Management of Cervical Spine Disease in Downs Syndrome













- Slides: 70
Management of Cervical Spine Disease in Down's Syndrome: A Neurosurgical perspective Dominic Thompson Department of Paediatric Neurosurgery Great Ormond Street London
Flemish (1515) Anon Am J Med Genetics
Cervical spinal pathology in Downs syndrome -The controversies • • Aetiology Diagnosis Screening Treatment
Aetiology
Aetiology • Primary features • Ligamentous laxity • Hypotonia • Hypermobility
Aetiology • Primary features • Skeletal consequences • Ligamentous laxity • Hypotonia • Hypermobility • • Craniovertebral instability Scoliosis Hip instability Patellar instability
Cervical spinal pathology in Downs syndrome • • Occipito-atlantal subluxation Atlantoaxial subluxation Os Odontoideum Incomplete C 1 ring Cervical stenosis Segmentation anomaly Premature cervical spondylarthrotic myelopathy
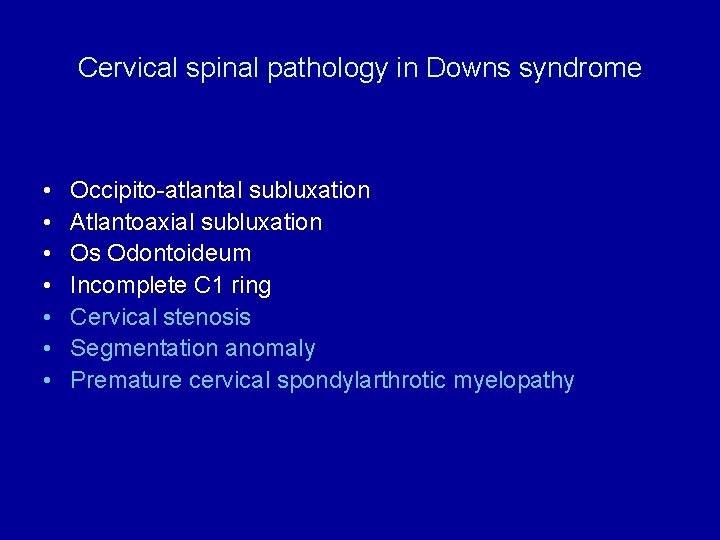
Cervical spinal pathology in Downs syndrome • • Occipito-atlantal subluxation Atlantoaxial subluxation Os Odontoideum Incomplete C 1 ring Cervical stenosis Segmentation anomaly Premature cervical spondylarthrotic myelopathy
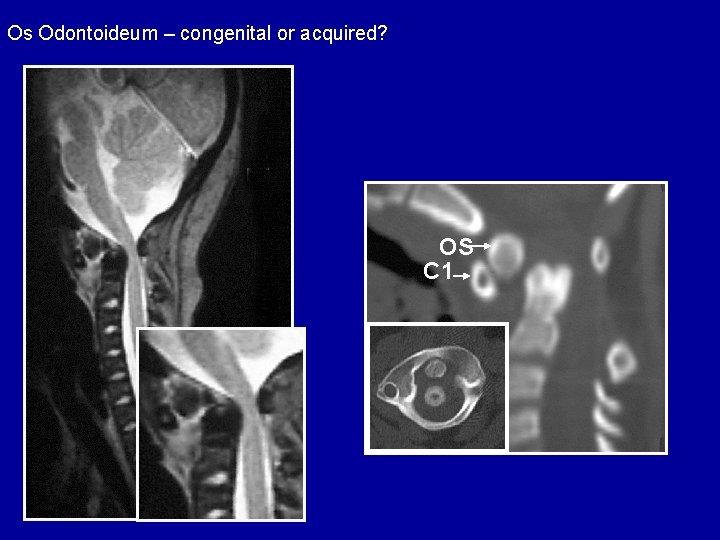
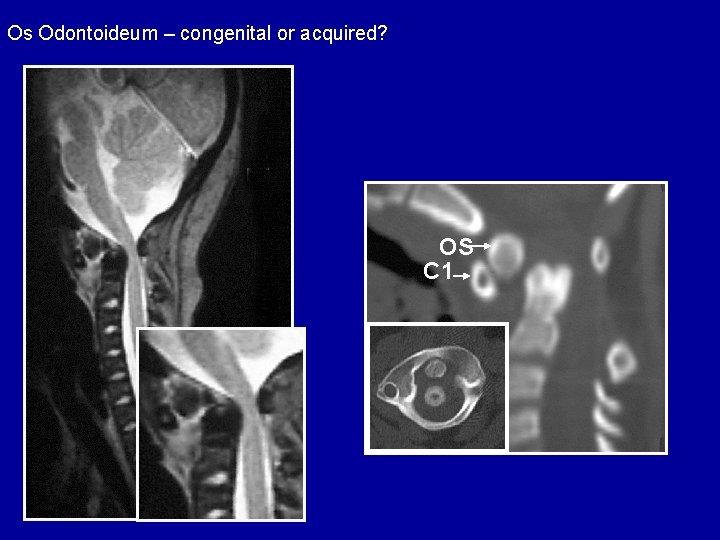
Os Odontoideum – congenital or acquired? OS C 1

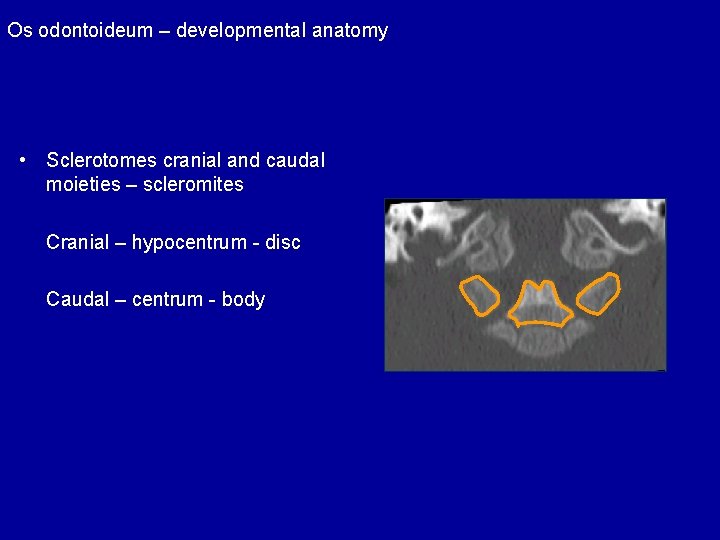
Os odontoideum – developmental anatomy • Sclerotomes cranial and caudal moieties – scleromites Cranial – hypocentrum - disc Caudal – centrum - body
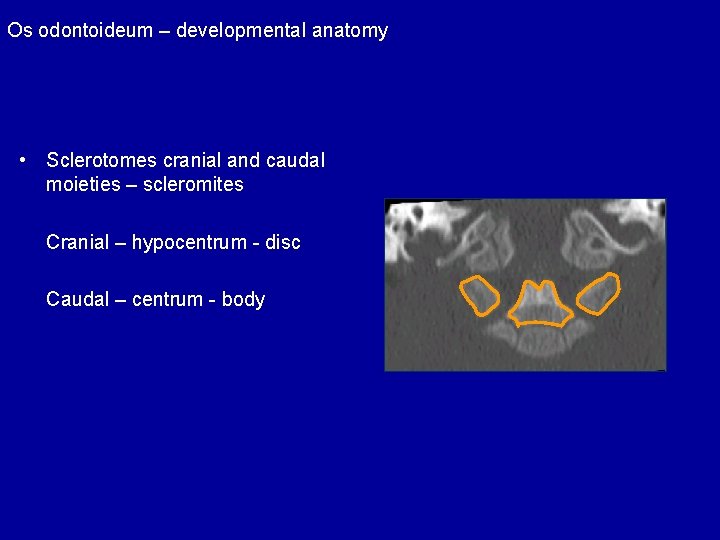
Os odontoideum – developmental anatomy • Sclerotomes cranial and caudal moieties – scleromites Cranial – hypocentrum - disc Caudal – centrum - body
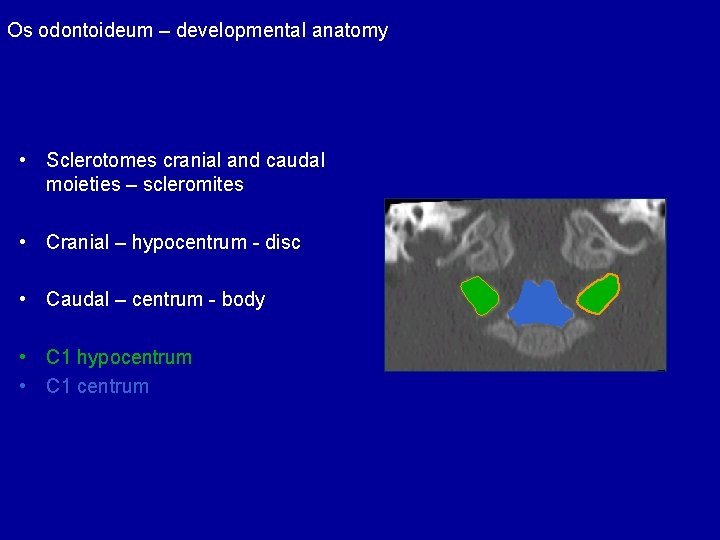
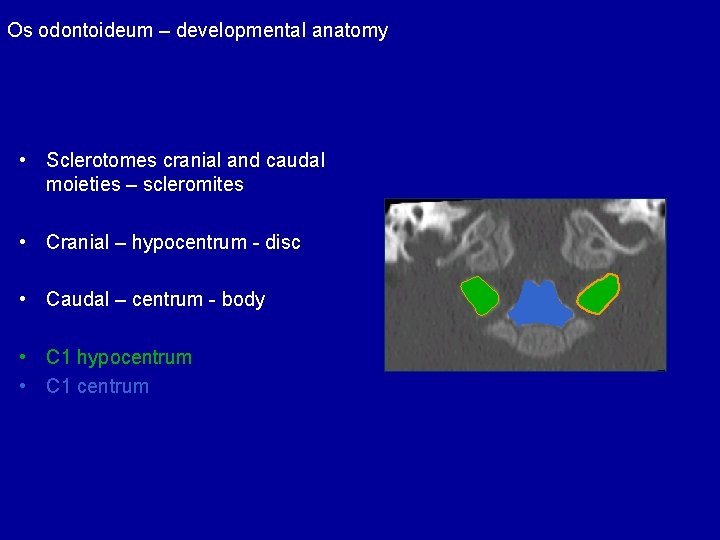
Os odontoideum – developmental anatomy • Sclerotomes cranial and caudal moieties – scleromites • Cranial – hypocentrum - disc • Caudal – centrum - body • C 1 hypocentrum • C 1 centrum
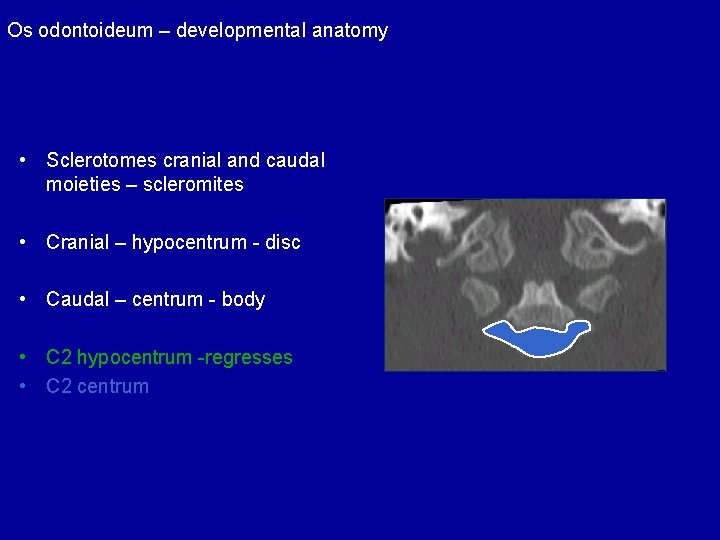
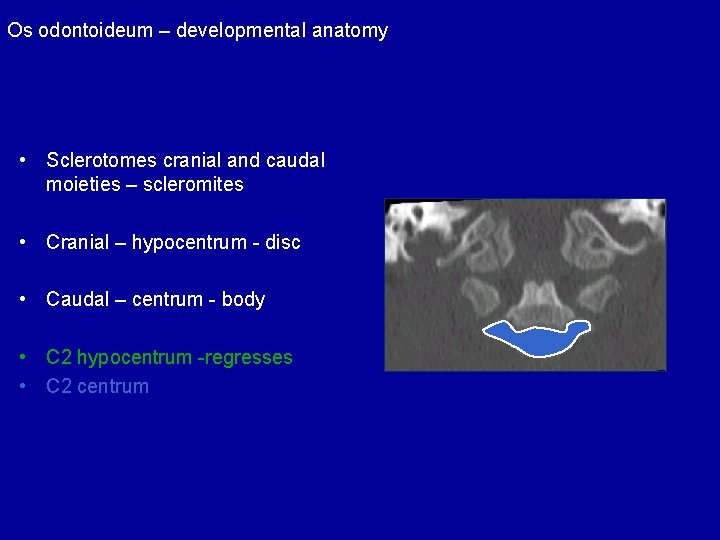
Os odontoideum – developmental anatomy • Sclerotomes cranial and caudal moieties – scleromites • Cranial – hypocentrum - disc • Caudal – centrum - body • C 2 hypocentrum -regresses • C 2 centrum
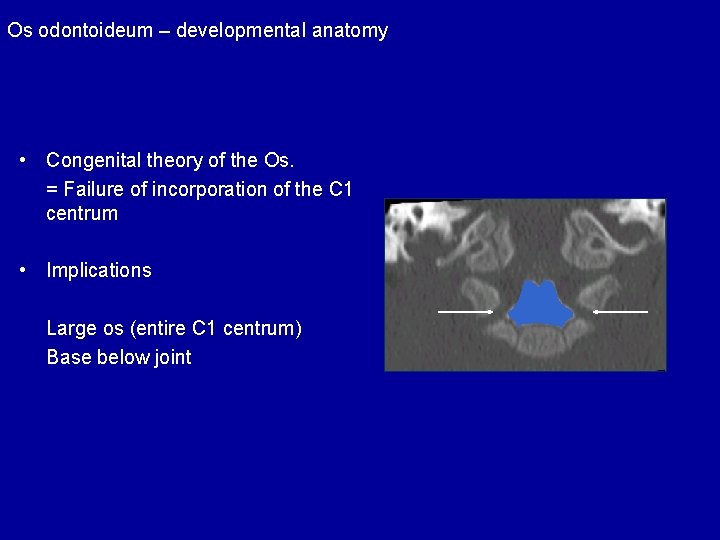
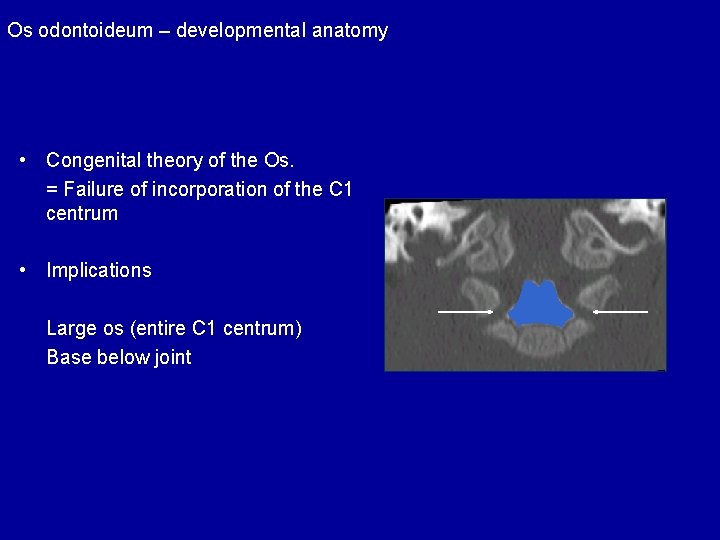
Os odontoideum – developmental anatomy • Congenital theory of the Os. = Failure of incorporation of the C 1 centrum • Implications Large os (entire C 1 centrum) Base below joint
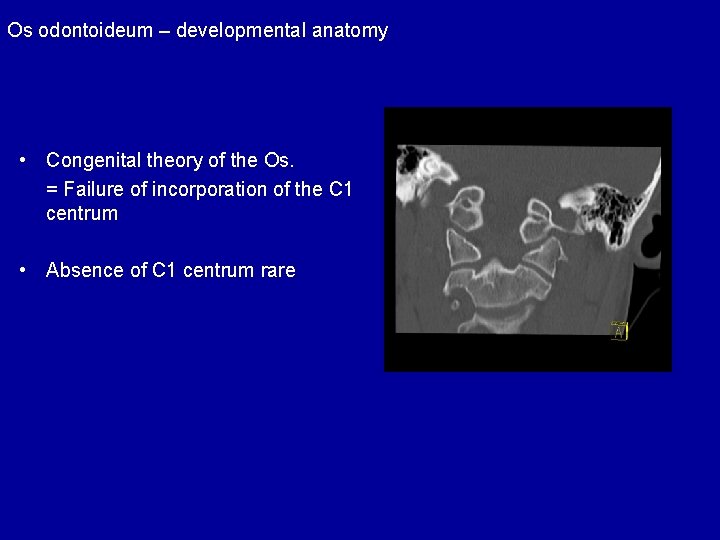
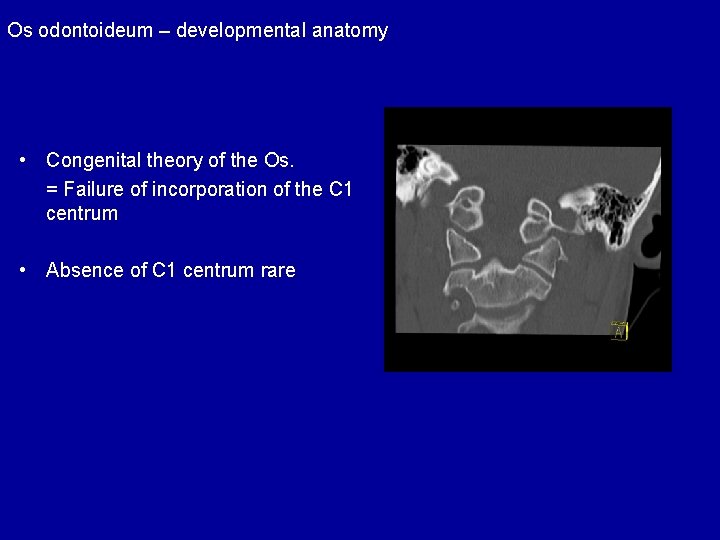
Os odontoideum – developmental anatomy • Congenital theory of the Os. = Failure of incorporation of the C 1 centrum • Absence of C 1 centrum rare
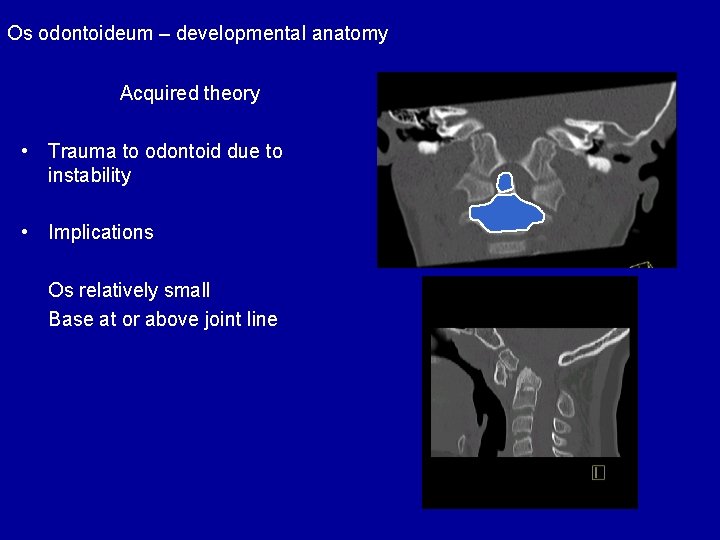
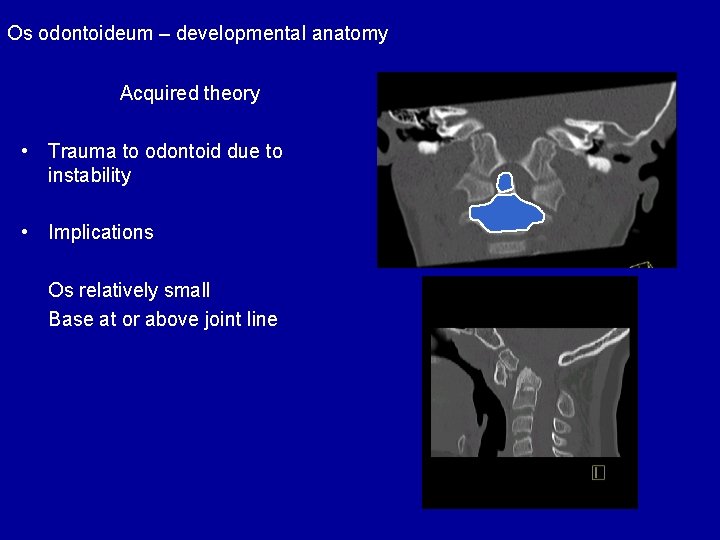
Os odontoideum – developmental anatomy Acquired theory • Trauma to odontoid due to instability • Implications Os relatively small Base at or above joint line
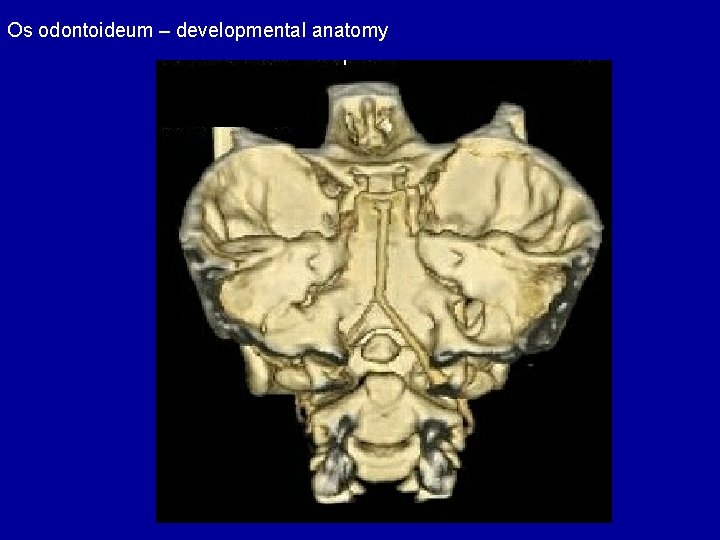
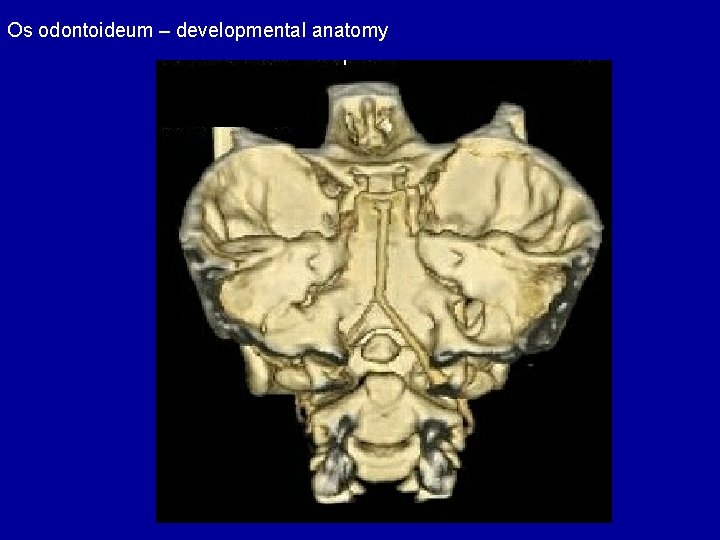
Os odontoideum – developmental anatomy
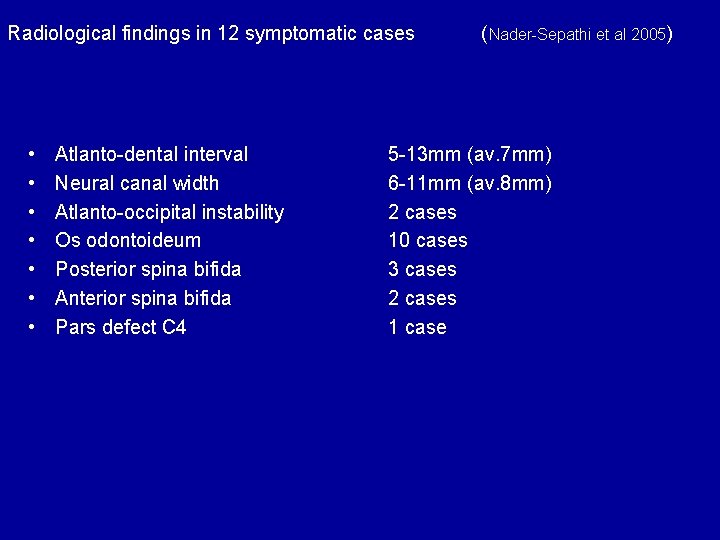
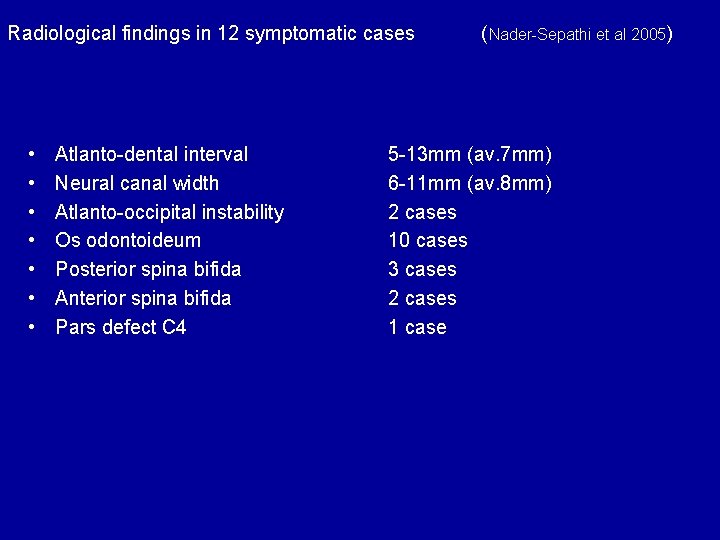
Radiological findings in 12 symptomatic cases • • Atlanto-dental interval Neural canal width Atlanto-occipital instability Os odontoideum Posterior spina bifida Anterior spina bifida Pars defect C 4 (Nader-Sepathi et al 2005) 5 -13 mm (av. 7 mm) 6 -11 mm (av. 8 mm) 2 cases 10 cases 3 cases 2 cases 1 case

Radiological findings in 12 symptomatic cases • • Atlanto-dental interval Neural canal width Atlanto-occipital instability Os odontoideum Posterior spina bifida Anterior spina bifida Pars defect C 4 (Nader-Sepathi et al 2005) 5 -13 mm (av. 7 mm) 6 -11 mm (av. 8 mm) 2 cases 10 cases 3 cases 2 cases 1 case

Radiological findings in 12 symptomatic cases • • Atlanto-dental interval Neural canal width Atlanto-occipital instability Os odontoideum Posterior spina bifida Anterior spina bifida Pars defect C 4 (Nader-Sepathi et al 2005) 5 -13 mm (av. 7 mm) 6 -11 mm (av. 8 mm) 2 cases 10 cases 3 cases 2 cases 1 case
Craniovertebral instability Os Odontoideum Delayed Atlantal ossification
Diagnosis
Diagnosis of craniovertebral instability in Downs Syndrome Aims • To identify children with or at risk of spinal cord damage due to craniovertebral instability • To instigate effective treatment

What to measure?

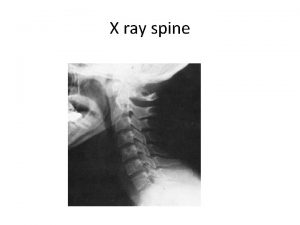
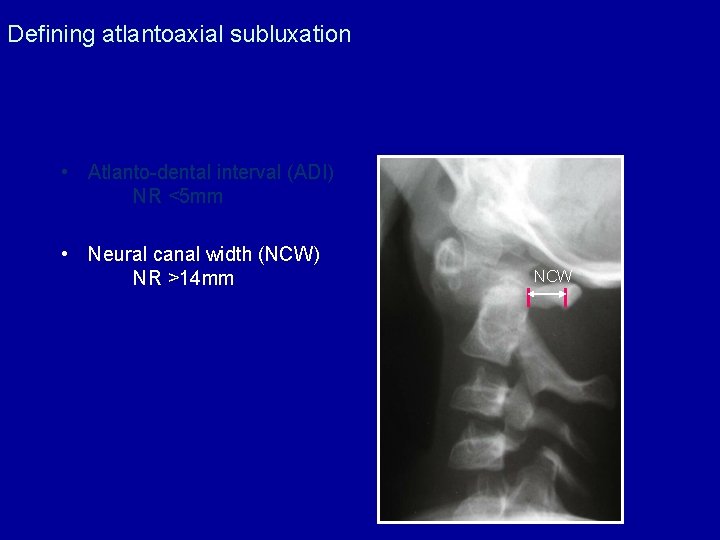
Defining atlantoaxial subluxation • Atlanto-dental interval (ADI) NR <5 mm • Neural canal width (NCW) NR >14 mm ADI
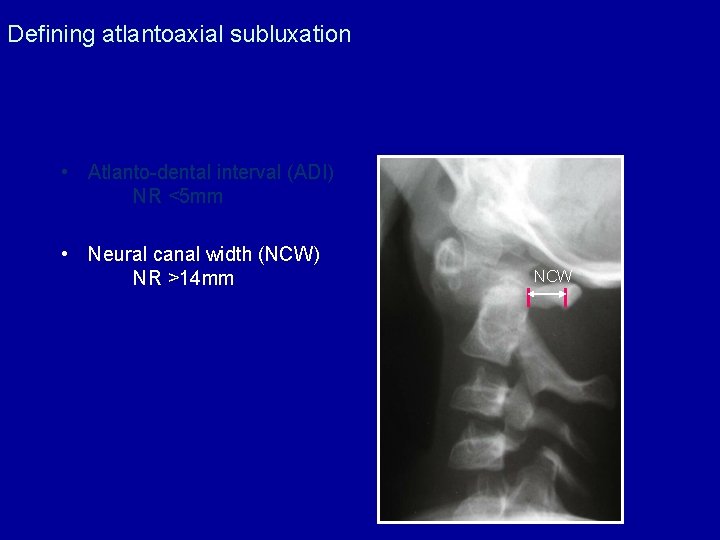
Defining atlantoaxial subluxation • Atlanto-dental interval (ADI) NR <5 mm • Neural canal width (NCW) NR >14 mm NCW
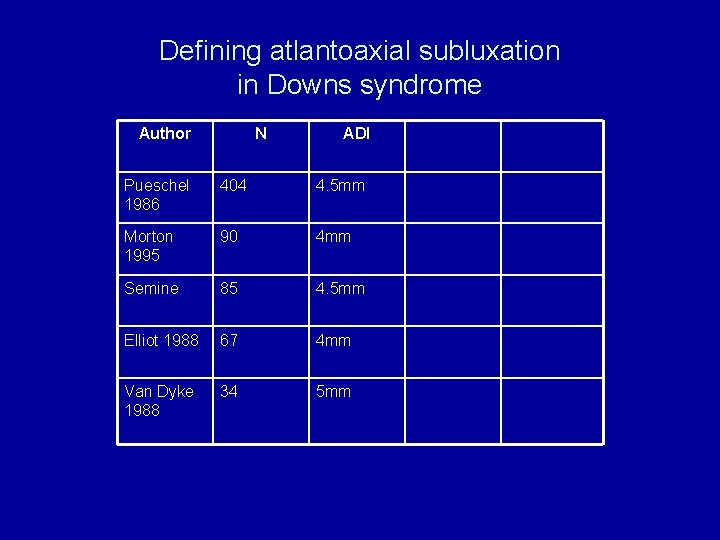
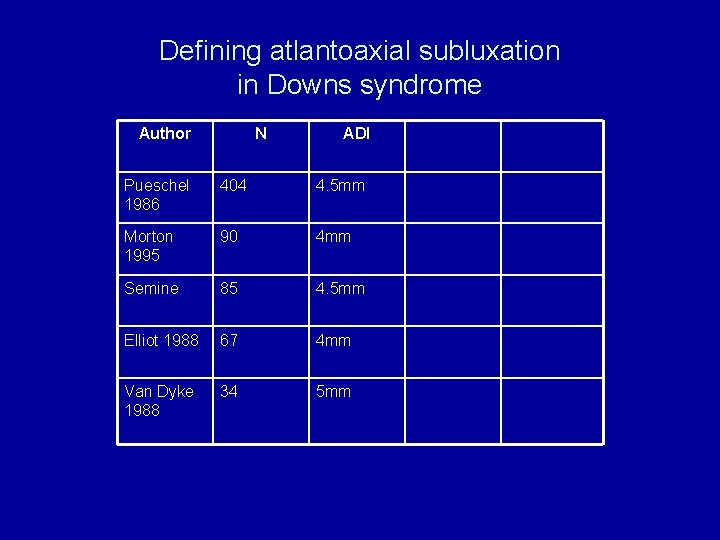
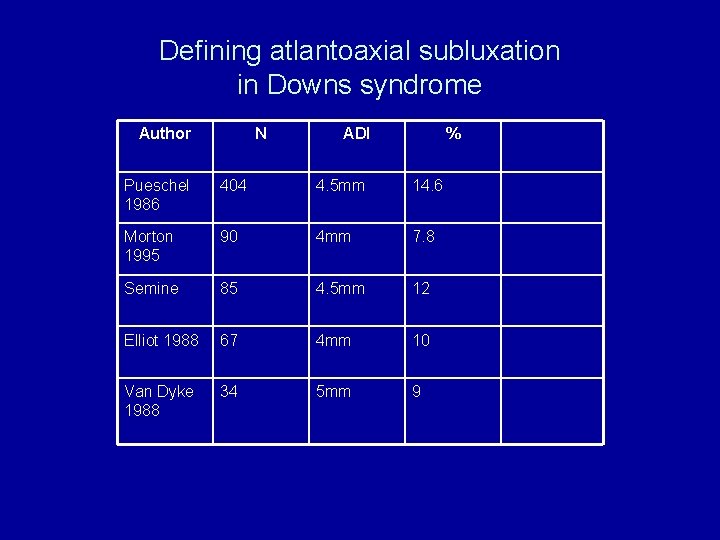
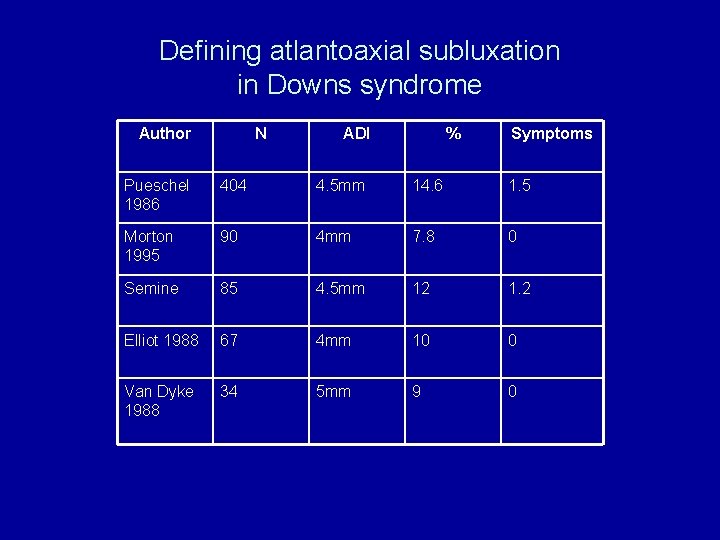
Defining atlantoaxial subluxation in Downs syndrome Author N ADI Pueschel 1986 404 4. 5 mm Morton 1995 90 4 mm Semine 85 4. 5 mm Elliot 1988 67 4 mm Van Dyke 1988 34 5 mm
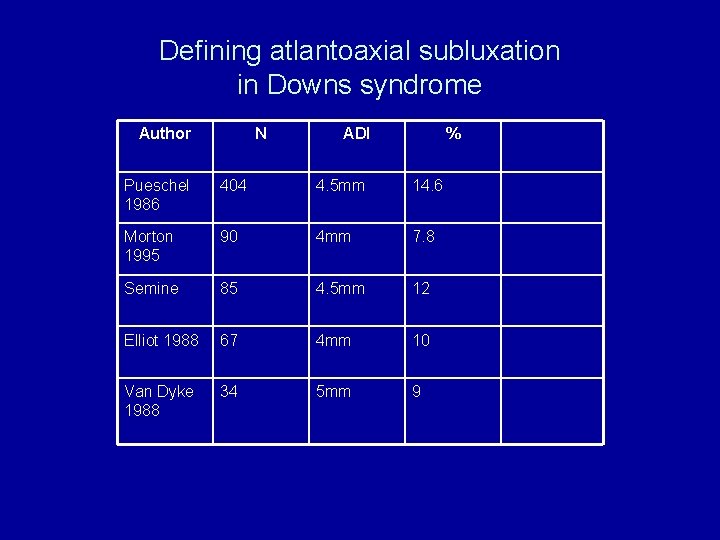
Defining atlantoaxial subluxation in Downs syndrome Author N ADI % Pueschel 1986 404 4. 5 mm 14. 6 Morton 1995 90 4 mm 7. 8 Semine 85 4. 5 mm 12 Elliot 1988 67 4 mm 10 Van Dyke 1988 34 5 mm 9
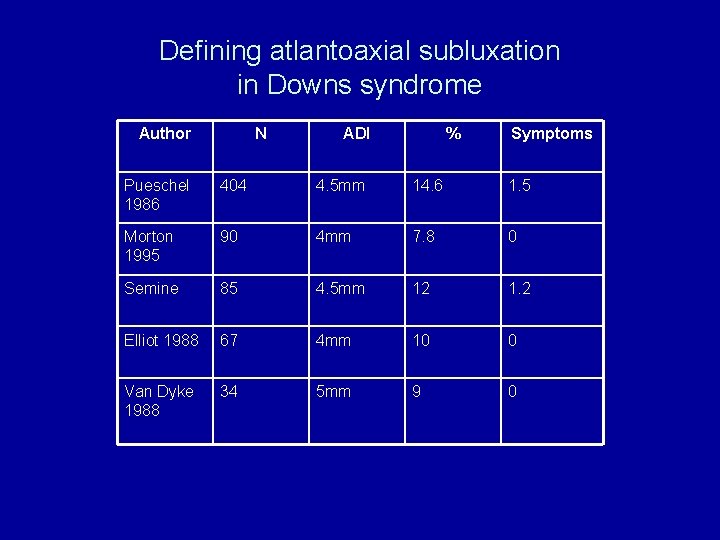
Defining atlantoaxial subluxation in Downs syndrome Author N ADI % Symptoms Pueschel 1986 404 4. 5 mm 14. 6 1. 5 Morton 1995 90 4 mm 7. 8 0 Semine 85 4. 5 mm 12 1. 2 Elliot 1988 67 4 mm 10 0 Van Dyke 1988 34 5 mm 9 0
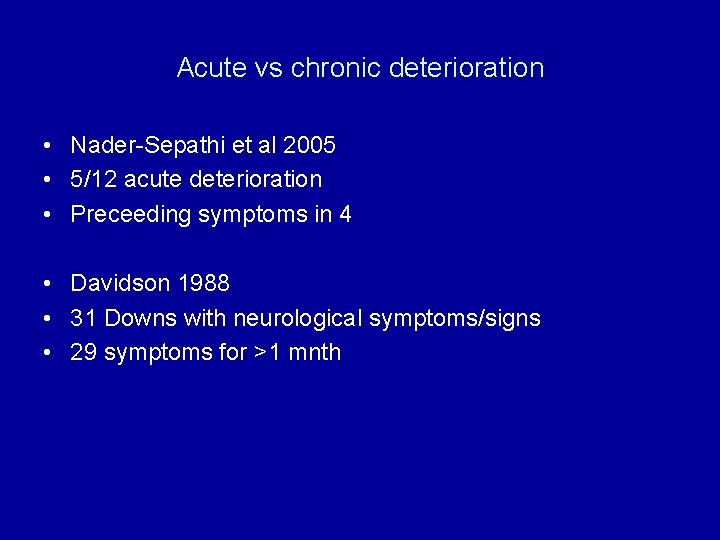
Acute vs chronic deterioration • Nader-Sepathi et al 2005 • 5/12 acute deterioration • Preceeding symptoms in 4 • Davidson 1988 • 31 Downs with neurological symptoms/signs • 29 symptoms for >1 mnth
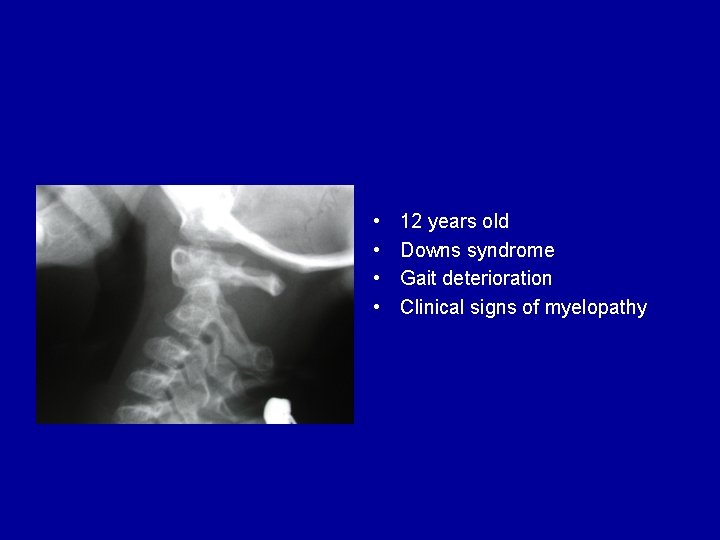
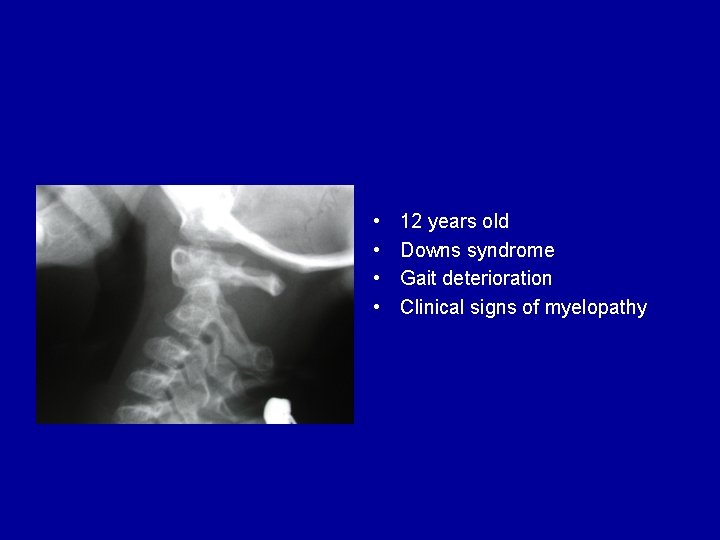
• • 12 years old Downs syndrome Gait deterioration Clinical signs of myelopathy
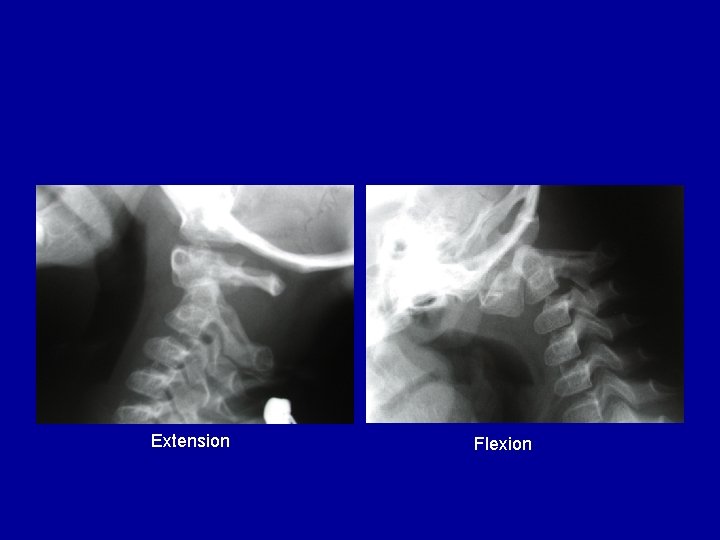
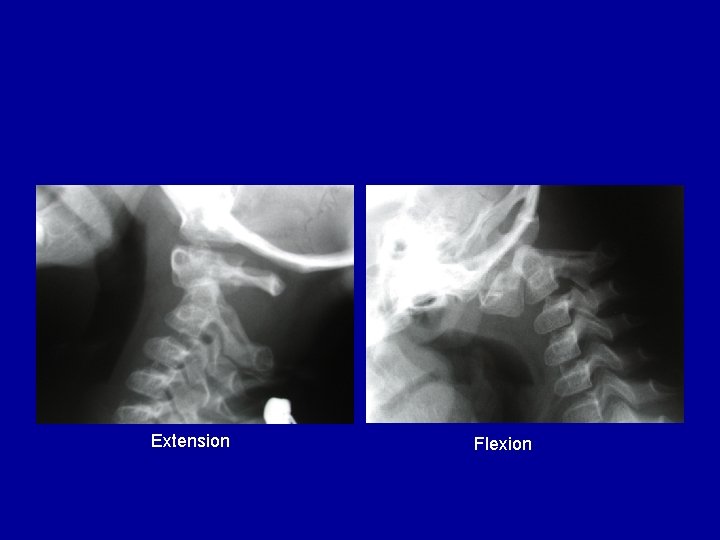
Extension Flexion
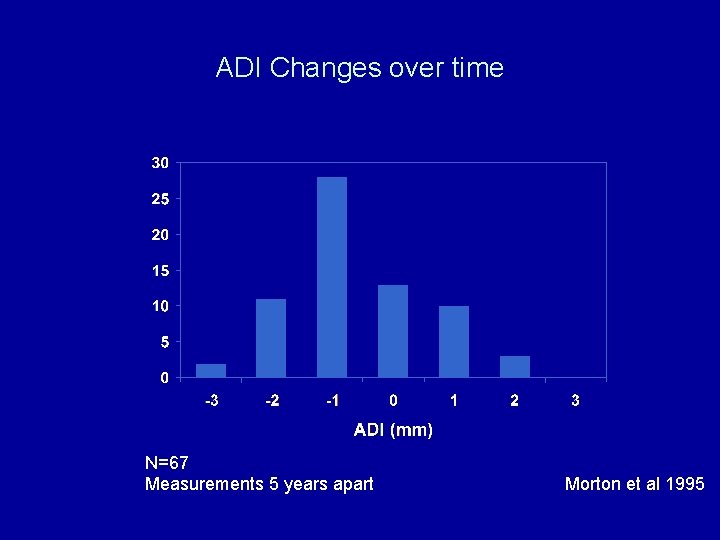
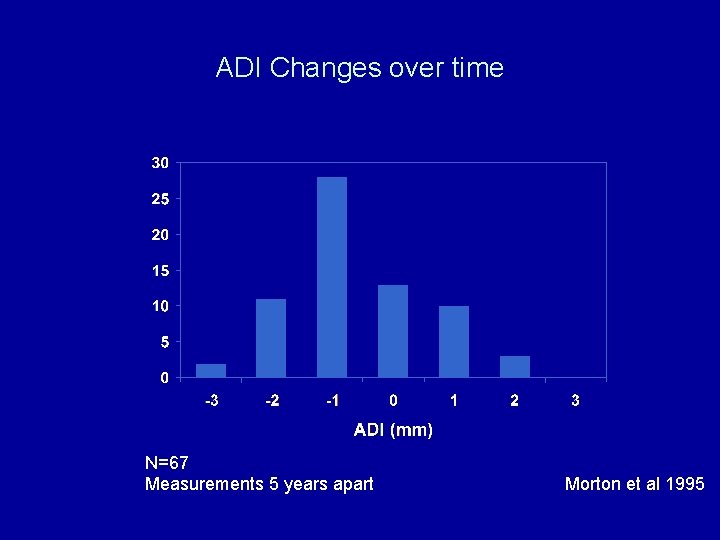
ADI Changes over time N=67 Measurements 5 years apart Morton et al 1995
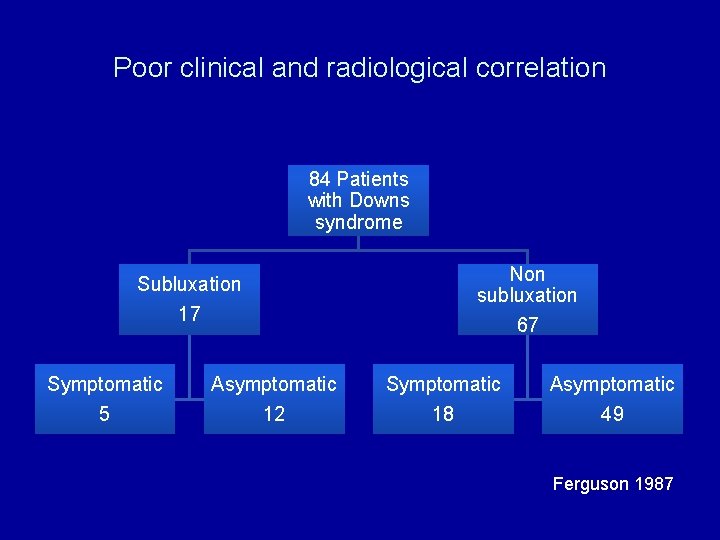
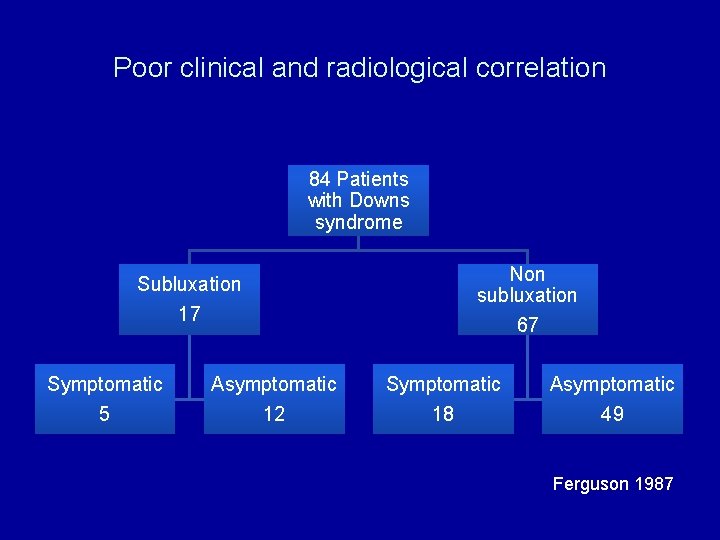
Poor clinical and radiological correlation 84 Patients with Downs syndrome Subluxation 17 Symptomatic 5 Asymptomatic 12 Non subluxation 67 Symptomatic 18 Asymptomatic 49 Ferguson 1987
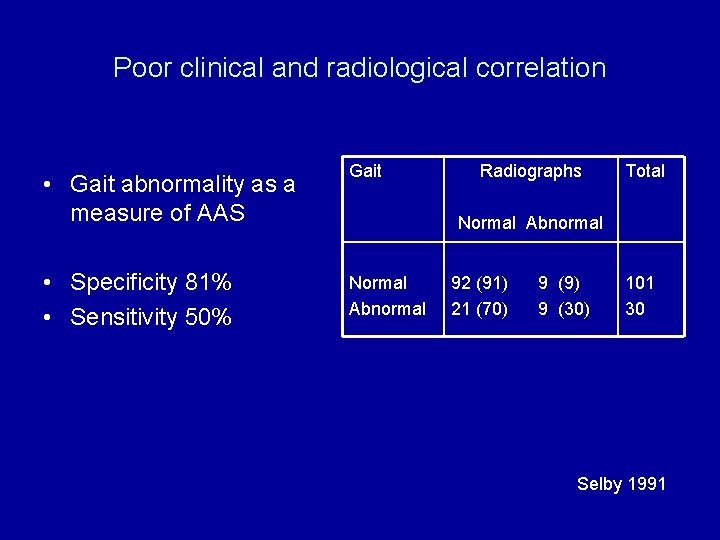
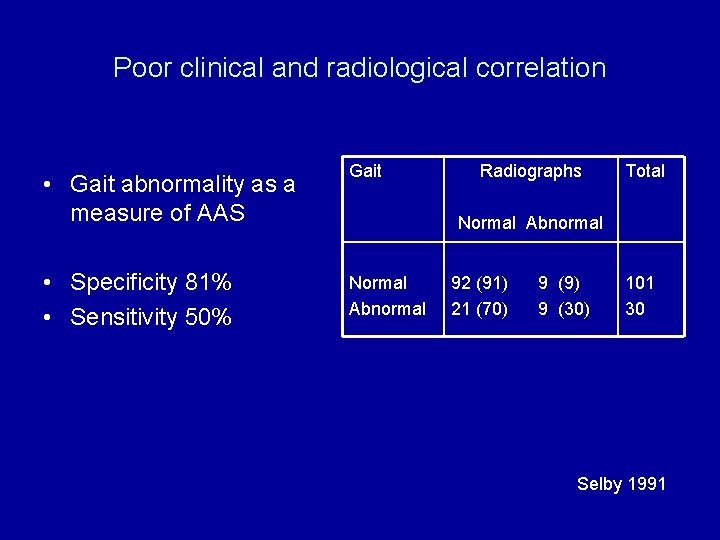
Poor clinical and radiological correlation • Gait abnormality as a measure of AAS • Specificity 81% • Sensitivity 50% Gait Radiographs Total Normal Abnormal 92 (91) 21 (70) 9 (9) 9 (30) 101 30 Selby 1991
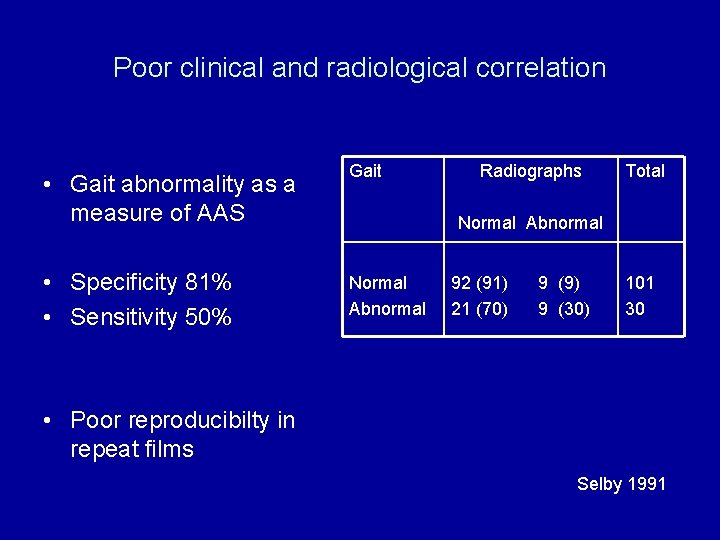
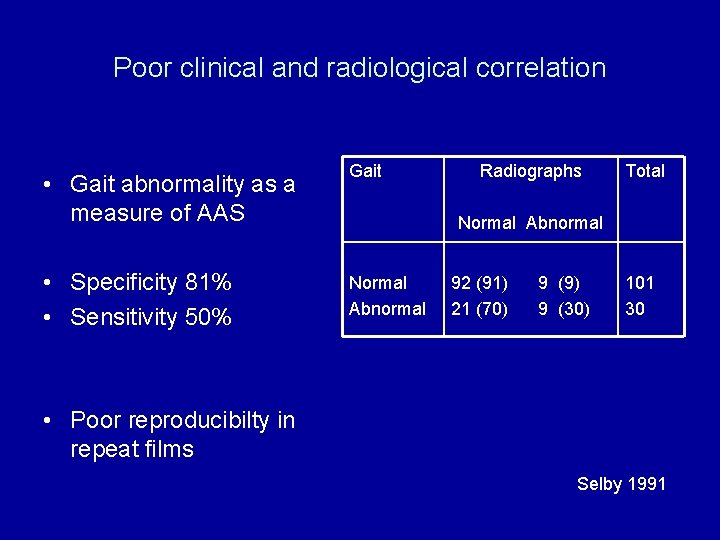
Poor clinical and radiological correlation • Gait abnormality as a measure of AAS • Specificity 81% • Sensitivity 50% Gait Radiographs Total Normal Abnormal 92 (91) 21 (70) 9 (9) 9 (30) 101 30 • Poor reproducibilty in repeat films Selby 1991
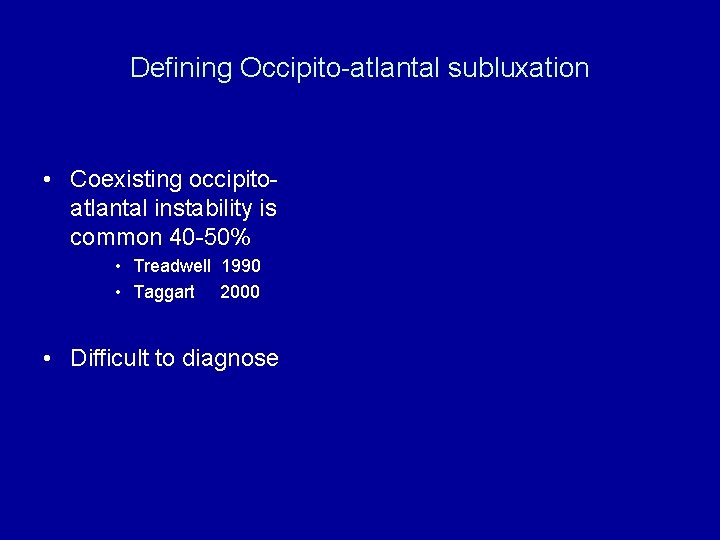
Defining Occipito-atlantal subluxation • Coexisting occipitoatlantal instability is common 40 -50% • Treadwell 1990 • Taggart 2000 • Difficult to diagnose
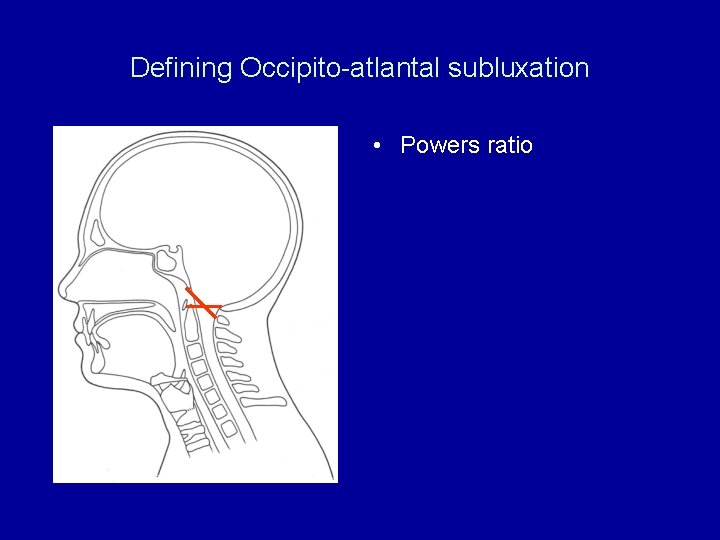
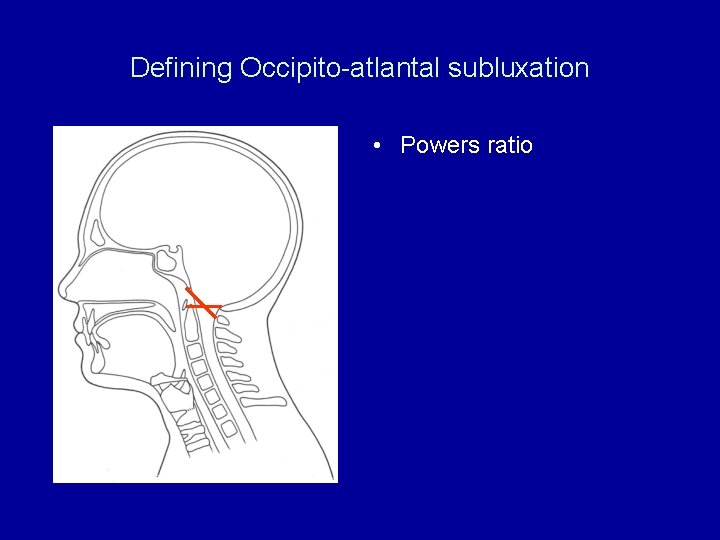
Defining Occipito-atlantal subluxation • Powers ratio
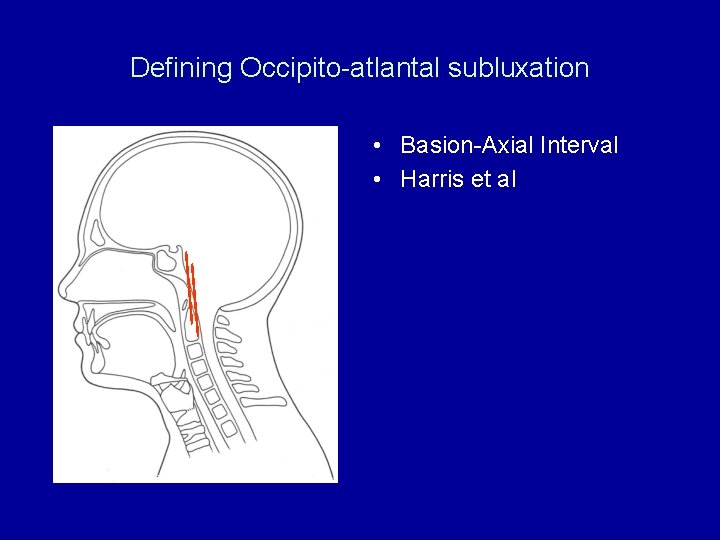
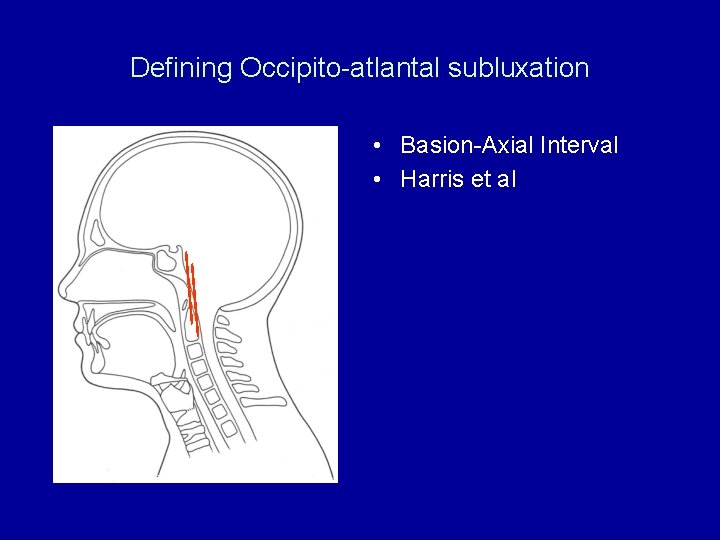
Defining Occipito-atlantal subluxation • Basion-Axial Interval • Harris et al
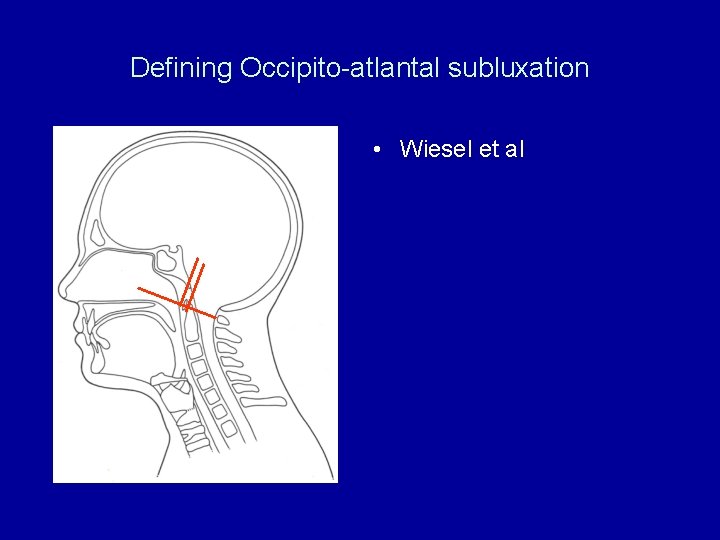
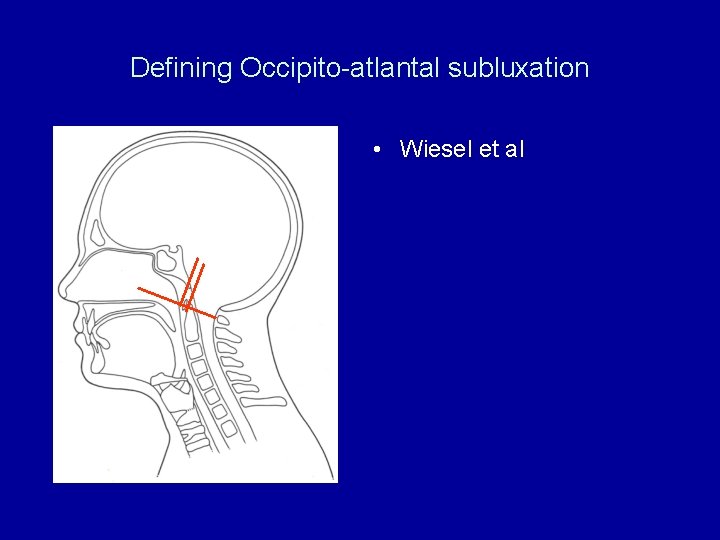
Defining Occipito-atlantal subluxation • Wiesel et al
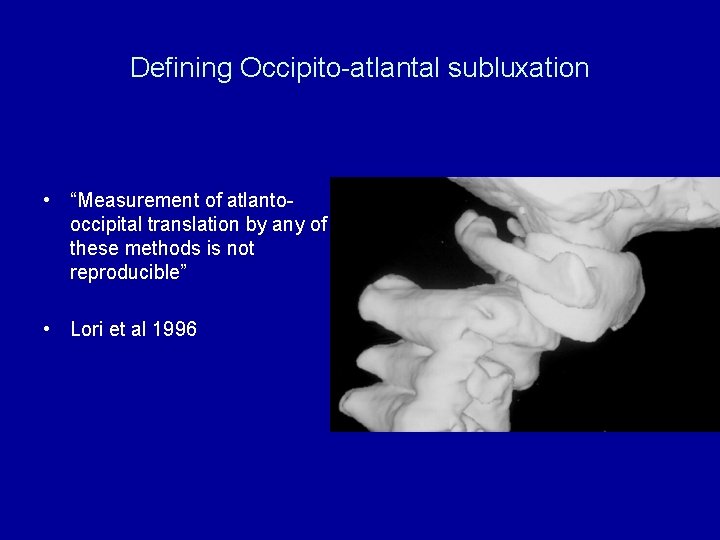
Defining Occipito-atlantal subluxation • “Measurement of atlantooccipital translation by any of these methods is not reproducible” • Lori et al 1996
Limitations of Radiographic Measurements in Downs Syndrome • • ADI No consensus on measurement Poor reproducibility Poor correlation with symptoms O-C instability, present but difficult to measure
Screening
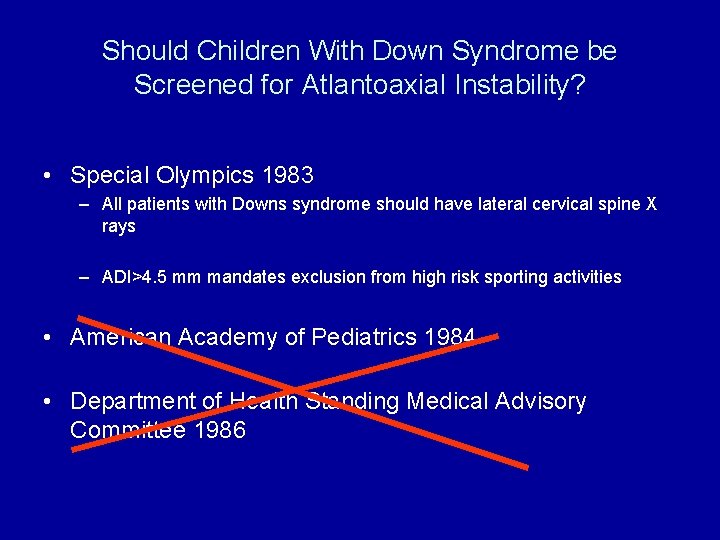
Should Children With Down Syndrome be Screened for Atlantoaxial Instability?
Should Children With Down Syndrome be Screened for Atlantoaxial Instability? • Special Olympics 1983 – All patients with Downs syndrome should have lateral cervical spine X rays – ADI>4. 5 mm mandates exclusion from high risk sporting activities • American Academy of Pediatrics 1984 • Department of Health Standing Medical Advisory Committee 1986
Should Children With Down Syndrome be Screened for Atlantoaxial Instability? • Special Olympics 1983 – All patients with Downs syndrome should have lateral cervical spine X rays – ADI>4. 5 mm mandates exclusion from high risk sporting activities • American Academy of Pediatrics 1984 • Department of Health Standing Medical Advisory Committee 1986
Screening • Incidence must be common • Screening test should be sensitive and specific • Asymptomatic AAS must be a risk factor for symptomatic AAS • A safe and effective intervention should be available
British Guidelines 2009 Downs Medical Interest Group of UK Cervical spine X rays are not recommended for the asymptomatic child with Downs syndrome , Medical personnel and carers need to be aware of the potential for neurological symptoms to develop
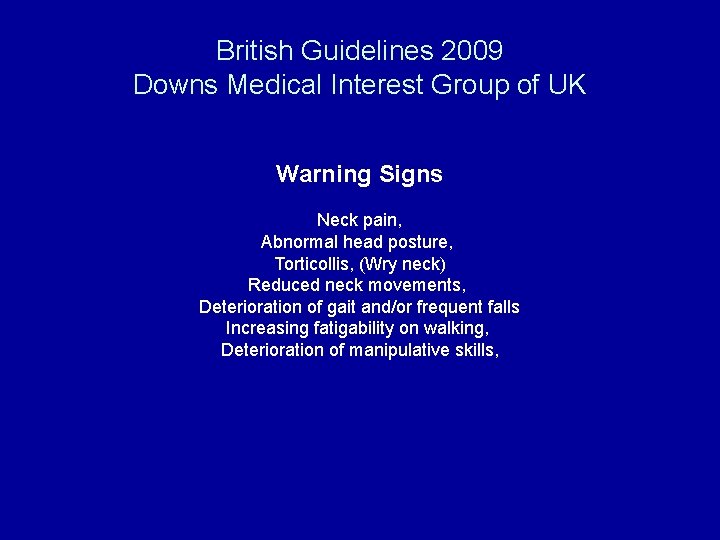
British Guidelines 2009 Downs Medical Interest Group of UK Warning Signs Neck pain, Abnormal head posture, Torticollis, (Wry neck) Reduced neck movements, Deterioration of gait and/or frequent falls Increasing fatigability on walking, Deterioration of manipulative skills,

British Guidelines 2009 Downs Medical Interest Group of UK Action Full physical and neurological examination Specialist Referral
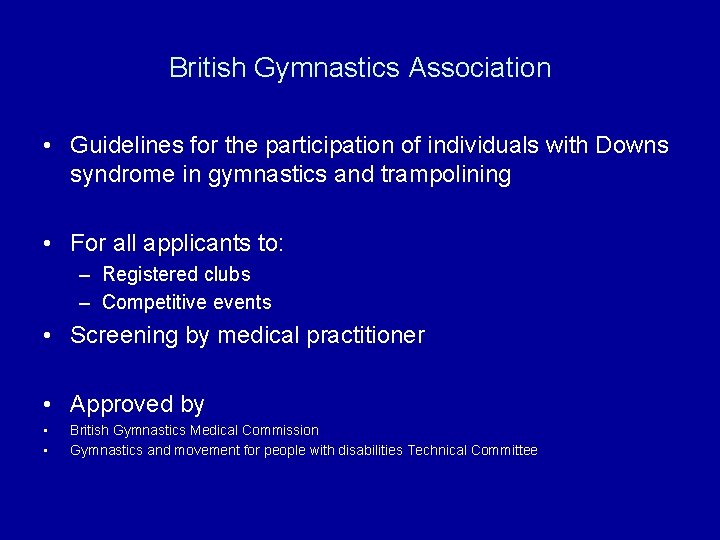
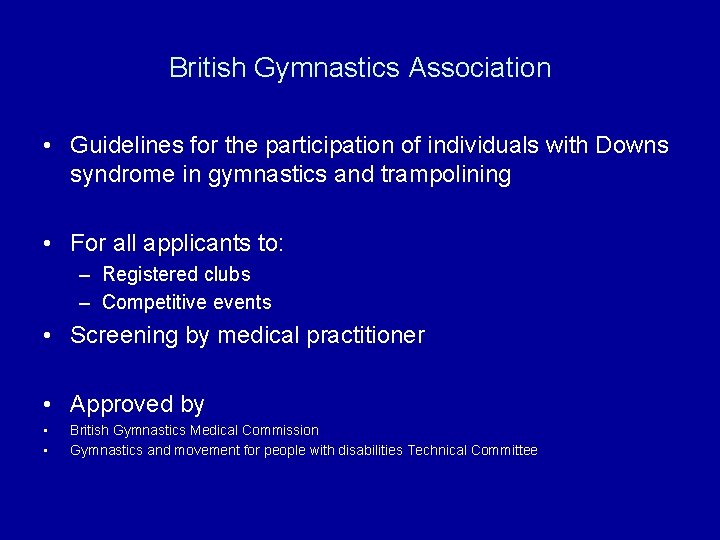
British Gymnastics Association • Guidelines for the participation of individuals with Downs syndrome in gymnastics and trampolining • For all applicants to: – Registered clubs – Competitive events • Screening by medical practitioner • Approved by • • British Gymnastics Medical Commission Gymnastics and movement for people with disabilities Technical Committee
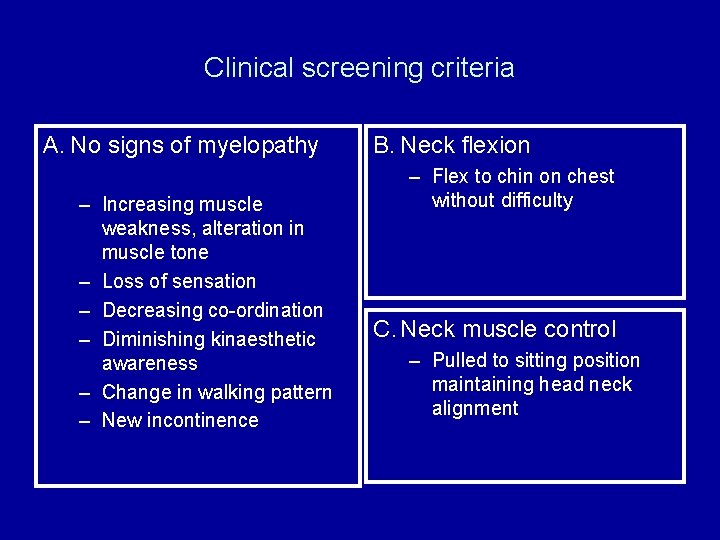
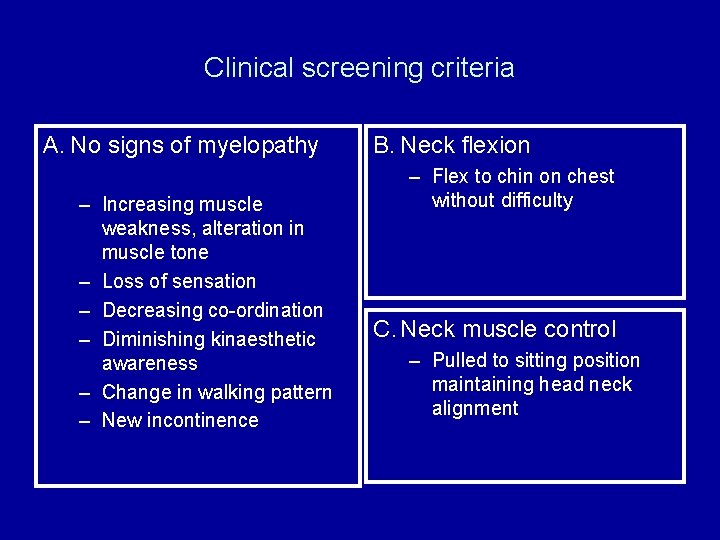
Clinical screening criteria A. No signs of myelopathy – Increasing muscle weakness, alteration in muscle tone – Loss of sensation – Decreasing co-ordination – Diminishing kinaesthetic awareness – Change in walking pattern – New incontinence B. Neck flexion – Flex to chin on chest without difficulty C. Neck muscle control – Pulled to sitting position maintaining head neck alignment
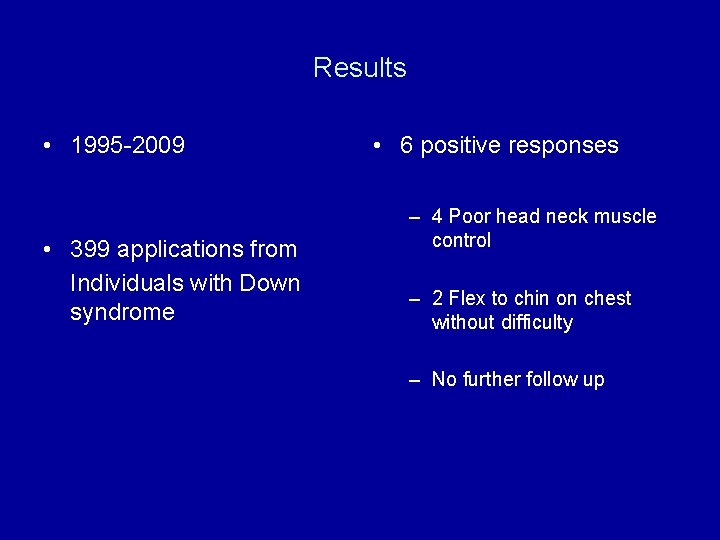
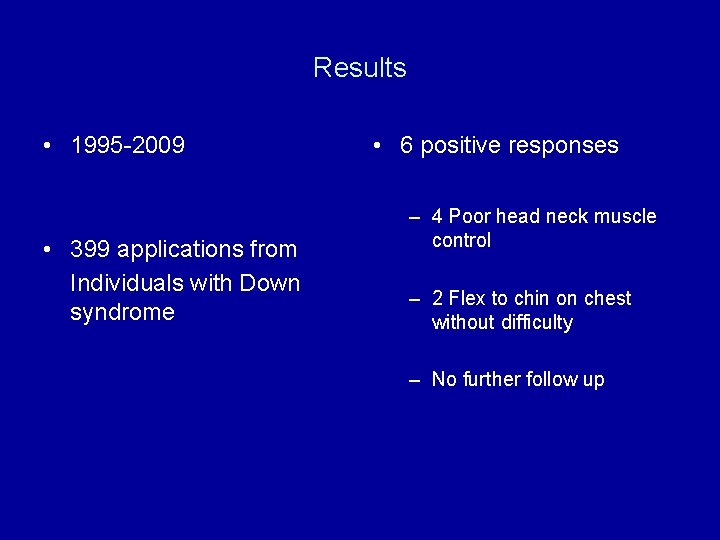
Results • 1995 -2009 • 399 applications from Individuals with Down syndrome • 6 positive responses – 4 Poor head neck muscle control – 2 Flex to chin on chest without difficulty – No further follow up

Results • 393 granted membership • No injuries referable to the cervical spine reported during the time period • 3 in National Squad

Treatment

Treatment • “A safe an effective intervention should be available”
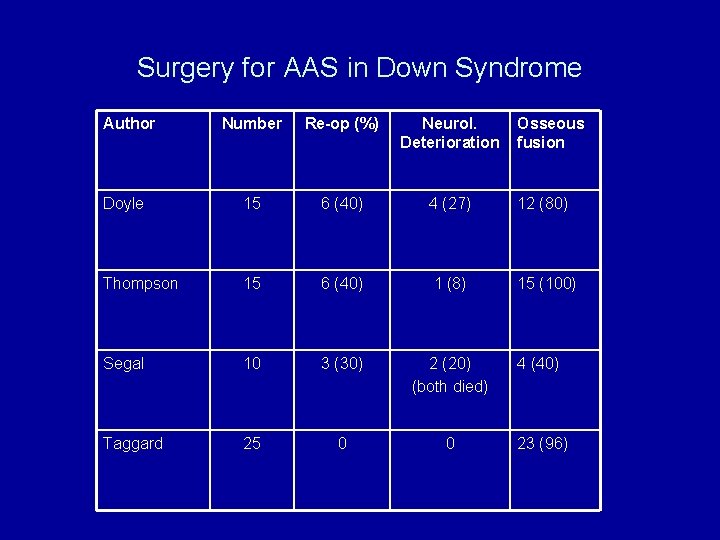
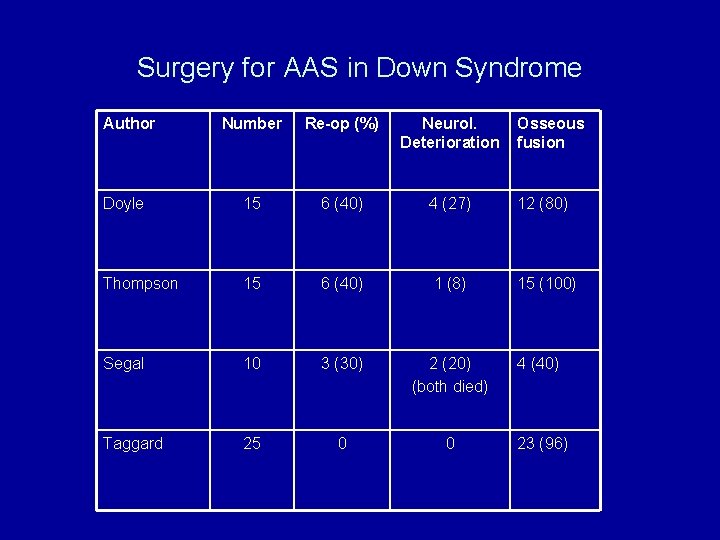
Surgery for AAS in Down Syndrome Author Number Re-op (%) Neurol. Deterioration Osseous fusion Doyle 15 6 (40) 4 (27) 12 (80) Thompson 15 6 (40) 1 (8) 15 (100) Segal 10 3 (30) 2 (20) (both died) 4 (40) Taggard 25 0 0 23 (96)

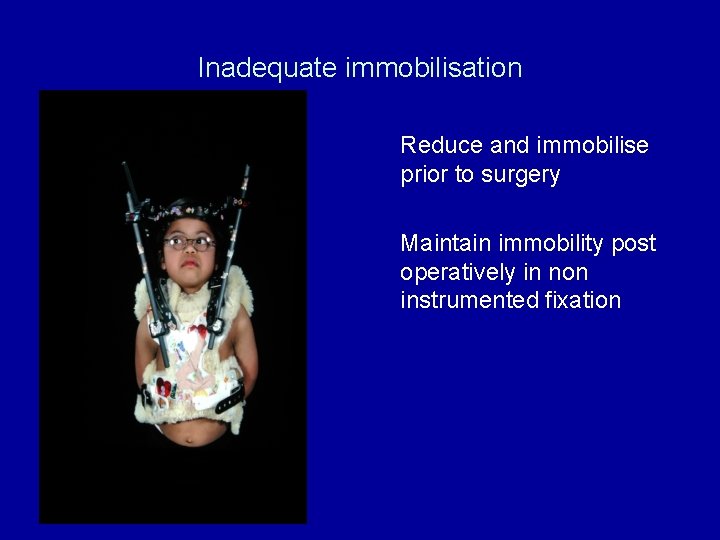
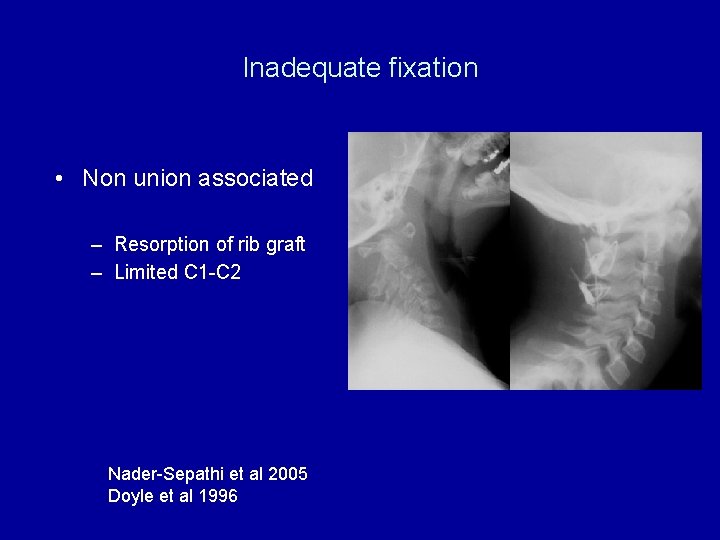
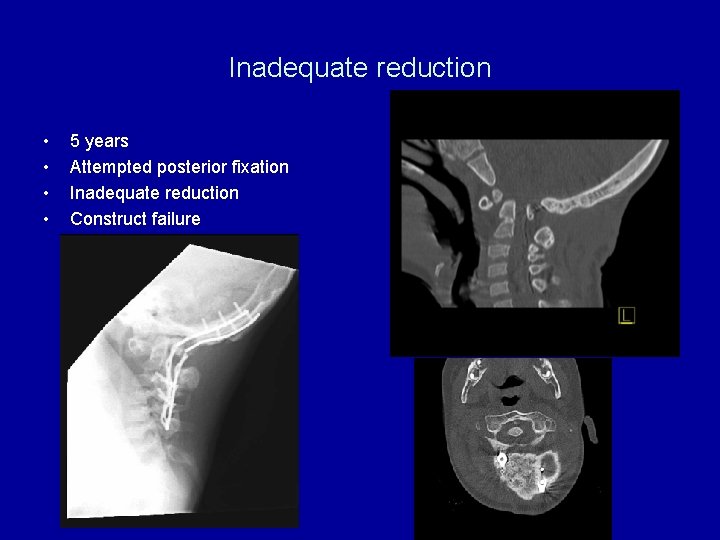
Reasons for failure N=15, 6 failures • • Inadequate immobilisation Inadequate reduction Inadequate fixation Inadequate age
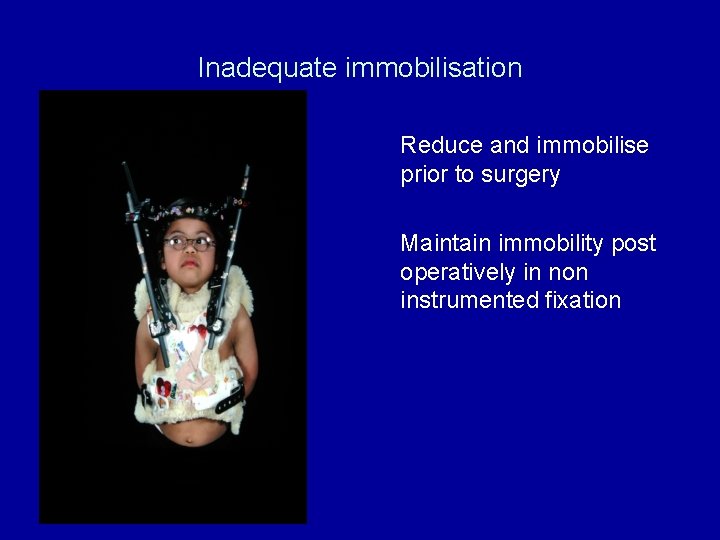
Inadequate immobilisation Reduce and immobilise prior to surgery Maintain immobility post operatively in non instrumented fixation
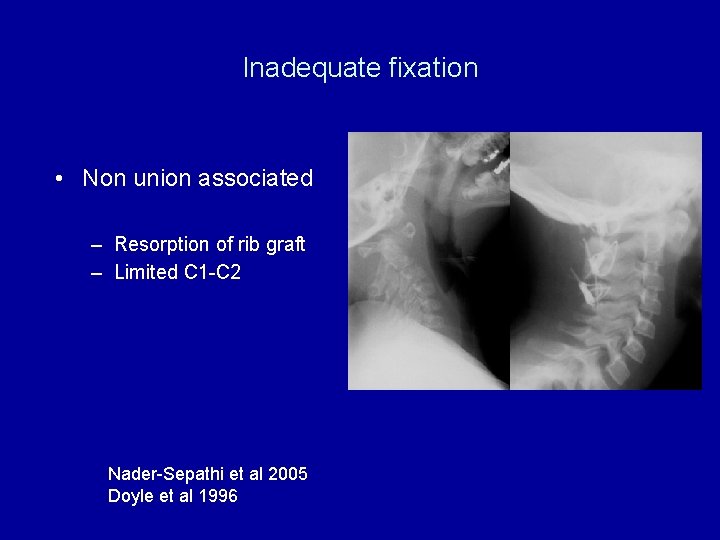
Inadequate fixation • Non union associated – Resorption of rib graft – Limited C 1 -C 2 Nader-Sepathi et al 2005 Doyle et al 1996
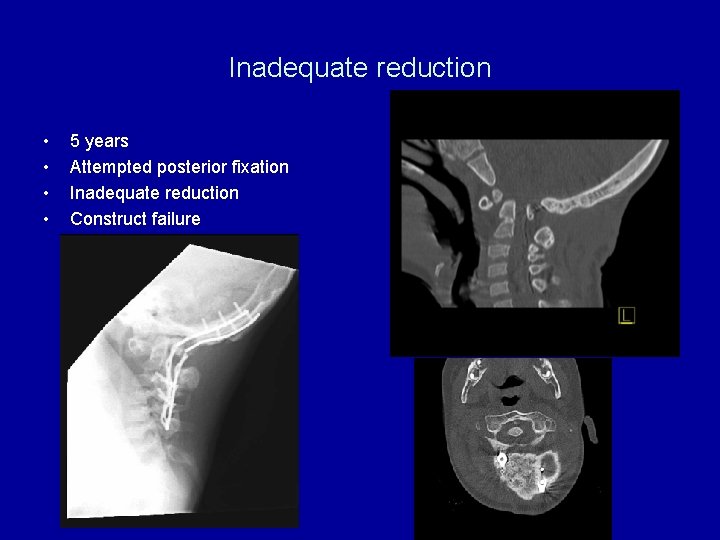
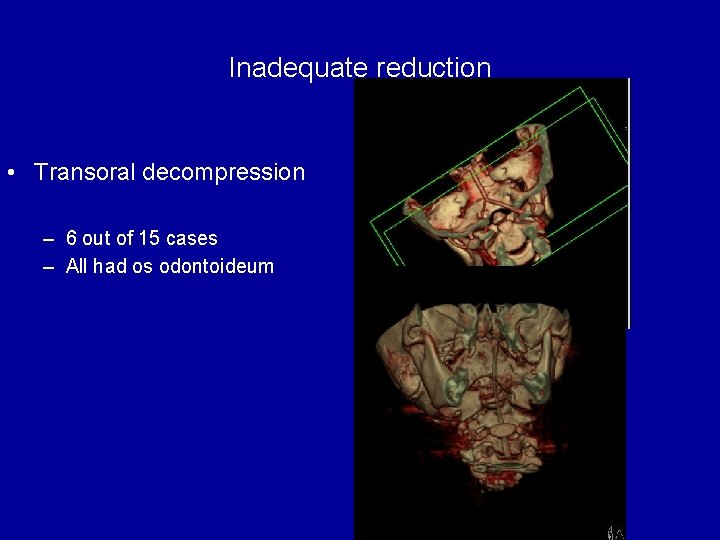
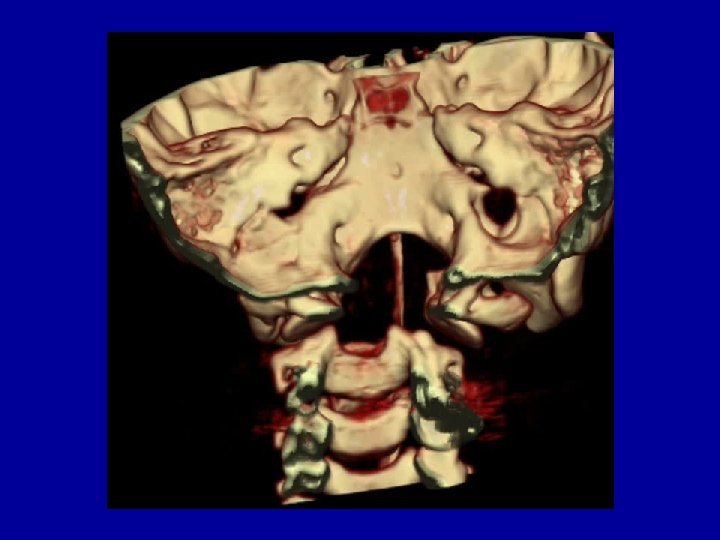
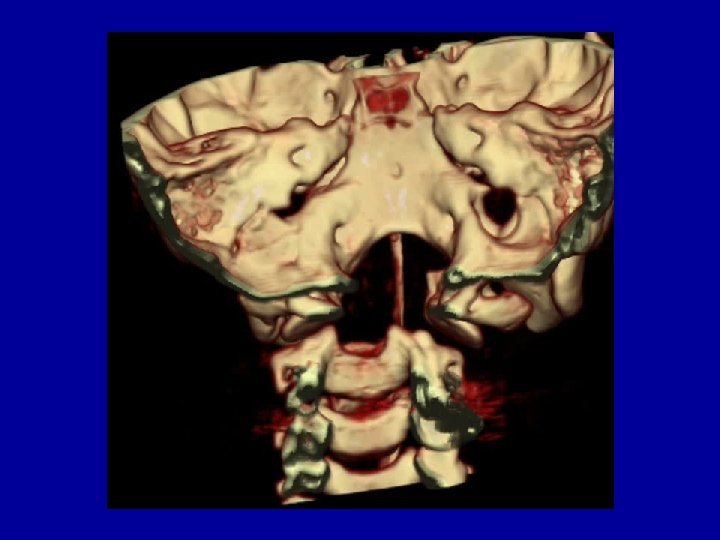
Inadequate reduction • • 5 years Attempted posterior fixation Inadequate reduction Construct failure

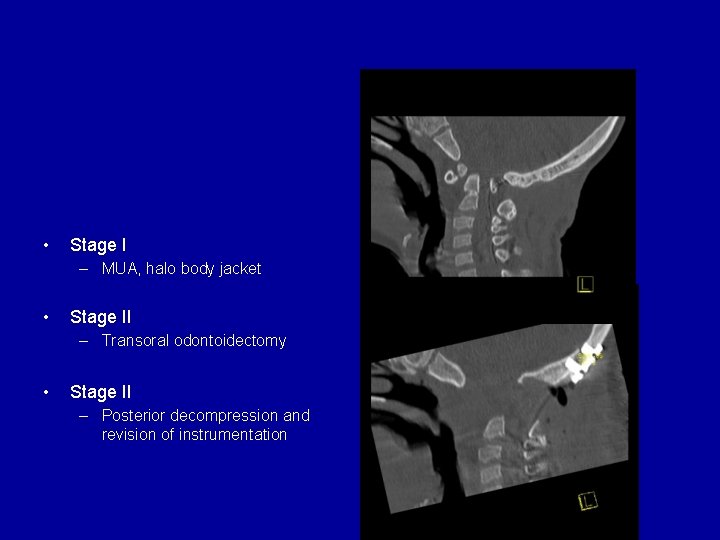
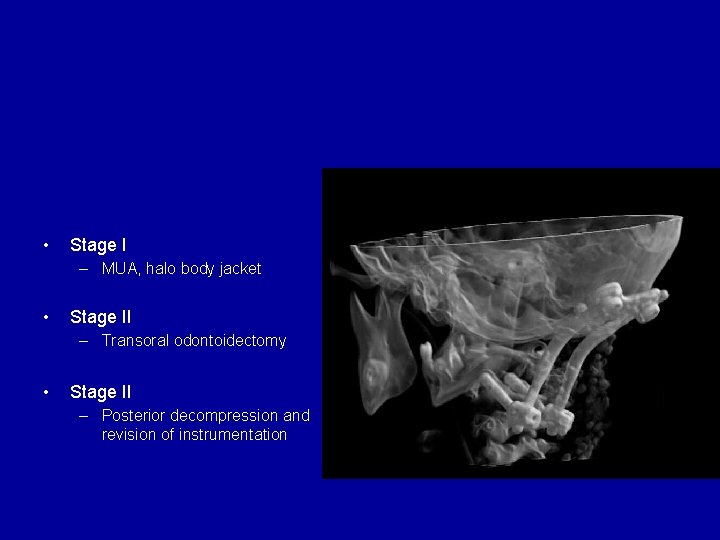
• Stage I – MUA, halo body jacket • Stage II – Transoral odontoidectomy • Stage II – Posterior decompression and revision of instrumentation
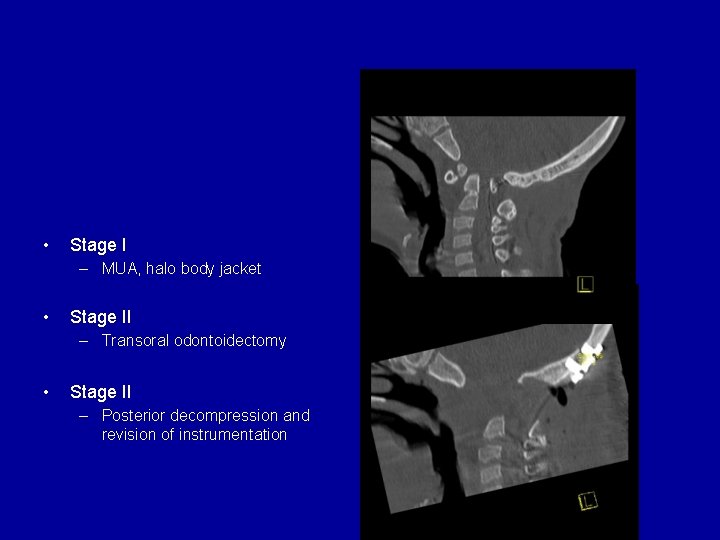
Case 1: Downs syndrome • Stage I – MUA, halo body jacket • Stage II – Transoral odontoidectomy • Stage II – Posterior decompression and revision of instrumentation
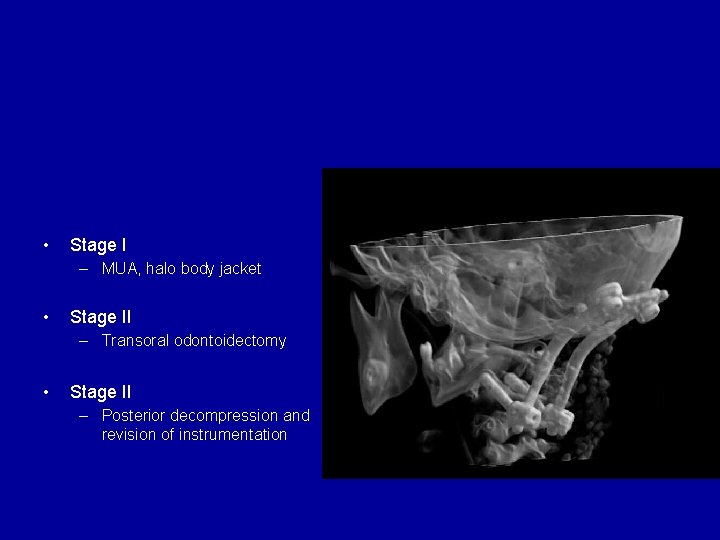
Case 1: Downs syndrome • Stage I – MUA, halo body jacket • Stage II – Transoral odontoidectomy • Stage II – Posterior decompression and revision of instrumentation
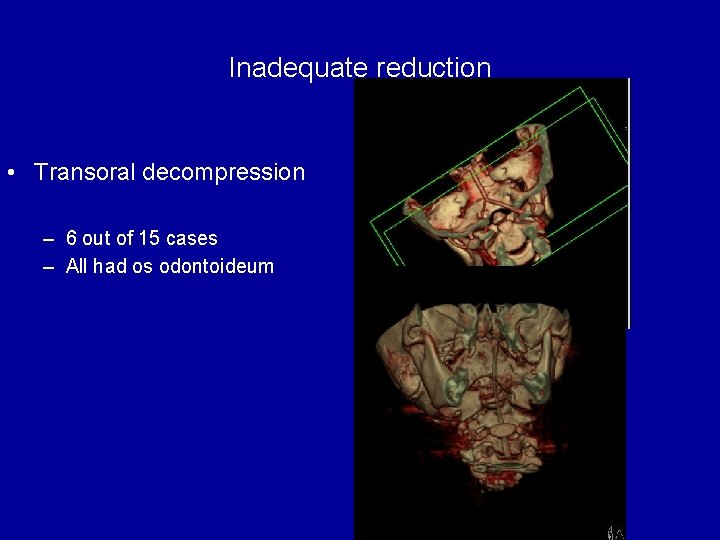
Inadequate reduction • Transoral decompression – 6 out of 15 cases – All had os odontoideum

Conclusions • Osseous anomalies at the CCJ may be consequence rather than cause of instability • Morphometric measures of AAI and OCI lack sufficient sensitivity and specificity to justify screening • Education rather than screening
Conclusions • Early investigation and treatment of symptomatic patients • Beware the child with Downs! • Ensure – Effective immobilisation – Adequate reduction – Rigid fixation

 Myriam srour
Myriam srour Reflexology tips
Reflexology tips Dodoma gas and electric
Dodoma gas and electric Downs cell
Downs cell Downs cell
Downs cell Downs cell
Downs cell Downs cell
Downs cell The life cycle of bureaus anthony downs summary
The life cycle of bureaus anthony downs summary Proceso downs sodio
Proceso downs sodio North downs benefice
North downs benefice Rick downs
Rick downs Downs view infant school
Downs view infant school Glucose ups and downs
Glucose ups and downs Anthony downs
Anthony downs Ra program ideas for upperclassmen
Ra program ideas for upperclassmen Communicable disease and non communicable disease
Communicable disease and non communicable disease Addison's disease vs cushing's syndrome
Addison's disease vs cushing's syndrome Flat thoracic spine
Flat thoracic spine Dorso lumbar region
Dorso lumbar region Shilla spine
Shilla spine Rib vertebral angle
Rib vertebral angle Hilton's law
Hilton's law Interalveolar septa mandible
Interalveolar septa mandible The story spine
The story spine The story spine
The story spine Mental spine of mandible
Mental spine of mandible Spine technologies (i) pvt. ltd
Spine technologies (i) pvt. ltd Range of motion meaning
Range of motion meaning Schober's test positive
Schober's test positive Iliac tubercle
Iliac tubercle Distance decay human geography
Distance decay human geography 5 binder spine template
5 binder spine template Mandibula
Mandibula Short spine board
Short spine board Quartiere spine bianche matera
Quartiere spine bianche matera Spine vs thorn
Spine vs thorn Extreme networks campus fabric
Extreme networks campus fabric What are c spine precautions
What are c spine precautions Scottie dog lumbar spine
Scottie dog lumbar spine Axial skeleton vertebrae
Axial skeleton vertebrae Chapter 28 head and spine injuries
Chapter 28 head and spine injuries Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 20 worksheet the spine
Chapter 20 worksheet the spine Anterior superior iliac spine
Anterior superior iliac spine Racetrack layout adalah
Racetrack layout adalah Ans
Ans Straight store layout
Straight store layout Soleal line
Soleal line Cervical facet referral pattern
Cervical facet referral pattern Site:slidetodoc.com
Site:slidetodoc.com Spine arthrokinematics
Spine arthrokinematics Sacral region
Sacral region Spine blood spatter definition
Spine blood spatter definition Spine allignment
Spine allignment The clavicle and the scapula form the
The clavicle and the scapula form the Rattle spine nms
Rattle spine nms Spine pathology
Spine pathology Decussation of pyramids
Decussation of pyramids Figure 13-1 the spinal cord
Figure 13-1 the spinal cord Spine meninges
Spine meninges Spine
Spine Scistosoma
Scistosoma Emory spine center
Emory spine center Mdcalc nexus c spine
Mdcalc nexus c spine Josh yamada
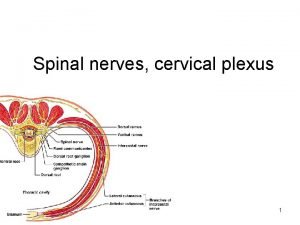
Josh yamada Spinal nerves names
Spinal nerves names Nexus rules c spine
Nexus rules c spine Lat dorsi innervation
Lat dorsi innervation Muscles of thoracic spine
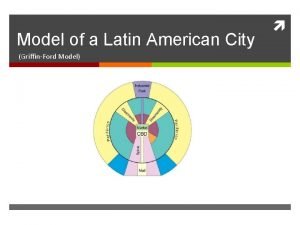
Muscles of thoracic spine Latin american city model spine
Latin american city model spine Position keeping
Position keeping