Management and Safety of students with Diabetes Kanika
Management and Safety of students with Diabetes Kanika Ghai MD Division Director Pediatric Endocrinology Advocate Children’s Hospital April 9, 2019
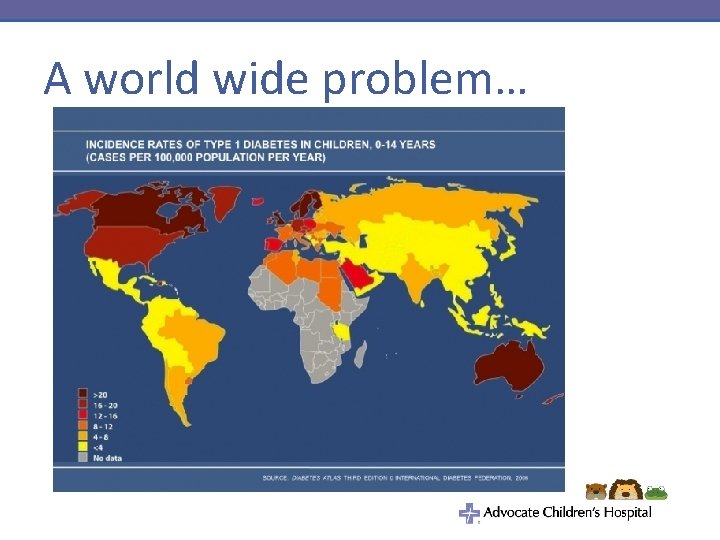
A world wide problem…
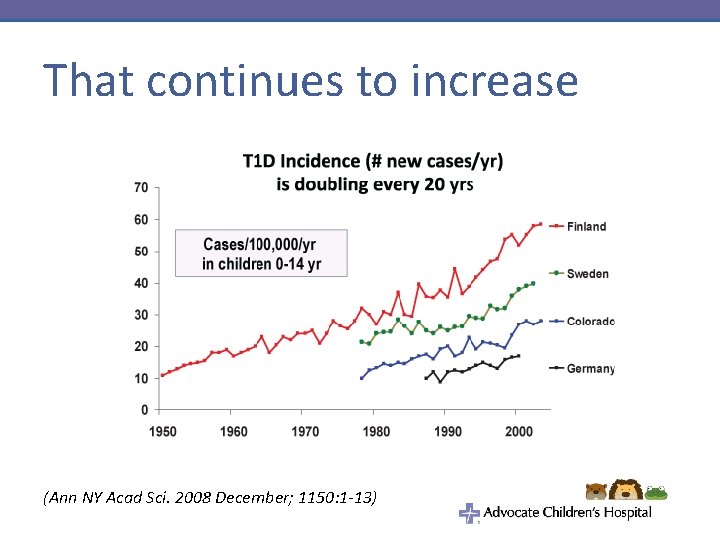
That continues to increase (Ann NY Acad Sci. 2008 December; 1150: 1 -13)
• About 200, 000 Americans under age 20 are estimated to have diagnosed diabetes • approximately 0. 25% of those under age 20 have diagnosed diabetes
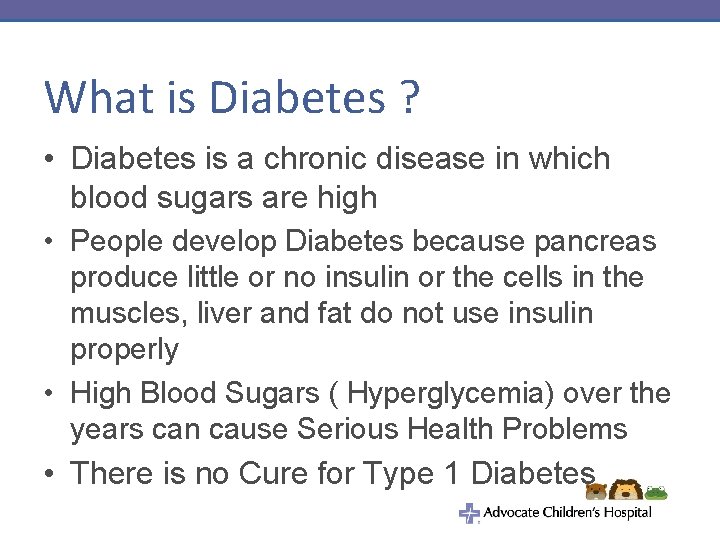
What is Diabetes ? • Diabetes is a chronic disease in which blood sugars are high • People develop Diabetes because pancreas produce little or no insulin or the cells in the muscles, liver and fat do not use insulin properly • High Blood Sugars ( Hyperglycemia) over the years can cause Serious Health Problems • There is no Cure for Type 1 Diabetes
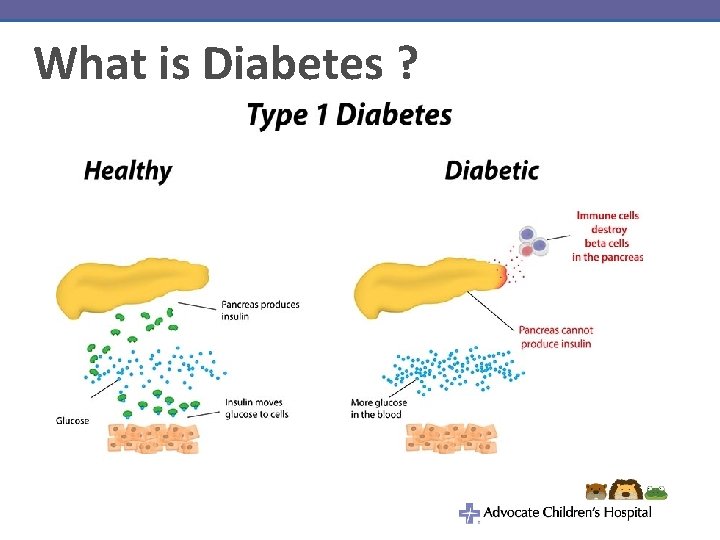
What is Diabetes ?
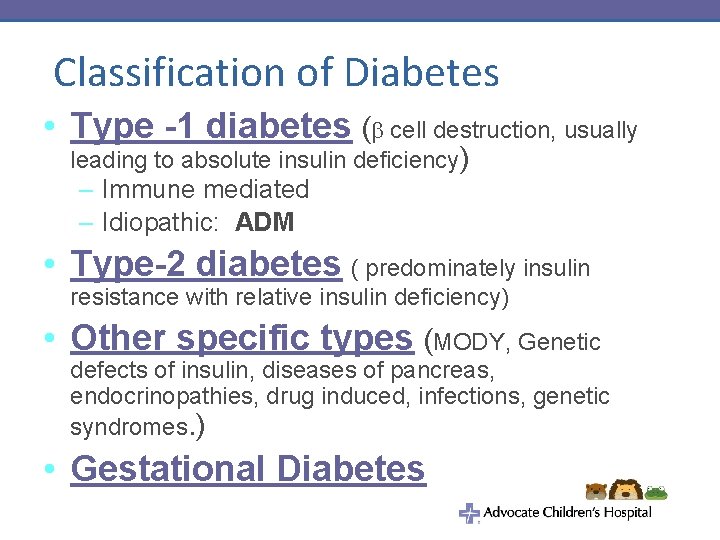
Classification of Diabetes • Type -1 diabetes ( cell destruction, usually leading to absolute insulin deficiency) – Immune mediated – Idiopathic: ADM • Type-2 diabetes ( predominately insulin resistance with relative insulin deficiency) • Other specific types (MODY, Genetic defects of insulin, diseases of pancreas, endocrinopathies, drug induced, infections, genetic syndromes. ) • Gestational Diabetes

T 1 DM vs T 2 DM • Type 1 diabetes mellitus – Autoimmune in nature – Requires insulin administration from time of diagnosis • Type 2 diabetes mellitus – Typically related to obesity – May be treated with diet, oral medications or insulin therapy
Presentation of Diabetes • Extremely variable – May be asymptomatic found on routine screening – May be critically ill – requiring intensive care • May initially present as diabetic ketoacidosis – results from a lack of insulin – body switches to burning fatty acids and producing acidic ketone bodies – Vomiting, dehydration, deep gasping breathing and mental status changes are typical symptoms.

Signs & Symptoms of Diabetes • • Increased thirst Increased urination “accidents” – daytime or nighttime Weight loss Abdominal pain Nausea / emesis Headaches Blurry vision
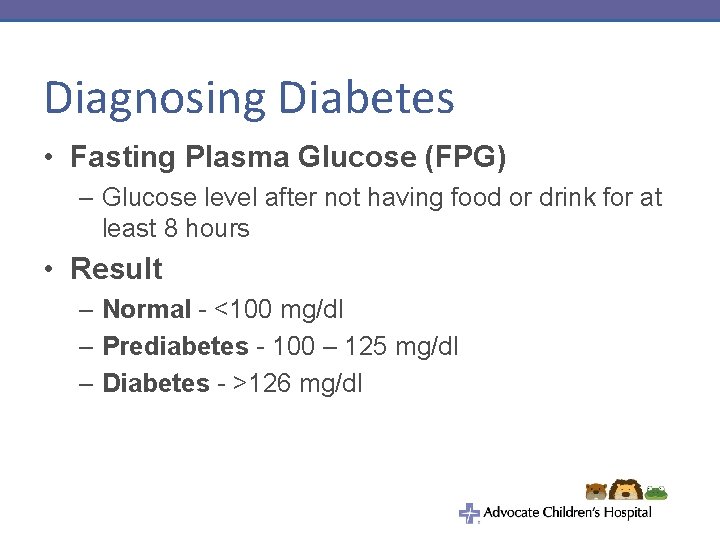
Diagnosing Diabetes • Fasting Plasma Glucose (FPG) – Glucose level after not having food or drink for at least 8 hours • Result – Normal - <100 mg/dl – Prediabetes - 100 – 125 mg/dl – Diabetes - >126 mg/dl
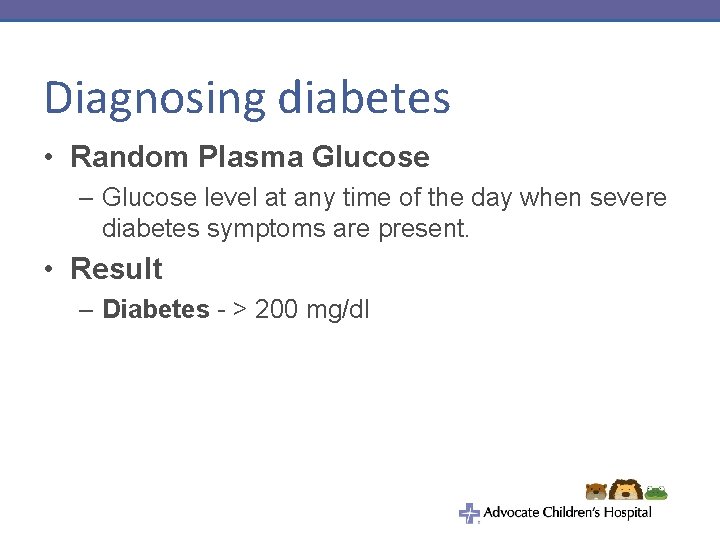
Diagnosing diabetes • Random Plasma Glucose – Glucose level at any time of the day when severe diabetes symptoms are present. • Result – Diabetes - > 200 mg/dl
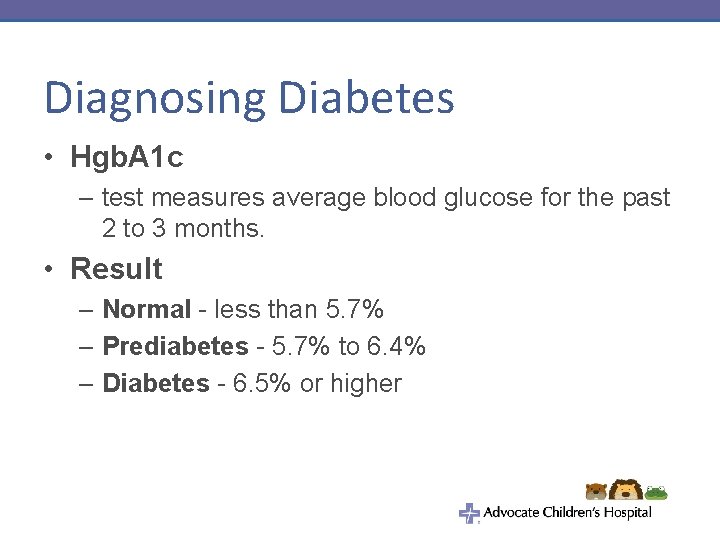
Diagnosing Diabetes • Hgb. A 1 c – test measures average blood glucose for the past 2 to 3 months. • Result – Normal - less than 5. 7% – Prediabetes - 5. 7% to 6. 4% – Diabetes - 6. 5% or higher
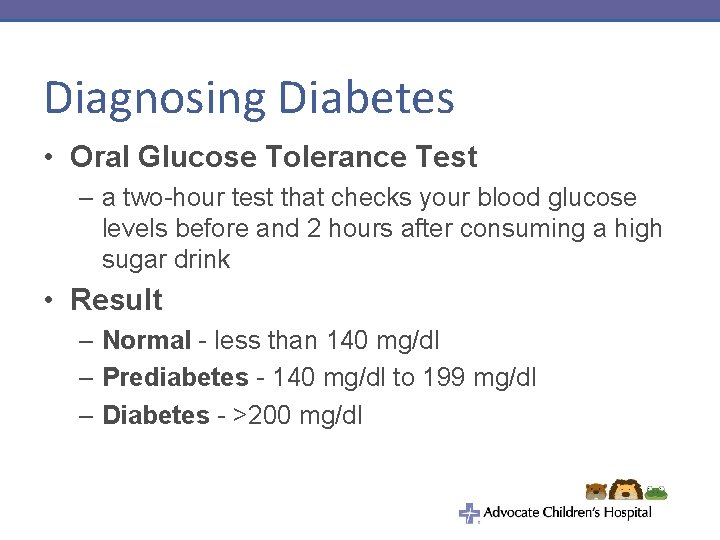
Diagnosing Diabetes • Oral Glucose Tolerance Test – a two-hour test that checks your blood glucose levels before and 2 hours after consuming a high sugar drink • Result – Normal - less than 140 mg/dl – Prediabetes - 140 mg/dl to 199 mg/dl – Diabetes - >200 mg/dl
Treatment • • Insulin therapy : Most important Nutrition: High fiber, Less Free Sugar Active Lifestyle Frequent monitoring : Adjustments to correct high and low Blood sugars • Prevention of High and Low blood sugars. Anticipate high or low Blood sugars from Blood sugar trends and intervene before they get abnormal
Blood glucose monitoring • Allows one to determine the concentration of glucose in blood • Helps guide management • When to be done – Before meals or snacks – Before bedtime – With changes in insulin doses – Before activity – When symptomatic • Should be performed on finger-tip
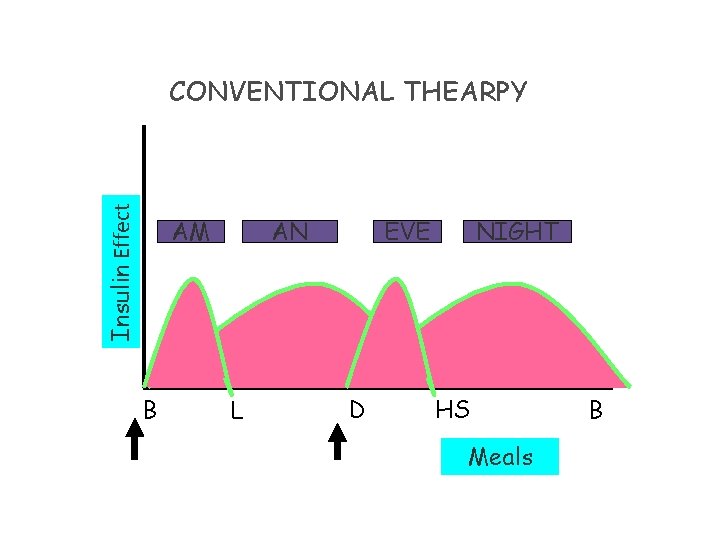
Insulin Effect CONVENTIONAL THEARPY AM B AN L EVE D NIGHT HS Meals B
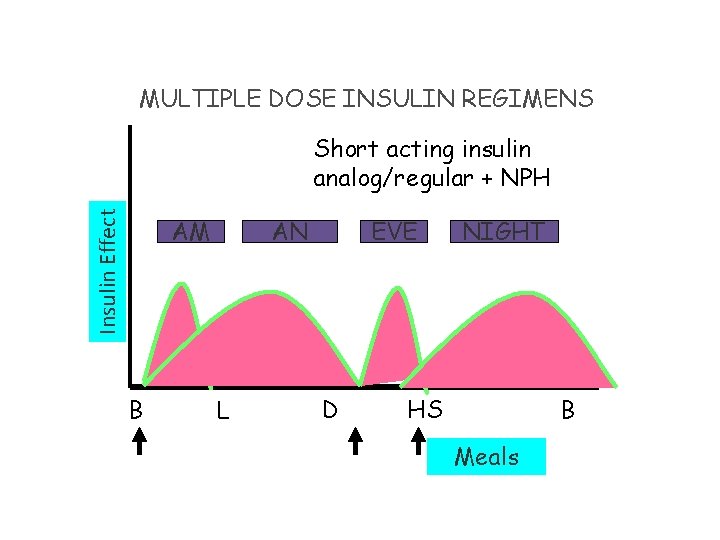
MULTIPLE DOSE INSULIN REGIMENS Insulin Effect Short acting insulin analog/regular + NPH AM B AN L EVE D NIGHT HS B Meals

Multiple Dose Insulin Regimens Insulin Effect Novolog/Humalog/Apidra/Reg + Lantus/ Levemir/UL AM B AN L EVE D NIGHT HS Meals B
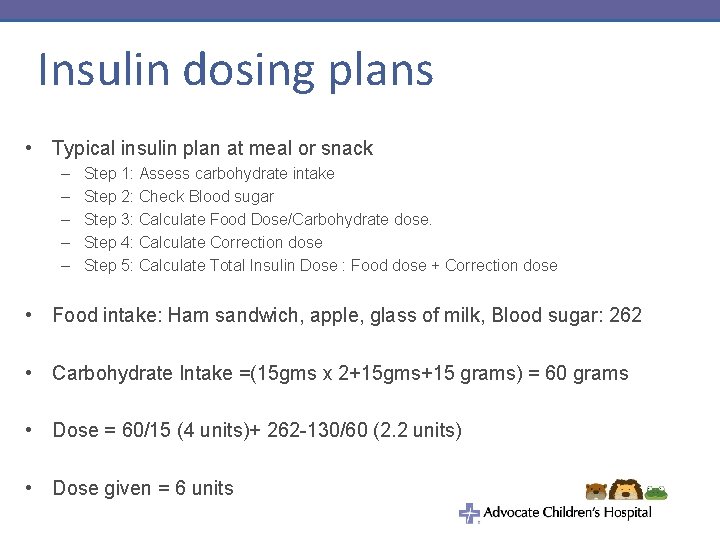
Insulin dosing plans • Typical insulin plan at meal or snack – – – Step 1: Assess carbohydrate intake Step 2: Check Blood sugar Step 3: Calculate Food Dose/Carbohydrate dose. Step 4: Calculate Correction dose Step 5: Calculate Total Insulin Dose : Food dose + Correction dose • Food intake: Ham sandwich, apple, glass of milk, Blood sugar: 262 • Carbohydrate Intake =(15 gms x 2+15 gms+15 grams) = 60 grams • Dose = 60/15 (4 units)+ 262 -130/60 (2. 2 units) • Dose given = 6 units
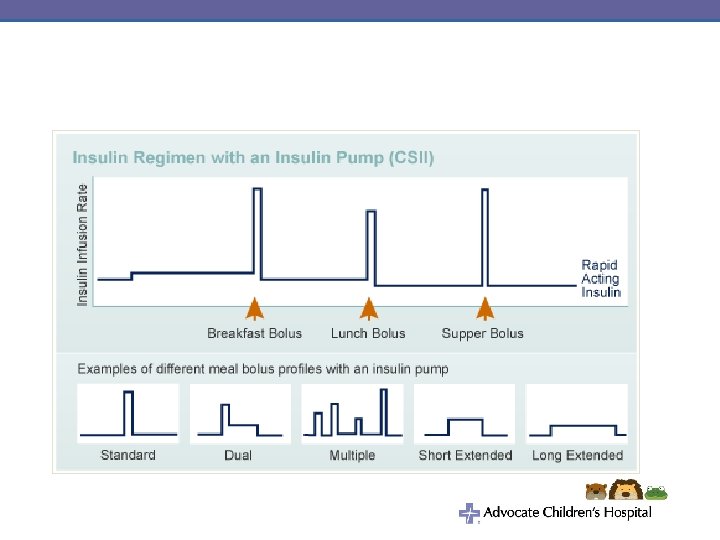
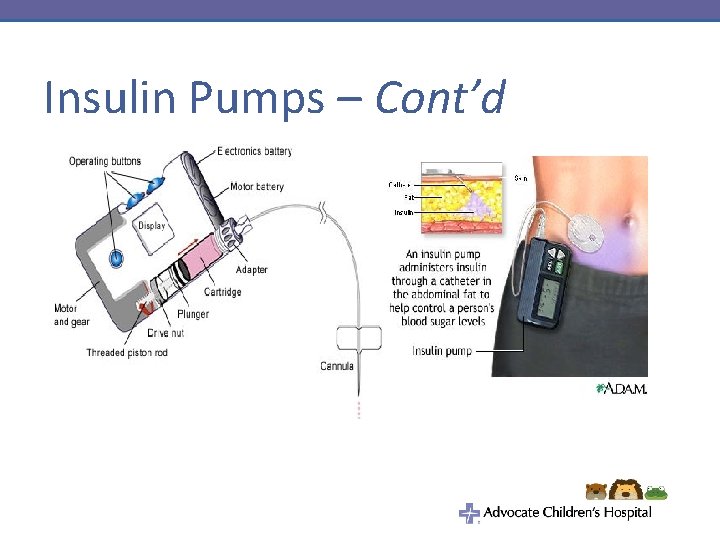
Insulin Pumps – Cont’d
Insulin Pumps


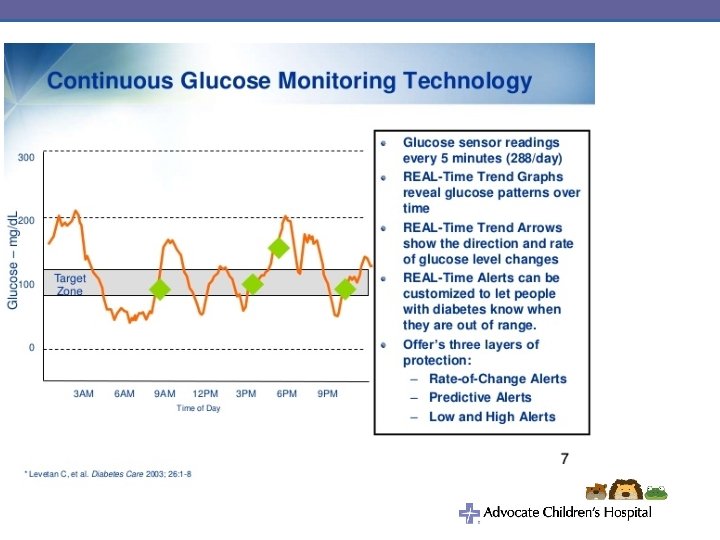
Glucose sensors – 3 parts: 1. Sensor 2. Transmitter 3. Receiver
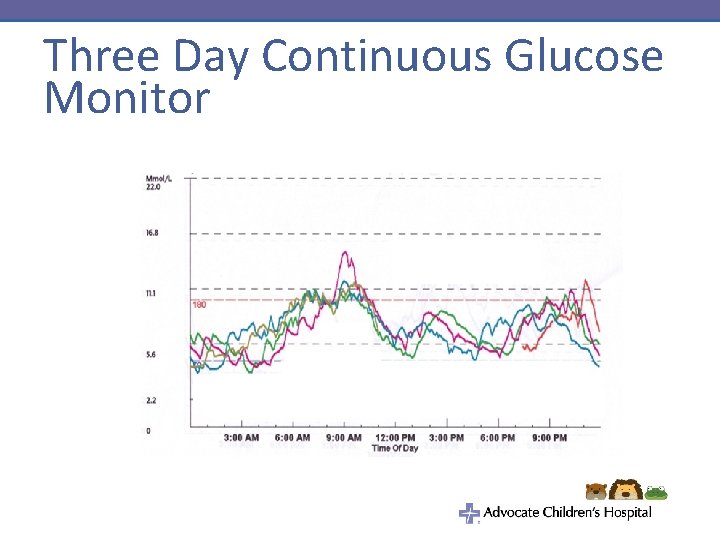
Three Day Continuous Glucose Monitor
Caring for a child with diabetes • A lot of a child’s diabetes cares will take place at school • Illinois has in place the Care of Students with Diabetes Act – Provides requirements school must meet in regards to care of diabetes – Difficult for many schools to have required training and personnel available • A partnership between nurse, students, parents and medical home
Effective Diabetes Management at School • Goal: Keep Blood sugar levels within target range determined by health care team • Assist Student in performing Diabetes care tasks • Designating Trained Diabetes Personnel
How to plan Effective management in School Setting • Assemble health care team • Review Federal Laws • Assemble Student’s health care plan – Diabetes Management plan (health care team) – Individualized health care plan ( school nurse) – Emergency care plans(school nurse) • Prepare Student’s education plan • Train School Personnel • Diabetes Management Training resources
Review Federal Laws • Section 504 of the Rehabilitation act of 1973 (section 504) • American with Disabilities Act of 1990 (ADA) • Individuals with Disabilities Education act (IDEA)
Diabetes Care Plan • Also known as a diabetes medical management plan (DMMP) • Provides direction for diabetes cares at school • Per Diabetes Care Act a DMMP is required: – “upon enrollment, as soon as practical following a student's diagnosis; or when a student's care needs change during the school year. Parents shall be responsible for informing the school in a timely manner of any changes to the diabetes care plan and their emergency contact numbers. ”
Diabetes Care Plan • Provides information on: – Monitoring of blood glucose – Dosing of insulin • Authorization for insulin use – Treatment of hypoglycemia • Authorization for glucagon use – Treatment of hyperglycemia – Use of insulin pump – Physical activity and sports – Nutrition
Train School Personnel • Level 1 Training: All school personnel • Level 2 Training: school personnel who have responsibility for the student • • Level 3: School staff designated as trained Diabetes personnel
Help students lmplement Effective Diabetes management • • • Check BG Plan Disposal of sharps Recognize and Rx low BG Recognize and Rx high BG Administer insulin and/or other Diabetes medication Plan for emergency Plan Individualized meal plan Plan for special events, field trips Promote Regular physical activity Deal with emotional and social issues
Hypoglycemia • • Too much Insulin Missing or delaying meals or snacks Not eating enough food (carbohydrates) Getting additional, intense, unplanned physical activity • Being ill particularly with gastrointestinal illness • Hypoglycemia is not always preventable • Not every student can recognize hypoglycemia
Checklist for Hypoglycemia • Mild/moderate : Oral glucose and recheck BG – Student should not be left alone or sent anywhere alone or with another student • Severe: Glucagon use – Position child to side – Do not feed orally – Call 911 – Administer Glucagon – Call parents /guardian – Stay with student

Checklist for Hyperglycemia • • • Check BG and repeat every 2 hours Check urine ketones Give insulin correction dose Give Extra fluids (sugar free) Allow unrestricted access to restroom Restrict participation in physical activity per DMPP Notify parents Pump: Check if pump is connected properly For suspected pump failure give insulin via injection
Thank You …
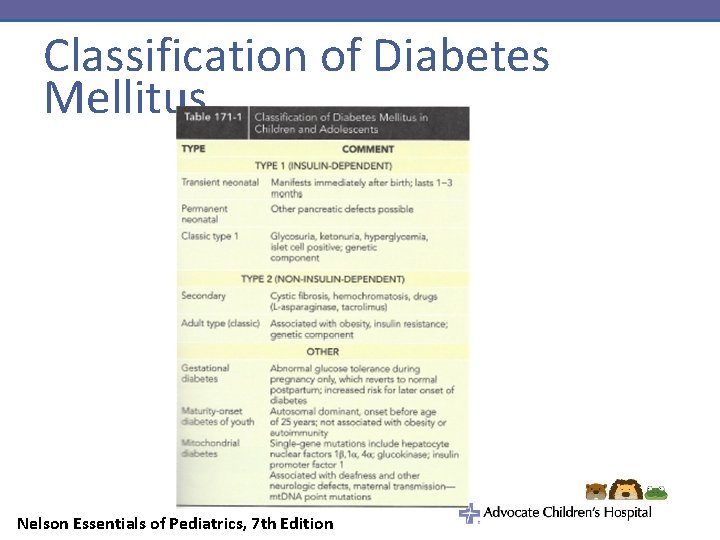
Classification of Diabetes Mellitus Nelson Essentials of Pediatrics, 7 th Edition
- Slides: 42