Management of Fetal Anomalies Beyond the Age of
Management of Fetal Anomalies Beyond the Age of Viability Dr. Sawsan Al-Obaidly Consultant, Maternal-Fetal Medicine Obstetrics and Gynecology Department, Women’s Hospital, HMC
Disclosures • None
Objectives • • • Spectrum of fetal anomalies Obstetric impact of fetal anomalies Hydrocephalus The concept of Fetus as a patient Women counselling of severe fetal anomalies Guidelines for management
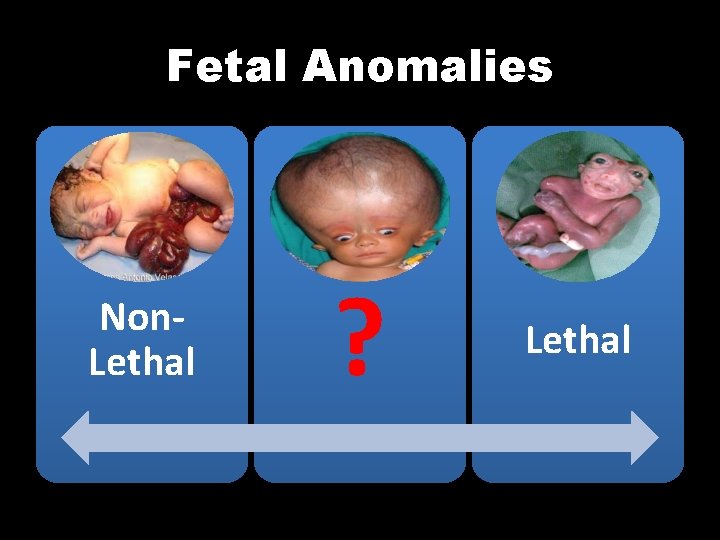
Fetal Anomalies Non. Lethal ? Lethal
Lethal Anomalies The word ‘lethal’ is derived from the Latin ‘letalis’ (deadly), and related to a Greek word meaning ‘oblivion, ’ referring to the myth that the souls of the dead forgot their lives on Earth after drinking the waters of the River Lethe. Conventionally, ‘lethal’ is used to describe something (e. g. an action or agent) that will cause death Oxford English Dictionary online. Oxford University Press; 1989. http: //www. oed. com/.
• lethal condition invariably leads to death, i. e. , there is no effective treatment that will prevent a condition, disease, or injury from causing death in the near future’ Chervenak F, Mc. Cullough LB. Responsibly counselling women about the clinical management of pregnancies complicated by severe fetal anomalies. J Med Ethics 2012; 38: 397 e 8.
Malformations most frequently described as ‘lethal’ conditions • • • Potter's syndrome/renal agenesis Anencephaly/acrania Thanatophoric dwarfism Trisomy 13 or 18 Holoprosencephaly Wilkinson DJC, Thiele P, Watkins A, De Crespigny L. Fatally flawed? A review and ethical analysis of lethal congenital malformations. Br J Obstet Gynaecol 2012; 119: 1302 e 7.
Severe Fetal Anomalies Beyond The Age of Viability
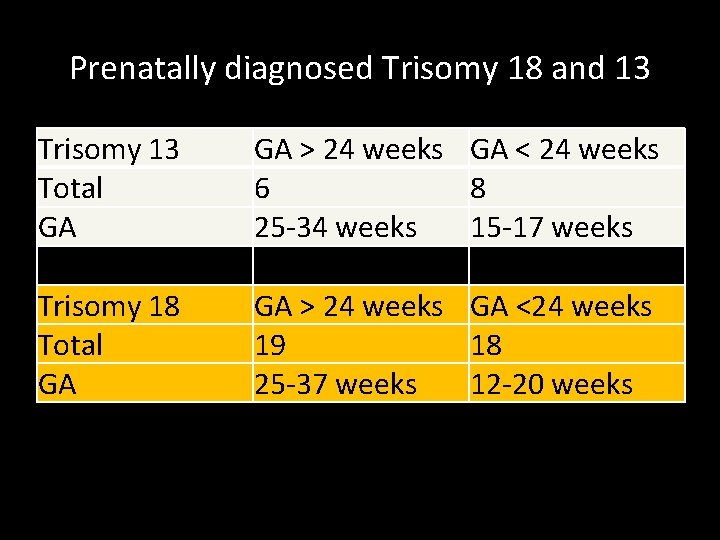
Prenatally diagnosed Trisomy 18 and 13 Trisomy 13 Total GA GA > 24 weeks GA < 24 weeks 6 8 25 -34 weeks 15 -17 weeks Trisomy 18 Total GA GA > 24 weeks GA <24 weeks 19 18 25 -37 weeks 12 -20 weeks
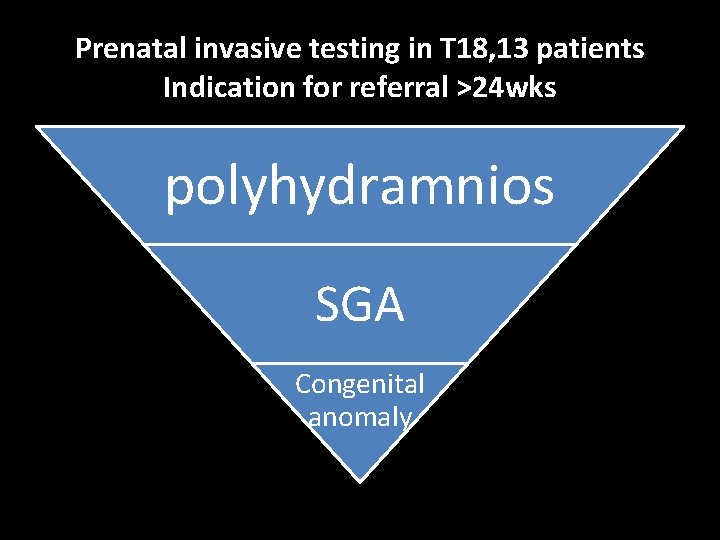
Prenatal invasive testing in T 18, 13 patients Indication for referral >24 wks polyhydramnios SGA Congenital anomaly
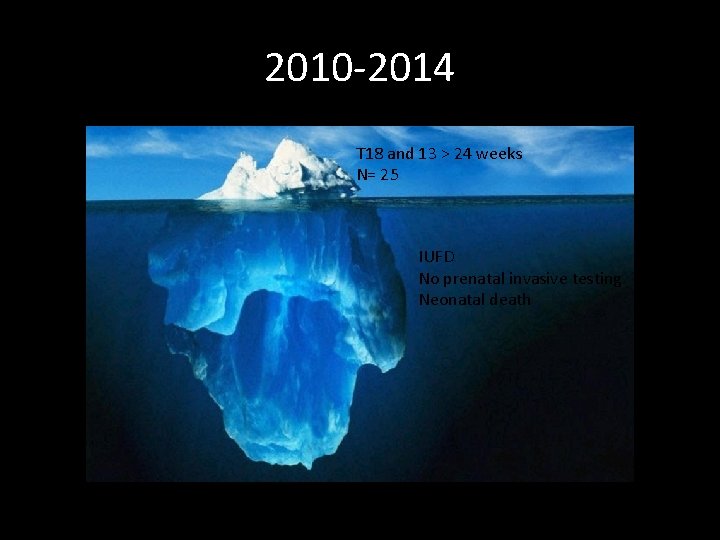
2010 -2014 T 18 and 13 > 24 weeks N= 25 IUFD No prenatal invasive testing Neonatal death
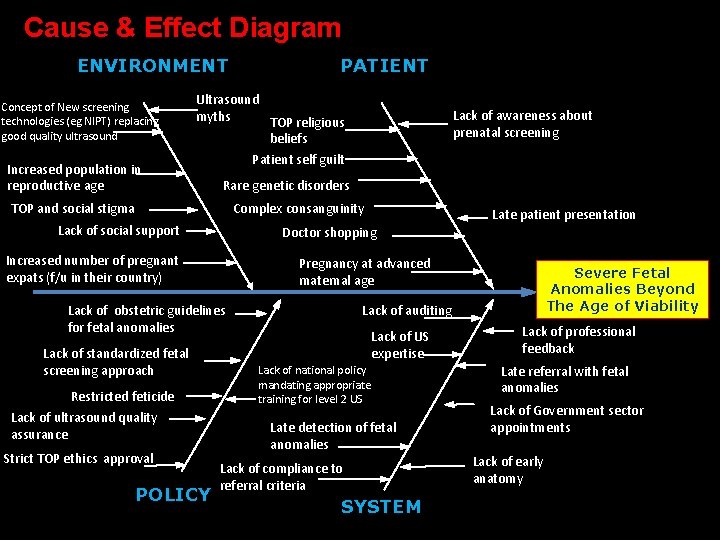
Cause & Effect Diagram ENVIRONMENT Concept of New screening technologies (eg NIPT) replacing good quality ultrasound Increased population in reproductive age PATIENT Ultrasound myths TOP religious beliefs Patient self guilt Lack of awareness about prenatal screening Rare genetic disorders TOP and social stigma Complex consanguinity Lack of social support Doctor shopping Increased number of pregnant expats (f/u in their country) Pregnancy at advanced maternal age Lack of obstetric guidelines for fetal anomalies Lack of standardized fetal screening approach Restricted feticide Lack of ultrasound quality assurance Strict TOP ethics approval POLICY Late patient presentation Severe Fetal Anomalies Beyond The Age of Viability Lack of auditing Lack of US expertise Lack of national policy mandating appropriate training for level 2 US Late detection of fetal anomalies Lack of compliance to referral criteria SYSTEM Lack of professional feedback Late referral with fetal anomalies Lack of Government sector appointments Lack of early anatomy
Potential Obstetric Impact of Fetal Anomalies Beyond Viability
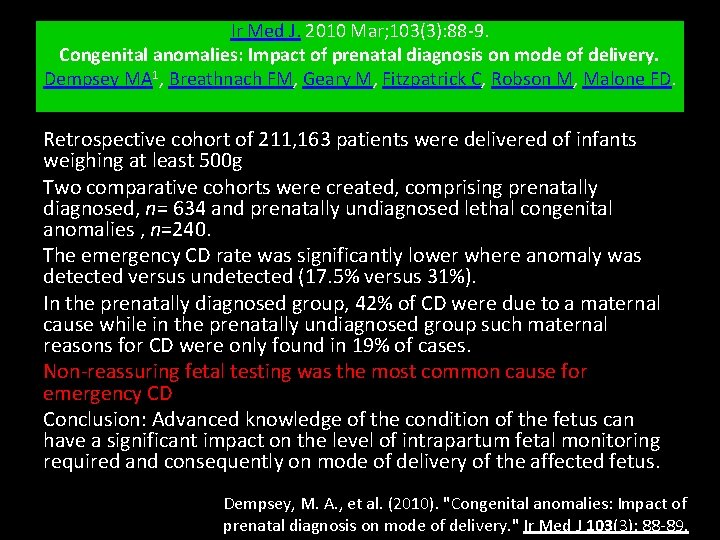
Ir Med J. 2010 Mar; 103(3): 88 -9. Congenital anomalies: Impact of prenatal diagnosis on mode of delivery. Dempsey MA 1, Breathnach FM, Geary M, Fitzpatrick C, Robson M, Malone FD. Retrospective cohort of 211, 163 patients were delivered of infants weighing at least 500 g Two comparative cohorts were created, comprising prenatally diagnosed, n= 634 and prenatally undiagnosed lethal congenital anomalies , n=240. The emergency CD rate was significantly lower where anomaly was detected versus undetected (17. 5% versus 31%). In the prenatally diagnosed group, 42% of CD were due to a maternal cause while in the prenatally undiagnosed group such maternal reasons for CD were only found in 19% of cases. Non-reassuring fetal testing was the most common cause for emergency CD Conclusion: Advanced knowledge of the condition of the fetus can have a significant impact on the level of intrapartum fetal monitoring required and consequently on mode of delivery of the affected fetus. Dempsey, M. A. , et al. (2010). "Congenital anomalies: Impact of prenatal diagnosis on mode of delivery. " Ir Med J 103(3): 88 -89.
• Largest series of anencephaly beyond viability • n=37 cases • Primi= 24% (9/37). GA at diagnosis 21 wks (21 -41). IOL 54% (20/37). GA at birth 34 wks (25 -44). • Vaginal birth 70% (26/37). Primary C-section 8% (3/37). Repeat C-section 22% (8/37). • No differences in achieving vaginal birth in the spontaneous compared to the induced group. One case of shoulder dystocia. No cases of APH, PPH or uterine rupture. • Conclusion: Apart from tendency for post-term pregnancies, the prenatal diagnosis of anencephaly poses no significant increased maternal risk. http: //onlinelibrary. wiley. com/doi/10. 1111/1471 -0528. 14099/epdf
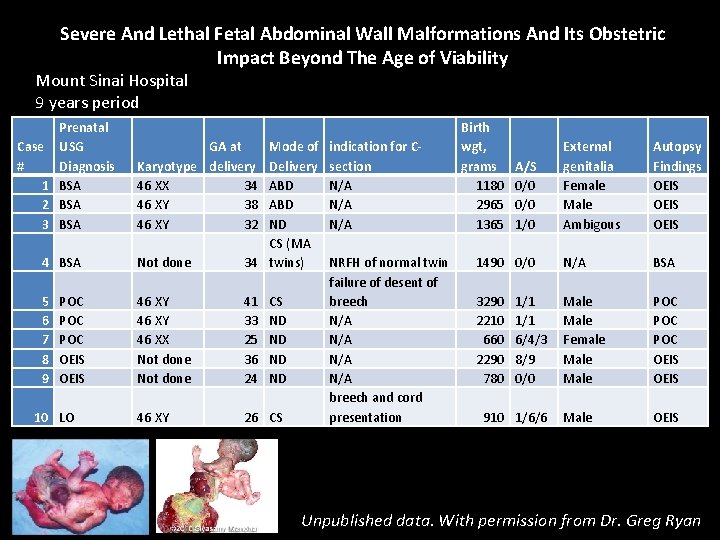
Severe And Lethal Fetal Abdominal Wall Malformations And Its Obstetric Impact Beyond The Age of Viability Mount Sinai Hospital 9 years period Prenatal Case USG # Diagnosis 1 BSA 2 BSA 3 BSA GA at Karyotype delivery 46 XX 34 46 XY 38 46 XY 32 indication for Csection N/A N/A 4 BSA Not done Mode of Delivery ABD ND CS (MA 34 twins) 5 6 7 8 9 46 XY 46 XX Not done 41 33 25 36 24 46 XY 26 CS NRFH of normal twin failure of desent of breech N/A N/A breech and cord presentation POC POC OEIS 10 LO CS ND ND Birth wgt, grams 1180 2965 1365 External genitalia Female Male Ambigous Autopsy Findings OEIS 1490 0/0 N/A BSA 3290 2210 660 2290 780 Male Female Male POC POC OEIS Male OEIS A/S 0/0 1/0 1/1 6/4/3 8/9 0/0 910 1/6/6 Unpublished data. With permission from Dr. Greg Ryan
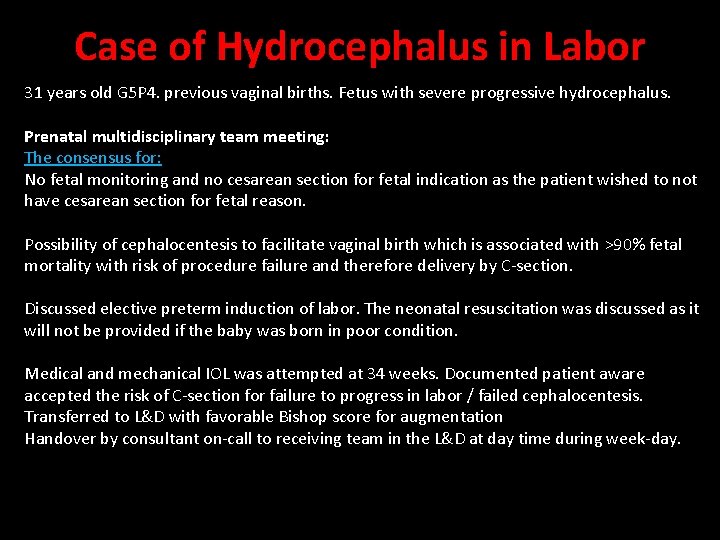
Case of Hydrocephalus in Labor 31 years old G 5 P 4. previous vaginal births. Fetus with severe progressive hydrocephalus. Prenatal multidisciplinary team meeting: The consensus for: No fetal monitoring and no cesarean section for fetal indication as the patient wished to not have cesarean section for fetal reason. Possibility of cephalocentesis to facilitate vaginal birth which is associated with >90% fetal mortality with risk of procedure failure and therefore delivery by C-section. Discussed elective preterm induction of labor. The neonatal resuscitation was discussed as it will not be provided if the baby was born in poor condition. Medical and mechanical IOL was attempted at 34 weeks. Documented patient aware accepted the risk of C-section for failure to progress in labor / failed cephalocentesis. Transferred to L&D with favorable Bishop score for augmentation Handover by consultant on-call to receiving team in the L&D at day time during week-day.
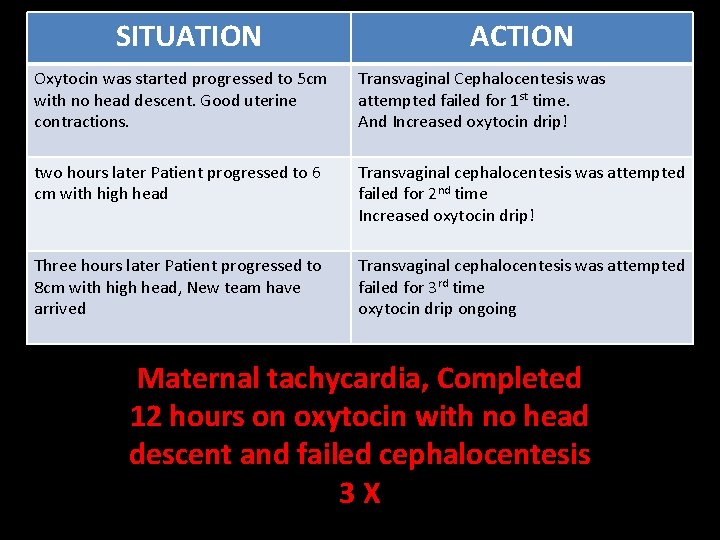
SITUATION ACTION Oxytocin was started progressed to 5 cm with no head descent. Good uterine contractions. Transvaginal Cephalocentesis was attempted failed for 1 st time. And Increased oxytocin drip! two hours later Patient progressed to 6 cm with high head Transvaginal cephalocentesis was attempted failed for 2 nd time Increased oxytocin drip! Three hours later Patient progressed to 8 cm with high head, New team have arrived Transvaginal cephalocentesis was attempted failed for 3 rd time oxytocin drip ongoing Maternal tachycardia, Completed 12 hours on oxytocin with no head descent and failed cephalocentesis 3 X
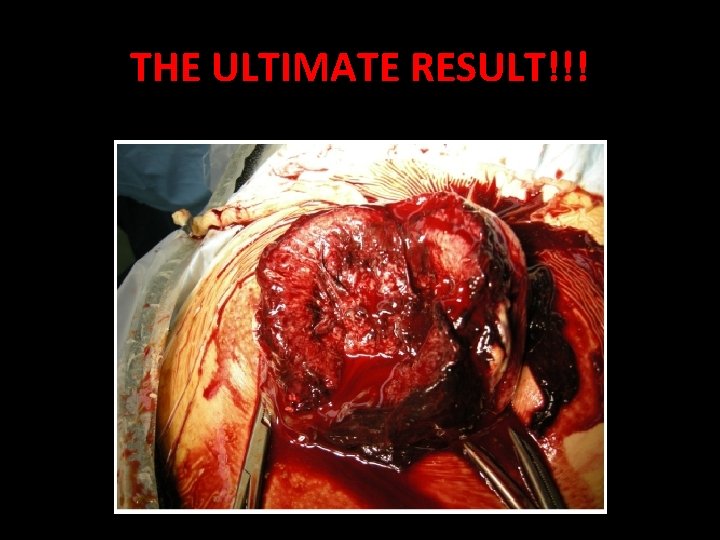
THE ULTIMATE RESULT!!!
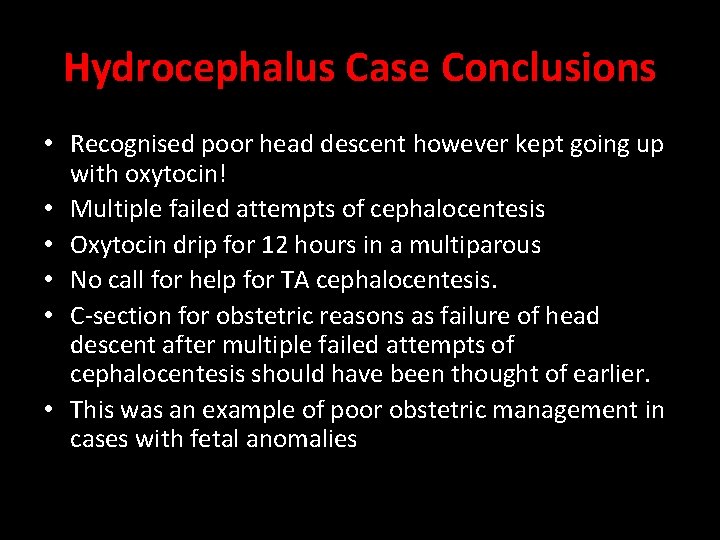
Hydrocephalus Case Conclusions • Recognised poor head descent however kept going up with oxytocin! • Multiple failed attempts of cephalocentesis • Oxytocin drip for 12 hours in a multiparous • No call for help for TA cephalocentesis. • C-section for obstetric reasons as failure of head descent after multiple failed attempts of cephalocentesis should have been thought of earlier. • This was an example of poor obstetric management in cases with fetal anomalies
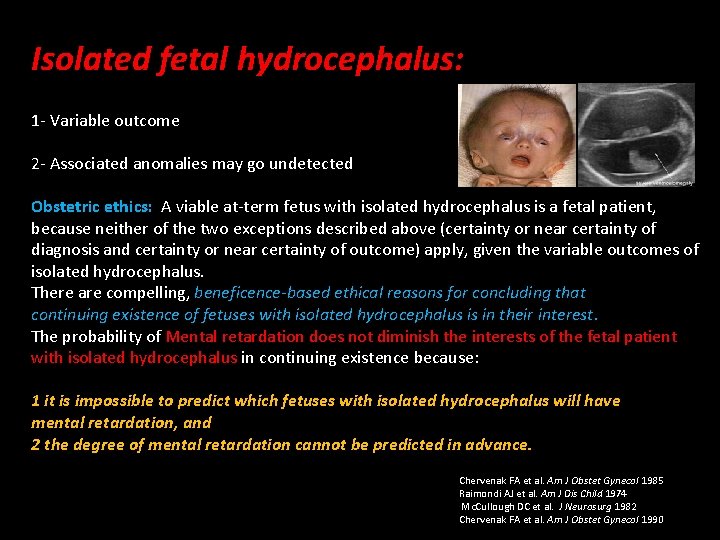
Isolated fetal hydrocephalus: 1 - Variable outcome 2 - Associated anomalies may go undetected Obstetric ethics: A viable at-term fetus with isolated hydrocephalus is a fetal patient, because neither of the two exceptions described above (certainty or near certainty of diagnosis and certainty or near certainty of outcome) apply, given the variable outcomes of isolated hydrocephalus. There are compelling, beneficence-based ethical reasons for concluding that continuing existence of fetuses with isolated hydrocephalus is in their interest. The probability of Mental retardation does not diminish the interests of the fetal patient with isolated hydrocephalus in continuing existence because: 1 it is impossible to predict which fetuses with isolated hydrocephalus will have mental retardation, and 2 the degree of mental retardation cannot be predicted in advance. Chervenak FA et al. Am J Obstet Gynecol 1985 Raimondi AJ et al. Am J Dis Child 1974 Mc. Cullough DC et al. J Neurosurg 1982 Chervenak FA et al. Am J Obstet Gynecol 1990
The decision to offer cephalocentesis in such cases (alobar holoprosencephaly) is based on our beneficence-based obligation to the pregnant woman to allow her to avoid cesarean delivery, which would be of little benefit to the fetus. In view of the short- and long-term consequences of cesarean delivery, the physician can therefore justifiably undertake interventions for maternal benefit that risk fetal death. Because of these reasons, fetal heart rate monitoring is not indicated after cephalocentesis, as cesarean delivery for an abnormal fetal heart tracing would not be appropriate. A classical incision would preclude future trial of labor due to the risk of uterine rupture. Chasen, S. T. , et al. (2001). "The role of cephalocentesis in modern obstetrics. " Am J Obstet Gynecol 185(3): 734 -736.
In summary, Cephalocentesis to allow vaginal delivery is indicated in fetal hydrocephalus with associated anomalies that are either incompatible with life or associated with the severest forms of neurologic dysfunction. In these situations, the benefit of avoiding cesarean delivery clearly outweighs the risk of fetal death or injury associated with cephalocentesis.
Ethics and Non-treatment of Severe Hydrocephalus Ethics and Treatment of Severe Hydrocephalus? WILKINSON D. Ethical Dilemmas in Postnatal Treatment of Severe Congenital Hydrocephalus. Cambridge Quarterly of Healthcare Ethics. 2016; 25(1): 84 -92.
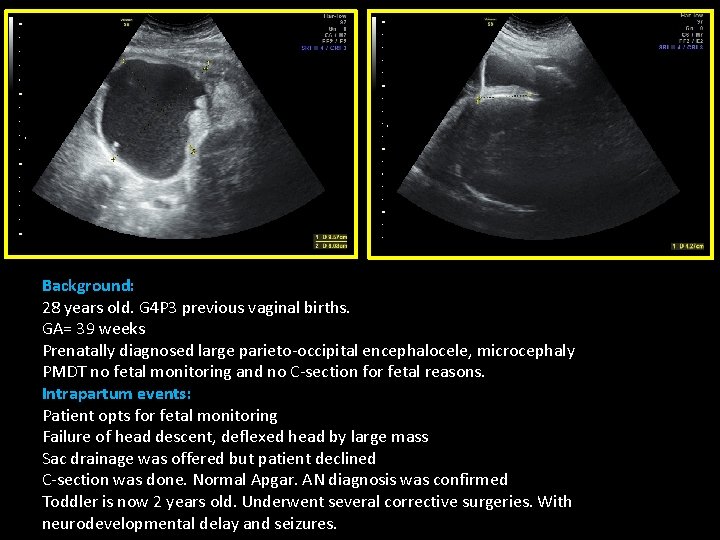
Background: 28 years old. G 4 P 3 previous vaginal births. GA= 39 weeks Prenatally diagnosed large parieto-occipital encephalocele, microcephaly PMDT no fetal monitoring and no C-section for fetal reasons. Intrapartum events: Patient opts for fetal monitoring Failure of head descent, deflexed head by large mass Sac drainage was offered but patient declined C-section was done. Normal Apgar. AN diagnosis was confirmed Toddler is now 2 years old. Underwent several corrective surgeries. With neurodevelopmental delay and seizures.
Maternal-Fetal Conflict
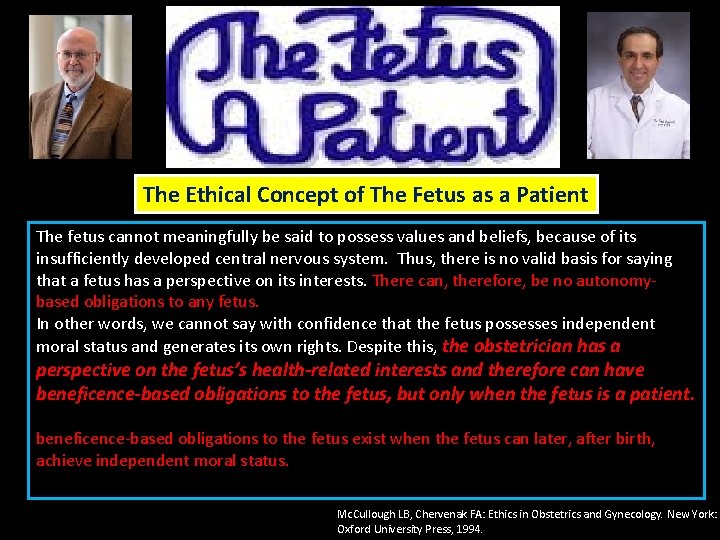
The Ethical Concept of The Fetus as a Patient The fetus cannot meaningfully be said to possess values and beliefs, because of its insufficiently developed central nervous system. Thus, there is no valid basis for saying that a fetus has a perspective on its interests. There can, therefore, be no autonomybased obligations to any fetus. In other words, we cannot say with confidence that the fetus possesses independent moral status and generates its own rights. Despite this, the obstetrician has a perspective on the fetus’s health-related interests and therefore can have beneficence-based obligations to the fetus, but only when the fetus is a patient. beneficence-based obligations to the fetus exist when the fetus can later, after birth, achieve independent moral status. Mc. Cullough LB, Chervenak FA: Ethics in Obstetrics and Gynecology. New York: Oxford University Press, 1994.
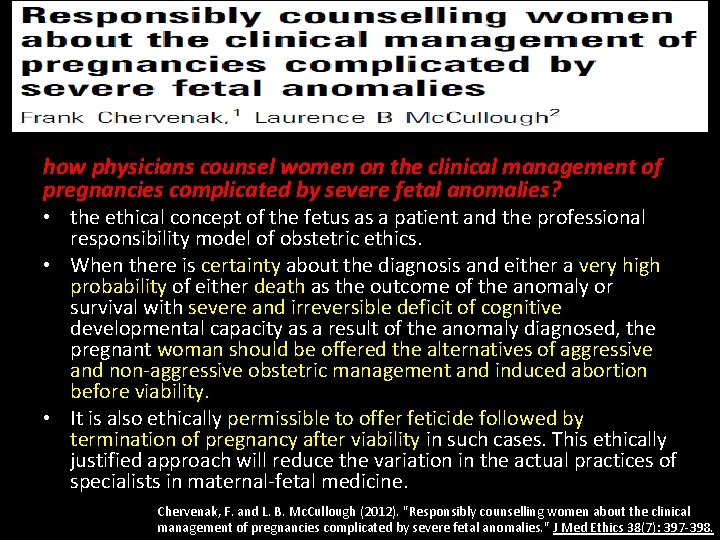
how physicians counsel women on the clinical management of pregnancies complicated by severe fetal anomalies? • the ethical concept of the fetus as a patient and the professional responsibility model of obstetric ethics. • When there is certainty about the diagnosis and either a very high probability of either death as the outcome of the anomaly or survival with severe and irreversible deficit of cognitive developmental capacity as a result of the anomaly diagnosed, the pregnant woman should be offered the alternatives of aggressive and non-aggressive obstetric management and induced abortion before viability. • It is also ethically permissible to offer feticide followed by termination of pregnancy after viability in such cases. This ethically justified approach will reduce the variation in the actual practices of specialists in maternal-fetal medicine. Chervenak, F. and L. B. Mc. Cullough (2012). "Responsibly counselling women about the clinical management of pregnancies complicated by severe fetal anomalies. " J Med Ethics 38(7): 397 -398.
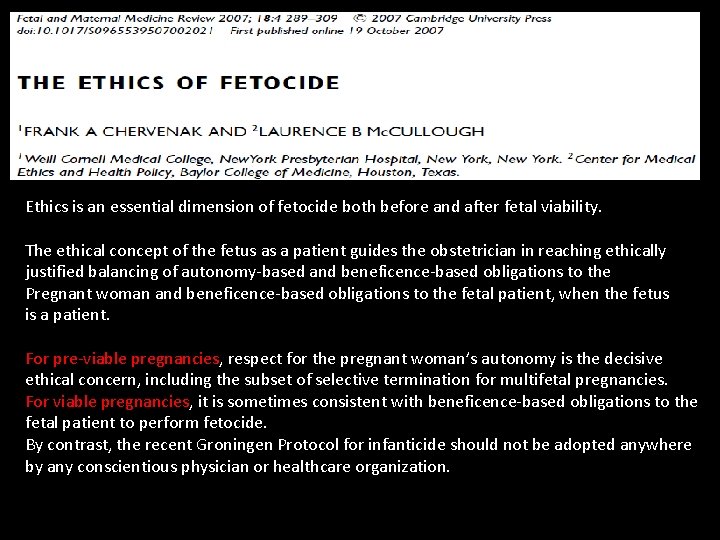
Ethics is an essential dimension of fetocide both before and after fetal viability. The ethical concept of the fetus as a patient guides the obstetrician in reaching ethically justified balancing of autonomy-based and beneficence-based obligations to the Pregnant woman and beneficence-based obligations to the fetal patient, when the fetus is a patient. For pre-viable pregnancies, respect for the pregnant woman’s autonomy is the decisive ethical concern, including the subset of selective termination for multifetal pregnancies. For viable pregnancies, it is sometimes consistent with beneficence-based obligations to the fetal patient to perform fetocide. By contrast, the recent Groningen Protocol for infanticide should not be adopted anywhere by any conscientious physician or healthcare organization.
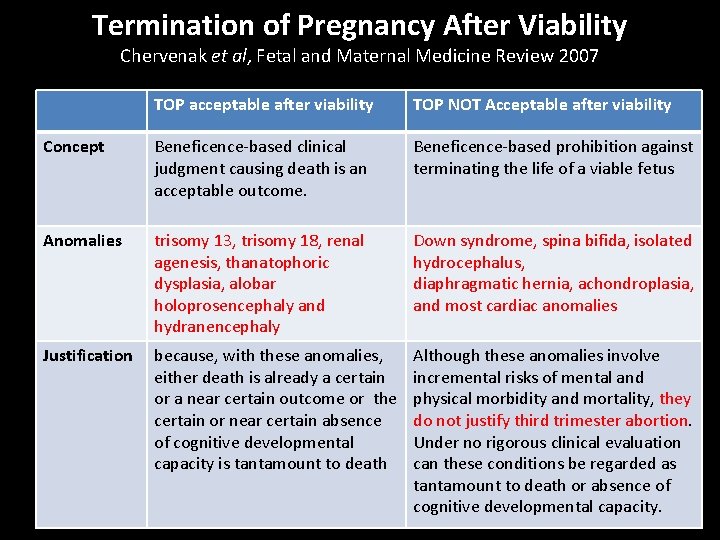
Termination of Pregnancy After Viability Chervenak et al, Fetal and Maternal Medicine Review 2007 TOP acceptable after viability TOP NOT Acceptable after viability Concept Beneficence-based clinical judgment causing death is an acceptable outcome. Beneficence-based prohibition against terminating the life of a viable fetus Anomalies trisomy 13, trisomy 18, renal agenesis, thanatophoric dysplasia, alobar holoprosencephaly and hydranencephaly Down syndrome, spina bifida, isolated hydrocephalus, diaphragmatic hernia, achondroplasia, and most cardiac anomalies Justification because, with these anomalies, either death is already a certain or a near certain outcome or the certain or near certain absence of cognitive developmental capacity is tantamount to death Although these anomalies involve incremental risks of mental and physical morbidity and mortality, they do not justify third trimester abortion. Under no rigorous clinical evaluation can these conditions be regarded as tantamount to death or absence of cognitive developmental capacity.
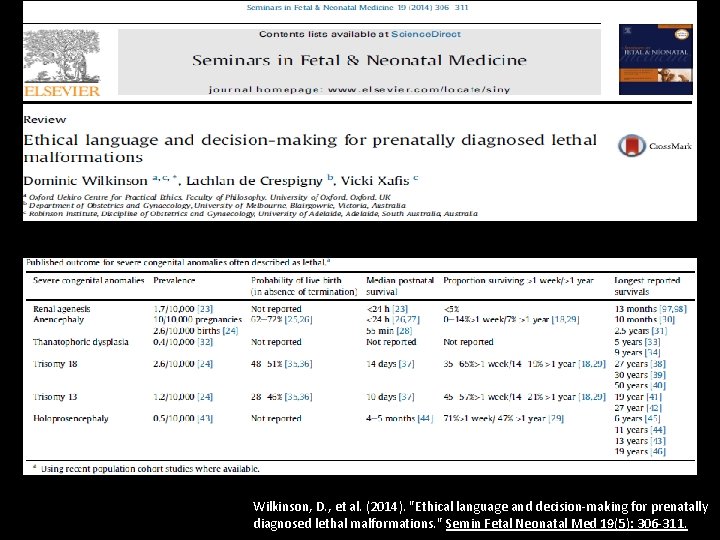
Wilkinson, D. , et al. (2014). "Ethical language and decision-making for prenatally diagnosed lethal malformations. " Semin Fetal Neonatal Med 19(5): 306 -311.
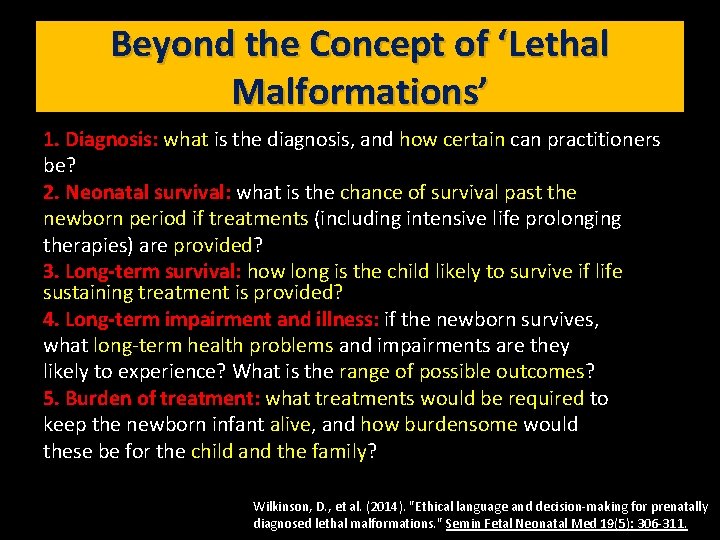
Beyond the Concept of ‘Lethal Malformations’ 1. Diagnosis: what is the diagnosis, and how certain can practitioners be? 2. Neonatal survival: what is the chance of survival past the newborn period if treatments (including intensive life prolonging therapies) are provided? 3. Long-term survival: how long is the child likely to survive if life sustaining treatment is provided? 4. Long-term impairment and illness: if the newborn survives, what long-term health problems and impairments are they likely to experience? What is the range of possible outcomes? 5. Burden of treatment: what treatments would be required to keep the newborn infant alive, and how burdensome would these be for the child and the family? Wilkinson, D. , et al. (2014). "Ethical language and decision-making for prenatally diagnosed lethal malformations. " Semin Fetal Neonatal Med 19(5): 306 -311.
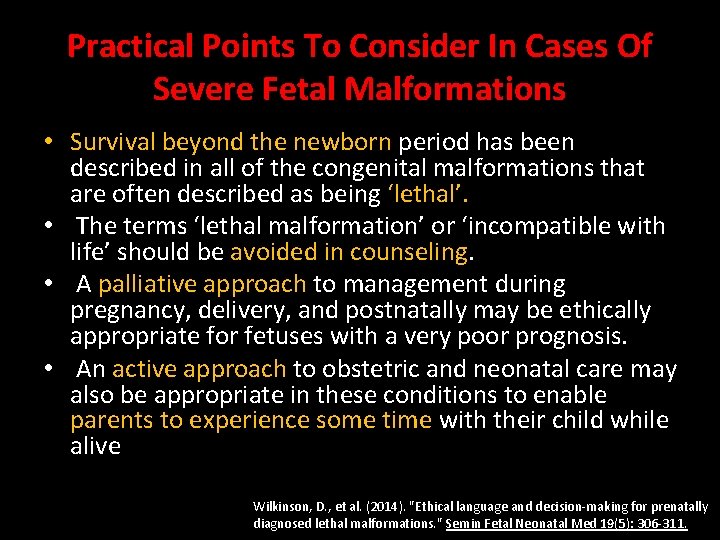
Practical Points To Consider In Cases Of Severe Fetal Malformations • Survival beyond the newborn period has been described in all of the congenital malformations that are often described as being ‘lethal’. • The terms ‘lethal malformation’ or ‘incompatible with life’ should be avoided in counseling. • A palliative approach to management during pregnancy, delivery, and postnatally may be ethically appropriate for fetuses with a very poor prognosis. • An active approach to obstetric and neonatal care may also be appropriate in these conditions to enable parents to experience some time with their child while alive Wilkinson, D. , et al. (2014). "Ethical language and decision-making for prenatally diagnosed lethal malformations. " Semin Fetal Neonatal Med 19(5): 306 -311.


Ethics Committee • • Obstetrician Maternal-Fetal Medicine Neonatologist Medical director Ethicist Anesthetist Obstetric nurse +∕-
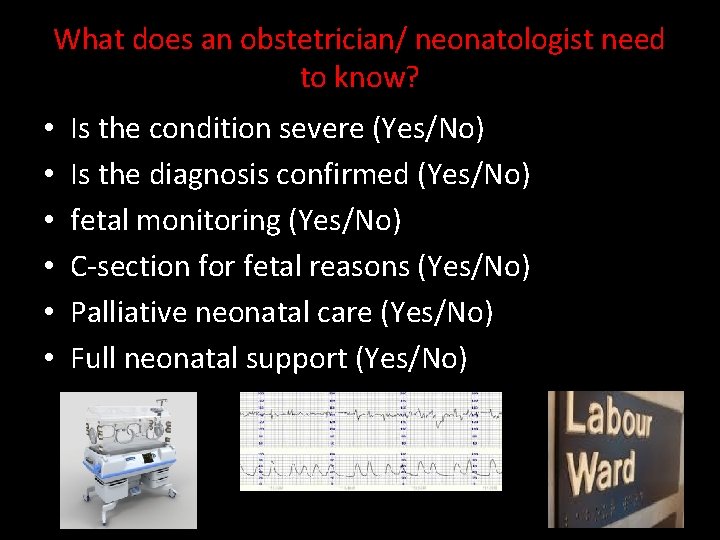
What does an obstetrician/ neonatologist need to know? • • • Is the condition severe (Yes/No) Is the diagnosis confirmed (Yes/No) fetal monitoring (Yes/No) C-section for fetal reasons (Yes/No) Palliative neonatal care (Yes/No) Full neonatal support (Yes/No)
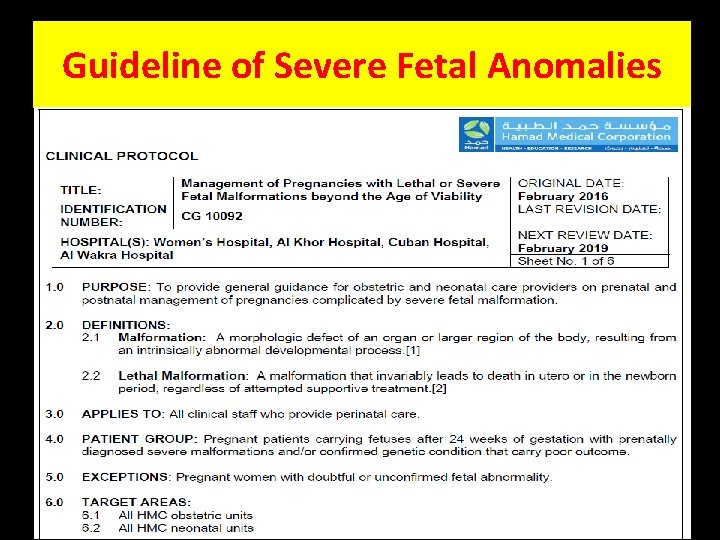
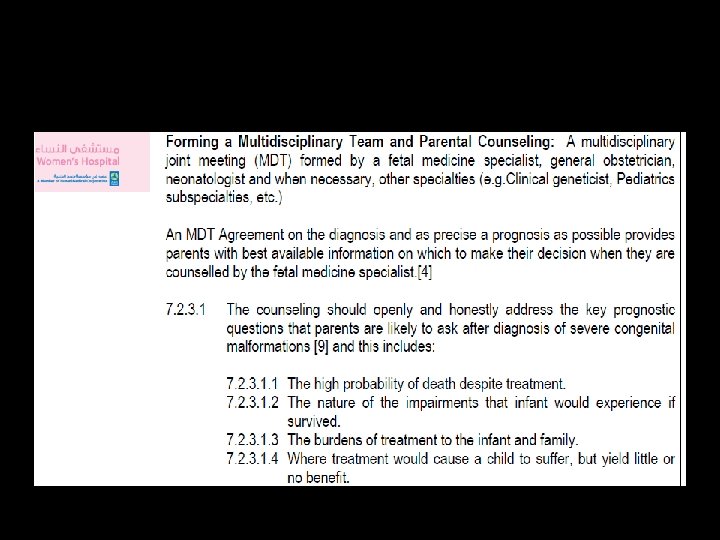
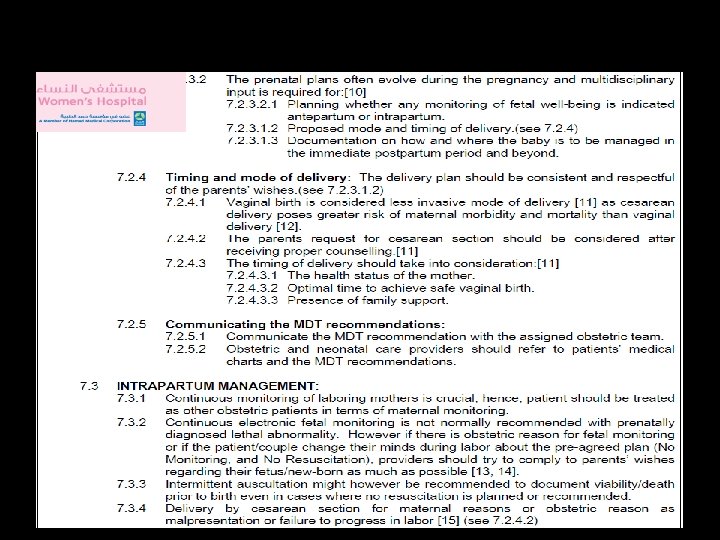
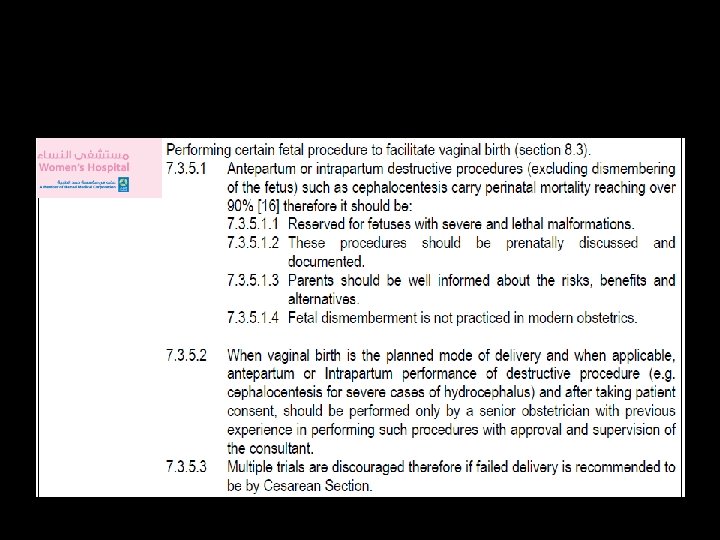
Guideline of Severe Fetal Anomalies
Summary and Conclusions • Fetal anomalies beyond viability may be an obstetric challenge. • Early detection, early anatomy screening policy and good quality ultrasound may optimize the pregnancy outcome. • Multidisciplinary input • TOP option where possible • Maternal-focused obstetric care and perinatal palliative care when appropriate • Whenever appropriate, fetal-oriented obstetric care and some life-sustaining treatments for these conditions where this is consistent with a woman's wishes and the child's best interests. • Further research on this subject based on our local data

Thank You qatarfetus@gmail. com
- Slides: 44