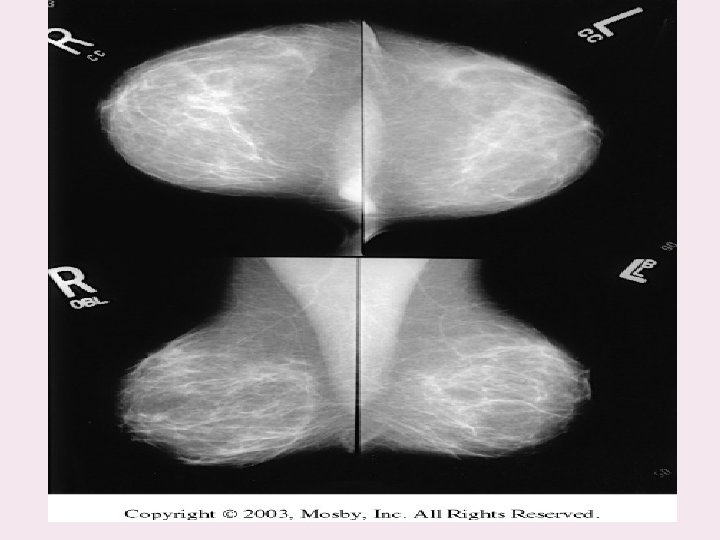
Mammography is the radiographic examination of the breast

Mammography is the radiographic examination of the breast tissue (soft tissue radiography). To visualize normal structures and pathology within the breast
• Mammography is the process of using low-energy X-rays (usually around 30 k. Vp) to examine the human breast and is used as a diagnostic and a screening tool. • The goal of mammography is the early detection of breast cancer
A mammogram is an x-ray picture of the breast. It can be used to check for breast cancer in women who have no signs or symptoms of the disease. It can also be used. if you have a lump or other sign of breast cancer.

Mammograms are also recommended for younger women who have symptoms of breast cancer or who have a high risk of the disease
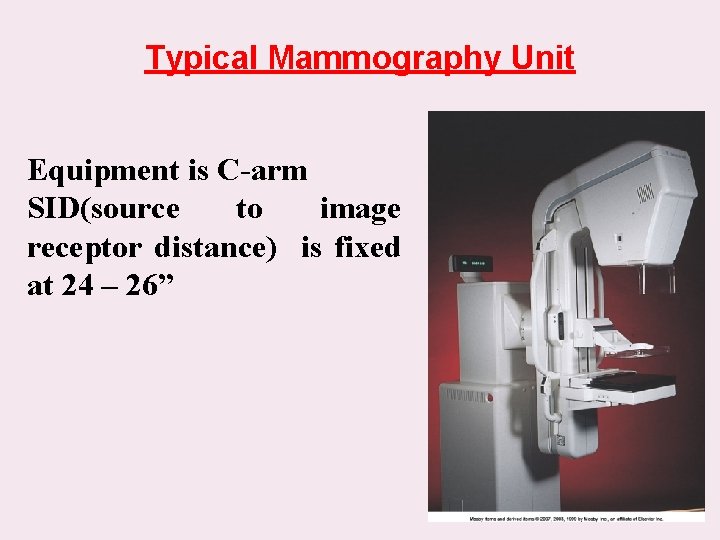
Typical Mammography Unit Equipment is C-arm SID(source to image receptor distance) is fixed at 24 – 26”
Mammography Equipment Dedicated units have high-frequency generators Provide more precise control of k. Vp, m. A, and exposure time Specially designed to produce high-contrast and high-resolution images
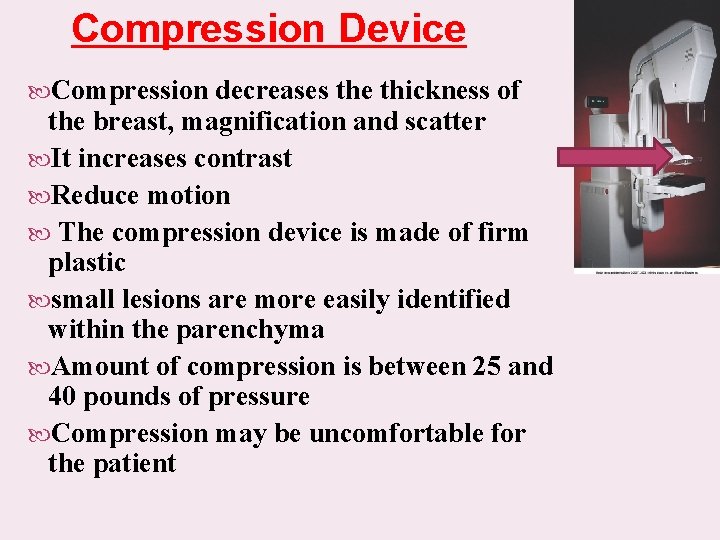
Compression Device Compression decreases the thickness of the breast, magnification and scatter It increases contrast Reduce motion The compression device is made of firm plastic small lesions are more easily identified within the parenchyma Amount of compression is between 25 and 40 pounds of pressure Compression may be uncomfortable for the patient
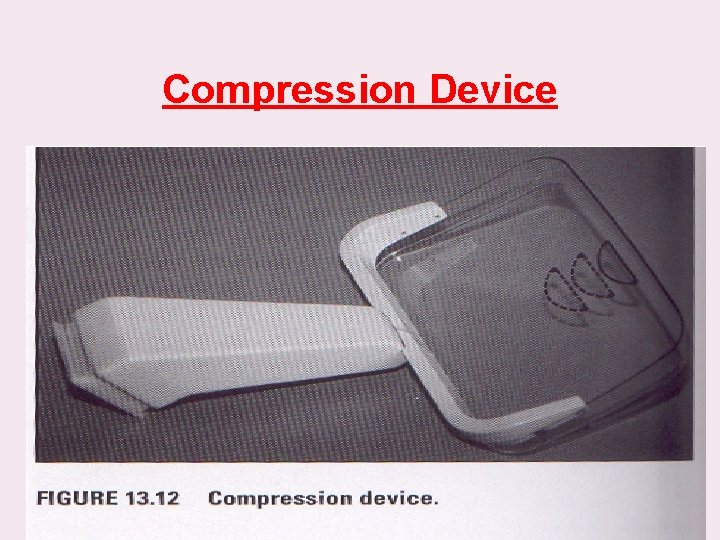
Compression Device
Screen-Film Systems Mammography cassettes contain a single screen The film is single emulsion
Radiation protection Absorbed doses are high in mammography due to the low kvp necessary to maximize the small differences in attenuation between tissues in the breast. The breast is one of the most radio-sensitive tissues in the body. Careful technique is essential to avoid the need for repeat projections. Gonad protection.
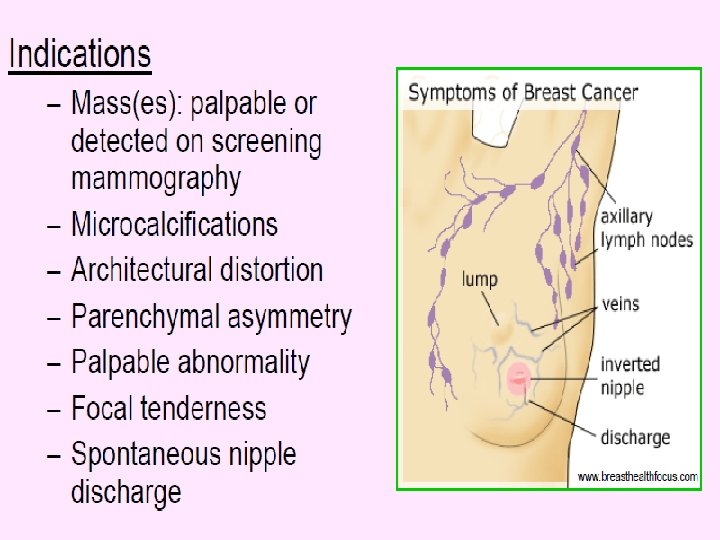
Lesion characteristics: Masses are assessed by shape, margin and density. The shape may be round, oval, irregular or lobulated, and the margin (or surface) may be smooth, obscured (by surrounding tissue), indistinct Any of these may be hyper-, iso- or hypodense. Benign lesions tend to be round or oval and welldefined, whereas malignancies tend to be irregular in shape and outline and are often hyperdense.
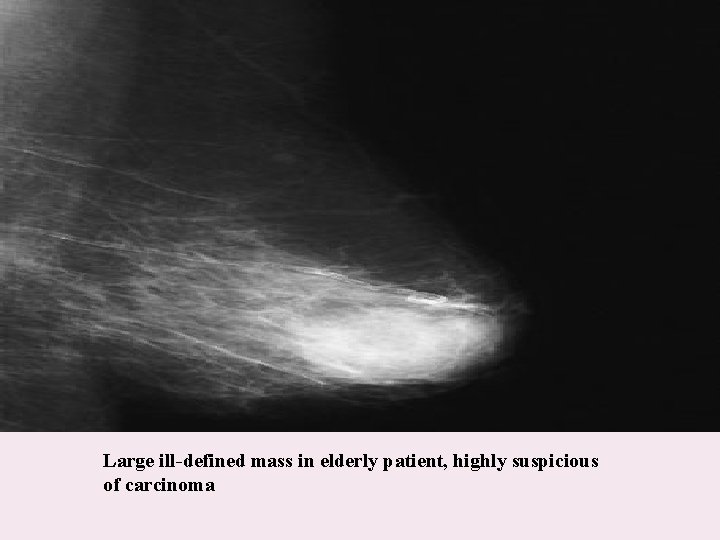
Large ill-defined mass in elderly patient, highly suspicious of carcinoma
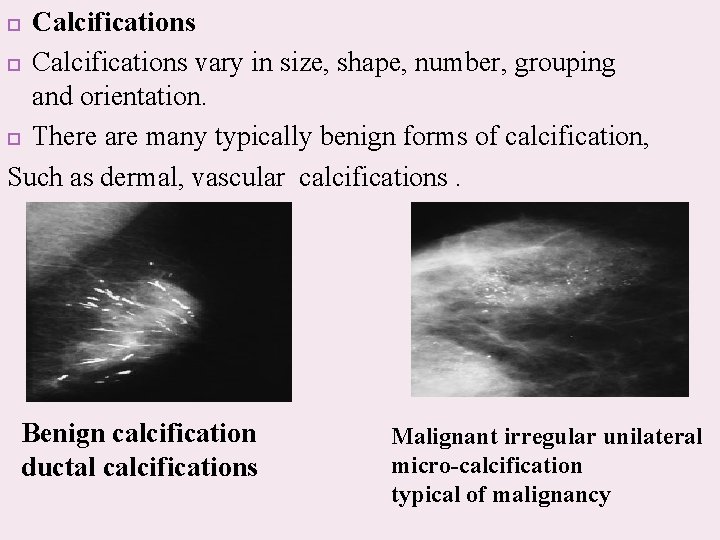
Calcifications vary in size, shape, number, grouping and orientation. There are many typically benign forms of calcification, Such as dermal, vascular calcifications. Benign calcification ductal calcifications Malignant irregular unilateral micro-calcification typical of malignancy
Mammography is used to detect a number of abnormalities, the two main ones being: • Calcifications. • Masses.
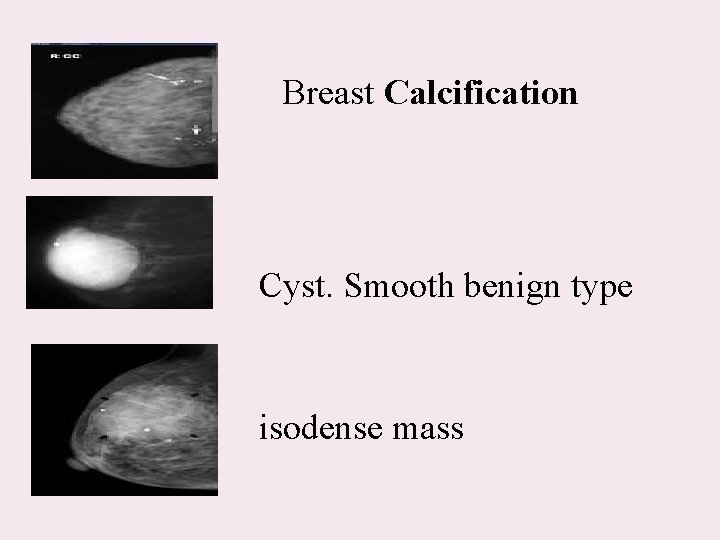
Breast Calcification Cyst. Smooth benign type isodense mass
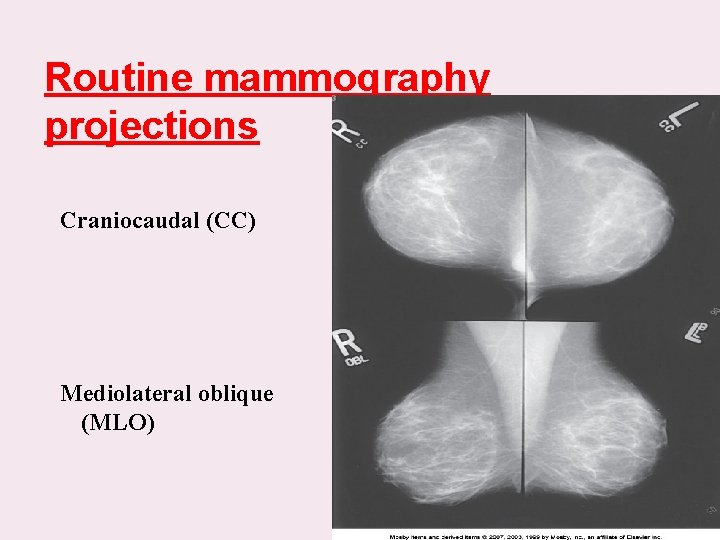
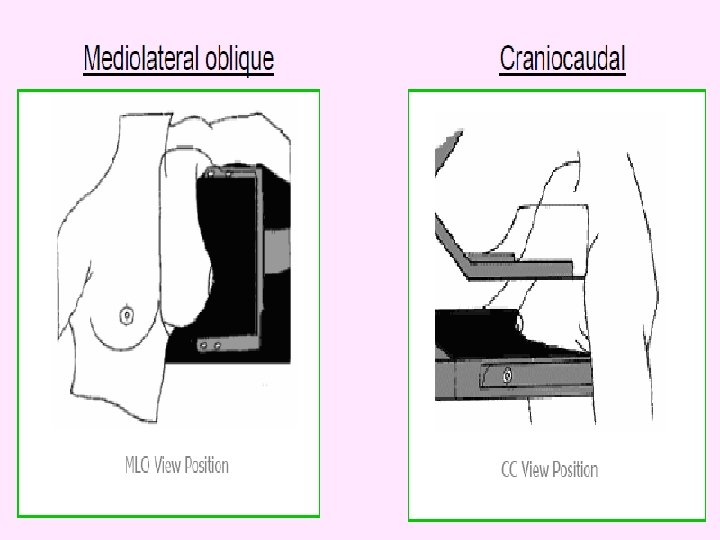
Routine mammography projections Craniocaudal (CC) Mediolateral oblique (MLO)
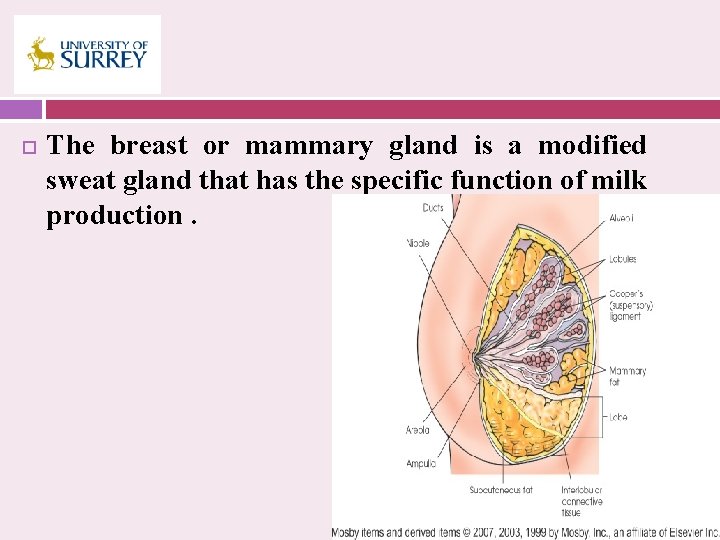
The breast or mammary gland is a modified sweat gland that has the specific function of milk production.
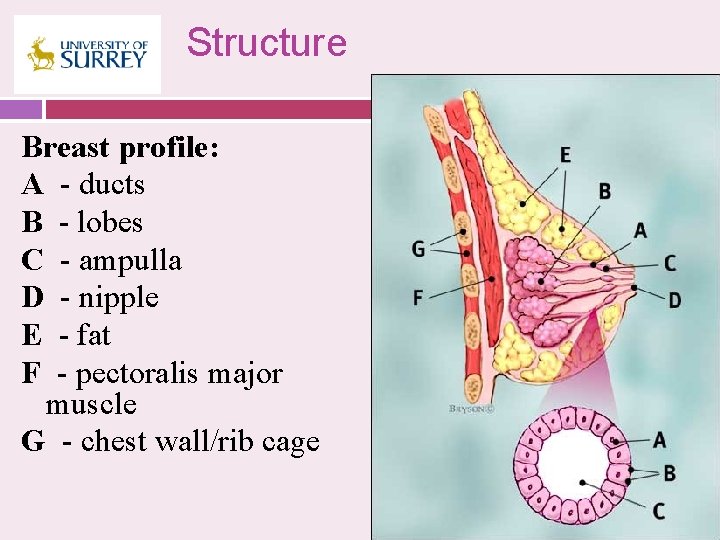
Structure Breast profile: A - ducts B - lobes C - ampulla D - nipple E - fat F - pectoralis major muscle G - chest wall/rib cage
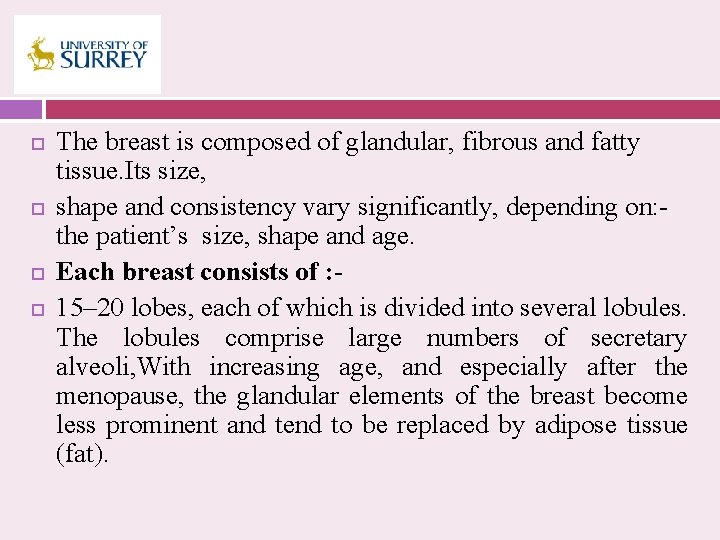
The breast is composed of glandular, fibrous and fatty tissue. Its size, shape and consistency vary significantly, depending on: the patient’s size, shape and age. Each breast consists of : 15– 20 lobes, each of which is divided into several lobules. The lobules comprise large numbers of secretary alveoli, With increasing age, and especially after the menopause, the glandular elements of the breast become less prominent and tend to be replaced by adipose tissue (fat).
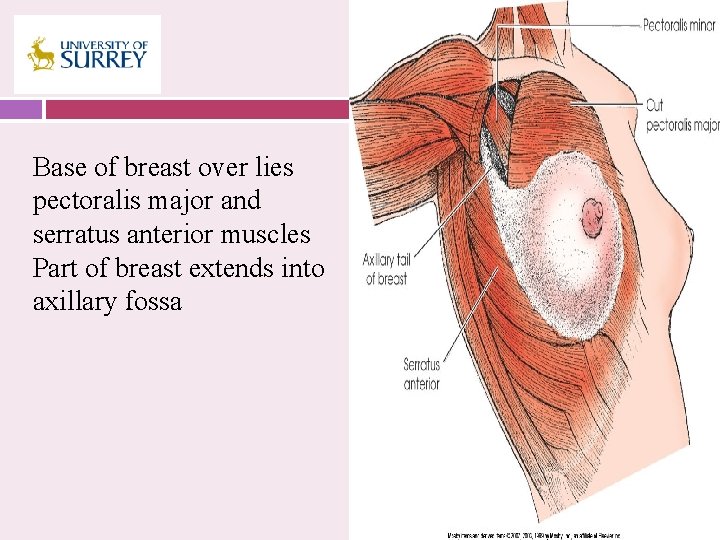
Base of breast over lies pectoralis major and serratus anterior muscles Part of breast extends into axillary fossa
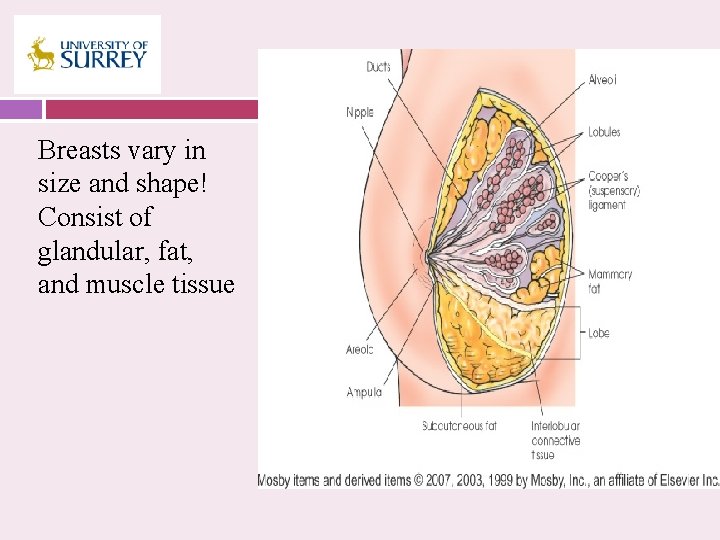
Breasts vary in size and shape! Consist of glandular, fat, and muscle tissue
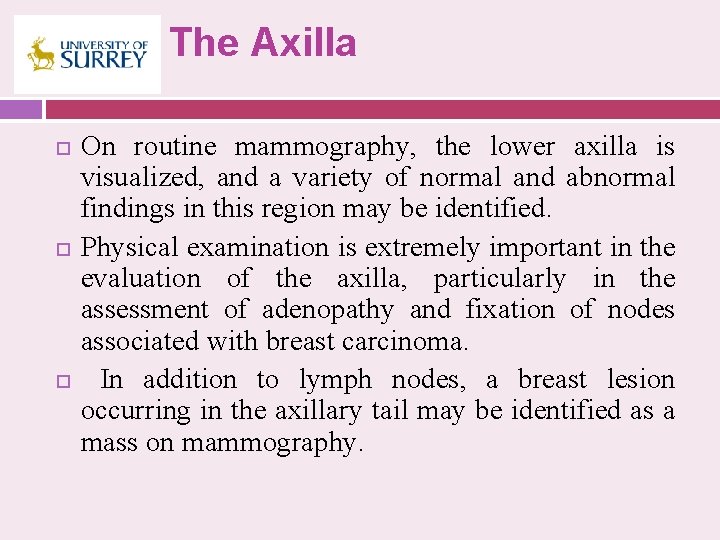
The Axilla On routine mammography, the lower axilla is visualized, and a variety of normal and abnormal findings in this region may be identified. Physical examination is extremely important in the evaluation of the axilla, particularly in the assessment of adenopathy and fixation of nodes associated with breast carcinoma. In addition to lymph nodes, a breast lesion occurring in the axillary tail may be identified as a mass on mammography.
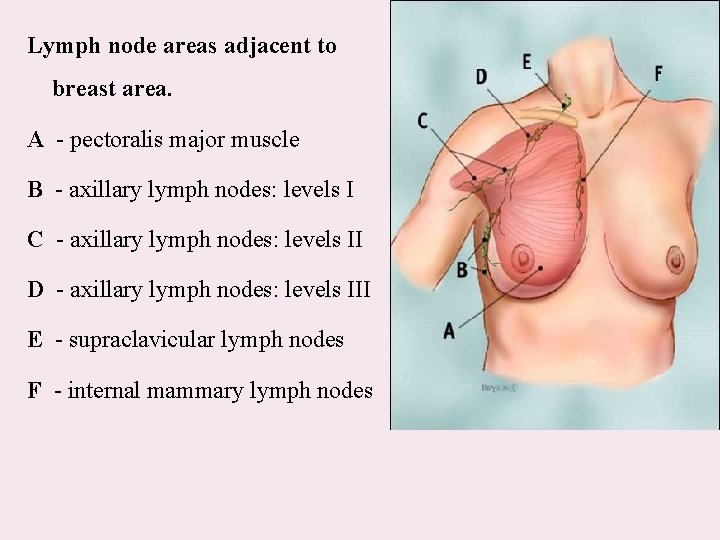
Lymph node areas adjacent to breast area. A - pectoralis major muscle B - axillary lymph nodes: levels I C - axillary lymph nodes: levels II D - axillary lymph nodes: levels III E - supraclavicular lymph nodes F - internal mammary lymph nodes
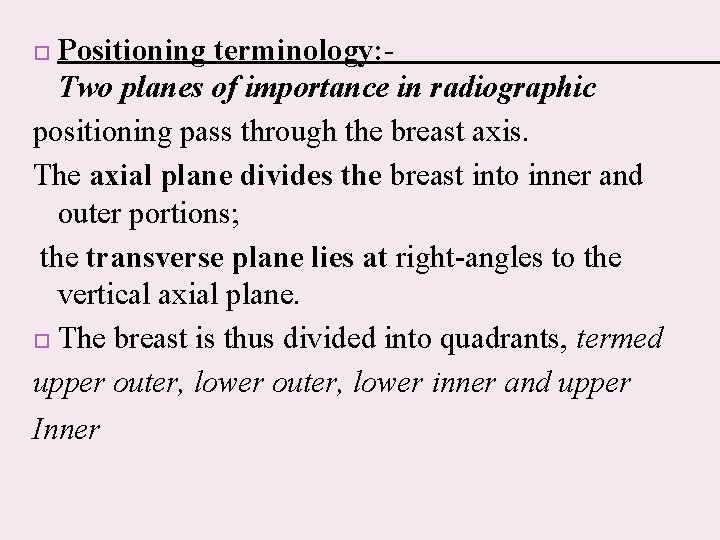
Positioning terminology: Two planes of importance in radiographic positioning pass through the breast axis. The axial plane divides the breast into inner and outer portions; the transverse plane lies at right-angles to the vertical axial plane. The breast is thus divided into quadrants, termed upper outer, lower inner and upper Inner
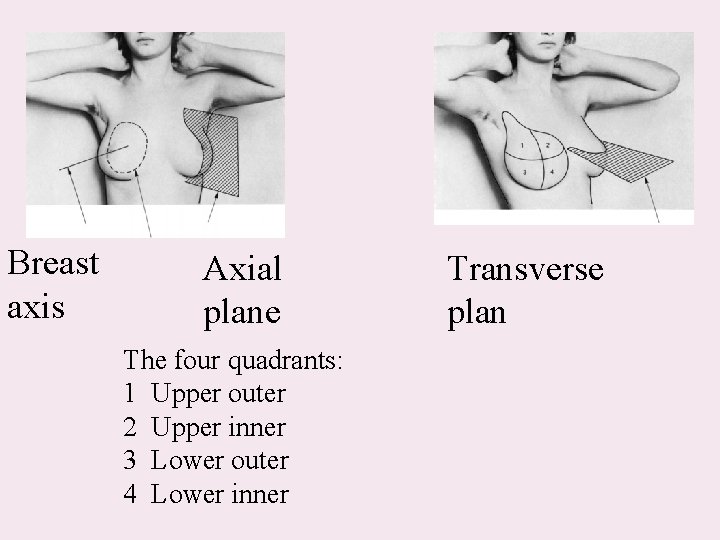
Breast axis Axial plane The four quadrants: 1 Upper outer 2 Upper inner 3 Lower outer 4 Lower inner Transverse plan
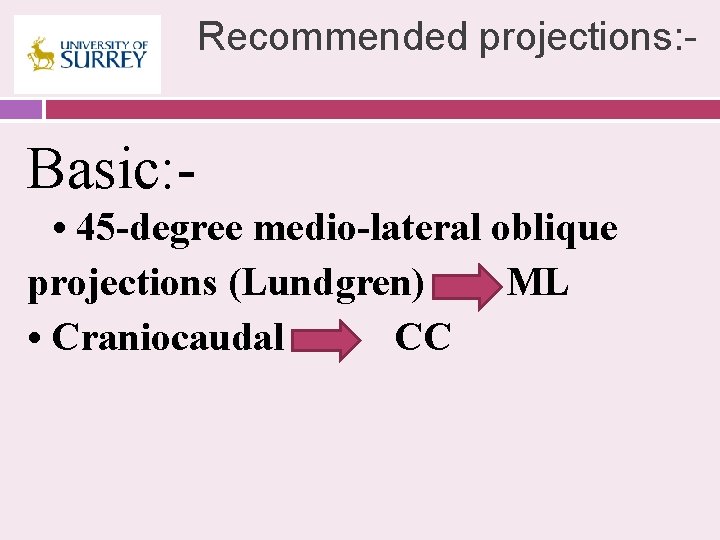
Recommended projections: - Basic: • 45 -degree medio-lateral oblique projections (Lundgren) ML • Craniocaudal CC
Supplementary : • Extended cranio-caudal laterally • Extended cranio-caudal medially rotated • Extended cranio-caudal • Medio-lateral • Latero-medial • Axillary tail
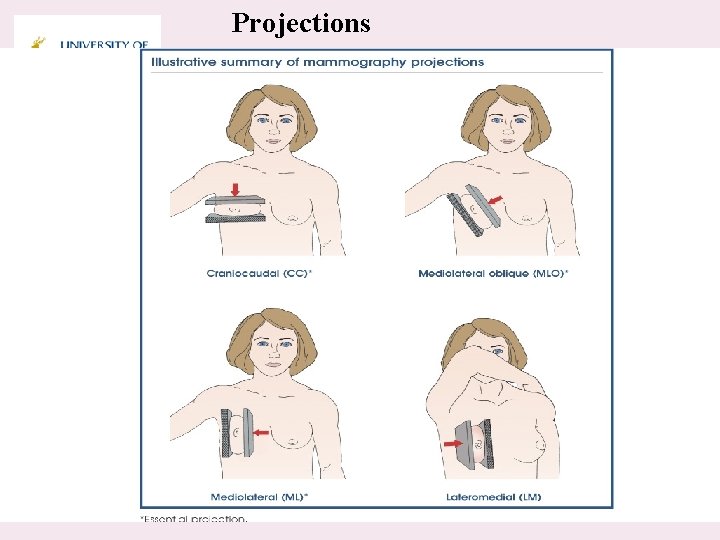
Projections
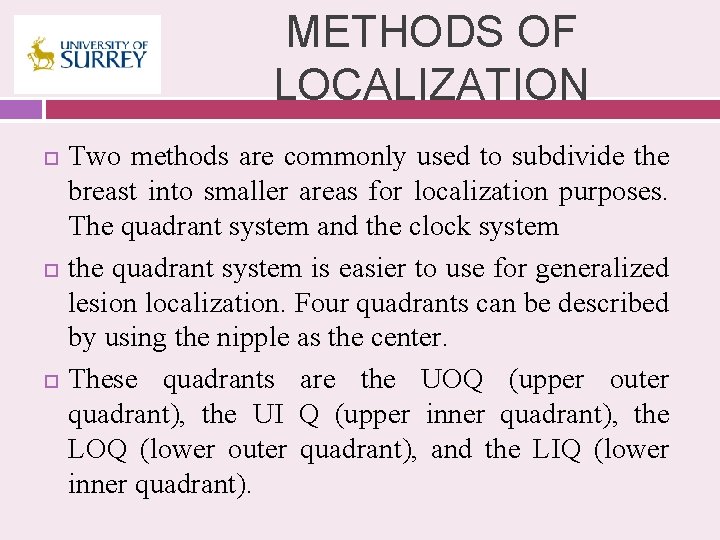
METHODS OF LOCALIZATION Two methods are commonly used to subdivide the breast into smaller areas for localization purposes. The quadrant system and the clock system the quadrant system is easier to use for generalized lesion localization. Four quadrants can be described by using the nipple as the center. These quadrants are the UOQ (upper outer quadrant), the UI Q (upper inner quadrant), the LOQ (lower outer quadrant), and the LIQ (lower inner quadrant).
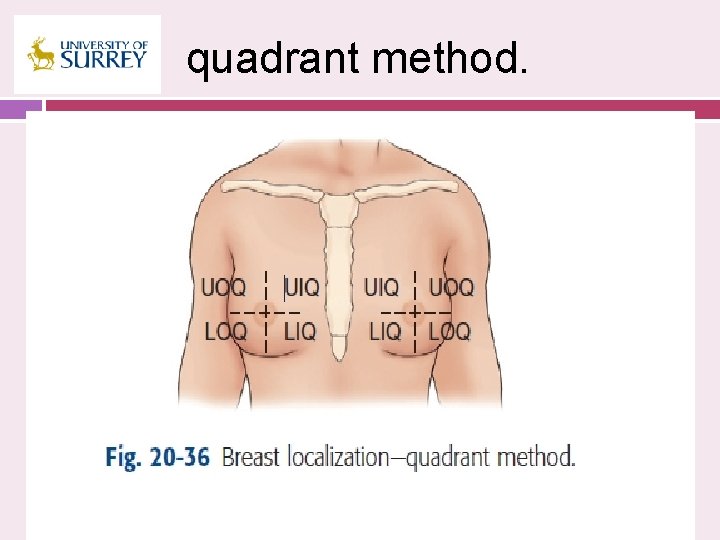
quadrant method.
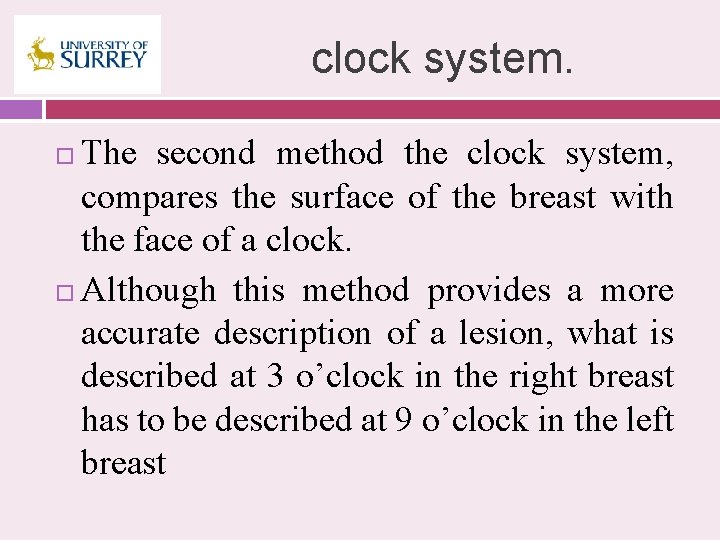
clock system. The second method the clock system, compares the surface of the breast with the face of a clock. Although this method provides a more accurate description of a lesion, what is described at 3 o’clock in the right breast has to be described at 9 o’clock in the left breast
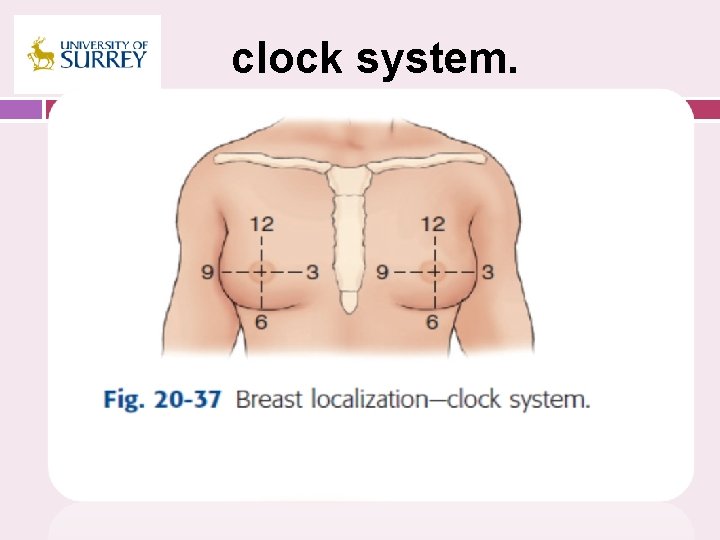
clock system.
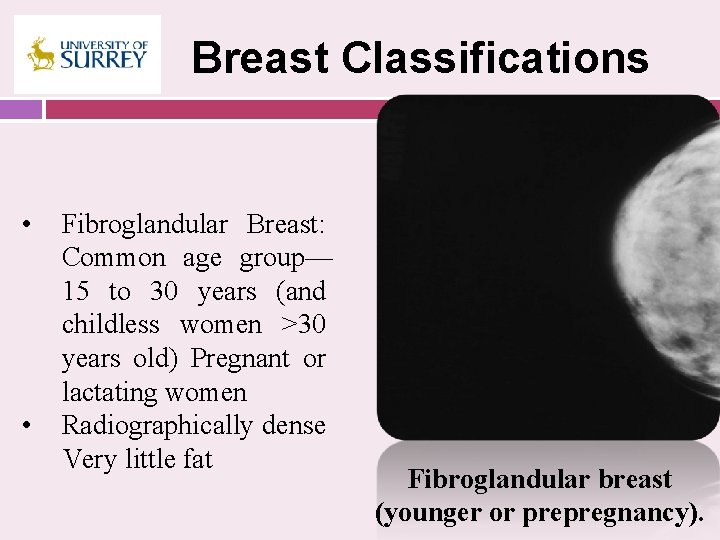
Breast Classifications • • Fibroglandular Breast: Common age group— 15 to 30 years (and childless women >30 years old) Pregnant or lactating women Radiographically dense Very little fat Fibroglandular breast (younger or prepregnancy).
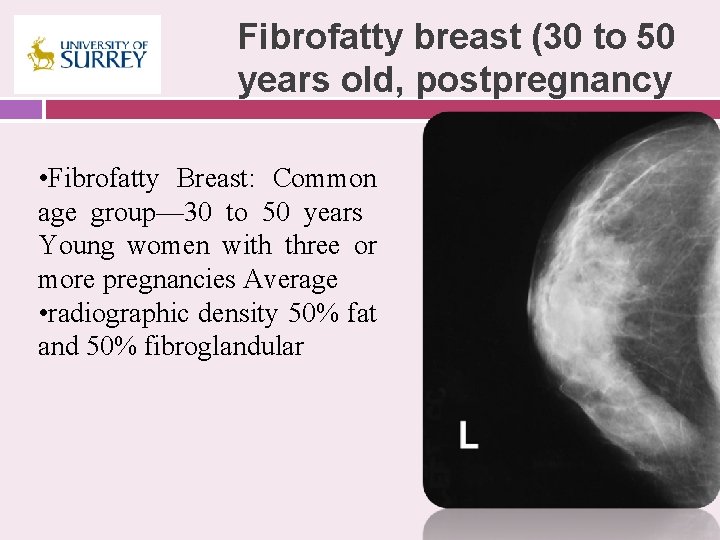
Fibrofatty breast (30 to 50 years old, postpregnancy • Fibrofatty Breast: Common age group— 30 to 50 years Young women with three or more pregnancies Average • radiographic density 50% fat and 50% fibroglandular
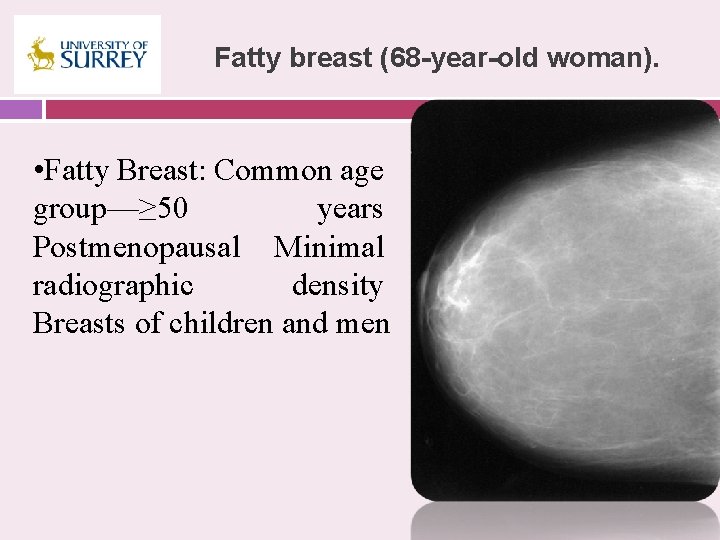
Fatty breast (68 -year-old woman). • Fatty Breast: Common age group—≥ 50 years Postmenopausal Minimal radiographic density Breasts of children and men
Positioning and Technical Considerations Ø Ø Ø PATIENT PREPARATION The technologist explains the procedure and documents any relevant patient history as per departmental protocol. Generally, the patient history includes the following: Number of pregnancies Family history of cancer, including breast cancer (relationship of relative) Medications (e. g. , hormone therapy) currently taken Previous breast surgery Previous mammograms, when and where performed Reason for current visit, such as screening mammogram, lumps, pain, or discharge
BREAST POSITIONING The base of the breast is the portion near the chest wall, and the area near the nipple is termed the apex. In either the craniocaudal(CC) or the mediolateral (ML) projection, the base of the breast is much thicker and contains denser tissues than are found at the apex. To overcome this normal anatomic difference found in the breast, a compression device is used in combination with a specially designed tube, so that the more intense central ray (CR) of the x-ray beam penetrates the thicker base of the breast.
COMPRESSION* Six reasons for the use of compression are as follows: 1. To decrease thickness of the breast and make it more uniform 2. To bring the breast structures as close to the image receptor (IR) as possible 3. To decrease the dose needed and the amount of scattered radiation 4. To decrease motion and geometric unsharpness 5. To increase contrast by allowing a decrease in exposure factors 6. To separate breast structures that may be superimposed
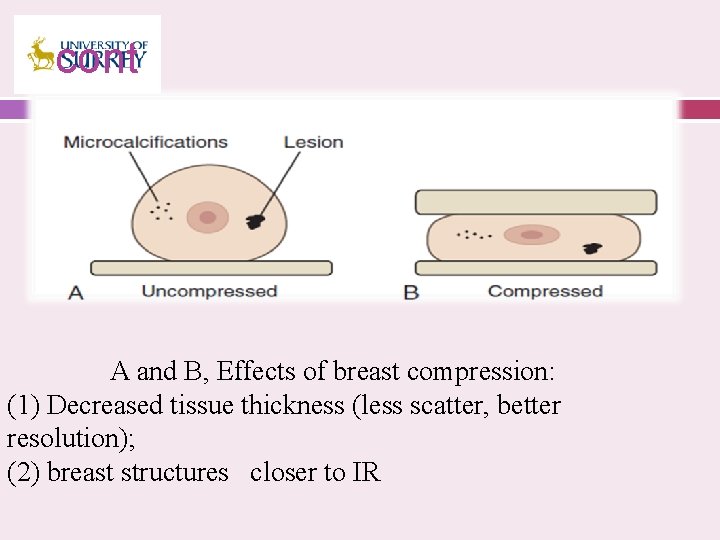
cont A and B, Effects of breast compression: (1) Decreased tissue thickness (less scatter, better resolution); (2) breast structures closer to IR
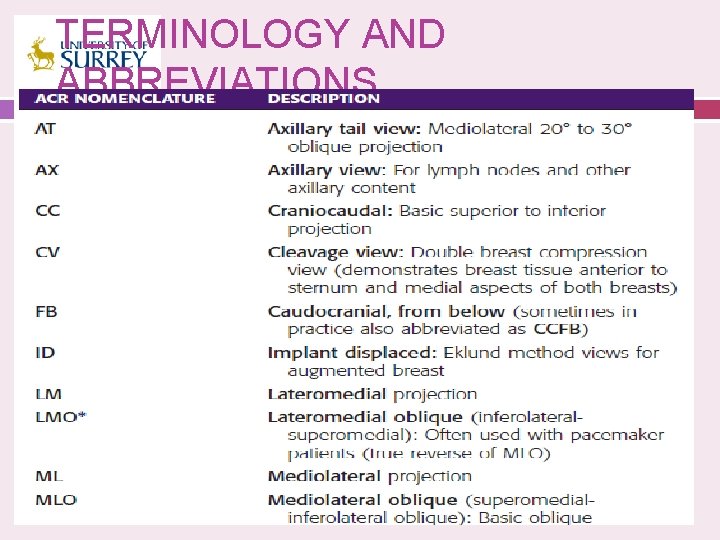
TERMINOLOGY AND ABBREVIATIONS
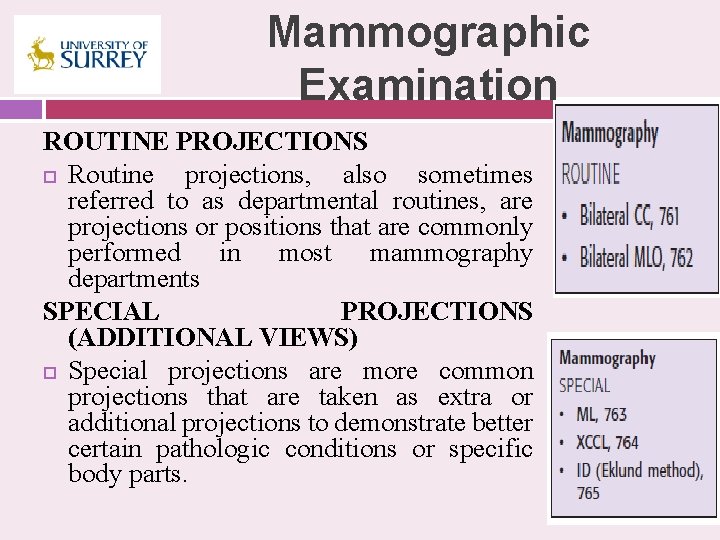
Mammographic Examination ROUTINE PROJECTIONS Routine projections, also sometimes referred to as departmental routines, are projections or positions that are commonly performed in most mammography departments SPECIAL PROJECTIONS (ADDITIONAL VIEWS) Special projections are more common projections that are taken as extra or additional projections to demonstrate better certain pathologic conditions or specific body parts.
THE END
- Slides: 46