MANAGEMENT OF BARRETTS OESOPHAGUS Joint Hospital Surgical Grand
MANAGEMENT OF BARRETT’S OESOPHAGUS Joint Hospital Surgical Grand Round United Christian Hospital Dr C Leung
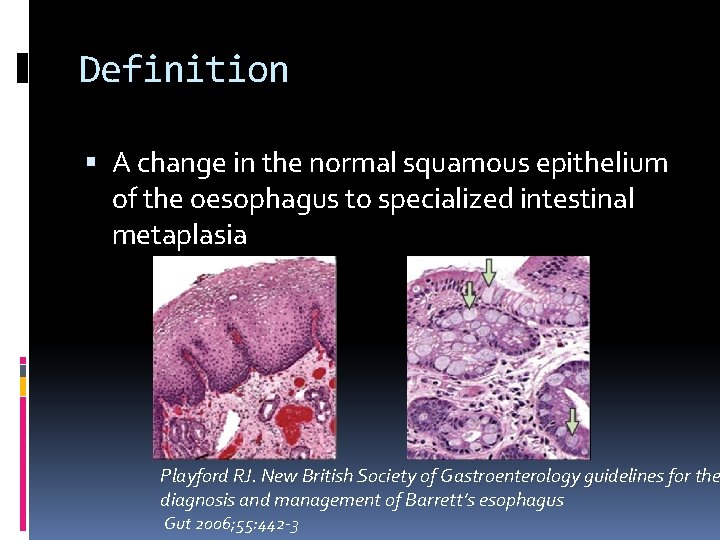
Definition A change in the normal squamous epithelium of the oesophagus to specialized intestinal metaplasia Playford RJ. New British Society of Gastroenterology guidelines for the diagnosis and management of Barrett’s esophagus Gut 2006; 55: 442 -3
Background Prevalence � 1. 6 -5. 6% � 10 -15% in patients with reflux symptoms Premalignant condition � 30 -40 fold increased risk of oesophageal CA
Etiology Combined acid and bile reflux > 50% of patients with GERD had abnormal levels of acid and bile in the oesophagus Barrett’s esophagus patients have the highest level Fein M. Br J Surg 2006; 93: 1475 -82
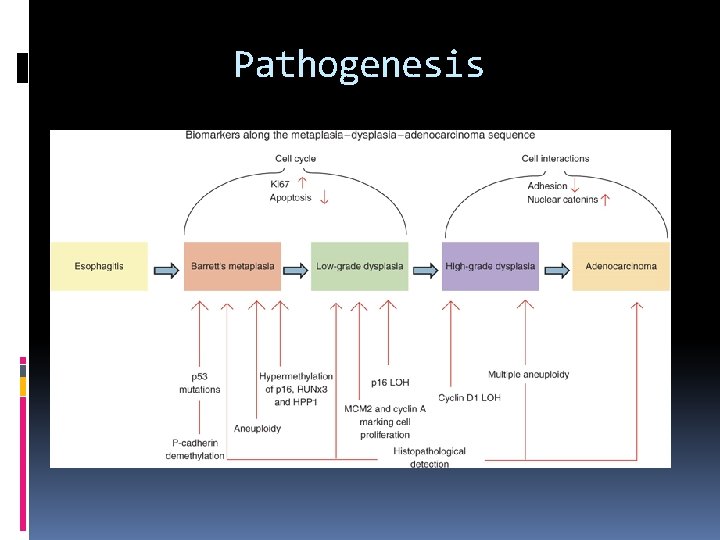
Pathogenesis
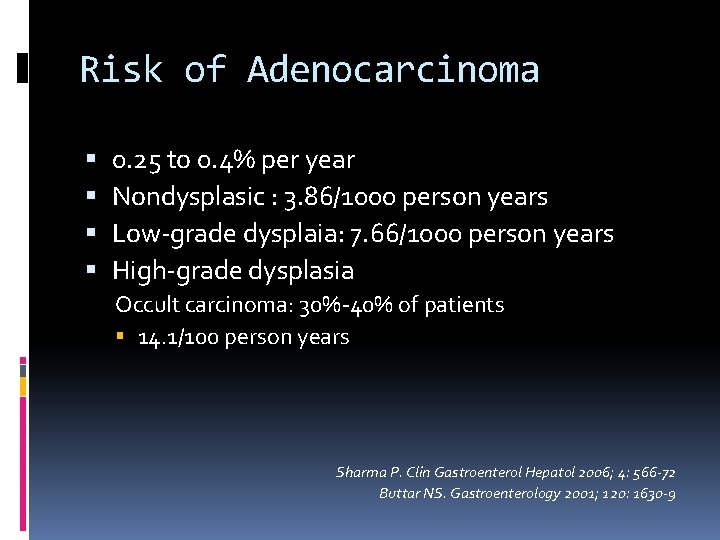
Risk of Adenocarcinoma 0. 25 to 0. 4% per year Nondysplasic : 3. 86/1000 person years Low-grade dysplaia: 7. 66/1000 person years High-grade dysplasia Occult carcinoma: 30%-40% of patients 14. 1/100 person years Sharma P. Clin Gastroenterol Hepatol 2006; 4: 566 -72 Buttar NS. Gastroenterology 2001; 120: 1630 -9
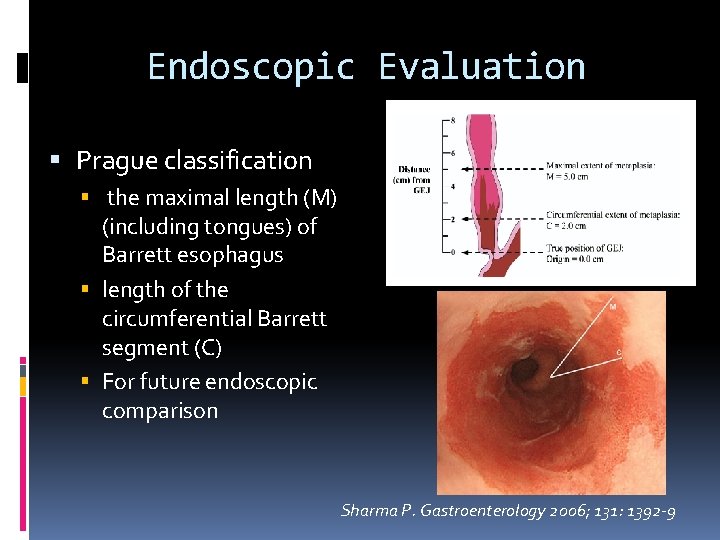
Endoscopic Evaluation Prague classification the maximal length (M) (including tongues) of Barrett esophagus length of the circumferential Barrett segment (C) For future endoscopic comparison Sharma P. Gastroenterology 2006; 131: 1392 -9
Biopsies Seattle protocol 4 quadrant jumbo bx at 1 cm intervals throughout whole length of Barrett’s Separate target bx of any irregularities (nodules/erythema/ erosions) Reid BJ. Am J Gastroenterol 2000; 95: 3089 -95.
Treatment rationale Removal of diseased mucosa, not entire organ Prevent disease progression to adeno. CA
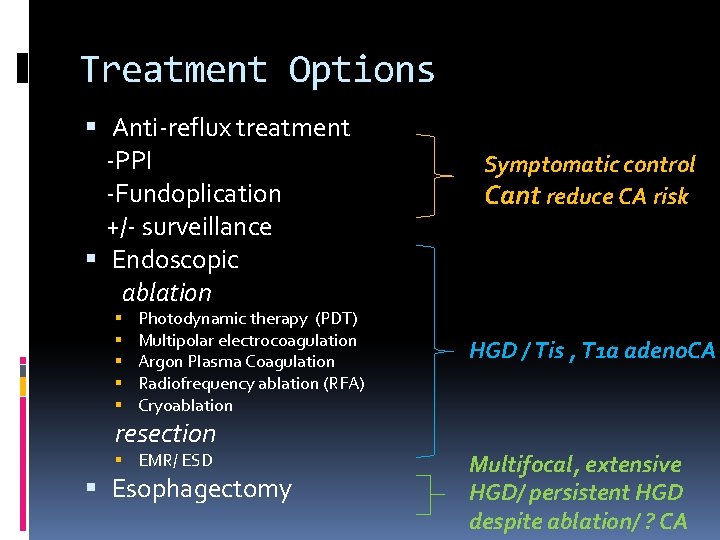
Treatment Options Anti-reflux treatment -PPI -Fundoplication +/- surveillance Endoscopic ablation Photodynamic therapy (PDT) Multipolar electrocoagulation Argon Plasma Coagulation Radiofrequency ablation (RFA) Cryoablation resection EMR/ ESD Esophagectomy Symptomatic control Cant reduce CA risk HGD / Tis , T 1 a adeno. CA Multifocal, extensive HGD/ persistent HGD despite ablation/ ? CA
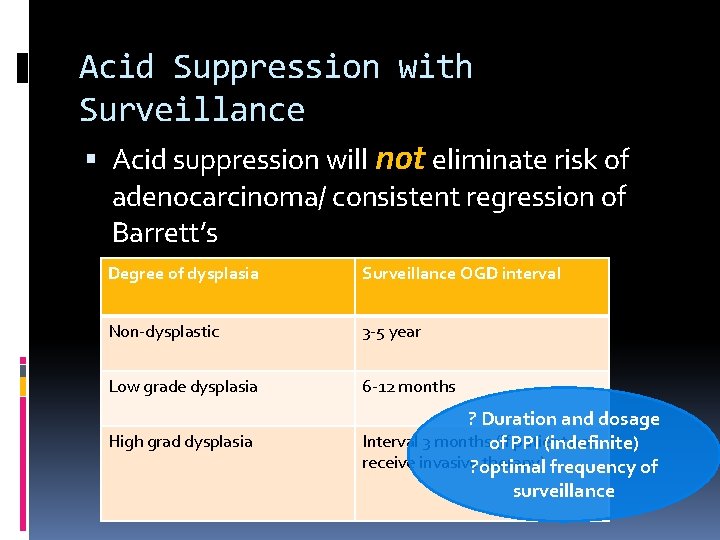
Acid Suppression with Surveillance Acid suppression will not eliminate risk of adenocarcinoma/ consistent regression of Barrett’s Degree of dysplasia Surveillance OGD interval Non-dysplastic 3 -5 year Low grade dysplasia 6 -12 months High grad dysplasia ? Duration and dosage Interval 3 monthsof (if PPI patient not (indefinite) receive invasive? optimal therapy) frequency of surveillance
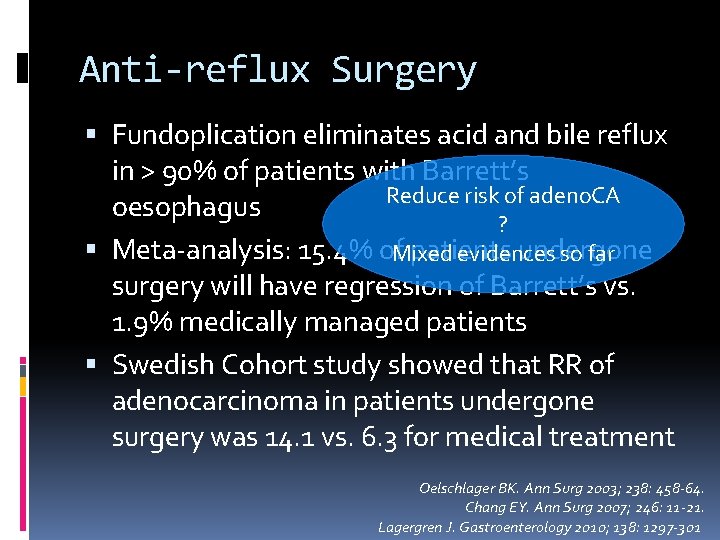
Anti-reflux Surgery Fundoplication eliminates acid and bile reflux in > 90% of patients with Barrett’s Reduce risk of adeno. CA oesophagus ? Meta-analysis: 15. 4% of. Mixed patients undergone evidences so far surgery will have regression of Barrett’s vs. 1. 9% medically managed patients Swedish Cohort study showed that RR of adenocarcinoma in patients undergone surgery was 14. 1 vs. 6. 3 for medical treatment Oelschlager BK. Ann Surg 2003; 238: 458 -64. Chang EY. Ann Surg 2007; 246: 11 -21. Lagergren J. Gastroenterology 2010; 138: 1297 -301
PPI vs fundoplication Surgery can definitely treat reflux-related symptoms, but its role in protection against adenocarcinoma should be cautious Effectiveness in eliminating reflux symptoms Co- morbidities Patient’s choice/ compliance Medications S/E
Photodynamic Therapy Injecting a light-sensitizing drug into patient, then expose the portion of oesophagus to a specific wavelength Found NOT effective in eliminating Barrett’s ‘Buried glands’: a layer of normal-appearing squamous epithelium is present but under this layer, Barret’s metaplasia still present Stricture Phototoxicity Menon D. BMC Gastroenterol 2010; 10: 111.
Argon Plasma Coagulation Systemic review: more effective than PDT, 3 month complete eradication 80% Less complications like stricture or bleeding Odynophagia 10% Li YM. Dig Dis Sci 2008; 53: 2837 -46.
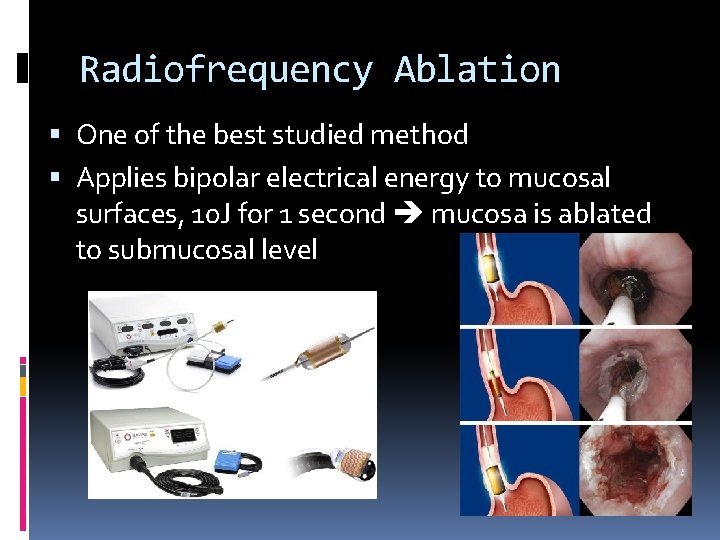
Radiofrequency Ablation One of the best studied method Applies bipolar electrical energy to mucosal surfaces, 10 J for 1 second mucosa is ablated to submucosal level
Radiofrequency ablation Need standardized FU as complete ablation with single treatment in only 70% of patients FU OGD 3 months and 1 year, if not complete ablated repeat RFA
Radiofrequency ablation Shaheen NJ (2009): Multicentre RCT Can eliminate Barrett’s oesophagus with high grade dysplasia and reduce risk of oesophageal carcinoma Wani S (2009): Meta-analysis Reduction in carcinoma progression in high-grade dysplasia Shaheen NJ (2011): Long term results 3 years follow-up: complete eradication persist in 96% patients with high-grade dysplaia Adenocarcinoma occurred in one per 181 patientyears of follow-up
Radiofrequency ablation Promising results S/E : esophageal stricture, GIB, chest pain Sustaintially lower than those in photodynamic therapy Long term data needed
Cryoablation Endoscopically directed spray of liquid nitrogen at -196 o. C Complete eradication of high grade dysplasia occurs in 68 -97% of patients Not well studied as RFA ? Treat patient refractory to RFA Dumot JA. Gastrointest Endosc 2009; 70: 635 -44. Shaheen NJ. Gastrointest Endosc 2010; 71: 680 -5.
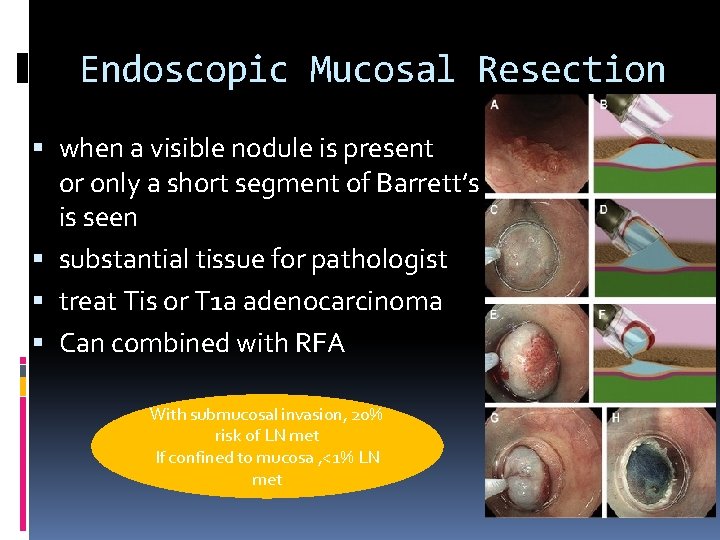
Endoscopic Mucosal Resection when a visible nodule is present or only a short segment of Barrett’s is seen substantial tissue for pathologist treat Tis or T 1 a adenocarcinoma Can combined with RFA With submucosal invasion, 20% risk of LN met If confined to mucosa , <1% LN met
Endoscopic therapy No single endotherapy achieve complete eradication without complications Recurrence For mucosal lesion Buried metaplasia
Esophagectomy ‘gold standard’ for high grade dysplasia and early adenocarinoma 20 -40% of patients harbour early adenocarcinoma in HGD (old data) Mortality can be as low as 1% in high vol centre Significant morbidity For multifocal , too extensive HGD / intractable HGD /suspicious of carcinoma
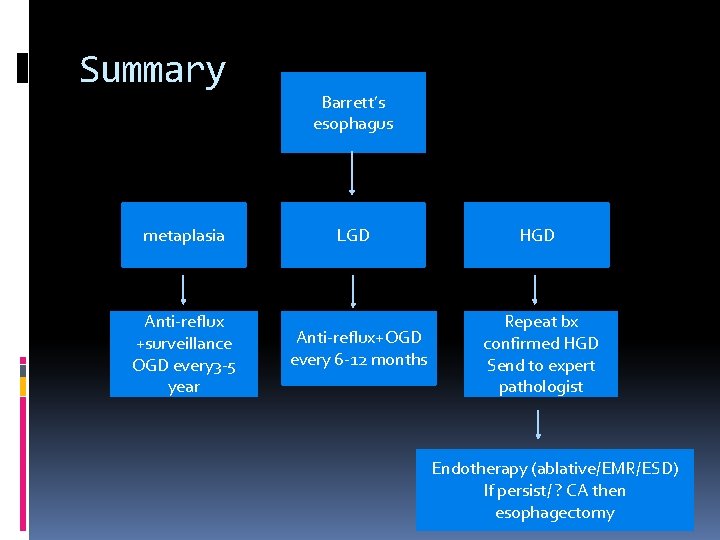
Summary metaplasia Anti-reflux +surveillance OGD every 3 -5 year Barrett’s esophagus LGD Anti-reflux+OGD every 6 -12 months HGD Repeat bx confirmed HGD Send to expert pathologist Endotherapy (ablative/EMR/ESD) If persist/ ? CA then esophagectomy
Take Home Messages Barrett’s esophagus is a pre-malignant condition Diagnosis relies on both endoscopic and histological findings Management should be based on risks stratification Emerging evidence on the use of endoscopic therapy Treatment should be individualized
- Slides: 25