MANAGEMENT OF ATYPICAL MELANOCYTIC PROLIFERATIONS A RETROSPECTIVE REVIEW
- Slides: 1
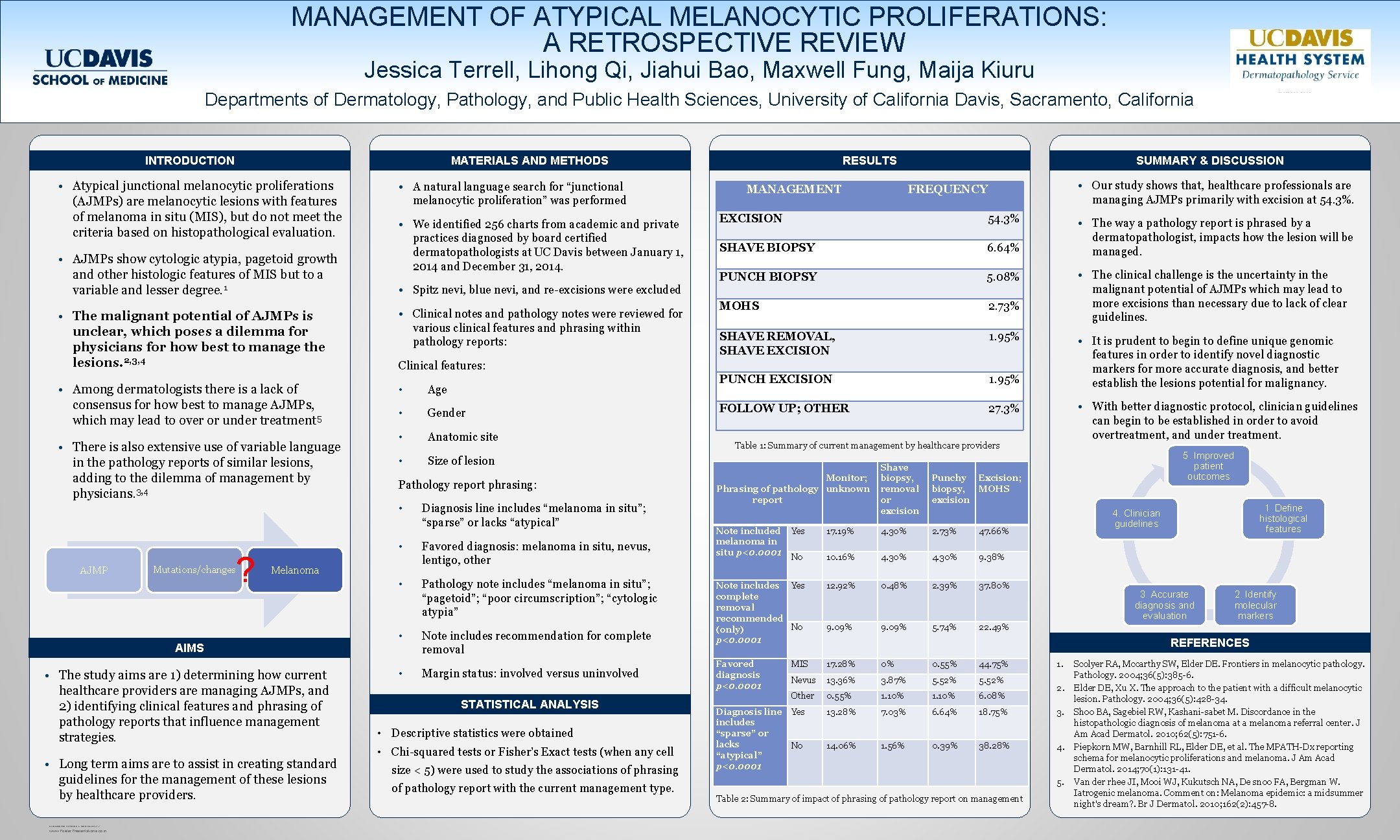
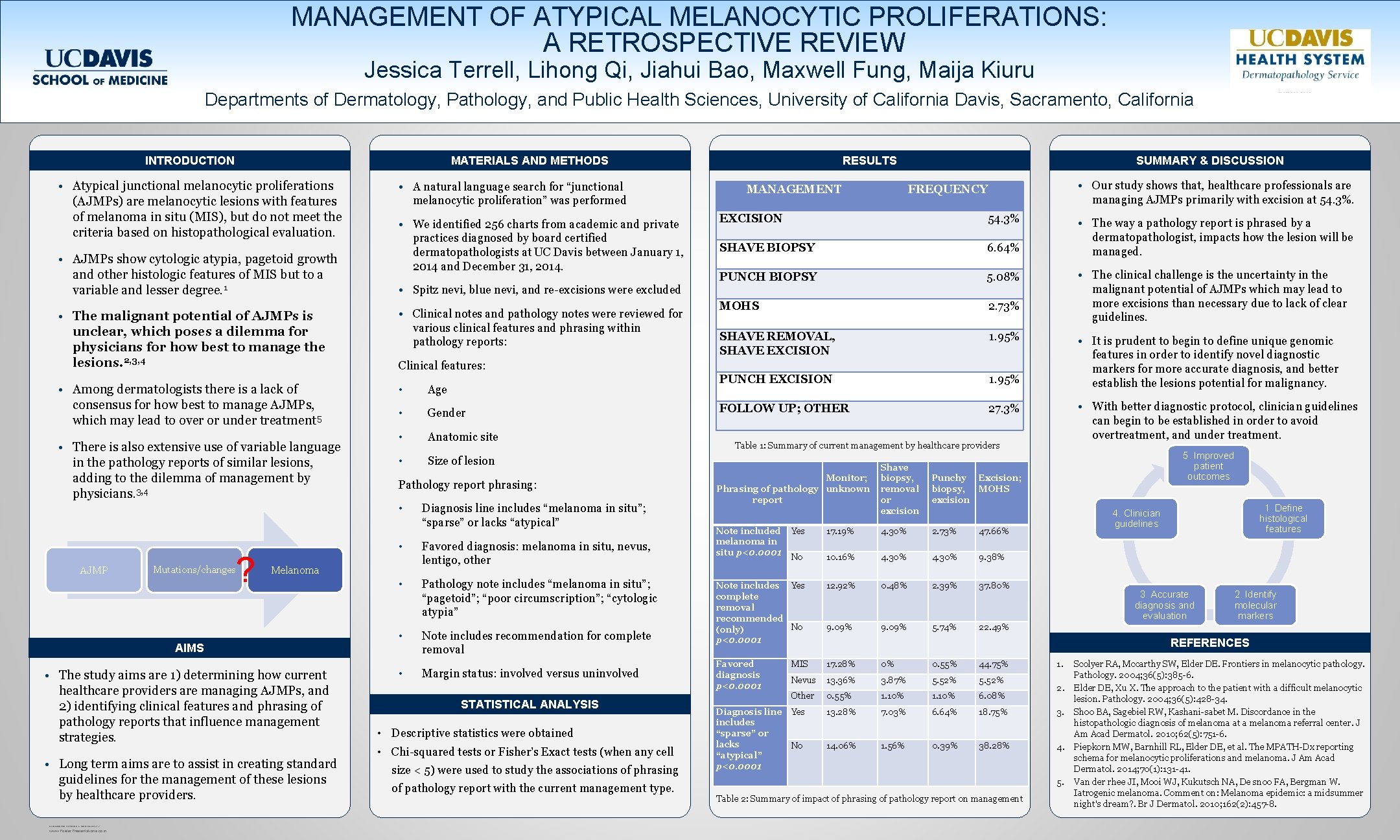
MANAGEMENT OF ATYPICAL MELANOCYTIC PROLIFERATIONS: A RETROSPECTIVE REVIEW Jessica Terrell, Lihong Qi, Jiahui Bao, Maxwell Fung, Maija Kiuru Departments of Dermatology, Pathology, and Public Health Sciences, University of California Davis, Sacramento, California INTRODUCTION MATERIALS AND METHODS • Atypical junctional melanocytic proliferations (AJMPs) are melanocytic lesions with features of melanoma in situ (MIS), but do not meet the criteria based on histopathological evaluation. • AJMPs show cytologic atypia, pagetoid growth and other histologic features of MIS but to a variable and lesser degree. 1 • The malignant potential of AJMPs is unclear, which poses a dilemma for physicians for how best to manage the lesions. 2, 3, 4 • Among dermatologists there is a lack of consensus for how best to manage AJMPs, which may lead to over or under treatment 5 • There is also extensive use of variable language in the pathology reports of similar lesions, adding to the dilemma of management by physicians. 3, 4 • A natural language search for “junctional melanocytic proliferation” was performed • We identified 256 charts from academic and private practices diagnosed by board certified dermatopathologists at UC Davis between January 1, 2014 and December 31, 2014. • Spitz nevi, blue nevi, and re-excisions were excluded • Clinical notes and pathology notes were reviewed for various clinical features and phrasing within pathology reports: Mutations/changes ? • Age • Gender • Anatomic site • Size of lesion Pathology report phrasing: • The study aims are 1) determining how current healthcare providers are managing AJMPs, and 2) identifying clinical features and phrasing of pathology reports that influence management strategies. • Long term aims are to assist in creating standard guidelines for the management of these lesions by healthcare providers. RESEARCH POSTER PRESENTATION DESIGN © 2012 www. Poster. Presentations. com Diagnosis line includes “melanoma in situ”; “sparse” or lacks “atypical” • Favored diagnosis: melanoma in situ, nevus, lentigo, other • Pathology note includes “melanoma in situ”; “pagetoid”; “poor circumscription”; “cytologic atypia” • Note includes recommendation for complete removal Melanoma AIMS MANAGEMENT SUMMARY & DISCUSSION • Our study shows that, healthcare professionals are managing AJMPs primarily with excision at 54. 3%. FREQUENCY EXCISION 54. 3% SHAVE BIOPSY 6. 64% PUNCH BIOPSY 5. 08% MOHS 2. 73% SHAVE REMOVAL, SHAVE EXCISION 1. 95% PUNCH EXCISION 1. 95% FOLLOW UP; OTHER 27. 3% • The way a pathology report is phrased by a dermatopathologist, impacts how the lesion will be managed. • The clinical challenge is the uncertainty in the malignant potential of AJMPs which may lead to more excisions than necessary due to lack of clear guidelines. • It is prudent to begin to define unique genomic features in order to identify novel diagnostic markers for more accurate diagnosis, and better establish the lesions potential for malignancy. Clinical features: • AJMP RESULTS • Margin status: involved versus uninvolved STATISTICAL ANALYSIS • Descriptive statistics were obtained • Chi-squared tests or Fisher’s Exact tests (when any cell size < 5) were used to study the associations of phrasing of pathology report with the current management type. • With better diagnostic protocol, clinician guidelines can begin to be established in order to avoid overtreatment, and under treatment. Table 1: Summary of current management by healthcare providers Monitor; Phrasing of pathology unknown report Note included melanoma in situ p<0. 0001 Shave biopsy, removal or excision Punchy Excision; biopsy, MOHS excision 5. Improved patient outcomes 1. Define histological features 4. Clinician guidelines Yes 17. 19% 4. 30% 2. 73% 47. 66% No 10. 16% 4. 30% 9. 38% Note includes Yes complete removal recommended No (only) p<0. 0001 12. 92% 0. 48% 2. 39% 37. 80% 9. 09% 5. 74% 22. 49% Favored diagnosis p<0. 0001 MIS 17. 28% 0% 0. 55% 44. 75% Nevus 13. 36% 3. 87% 5. 52% Other 0. 55% 1. 10% 6. 08% Diagnosis line includes “sparse” or lacks “atypical” p<0. 0001 Yes 13. 28% 7. 03% 6. 64% 18. 75% 3. No 14. 06% 1. 56% 0. 39% 38. 28% 4. 3. Accurate diagnosis and evaluation 2. Identify molecular markers REFERENCES 1. 2. 5. Table 2: Summary of impact of phrasing of pathology report on management Scolyer RA, Mccarthy SW, Elder DE. Frontiers in melanocytic pathology. Pathology. 2004; 36(5): 385 -6. Elder DE, Xu X. The approach to the patient with a difficult melanocytic lesion. Pathology. 2004; 36(5): 428 -34. Shoo BA, Sagebiel RW, Kashani-sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center. J Am Acad Dermatol. 2010; 62(5): 751 -6. Piepkorn MW, Barnhill RL, Elder DE, et al. The MPATH-Dx reporting schema for melanocytic proliferations and melanoma. J Am Acad Dermatol. 2014; 70(1): 131 -41. Van der rhee JI, Mooi WJ, Kukutsch NA, De snoo FA, Bergman W. Iatrogenic melanoma. Comment on: Melanoma epidemic: a midsummer night's dream? . Br J Dermatol. 2010; 162(2): 457 -8.