Management of DM and its complications Complications are






- Slides: 65
Management of DM and its complications
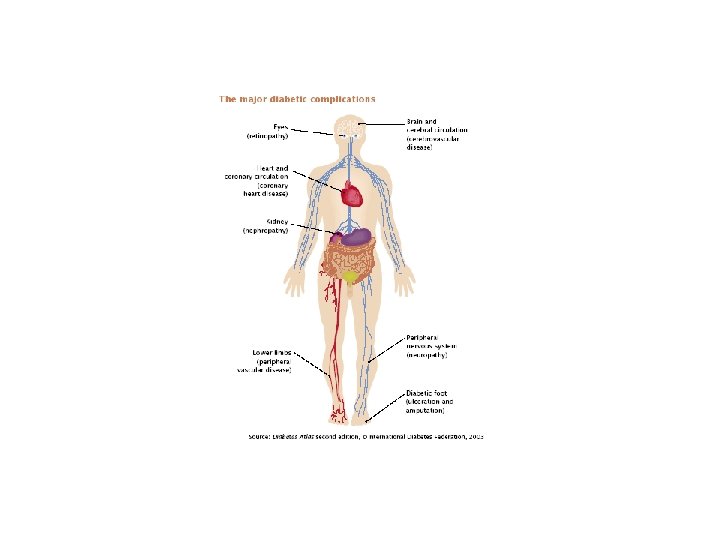
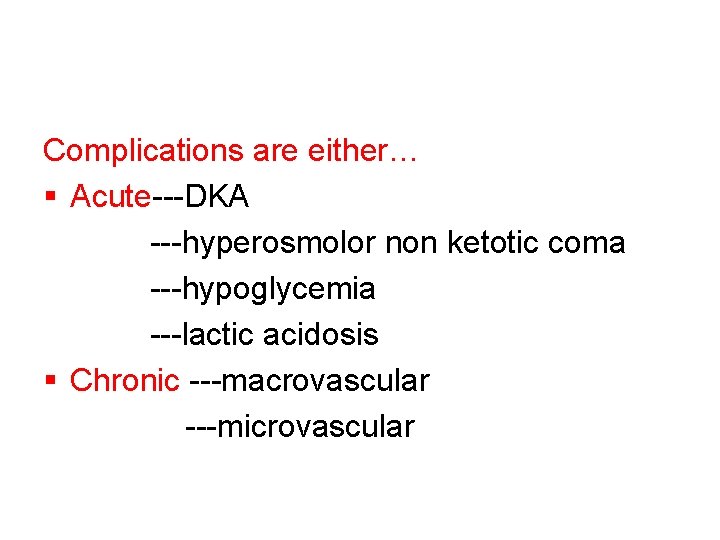
Complications are either… § Acute---DKA ---hyperosmolor non ketotic coma ---hypoglycemia ---lactic acidosis § Chronic ---macrovascular ---microvascular
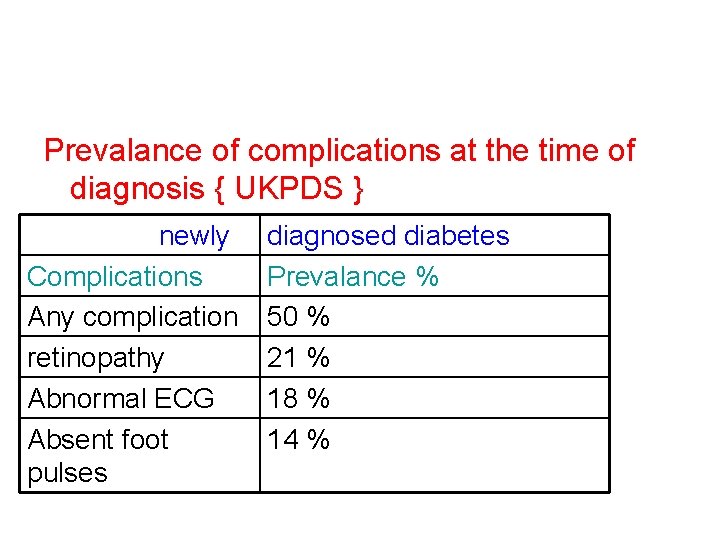
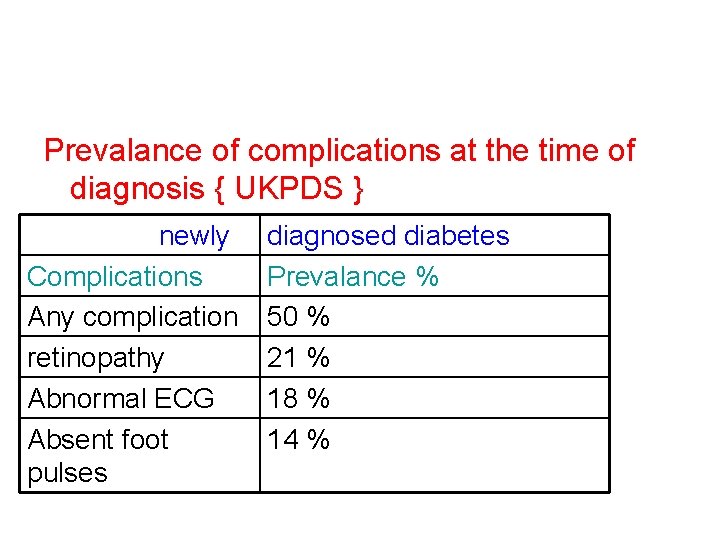
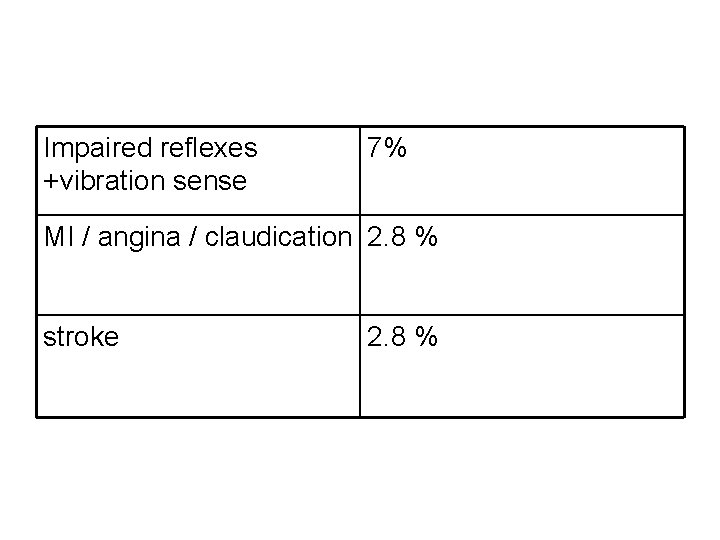
Prevalance of complications at the time of diagnosis { UKPDS } newly Complications Any complication retinopathy Abnormal ECG Absent foot pulses diagnosed diabetes Prevalance % 50 % 21 % 18 % 14 %
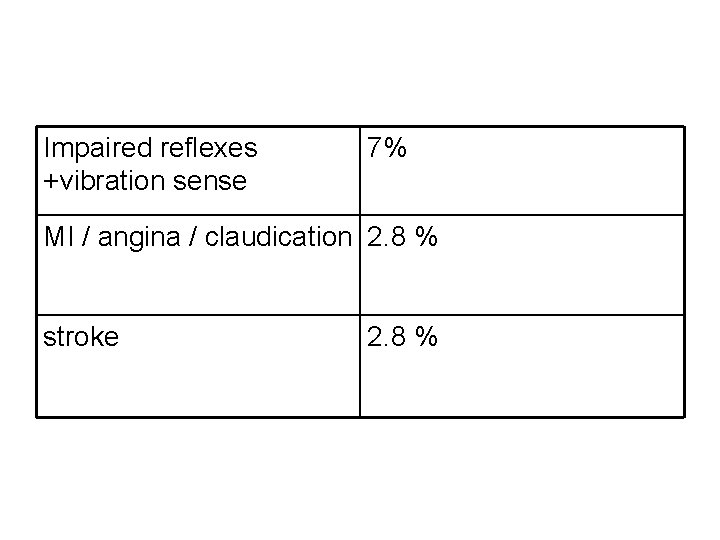
Impaired reflexes +vibration sense 7% MI / angina / claudication 2. 8 % stroke 2. 8 %
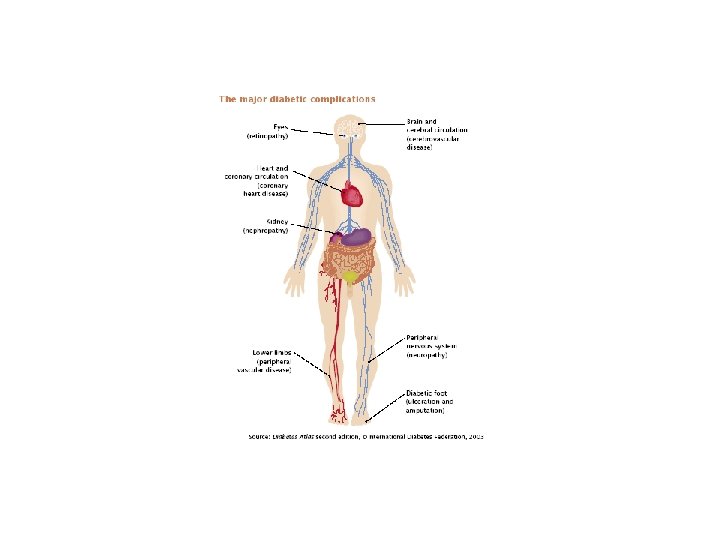
Chronic complications § Macrovascular § microvascular
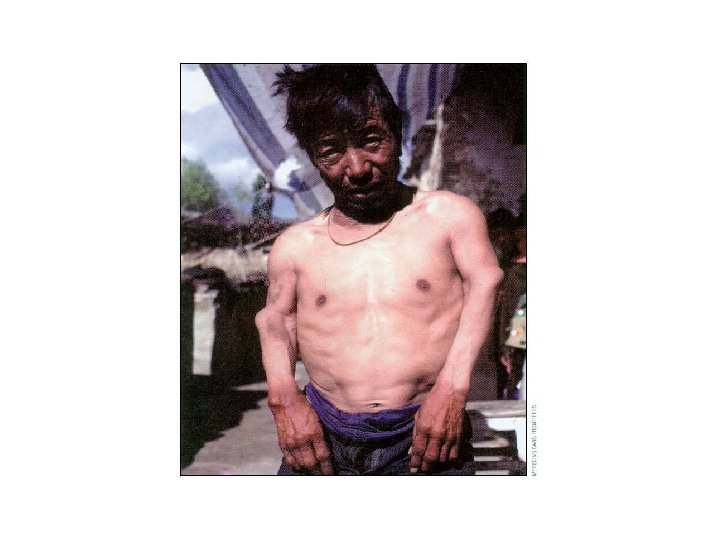
Macrovascular complication § 40 -50 % of people with DM die from these complications § Factors that contribute to the ↑ risk include 1 -↑ prevalance of hypertension in diabetics 2 --↑ lipid profile 3—abnoramlity in clotting system 4—effect of hyperglycemia on progression of atherosclerotic lesions
Macrovascular complications § § Stroke MI Peripheral vascular disease Foot problems
Microvascular complications § § Retinopathy Nephropathy Neuropathy Foot problems
Coronary artery disease § Coronary artery disease accounts for the majority of diabetic deaths § Certain features of CAD in diabetics include: Ø Adjusted for age MI is 2 -5 times more frequent in patients with diabetes Ø Pts with DM who have MI have a lower survival rate compared to pts without DM Ø ↑ incidence of silent MI – 40% Ø Silent MI may present as new onset of CCF Ø Small vessel disease with relatively patent coronary arteries are more common
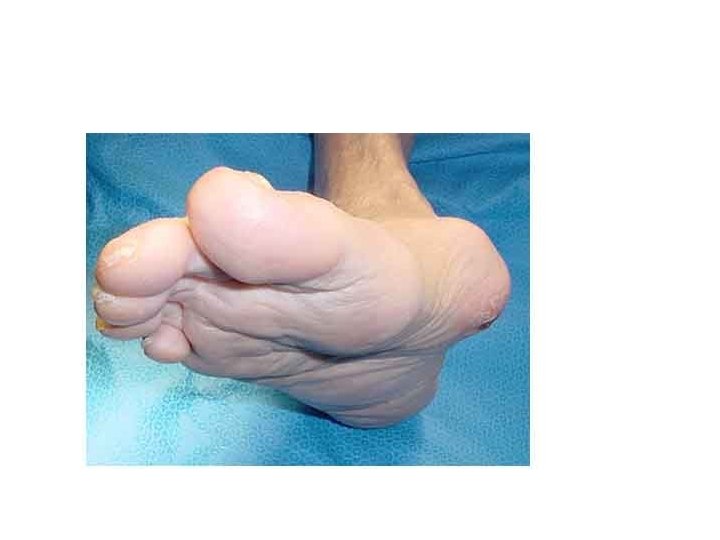
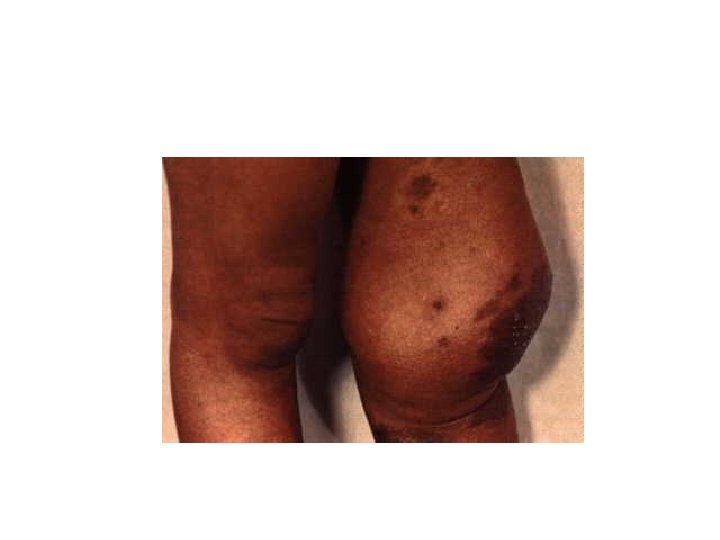
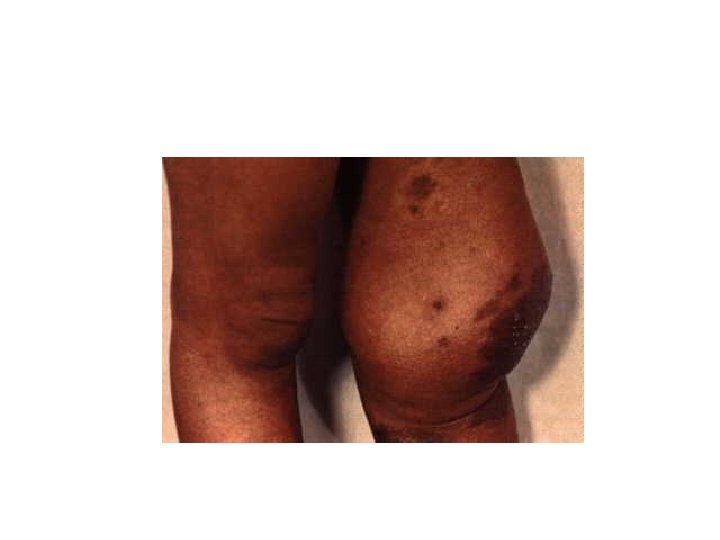
Peripheral vascular disease {PVD} Special characteristics of PVD Ø Location—tibial + popliteal arteries are common----aorta , ileal, femoral –rare Ø Extend—multi segmental occlusion Ø Progression—accelerated progression compared to non diabetics Ø Gangrene---risk ↑ more than non diabetics over 40 yrs of age
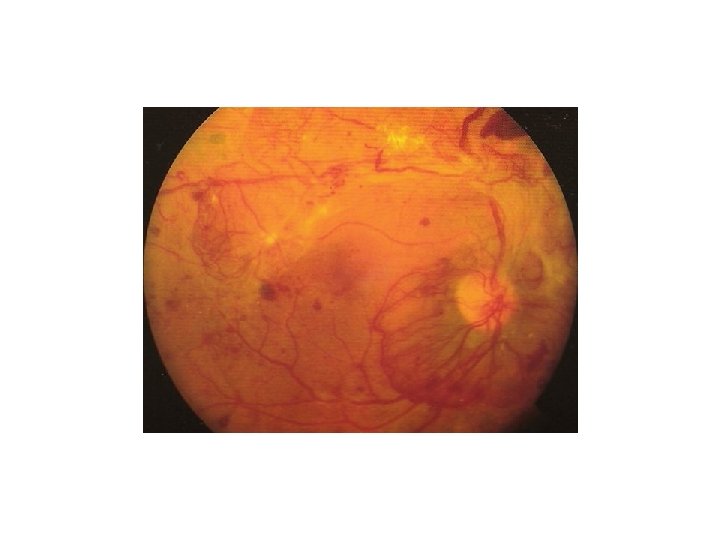
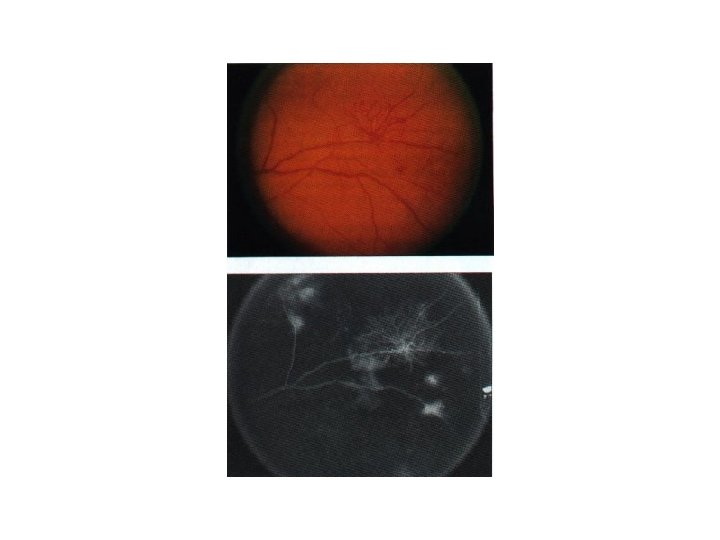
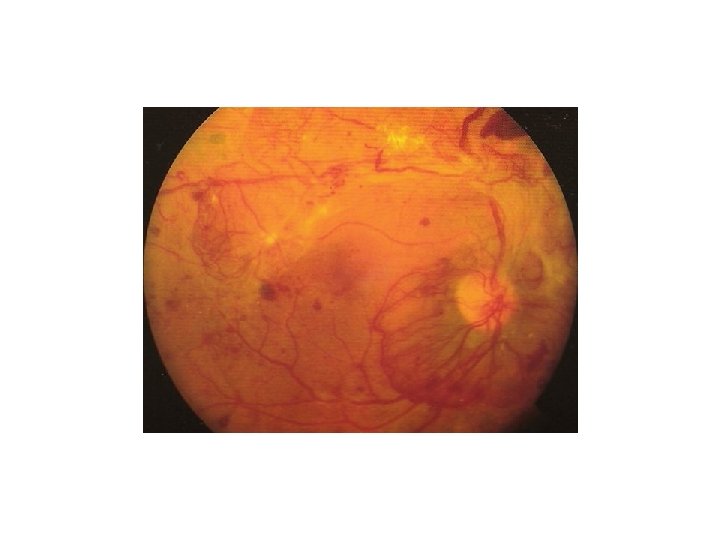
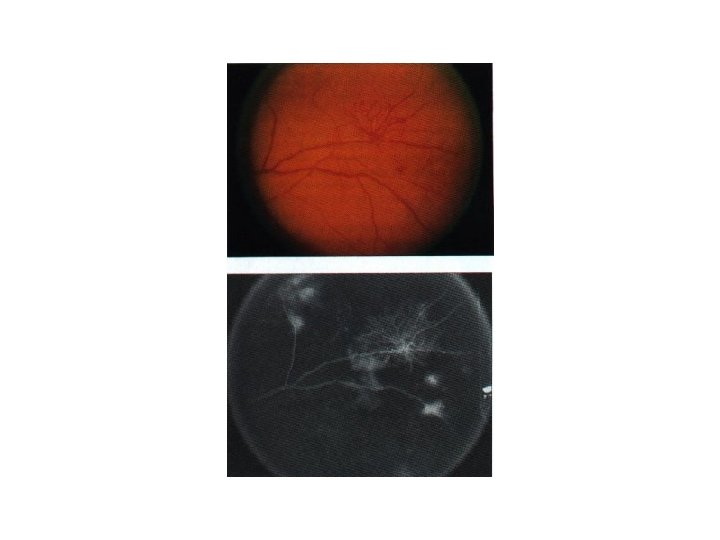
Retinopathy § Background—this is the most common type of retinopathy --not usually seen untill after 10 yrs of DM ---may be found in 30 % of pts with type 2 DM § Proliferative § maculopathy
Nephropathy Consists of the following clinical stages: Ø ↑ GFR > 150 mls /min Ø Microalbuminurea 30 -300 mg /24 hrs Ø Clinical albuminuria also called macroalbuminuria > 300 mg/ 24 hrs Ø Worsening of proteinuria , hypertension and ↓GFR Ø Kidney failure occurs when GFR ↓ to ≤ 10 mls/min
Factors influencing renal function in DM § Glomerular basement membrane damage → diabetic nephropathy § Renal artery stenosis and ischaemia due to atherosclerosis § Ascending infection § Renal papillary necrosis
Neuropathy Different clinical presentations § Symmetrical sensory polyneuropathy § Mononeuritis multilplex § Autonomic neuropathy
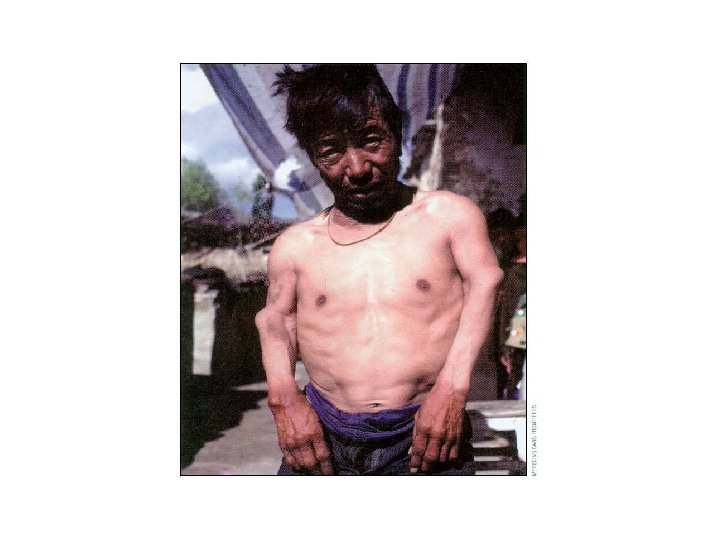
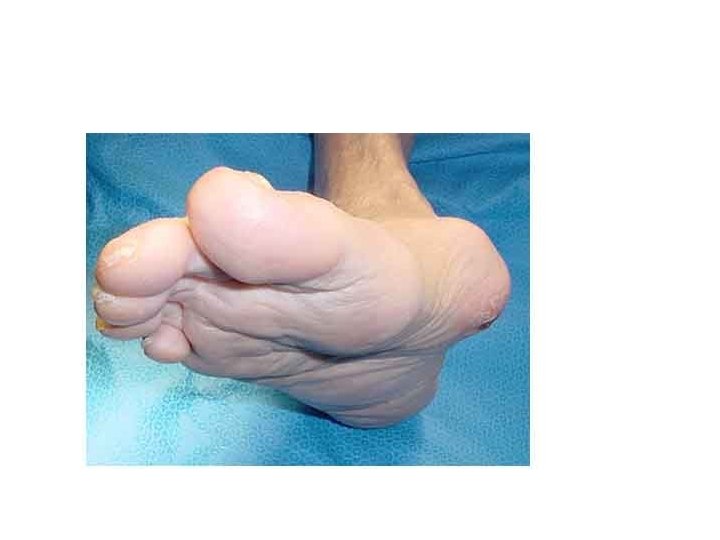
Sensory neuropathy § Insidious onset of loss of sensation in feet and hands—gloves and stockings § Loss of vibration sense and reduced or absent ankle or knee jerk § Loss of peripheral nerve function results in wasting of small muscles of feet and hands
Mononeuritis multiplex § Nerves commonly affected are 3 rd and 6 th § Amyotrophic motor neuropathy characterized by unilateral or bilateral pain and weakness of the quadriceps—they often recover spontanously § Median nerve palsy leeds to carpal tunnel syndrome § Peroneal nerve palsy leeds to foot drop
Autonomic neuropathy § CVS—loss of vagal { parasympathetic tone} produces --resting tachycardia --loss of sinus rhythm –change in heart rate with respiration ---sinus arrythmia § Loss of sympathetic activity in arterioles results in peripheral vasodilatation and postural hypotension Ø Rx—support stockings Ø --fludrocortisone Ø -alfa blockers
GIT § Gastroparesis--Delayed gastric emptying results in early statiety or recurrent vomiting v --treated with –dopamine agonist Ø metochlorpramide Ø domperidone Ø erythromycin § Nocturnal diarrhea Ø loperamide § Constipation due to colonic atony Ø laxatives
Autonomic bladder § Loss of bladder smooth muscle tone results in incomplete emptying , stasis , and ↑ risk of infection § In severe cases the bladder is persistantly distended—atonic which results in over flow incontinance Ø sympathomimetics—carbachol Ø antichilinesterase drugs
Gustatory sweating § Eating cause excessive facial sweating Ø Anticholinergic drugs--probantheline Erectile dysfunction § impotence
Foot disease § Neuropathic foot ulcer § Ischaemic foot ulcer § Charcots arthropathy
Can we prevent type 2 DM § Before pts develop DM , they almost always have “ pre diabetes” § Clinical trails have documented that dietary changes and regular exercise prevent or delay the development of overt DM in individuals at high risk
Risk factors for type 2 DM § Age > 45 § 1 st degree relative with type 2 DM § History of gestational diabetes or delivery of infant >9 lbs § PCO § Abdominal obesity § CVD, hypertension , dyslipidemia , other metabolic syndrome features
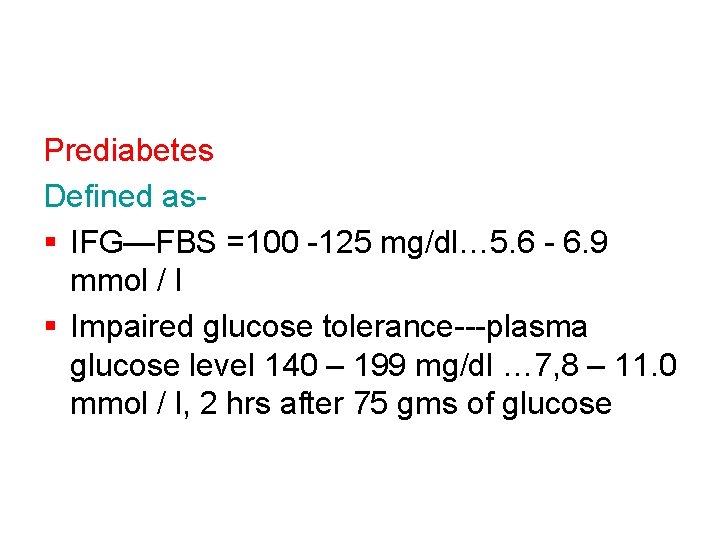
Prediabetes Defined as§ IFG—FBS =100 -125 mg/dl… 5. 6 - 6. 9 mmol / l § Impaired glucose tolerance---plasma glucose level 140 – 199 mg/dl … 7, 8 – 11. 0 mmol / l, 2 hrs after 75 gms of glucose
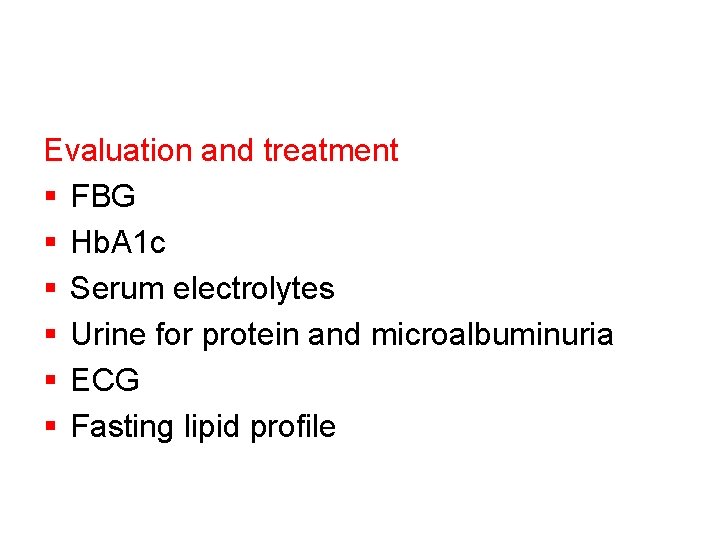
Evaluation and treatment § FBG § Hb. A 1 c § Serum electrolytes § Urine for protein and microalbuminuria § ECG § Fasting lipid profile
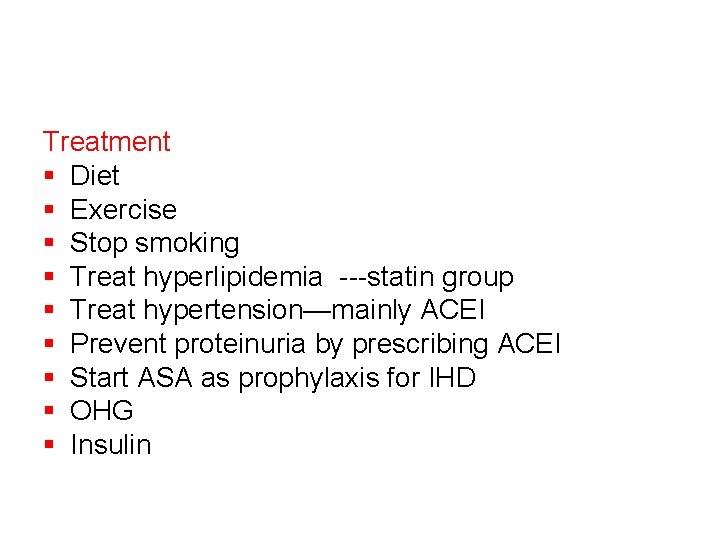
Treatment § Diet § Exercise § Stop smoking § Treat hyperlipidemia ---statin group § Treat hypertension—mainly ACEI § Prevent proteinuria by prescribing ACEI § Start ASA as prophylaxis for IHD § OHG § Insulin
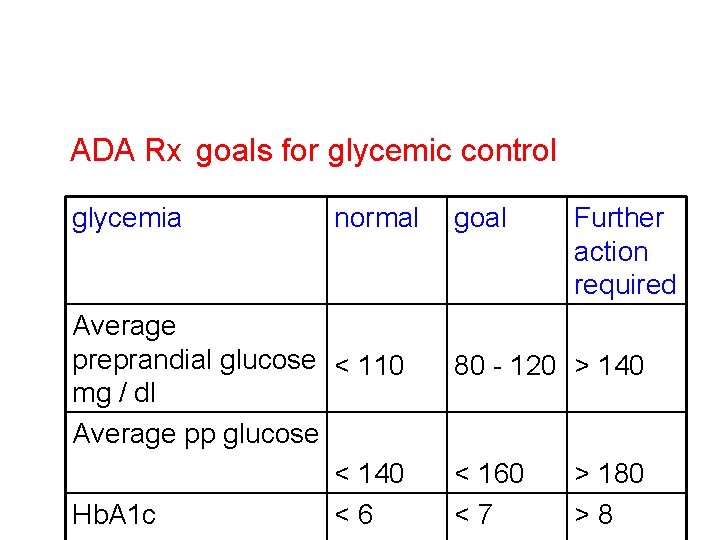
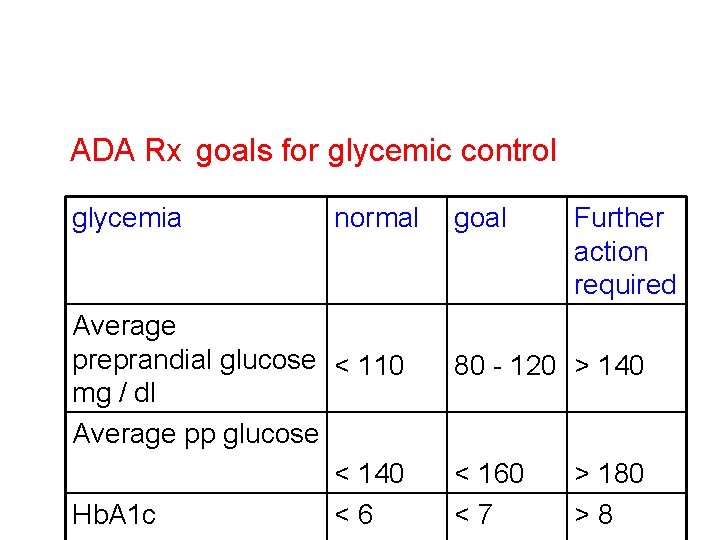
ADA Rx goals for glycemic control glycemia normal Average preprandial glucose < 110 mg / dl Average pp glucose < 140 Hb. A 1 c <6 goal Further action required 80 - 120 > 140 < 160 <7 > 180 >8
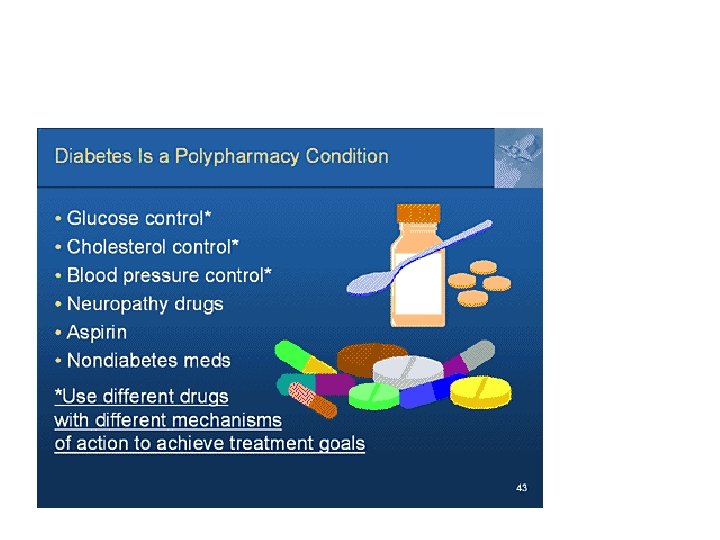
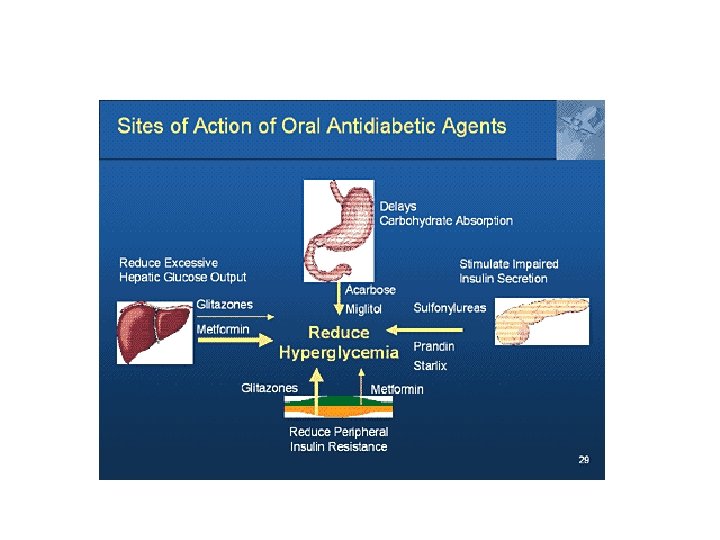
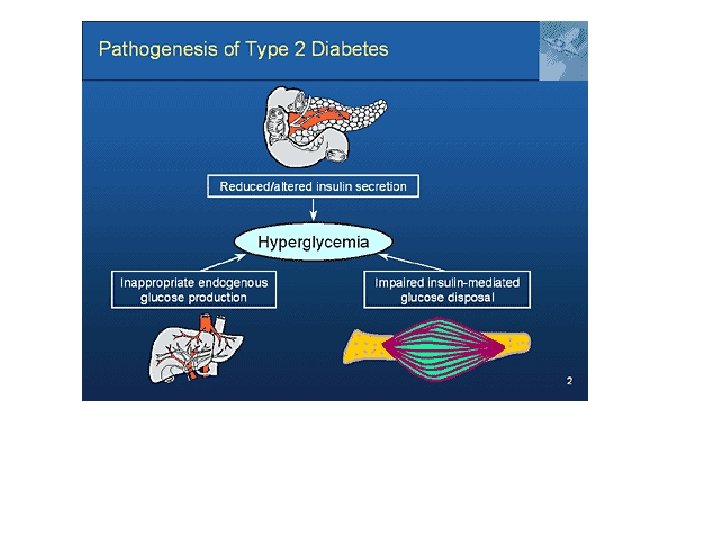
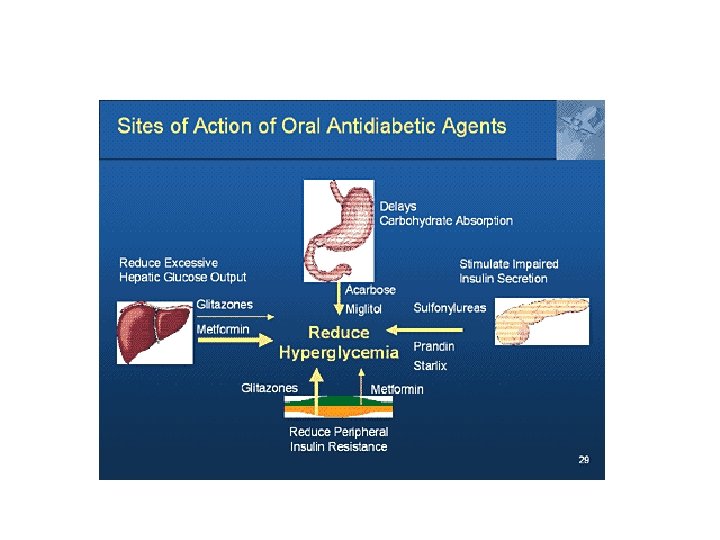
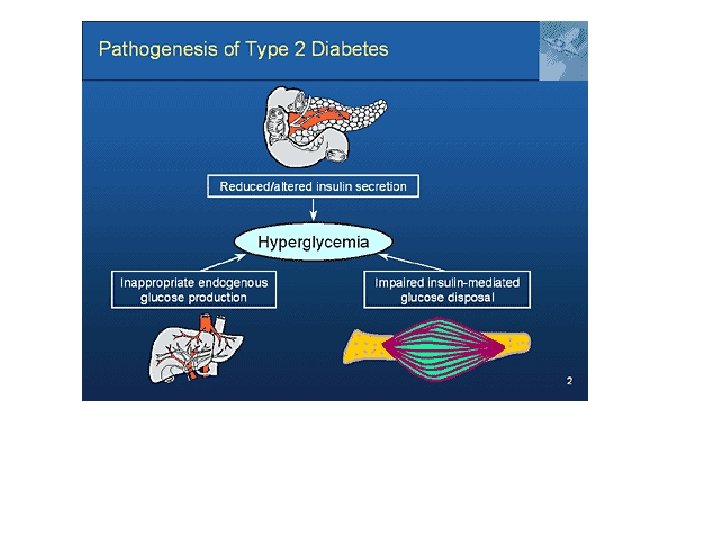
OHG v Biguanides— Ø Suppress hepatic glucose production Ø Decrease intestinal glucose absorption Ø Improve insulin sensitivity § metformin v Sulphonylurea Ø Increase pancreatic insulin secretion § —glimepiride § ---glipizide § ---glyburide § ---chlorpropamide
Thiazolidinediones— Ø↓ post prandial hyperglycemia §---Rosiglitazone §---poglitazone
Cont. . v Alfa glucosidase inhibitors— Ø ↓post prandial hyperglycemia by decreasing GIT carbohydrate absorption § arcabose v Meglitinides--Ø Increase pancreatic insulin secretion through different glucose binding sites than used by sulphonylureas § repaglinide
v. Type 2 diabetes is a progressive disease v. Over time most pts will need insulin to control glucose
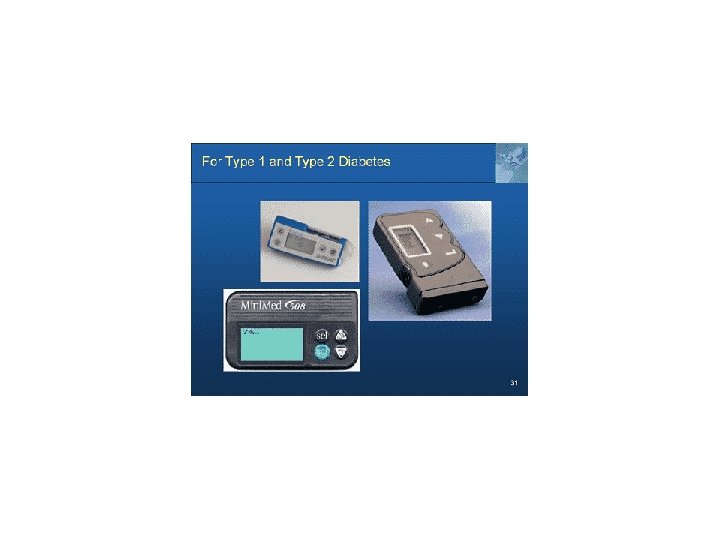
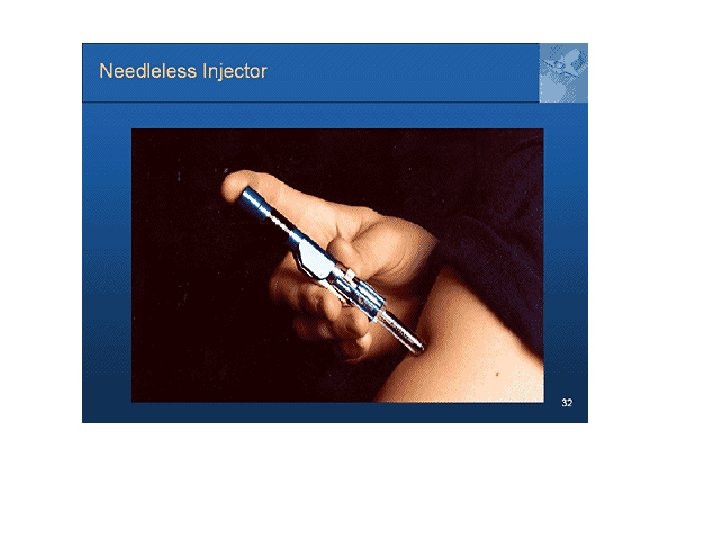
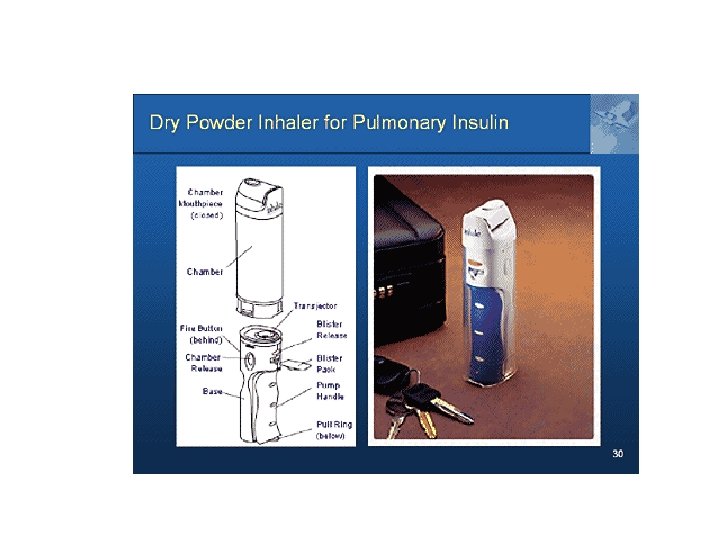
Insulin therapy in type 2 diabetes § Don, t wait forever § Don, t be afraid of hypoglycemia § Consider combination therapy § Don, t under insulinize § Consider insulin pump therapy

DIABETIC KETOACIDOSIS Leading cause of death in pts with type 1 diabetes under the age of 20 yrs
Risk factors for DKA § Results from absolute or relative insulin deffeciency § Missing the dose of insulin § Infection § Increase food intake § Stress like MI or surgery
Diagnosis Triad of. § Hyperglycemia—glucose more than 15 mmol /l § Metabolic acidosis—PH < 7. 2 ---HCO 3 <17 mmol /l § Ketones in the urine
Principles of management § Rehydration § Insulin § Correction of K+ § Correction of acidosis § + / - antibiotics
Rehydration § 1 litre NS over 30 min § 1 litre over 1 hr § 1 litre over 2 hrs § 1 litre over 4 hrs § I litre over 6 hrs Change ½ saline once BS reaches 13 mmol / l
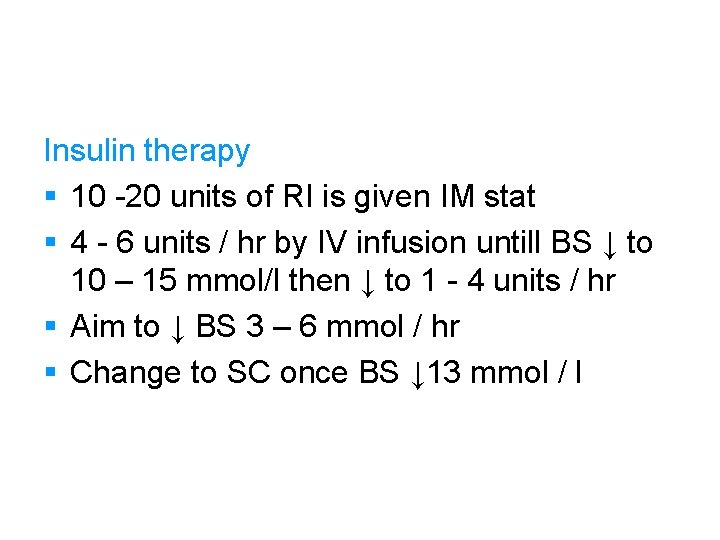
Insulin therapy § 10 -20 units of RI is given IM stat § 4 - 6 units / hr by IV infusion untill BS ↓ to 10 – 15 mmol/l then ↓ to 1 - 4 units / hr § Aim to ↓ BS 3 – 6 mmol / hr § Change to SC once BS ↓ 13 mmol / l
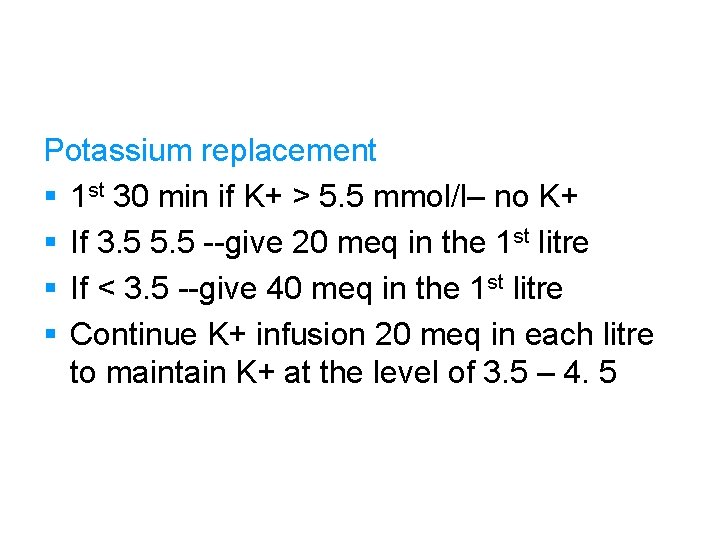
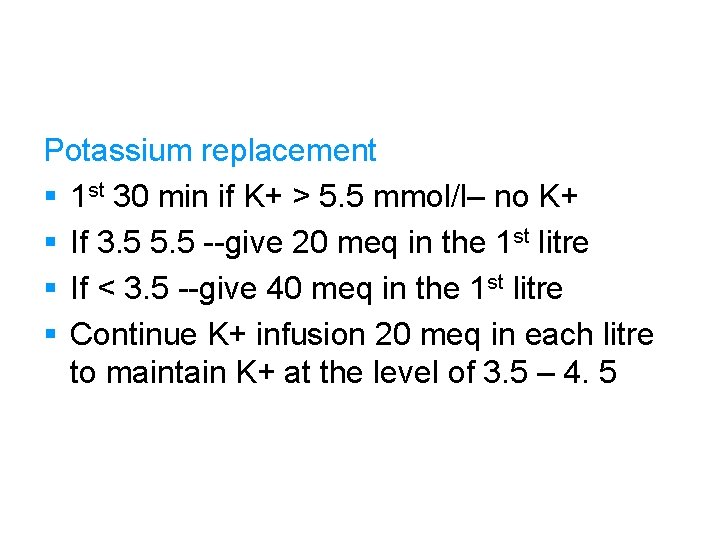
Potassium replacement § 1 st 30 min if K+ > 5. 5 mmol/l– no K+ § If 3. 5 5. 5 --give 20 meq in the 1 st litre § If < 3. 5 --give 40 meq in the 1 st litre § Continue K+ infusion 20 meq in each litre to maintain K+ at the level of 3. 5 – 4. 5
Bicarbonte replacement Bicarbonate is replaced when the PH is between 7. 0 – 7. 1 Antibiotics These are used when there is strong suspicion of infection
HYPOGLYCEMIA Causes § Missed delayed or inadequate meal § Unaccustomed exercise § Alcohol § Increase dose of drugs. . insulin or OHG § Gastroparesis § Malabsorption § factitious
NON KETOTIC HYPEROSMOLAR DIABETIC COMA Characterized by § Severe hyperglycemia--> 50 mmol / l § No ketones in the urine § Severe dehydration § Occurs in the elderly § Risk of thrombosis is high § Mortality is high
Management Differs from DKA in the following § Very sensitive to insulin so very small dose should be started § Calculate osmolality and start either ½ or ¼ saline Plasma osmolality =2 Na + 2 K + glu + urea=280 - 295
Cont. . § Prophylactic SC heparin § Fluid replacement should be adjusted according to CVP