Management Of Exacerbations Of Chronic Obstructive Pulmonary Disease
Management Of Exacerbations Of Chronic Obstructive Pulmonary Disease D. Anan Esmail
Acute Exacerbations of COPD Cough increases in frequency and severity Sputum production increases in volume and/or changes character Dyspnea increases
These episodes vary in severity from: Mild exacerbations • only one of the three cardinal symptoms moderate to severe exacerbations • at least two of the three cardinal symptoms
HOME MANAGEMENT OF COPD EXACERBATIONS
glucocorticoids bronchodilator Antibiotics management of COPD EXACERBATIONS
Inhaled short-acting beta adrenergic agonists mainstay of therapy of acute exacerbation COPD rapid onset of action efficacy in producing bronchodilation

Inhaled short-acting beta adrenergic agonists administered by a metered dose inhaler (MDI) with a spacer device
Inhaled short-acting beta adrenergic agonists two inhalations by MDI every four to six hours
Inhaled short-acting beta adrenergic agonists Patients who already have a nebulizer at home
Inhaled short-acting beta adrenergic agonists administration of beta adrenergic agonists via nebulizer is helpful during COPD exacerbations
Inhaled short-acting beta adrenergic agonists most studies have not supported a greater effect from nebulizer treatments over properly administered metered dose inhaler medication
Inhaled short-acting beta adrenergic agonists may be combined with a short acting anticholinergic agent
Inhaled short-acting beta adrenergic agonists combination therapy produces bronchodilation in excess of that achieved by either agent alone
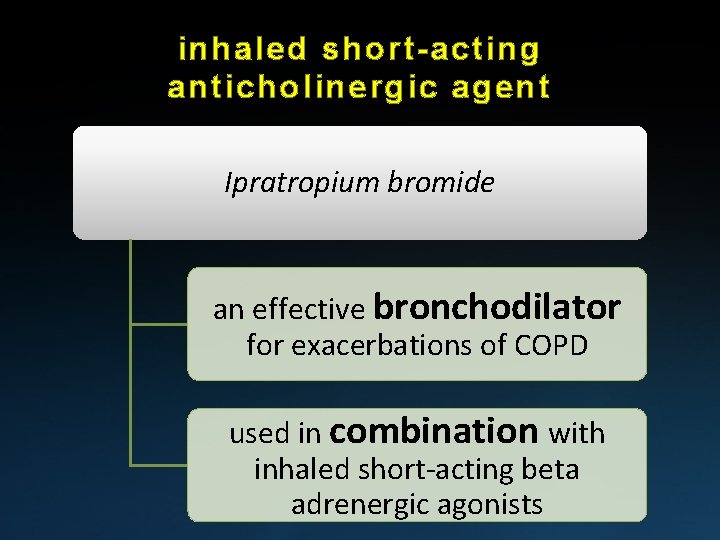
inhaled short-acting anticholinergic agent Ipratropium bromide an effective bronchodilator for exacerbations of COPD used in combination with inhaled short-acting beta adrenergic agonists
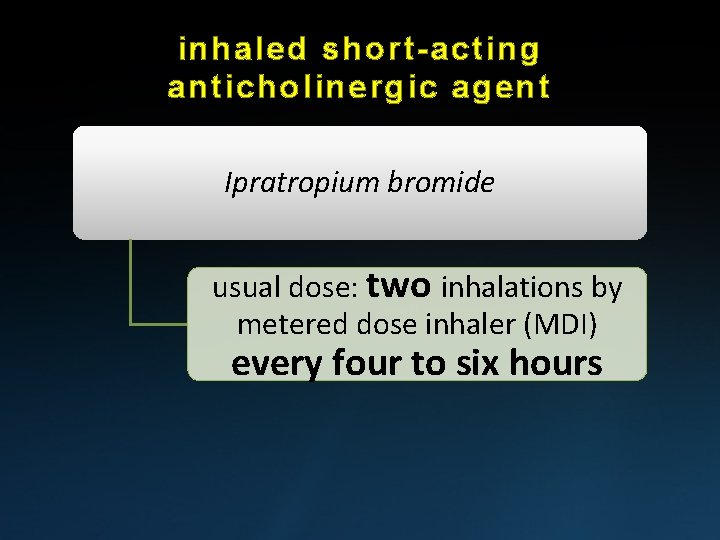
inhaled short-acting anticholinergic agent Ipratropium bromide usual dose: two inhalations by metered dose inhaler (MDI) every four to six hours
glucocorticoids bronchodilator Antibiotics management of COPD EXACERBATIONS
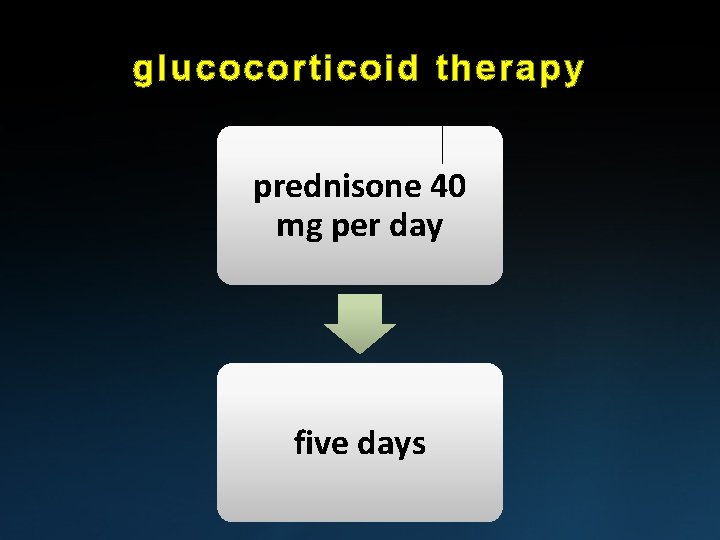
glucocorticoid therapy prednisone 40 mg per day five days
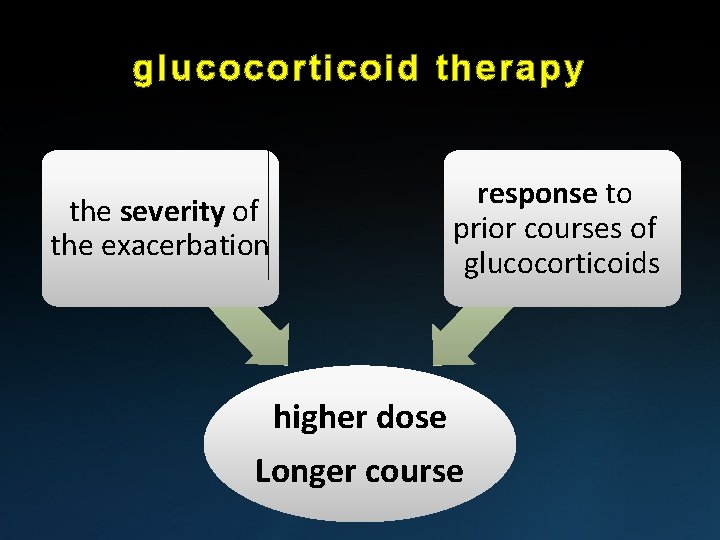
glucocorticoid therapy the severity of the exacerbation response to prior courses of glucocorticoids higher dose Longer course
inhaled glucocorticoids The efficacy of inhaled glucocorticoids on the course of a COPD exacerbation has not been studied
inhaled glucocorticoids should not be used as a substitute for systemic glucocorticoid therapy in COPD exacerbations
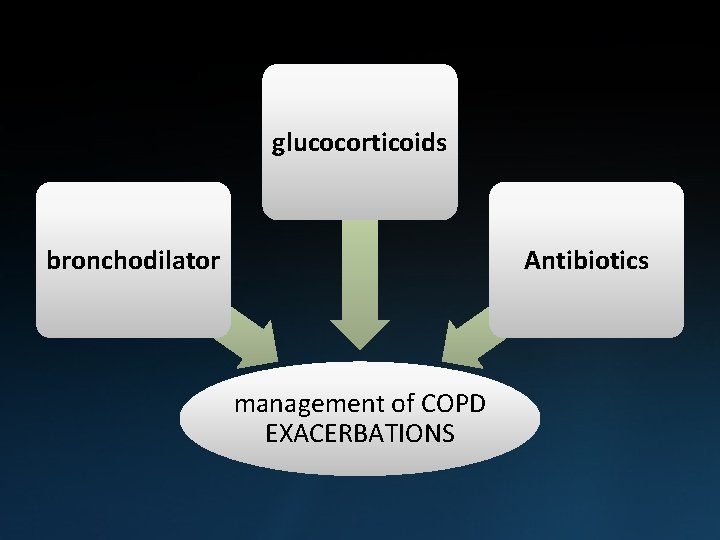
glucocorticoids bronchodilator Antibiotics management of COPD EXACERBATIONS
Antibiotics guidelines recommend antibiotic therapy only for: patients have bacterial infection
Antibiotics guidelines recommend antibiotic therapy only for: moderate or severe exacerbation of COPD
Antibiotics The initial antibiotic regimen should target likely bacterial pathogens Haemophilus influenzae Moraxella catarrhalis Streptococcus pneumoniae
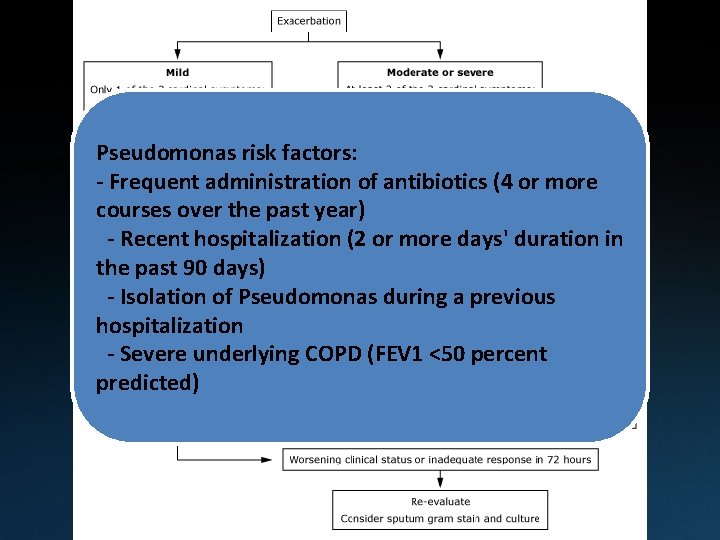
Pseudomonas risk factors: - Frequent administration of antibiotics (4 or more courses over the past year) - Recent hospitalization (2 or more days' duration in (Grade 2 B) the past 90 days) - Isolation of Pseudomonas during a previous hospitalization - Severe underlying COPD (FEV 1 <50 percent predicted)
HOSPITAL MANAGEMENT OF COPD EXACERBATIONS
glucocorticoids bronchodilator Antibiotics management of COPD EXACERBATIONS
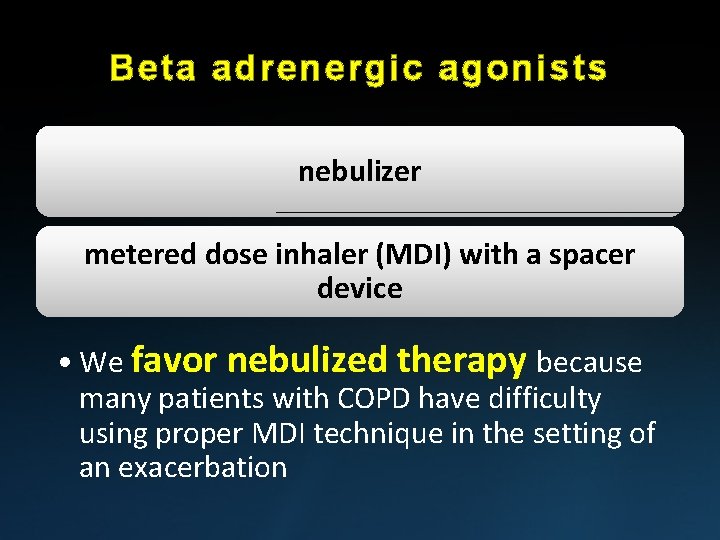
Beta adrenergic agonists nebulizer metered dose inhaler (MDI) with a spacer device • We favor nebulized therapy because many patients with COPD have difficulty using proper MDI technique in the setting of an exacerbation
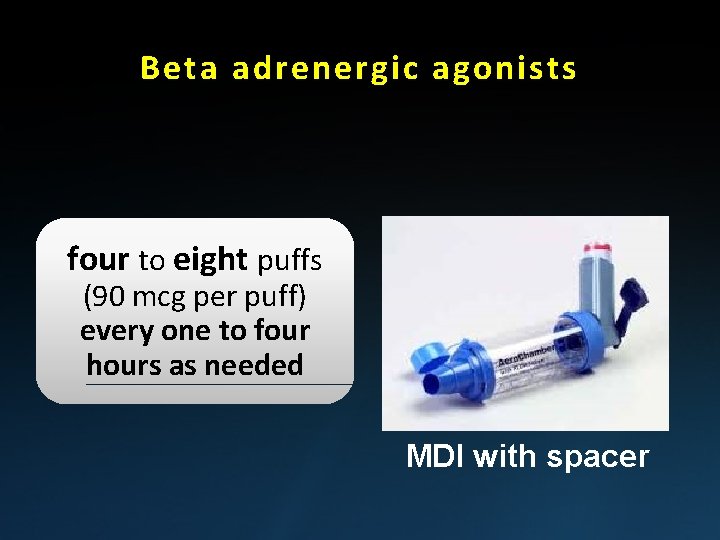
Beta adrenergic agonists four to eight puffs (90 mcg per puff) every one to four hours as needed MDI with spacer
Beta adrenergic agonists albuterol 2. 5 mg every one to four hours as needed nebulization
Beta adrenergic agonists Increasing dose of albuterol to 5 mg does not have a significant impact on spirometry or clinical outcomes nebulization
Beta adrenergic agonists continuously nebulized beta agonists have not been shown to confer an advantage in COPD nebulization
Beta adrenergic agonists using air, rather than oxygen-driven bronchodilator nebulization
Anticholinergic agents two to four puffs (18 mcg per puff) every four hours as needed MDI with spacer
Anticholinergic agents Ipratropium 500 mcg every four hours as needed nebulization
Systemic glucocorticoids improve symptoms and lung function reduced treatment failure decrease the length of hospital stay
Systemic glucocorticoids Oral glucocorticoids rapidly absorbed (peak serum levels achieved at one hour after ingestion) appear equally efficacious to intravenous glucocorticoids
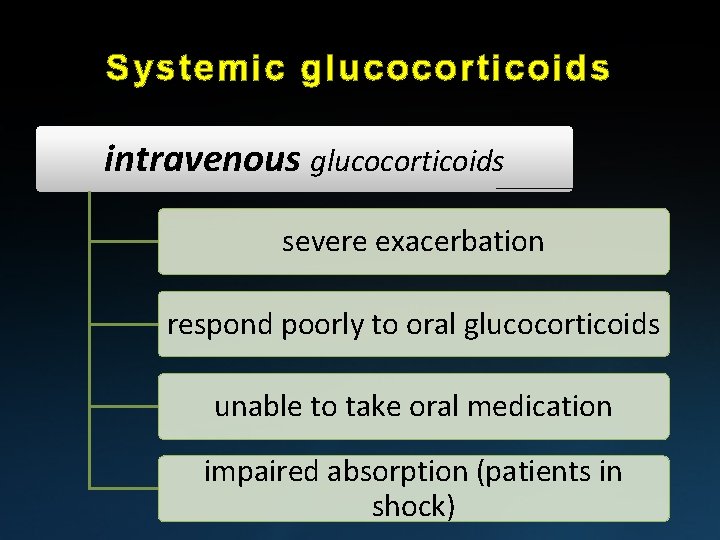
Systemic glucocorticoids intravenous glucocorticoids severe exacerbation respond poorly to oral glucocorticoids unable to take oral medication impaired absorption (patients in shock)
Systemic glucocorticoids Dose prednisone 40 mg once daily
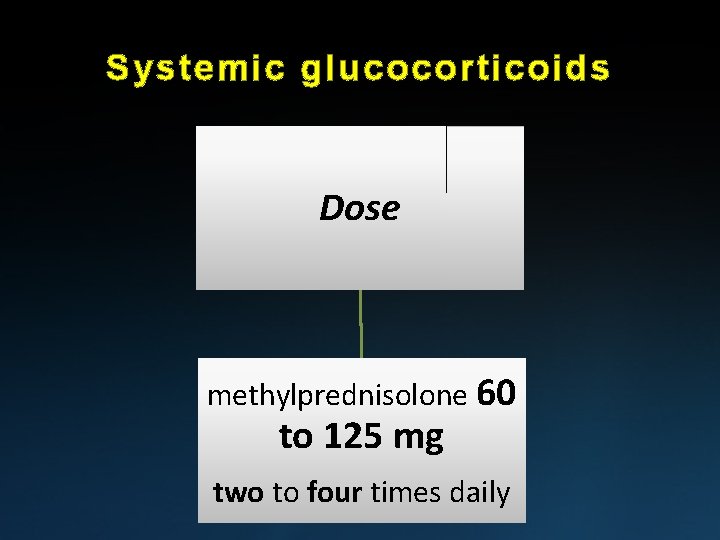
Systemic glucocorticoids Dose methylprednisolone 60 to 125 mg two to four times daily
Systemic glucocorticoids evidence favors using a moderate rather than high dose of glucocorticoids for most patients with an exacerbation of COPD
Systemic glucocorticoids higher dose: methylprednisolone >240 mg/day • not associated with a mortality benefit • shorter hospital and ICU lengths of stay
Systemic glucocorticoids The optimal duration of systemic glucocorticoid therapy depends on the severity of the exacerbation and the observed response to therapy (5 to 14 days)
Systemic glucocorticoids longer duration No additional benefit more glucocorticoidrelated side effects
glucocorticoid therapy adverse effects hyperglycimia
glucocorticoid therapy adverse effects upper gastrointestinal bleeding
glucocorticoid therapy adverse effects psychiatric disorders
Antibiotic treatment of acute exacerbations of COPD (hospitalized)
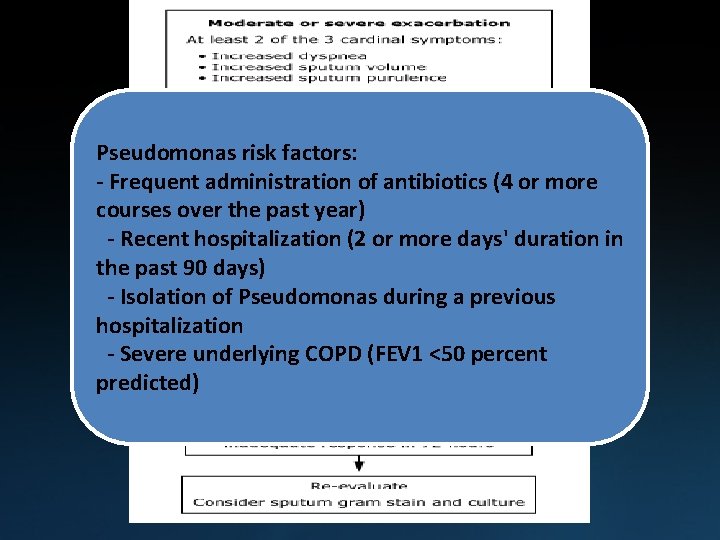
Pseudomonas risk factors: - Frequent administration of antibiotics (4 or more courses over the past year) - Recent hospitalization (2 or more days' duration in the past 90 days) - Isolation of Pseudomonas during a previous hospitalization - Severe underlying COPD (FEV 1 <50 percent predicted)
Adjunctive care Thromboprophylaxis • Hospitalization for exacerbations of COPD increases the risk for deep venous thrombosis and pulmonary embolism

Adjunctive care cigarette smoking cessation

Adjunctive care nutritional support

Adjunctive care continuation of ongoing supplemental oxygen therapy
Adjunctive care • administration of supplemental oxygen should target ¶pulse oxygen saturation (Sp. O ) of 88 to 92 percent
Adjunctive care • administration of supplemental oxygen should target ¶arterial oxygen tension (Pa. O ) of approximately 60 to 70 mm. Hg
Adjunctive care A high Fi. O is not required to correct the hypoxemia associated with most exacerbations of COPD
Adjunctive care the risk of prompting worsened hypercapnia with excess supplemental oxygen
Oxygen therapy Hypercapnia is generally well tolerated in patients whose (Pa. CO ) is chronically elevated
Oxygen therapy Adequate oxygenation to achieve an oxygen saturation of 88 to 92 percent must be assured, even if it leads to acute hypercapnia
Oxygen therapy mechanical ventilation may be required if hypercapnia is associated with • depressed mental status • profound acidemia • cardiac dysrhythmias
MECHANICAL VENTILATION • Noninvasive ventilation ¶preferred method of ventilatory support ¶improves numerous clinical outcomes
MECHANICAL VENTILATION • Invasive ventilation ¶patients fail NPPV ¶do not tolerate NPPV ¶have contraindications to NPPV
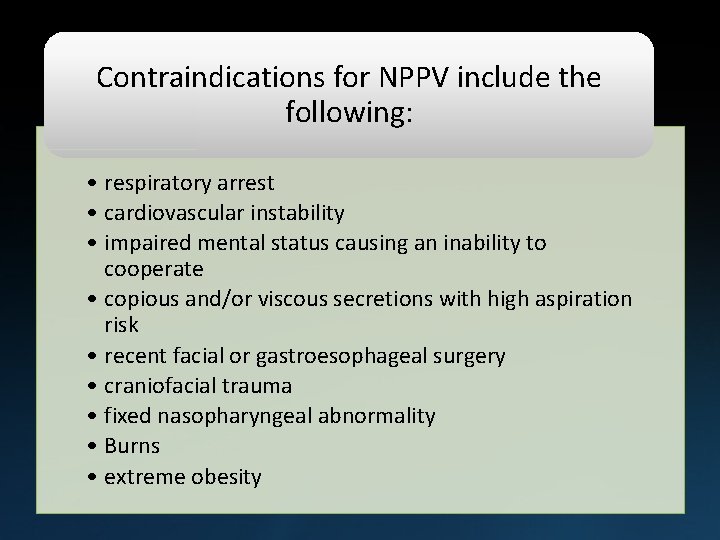
Contraindications for NPPV include the following: • respiratory arrest • cardiovascular instability • impaired mental status causing an inability to cooperate • copious and/or viscous secretions with high aspiration risk • recent facial or gastroesophageal surgery • craniofacial trauma • fixed nasopharyngeal abnormality • Burns • extreme obesity
Treatments without documented benefit not been shown to confer benefit for patients with a COPD exacerbation
Treatments without documented benefit Mucoactive agents mechanical techniques to augment sputum clearance
Treatments without documented benefit Methylxanthines • aminophylline and theophylline, are considered second-line therapy for exacerbations of COPD • nausea and vomiting, tremor, palpitations, arrhythmias
Treatments without documented benefit Nebulized magnesium • no effect on FEV when added to nebulized salbutamol (albuterol) in patients with exacerbations of COPD
Treatments without documented benefit Subcutaneous injection of short-acting beta adrenergic agonists (eg, terbutaline, epinephrine) almost never used for COPD exacerbations (Arrhythmias , myocardial ischemia)
PROGNOSIS Exacerbations of COPD are associated with increased mortality (3 to 9 %)
Factors Associated With Increased Mortality
Increased age - male gender Severity of airway obstruction (FEV 1) prior hospitalization for COPD
Hypercapnia urea >8 mmol/L presence of Pseudomonas aeruginosa in the patient’s sputum
PREVENTION • smoking cessation
PREVENTION • pulmonary rehabilitation
PREVENTION • vaccination seasonal influenza and pneumococcus
PREVENTION • proper use of medications (metered dose inhaler technique)
PREVENTION use of an action plan earlier recognition of an exacerbation by the patient earlier initiation of antibiotics earlier initiation of glucocorticoids
PREVENTION Prophylactic antibiotics • we suggest not administering antibiotic prophylaxis For most patients with COPD

- Slides: 79