Management of Atrial Fibrillation Preoperative and Perioperative Considerations
Management of Atrial Fibrillation: Pre-operative and Peri-operative Considerations An Update from the 2014 AHA/ACC/HRS Guidelines Anesthesiology Grand Rounds Department of Anesthesia, Albany Medical Center October 23, 2014 Mandeep S. Sidhu, MD, MBA, FACC Assistant Professor of Medicine, Albany Medical College Adjunct Assistant Professor of Management, Union Graduate College Co-Investigator, Faculty and Regional Co-Leader, ISCHEMIA Trial
Conflict of Interest: None • Disclosures: – Clinical Coordinating Center u NHLBI Funding: ISCHEMIA Trial Faculty, Clinical Coordinating Center Satellite with NYU Medical Center Co-Investigator and Co-Regional Leader of North Region(USA) u Industry Funding: Amgen for FOURIER Trial u u u Fellow, American College of Cardiology Board Member, Capital Region AHA/ASA Board of Advisors. Member, Heart Rhythm Society Member, American Heart and Stroke Association Member, AHA/ASA Atrial Fibrillation GWTG Clinical Working Group/Committee Adjunct Faculty, Health Care Management MD/MS/MBA program, School of Management, Union Graduate College
Agenda • Outline – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
Most Recent US Guidelines… March 2014
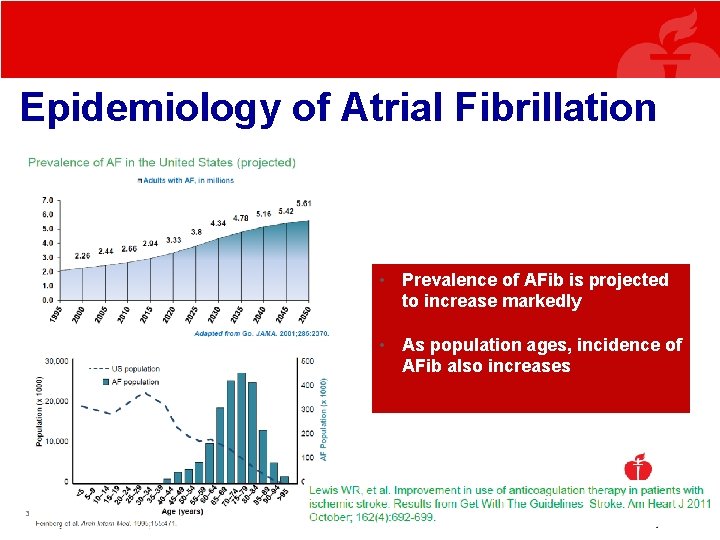
Epidemiology of Atrial Fibrillation • Prevalence of AFib is projected to increase markedly • As population ages, incidence of AFib also increases 3/9/2021 © 2013, American Heart Association 5
Epidemiology of Atrial Fibrillation Continued • Prevalence: 2. 7 to 6. 1 million in 2010 (8% in those over 80 years) • Incidence: – 0. 2%/year (15 -44 yrs) – 1. 1%/year (> 80 yrs) • As the population ages, this number will increase and especially with rise in CAD, DM, HTN, and obesity/OSA. Go et al. Heart Disease and Stroke Statistics−− 2013, Circulation 2013
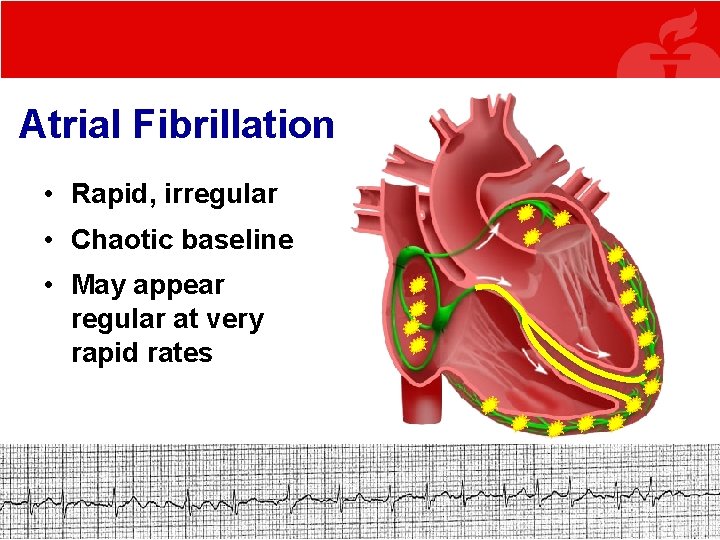
Atrial Fibrillation • Rapid, irregular • Chaotic baseline • May appear regular at very rapid rates
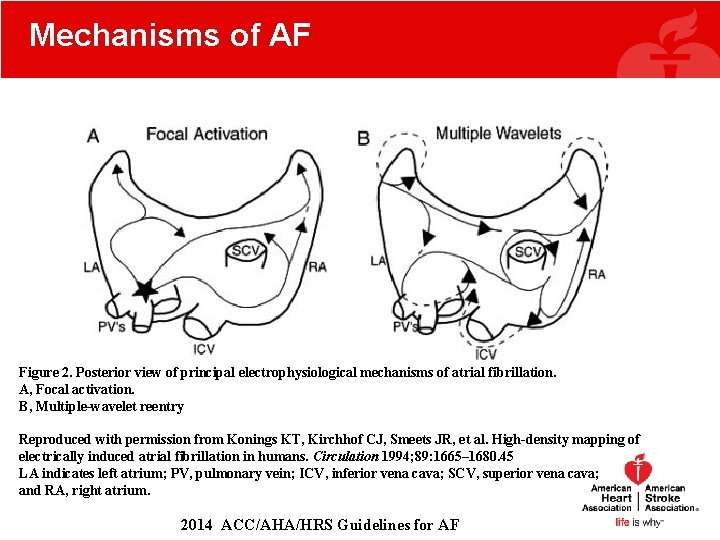
Mechanisms of AF Figure 2. Posterior view of principal electrophysiological mechanisms of atrial fibrillation. A, Focal activation. B, Multiple-wavelet reentry Reproduced with permission from Konings KT, Kirchhof CJ, Smeets JR, et al. High-density mapping of electrically induced atrial fibrillation in humans. Circulation 1994; 89: 1665– 1680. 45 LA indicates left atrium; PV, pulmonary vein; ICV, inferior vena cava; SCV, superior vena cava; and RA, right atrium. 2014 ACC/AHA/HRS Guidelines for AF
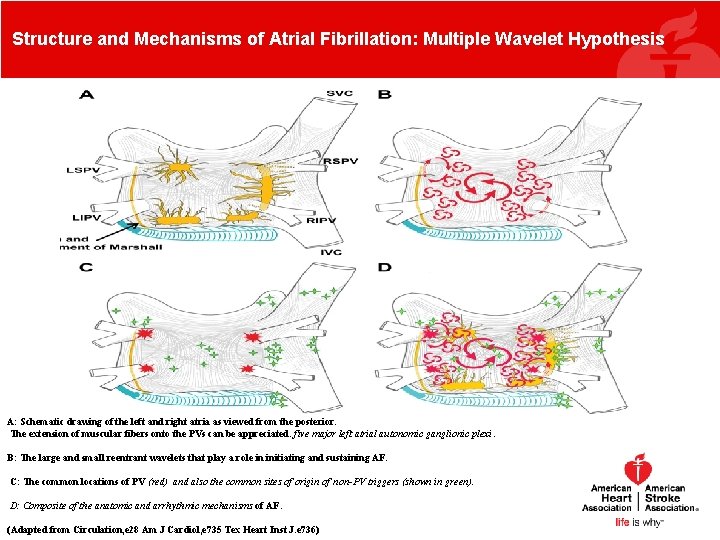
Structure and Mechanisms of Atrial Fibrillation: Multiple Wavelet Hypothesis A: Schematic drawing of the left and right atria as viewed from the posterior. The extension of muscular fibers onto the PVs can be appreciated. five major left atrial autonomic ganglionic plexi. B: The large and small reentrant wavelets that play a role in initiating and sustaining AF. C: The common locations of PV (red) and also the common sites of origin of non-PV triggers (shown in green). D: Composite of the anatomic and arrhythmic mechanisms of AF. (Adapted from Circulation, e 28 Am J Cardiol, e 735 Tex Heart Inst J. e 736)
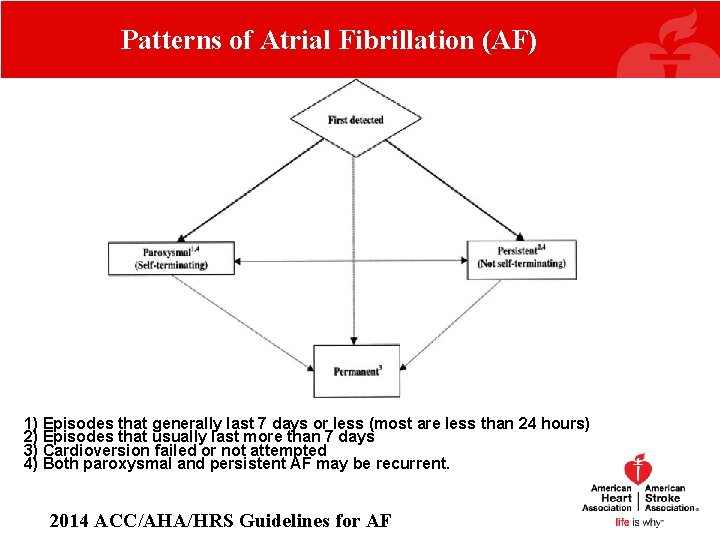
Patterns of Atrial Fibrillation (AF) 1) Episodes that generally last 7 days or less (most are less than 24 hours) 2) Episodes that usually last more than 7 days 3) Cardioversion failed or not attempted 4) Both paroxysmal and persistent AF may be recurrent. 2014 ACC/AHA/HRS Guidelines for AF
Agenda • Outline – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
Assessment of Stroke Risk: Use CHA 2 DS 2 -VASc In assessing risk of stroke in a patient with nonvalvular AF, CHA 2 DS 2 -VASc should be used, as opposed to the CHADS 2 score. (Class I recommendation)
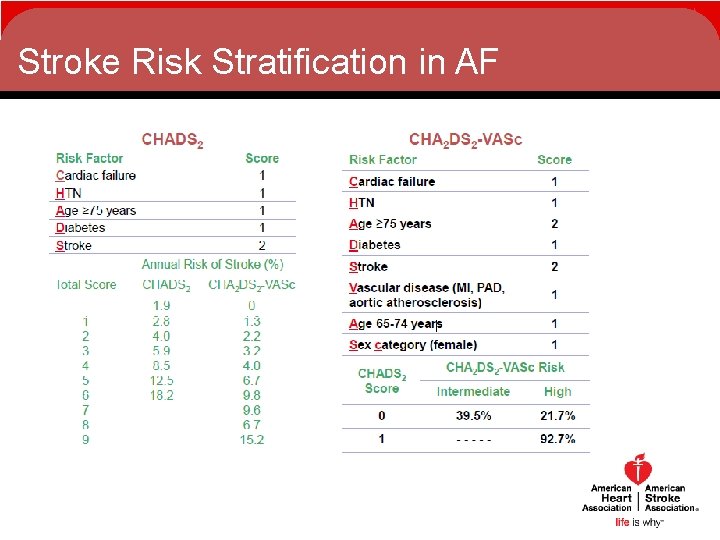
Stroke Risk Stratification in AF
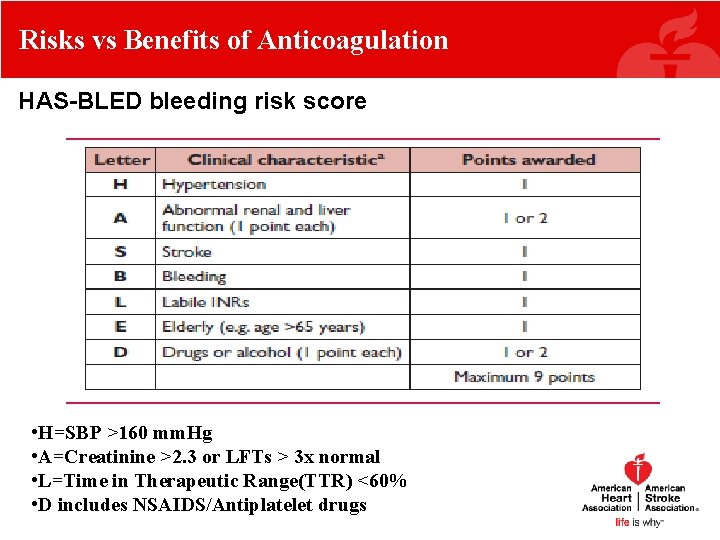
Risks vs Benefits of Anticoagulation HAS-BLED bleeding risk score • H=SBP >160 mm. Hg • A=Creatinine >2. 3 or LFTs > 3 x normal • L=Time in Therapeutic Range(TTR) <60% • D includes NSAIDS/Antiplatelet drugs
Recommendations for Oral Anticoagulation For nonvalvular AF patients with a history of stroke or transient ischemic attack, or a CHA 2 DS 2 -VASc score ≥ 2, oral anticoagulation is recommended (Class I). Options for oral anticoagulation include warfarin, dabigatran, rivaroxaban, and apixaban.
CHA 2 DS 2 -VASc score = 0 For patients with nonvalvular AF and a CHA 2 DS 2 -VASc score of 0, it is reasonable to omit antithrombotic therapy (Class IIa).
CHA 2 DS 2 -VASc score = 1 In a patient with nonvalvular AF and a CHA 2 DS 2 -VASc score of 1, options for treatment include (Class IIb recommendation): o No antithrombotic therapy o Oral anticoagulation o Aspirin
Prosthetic Heart Valves with AF None of the new novel oral anticoagulants (dabigatran, rivaroxaban, or apixaban) are recommended to be used in patients with AF and a mechanical or bioprosthetic heart valve (Class III harm).
Hypertrophic Cardiomyopathy Oral anticoagulation should be prescribed to patients with hypertrophic cardiomyopathy and AF irrespective of the CHA 2 DS 2 -VASc score (Class I).
Bridging Therapy • Bridging therapy with low molecular weight heparin or unfractionated heparin is recommended if warfarin is interrupted in a patient with a mechanical heart valve and AF. Bridging therapy should balance risks of stroke and bleeding. (Class I, LOE C) • Without a mechanical heart valve, bridging therapy decisions should balance stroke and bleeding risks against the duration of time patient will not be anticoagulated. (Class I, LOE C)
Other Class I/IIa Recommendations Related to Anticoagulation • In atrial flutter, antithrombotic therapy is recommended as for AF (Class I-LOE C) • With CHA 2 DS 2 -VASc score ≥ 2 and end-stage CKD (Cr. Cl <15 m. L/min) or on hemodialysis, it is reasonable to prescribe warfarin for oral anticoagulation. (Class IIa, LOE B) • Evaluate renal function prior to initiation of direct thrombin or factor Xa inhibitors, and re-evaluate when clinically indicated and at least annually. (Class I, LOE B)
Recommendations for Patients Who Undergo PCI • For PCI in AF patients, Bare Metal Stenting(BMS) may be considered to minimize the duration of dual antiplatelet therapy. (Class IIb, LOE C) • Following coronary revascularization in patients with AF CHA 2 DS 2 -VASc score of ≥ 2, it may be reasonable to use clopidogrel concurrently with oral anticoagulants, but without aspirin. (Class IIb, LOE C)
Agenda • Outline – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
Rate Control A strict rate control strategy (<80 bpm) in patients with persistent/permanent AF is recommended (Class IIa). A single randomized controlled trial (RACE) suggested that a lenient (<110 bpm) rate control strategy was as effective as more stringent rate control, but the guidelines committee determined that these results were not definitive.
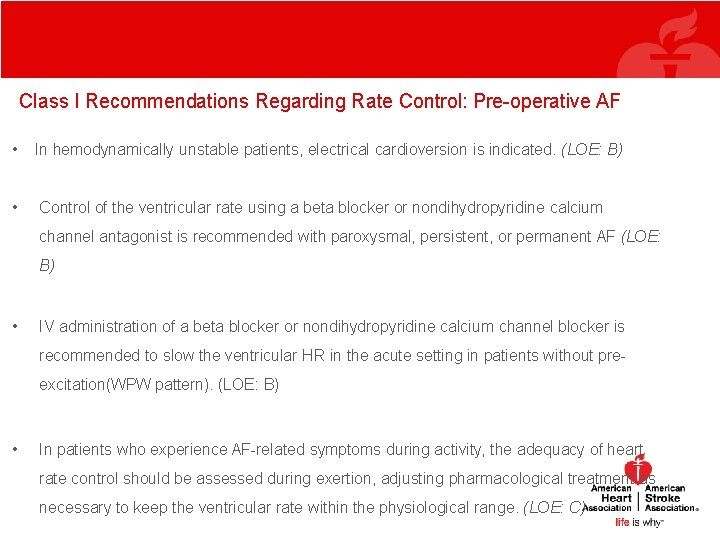
Class I Recommendations Regarding Rate Control: Pre-operative AF • In hemodynamically unstable patients, electrical cardioversion is indicated. (LOE: B) • Control of the ventricular rate using a beta blocker or nondihydropyridine calcium channel antagonist is recommended with paroxysmal, persistent, or permanent AF (LOE: B) • IV administration of a beta blocker or nondihydropyridine calcium channel blocker is recommended to slow the ventricular HR in the acute setting in patients without preexcitation(WPW pattern). (LOE: B) • In patients who experience AF-related symptoms during activity, the adequacy of heart rate control should be assessed during exertion, adjusting pharmacological treatment as necessary to keep the ventricular rate within the physiological range. (LOE: C)
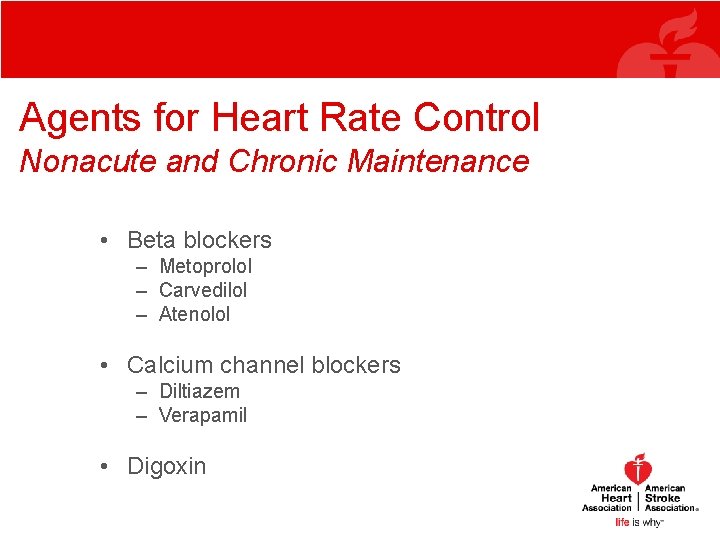
Agents for Heart Rate Control Nonacute and Chronic Maintenance • Beta blockers – Metoprolol – Carvedilol – Atenolol • Calcium channel blockers – Diltiazem – Verapamil • Digoxin
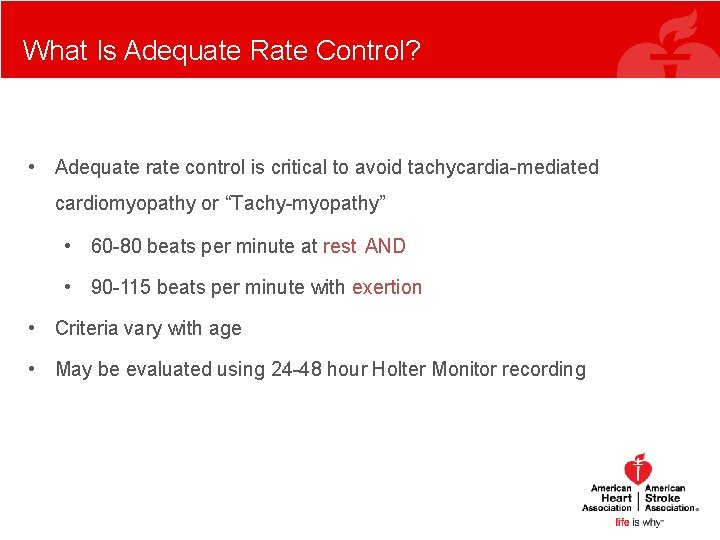
What Is Adequate Rate Control? • Adequate rate control is critical to avoid tachycardia-mediated cardiomyopathy or “Tachy-myopathy” • 60 -80 beats per minute at rest AND • 90 -115 beats per minute with exertion • Criteria vary with age • May be evaluated using 24 -48 hour Holter Monitor recording
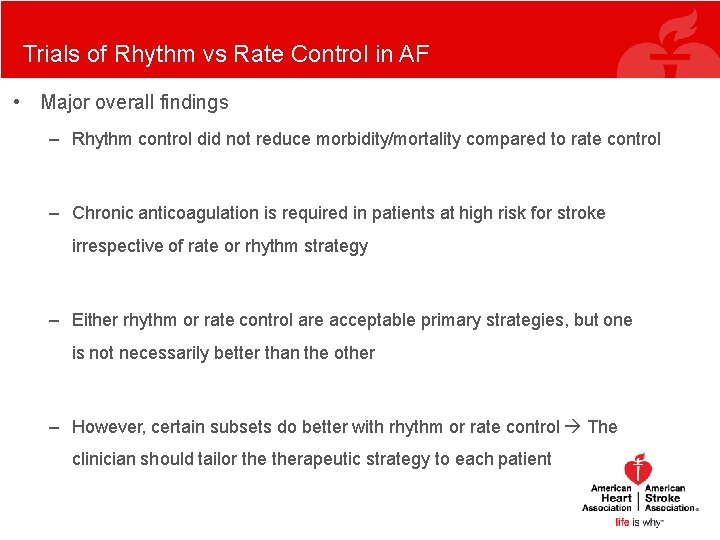
Trials of Rhythm vs Rate Control in AF • Major overall findings – Rhythm control did not reduce morbidity/mortality compared to rate control – Chronic anticoagulation is required in patients at high risk for stroke irrespective of rate or rhythm strategy – Either rhythm or rate control are acceptable primary strategies, but one is not necessarily better than the other – However, certain subsets do better with rhythm or rate control The clinician should tailor therapeutic strategy to each patient
Clinical Considerations for Management Strategy of Rate Versus Rhythm Control in AF • Duration and patterns of AF • Type and severity of symptoms • Associated cardiovascular disease • Potential for changes in cardiac function over time
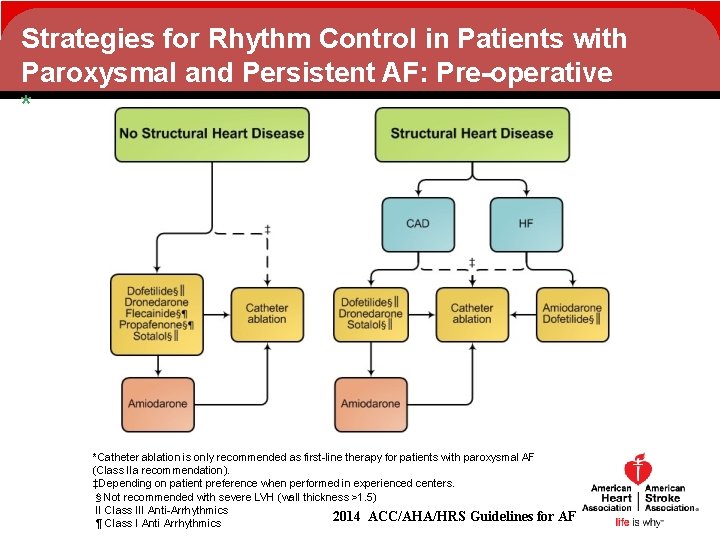
Strategies for Rhythm Control in Patients with Paroxysmal and Persistent AF: Pre-operative * *Catheter ablation is only recommended as first-line therapy for patients with paroxysmal AF (Class IIa recommendation). ‡Depending on patient preference when performed in experienced centers. §Not recommended with severe LVH (wall thickness >1. 5) c II Class III Anti-Arrhythmics 2014 ACC/AHA/HRS Guidelines for ¶ Class I Anti Arrhythmics AF
Left Ventricular Hypertrophy As in the earlier guidelines, the committee recommends against the use of certain antiarrhythmic medications (flecainide, propafenone, dofetilide, and sotalol) in patients with severe left ventricular hypertrophy (LVH). In the current guidelines, severe LVH is now defined as wall thickness exceeding 1. 5 cm.
Selection of AADs • AAD therapy needs to be tailored to each individual patient • Amiodarone – Second-line therapy for all AF patients; first-line with HF or HTN and LVH • Dofetilide – Second-line therapy for most AF patients except with HF and/or CAD – Not recommended in patients with HTN and LVH – Not effective and not approved for use in paroxysmal AF • Dronedarone, flecainide, propafenone, and sotalol – First-line in AF patients with HTN and no LVH or no heart disease – Dronedarone and sotalol recommended first-line in AF patients with CAD – Not recommended in AF patients with HTN and LVH or HF – Dronedarone should not be used in patients with permanent AF Wann LS, et al. Circulation. 2011; 123(1): 104 -123. Camm AJ, et al. Eur Heart J.
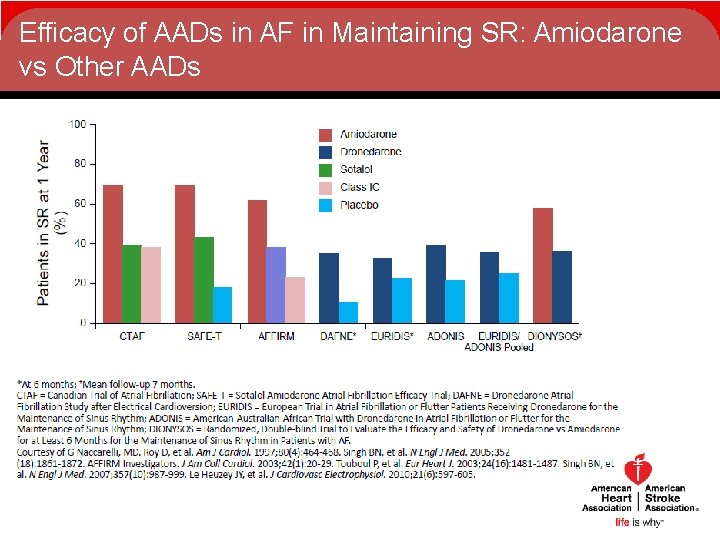
Efficacy of AADs in AF in Maintaining SR: Amiodarone vs Other AADs 100 Amiodaron e Patients in SR at 1 Year (%) 80 Dronedaron e Sotalol 60 Class IC Placeb o 40 20 0 CTAF SAFE-T AFFIRM DAFNE* EURIDIS* ADONIS EURIDIS/ DIONYSOS†
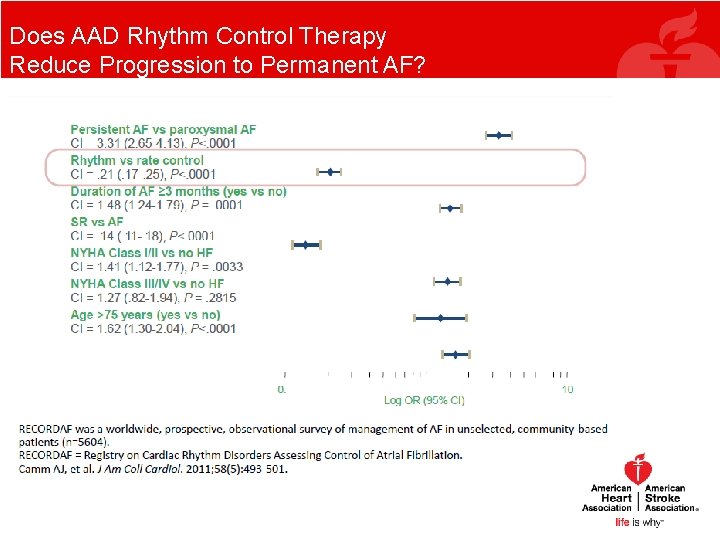
Does AAD Rhythm Control Therapy Reduce Progression to Permanent AF?
Agenda • Outline – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
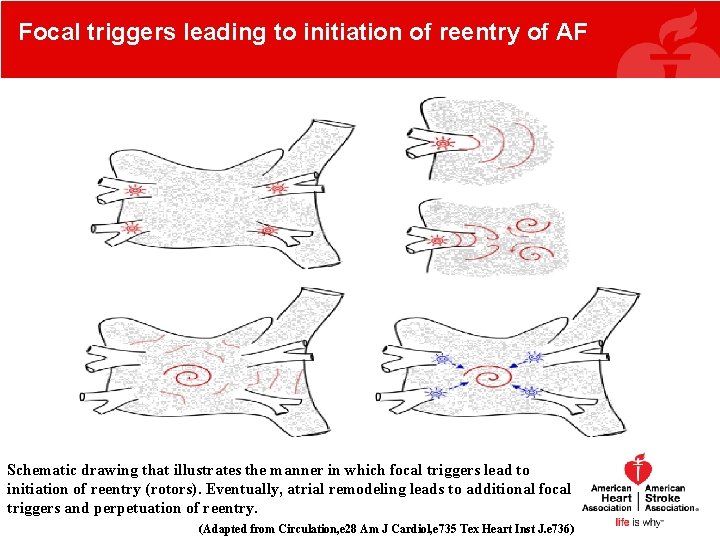
Focal triggers leading to initiation of reentry of AF Schematic drawing that illustrates the manner in which focal triggers lead to initiation of reentry (rotors). Eventually, atrial remodeling leads to additional focal triggers and perpetuation of reentry. (Adapted from Circulation, e 28 Am J Cardiol, e 735 Tex Heart Inst J. e 736)
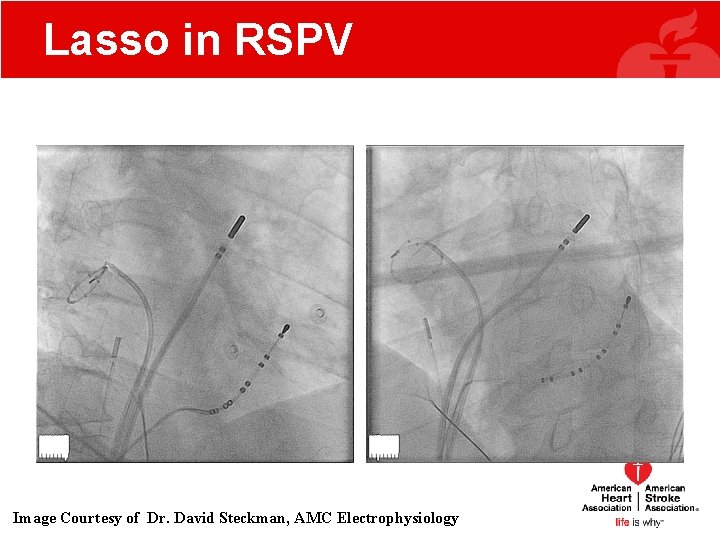
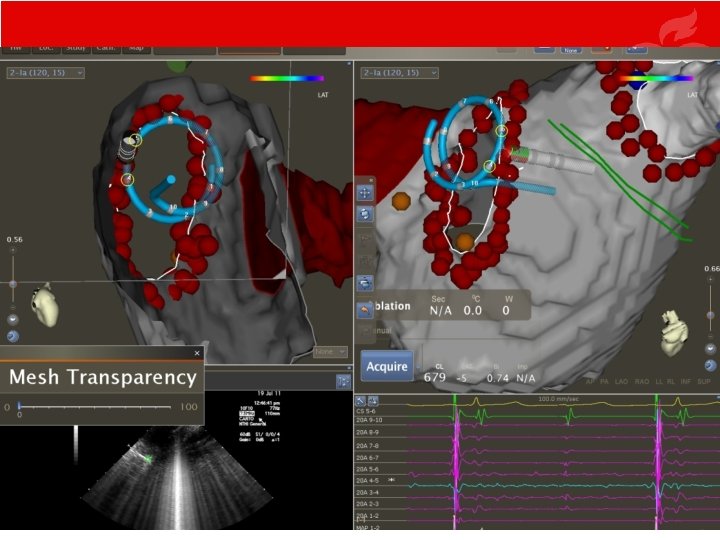
Lasso in RSPV RAO LAO Image Courtesy of Dr. David Steckman, AMC Electrophysiology
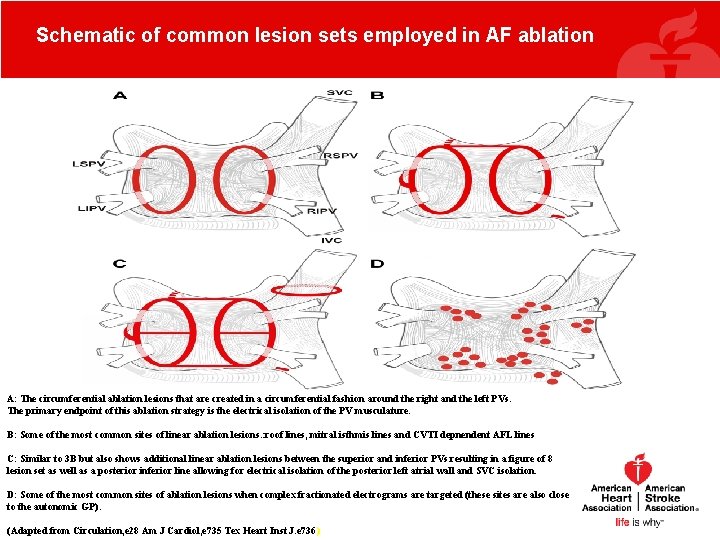
Schematic of common lesion sets employed in AF ablation A: The circumferential ablation lesions that are created in a circumferential fashion around the right and the left PVs. The primary endpoint of this ablation strategy is the electrical isolation of the PV musculature. B: Some of the most common sites of linear ablation lesions. : roof lines, mitral isthmis lines and CVTI depnendent AFL lines C: Similar to 3 B but also shows additional linear ablation lesions between the superior and inferior PVs resulting in a figure of 8 lesion set as well as a posterior inferior line allowing for electrical isolation of the posterior left atrial wall and SVC isolation. D: Some of the most common sites of ablation lesions when complex fractionated electrograms are targeted (these sites are also close to the autonomic GP). (Adapted from Circulation, e 28 Am J Cardiol, e 735 Tex Heart Inst J. e 736)
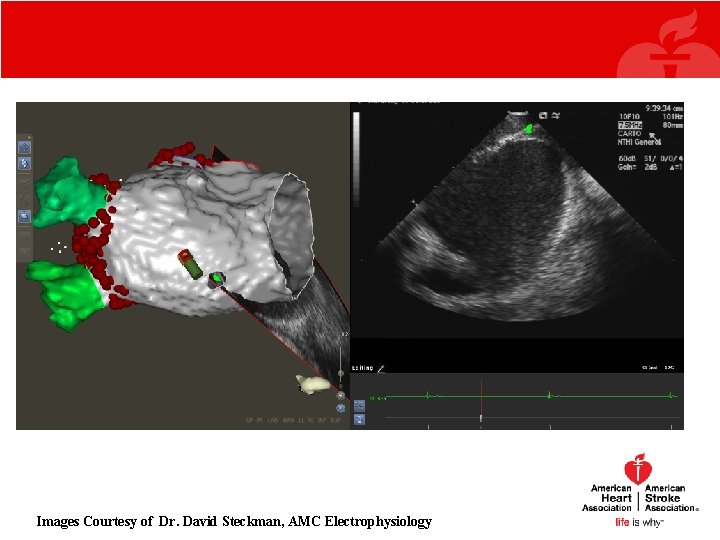
Images Courtesy of Dr. David Steckman, AMC Electrophysiology
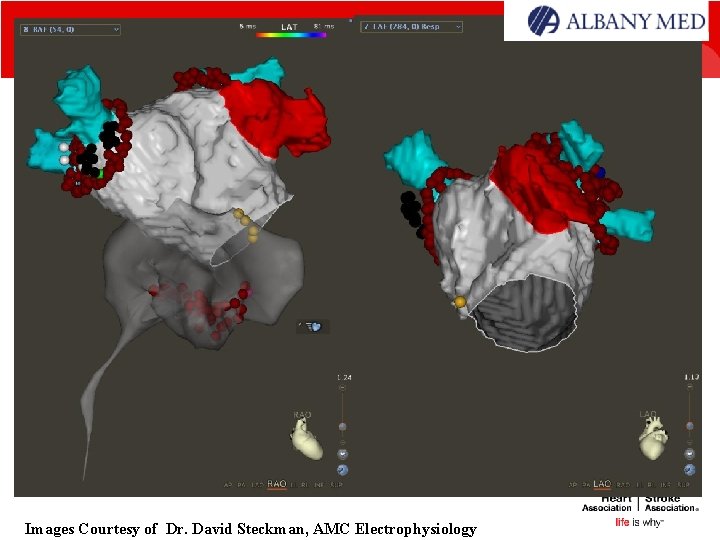
Images Courtesy of Dr. David Steckman, AMC Electrophysiology
Catheter Ablation Catheter ablation is useful in patients with symptomatic, paroxysmal AF who have not responded to or tolerated antiarrhythmic medications (Class I). This recommendation is the same as in the previous guideline.
Catheter Ablation • AF catheter ablation is reasonable for selected patients with symptomatic persistent AF refractory or intolerant to at least class I or III antiarrhythmic medication. (Class IIa, Level of Evidence: A) This recommendation is the same as in the previous guideline.
Catheter Ablation as First Line Therapy Catheter ablation is also reasonable in selected patients with symptomatic, paroxysmal AF prior to a trial of medical therapy, provided that it can be performed at an experienced center (Class IIa). This is a new recommendation.
Agenda • Outline – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
Peri-operative Arrhythmias • Increased morbidity, prolonged ICU stay and hospitalization with increased costs. • Data from several studies suggest incidence of postoperative arrhythmia after CT surgery is 30 -40% with post op AF as #1. • For non cardiothoracic procedures, the incidence ranges from 4 -20%, depending on type of surgery performed. • Bradyarrhythmias are also common after cardiac surgery and occur most frequently in the early postoperative period, and related to the fluctuation of vagal tone caused by direct surgical injury and local edema. Melduni RM, Koshino Y, Shen WK Mayo Clinic Proceedings 28(2012) 729 -743.
Peri-operative Arrhythmias • Initial management of patients with perioperative atrial arrhythmia depends on the hemodynamic effect on the clinical status. • First step is to eliminate any potential precipitating factors. • Multiple studies have demonstrated that BB reduces the risk of AF by up to 61% compared with placebo. Routine administration of beta blocker after CT surgery should be the standard of care to prevent AF. • Sustained monomorphic or polymorphic ventricular arrhythmias uncommon with approximately 1 -3% of patients usually within the first 7 days after surgery. Melduni RM, Koshino Y, Shen WK Mayo Clinic Proceedings 28(2012) 729 -743.
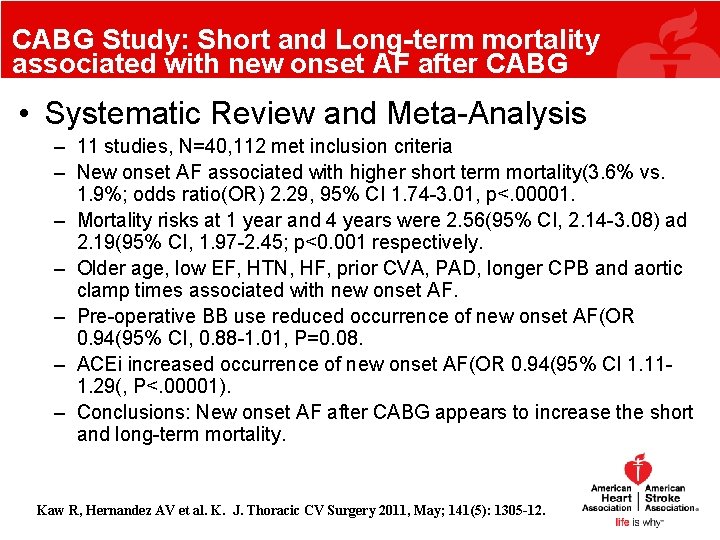
CABG Study: Short and Long-term mortality associated with new onset AF after CABG • Systematic Review and Meta-Analysis – 11 studies, N=40, 112 met inclusion criteria – New onset AF associated with higher short term mortality(3. 6% vs. 1. 9%; odds ratio(OR) 2. 29, 95% CI 1. 74 -3. 01, p<. 00001. – Mortality risks at 1 year and 4 years were 2. 56(95% CI, 2. 14 -3. 08) ad 2. 19(95% CI, 1. 97 -2. 45; p<0. 001 respectively. – Older age, low EF, HTN, HF, prior CVA, PAD, longer CPB and aortic clamp times associated with new onset AF. – Pre-operative BB use reduced occurrence of new onset AF(OR 0. 94(95% CI, 0. 88 -1. 01, P=0. 08. – ACEi increased occurrence of new onset AF(OR 0. 94(95% CI 1. 111. 29(, P<. 00001). – Conclusions: New onset AF after CABG appears to increase the short and long-term mortality. Kaw R, Hernandez AV et al. K. J. Thoracic CV Surgery 2011, May; 141(5): 1305 -12.
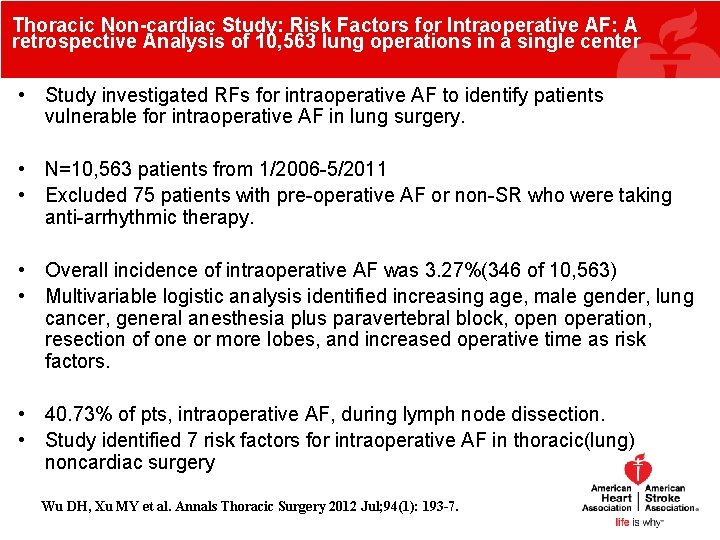
Thoracic Non-cardiac Study: Risk Factors for Intraoperative AF: A retrospective Analysis of 10, 563 lung operations in a single center • Study investigated RFs for intraoperative AF to identify patients vulnerable for intraoperative AF in lung surgery. • N=10, 563 patients from 1/2006 -5/2011 • Excluded 75 patients with pre-operative AF or non-SR who were taking anti-arrhythmic therapy. • Overall incidence of intraoperative AF was 3. 27%(346 of 10, 563) • Multivariable logistic analysis identified increasing age, male gender, lung cancer, general anesthesia plus paravertebral block, open operation, resection of one or more lobes, and increased operative time as risk factors. • 40. 73% of pts, intraoperative AF, during lymph node dissection. • Study identified 7 risk factors for intraoperative AF in thoracic(lung) noncardiac surgery Wu DH, Xu MY et al. Annals Thoracic Surgery 2012 Jul; 94(1): 193 -7.
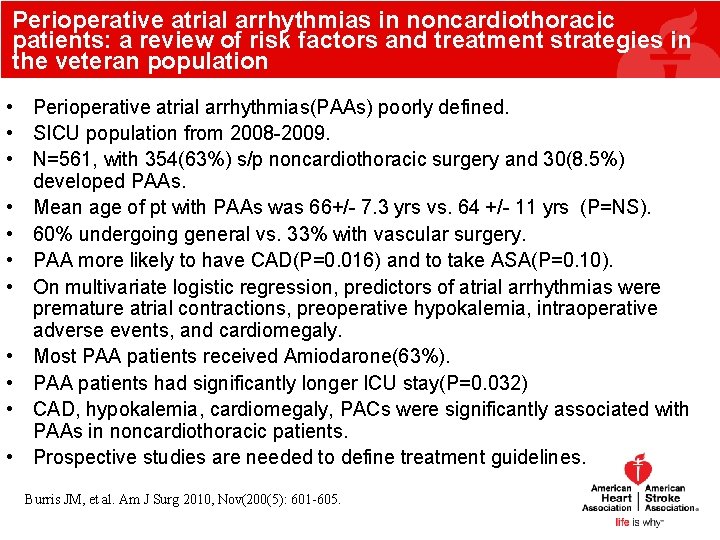
Perioperative atrial arrhythmias in noncardiothoracic patients: a review of risk factors and treatment strategies in the veteran population • Perioperative atrial arrhythmias(PAAs) poorly defined. • SICU population from 2008 -2009. • N=561, with 354(63%) s/p noncardiothoracic surgery and 30(8. 5%) developed PAAs. • Mean age of pt with PAAs was 66+/- 7. 3 yrs vs. 64 +/- 11 yrs (P=NS). • 60% undergoing general vs. 33% with vascular surgery. • PAA more likely to have CAD(P=0. 016) and to take ASA(P=0. 10). • On multivariate logistic regression, predictors of atrial arrhythmias were premature atrial contractions, preoperative hypokalemia, intraoperative adverse events, and cardiomegaly. • Most PAA patients received Amiodarone(63%). • PAA patients had significantly longer ICU stay(P=0. 032) • CAD, hypokalemia, cardiomegaly, PACs were significantly associated with PAAs in noncardiothoracic patients. • Prospective studies are needed to define treatment guidelines. Burris JM, et al. Am J Surg 2010, Nov(200(5): 601 -605.
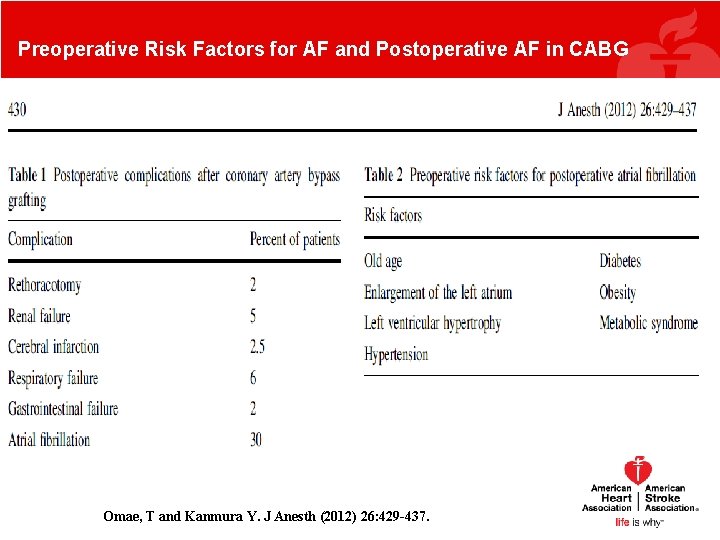
Preoperative Risk Factors for AF and Postoperative AF in CABG Omae, T and Kanmura Y. J Anesth (2012) 26: 429 -437.
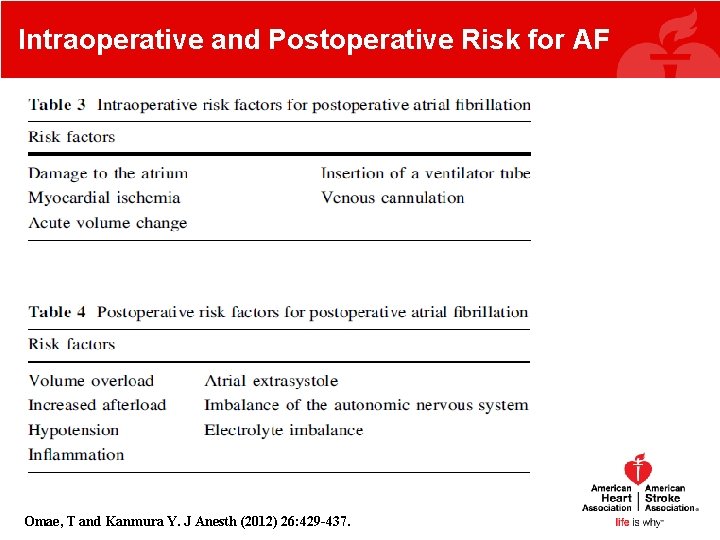
Intraoperative and Postoperative Risk for AF Omae, T and Kanmura Y. J Anesth (2012) 26: 429 -437.
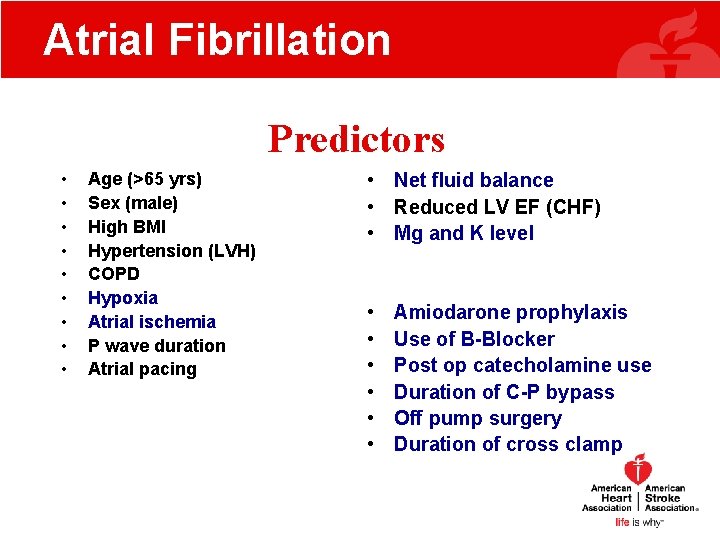
Atrial Fibrillation Predictors • • • Age (>65 yrs) Sex (male) High BMI Hypertension (LVH) COPD Hypoxia Atrial ischemia P wave duration Atrial pacing • Net fluid balance • Reduced LV EF (CHF) • Mg and K level • • • Amiodarone prophylaxis Use of B-Blocker Post op catecholamine use Duration of C-P bypass Off pump surgery Duration of cross clamp
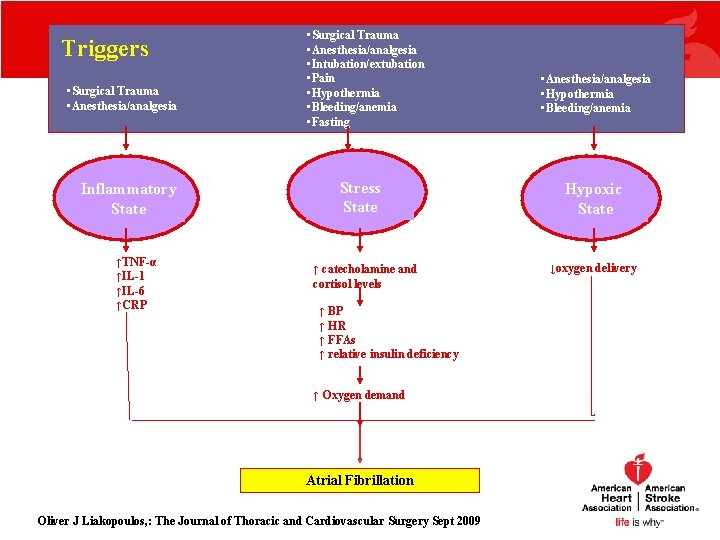
Triggers • Surgical Trauma • Anesthesia/analgesia Inflammatory State ↑TNF-α ↑IL-1 ↑IL-6 ↑CRP • Surgical Trauma • Anesthesia/analgesia • Intubation/extubation • Pain • Hypothermia • Bleeding/anemia • Fasting Stress State ↑ catecholamine and cortisol levels ↑ BP ↑ HR ↑ FFAs ↑ relative insulin deficiency ↑ Oxygen demand Atrial Fibrillation Oliver J Liakopoulos, : The Journal of Thoracic and Cardiovascular Surgery Sept 2009 • Anesthesia/analgesia • Hypothermia • Bleeding/anemia Hypoxic State ↓oxygen delivery
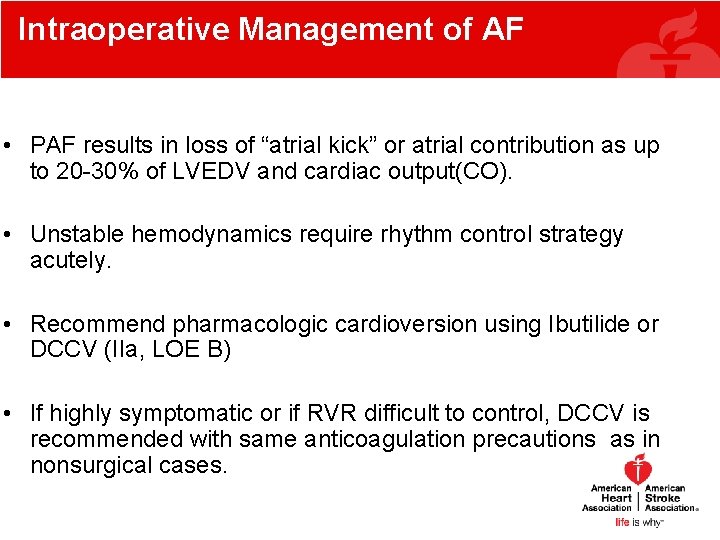
Intraoperative Management of AF • PAF results in loss of “atrial kick” or atrial contribution as up to 20 -30% of LVEDV and cardiac output(CO). • Unstable hemodynamics require rhythm control strategy acutely. • Recommend pharmacologic cardioversion using Ibutilide or DCCV (IIa, LOE B) • If highly symptomatic or if RVR difficult to control, DCCV is recommended with same anticoagulation precautions as in nonsurgical cases.
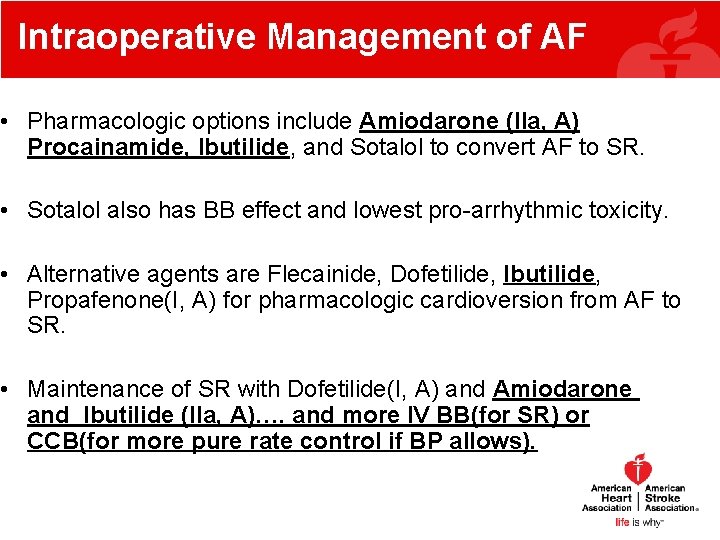
Intraoperative Management of AF • Pharmacologic options include Amiodarone (IIa, A) Procainamide, Ibutilide, and Sotalol to convert AF to SR. • Sotalol also has BB effect and lowest pro-arrhythmic toxicity. • Alternative agents are Flecainide, Dofetilide, Ibutilide, Propafenone(I, A) for pharmacologic cardioversion from AF to SR. • Maintenance of SR with Dofetilide(I, A) and Amiodarone and Ibutilide (IIa, A)…. and more IV BB(for SR) or CCB(for more pure rate control if BP allows).
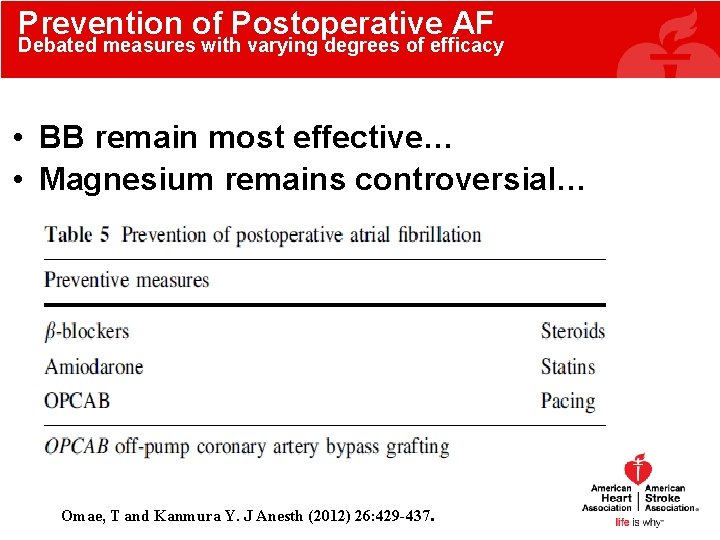
Prevention of Postoperative AF Debated measures with varying degrees of efficacy • BB remain most effective… • Magnesium remains controversial… Omae, T and Kanmura Y. J Anesth (2012) 26: 429 -437.
Conclusions: • Summary – Atrial Fibrillation Management: Update from 2014 Guidelines – Assessment of Thromboembolism and Stroke Risk – Overview of Oral Anticoagulation – Rate vs. Rhythm Control – Role of Catheter Ablation in Atrial Fibrillation Management – Perioperative Management of Atrial Fibrillation
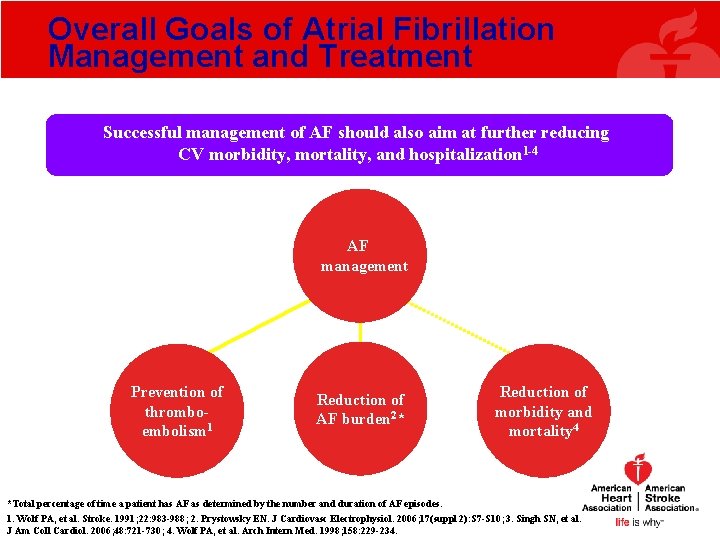
Overall Goals of Atrial Fibrillation Management and Treatment Successful management of AF should also aim at further reducing CV morbidity, mortality, and hospitalization 1 -4 AF management Prevention of thromboembolism 1 Reduction of AF burden 2* Reduction of morbidity and mortality 4 *Total percentage of time a patient has AF as determined by the number and duration of AF episodes. 1. Wolf PA, et al. Stroke. 1991; 22: 983 -988; 2. Prystowsky EN. J Cardiovasc Electrophysiol. 2006; 17(suppl 2): S 7 -S 10; 3. Singh SN, et al. J Am Coll Cardiol. 2006; 48: 721 -730; 4. Wolf PA, et al. Arch Intern Med. 1998; 158: 229 -234.
Atrial Fibrillation Guidelines, March 28, 2014 January CT, Wann LS, Alpert JS, Calkins H, Cleveland JC Jr, Cigarroa JE, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. JACC and Circulation 2014
Acknowledgements and Special Thanks • Sona, Harmaan and Ranveer… • AMC Interventional EP Colleagues: University Cardiology – Drs. Henry Tan and David Steckman(PVI Images courtesy of DS) • AMC/VA Colleagues: – Drs. William E. Boden and Joseph D. Sacco • AHA Colleagues including Dr. N. Mark Estes (Tufts Medical Center) • ACP Colleague, Dr. Katherine Cabral…stay tuned next week for 10/30/14 Anesthesia Grand Rounds on Pharmacology and Perioperative Management of Anticoagulants in Atrial Fibrillation
Management of Atrial Fibrillation: Pre-operative and Perioperative Considerations An Update from the 2014 AHA/ACC/HRS Guidelines Anesthesiology Grand Rounds Department of Anesthesia, Albany Medical Center October 23, 2014 Mandeep S. Sidhu, MD, MBA, FACC Assistant Professor of Medicine, Albany Medical College Adjunct Assistant Professor of Management, Union Graduate College Co-Investigator, Faculty and Regional Co-Leader, ISCHEMIA Trial
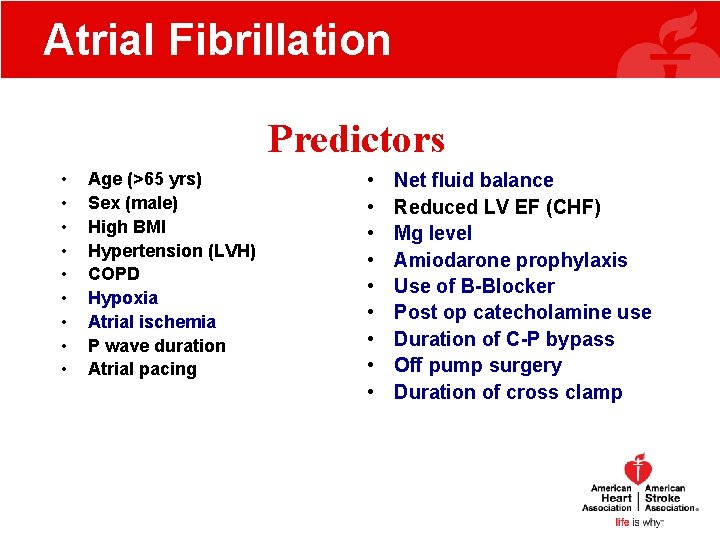
Atrial Fibrillation Predictors • • • Age (>65 yrs) Sex (male) High BMI Hypertension (LVH) COPD Hypoxia Atrial ischemia P wave duration Atrial pacing • • • Net fluid balance Reduced LV EF (CHF) Mg level Amiodarone prophylaxis Use of B-Blocker Post op catecholamine use Duration of C-P bypass Off pump surgery Duration of cross clamp
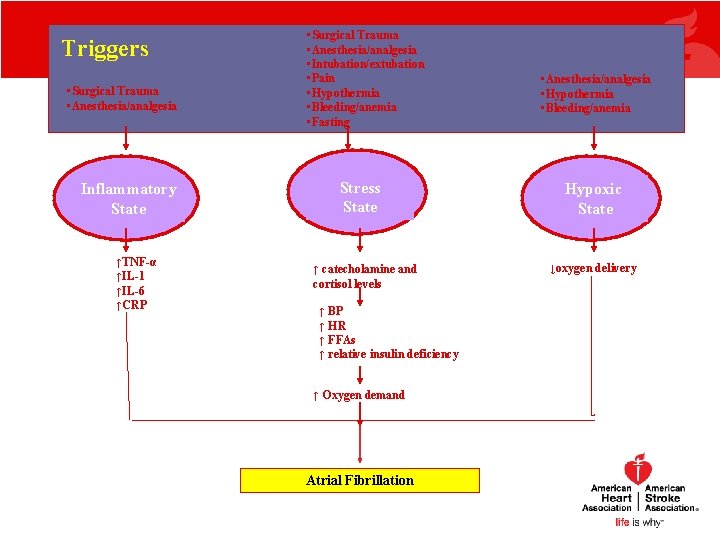
Triggers • Surgical Trauma • Anesthesia/analgesia Inflammatory State ↑TNF-α ↑IL-1 ↑IL-6 ↑CRP • Surgical Trauma • Anesthesia/analgesia • Intubation/extubation • Pain • Hypothermia • Bleeding/anemia • Fasting Stress State ↑ catecholamine and cortisol levels ↑ BP ↑ HR ↑ FFAs ↑ relative insulin deficiency ↑ Oxygen demand Atrial Fibrillation • Anesthesia/analgesia • Hypothermia • Bleeding/anemia Hypoxic State ↓oxygen delivery
Atrial Fibrillation • Statins for prevention of AF after Cardiac surgery (anti-inflammatory effect). Oliver J Liakopoulos, : The Journal of Thoracic and Cardiovascular Surgery Sept 2009
Atrial Fibrillation • Literature search : Influence of preop statin therapy on the incidence of post op AF • Total 17, 643 pts having heart surgery. • 58. 4 % with preop. statin Rx • 41. 6 % without Oliver J Liakopoulos, : The Journal of Thoracic and Cardiovascular Surgery Sept 2009
Atrial Fibrillation • • • Total AF incidence 24. 6 % Pre op statin group 22. 3 % Without 27. 8 % (P<0. 001) Absolute reduction 5. 5% Relative risk reduction 19. 9 % Oliver J Liakopoulos, : The Journal of Thoracic and Cardiovascular Surgery Sept 2009
Atrial Fibrillation • AF is associated with increase long term risk of stroke , all cause mortality, especially in women • Mortality rate of AF patients is 2 X that of patients in NSR with similar heart disease • In the Framingham study, the annual risk of stroke secondary to AF was 1. 5% in participants 50 to 59 Y old and 23. 5% in those aged 80 to 89 Y
Normal Sinus Rhythm • Regular • Synchronous
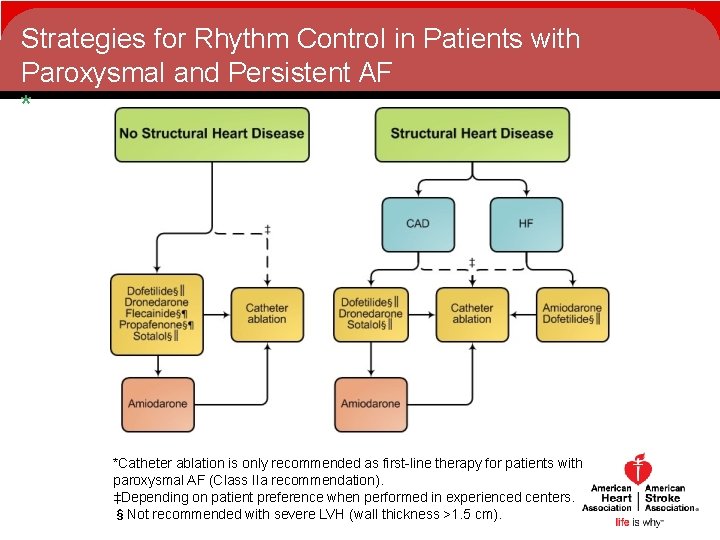
Strategies for Rhythm Control in Patients with Paroxysmal and Persistent AF * *Catheter ablation is only recommended as first-line therapy for patients with paroxysmal AF (Class IIa recommendation). ‡Depending on patient preference when performed in experienced centers. §Not recommended with severe LVH (wall thickness >1. 5 cm).
- Slides: 70