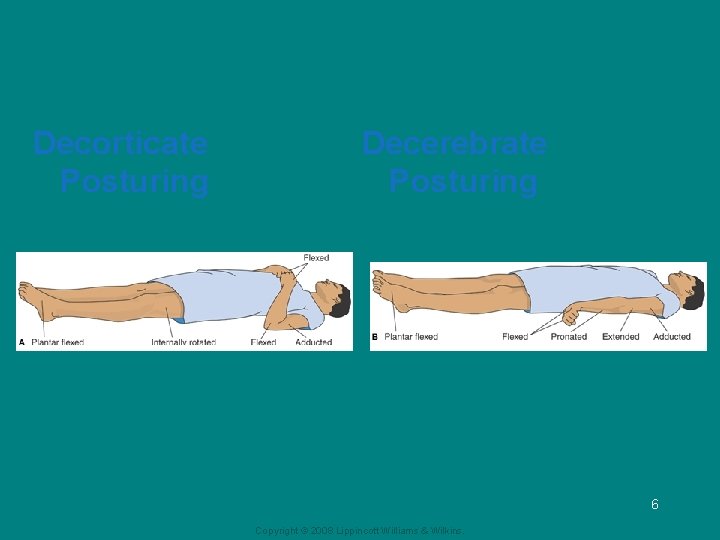
Decorticate Posturing Decerebrate Posturing 6 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Diagnosis of the Patient With Altered Level of Consciousness • • • Ineffective airway clearance Risk of injury Deficient fluid volume Impaired oral mucosa Risk for impaired skin integrity and impaired tissue integrity (cornea) Ineffective thermoregulation Impaired urinary elimination and bowel incontinence Disturbed sensory perception Interrupted family processes Copyright © 2008 Lippincott Williams & Wilkins. 7
Collaborative Problems/Potential Complications • Respiratory distress or failure • Pneumonia • Aspiration • Pressure ulcer • Deep vein thrombosis (DVT) • Contractures 8 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Planning the Care of the Patient With Altered LOC • Goals include: – – – – – Maintenance of clear airway (this is priority) Protection from injury Attainment of fluid volume balance Maintenance of skin integrity Absence of corneal irritation Effective thermoregulation Accurate perception of environmental stimuli Maintenance of intact family or support system Absence of complications 9 Copyright © 2008 Lippincott Williams & Wilkins.
Interventions • compensate for the patient's loss of protective reflexes and to assume responsibility for total patient care; protection includes maintaining the patient’s dignity and privacy • Maintain an airway (PRIORITY) – Frequent monitoring of respiratory status including auscultation of lung sounds – Position the patient to promote accumulation of secretions and prevent obstruction of upper airway: HOB elevated 30°, lateral position – Provide suctioning, oral hygiene, and CPT – Monitor ability patient’s to maintain airway and manage secretions 10 Copyright © 2008 Lippincott Williams & Wilkins.
Maintaining Tissue Integrity • Assess skin frequently, especially areas with high potential for breakdown • Turn patient frequently; use turning schedule • Carefully position patient in correct body alignment • Perform passive range of motion • Use splints, foam boots, trochanter rolls, and specialty beds as needed • Clean eyes with cotton balls moistened with saline • Implement measures to protect eyes • Provide frequent, scrupulous oral care Copyright © 2008 Lippincott Williams & Wilkins. 11
Interventions • Maintain fluid status – Assess fluid status by examining tissue turgor and mucosa, lab data, and I&O – Administer IVs, tube feedings, and fluids via feeding tube as required: monitor ordered rate of IV fluids carefully • Maintain body temperature – Adjust environment and cover patient appropriately – If temperature is elevated, use minimum amount of bedding, administer acetaminophen, and allow fan to blow over patient to increase cooling – Monitor temperature frequently and use measures to prevent shivering 12 Copyright © 2008 Lippincott Williams & Wilkins.
Promoting Bowel and Bladder Function • Assess for urinary retention and urinary incontinence • May require indwelling or intermittent catherization • Initiate bladder-training program • Assess for abdominal distention, potential constipation, and bowel incontinence • Monitor bowel movements • Promote elimination with stool softeners, glycerin suppositories, or enemas as indicated 13 Copyright © 2008 Lippincott Williams & Wilkins.
Sensory Stimulation and Communication • Talk to and touch the patient and encourage the family to talk to and touch the patient • Maintain normal day–night pattern of activity • Orient the patient frequently • A patient aroused from coma may experience a period of agitation; minimize stimulation at this time • Initiate programs for sensory stimulation • Reinforce and provide consistent information to family 14 Copyright © 2008 Lippincott Williams & Wilkins.
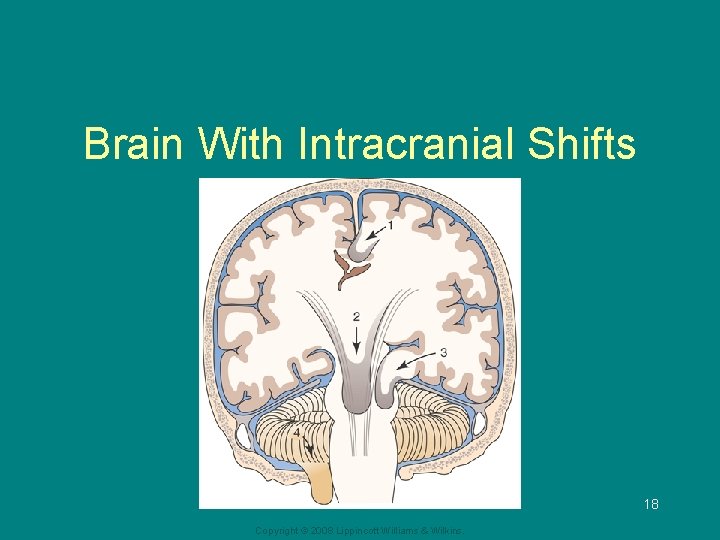
Increased Intracranial Pressure (ICP) • Monro-Kellie hypothesis: because of limited space in the skull, an increase in any one skull component—brain tissue, blood, or CSF—will cause a change in the volume of the others • Compensation to maintain a normal ICP of 10 to 20 mm Hg is normally accomplished by shifting or displacing CSF • With disease or injury, ICP may increase • Increased ICP decreases cerebral perfusion, causes ischemia, cell death, and (further) edema 15 Copyright © 2008 Lippincott Williams & Wilkins.
Increased Intracranial Pressure (cont. ) • Brain tissues may shift through the dura and result in herniation • Decreased cerebral blood flow – Systemic BP rises to maintain cerebral flow • Occurs w/ low HR and irregular respiration – CO 2 plays a role; decreased CO 2 results in vasoconstriction, and increased CO 2 results in vasodilation 16 Copyright © 2008 Lippincott Williams & Wilkins.
Increased Intracranial Pressure • Cerebral Edema – Defined as an abnormal accumulation of fluid in the brain tissue – As the brain swells, body attempts to compensate for increased ICP • Autoregulation (blood vessels) • Decreased CSF production 17 Copyright © 2008 Lippincott Williams & Wilkins.
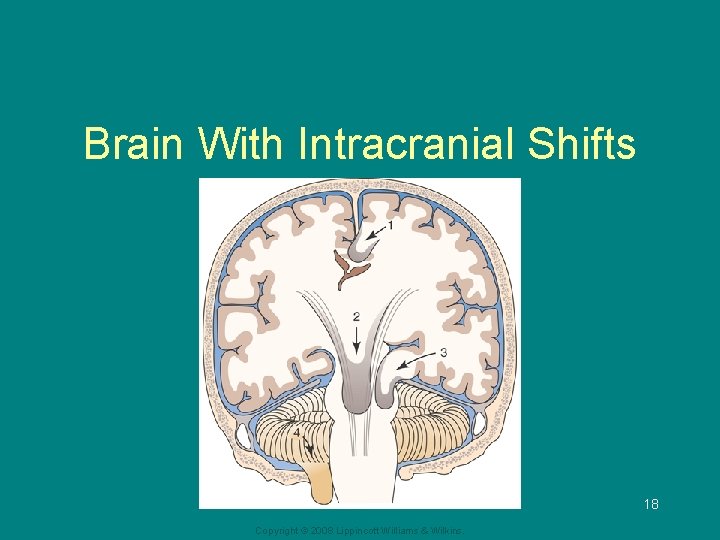
Brain With Intracranial Shifts 18 Copyright © 2008 Lippincott Williams & Wilkins.
ICP and CPP • CPP (cerebral perfusion pressure) is closely linked to ICP • CPP = MAP (mean arterial pressure) – ICP • Normal CPP is 60 to 100 • A CPP of less than 50 results in permanent neurolgic damage 19 Copyright © 2008 Lippincott Williams & Wilkins.
Manifestations of Increased ICP —Early • Changes in level of consciousness (FIRST) • Any change in condition – Restlessness, confusion, increasing drowsiness, increased respiratory effort, and purposeless movements • Pupillary changes and impaired ocular movements • Weakness in one extremity or one side • Headache: constant, increasing in intensity, or aggravated by movement or straining 20 Copyright © 2008 Lippincott Williams & Wilkins.
Manifestations of Increased ICP —Late • Respiratory and vasomotor changes • VS: – Cushing’s triad: bradycardia, hypertension (with widened pulse pressure), and bradypnea • Vomiting 21 Copyright © 2008 Lippincott Williams & Wilkins.
Manifestations of Increased ICP —Late (cont. ) • Further deterioration of LOC; stupor to coma • Hemiplegia, decortication, decerebration, or flaccidity • Respiratory pattern alterations including Cheyne-Stokes breathing and arrest • Loss of brain stem reflexes: pupil, gag, corneal, and swallowing Copyright © 2008 Lippincott Williams & Wilkins. 22
Increased Intracranial Pressure • Diagnostic studies – CT, cerebral angiogram, MRI, direct pressure measurement (via ventriculostomy) • Complications – – Inadequate cerebral perfusion Brain stem herniation Diabetes insipidus SIADH 23 Copyright © 2008 Lippincott Williams & Wilkins.
Increased Intracranial Pressure Collaborative Care – Monitoring ICP • Usually with ventriculostomy for ICP monitoring – Decreasing cerebral edema • Osmotic diuretics • Corticosteroids – Controlling fever – Cerebral oxygenation – Maintaining cerebral perfusion • Maintaining systemic BP and increasing CO 24 Copyright © 2008 Lippincott Williams & Wilkins.
Increased Intracranial Pressure – Reducing metabolic cellular demands • Sedation (propofol most common) • Barbiturate coma – Reducing CSF and IC blood volume • Ventriculostomy - CSF drainage • Hyperventilation as short term measure only for refractory increased ICP 25 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Assessment of the Patient With Increased Intracranial Pressure • Conduct frequent and ongoing neurologic assessment • Evaluate neurologic status as completely as possible • Glasgow Coma Scale • Pupil checks • Assess selected cranial nerves • Take frequent vital signs • Assess intracranial pressure 26 Copyright © 2008 Lippincott Williams & Wilkins.
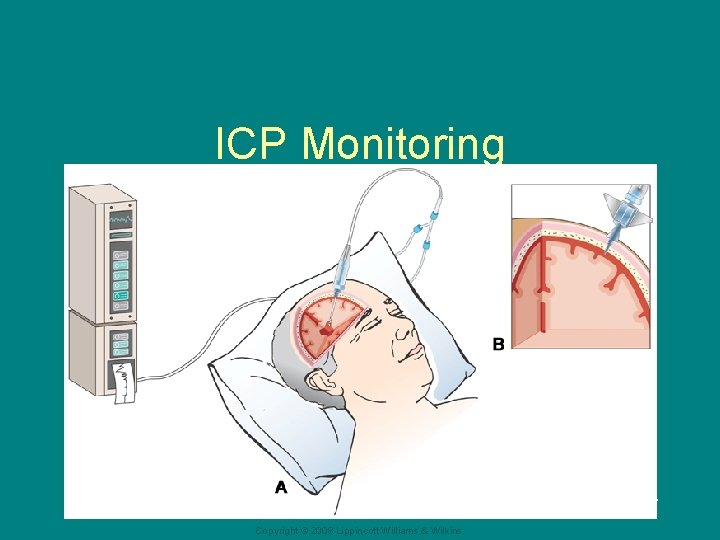
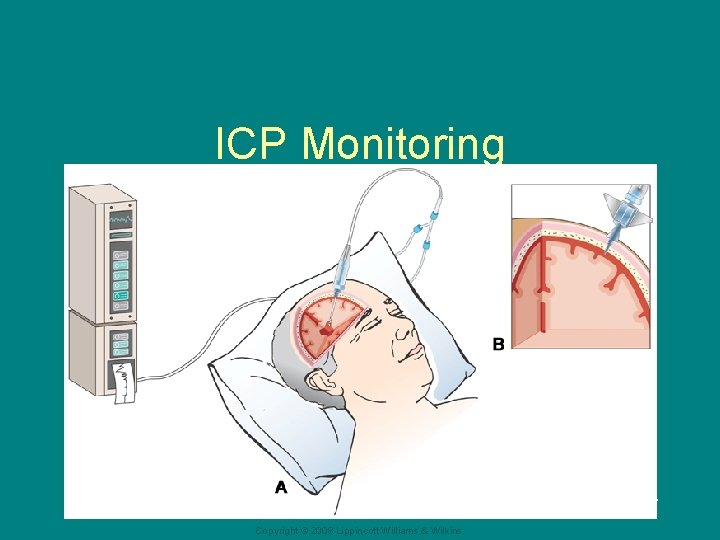
ICP Monitoring 27 Copyright © 2008 Lippincott Williams & Wilkins.
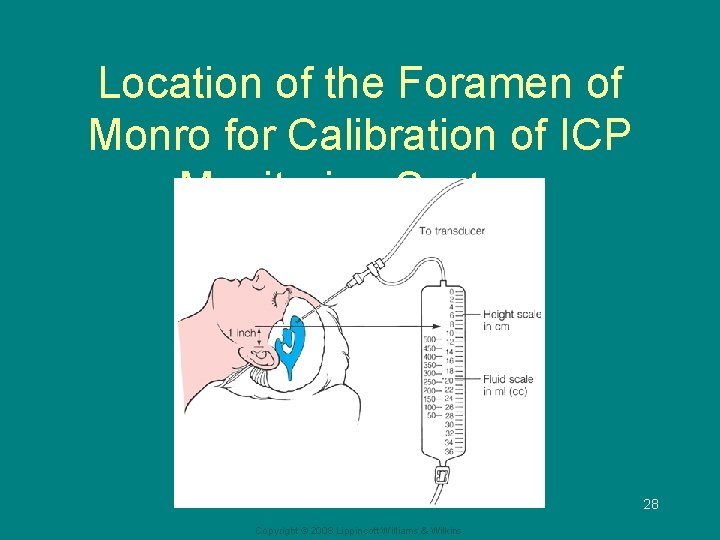
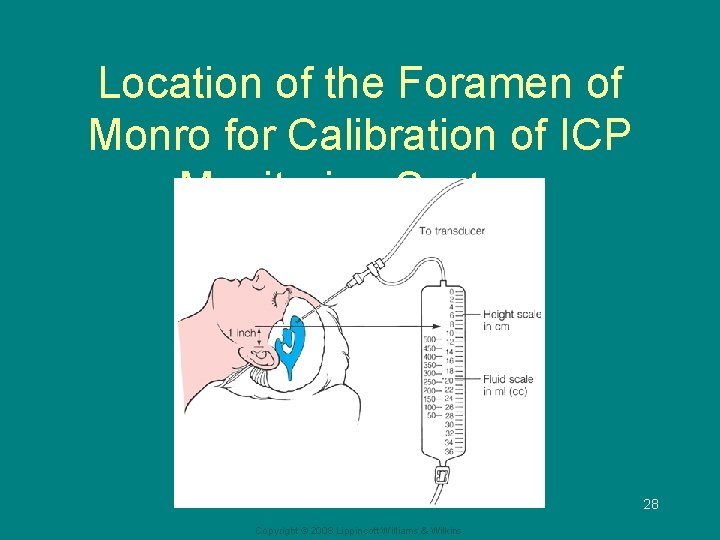
Location of the Foramen of Monro for Calibration of ICP Monitoring System 28 Copyright © 2008 Lippincott Williams & Wilkins.
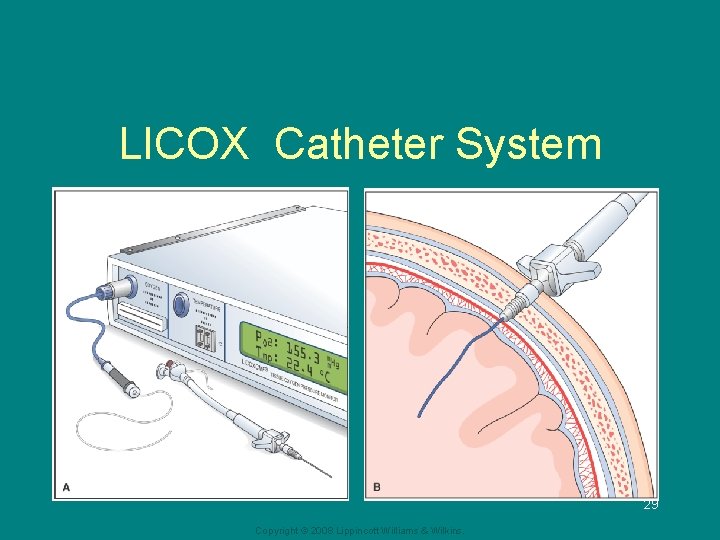
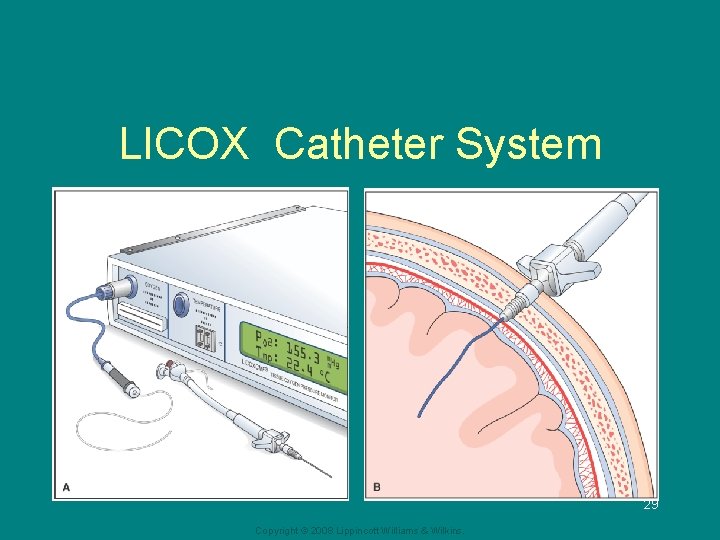
LICOX Catheter System 29 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Diagnosis of the Patient With Increased Intracranial Pressure • Ineffective tissue perfusion, cerebral • Ineffective airway clearance • Ineffective breathing pattern • Deficient fluid volume related to fluid restriction • Risk for infection related to ICP monitoring • Impaired physical mobility Copyright © 2008 Lippincott Williams & Wilkins. 30
Nursing Process—Planning for Patient With Increased Intracranial Pressure • Major goals may include: – Maintenance of patent airway – Normalization of respirations – Adequate cerebral tissue perfusion – Fluid balance – Absence of infection – Absence of complications 31 Copyright © 2008 Lippincott Williams & Wilkins.
Interventions • Frequent monitoring of respiratory status, LOC, lung sounds and measure to maintain a patent airway • Position with the head in neutral position and HOB elevation to promote venous drainage • Avoid hip flexion, Valsalva maneuver, abdominal distention, or other stimuli that may increase ICP • Maintain a calm, quiet atmosphere and protect patient from stress • Monitor fluid status carefully; during acute phase, monitor I&O every hour • Use strict sterile technique for management of ICP monitoring system • Monitor for signs/symptoms of infection Copyright © 2008 Lippincott Williams & Wilkins. 32
Interventions • Monitor for early signs of increased ICP – LOC change, pupillary/EOM changes, weakness, HA • Monitor for late signs of increased ICP – LOC deteriorates, Cushing’s triad, vomiting, posturing, loss of reflexes • Monitor ICP if indicated • Monitor for secondary complications 33 Copyright © 2008 Lippincott Williams & Wilkins.
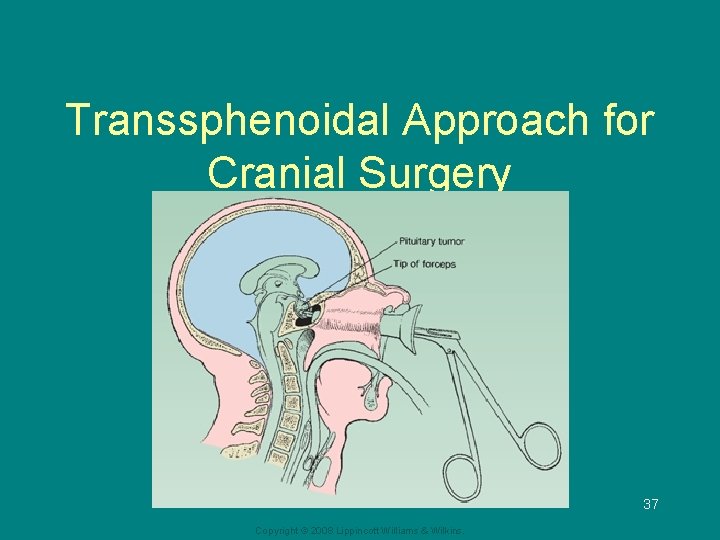
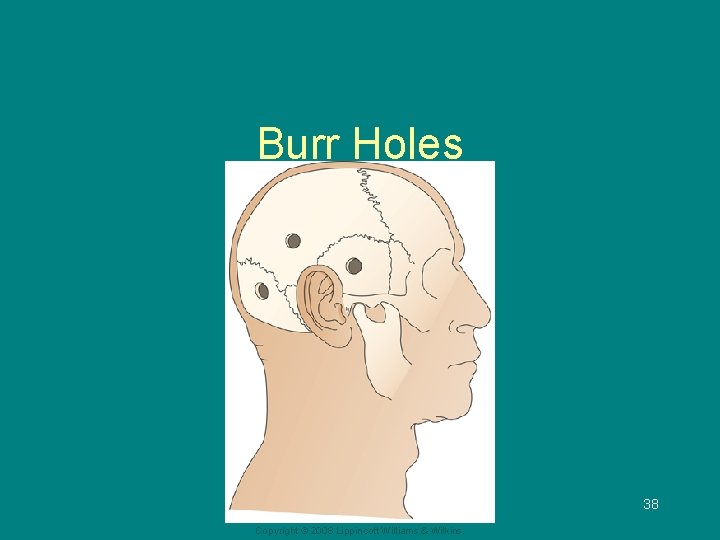
Intracranial Surgery • Craniotomy: opening of the skull – Purposes: remove tumor, relieve elevated ICP, evacuate a blood clot, and control hemorrhage • Craniectomy: excision of a portion of the skull • Burr holes: circular openings for exploration or diagnosis, to provide access to ventricles, for shunting procedures, to aspirate a hematoma or abscess, or to make a bone flap 34 Copyright © 2008 Lippincott Williams & Wilkins.
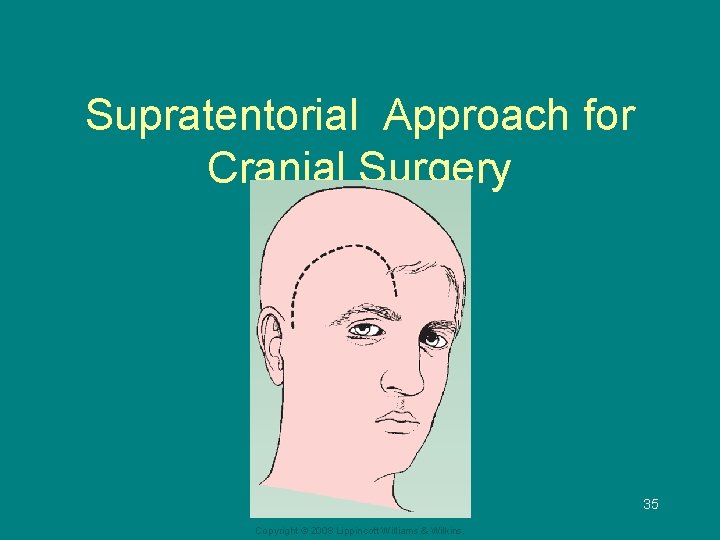
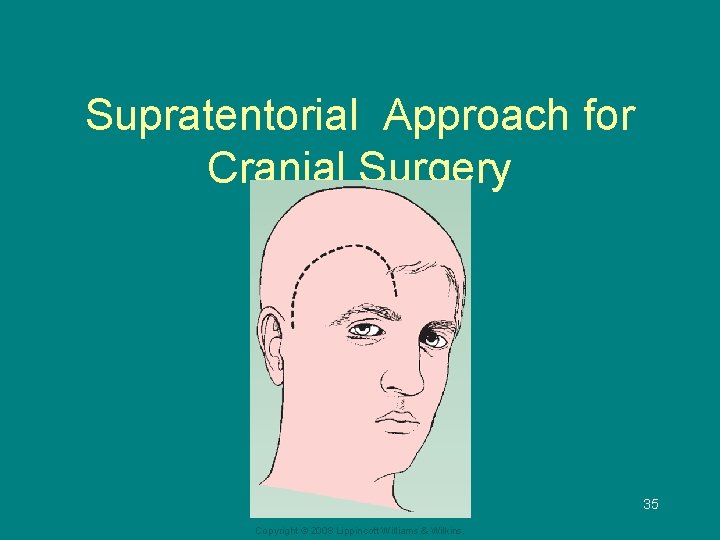
Supratentorial Approach for Cranial Surgery 35 Copyright © 2008 Lippincott Williams & Wilkins.
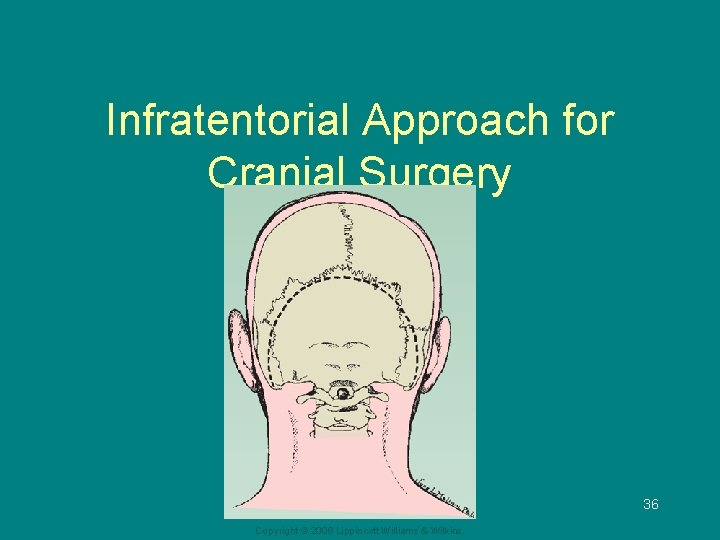
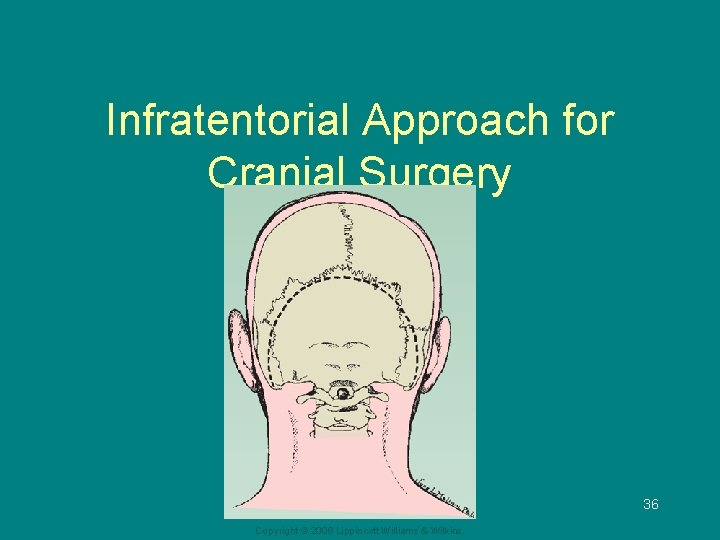
Infratentorial Approach for Cranial Surgery 36 Copyright © 2008 Lippincott Williams & Wilkins.
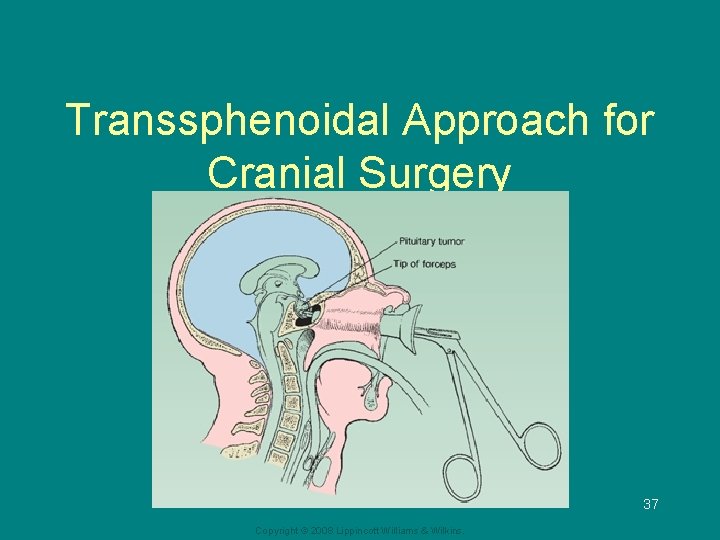
Transsphenoidal Approach for Cranial Surgery 37 Copyright © 2008 Lippincott Williams & Wilkins.
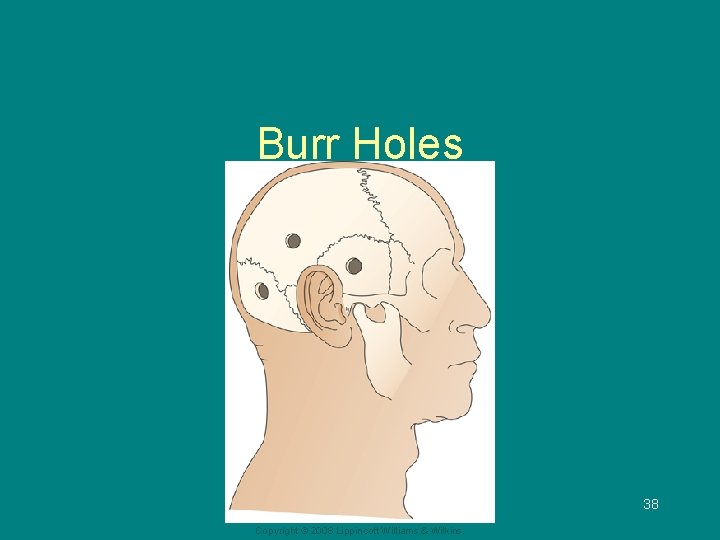
Burr Holes 38 Copyright © 2008 Lippincott Williams & Wilkins.
Preoperative Care—Medical Management • Preoperative diagnostic procedures may include CT scan, MRI, angiography, or transcranial Doppler flow studies • Medications are usually given to reduce risk of seizures (phenytoin) • Corticosteroids, fluid restriction, hyperosmotic agents (mannitol), and diuretics may be used to reduce cerebral edema • Antibiotics may be administered to reduce potential infection Copyright © 2008 Lippincott Williams & Wilkins. 39
Preoperative Care—Nursing Management • Obtain baseline neurologic assessment • Assess patient and family understanding of and preparation for surgery • Provide information, reassurance, and support 40 Copyright © 2008 Lippincott Williams & Wilkins.
Postoperative Care • Postoperative care is aimed at detecting and reducing cerebral edema, relieving pain, preventing seizures, and monitoring ICP and neurologic status • The patient may be intubated and have arterial and central venous lines, ventriculostomy 41 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Process—Assessment of the Patient Undergoing Intracranial Surgery • Careful, frequent monitoring of respiratory function, including ABGs • Monitor VS and LOC frequently; note any potential signs of increasing ICP • Assess dressing and for evidence of bleeding or CSF drainage • Monitor for potential seizures; if seizures occur, carefully record and report them • Monitor for signs and symptoms of complications • Monitor fluid status and laboratory data Copyright © 2008 Lippincott Williams & Wilkins. 42
Nursing Process—Diagnosis of the Patient Undergoing Intracranial Surgery • Ineffective tissue perfusion • Disturbed sensory perception • Body image disturbance • Impaired communication (aphasia) • Risk for impaired skin integrity • Impaired physical mobility 43 Copyright © 2008 Lippincott Williams & Wilkins.
Collaborative Problems/Potential Complications • Increased ICP • Bleeding and hypovolemic shock • Fluid and electrolyte disturbances • Infection • Seizures Copyright © 2008 Lippincott Williams & Wilkins. 44
Nursing Process—Planning the Care of the Patient Undergoing Intracranial Surgery • Major goals may include: – – – Improved cerebral tissue perfusion Adequate thermoregulation Normal ventilation and gas exchange Ability to cope with sensory deprivation Adaptation to changes in body image Absence of complications 45 Copyright © 2008 Lippincott Williams & Wilkins.
Maintaining Cerebral Perfusion • Monitor respiratory status; even slight hypoxia or hypercapnia can affect cerebral perfusion • Assess VS and neurologic status every 15 minutes to one hour • Implement strategies to reduce cerebral edema; cerebral edema peaks in 24 to 36 hours • Implement strategies to control factors that increase ICP • Avoid extreme head rotation • Head of bed may be elevated 30° according to needs related to the surgery and surgeon’s preference 46 Copyright © 2008 Lippincott Williams & Wilkins.
Interventions • Regulate temperature – Cover patient appropriately – Treat high temperature elevations vigorously; apply ice bags, use hypothermia blanket, and administer prescribed acetaminophen • Improve gas exchange – Turn and reposition the patient every 2 hours – Encourage deep breathing and incentive spirometry – Suction or encourage coughing cautiously as needed (suctioning and coughing increase ICP) – Humidify oxygen to help loosen secretions Copyright © 2008 Lippincott Williams & Wilkins. 47
Interventions (cont. ) • Sensory deprivation – Periorbital may impair vision, so announce your presence to avoid startling the patient; cool compresses over eyes and HOB elevation may be used to reduce edema if not contraindicated • Enhance self-image – Encourage verbalization – Encourage social interaction and social support – Pay attention to grooming – Cover head with. Copyright turban © 2008 Lippincott Williams & Wilkins. 48
Interventions (cont. ) • Monitor I&O, weight, blood glucose, serum, urine electrolyte levels, osmolality, and urine specific gravity • Preventing infections – Assess incision for signs of hematoma or infection – Assess for potential CSF leak – Instruct patient to avoid coughing, sneezing, or nose blowing, which may increase the risk of CSF leakage – Use strict aseptic technique • Monitoring for increased ICP and bleeding 49 Copyright © 2008 Lippincott Williams & Wilkins.
Seizures • Uncontrolled, paroxysmal electrical discharge of neurons in the brain that disrupts normal function • Classification of seizures: see table 59 -6 – Partial seizures: begin in one part of the brain § Simple partial: consciousness remains intact § Complex partial: impairment of consciousness – Generalized seizures: involve the whole brain • Includes tonic-clonic, absence 50 Copyright © 2008 Lippincott Williams & Wilkins.
Specific Causes of Seizures • Head trauma • Drug -related processes • Infectious processes • Intracranial events • Metabolic imbalances • Medical disorders • Other • Table 58 -8 Copyright © 2008 Lippincott Williams & Wilkins. 51
Plan of Care for a Patient Experiencing a Seizure • Observation and documentation of patient signs and symptoms before, during, and after seizure – Eg, aura, type of movements, pupils, incontinence, changes in consciousness, cognitive • Nursing actions during seizure for patient safety and protection • See handout; table 59 -12 for home teaching • After seizure care, prevent complications 52 Copyright © 2008 Lippincott Williams & Wilkins.
Epilepsy • Acondition in which a person has spontaneously recurring seizures – Classified by patterns of clinical features, including onset, family history and seizure type – Idiopathic or secondary • Causes – Include idiopathic, birth trauma, head injury, infectious disease, toxins, circulatory problems, brain tumor, abcess, congenital malformations, 53 Copyright © 2008 Lippincott Williams & Wilkins.
Epilepsy • Diagosis – History and physical exam – Electroencephalogram – Video recording of seizures • Treatment – Pharmacologic (treat, not cure) • Review epilepsy meds - table 59 -9 – Surgical management • For cessation or reduction of seizures (see table 5910) 54 Copyright © 2008 Lippincott Williams & Wilkins.
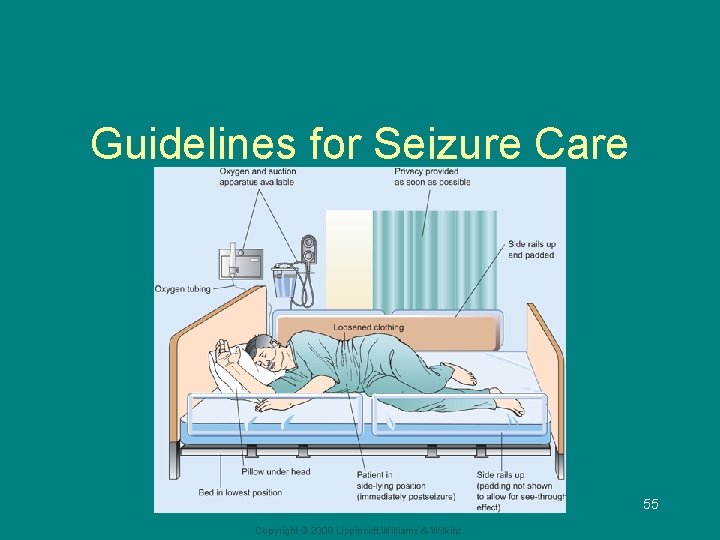
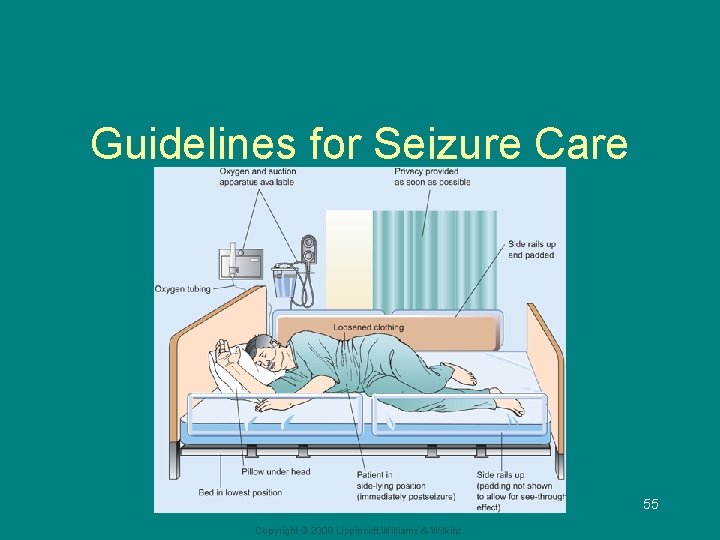
Guidelines for Seizure Care 55 Copyright © 2008 Lippincott Williams & Wilkins.
Status Epilepticus • Acute prolonged seizure activity; a series of generalized seizures that occur without full recovery of consciousness between attacks • Generally lasts longer than 30 minutes • Heavy metabolic demand may result in interference with respiration and hypoxia of the brain • Medical management is aimed at stopping the seizures – Airway – IV lorazepam, diazepam for abrupt cessation – Phenytoin or fosphenytoin for maintenace of seizure-free 56 state; phenobarbital in extreme cases Copyright © 2008 Lippincott Williams & Wilkins.
Headache • Also called cephalgia • Primary headache has no known organic cause and includes migraine, tension headache, and cluster headache • Secondary headache is a symptom with an organic cause such as a brain tumor or aneurysm • Headache may cause significant discomfort for the person and can interfere with activities and lifestyle 57 Copyright © 2008 Lippincott Williams & Wilkins.
Headache • Migraine – Characterized by periodic and recurrent attacks of severe HA lasting 4 -72 hours – Throbbing pain – Most common in women , 25 -55 years – Familial tendency – Subtypes • May be with or without aura 58 Copyright © 2008 Lippincott Williams & Wilkins.
Headache • Migraine – Triggers include menstrual cycles, bright light, stress, sleep deprivation, medications, foods (MSG, tyramine, nitrites, milk products, red wine, chocolate) – Phases • Prodrome (60%) • Aura (30%)-neurologic symptoms correspond to cerebral vasoconstriction • Headache-severe, throbbing; may have N/V, photophobia; 4 -72 hours • Recovery-exhaustion, muscle aches 59 Copyright © 2008 Lippincott Williams & Wilkins.
Headache • Migraine Treatment – Abortive - relief of HA in progress • Includes NSAIDS, opiods, triptans (serotonin receptor agonists) , ergotamine preparations (table 59 -3) – Prevention • • Avoidance of triggers Beta blockers Antiepileptics Calcium channel blockers Antidepressants Botox Relaxation therapy Copyright © 2008 Lippincott Williams & Wilkins. 60
Headache • Tension-type headache – Chronic, mild to moderate in intensity, most common type – May last days-weeks-months – Muscular origin vs. neurovascular origin – Characterized by steady pressure that usually begins in the forehead, temples, or neck – Treated symptomatically: heat, massage, analgesics, muscle relaxants 61 Copyright © 2008 Lippincott Williams & Wilkins.
Headache • Cluster headache – Severe form of vascular headache; may be precipitated by ETOH, vasodilators, nitrites, histamines – Described as sharp, stabbing, intense – Far more common in men – Treatment • Abortive may include 100% oxygen x 15 minutes, , triptans, NSAIDS, opioids • Preventive therapy may include beta blockers, ergotamine, lithium, naproxen 62 Copyright © 2008 Lippincott Williams & Wilkins.
Assessment of Headache • A detailed description of the headache is obtained • Include medication history and use • The types of headaches manifest differently in different persons, and symptoms in one individual may also may change over time • Although most headaches do not indicate serious disease, persistent headaches require investigation 63 Copyright © 2008 Lippincott Williams & Wilkins.
Assessment of Headache (cont. ) • Persons undergoing a headache evaluation require a detailed history and physical assessment with neurological exam to rule out various physical and psychological causes • Diagnostic testing may be used to evaluate the underlying cause if the neurologic exam is abnormal 64 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Management of Headache—Pain • Provide individualized care and treatment • Prophylactic medications and teaching • Migraines and cluster headaches require abortive medications instituted as soon as possible with onset • Provide medications as prescribed • Provide comfort measures 65 Copyright © 2008 Lippincott Williams & Wilkins.
Nursing Management of Headache— Teaching • Help patient identify triggers and develop preventive strategies and lifestyle changes for headache prevention • Provide medication instruction and treatment regimen • Implement stress reduction techniques • Implement nonpharmacologic therapies • Provide follow-up care • Encourage healthy lifestyle and health promotion activities Copyright © 2008 Lippincott Williams & Wilkins. 66