Management of Macrophage Activation Syndrome MAS Vahid Ziaee



- Slides: 25
Management of Macrophage Activation Syndrome (MAS) Vahid Ziaee MD Children Medical Centre Tehran University of Medical Sciences
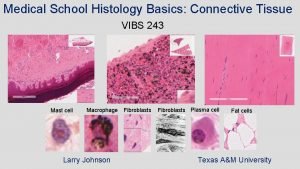
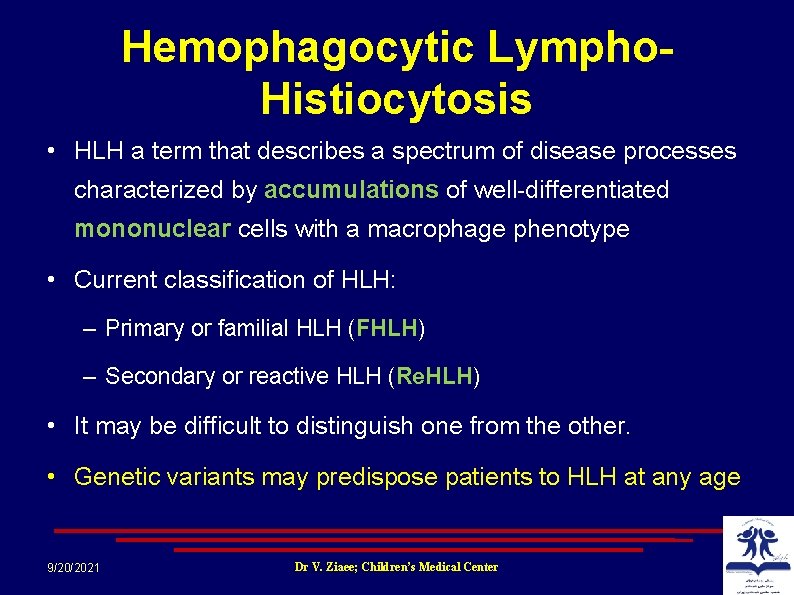
Hemophagocytic Lympho. Histiocytosis • HLH a term that describes a spectrum of disease processes characterized by accumulations of well differentiated mononuclear cells with a macrophage phenotype • Current classification of HLH: – Primary or familial HLH (FHLH) – Secondary or reactive HLH (Re. HLH) • It may be difficult to distinguish one from the other. • Genetic variants may predispose patients to HLH at any age 9/20/2021 Dr V. Ziaee; Children’s Medical Center
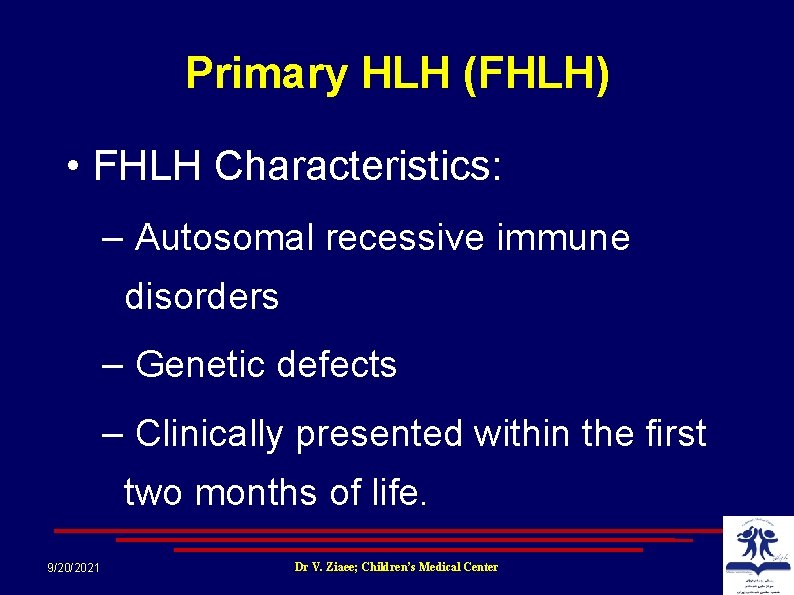
Primary HLH (FHLH) • FHLH Characteristics: – Autosomal recessive immune disorders – Genetic defects – Clinically presented within the first two months of life. 9/20/2021 Dr V. Ziaee; Children’s Medical Center
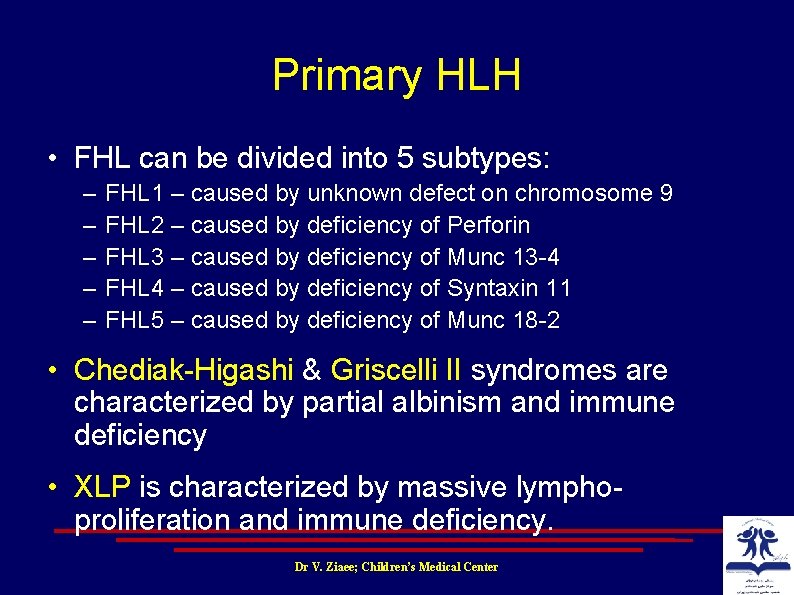
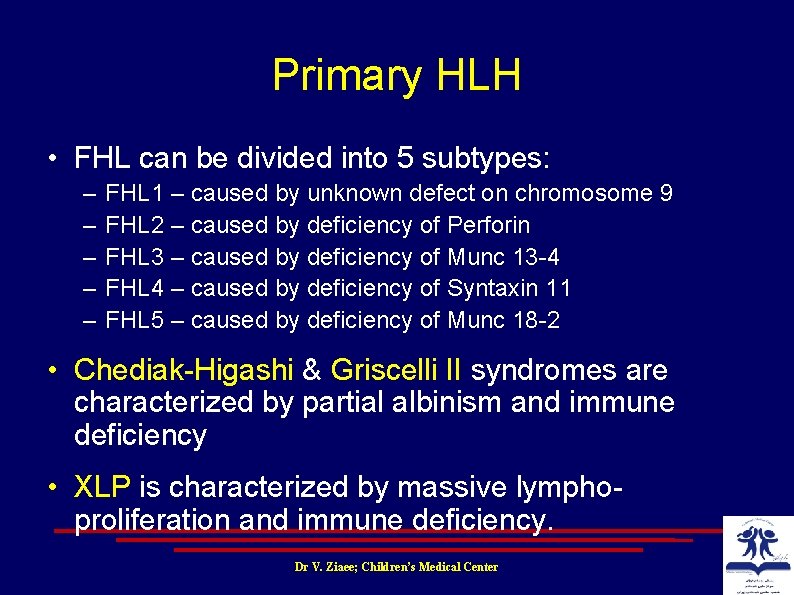
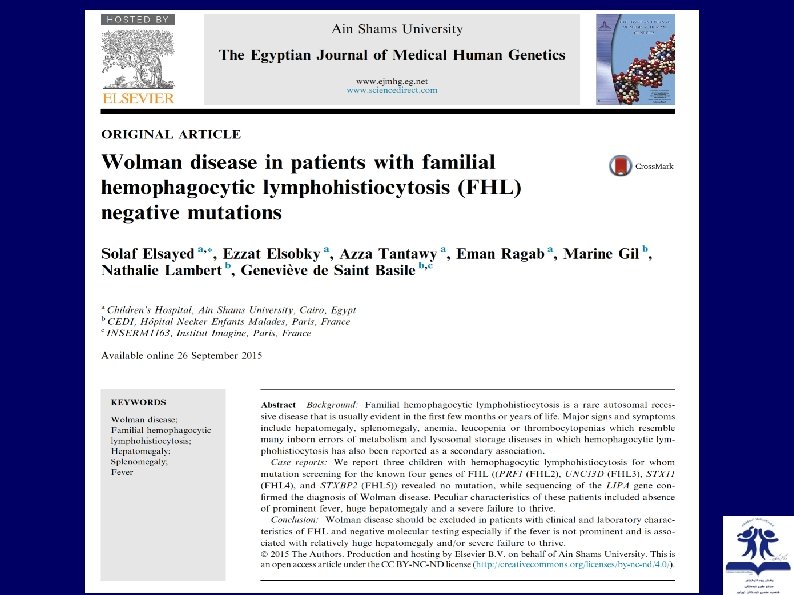
Primary HLH • FHL can be divided into 5 subtypes: – – – FHL 1 – caused by unknown defect on chromosome 9 FHL 2 – caused by deficiency of Perforin FHL 3 – caused by deficiency of Munc 13 4 FHL 4 – caused by deficiency of Syntaxin 11 FHL 5 – caused by deficiency of Munc 18 2 • Chediak Higashi & Griscelli II syndromes are characterized by partial albinism and immune deficiency • XLP is characterized by massive lympho proliferation and immune deficiency. Dr V. Ziaee; Children’s Medical Center
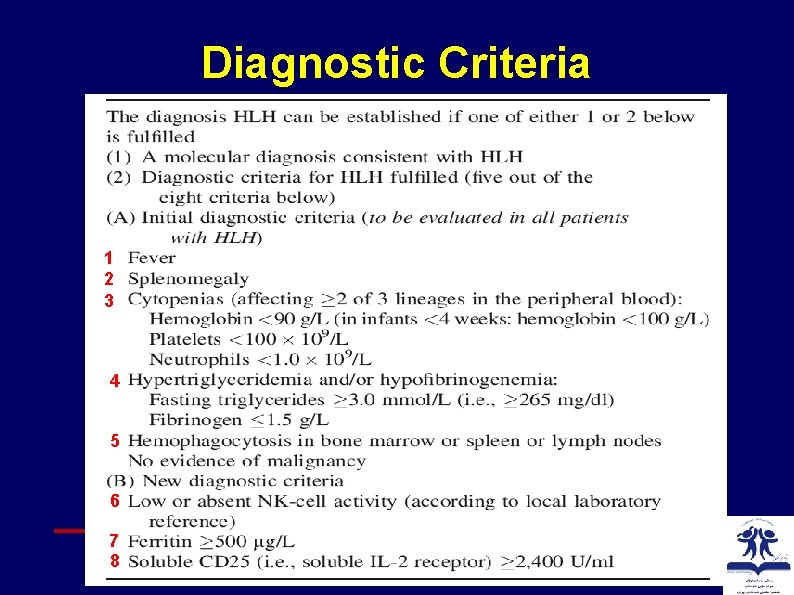
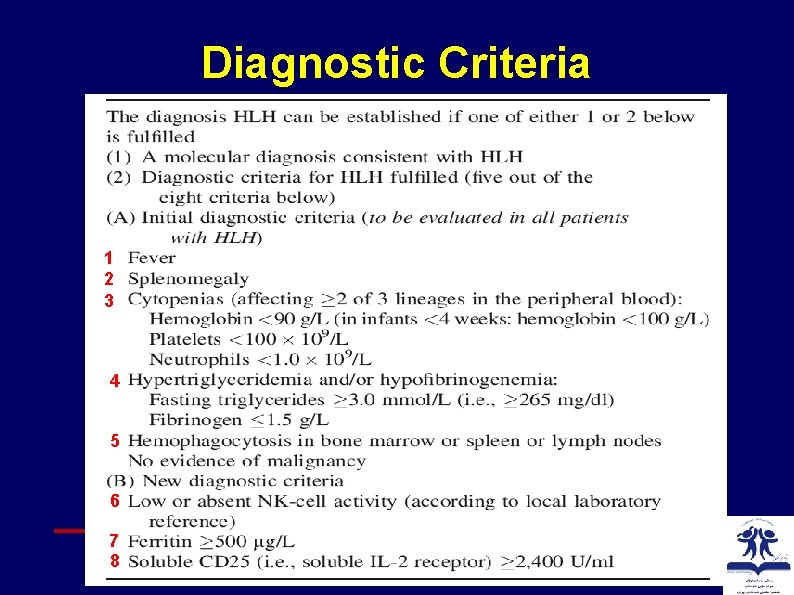
Diagnostic Criteria 1 2 3 4 5 6 7 8 Dr V. Ziaee; Children’s Medical Center

Diagnostic guideline Dr V. Ziaee; Children’s Medical Center
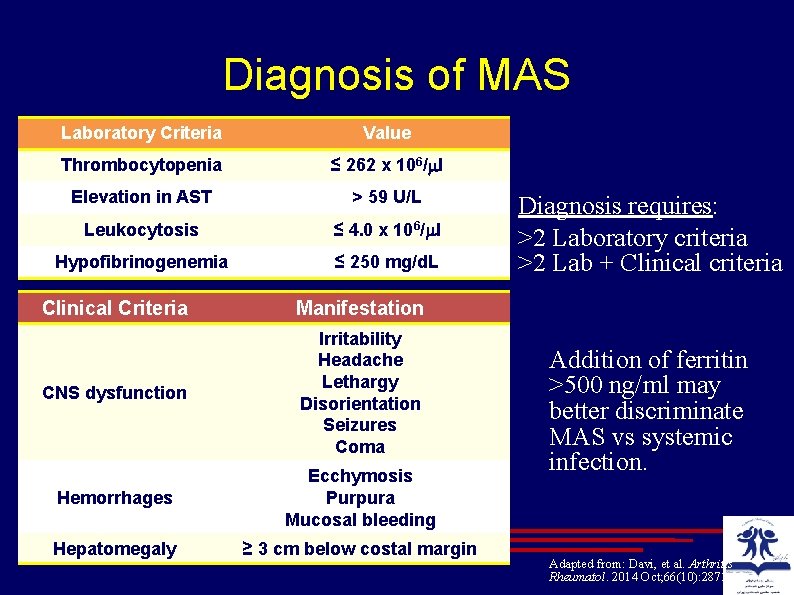
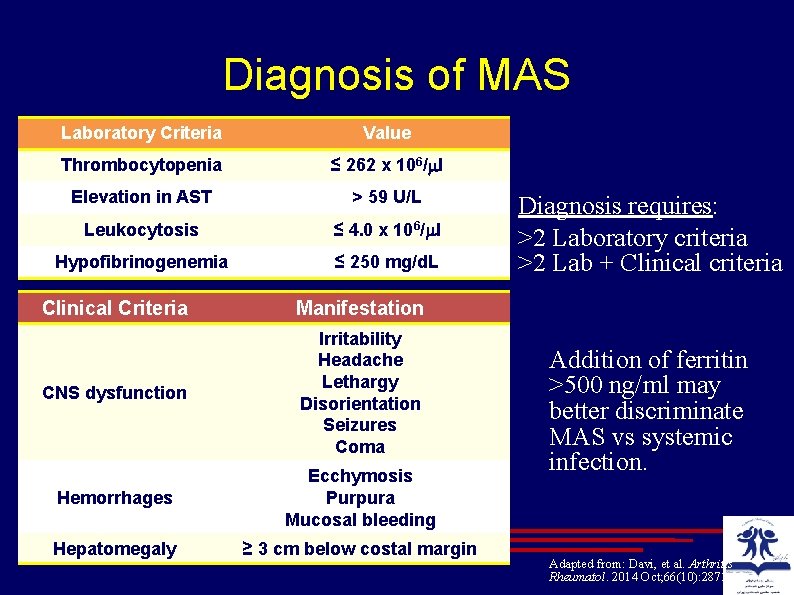
Diagnosis of MAS Laboratory Criteria Value Thrombocytopenia ≤ 262 x 106/ l Elevation in AST > 59 U/L Leukocytosis ≤ 4. 0 x 106/ l Hypofibrinogenemia ≤ 250 mg/d. L Clinical Criteria Manifestation CNS dysfunction Irritability Headache Lethargy Disorientation Seizures Coma Hemorrhages Ecchymosis Purpura Mucosal bleeding Hepatomegaly ≥ 3 cm below costal margin Diagnosis requires: >2 Laboratory criteria >2 Lab + Clinical criteria Addition of ferritin >500 ng/ml may better discriminate MAS vs systemic infection. Adapted from: Davi, et al. Arthritis Rheumatol. 2014 Oct; 66(10): 2871 -80.

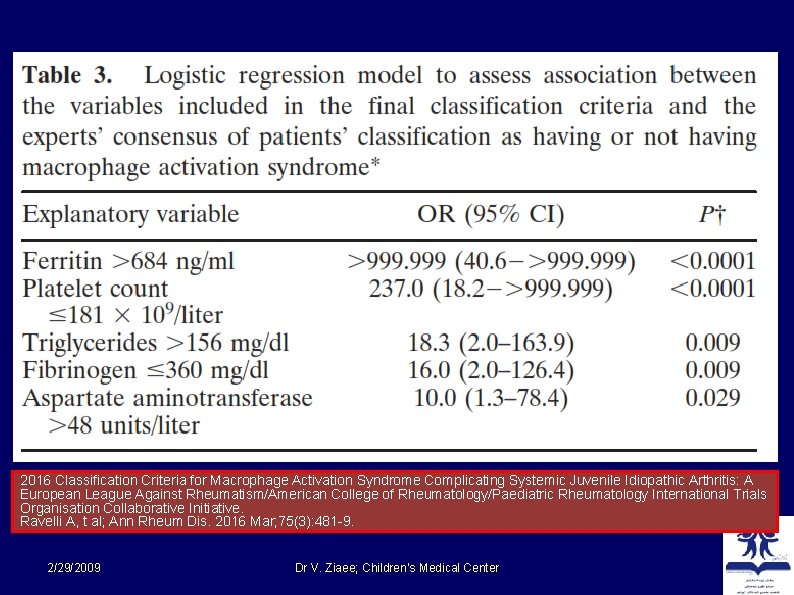
New Diagnostic Criteria 1 2 3 4 2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Ravelli A, t al; Ann Rheum Dis. 2016 Mar; 75(3): 481 9. 2/29/2009 Dr V. Ziaee; Children’s Medical Center
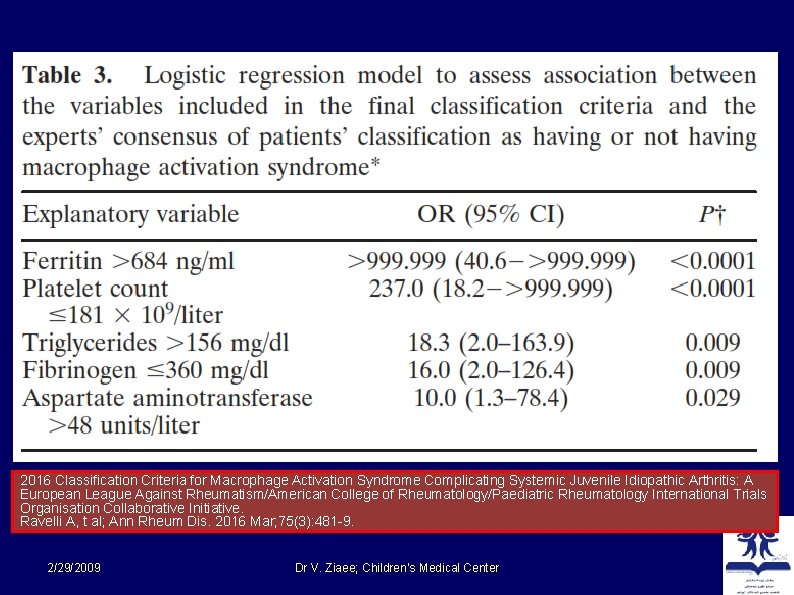
2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Ravelli A, t al; Ann Rheum Dis. 2016 Mar; 75(3): 481 9. 2/29/2009 Dr V. Ziaee; Children’s Medical Center
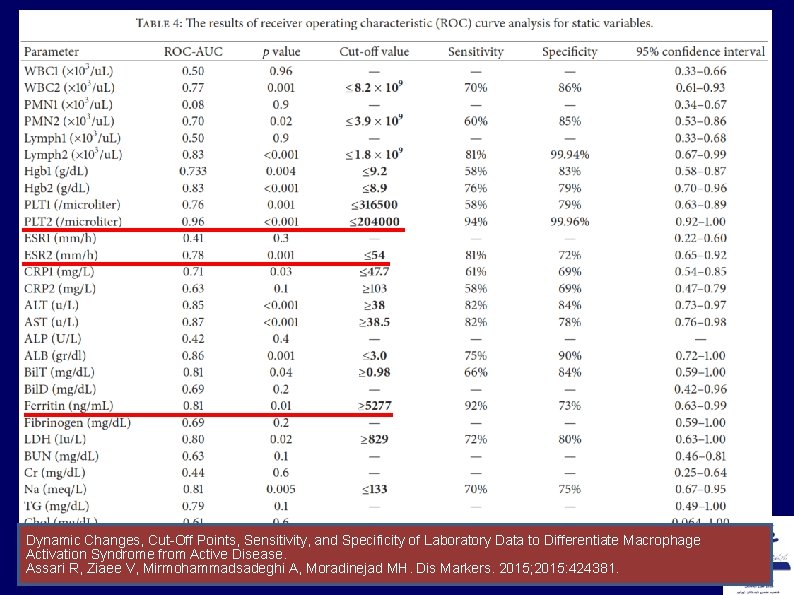
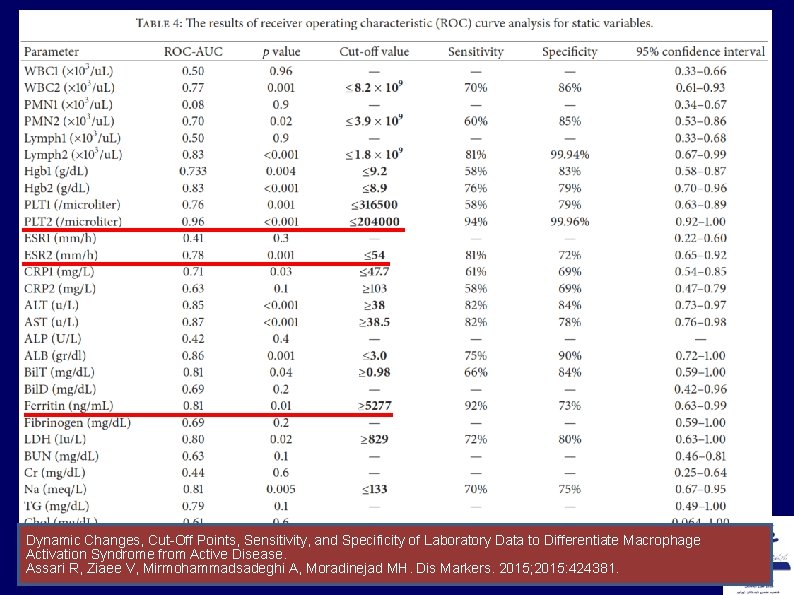
Dynamic Changes, Cut Off Points, Sensitivity, and Specificity of Laboratory Data to Differentiate Macrophage Activation Syndrome from Active Disease. 2/29/2009 Dr. Moradinejad V. Ziaee; Children’s Medical Center 2015; 2015: 424381. Assari R, Ziaee V, Mirmohammadsadeghi A, MH. Dis Markers.
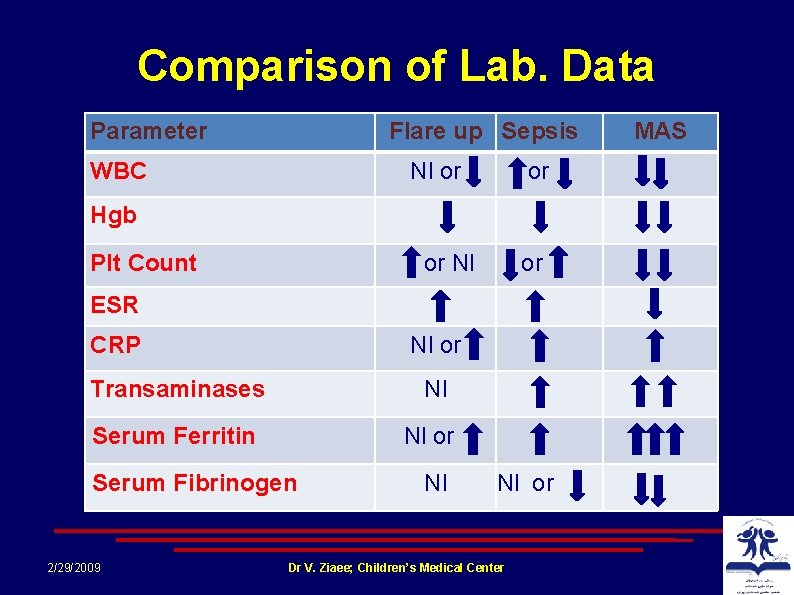
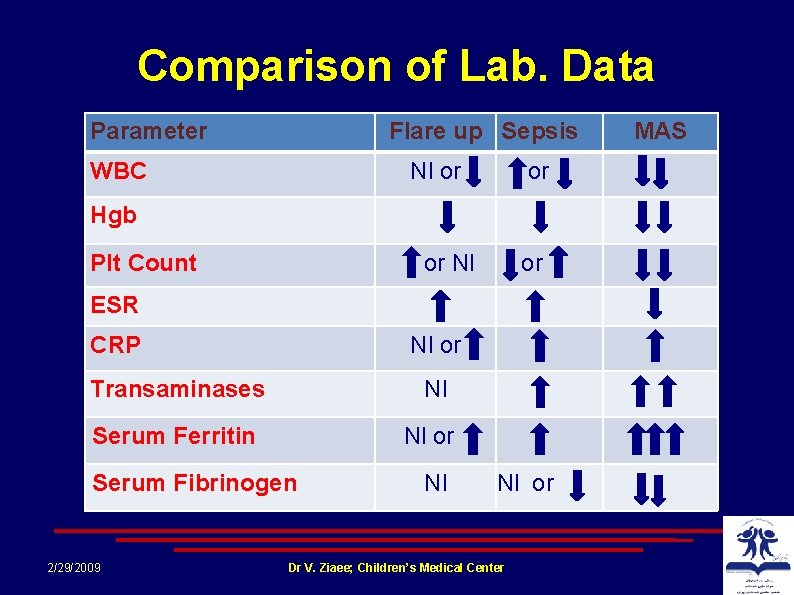
Comparison of Lab. Data Parameter Flare up Sepsis WBC Nl or or Hgb Plt Count or Nl or ESR CRP Nl or Transaminases Nl Serum Ferritin Nl or Serum Fibrinogen 2/29/2009 Nl Nl or Dr V. Ziaee; Children’s Medical Center MAS
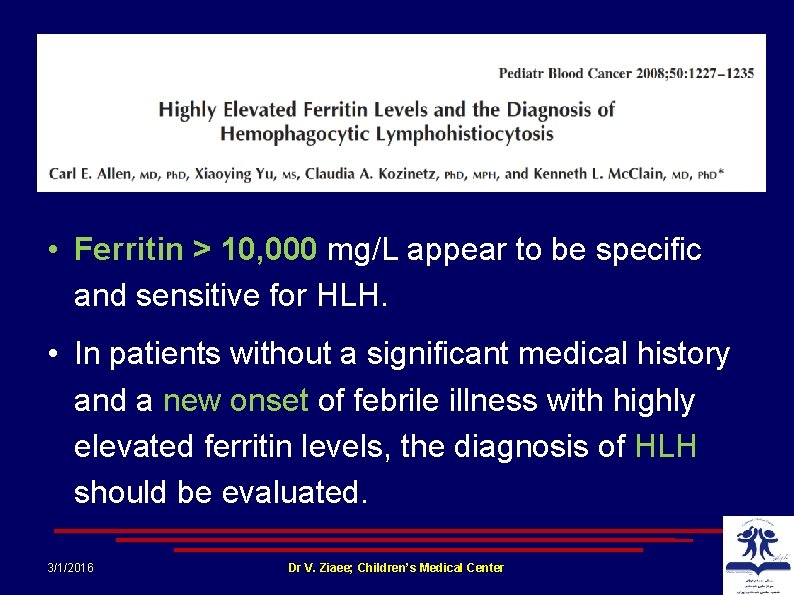
• Ferritin > 10, 000 mg/L appear to be specific and sensitive for HLH. • In patients without a significant medical history and a new onset of febrile illness with highly elevated ferritin levels, the diagnosis of HLH should be evaluated. 3/1/2016 Dr V. Ziaee; Children’s Medical Center
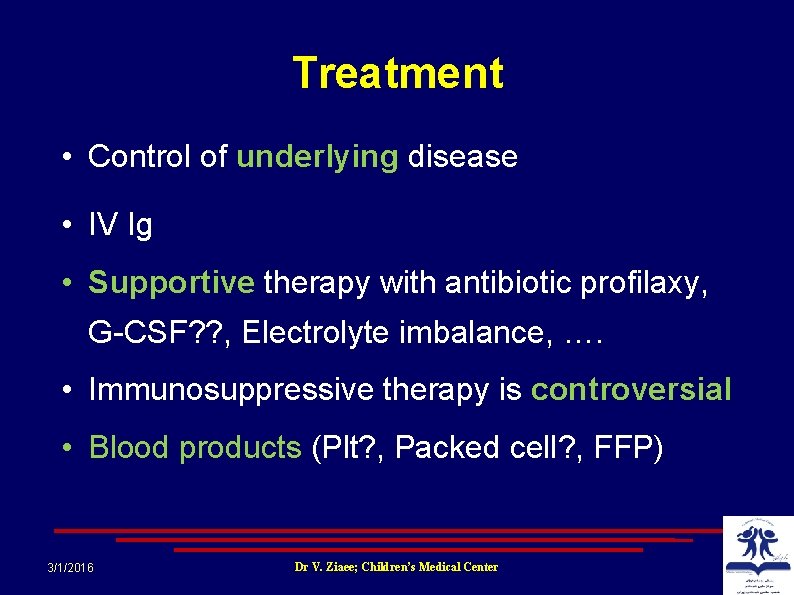
Treatment • Control of underlying disease • IV Ig • Supportive therapy with antibiotic profilaxy, G CSF? ? , Electrolyte imbalance, …. • Immunosuppressive therapy is controversial • Blood products (Plt? , Packed cell? , FFP) 3/1/2016 Dr V. Ziaee; Children’s Medical Center
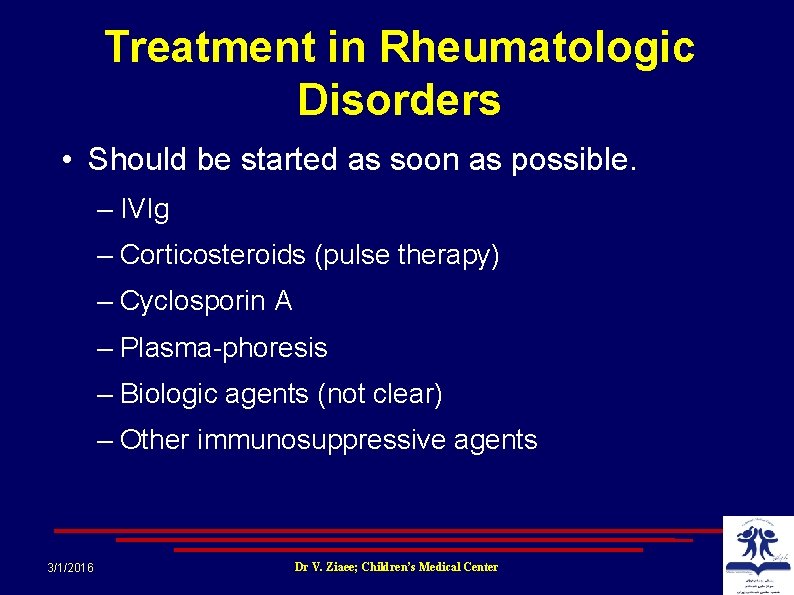
Treatment in Rheumatologic Disorders • Should be started as soon as possible. – IVIg – Corticosteroids (pulse therapy) – Cyclosporin A – Plasma phoresis – Biologic agents (not clear) – Other immunosuppressive agents 3/1/2016 Dr V. Ziaee; Children’s Medical Center
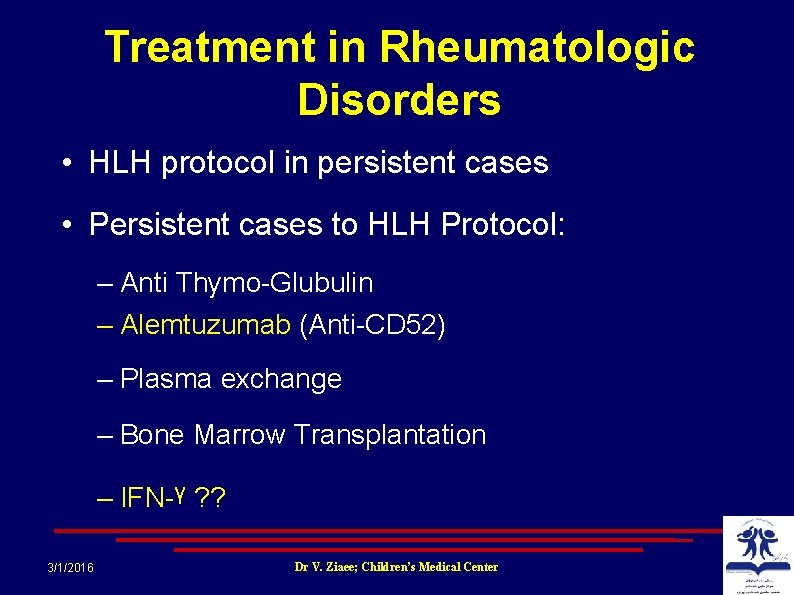
Treatment in Rheumatologic Disorders • HLH protocol in persistent cases • Persistent cases to HLH Protocol: – Anti Thymo Glubulin – Alemtuzumab (Anti CD 52) – Plasma exchange – Bone Marrow Transplantation – IFN ᵞ ? ? 3/1/2016 Dr V. Ziaee; Children’s Medical Center
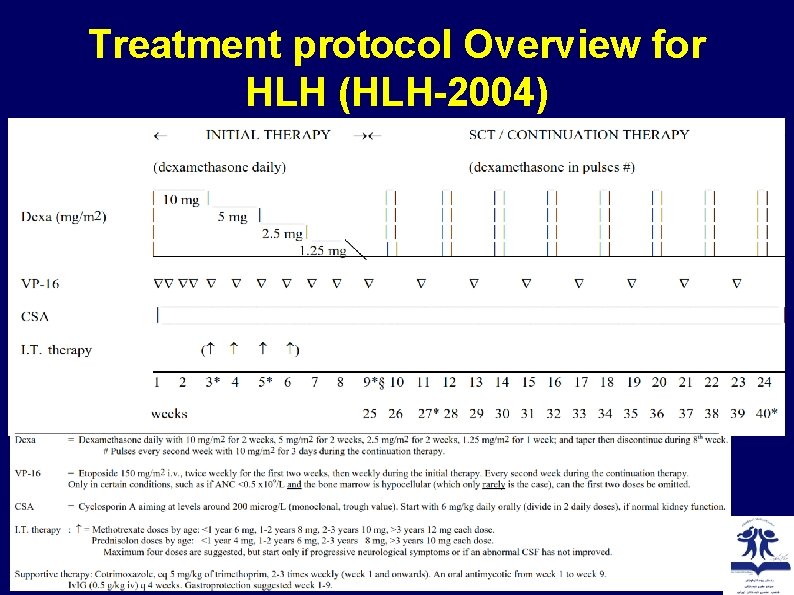
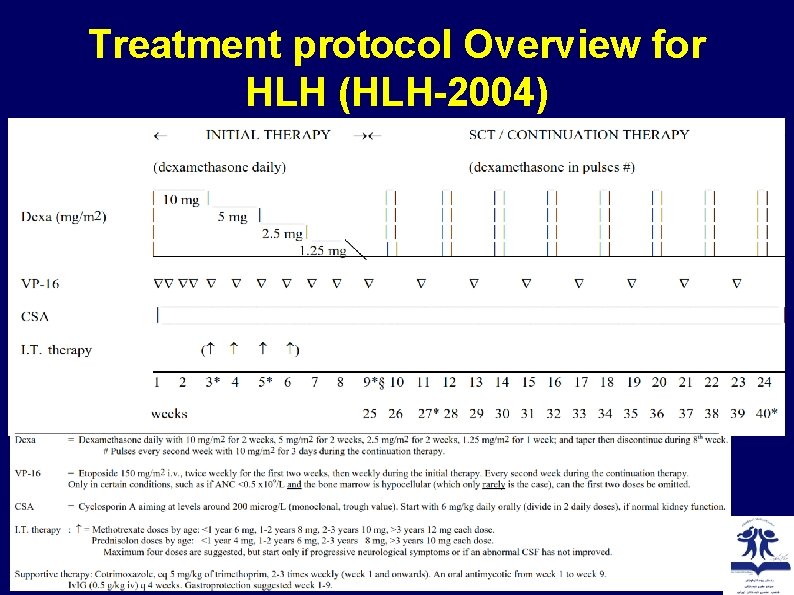
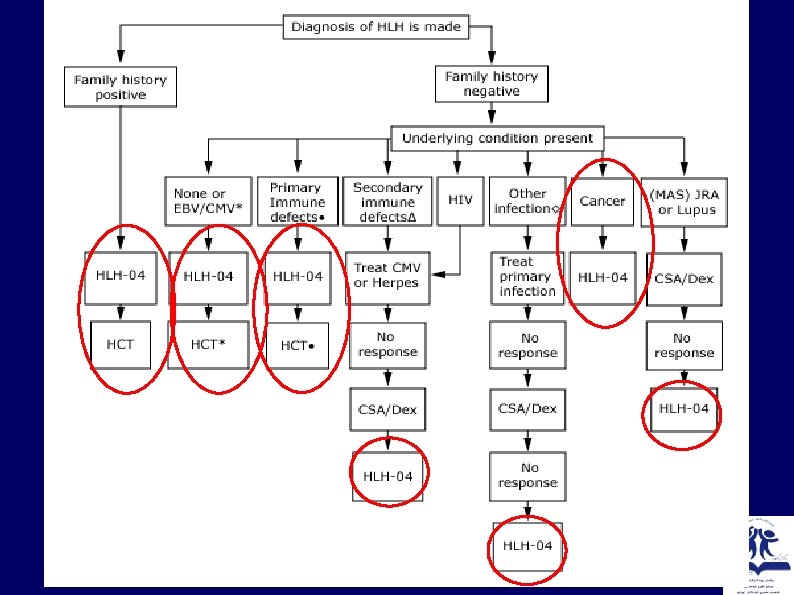
Treatment protocol Overview for HLH (HLH-2004) 3/3/2016 Dr V. Ziaee; Children’s Medical Center
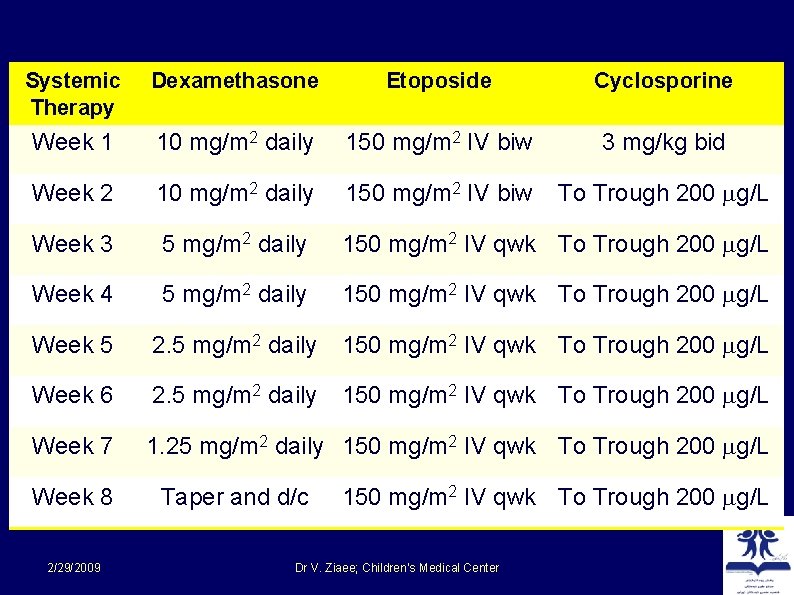
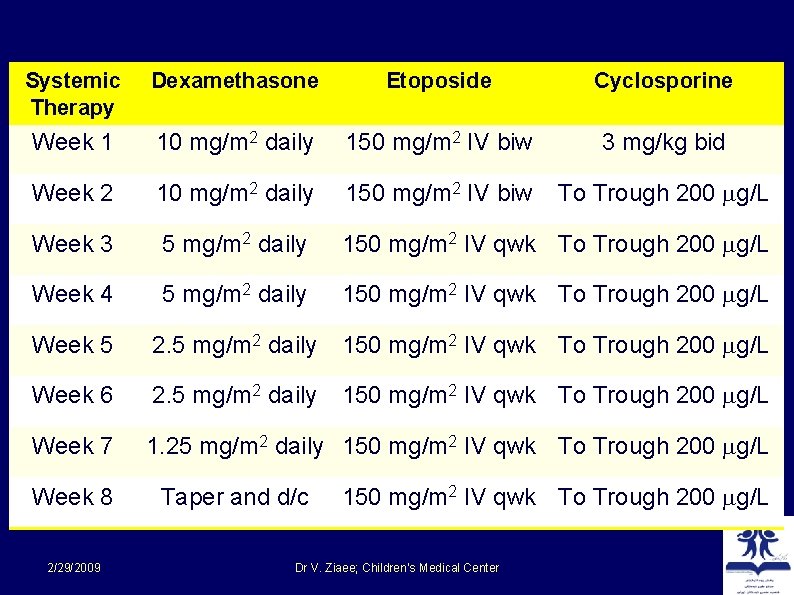
Systemic Therapy Dexamethasone Etoposide Cyclosporine Week 1 10 mg/m 2 daily 150 mg/m 2 IV biw 3 mg/kg bid Week 2 10 mg/m 2 daily 150 mg/m 2 IV biw To Trough 200 g/L Week 3 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 4 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 5 2. 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 6 2. 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 7 1. 25 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 8 2/29/2009 Taper and d/c 150 mg/m 2 IV qwk To Trough 200 g/L Dr V. Ziaee; Children’s Medical Center
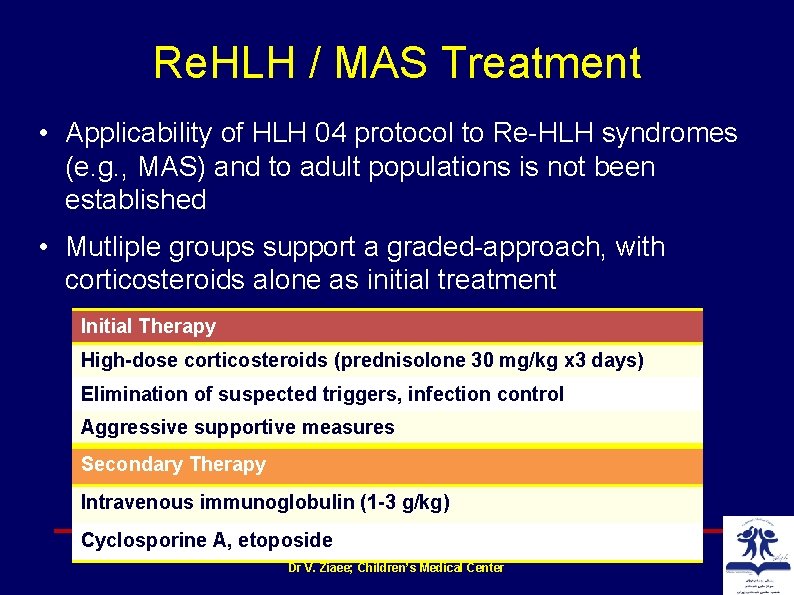
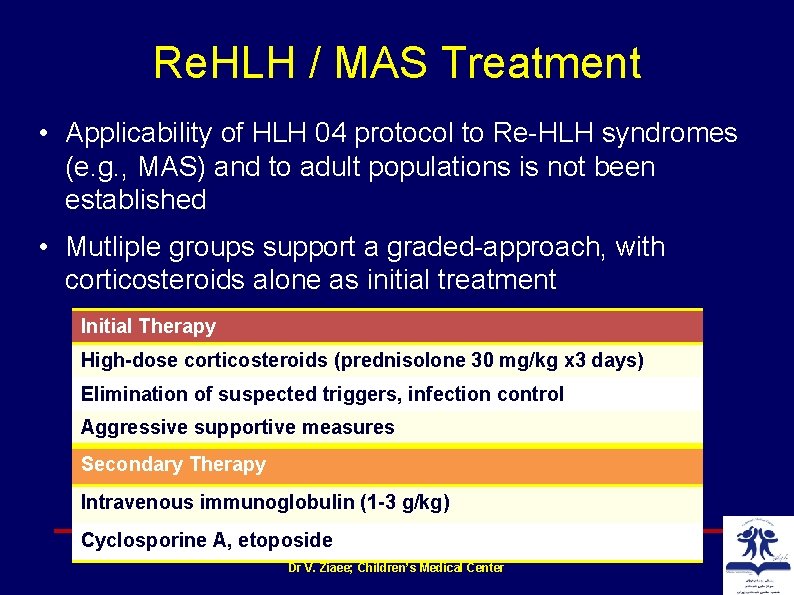
Re. HLH / MAS Treatment • Applicability of HLH 04 protocol to Re HLH syndromes (e. g. , MAS) and to adult populations is not been established • Mutliple groups support a graded approach, with corticosteroids alone as initial treatment Initial Therapy High-dose corticosteroids (prednisolone 30 mg/kg x 3 days) Elimination of suspected triggers, infection control Aggressive supportive measures Secondary Therapy Intravenous immunoglobulin (1 -3 g/kg) Cyclosporine A, etoposide Dr V. Ziaee; Children’s Medical Center
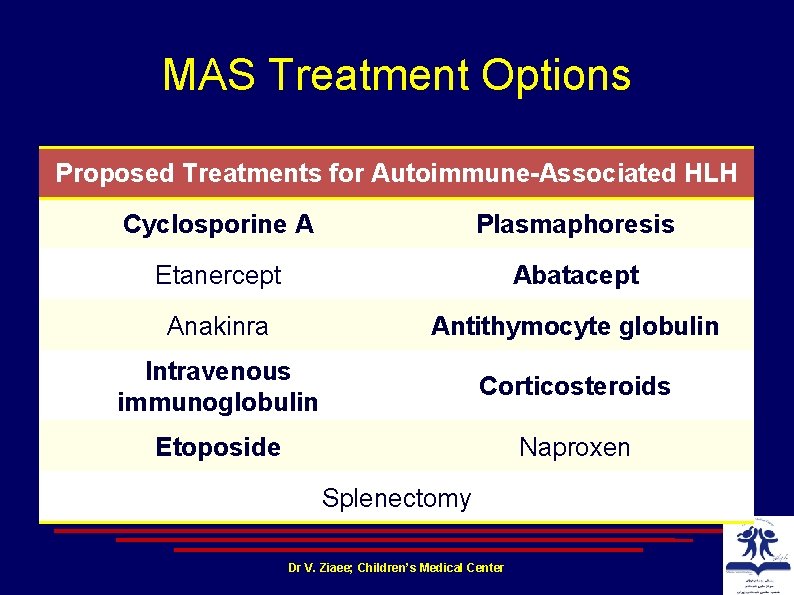
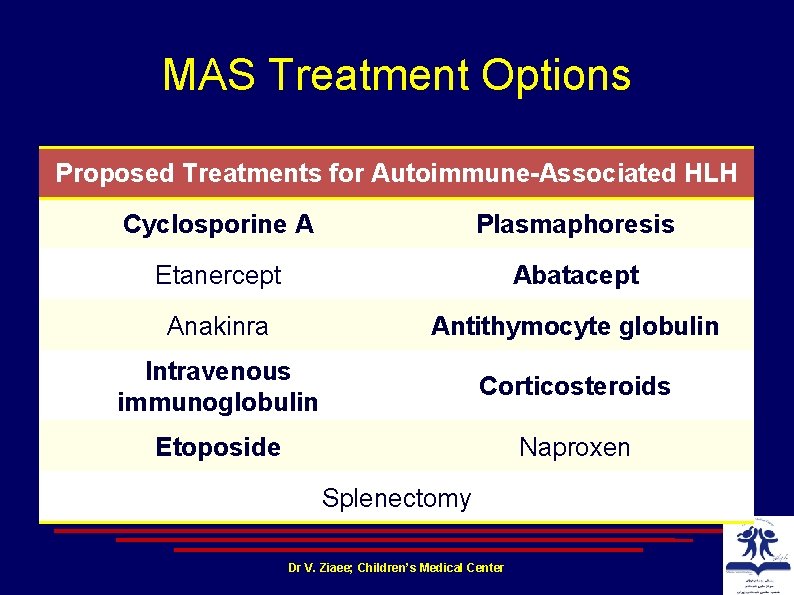
MAS Treatment Options Proposed Treatments for Autoimmune-Associated HLH Cyclosporine A Plasmaphoresis Etanercept Abatacept Anakinra Antithymocyte globulin Intravenous immunoglobulin Corticosteroids Etoposide Naproxen Splenectomy Dr V. Ziaee; Children’s Medical Center
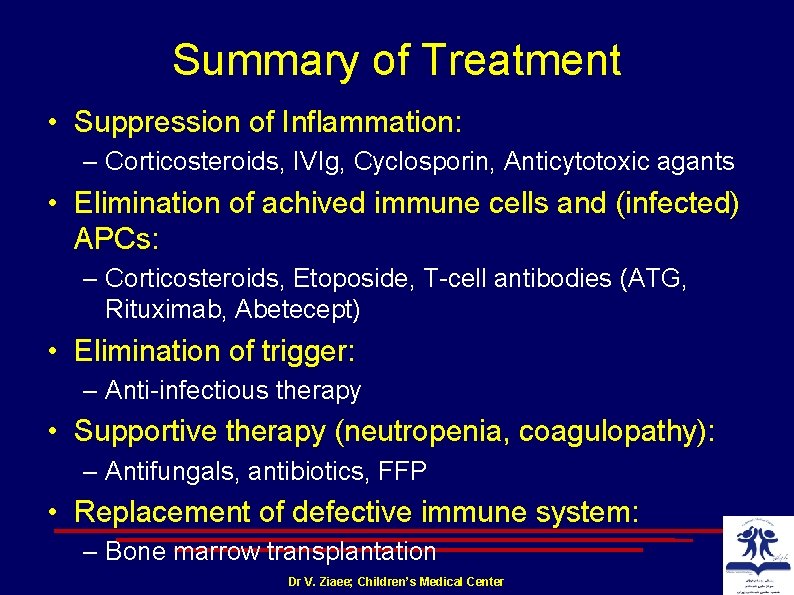
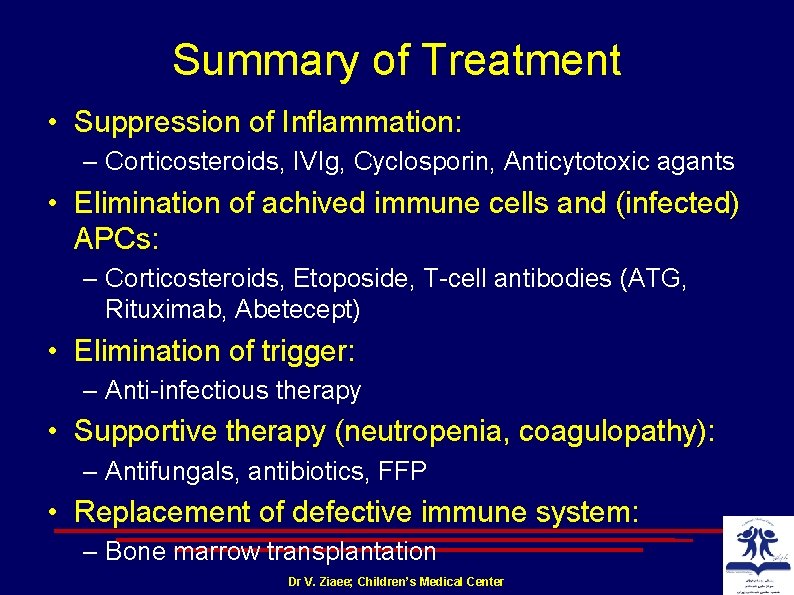
Summary of Treatment • Suppression of Inflammation: – Corticosteroids, IVIg, Cyclosporin, Anticytotoxic agants • Elimination of achived immune cells and (infected) APCs: – Corticosteroids, Etoposide, T cell antibodies (ATG, Rituximab, Abetecept) • Elimination of trigger: – Anti infectious therapy • Supportive therapy (neutropenia, coagulopathy): – Antifungals, antibiotics, FFP • Replacement of defective immune system: – Bone marrow transplantation Dr V. Ziaee; Children’s Medical Center
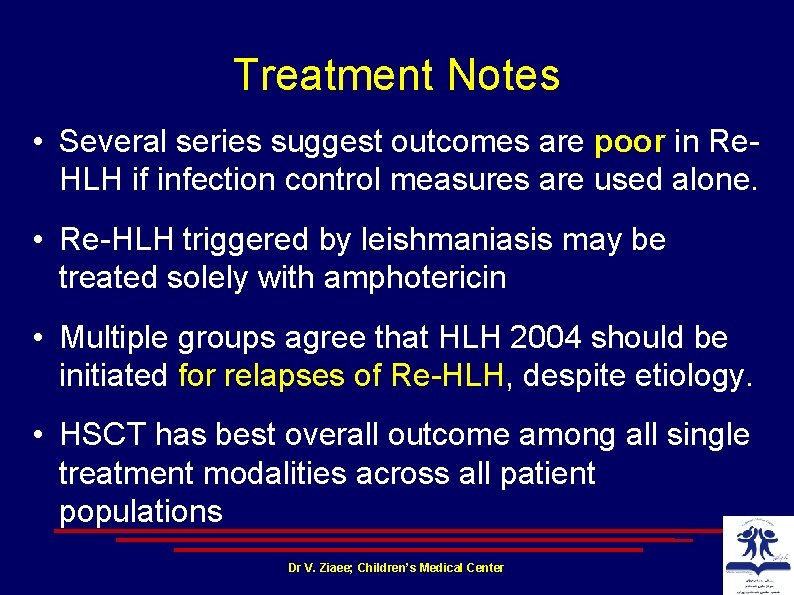
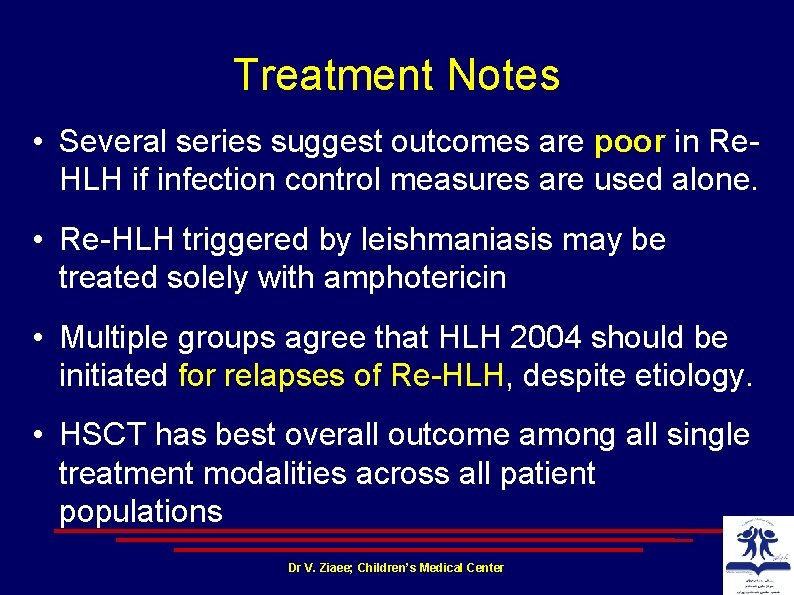
Treatment Notes • Several series suggest outcomes are poor in Re HLH if infection control measures are used alone. • Re HLH triggered by leishmaniasis may be treated solely with amphotericin • Multiple groups agree that HLH 2004 should be initiated for relapses of Re HLH, despite etiology. • HSCT has best overall outcome among all single treatment modalities across all patient populations Dr V. Ziaee; Children’s Medical Center
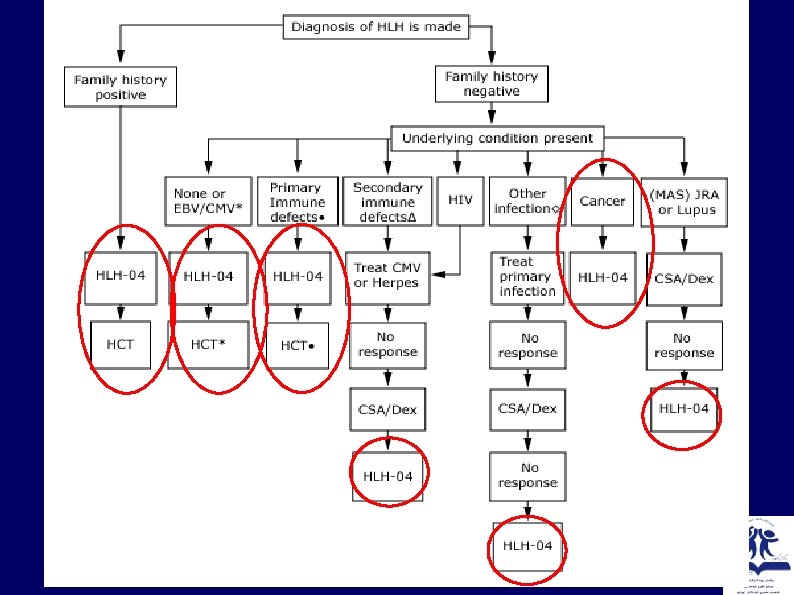
2/29/2009 Dr V. Ziaee; Children’s Medical Center
Dr V. Ziaee; Children’s Medical Center
Prognosis • Without therapy, mortality of patients with HLH is high • Those with an inherited mutation in an HLH gene have a survival of approximately two months without treatment. • Patients treated on the HLH 2004 protocol had a median survival of 54 percent at 6. 2 years (249 patients, median age eight months).

2/29/2009 Dr V. Ziaee; Children’s Medical Center
 Activation tree and activation record
Activation tree and activation record Macrophage
Macrophage Macrophage
Macrophage Fibroblast histology
Fibroblast histology Macrophage migration inhibitory factor
Macrophage migration inhibitory factor Mast cell activation syndrome
Mast cell activation syndrome Amalizumab
Amalizumab Steiner
Steiner Cyrus vahid
Cyrus vahid çində vahid dövlətin yaranması
çində vahid dövlətin yaranması Pichak group
Pichak group Vahid kazemi md
Vahid kazemi md Dr vahid khajoee
Dr vahid khajoee Content addressable memory
Content addressable memory Montillation of traxoline
Montillation of traxoline Vahid e5
Vahid e5 Vahid akhavan
Vahid akhavan Vahid hejazi
Vahid hejazi Letra para que mi amor no sea un sentimiento
Letra para que mi amor no sea un sentimiento Deseo poco y lo poco que deseo lo deseo poco facundo cabral
Deseo poco y lo poco que deseo lo deseo poco facundo cabral El dia mas bello hoy
El dia mas bello hoy Caminaba un dia con mi padre cuando de pronto me pregunto
Caminaba un dia con mi padre cuando de pronto me pregunto Años despues de cristo
Años despues de cristo Mordio lleva tilde
Mordio lleva tilde Ejercicios de diptongos e hiatos resueltos
Ejercicios de diptongos e hiatos resueltos Windows microsoft.com
Windows microsoft.com