MANAGEMENT OF EARLY BREAST CANCER BY GEMY MARIA
MANAGEMENT OF EARLY BREAST CANCER BY GEMY MARIA GEORGE 2002 BATCH
Early breast cancer 1. STAGE 0 INSITU CARCINOMA DCIS, LCIS 2. STAGE I T 1 N 0 M 0 3. STAGE II A- T 0 N 1 M 0 T 1 N 1 M 0 T 2 N 0 M 0 B -T 2 N 1 M 0.
TRIPLE ASSESSMENT o o o CLINCAL ASSESSMENT. RADIOLOGICAL IMAGING. TISSUE DIAGNOSIS

INVESTIGATIONS o ROUTINE BLOOD EXAMINATIONHb, TC, DC, ESR o BT, CT o ECG o CXR
BREAST IMAGING o o o MAMMOGRAPHY USG MRI
MAMMOGRAPHY o o o DELIVERS LOW VOLTAGE HIGH AMPERAGE X-RAYS AVERAGE DOSE 0. 1 c. Gy 2 TYPESn SCREENING & DIAGNOSTIC
MAMMOGRAPHY o SCREENING n n FOR ASYMPTOMATIC WOMEN AGED>40 YRS ANNUALLY. YOUNGER WOMEN IN HIGH RISK GROUP o DIAGNOSTIC n n n FOR A WOMAN WHO HAS A COMPLAINT( LUMP, PAIN, NIPPLE DISCHARGE…. ) PAST HISTORY OF BREAST CANCER A FINDING ON SCREENING MAMMOGRAM THAT REQUIRES FURTHER EVALUATION.
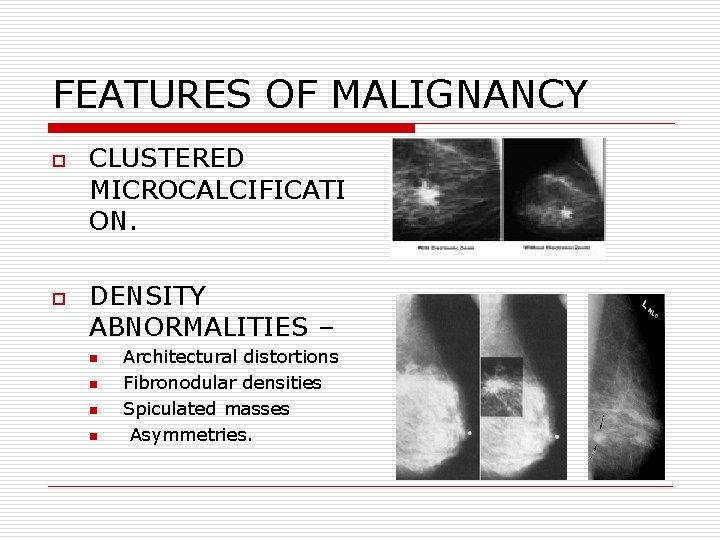
FEATURES OF MALIGNANCY o o CLUSTERED MICROCALCIFICATI ON. DENSITY ABNORMALITIES – n n Architectural distortions Fibronodular densities Spiculated masses Asymmetries.
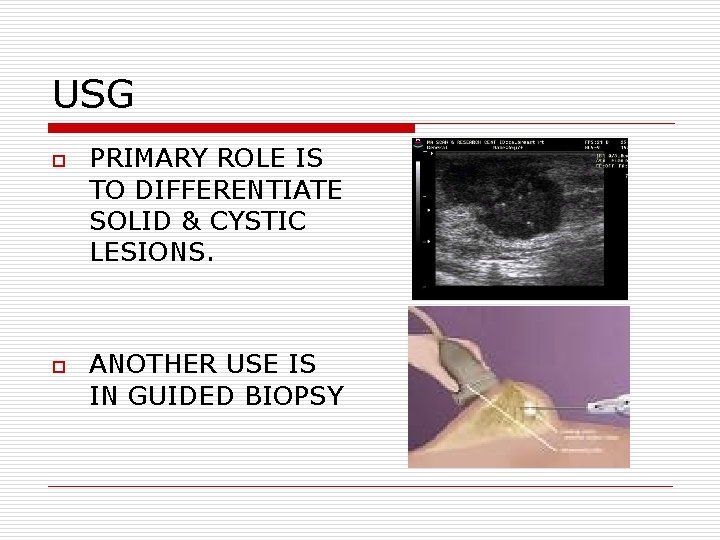
USG o o PRIMARY ROLE IS TO DIFFERENTIATE SOLID & CYSTIC LESIONS. ANOTHER USE IS IN GUIDED BIOPSY
DISADVANTAGES o o o DOES NOT DISPLAY MICRO CALCIFICATION…. SENSITIVITY IS LIMITED IN FATTY BREAST. HIGH FALSE POSITIVITY
MRI o o o TO DISTINGUISH SCAR FROM RECURRANCE. GOLD STANDARD FOR IMAGING BREAST WITH IMPLANTS. FOR WORK-UP OF AXILLARY METASTATIC LYMPHADENOPATHY. .
BIOPSY o o o FNAC TRU-CUT BIOPSY INCISION BIOPSY EXCISION BIOPSY SENTINEL LN BIOPSY
FNAC o o o PERFORMED WHEN A CLINICALLY PALPABLE MASS IS EVIDENT. USES 21 G NEEDLE & 10 ml SYRINGE. ASPIRATE IS SMEARED INTO SLIDE & FIXED.
FNAC-contd… o ADVANTAGES n immediate results, n no incision, n minimal discomfort, n no tumor spillage. o DISADVANTAGES n -can’t diff. insitu& invasive ca, n false negative results(15%).
TRU-CUT BIOPSY o o o PROVIDES MORE DETAILED HISTOPATHOLOGIC INFORMATION. DIFFERENTIATES BETWEEN INSITU & INVASIVE CA. STAINING FOR RECEPTOR STATUS.
INCISION BIOPSY o o o FOR PATIENTS WITH LARGE PRIMARY( >5 cm)LESIONS. INCISION OF A SMALL PORTION OF TISSUE THAT IS NOT NECRTIC. PERMITS HISTOLOGIC & HORMONAL RECEPTOR STATUS ANALYSIS.
EXCISION BIOPSY REMOVAL OF ENTIRE LESION & A MARGIN OF NORMAL BREAST PARENCHYMA. o
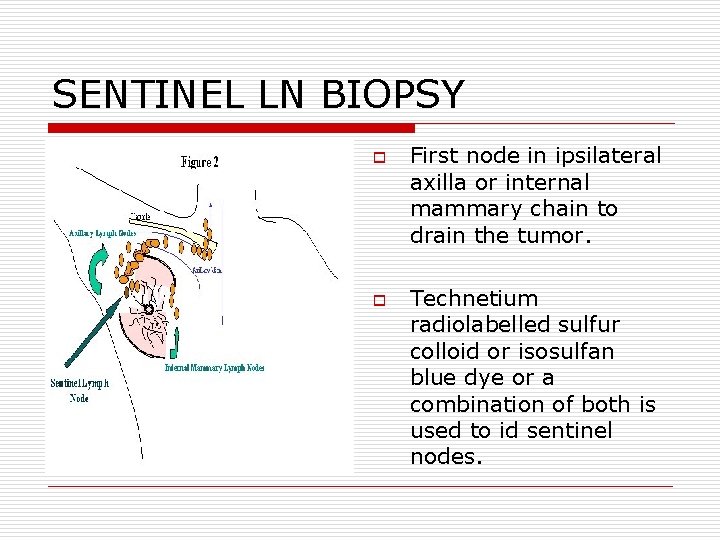
SENTINEL LN BIOPSY o o First node in ipsilateral axilla or internal mammary chain to drain the tumor. Technetium radiolabelled sulfur colloid or isosulfan blue dye or a combination of both is used to id sentinel nodes.

MANAGEMENT OF INSITU CA PRE INVASIVE CA THAT HAS NOT BREACHED THE EPITHELIAL BASEMENT MEMBRANE.
STAGE 0 -DCIS o o o 10 -20% BILATERAL. TRUE PRECURSOR OF INVASIVE CA. (30 -50% RISK ) DCIS MAY BE CLASSIFIED BY VAN NUYS PRONOSTIC INDEX.
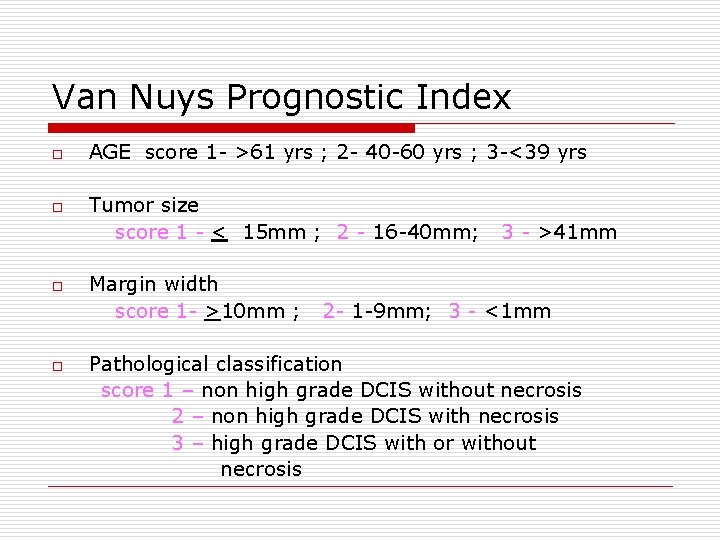
Van Nuys Prognostic Index o o AGE score 1 - >61 yrs ; 2 - 40 -60 yrs ; 3 -<39 yrs Tumor size score 1 - < 15 mm ; 2 - 16 -40 mm; Margin width score 1 - >10 mm ; 3 - >41 mm 2 - 1 -9 mm; 3 - <1 mm Pathological classification score 1 – non high grade DCIS without necrosis 2 – non high grade DCIS with necrosis 3 – high grade DCIS with or without necrosis
DCIS n OPTIONSo EXCISION + RT o MASTECTOMY
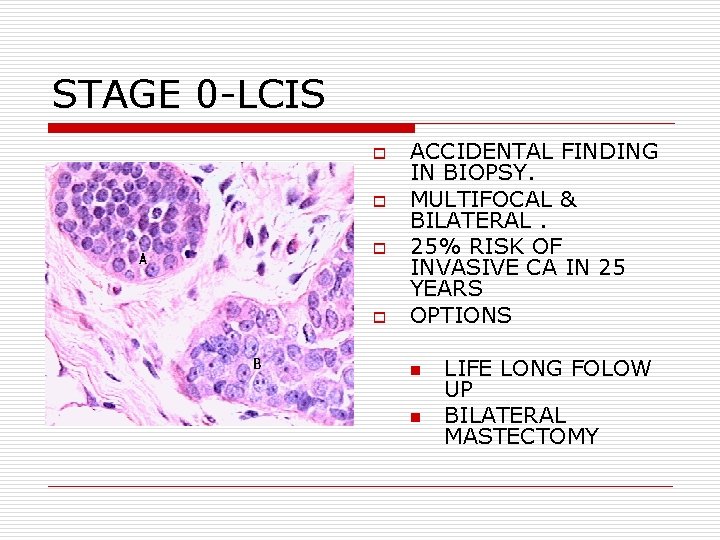
STAGE 0 -LCIS o o ACCIDENTAL FINDING IN BIOPSY. MULTIFOCAL & BILATERAL. 25% RISK OF INVASIVE CA IN 25 YEARS OPTIONS n n LIFE LONG FOLOW UP BILATERAL MASTECTOMY
MANAGEMENT OF EARLY INVASIVE CA o AIM n LOCOREGIONAL CONTROL. n SYSTEMIC CONTROL. n CONSERVATION OF LOCAL FORM & FUNCTION
TREATMENT o MULTIMODALITY TREATMENT n SURGERY n RADIOTHERAPY n CHEMOTHERAPY n HORMONAL THERAPY n OVARIAN ABLATION
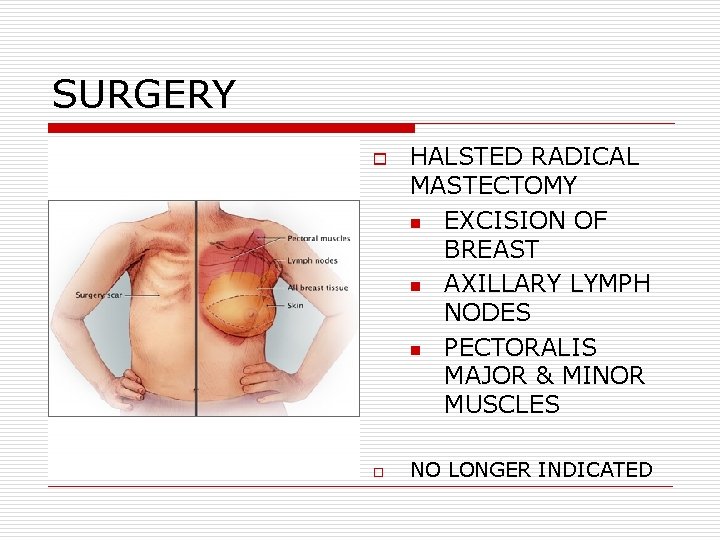
SURGERY o o HALSTED RADICAL MASTECTOMY n EXCISION OF BREAST n AXILLARY LYMPH NODES n PECTORALIS MAJOR & MINOR MUSCLES NO LONGER INDICATED
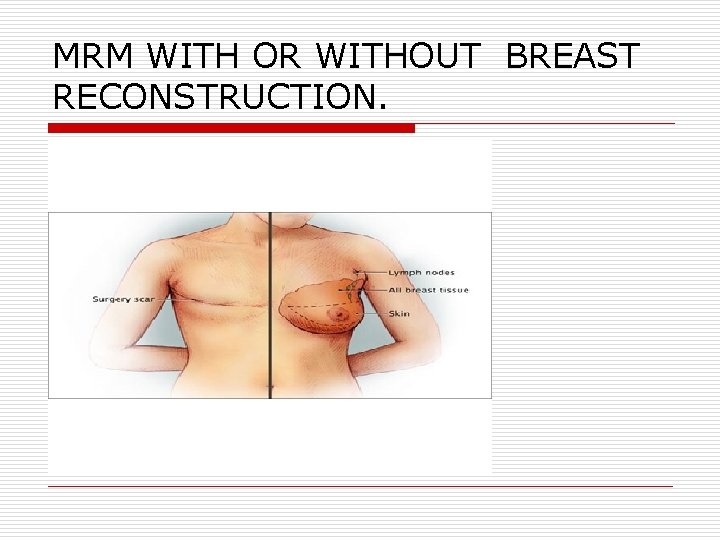
MRM WITH OR WITHOUT BREAST RECONSTRUCTION.
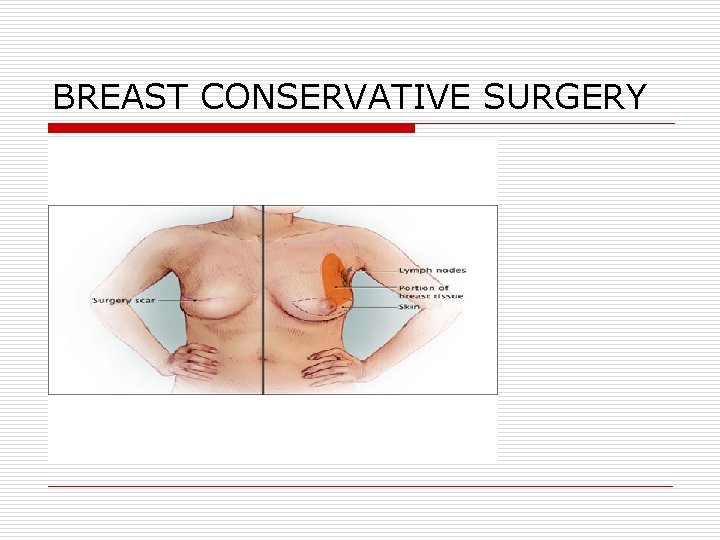
BREAST CONSERVATIVE SURGERY
WHY BREAST CONSERVATIVE SURGERY ? o OVER ALL SURVIVAL SIMILAR o SAVES THE BREAST o BUT PROPER PATIENT SELECTON IS IMPORTANT.
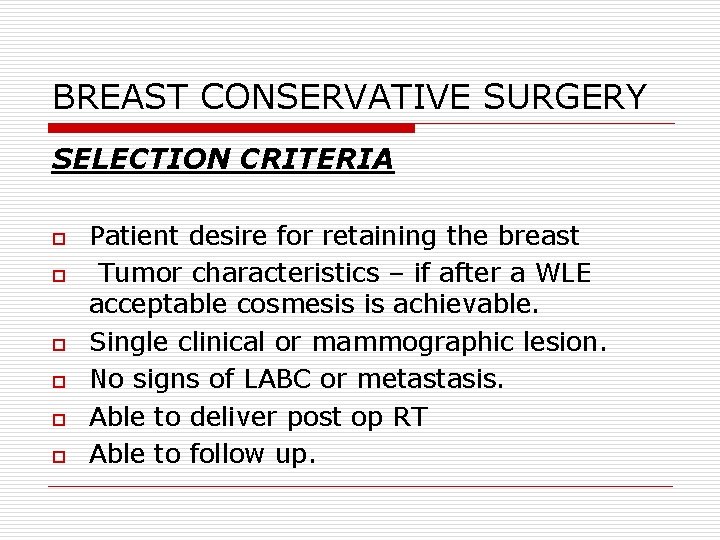
BREAST CONSERVATIVE SURGERY SELECTION CRITERIA o o o Patient desire for retaining the breast Tumor characteristics – if after a WLE acceptable cosmesis is achievable. Single clinical or mammographic lesion. No signs of LABC or metastasis. Able to deliver post op RT Able to follow up.
CONTRAINDICATIONS TUMOUR CHARACTERISTICS o n n n Multicentric Multifocal Large tumor to breast ratio Persistent +ve margins even after reasonable WLE Diffuse calcification… CONTRAINDICATIONS TO RADIOTHERAPY o n n n H/o previous irradiation to breast field– lymphomas 1 st and 2 nd trimester of pregnancy Active collagen vascular diseases
SURGERY o WIDE EXCISION o QUADRANTECTOMY

WIDE LOCAL EXCISION o REMOVAL OF TUMOUR PLUS A RIM OF ATLEAST 1 cm OF BREAST TISSUE.
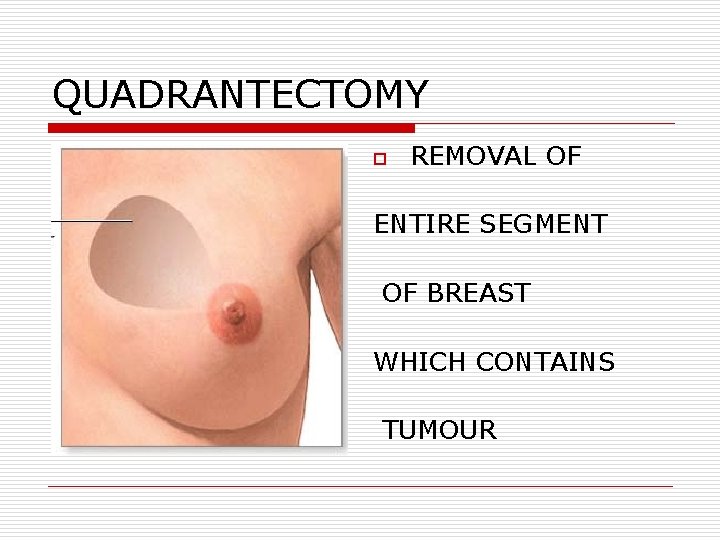
QUADRANTECTOMY o REMOVAL OF ENTIRE SEGMENT OF BREAST WHICH CONTAINS TUMOUR
n n EXCISION DONE WITH FROZEN SECTION TO CHECK MARGINS BEFORE CLOSURE. Patient whose margins are involved need a further local excision or a mastectomy.
WHAT TO DO WITH AXILLA ? o 2 OPTIONS o o SLNB AXILLARY DISSECTION
SENTINEL LYMPH NODE BIOPSY q MANAGEMENT OF AXILLA IN PATIENTS WITH CLINICALLY NODE NEGATIVE DISEASE. q THIS METHOD LOCALISES THE FIRST NODES THAT THE TUMOUR DRAINS TO.
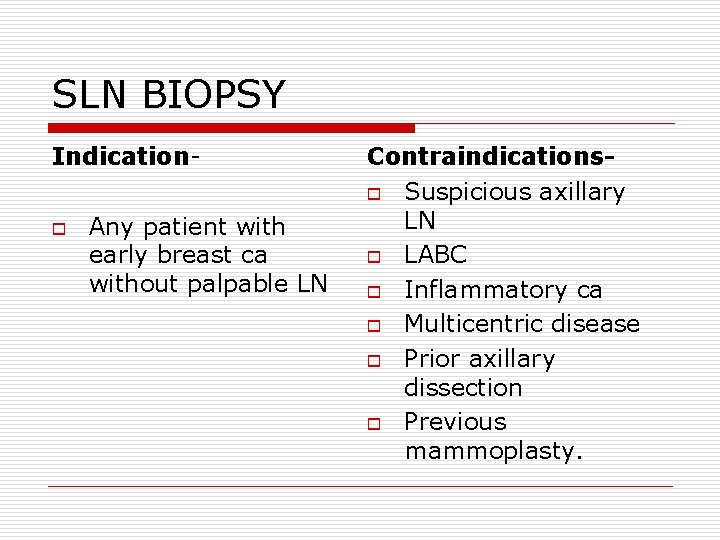
SLN BIOPSY Indicationo Any patient with early breast ca without palpable LN Contraindicationso Suspicious axillary LN o LABC o Inflammatory ca o Multicentric disease o Prior axillary dissection o Previous mammoplasty.
SLNB o o o Tc LABELED SULFUR COLLOIDISOSULPHAN BLUE DYE COMBINATION
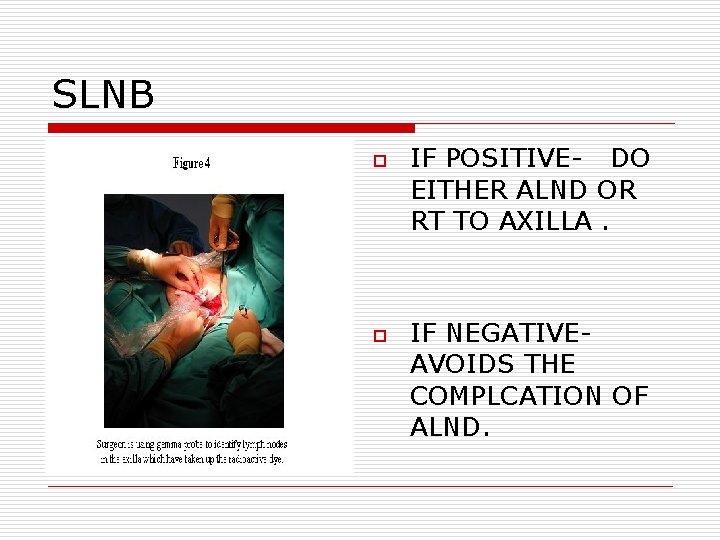
SLNB o o IF POSITIVE- DO EITHER ALND OR RT TO AXILLA. IF NEGATIVEAVOIDS THE COMPLCATION OF ALND.
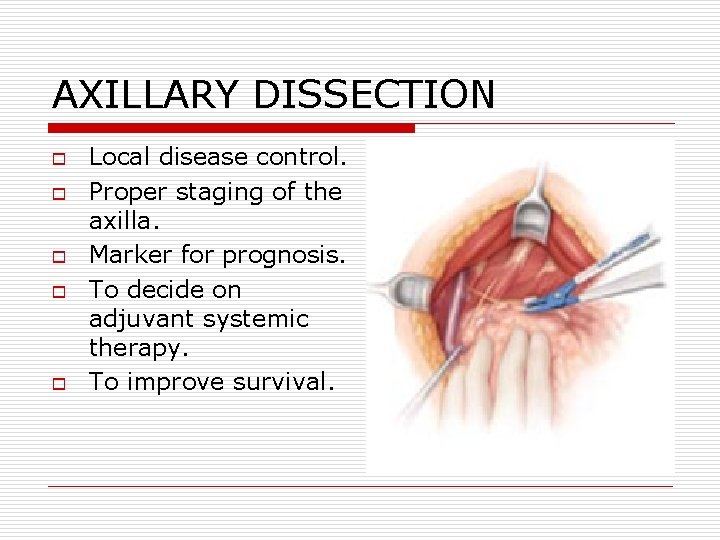
AXILLARY DISSECTION o o o Local disease control. Proper staging of the axilla. Marker for prognosis. To decide on adjuvant systemic therapy. To improve survival.
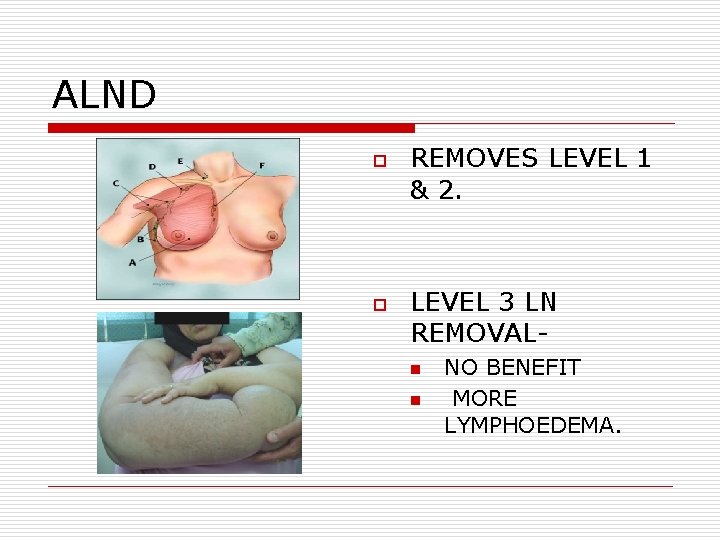
ALND o o REMOVES LEVEL 1 & 2. LEVEL 3 LN REMOVALn n NO BENEFIT MORE LYMPHOEDEMA.
BCS WITH RT o o BCS ALWAYS COMBINED WITH RT – TO CHEST WALL. EXCISION OF BREAST CANCER WITHOUT RT LEADS TO AN UNACCEPTABLE LOCAL RECURRENCE RATE.
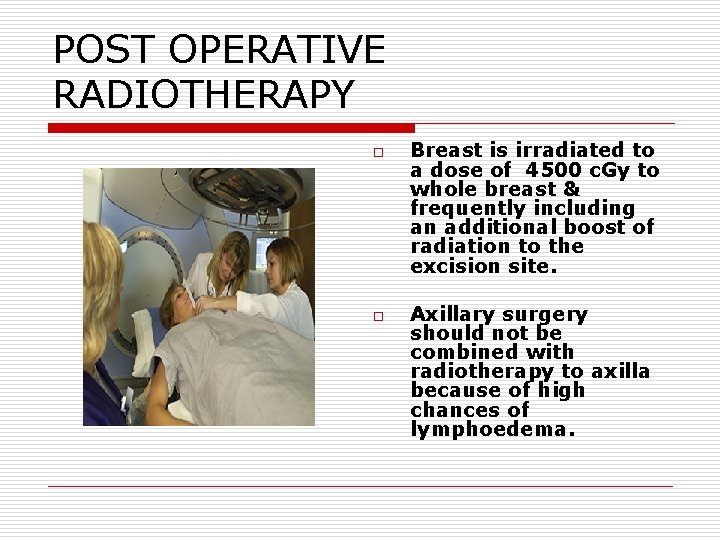
POST OPERATIVE RADIOTHERAPY o o Breast is irradiated to a dose of 4500 c. Gy to whole breast & frequently including an additional boost of radiation to the excision site. Axillary surgery should not be combined with radiotherapy to axilla because of high chances of lymphoedema.
MASTECTOMY o PATIENT PREFERENCE. o LARGE TUMOURS. o CENTRAL TUMORS BENEATH OR INVOLVING NIPPLE. o MULTIFOCAL DISEASE. o LOCAL RECURRANCE.
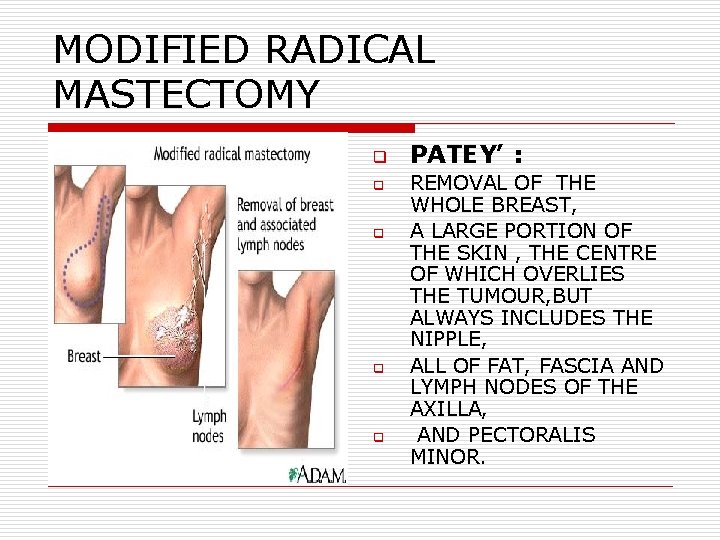
MODIFIED RADICAL MASTECTOMY q q q PATEY’ : REMOVAL OF THE WHOLE BREAST, A LARGE PORTION OF THE SKIN , THE CENTRE OF WHICH OVERLIES THE TUMOUR, BUT ALWAYS INCLUDES THE NIPPLE, ALL OF FAT, FASCIA AND LYMPH NODES OF THE AXILLA, AND PECTORALIS MINOR.
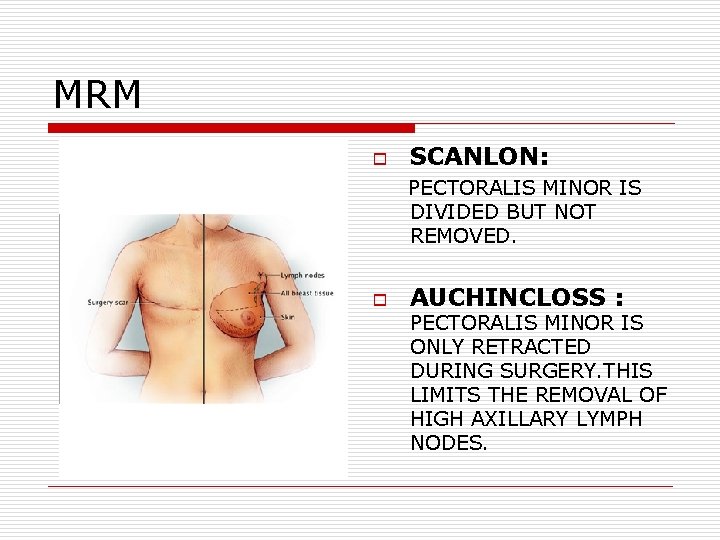
MRM o SCANLON: PECTORALIS MINOR IS DIVIDED BUT NOT REMOVED. o AUCHINCLOSS : PECTORALIS MINOR IS ONLY RETRACTED DURING SURGERY. THIS LIMITS THE REMOVAL OF HIGH AXILLARY LYMPH NODES.
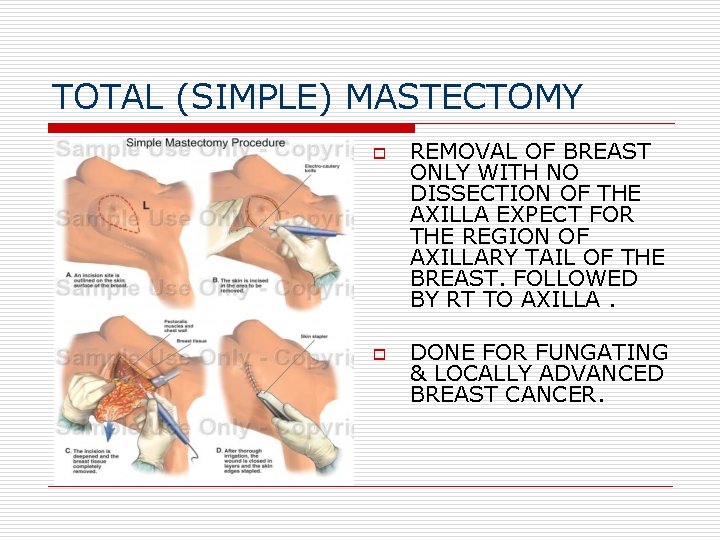
TOTAL (SIMPLE) MASTECTOMY o o REMOVAL OF BREAST ONLY WITH NO DISSECTION OF THE AXILLA EXPECT FOR THE REGION OF AXILLARY TAIL OF THE BREAST. FOLLOWED BY RT TO AXILLA. DONE FOR FUNGATING & LOCALLY ADVANCED BREAST CANCER.
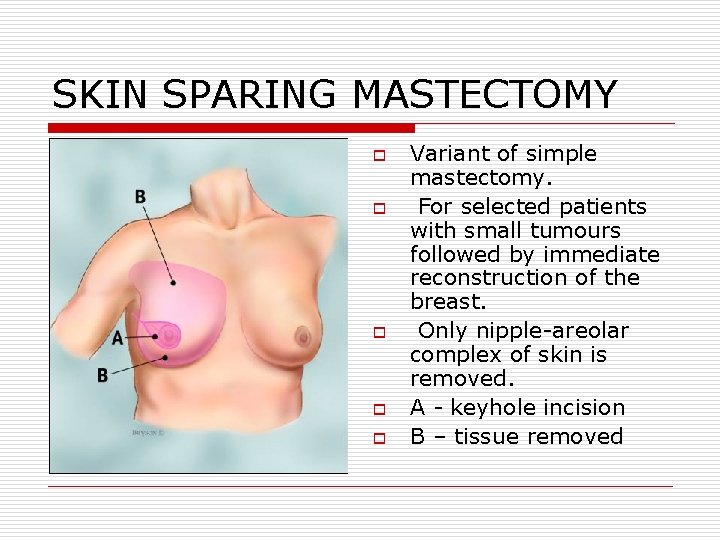
SKIN SPARING MASTECTOMY o o o Variant of simple mastectomy. For selected patients with small tumours followed by immediate reconstruction of the breast. Only nipple-areolar complex of skin is removed. A - keyhole incision B – tissue removed
MRM WITH RT ? o o NO RT NEEDED IF AXILLA IS NEGATIVE. GIVEN IF THE TUMOUR WAS HIGH GRADE, LARGE, HEAVILY NODE POSITIVE, OR IF THERE WAS EXTENSIVE LYMPHOVASCULAR INVASION.

SYSTEMIC THERAPY o o LOCOREGIONAL TREATMENT GIVES LOCAL CONTROL ONLY. OPTIONS n n n CHEMOTHERAPY HORMONE THERAPY OVARIAN ABLATION
CHEMOTHERAPY o o POST-OPERATIVE POLYCHEMOTHERAPY. MOST PREVALENT CHEMOTHERAPY COMBINATONS ARE n CAF(CYCLOPHOSPHA n CMF MIDE, DOXORUBICIN, 5 -FU) (CYCLOPHOSPHAMIDE, METHOTREXATE, 5 -FU)

CAF o o Six cycles – 3 WEEKLY THIS ANTHRACYCLINE CONTAINING REGIMEN – SLIGHTLY MORE EFFECTIVE THAN CMF.
EFFECTIVENESS OF CHEMOTHERAPY o DEPENDS ON n AGE/ MENOPAUSAL STATUS – o o n n ALL AGES(UPTO 70 YRS) BENEFIT. GREATEST BENEFIT IN PREMENOPAUSAL WOMEN NODAL STATUS – SIMILAR FOR NODE + ORTUMOUR GRADE.
HORMONAL THERAPY TAMOXIFEN o o o CURRENTLY THE FIRST LINE HORMONAL THERAPY. REDUCES ANNUAL RECURRENCE RATE. REDUCES THE INCIDENCE OF CONTRALATERAL BREAST CANCER.
TAMOXIFEN o o o SERM Weak estrogen agonist. In molar excess acts like an antagonist of estrogen activity in breast. Dose - 20 mg per day for 5 years.
SELECTIVE AROMATASE INHIBITORS Block the conversion of androstenedione to estrone. Eg: n n LETROZOLE, ANAST ROZOLE, FORMESTANE, EXAM ESTANE
SELECTIVE AROMATASE INHIBITORS o o 2 ND LINE IN POST MENOPAUSAL WOMEN FAILING TAMOXIFEN. EMERGING AS 1 ST LINE IN POST MENOPAUSAL WOMEN WITH ER POSITIVE BREAST CANCER.
OVARIAN ABLATION o PREMENOPAUSAL RECEPTOR POSITIVE WOMEN n SURGICAL n RADIOTHERAPY n LHRH AGONISTS

LHRH AGONISTS q q REMOVES ESTROGENIC STIMULATION IN PRE MENOPAUSAL WOMEN WITH FUNCTIONAL OVARIES. Eg: GOSERELIN, LE UPROLIDE.
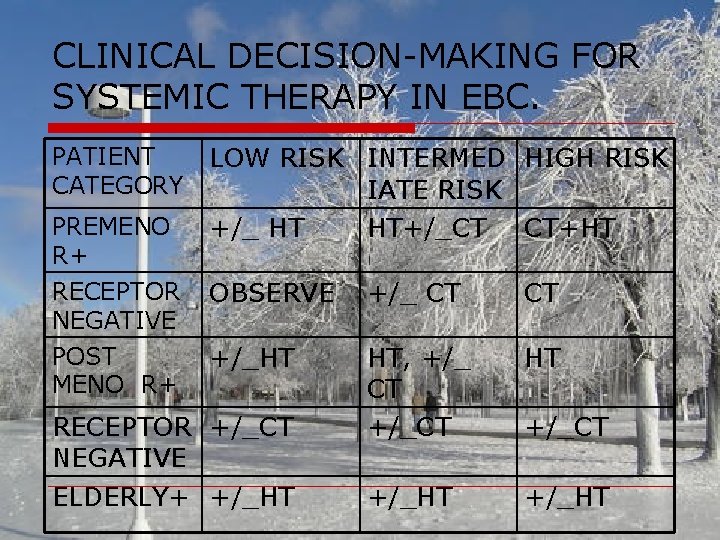
CLINICAL DECISION-MAKING FOR SYSTEMIC THERAPY IN EBC. PATIENT CATEGORY PREMENO R+ RECEPTOR NEGATIVE POST MENO R+ LOW RISK INTERMED HIGH RISK IATE RISK +/_ HT HT+/_CT CT+HT OBSERVE +/_ CT CT +/_HT HT, +/_ CT +/_CT HT +/_HT RECEPTOR +/_CT NEGATIVE ELDERLY+ +/_HT +/_CT
BREAST RECONSTRUCTION o o Surgical procedure that rebuilds the breast contour, and also the nippleareola complex. Aim is to achieve symmetry – ideally construct a symmetric breast, or adjust the contralateral breast by reduction or augmentation.
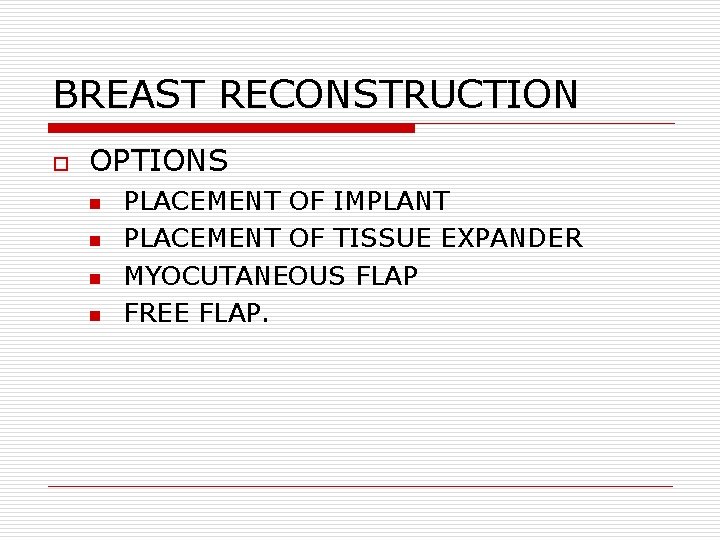
BREAST RECONSTRUCTION o OPTIONS n n PLACEMENT OF IMPLANT PLACEMENT OF TISSUE EXPANDER MYOCUTANEOUS FLAP FREE FLAP.
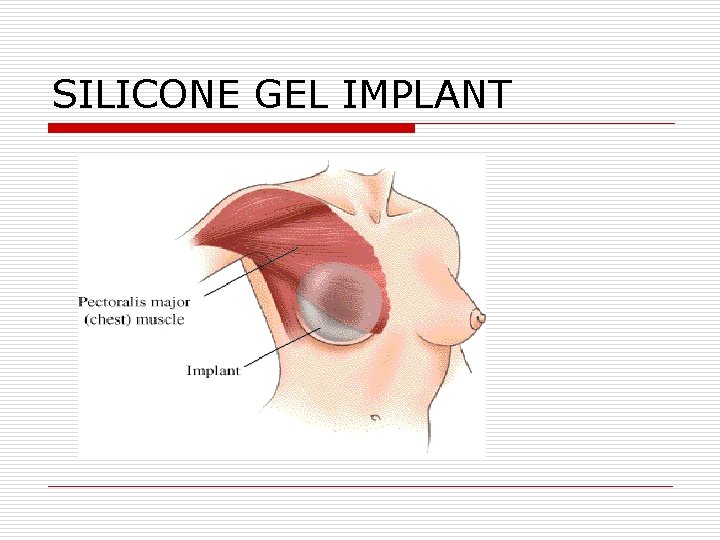
SILICONE GEL IMPLANT
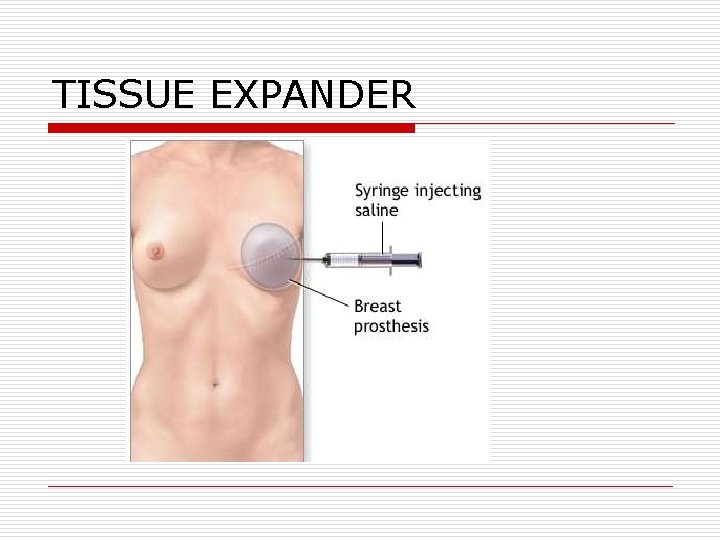
TISSUE EXPANDER
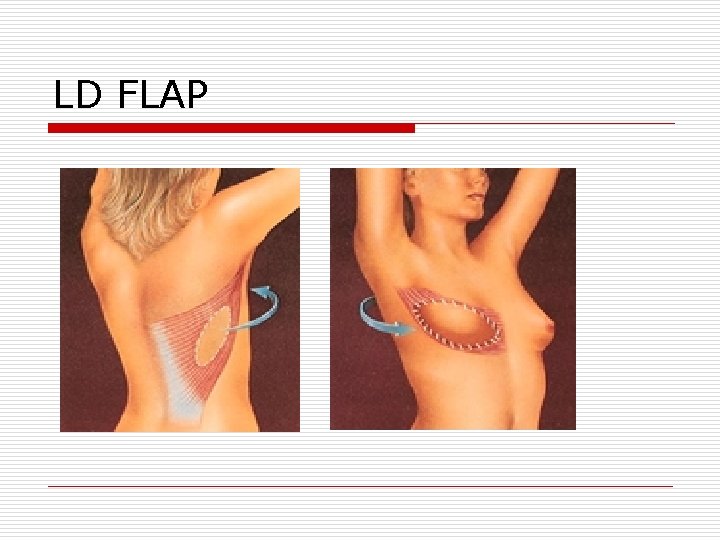
LD FLAP
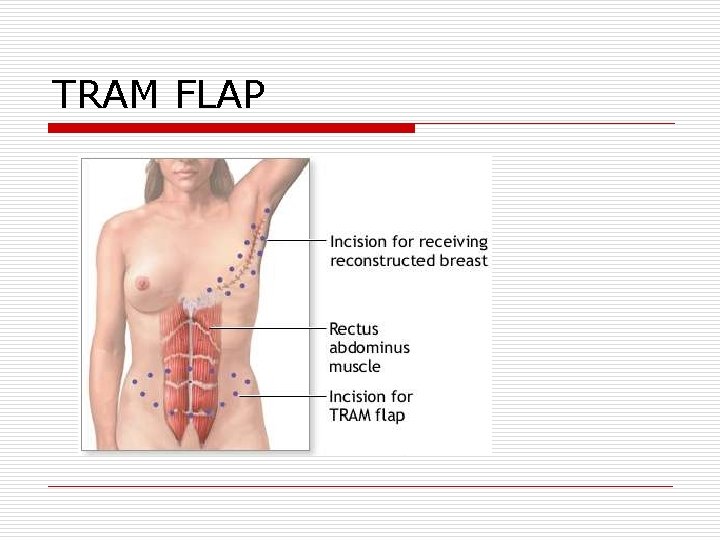
TRAM FLAP
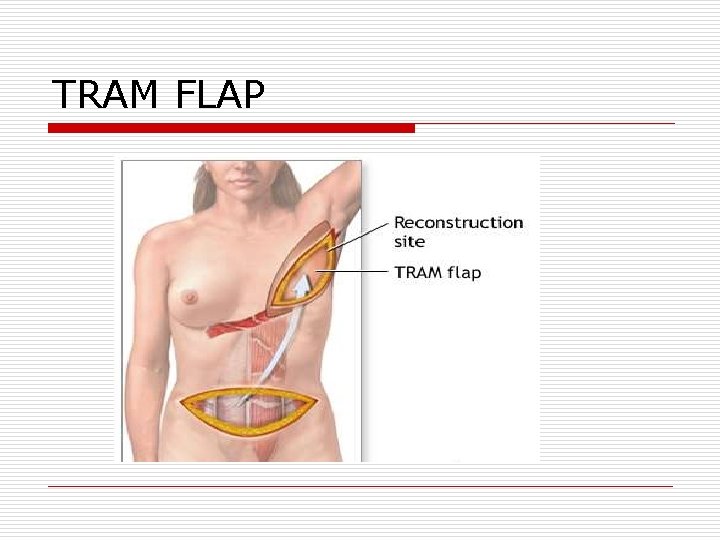
TRAM FLAP
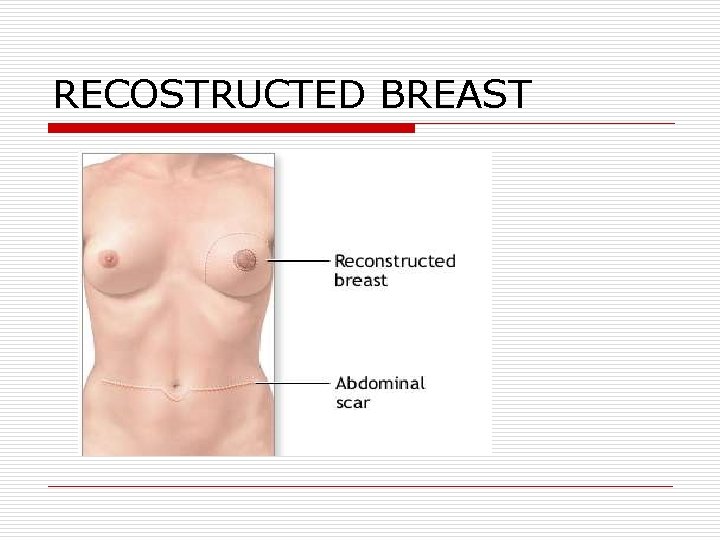
RECOSTRUCTED BREAST
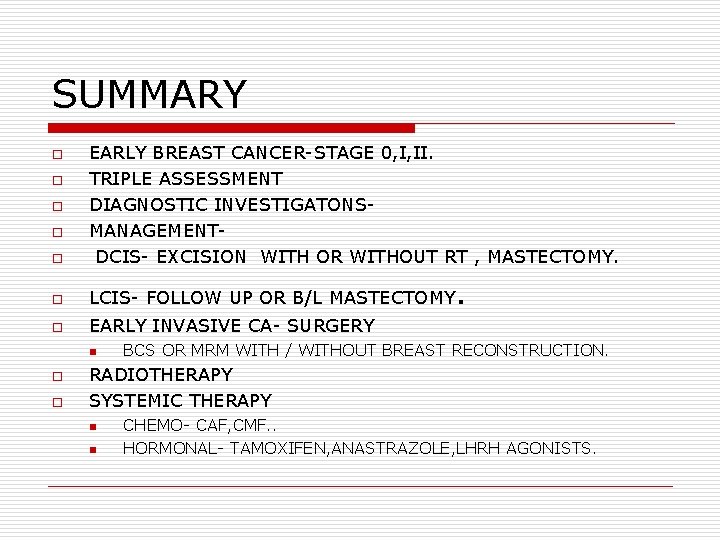
SUMMARY o EARLY BREAST CANCER-STAGE 0, I, II. TRIPLE ASSESSMENT DIAGNOSTIC INVESTIGATONSMANAGEMENTDCIS- EXCISION WITH OR WITHOUT RT , MASTECTOMY. o LCIS- FOLLOW UP OR B/L MASTECTOMY o EARLY INVASIVE CA- SURGERY o o n o o . BCS OR MRM WITH / WITHOUT BREAST RECONSTRUCTION. RADIOTHERAPY SYSTEMIC THERAPY n n CHEMO- CAF, CMF. . HORMONAL- TAMOXIFEN, ANASTRAZOLE, LHRH AGONISTS.

THANK YOU
- Slides: 71