Management of Central Venous Catheters Theresa Reed BSN
Management of Central Venous Catheters Theresa Reed, BSN, RN, VA-BC Manager, Vascular Access Team and Wound and Ostomy Nurses Texas Children’s Hospital Houston, TX PAGE 0
The single most important thing that you can do to prevent Vascular Access Device infections is to perform hand hygiene before you touch any part of the system. PAGE 1
When it comes to vascular access, what device is best for your patient? • Clear understanding of options for either low risk peripheral access or central access when infusates require central administration PAGE 2
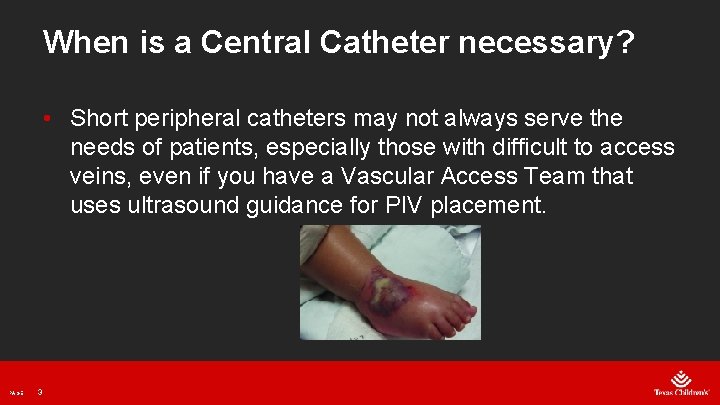
When is a Central Catheter necessary? • Short peripheral catheters may not always serve the needs of patients, especially those with difficult to access veins, even if you have a Vascular Access Team that uses ultrasound guidance for PIV placement. PAGE 3
The Infusion Nurses Society (INS) recommendations for vascular access device (VAD) planning based on: PAGE 4 • Prescribed therapy • Duration of therapy • Vascular characteristics • Patient age • Comorbidities • History of infusion therapy • Preference for VAD location • Ability and resources available to care for the device
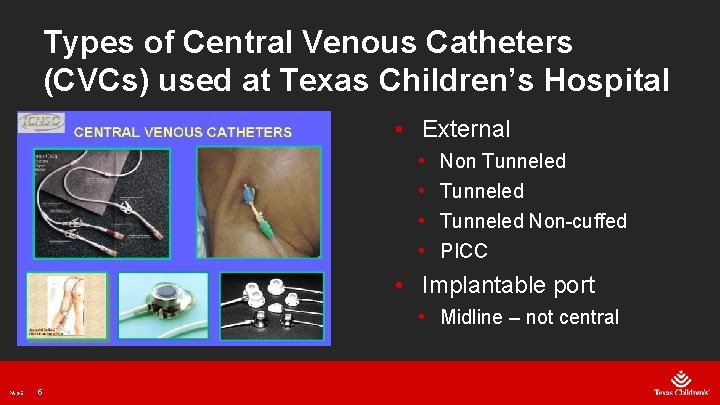
Types of Central Venous Catheters (CVCs) used at Texas Children’s Hospital • External • • Non Tunneled Non-cuffed PICC • Implantable port • Midline – not central PAGE 5
Non Tunneled CVCs • The non tunneled CVC • Inserted directly into the vein • There is no barrier against infection • If bacteria enters at the insertion site it can travel directly into the blood stream PAGE 6

Non Tunneled CVC • Used for more temporary central venous access • Can be pulled at the beside PAGE 7
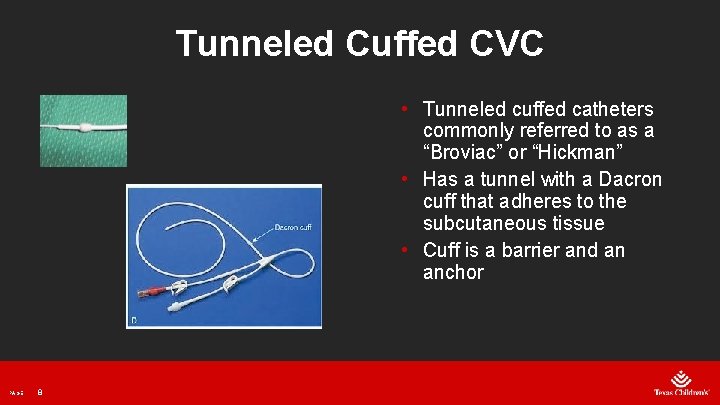
Tunneled Cuffed CVC • Tunneled cuffed catheters commonly referred to as a “Broviac” or “Hickman” • Has a tunnel with a Dacron cuff that adheres to the subcutaneous tissue • Cuff is a barrier and an anchor PAGE 8
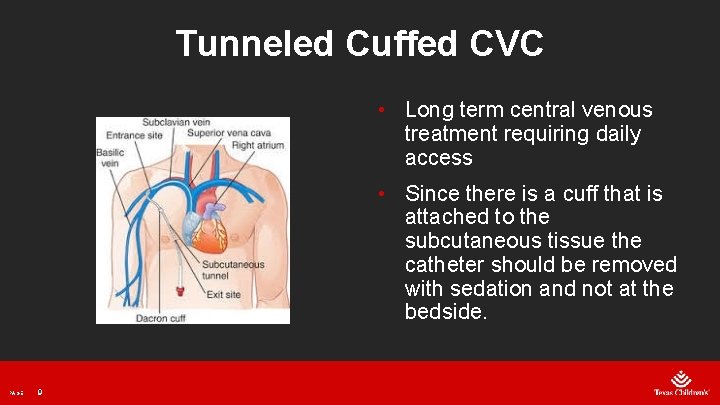
Tunneled Cuffed CVC • Long term central venous treatment requiring daily access • Since there is a cuff that is attached to the subcutaneous tissue the catheter should be removed with sedation and not at the bedside. PAGE 9
Tunneled Non Cuffed CVC • In Pediatrics this type of catheter used to cannulate the IJ and tunnel down the chest for better dressing adherence. • Most common PICC catheters are used for this type of insertion but is considered a tunneled non cuffed catheter if it is not in an extremity. PAGE 10
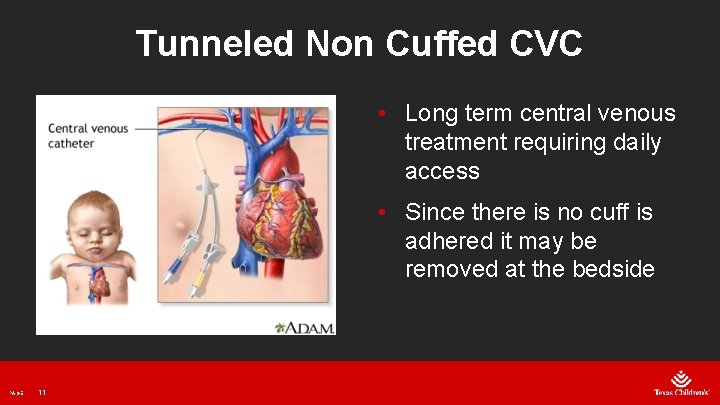
Tunneled Non Cuffed CVC • Long term central venous treatment requiring daily access • Since there is no cuff is adhered it may be removed at the bedside PAGE 11
PICC –Peripherally Inserted Central Catheter • PICC catheters are placed by NCVAT, Interventional Radiology or Surgery at Texas Children's Hospital (TCH). PAGE 12
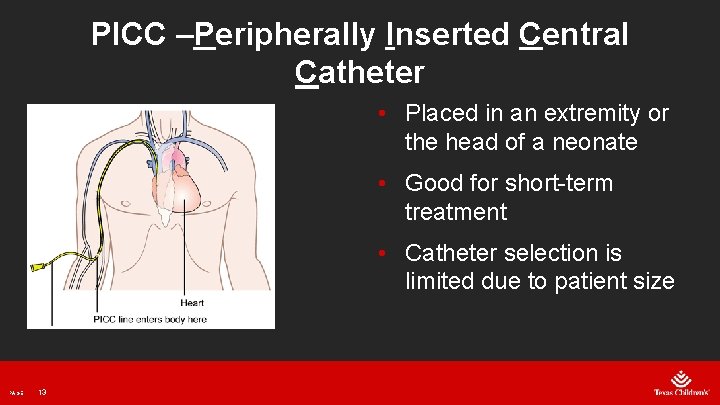
PICC –Peripherally Inserted Central Catheter • Placed in an extremity or the head of a neonate • Good for short-term treatment • Catheter selection is limited due to patient size PAGE 13
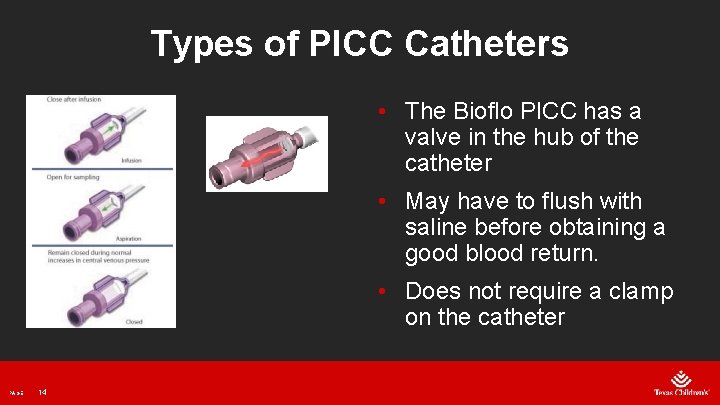
Types of PICC Catheters • The Bioflo PICC has a valve in the hub of the catheter • May have to flush with saline before obtaining a good blood return. • Does not require a clamp on the catheter PAGE 14
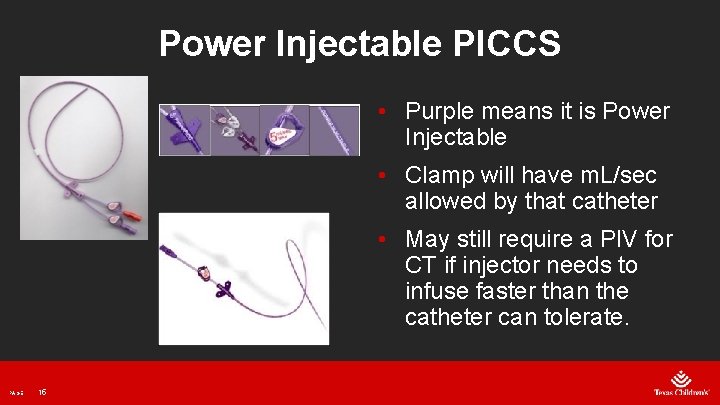
Power Injectable PICCS • Purple means it is Power Injectable • Clamp will have m. L/sec allowed by that catheter • May still require a PIV for CT if injector needs to infuse faster than the catheter can tolerate. PAGE 15
NEO PICCS • Placed by NCVAT in Newborn Center and CVICU • For infusion only, do not heparin lock due to small lumen size may occlude easily. • Rare for blood sampling, lumens too small PAGE 16
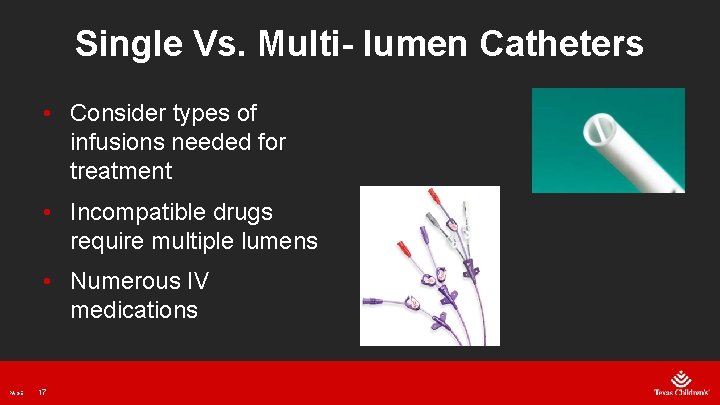
Single Vs. Multi- lumen Catheters • Consider types of infusions needed for treatment • Incompatible drugs require multiple lumens • Numerous IV medications PAGE 17
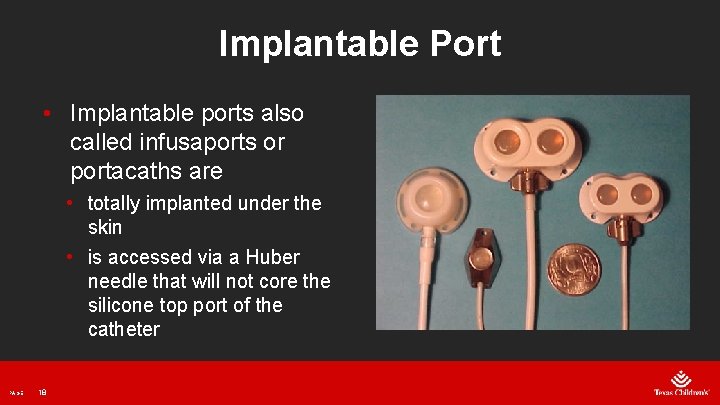
Implantable Port • Implantable ports also called infusaports or portacaths are • totally implanted under the skin • is accessed via a Huber needle that will not core the silicone top port of the catheter PAGE 18
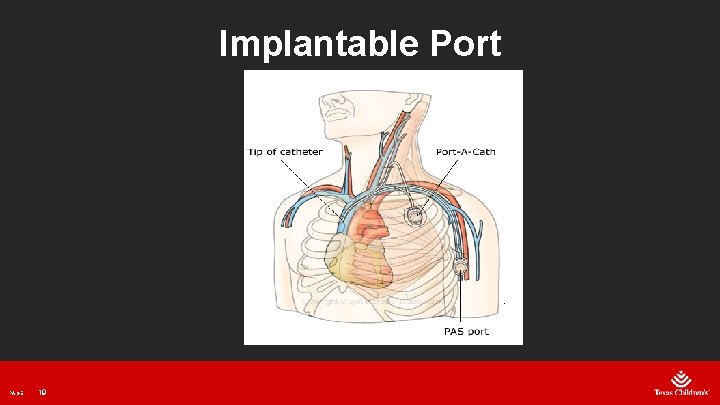
Implantable Port PAGE 19
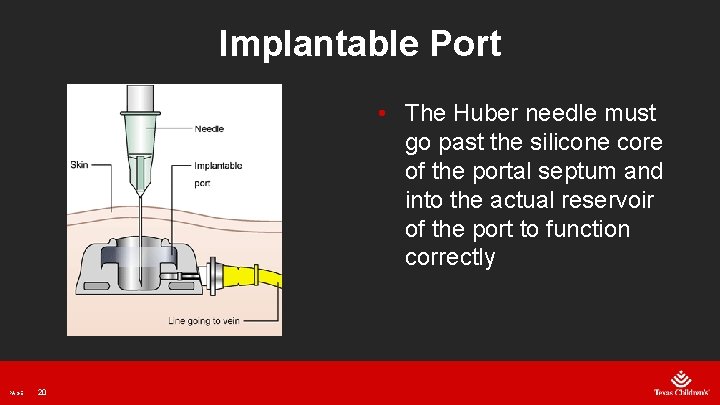
Implantable Port • The Huber needle must go past the silicone core of the portal septum and into the actual reservoir of the port to function correctly PAGE 20
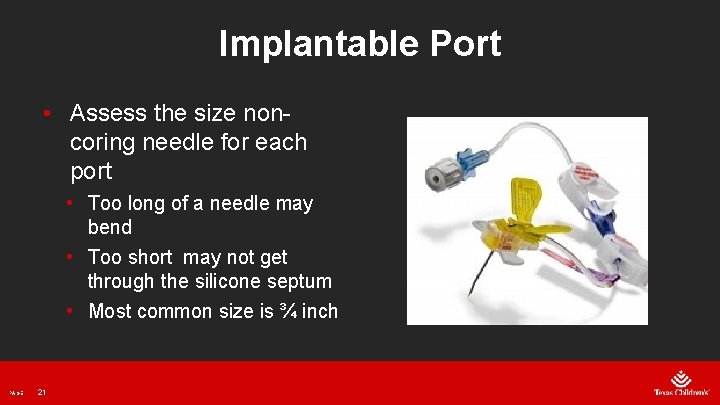
Implantable Port • Assess the size noncoring needle for each port • Too long of a needle may bend • Too short may not get through the silicone septum • Most common size is ¾ inch PAGE 21
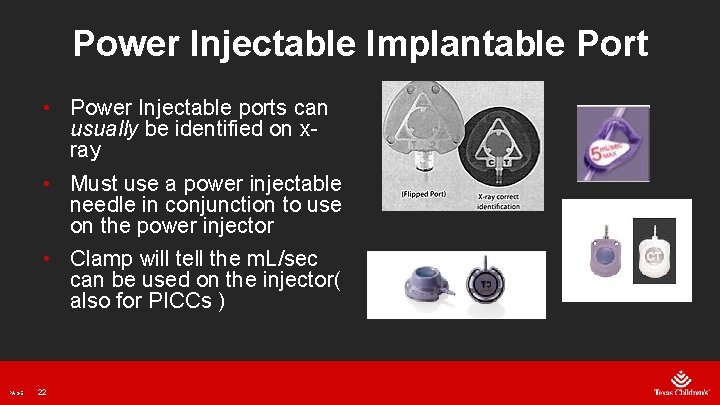
Power Injectable Implantable Port • Power Injectable ports can usually be identified on xray • Must use a power injectable needle in conjunction to use on the power injector • Clamp will tell the m. L/sec can be used on the injector( also for PICCs ) PAGE 22

Implantable Port Pain Protocol • Topical analgesics for the implantable port accesses: • Vapo-coolant spray • LMX • Dressing Removal: • Brava PAGE 23
Midline • Not Central • No TPN over 12. 5 % dextrose • No heparin over 10 units/m. L • No vesicants • Catheter terminates in axilla or lower on the arm PAGE 24
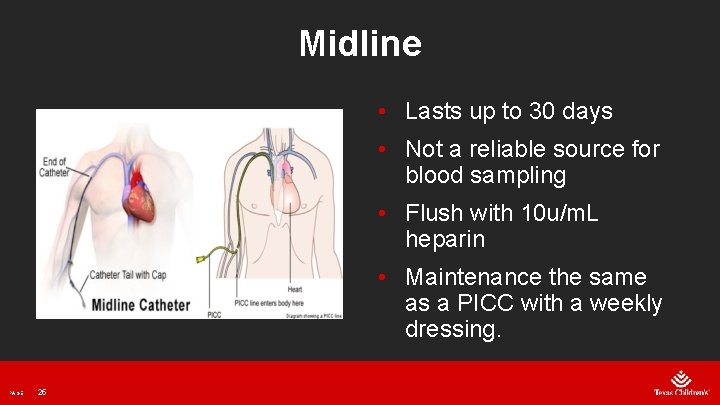
Midline • Lasts up to 30 days • Not a reliable source for blood sampling • Flush with 10 u/m. L heparin • Maintenance the same as a PICC with a weekly dressing. PAGE 25

CVC Policies and Troubleshooting PAGE 26
CVC Policies • Do not hand flush with anything less than a 10 -m. L syringe due to the larger pressure exerted with smaller syringes on smaller diameter catheters. • Smaller syringes need to be on a pump and not hand flushed PAGE 27
CVC Policies • Catheter removal • Removal of a tunneled cuffed CVC or implantable port is a medical act and must be done by a physician • The Vascular Access Team (VAT) or RN with competence determined by the specific unit may remove a non-tunneled CVC at TCH • At TCH there is a specific competency that is completed to remove a PICC • The VAT, RN trained by the VAT, or any advanced practice RN, PA, or physician may remove a PICC PAGE 28
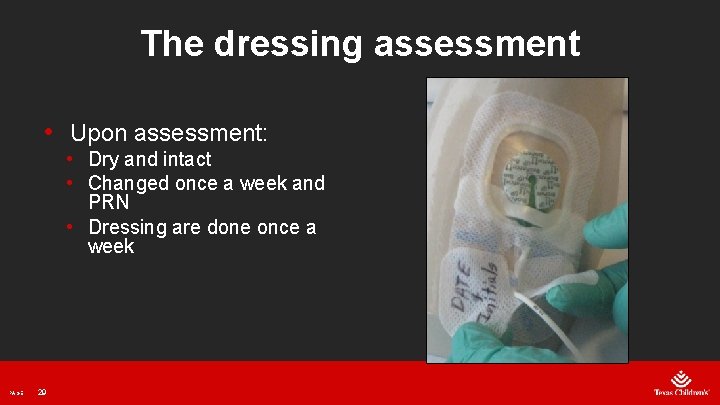
The dressing assessment • Upon assessment: • Dry and intact • Changed once a week and PRN • Dressing are done once a week PAGE 29
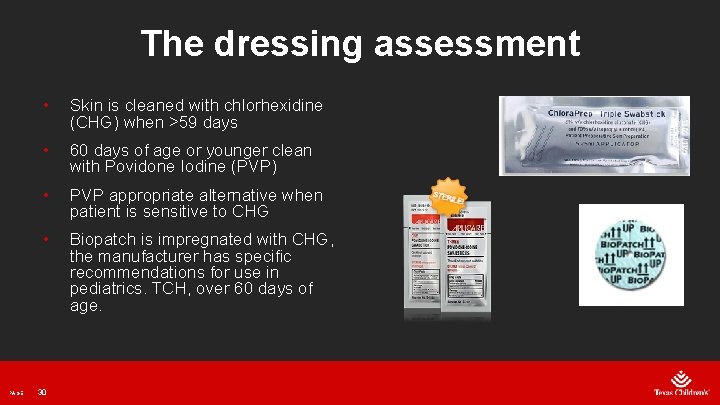
The dressing assessment PAGE • Skin is cleaned with chlorhexidine (CHG) when >59 days • 60 days of age or younger clean with Povidone Iodine (PVP) • PVP appropriate alternative when patient is sensitive to CHG • Biopatch is impregnated with CHG, the manufacturer has specific recommendations for use in pediatrics. TCH, over 60 days of age. 30
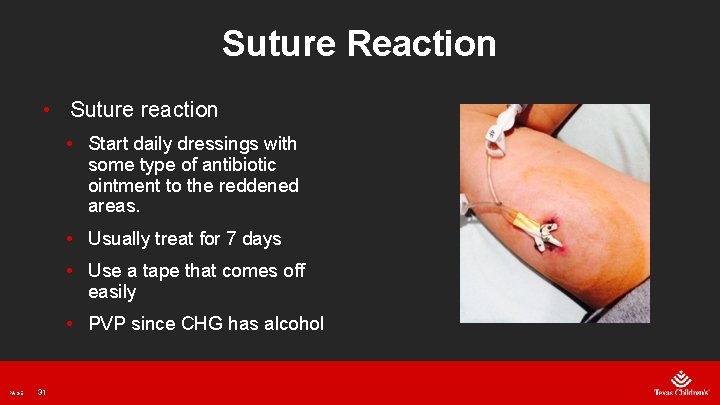
Suture Reaction • Suture reaction • Start daily dressings with some type of antibiotic ointment to the reddened areas. • Usually treat for 7 days • Use a tape that comes off easily • PVP since CHG has alcohol PAGE 31
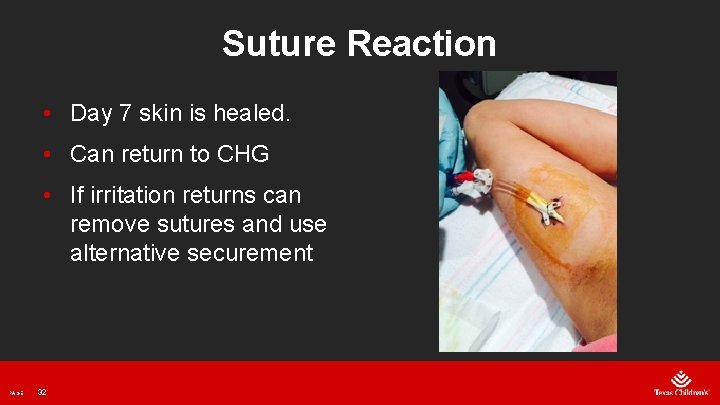
Suture Reaction • Day 7 skin is healed. • Can return to CHG • If irritation returns can remove sutures and use alternative securement PAGE 32
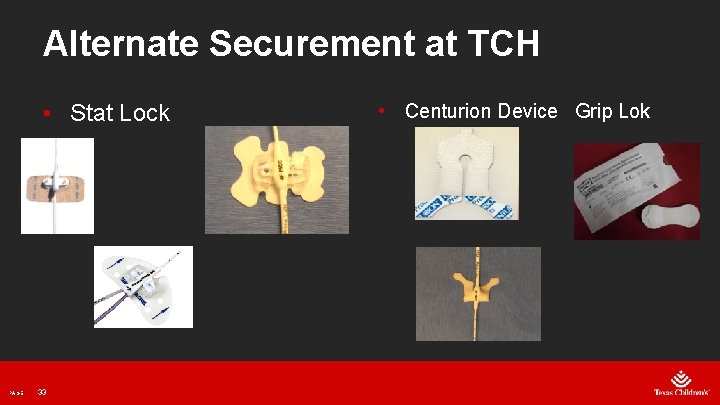
Alternate Securement at TCH • Stat Lock PAGE 33 • Centurion Device Grip Lok
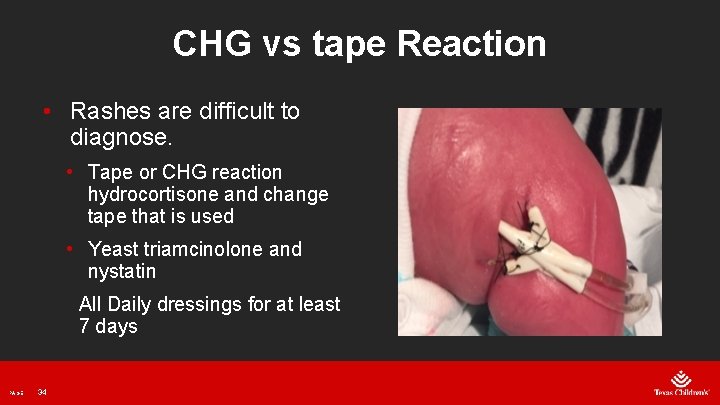
CHG vs tape Reaction • Rashes are difficult to diagnose. • Tape or CHG reaction hydrocortisone and change tape that is used • Yeast triamcinolone and nystatin All Daily dressings for at least 7 days PAGE 34

Rashes PAGE 35
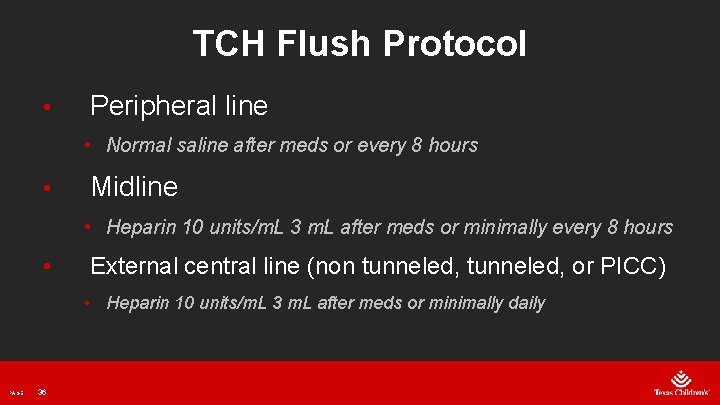
TCH Flush Protocol • Peripheral line • Normal saline after meds or every 8 hours • Midline • Heparin 10 units/m. L 3 m. L after meds or minimally every 8 hours • External central line (non tunneled, or PICC) • Heparin 10 units/m. L 3 m. L after meds or minimally daily PAGE 36
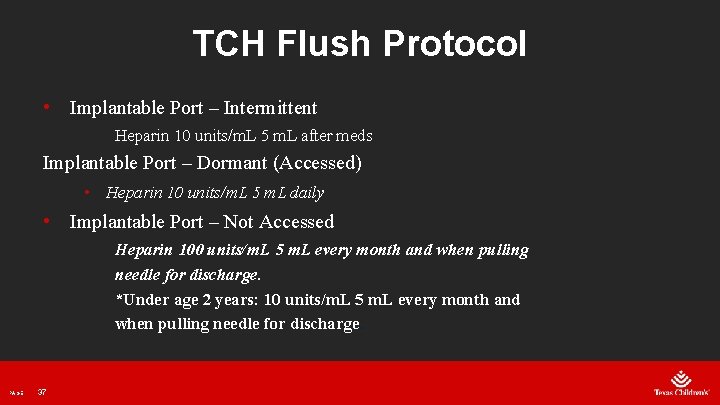
TCH Flush Protocol • Implantable Port – Intermittent Heparin 10 units/m. L 5 m. L after meds Implantable Port – Dormant (Accessed) • Heparin 10 units/m. L 5 m. L daily • Implantable Port – Not Accessed Heparin 100 units/m. L 5 m. L every month and when pulling needle for discharge. *Under age 2 years: 10 units/m. L 5 m. L every month and when pulling needle for discharge. PAGE 37
CVC Occlusions • Smaller gauge catheters used frequently in neonates and small pediatric patients are associated with higher incidence of complications. • These catheters function better if there is fluids running at a TKO rate it the fluids can be tolerated. • TKO is different for each patient, the rate it takes to keep it from backing up. PAGE 38
CVC Occlusions • An occlusion occurs when a CVC is no longer patent. The occlusion can either be partial, which is no blood return, or complete occlusion which is unable to flush or get a blood return. PAGE 39
CVC Occlusions • Three types of CVC occlusions: • Mechanical • Precipitate • Thrombotic PAGE 40
Mechanical CVC Occlusions • Caused by compression of the line by kinked tubing, that can be internal or external, a catheter secured over a joint or a clamped line. Another cause is “Pinch Off” syndrome. • Caused by a malpositioned catheter. PAGE 41
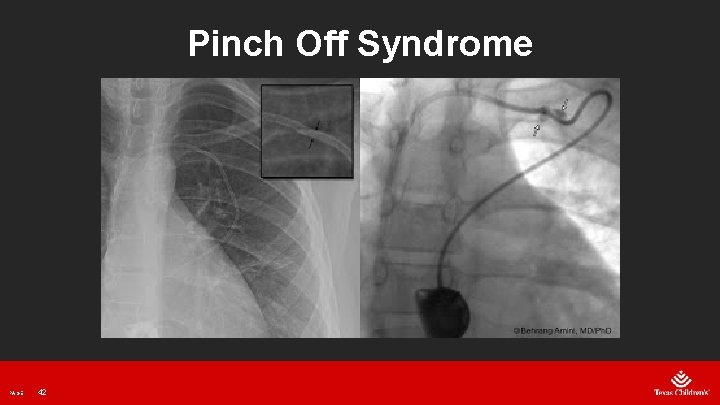
Pinch Off Syndrome PAGE 42
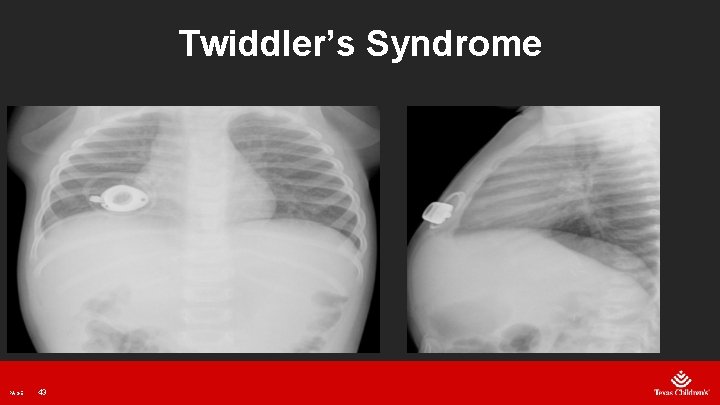
Twiddler’s Syndrome PAGE 43
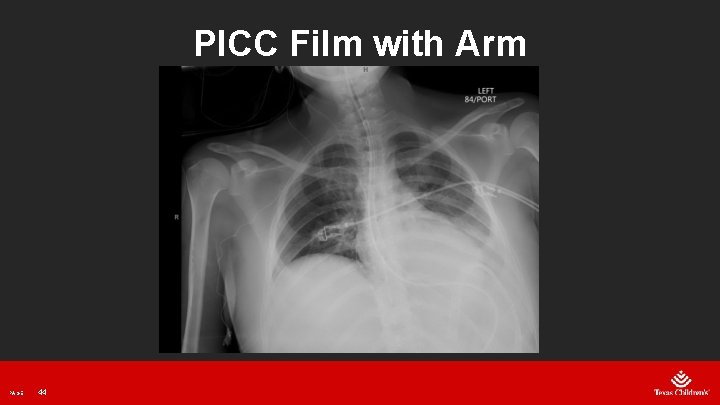
PICC Film with Arm PAGE 44
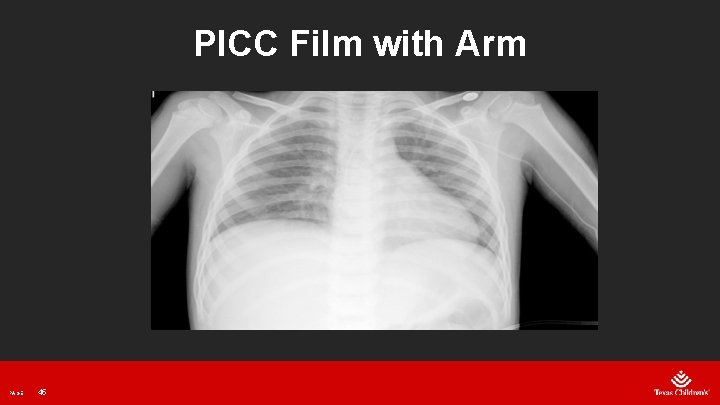
PICC Film with Arm PAGE 45
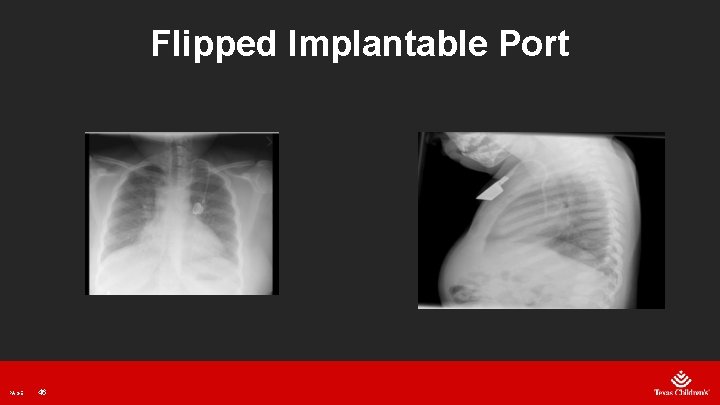
Flipped Implantable Port PAGE 46
Precipitate CVC Occlusions • When incompatible medications combine in the catheter lumen. A sudden occlusion can be a sign that a precipitation has occurred. • Smaller vessel size and lack of options for alternate access, many pediatric patients have single lumen catheters that require piggybacking to administer medications. PAGE 47
Precipitate CVC Occlusions • Mineral occlusions are typically treated with hydrochloric acid (0. 1 N HCL) due to calcium and phosphorus precipitations in Parenteral Nutrition. • 0. 1 N HCL is used to dissolve precipitates generated from acidic agents. PAGE 48
Precipitate CVC Occlusions • Mineral occlusions are typically treated with hydrochloric acid (0. 1 N HCL) due to calcium and phosphorus precipitations in Parenteral Nutrition. • 0. 1 N HCL is used to dissolve precipitates generated from acidic agents. PAGE 49
Thrombotic Occlusions • It is estimated that thrombotic occlusions occur at 60% of all CVC occlusions. • Within 2 weeks of insertion most catheters develop a fibrin sheath, does not indicate catheter malfunction but can lead to a partial occlusions. • CVCs with the tip in the lower third of the SVC have a lower risk of occlusion. PAGE 50
Thrombotic Occlusions • Can lead to CLABSI as it provides a perfect medium for bacteria growth. • Important to treat a catheter as soon as a potential line issue is noticed. PAGE 51
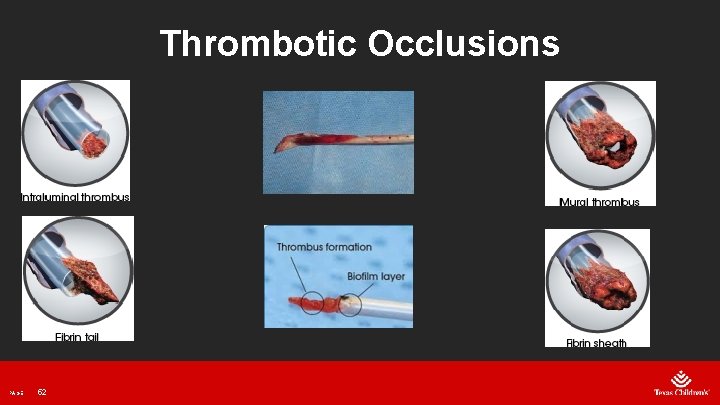
Thrombotic Occlusions PAGE 52
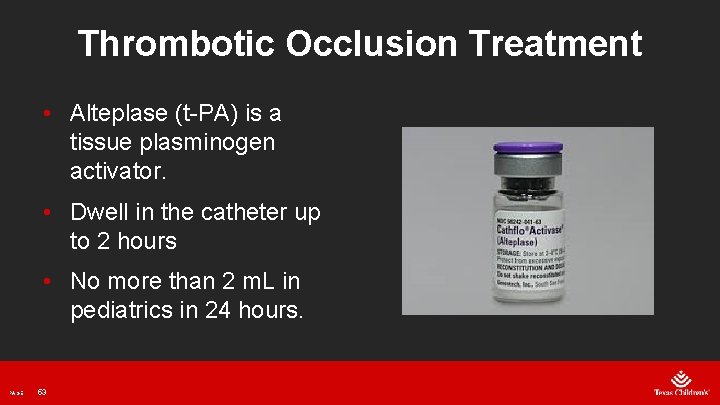
Thrombotic Occlusion Treatment • Alteplase (t-PA) is a tissue plasminogen activator. • Dwell in the catheter up to 2 hours • No more than 2 m. L in pediatrics in 24 hours. PAGE 53
Conclusion • Pediatric patients require CVCs to provide stable and reliable venous access for treatment. • Maintenance is crucial for successful treatment. • An occlusion can lead to: • Interruption of therapy • Risk for CLABSI • Increased health care costs PAGE 54
Conclusion • Proper selection of the vascular access device will help enable successful outcomes • Clinicians should be aware of the proper care and management of complications as they arise. • The quicker the troubleshooting begins, the more likely there will be resolution and IV therapy can be restored. PAGE 55
PAGE 56

VAT Community Work PAGE 57
References PAGE 1. Moureau N. How to establish an effective midline program : case of 2 hospitals. J of the Asso. For Vascular Access. 2015; 20(3) pp. 179 -188. 2. Infusion Nurses Society. Infusion Therapy Standards of practice. J. of Infus. Nurs. 2016; 39 (1 suppl): S 51 -S 54. 3. Davis M. Pediatric central venous catheter management : a review of current practice. J of the Asso. For Vascular Access. 2014; 18(2) pp. 93 -98. 4. Ast D. Ast T. Nonthrombotic complications related to central vascular access devices. J of Infus Nurs. 2014; 37(5): 349 -358. 5. Doellman D. Prevention, assessment, and treatment of central venous catheter occlusions in neonatal and young pediatric patients. J Infus Nurs. 2011; 34 (4): 251 -258. 6. Ullman A. Cooke M. Rickard C. Examining the role of securement and dressing products to prevent central venous access device failure: A narrative review. J of the Asso. For Vascular Access. 2015; 20(2): 99 -110. 7. Zerla P. Canelli A. Caravella G. et. Al. Open vs. closed-tip valved peripherally inserted central catheters and midlines: findings from a vascular access database. J of the Asso. For Vascular Access. 2015; 20 (3) : 169 -176. 58

Questions? PAGE 59
- Slides: 60