Management of Acute and Chronic Sinusitis Presentation Outline




- Slides: 56

Management of Acute and Chronic Sinusitis
Presentation Outline 1. Acute Sinusitis 2. Chronic Sinusitis
Importance in USA, one in five antibiotic prescriptions are for patients with sinusitis symptoms! (acute and chronic)
Acute Sinusitis
Definition • Acute sinusitis is defined as sinunasal inflammatory Sx & Hx lasting less than one month – Acute Viral Rhinosinusitis (AVRS) – Acute Bacterial Rhinosinusitis (ABRS)
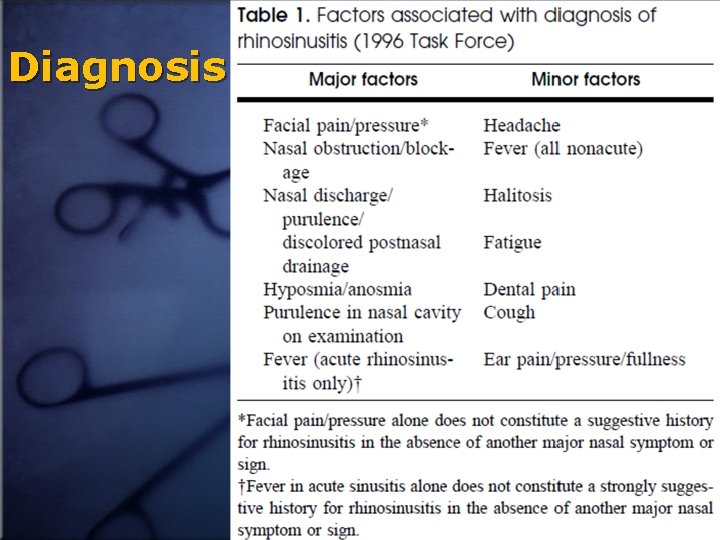
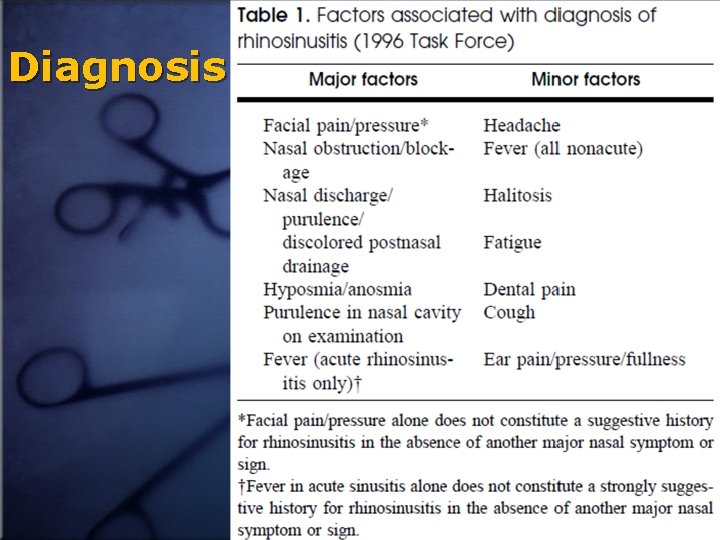
Diagnosis
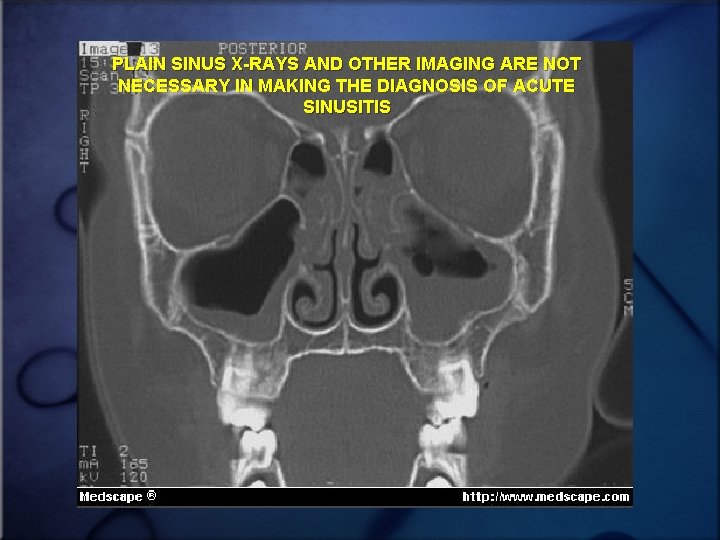
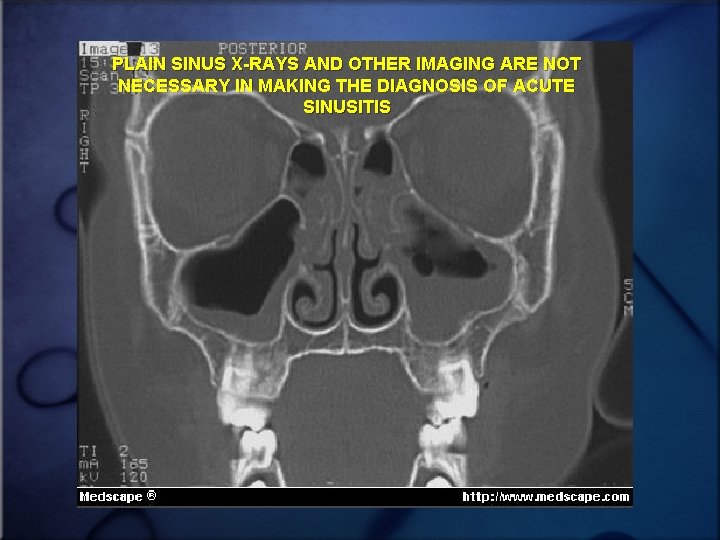
PLAIN SINUS X-RAYS AND OTHER IMAGING ARE NOT NECESSARY IN MAKING THE DIAGNOSIS OF ACUTE SINUSITIS
AVRS Treatment • Maintain adequate hydration • Steamy shower or increase humidity in your home or personal steam vaporizer • Apply warm facial packs • Analgesics (acetaminophen, ibuprofen, aspirin no less than 18 yr)
AVRS Treatment • Saline irrigation lavage • Decongestants (oral) – i. e. : Pseudoephedrine hydrochloride 60 mg every 4 to 6 hours, not to exceed 4 doses per 24 hours. • Decongestant nasal sprays for no longer than 5 days
AVRS Treatment • Adequate rest • Sleep with head of bed elevated • Avoid cigarette smoke and extremely cool or dry air
When to start Abx for ABRS – Persistence of symptoms for longer than 10 days – Worsening of symptoms after 7 days – Conditions Requiring Action Before Seven Days: • Fever >=39 and a documented history of sinusitis • Upper teeth pain (not of dental origin) • Severe symptoms • Known anatomical blockage
ABRS Germs • Streptococcus pneumoniae • nontypeable Haemophilus influenzae • Moraxella catarrhalis
ABRS Treatment • Abx: – Amoxicillin 500 mg tab three times per day x 10 -14 days… in under 18 yrs try 8090 mg/kg/day – For those allergic to amoxicillin: Trimethoprimsulfamethoxazole – For patients allergic to both amoxicillin and TMP/SMX, macrolides can be prescribed • Nasal steroid spray • Pain killer
Follow up • 3 day children • 7 day adult
Partial response • patient is symptomatically improved but not back to normal at the end of the first course of antibiotics – An additional 10 to 14 days of amoxicillin – TMP/SMX: one double strength tab BID x 14 days
Little or no improvement • Amoxicillin/Clavulanate • Cephalosporin 3 rd generation ie. Cefuroxime, Cefpodoxime, Cefprozil, or Cefdinir • Clarithromycin 500 mg BIDx 14 days • Azithromycin 500 mg every day x 3 days • Quinolones… • In patients who have not responded to three weeks of continuous antibiotic therapy practitioners should consider referral to ENT or Allergy for further workup
Invasive Fungal Sinusitis • Uncommon • Seen usually in immunocompromised or diabetic patients • Aspergillosis, mucormycosis • Requires high index of suspscion • Diagnosed by biopsy and culture • Therapy for invasive forms requires wide local debridement and IV Ampo. B

Chronic Rhinosinusitis
Definition • Chronic rhinosinusitis is a group of disorders characterized by: – inflammation of the mucosa of the nose and paranasal sinuses for at least 12 consecutive weeks’ duration
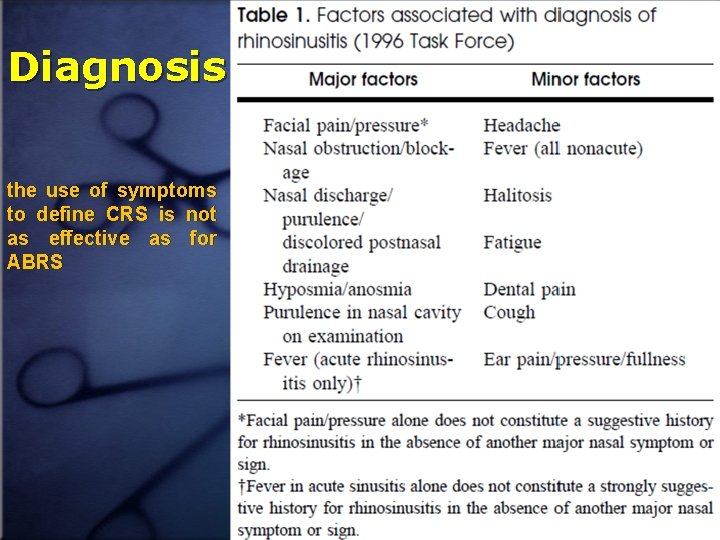
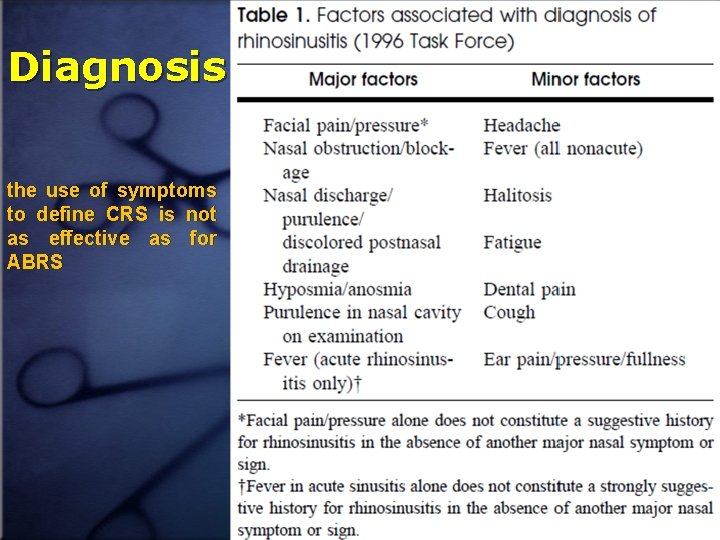
Diagnosis the use of symptoms to define CRS is not as effective as for ABRS
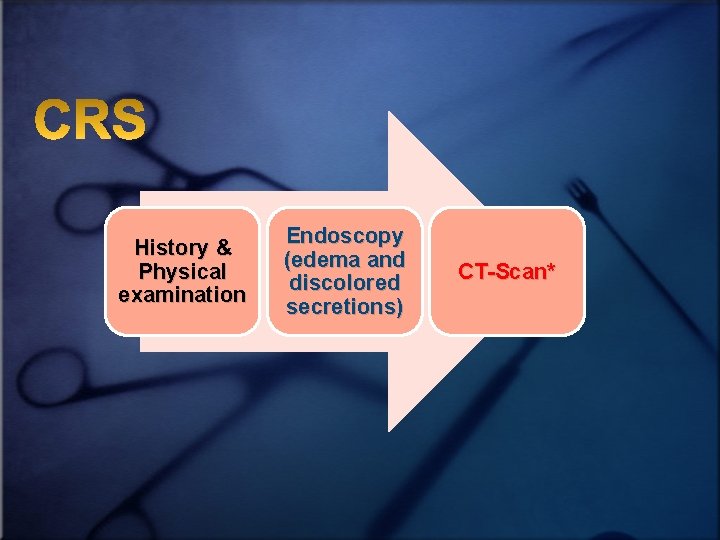
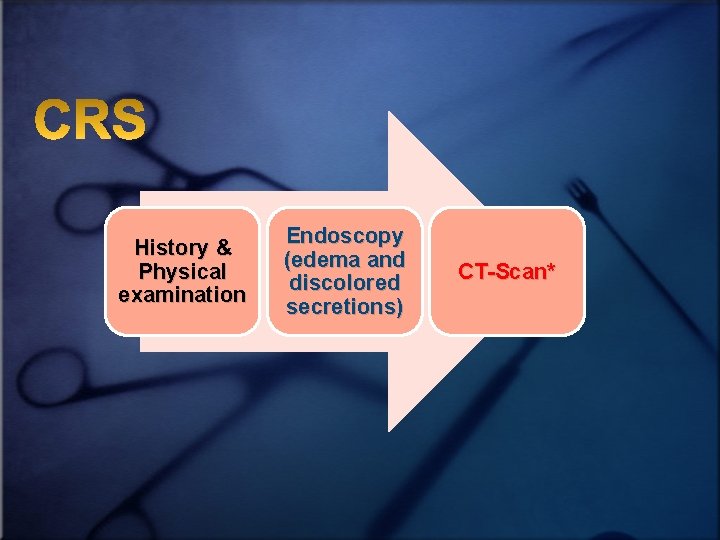
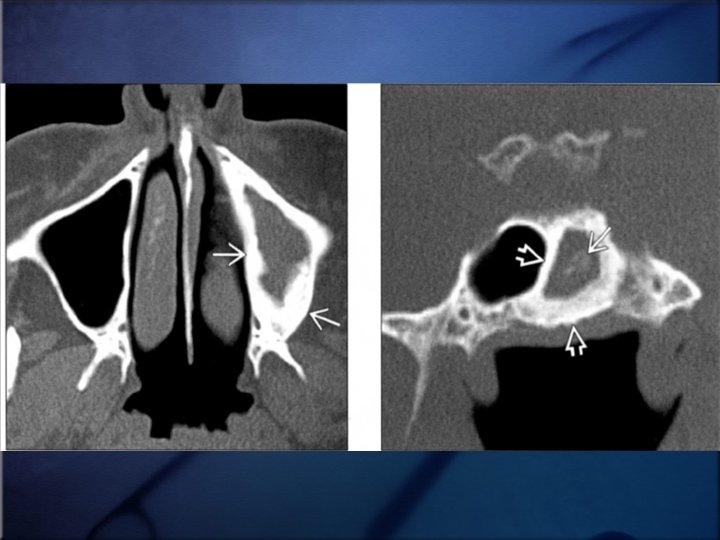
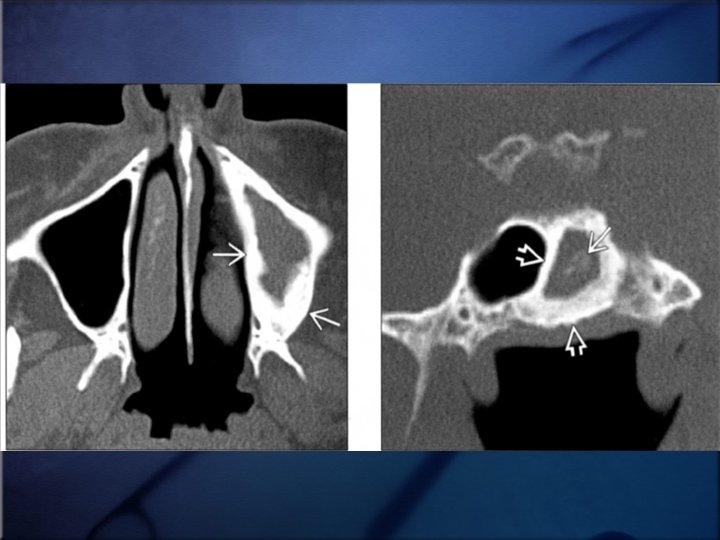
History & Physical examination Endoscopy (edema and discolored secretions) CT-Scan*
Etiology • The potential causes of CRS may be numerous, disparate, and frequently overlapping • A unified, accepted understanding of the etiology of CRS is still being sought
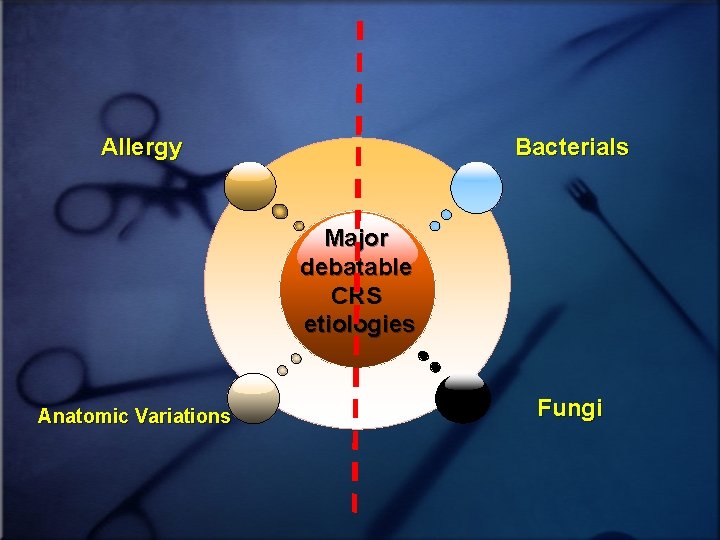
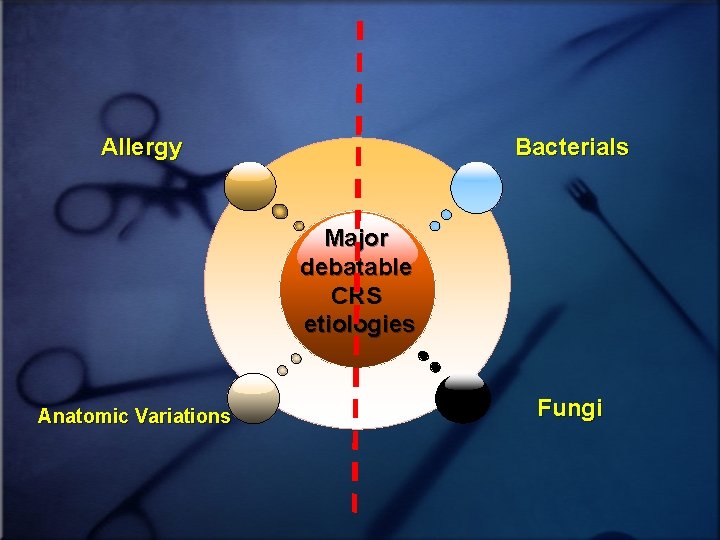
Allergy Bacterials Major debatable CRS etiologies Anatomic Variations Fungi
Allergy • The concordance of allergy and CRS ranges from 25% to 50%, with pediatric studies reporting the higher association • In the subpopulation of patients with CRS symptomatic enough to require surgery, allergy is present in 41% to 84% of patients • Perennial hypersensitivity Predominates (especially house dust mite)
• Allergic patients with CRS responded more poorly to medical management than allergic patients who did not have CRS • Impact of allergic rhinitis on surgical results in endoscopic sinus surgery success rate will be diminished about 10% (90% 80%) • The etiologic association between allergic rhinitis, and CRS is less clear yet (despite ABRS)
Bacterial Infection • The role of bacteria in the pathogenesis of CRS, remains elusive, elusive But: – – mostly of mixed Staphylococcus aureus infections, with a Coagulase-negative staphylococcus median of 3 different bacteries Anaerobic Gram-negative bacteria. • Despite the uncertainties surrounding the etiologic factors associated with CRS, antibiotic therapy has served as a mainstay of treatment
• Why their contribution is elusive? • Relative abundance of eosinophils and the paucity of neutrophilic inflammation in tissue samples of the most cases of CRS • This inflammatory response may be independent of infection
Probable Mechanisms • Chronic infection • Osteitis • Bacterial allergy • Superantigen (usually from SA) • Biofilms The exact role of bacteria in CRS remains unclear
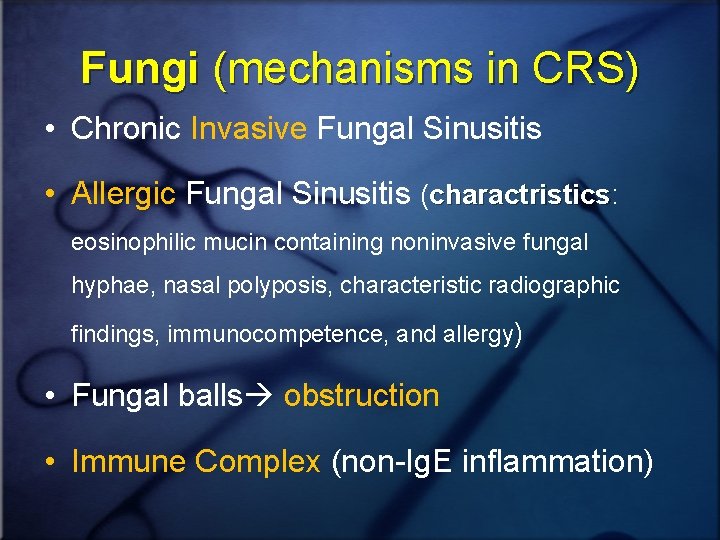
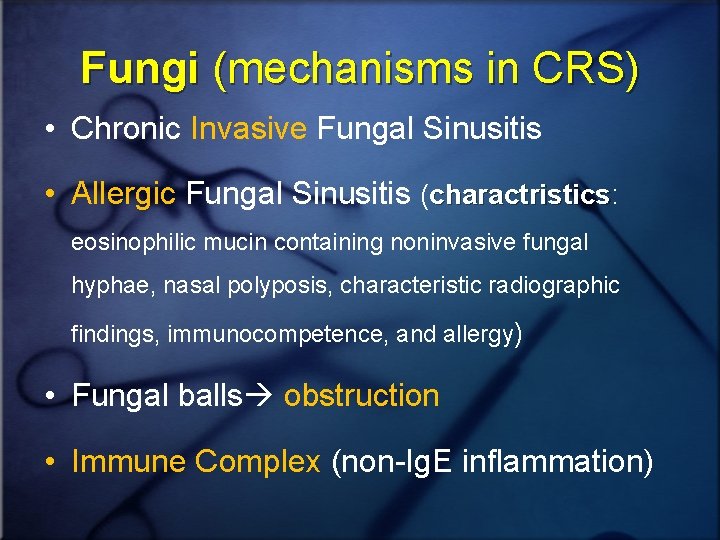
Fungi (mechanisms in CRS) • Chronic Invasive Fungal Sinusitis • Allergic Fungal Sinusitis (charactristics: charactristics eosinophilic mucin containing noninvasive fungal hyphae, nasal polyposis, characteristic radiographic findings, immunocompetence, and allergy) • Fungal balls obstruction • Immune Complex (non-Ig. E inflammation)
• At the current time, it appears that multiple conditions may play a direct or contributory role in the pathogenesis of CRS • Current literature supports the important role that bacteria and/or fungi, fungi appear to play in the pathogenesis of CRS
Anatomic Variants • May predispose to earlier obstruction of the sinuses, allowing for the development of CRS, although strong evidence is lacking

CRS medical therapies
Steroids • Topical (INCS): Four of the five clinical trials demonstrated significant improvement in symptoms • Although systemic steroids are widely used, no RCTs have investigated their use in CRS without polyposis
Antibiotics • There is a lack of RCT in the literature regarding to this topic, however, no difference between antibiotics was noted • But nowadays, Macrolids are in particular attention because in addition to effects, macrolides have antiinflammatory effects corticosteroids antibacterial some akin to interesting those of
• Also macrolides can possibly decrease biofilm formation and overall bacterial virulence • Regimens (3 mo duration): – Erythromycin Ethylsuccinate: 400 q 6 h up to 2 wk, then 400 BD up to 10 wk – Clarithromycin: 500 q 12 h up to 2 wk, then 500 daily up to 10 wk
Nasal douching • At least four RCTs have shown improvement in symptoms, symptoms quality of life and endoscopy and imaging findings • Nasal saline irrigation has been shown to potentially provide more benefit than nasal saline spray in patients with CRS • A 2007 Cochrane review concluded that nasal saline appears to have benefits as an adjunctive treatment for CRS
Antifungal agents • To date no convincing evidence of their efficacy over and above saline douching has been provided
Decongestants • No RCTs have been performed in CRS
Mucolytics • There is little evidence in the literature for the use of mucolytics such as bromhexine
Antihistamines • There is no evidence to support the use of antihistamines in CRS, and they are not recommended
Proton Pump inhibitors • The importance of GERD as a cause of CRS is unknown, unknown but it may be more important in the pediatric population than in adults • No RTCs have shown benefit • GERD may be more of a comorbid state than a cause of CRS
Conclusion • To date, however, because of the paucity of properly conducted trials, no absolute recommendation for a ‘correct regimen’ can be given
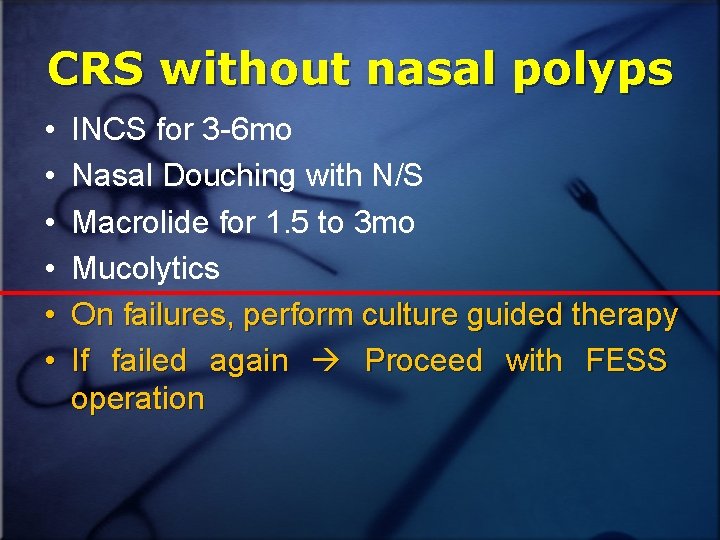
CRS without nasal polyps • • • INCS for 3 -6 mo Nasal Douching with N/S Macrolide for 1. 5 to 3 mo Mucolytics On failures, perform culture guided therapy If failed again Proceed with FESS operation
CRS with nasal polyps • INCS for undisclosed time! • Nasal Douching with N/S • Macrolide administration for 1. 5 - 3 mo • Oral corticosteroids for 10 days (20 -40 mg) • Montelukast
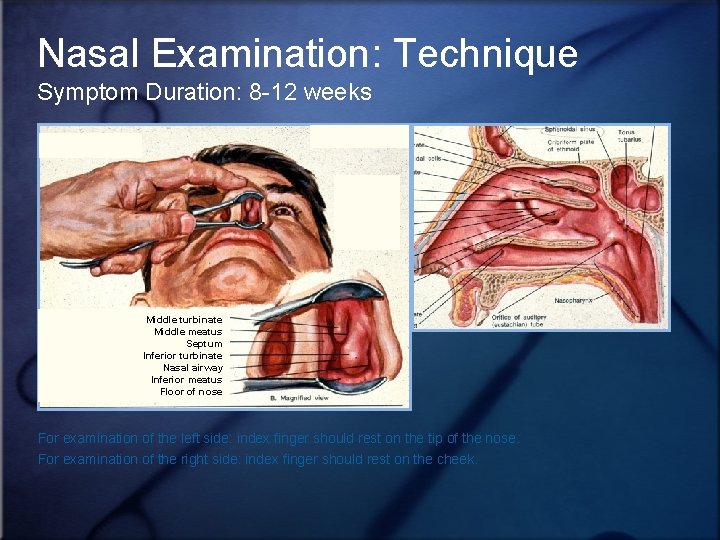
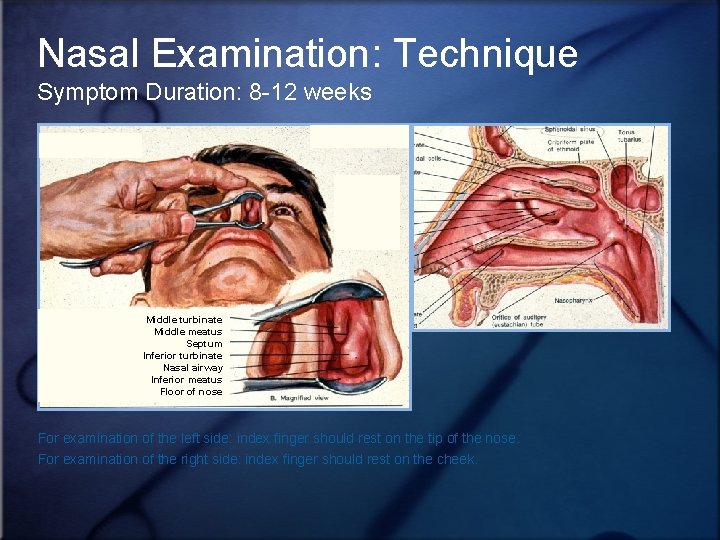
Nasal Examination: Technique Symptom Duration: 8 -12 weeks Middle turbinate Middle meatus Septum Inferior turbinate Nasal airway Inferior meatus Floor of nose For examination of the left side: index finger should rest on the tip of the nose. For examination of the right side: index finger should rest on the cheek.
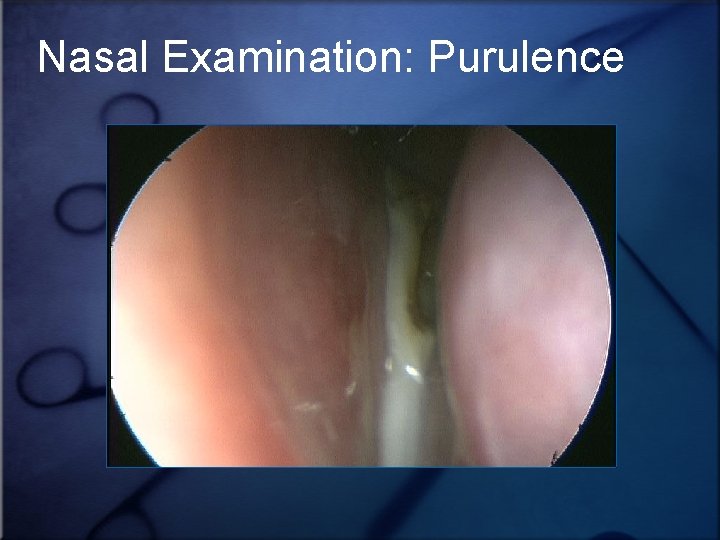
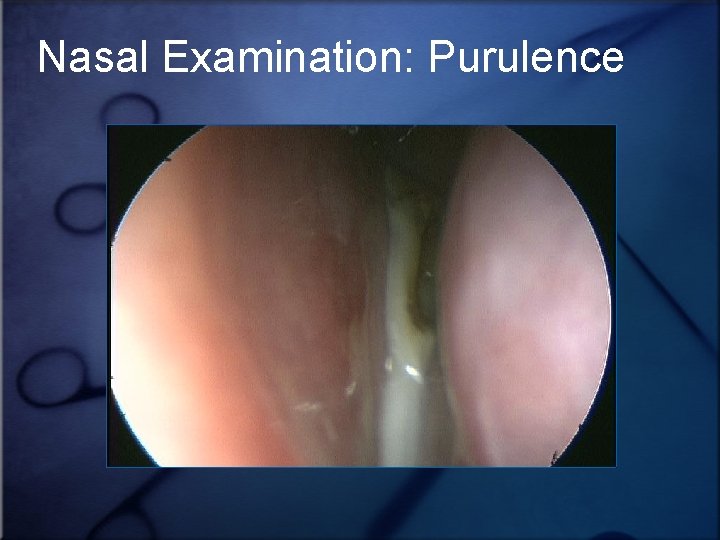
Nasal Examination: Purulence
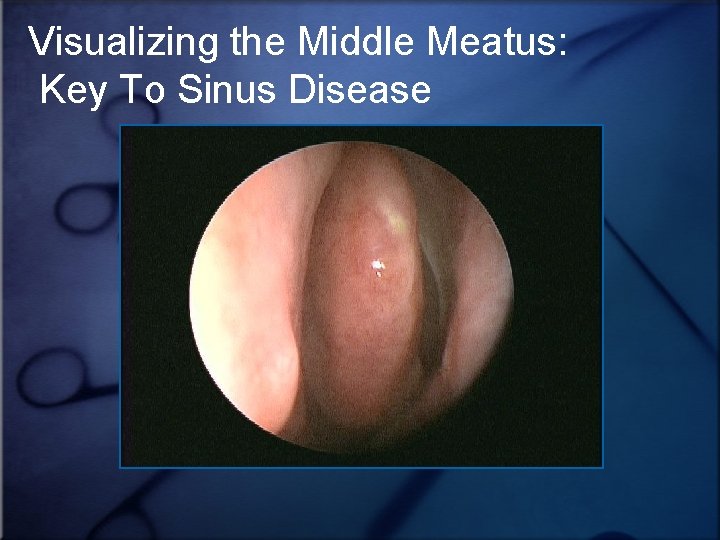
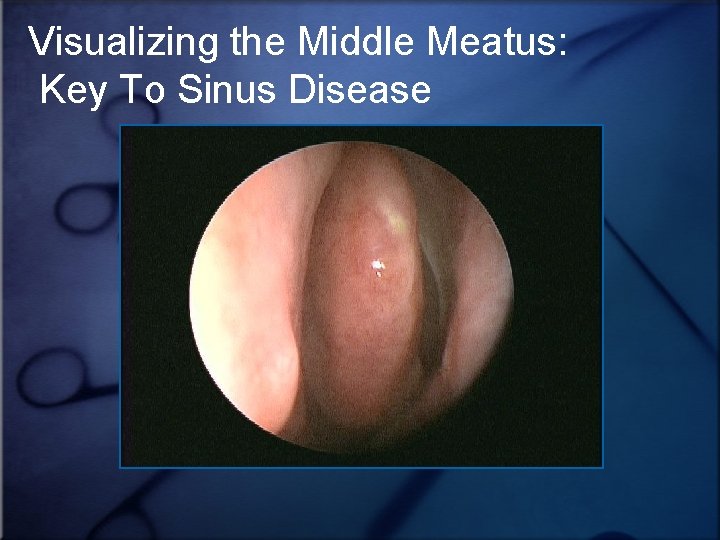
Visualizing the Middle Meatus: Key To Sinus Disease
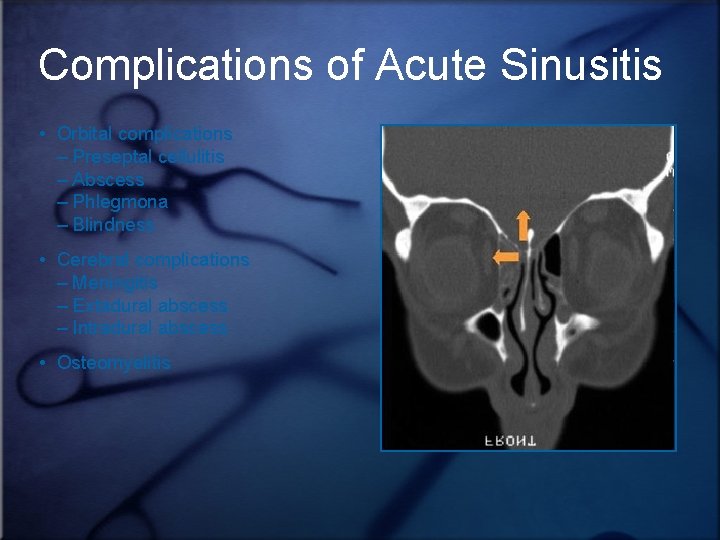
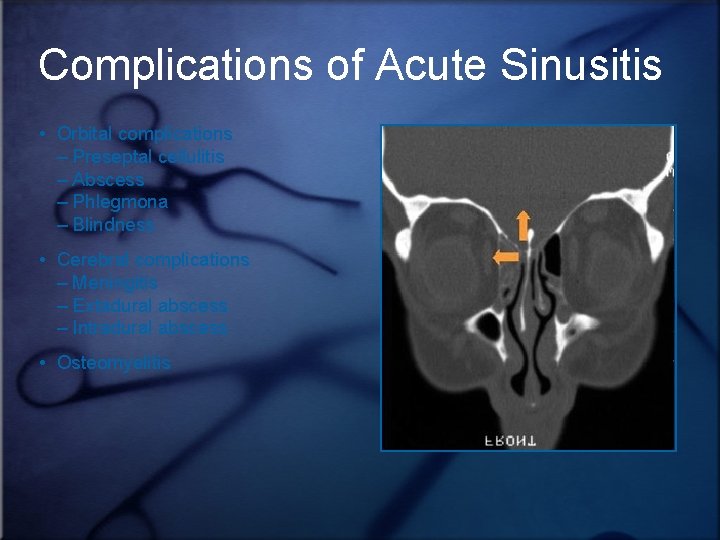
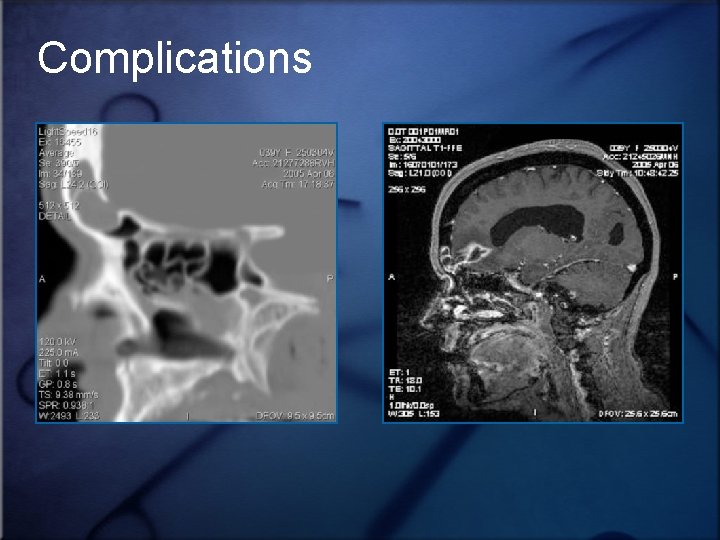
Complications of Acute Sinusitis • Orbital complications – Preseptal cellulitis – Abscess – Phlegmona – Blindness • Cerebral complications – Meningitis – Extadural abscess – Intradural abscess • Osteomyelitis
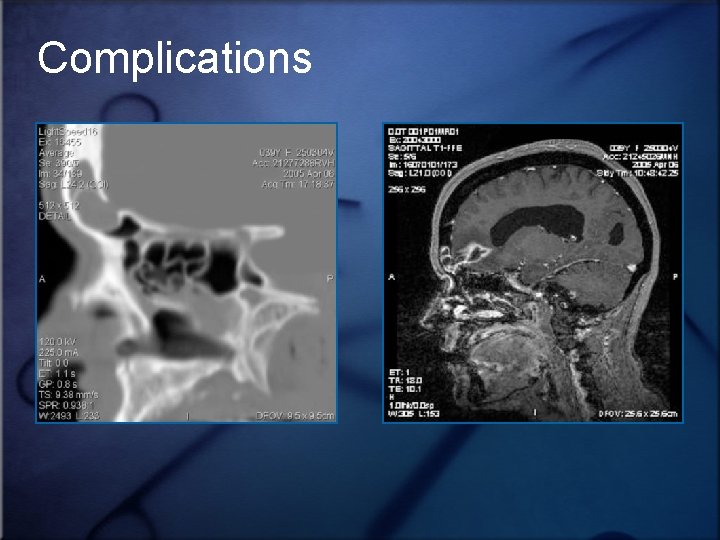
Complications
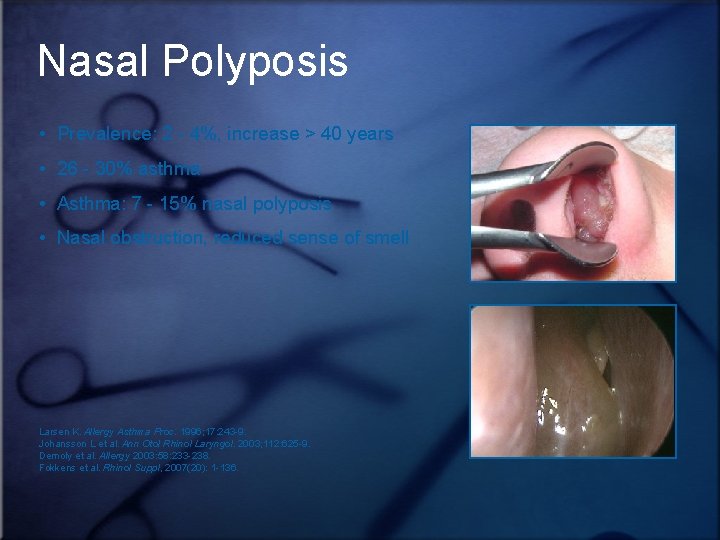
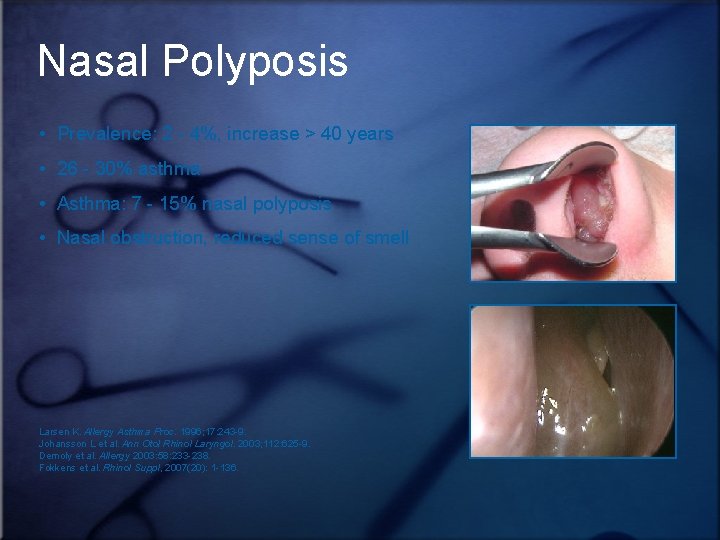
Nasal Polyposis • Prevalence: 2 - 4%, increase > 40 years • 26 - 30% asthma • Asthma: 7 - 15% nasal polyposis • Nasal obstruction, reduced sense of smell Larsen K. Allergy Asthma Proc. 1996; 17: 243 -9. Johansson L et al. Ann Otol Rhinol Laryngol. 2003; 112: 625 -9. Demoly et al. Allergy 2003: 58: 233 -238. Fokkens et al. Rhinol Suppl, 2007(20): 1 -136.
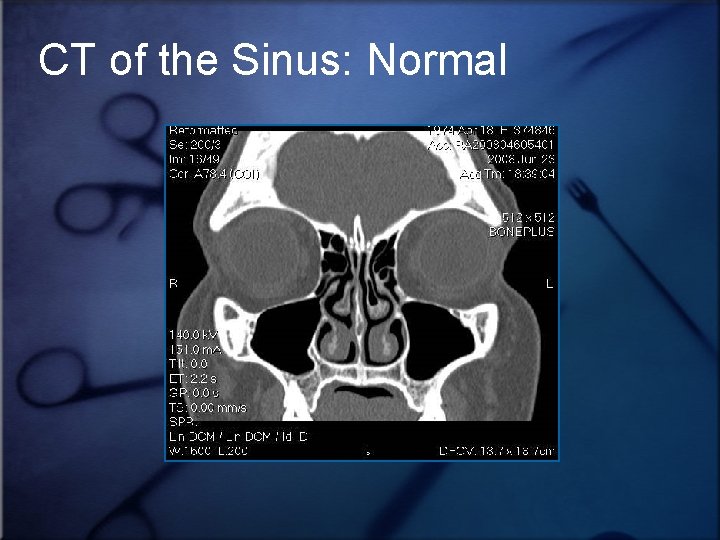
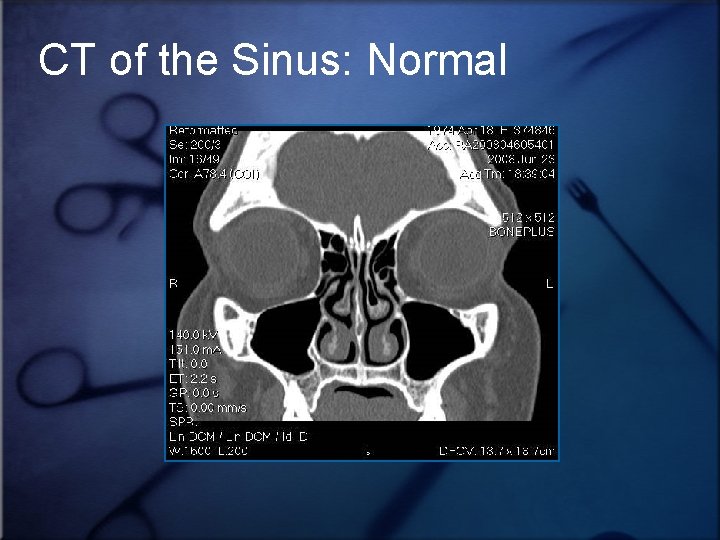
CT of the Sinus: Normal
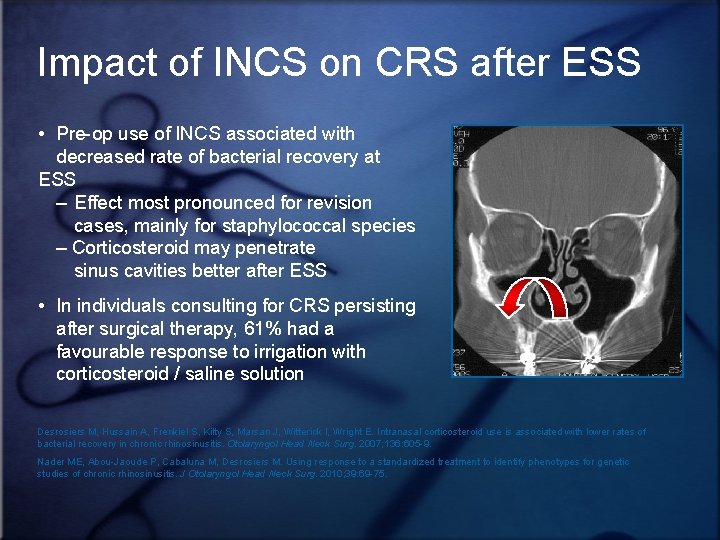
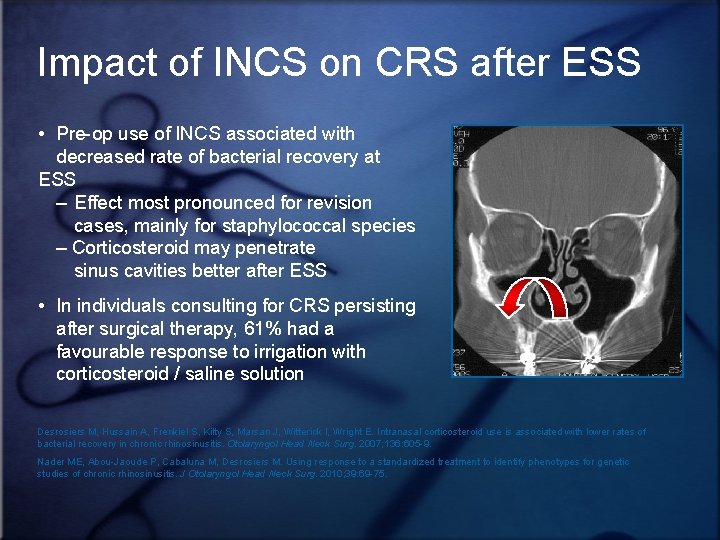
Impact of INCS on CRS after ESS • Pre-op use of INCS associated with decreased rate of bacterial recovery at ESS – Effect most pronounced for revision cases, mainly for staphylococcal species – Corticosteroid may penetrate sinus cavities better after ESS • In individuals consulting for CRS persisting after surgical therapy, 61% had a favourable response to irrigation with corticosteroid / saline solution Desrosiers M, Hussain A, Frenkiel S, Kilty S, Marsan J, Witterick I, Wright E. Intranasal corticosteroid use is associated with lower rates of bacterial recovery in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2007; 136: 605 -9. Nader ME, Abou-Jaoude P, Cabaluna M, Desrosiers M. Using response to a standardized treatment to identify phenotypes for genetic studies of chronic rhinosinusitis. J Otolaryngol Head Neck Surg. 2010; 39: 69 -75.

Thank You!