Management of Lumbar Stenosis Wayne Yap 16 th
Management of Lumbar Stenosis Wayne Yap 16 th Aug 2015
Prognosis • Natural history of lumbar spinal stenosis due to degenerative spondylosis relatively benign • 32 Patients with symptoms and imaging consistent with lumbar stenosis followed up for mean of 49 months without surgical intervention 1 • 70 % remained unchanged • 15 % worsened • 15 % improved • Over time adjacent spinal segments can become affected in almost half of patients 2, 3 1. 2. 3. Johnsson KE et al. The natural course of lumbar spinal stenosis. Clin Orthop Relat Res. 1992 Lee MJ et al. The natural history of degeneration of lumbar and cervical spines: a systematic review. Spine 2012 Oct; 37 S 18 -30 Xia XP et al. Prevalence of adjacent segment degeneration after spine surgery : a systematic review and meta analysis. Spine 2013 Apr; 38(7): 597 -608
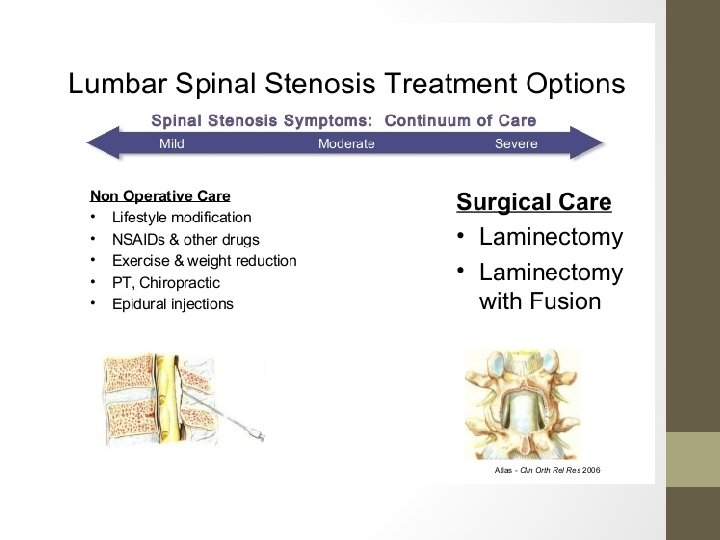
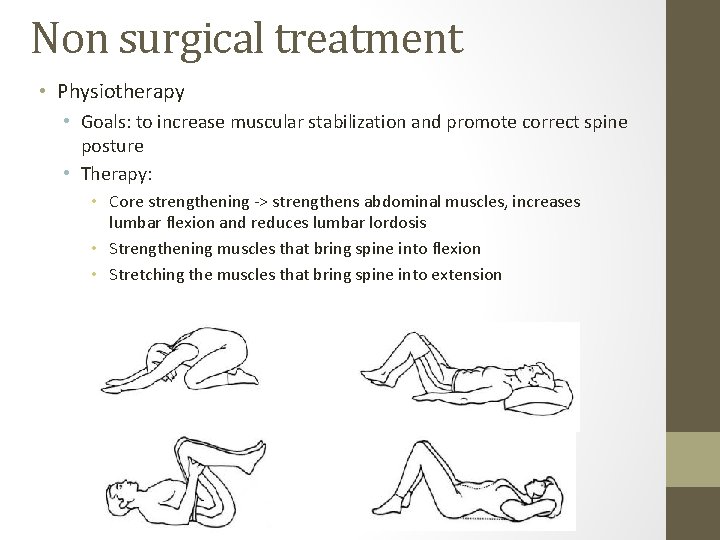
Non surgical treatment • Physiotherapy • Goals: to increase muscular stabilization and promote correct spine posture • Therapy: • Core strengthening -> strengthens abdominal muscles, increases lumbar flexion and reduces lumbar lordosis • Strengthening muscles that bring spine into flexion • Stretching the muscles that bring spine into extension

Non surgical treatment • Physiotherapy • Weight loss • Bicycling and aquatic exercise programs better choices • Bracing • Help reduce lordosis and improve exercise tolerance • Use is cautioned as prolonged use can lead to weakness of abdominal and core muscles, which may worsen prognosis • Patient education and activity limitation
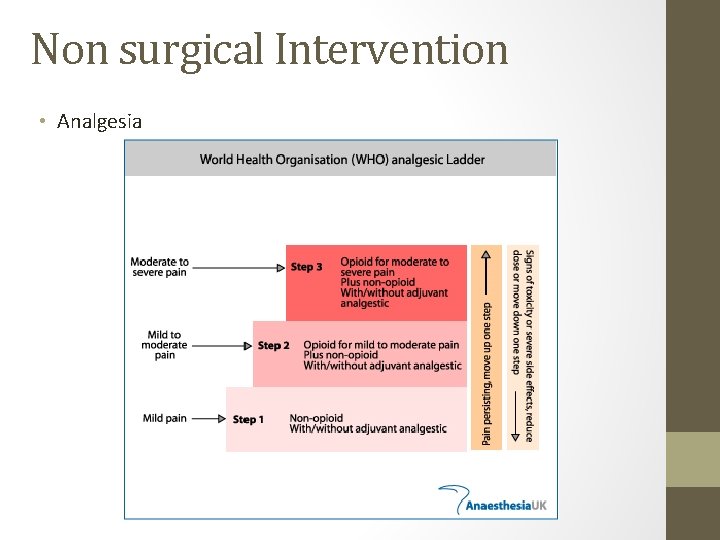
Non surgical Intervention • Analgesia
Non surgical intervention • Gabapentin and Pregabalin • GABA analog (anticonvulsant and analgesic property) • Voltage sensitive calcium and sodium channels accumulate at sites of axonal injury or demyelination • Binds to voltage sensitive calcium and sodium channels found in peripheral as well as central neurons in pathway • Inhibits neurotrasmitter release and thus reduction of abnormal axonal excitability • Has been shown to reduce pain scores, greater walking distance and reduction in sensory deficits 1 • No good evidence on whether gabapentin or pregabalin more efficacious 1. Tran DQ. Lumbar spinal stenosis: A brief review of non surgical management. Can J Anaesth. 2010 Jul; 57(7): 694 -703
Non surgical Intervention • Epidural injections (LA and Steroids) • Theory: • Lumbar spinal stenosis is caused by transient ischemia of nerves • Epidural injections of LA provide sympathetic blockade and vasodilation, increasing blood flow to neural tissue • LA curtails pain induced neuronal sensitization and release of pain neurotransmitters • Steroids thoght to reduce inflammatory edema of damaged nerve root, reduce transmission of nociceptive C fibres and reduce sensitization • Current evidence based off 2 RCTs (Fukusaki et al. 1 and Koc et al. 2) • Shown to improve pain and function in LSS, however benefits are short lived (<1 month) • Available evidence does not support addition of steroids to local anaesthetic agents 1. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain 1998; 14: 148 -51. 2. Koc Z, Ozcakir S, Sivrioglu K, Gurbet A, Kurcukoglu S. Effectiveness of physical therapy and epidural steroid injections in lumbar spinal stenosis. Spine (Phila Pa 1976) 2009; 34: 985 -9
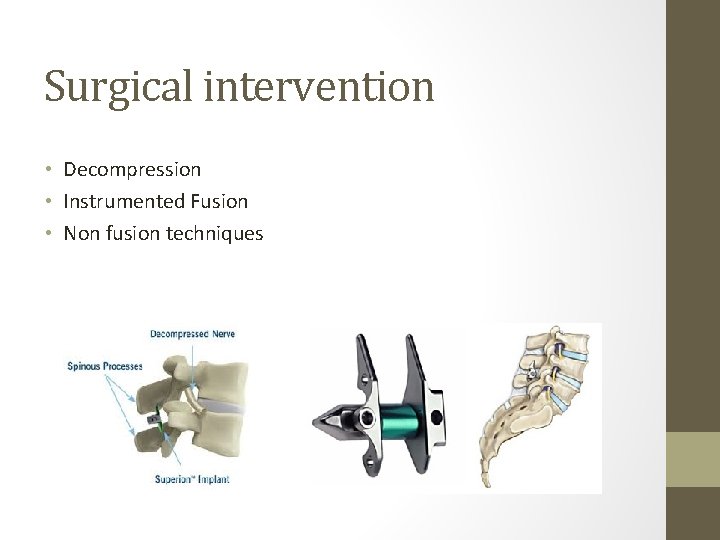
Surgical intervention • Decompression • Instrumented Fusion • Non fusion techniques
Surgical intervention Decompression • Indications for Decompression 3 • Progressive deterioriation of neurological function • Failure of conservative therapy • 3 months generally recommended 1, up to 6 months tolerated • Cauda equina / Conus medullaris • Goals • Improve radicular pain (80%) • Preserve neurological status • Patients who primarily present with a complaint of lower back pain may not show much improvement after decompression though severe stenosis seen in imaging studies 1, 2, 3 1. 2. 3. Lee JY, Whang PG, Lee JY, Phillips FM, Patel AA. Lumbar spinal stenosis. Instr Course Lect. 2013; 62: 383– 396. Mayer HM. Discogenic low back pain and degenerative lumbar spinal stenosis - how appropriate is surgical treatment? Schmerz. 2001; 15: 484– 491 Farzad OK. Lumbar spinal stenosis: Who should be fused? An updated review. Asian Spine J 2014 Aug; 8(4): 521 -530
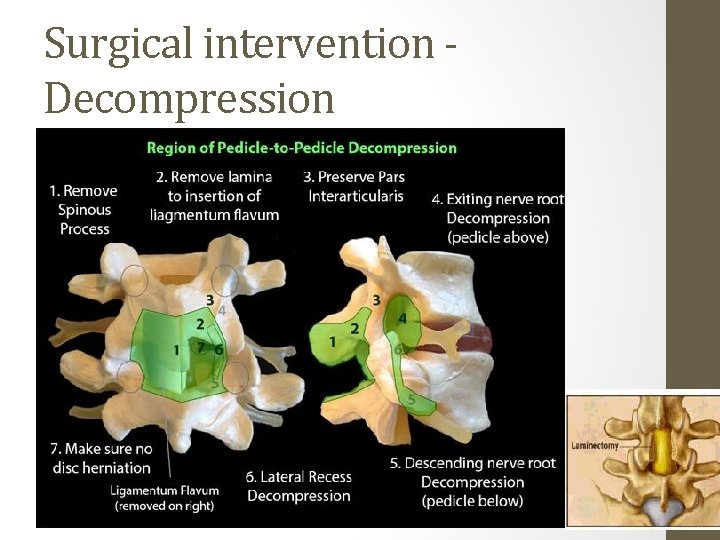
Surgical intervention Decompression • Laminectomy • Different forms exist depending on technique • Open surgical • Complete laminectomy (Wide pedicle to pedicle decompression) • Minimally invasive techniques • Hemilaminectomy • Laminotomy • Concept 1 • Avoid muscle crush injury by self retaining retractors • Do not disrupt tendon attachments sites of key muslces, particularly origin of multifidus muscle at the spinous process • Utilize known anatomic neurovascular and muscle compartment spaces • Minimize collateral soft tissue injury by limiting width of surgical corridor 1. Choll W Kim. The current state of minimally invasive spine surgery. J Bone Joint Surg Am, 2011 Mar 16; 93(6): 582 -596
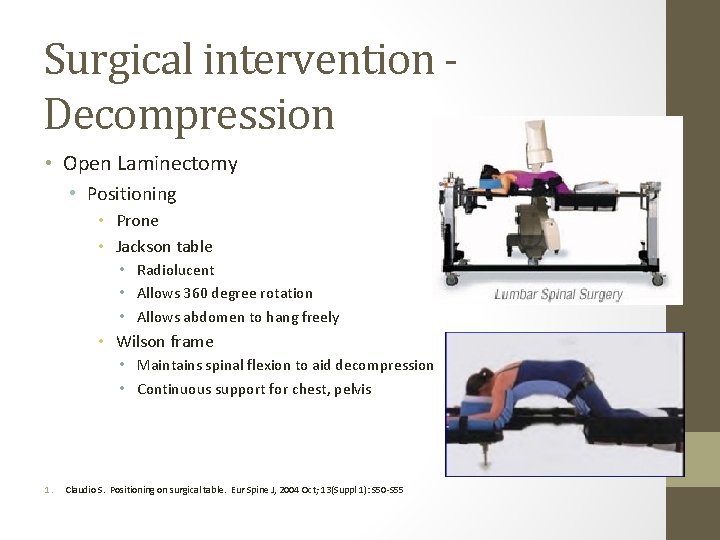
Surgical intervention Decompression • Open Laminectomy • Positioning • Prone • Jackson table • Radiolucent • Allows 360 degree rotation • Allows abdomen to hang freely • Wilson frame • Maintains spinal flexion to aid decompression • Continuous support for chest, pelvis 1. Claudio S. Positioning on surgical table. Eur Spine J, 2004 Oct; 13(Suppl 1): S 50 -S 55
Surgical intervention Decompression • Posterior approach to Lumbar Spine • Landmarks • Highest point iliac crest marks L 4/L 5 interspace • Skin incision • Midline internervous plane between 2 paraspinal muscles • Each erector spinae innervated by segmental nerves coming from posterior primary rami of lumbar nerves • Superficial dissection • Incise fat and lumbodorsal fascia to spinous process (preserve interspinous ligament • Detach erector spinae (spinalis, longissimus, iliocostalis) subperiosteally • Dissect down to spinous process and lamina to facet joint • Dissect multifidus subperiosteally and retract muscle laterally • Move medial to lateral sparing facet capsule 1. Claudio S. Positioning on surgical table. Eur Spine J, 2004 Oct; 13(Suppl 1): S 50 -S 55
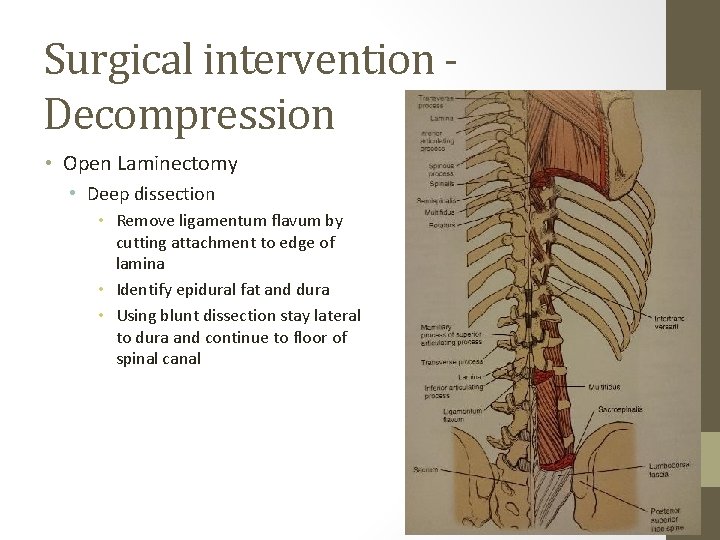
Surgical intervention Decompression • Open Laminectomy • Deep dissection • Remove ligamentum flavum by cutting attachment to edge of lamina • Identify epidural fat and dura • Using blunt dissection stay lateral to dura and continue to floor of spinal canal
Surgical intervention Decompression
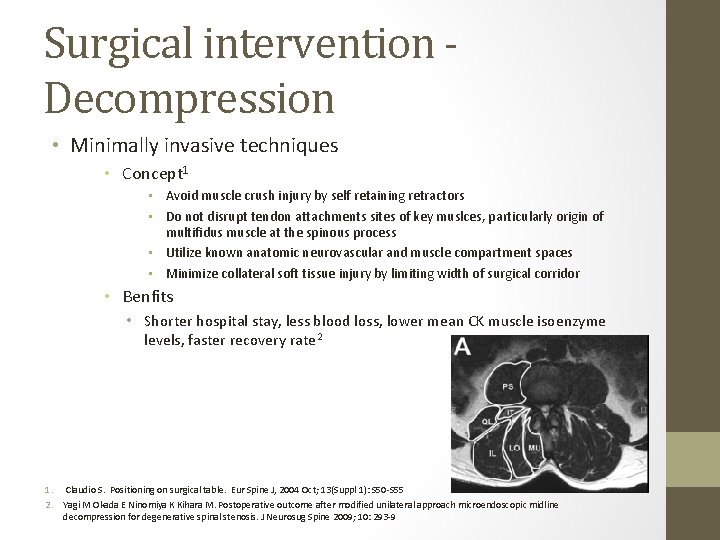
Surgical intervention Decompression • Minimally invasive techniques • Concept 1 • Avoid muscle crush injury by self retaining retractors • Do not disrupt tendon attachments sites of key muslces, particularly origin of multifidus muscle at the spinous process • Utilize known anatomic neurovascular and muscle compartment spaces • Minimize collateral soft tissue injury by limiting width of surgical corridor • Benfits • Shorter hospital stay, less blood loss, lower mean CK muscle isoenzyme levels, faster recovery rate 2 1. Claudio S. Positioning on surgical table. Eur Spine J, 2004 Oct; 13(Suppl 1): S 50 -S 55 2. Yagi M Okada E Ninomiya K Kihara M. Postoperative outcome after modified unilateral approach microendoscopic midline decompression for degenerative spinal stenosis. J Neurosug Spine 2009; 10: 293 -9
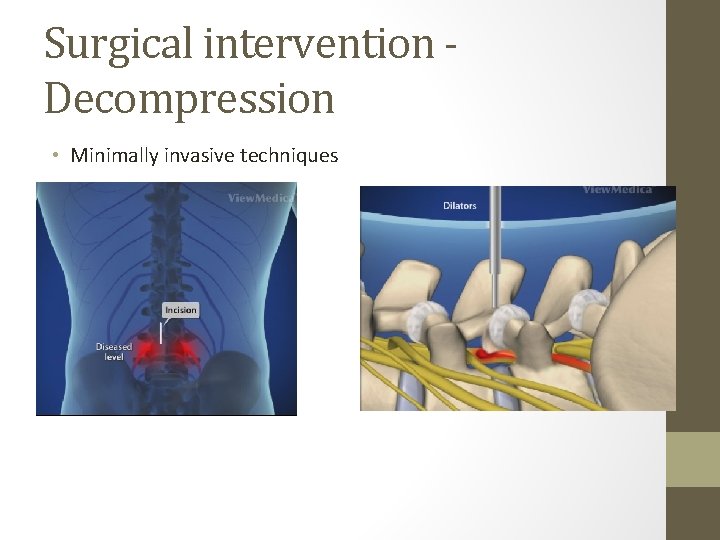
Surgical intervention Decompression • Minimally invasive techniques
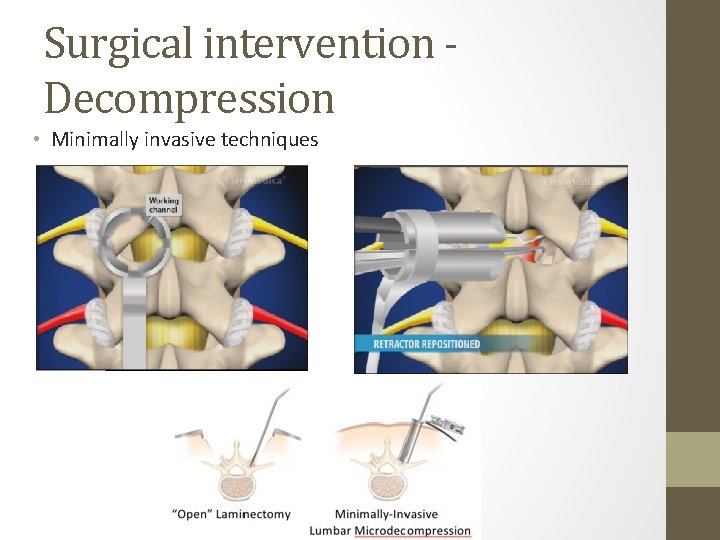
Surgical intervention Decompression • Minimally invasive techniques
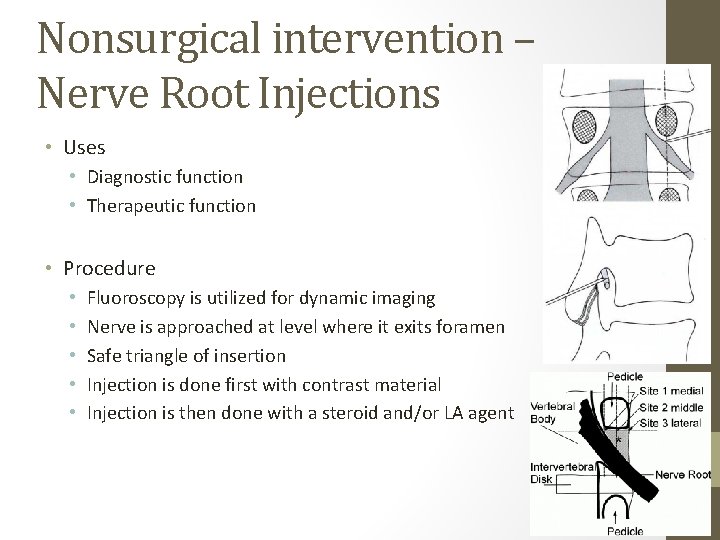
Nonsurgical intervention – Nerve Root Injections • Uses • Diagnostic function • Therapeutic function • Procedure • • • Fluoroscopy is utilized for dynamic imaging Nerve is approached at level where it exits foramen Safe triangle of insertion Injection is done first with contrast material Injection is then done with a steroid and/or LA agent
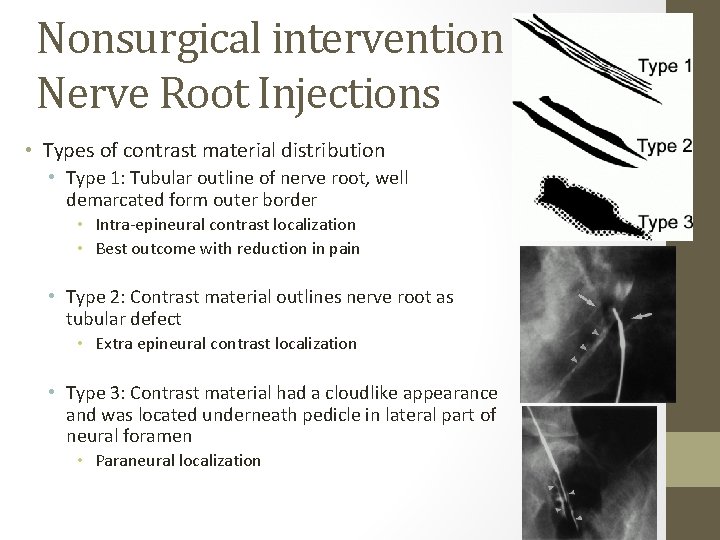
Nonsurgical intervention – Nerve Root Injections • Types of contrast material distribution • Type 1: Tubular outline of nerve root, well demarcated form outer border • Intra-epineural contrast localization • Best outcome with reduction in pain • Type 2: Contrast material outlines nerve root as tubular defect • Extra epineural contrast localization • Type 3: Contrast material had a cloudlike appearance and was located underneath pedicle in lateral part of neural foramen • Paraneural localization
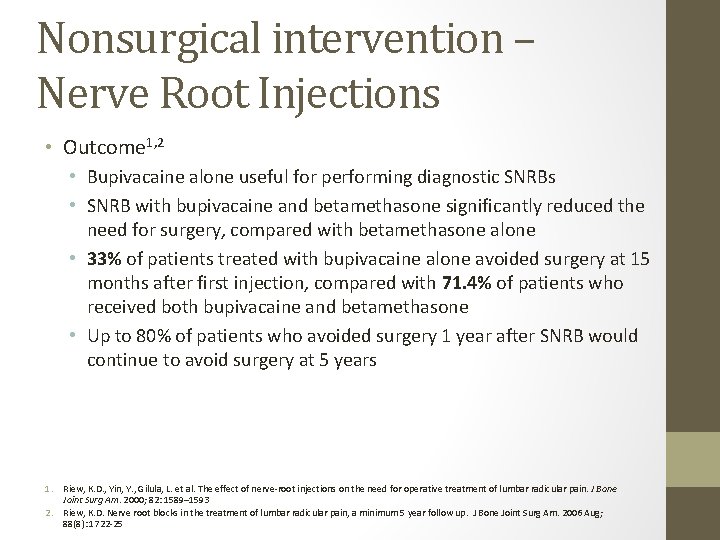
Nonsurgical intervention – Nerve Root Injections • Outcome 1, 2 • Bupivacaine alone useful for performing diagnostic SNRBs • SNRB with bupivacaine and betamethasone significantly reduced the need for surgery, compared with betamethasone alone • 33% of patients treated with bupivacaine alone avoided surgery at 15 months after first injection, compared with 71. 4% of patients who received both bupivacaine and betamethasone • Up to 80% of patients who avoided surgery 1 year after SNRB would continue to avoid surgery at 5 years 1. Riew, K. D. , Yin, Y. , Gilula, L. et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. J Bone Joint Surg Am. 2000; 82: 1589– 1593 2. Riew, K. D. Nerve root blocks in the treatment of lumbar radicular pain, a minimum 5 year follow up. J Bone Joint Surg Am. 2006 Aug; 88(8): 1722 -25
Surgical intervention - Fusion • Goals • Improve regional back pain • Indications for Fusion 1 • Pre operative indicators • Failed back surgery syndrome • Degenerative instability • Wide disc space 1. Farzad OK. Lumbar spinal stenosis: Who should be fused? An updated review. Asian Spine J 2014 Aug; 8(4): 521 -530
Surgical intervention - Fusion • Indications for Fusion 1 • Pre operative indicators • Degenerative instability • For patients with degenerative spondylolisthesis with spinal surgery • Low grade spondylolisthesis and decompression does not cause injury to facet joints, it will NOT increase probability of greater slippage 2 • Radicular complaints predominant WITHOUT back pain and spondylotic vertebra re-stabilized in slipped position, decompression alone is sufficient • Fusion generally recommended in 3, 4 • Wide disc space >2 mm • > 5 mm displacement or >10 -15 deg rotation on lateral standing flexion-extension lumbosacral radiographs • Slip greater than 25% (Grade 2 onwards) 1. 2. 3. 4. Farzad OK. Lumbar spinal stenosis: Who should be fused? An updated review. Asian Spine J 2014 Aug; 8(4): 521 -530 Epstein NE. Decompression in the surgical management of degenerative spondylolisthesis: advantages of a conservative approach in 290 patients. J Spinal Disord. 1998; 11: 116– 122. Chen YM, Jin AM, Zhang H, Zhu LX, Min SX, Zhang L. Indication of fusion for degenerative lumbar spinal stenosis treated by "windows technique" laminoforaminotomy. Zhonghua Wai Ke Za Zhi. 2010; 48: 31– 34. Carreon LY, Glassman SD, Howard J. Fusion and nonsurgical treatment for symptomatic lumbar degenerative disease: a systematic review of Oswestry Disability Index and MOS Short Form-36 outcomes. Spine J. 2008; 8: 747– 755.
Surgical intervention - Fusion • Goals • Improve regional back pain • Indications for Fusion 1 • Pre operative indicators • • Failed back surgery syndrome Degenerative instability Wide disc space Correction of deformity Symptomatic spondylolysis Refractory degenerative disc disease Adjacent segment disease • Operative indicators • Extensive decompression • Available bone stock 1. Farzad OK. Lumbar spinal stenosis: Who should be fused? An updated review. Asian Spine J 2014 Aug; 8(4): 521 -530

Surgical intervention - Fusion • Operative indicators • Extensive decompression • Bilateral facetectomy > 1/3 or ½ • Excision of > 50% of pars interarticularis • Bilateral discectomy in addition to partial facetectomy • Available bone stock • For successful fusion, adequate bone graft on host bed is needed • Small transverse process • High grade spondylolistehsis • Severe osteoporosis contraindication to instrumentation due to probability of implant dislodgement • Can consider pedicle screws with cement 1. Farzad OK. Lumbar spinal stenosis: Who should be fused? An updated review. Asian Spine J 2014 Aug; 8(4): 521 -530
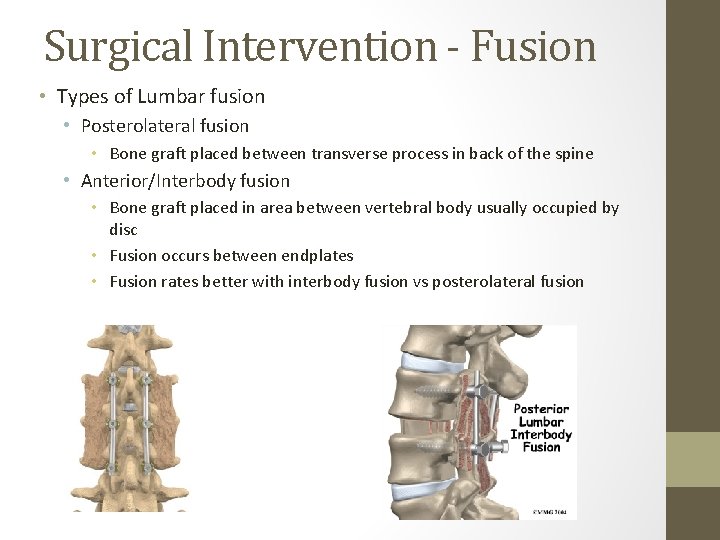
Surgical Intervention - Fusion • Types of Lumbar fusion • Posterolateral fusion • Bone graft placed between transverse process in back of the spine • Anterior/Interbody fusion • Bone graft placed in area between vertebral body usually occupied by disc • Fusion occurs between endplates • Fusion rates better with interbody fusion vs posterolateral fusion
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • • Transforaminal lumbar interbody fusion (TLIF) Posterior lumbar interbody fusion (PLIF) Anterior lumbar interbody fusion (ALIF) Transpsoas interbody fusion • Xtreme lateral interbody fusion (XLIF) • Direct lateral interbody fusion (DLIF) • Oblique lumbar lateral interbody fusion (OLLIF)
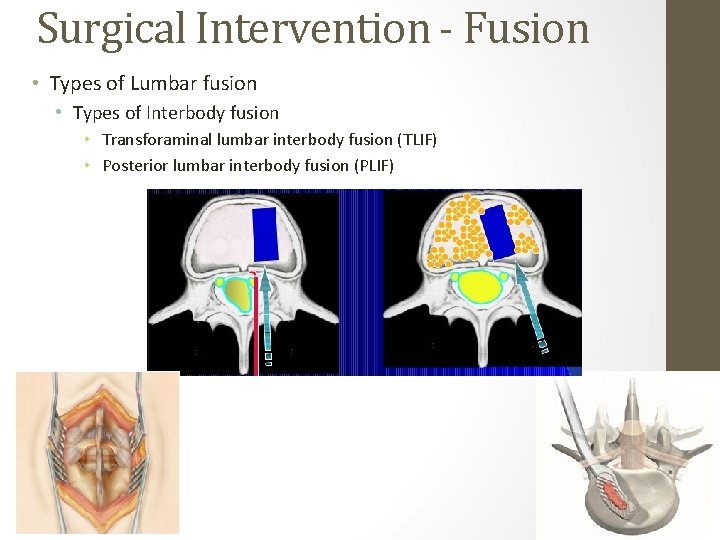
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • Transforaminal lumbar interbody fusion (TLIF) • Posterior lumbar interbody fusion (PLIF)
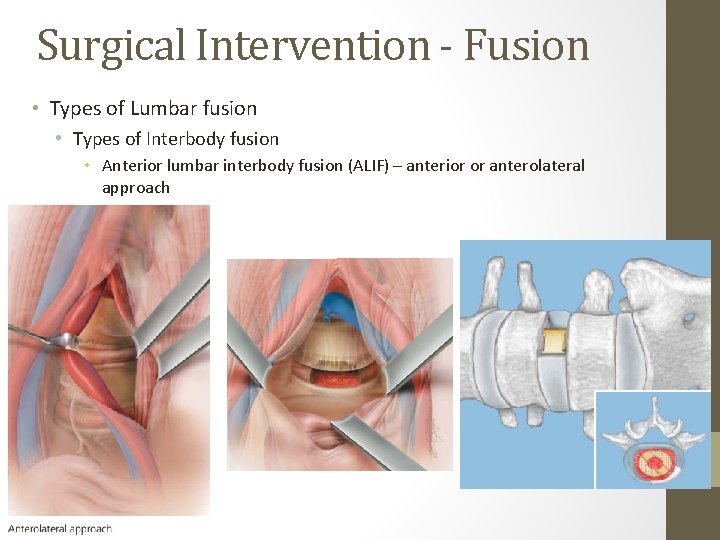
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • Anterior lumbar interbody fusion (ALIF) – anterior or anterolateral approach
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • Anterior lumbar interbody fusion (ALIF) – anterior or anterolateral approach • Risks • Retrograde ejaculation due to damage to superior hypogastric plexus • Vascular injury
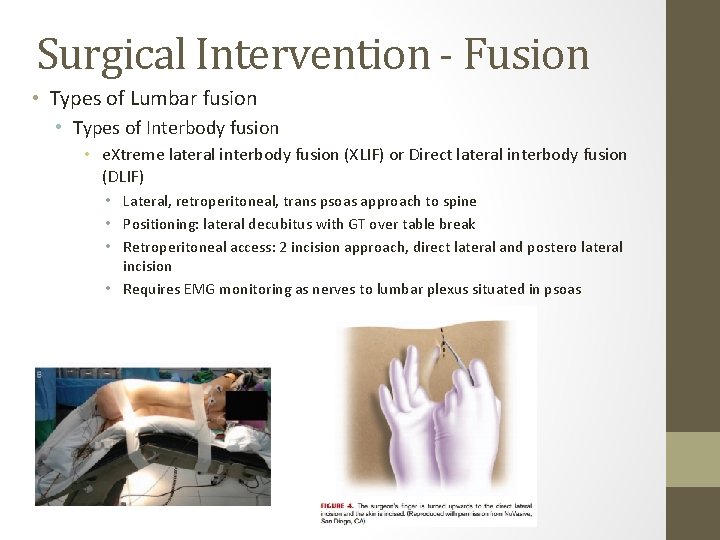
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • e. Xtreme lateral interbody fusion (XLIF) or Direct lateral interbody fusion (DLIF) • Lateral, retroperitoneal, trans psoas approach to spine • Positioning: lateral decubitus with GT over table break • Retroperitoneal access: 2 incision approach, direct lateral and postero lateral incision • Requires EMG monitoring as nerves to lumbar plexus situated in psoas
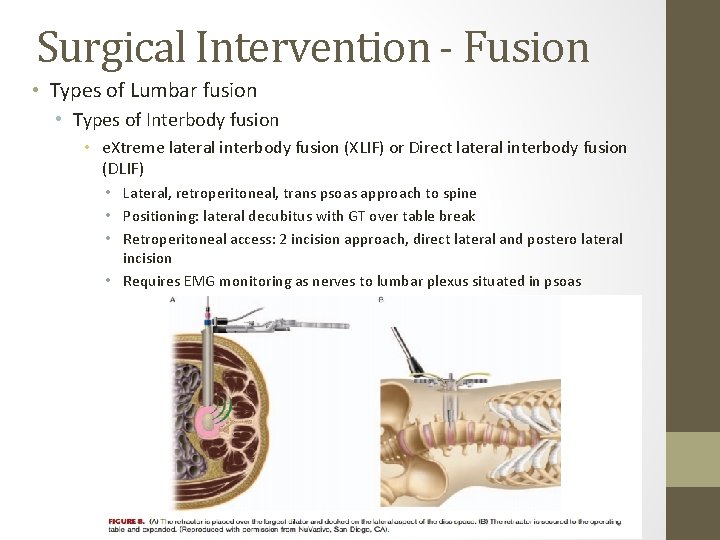
Surgical Intervention - Fusion • Types of Lumbar fusion • Types of Interbody fusion • e. Xtreme lateral interbody fusion (XLIF) or Direct lateral interbody fusion (DLIF) • Lateral, retroperitoneal, trans psoas approach to spine • Positioning: lateral decubitus with GT over table break • Retroperitoneal access: 2 incision approach, direct lateral and postero lateral incision • Requires EMG monitoring as nerves to lumbar plexus situated in psoas
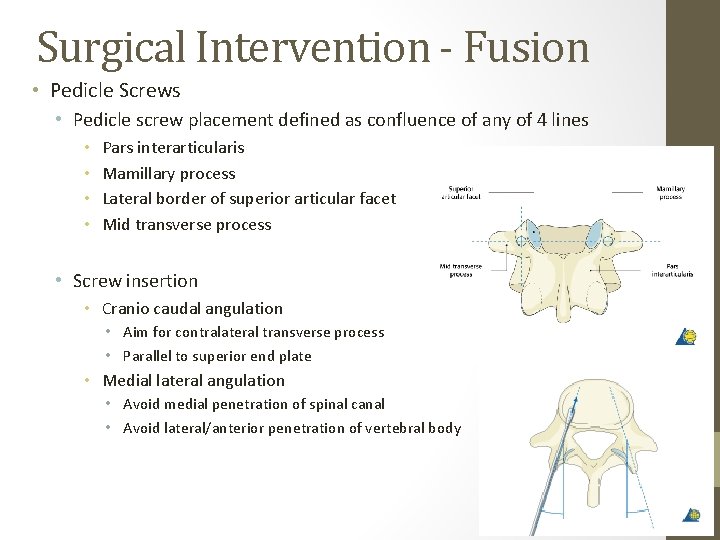
Surgical Intervention - Fusion • Pedicle Screws • Pedicle screw placement defined as confluence of any of 4 lines • • Pars interarticularis Mamillary process Lateral border of superior articular facet Mid transverse process • Screw insertion • Cranio caudal angulation • Aim for contralateral transverse process • Parallel to superior end plate • Medial lateral angulation • Avoid medial penetration of spinal canal • Avoid lateral/anterior penetration of vertebral body
Thank You
- Slides: 34