MALNUTRITION Screening and referral BALKH Nutrition Team 2014
MALNUTRITION – Screening and referral BALKH Nutrition Team 2014 05 December 2020
Objectives of training § To understand basics about undernutrition: definition, causes and consequences § To know how to perform anthropometric measurements – identify MAM and SAM children / PLW § To know and understand the management of acute malnutrition 05 December 2020 2
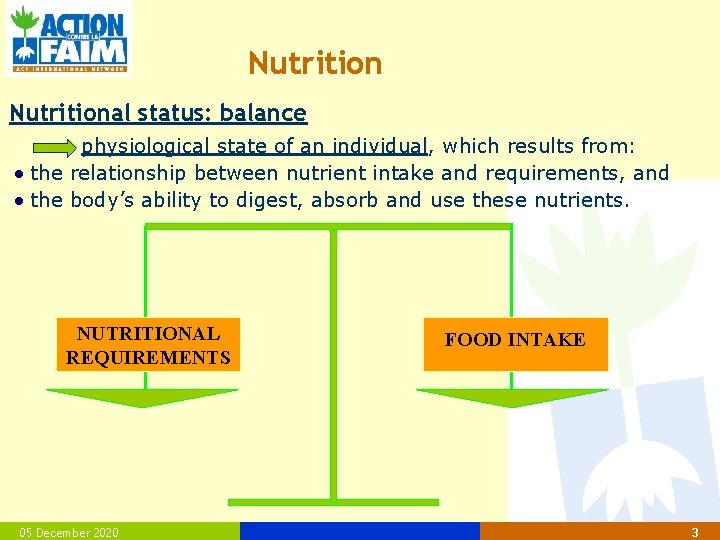
Nutritional status: balance physiological state of an individual, which results from: the relationship between nutrient intake and requirements, and the body’s ability to digest, absorb and use these nutrients. NUTRITIONAL REQUIREMENTS 05 December 2020 FOOD INTAKE 3
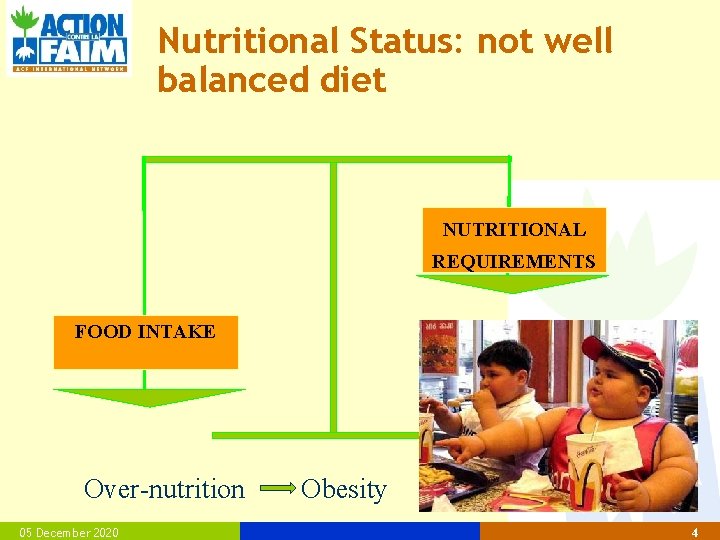
Nutritional Status: not well balanced diet NUTRITIONAL REQUIREMENTS FOOD INTAKE Over-nutrition 05 December 2020 Obesity 4
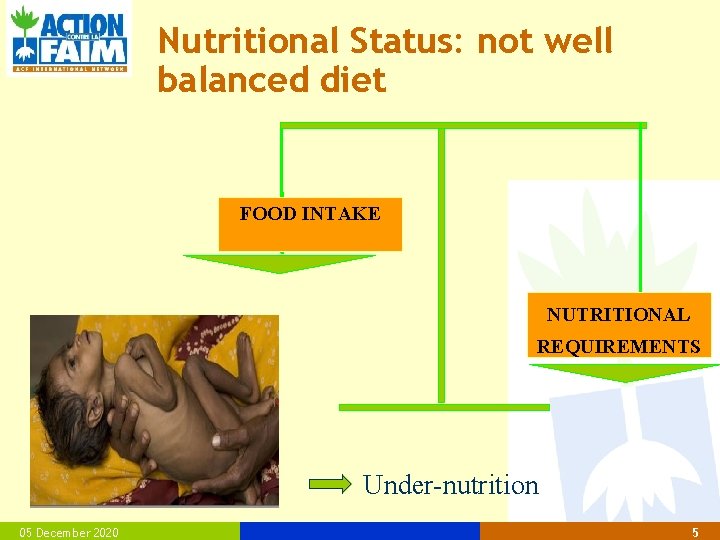
Nutritional Status: not well balanced diet FOOD INTAKE NUTRITIONAL REQUIREMENTS Under-nutrition 05 December 2020 5
Non-balanced nutrition can be caused by : § Sufficient quantity but insufficient quality of food (lack of diversified food) § Sufficient quality but insufficient quantity of food (lack of intake) § Insufficient quantity and quality of food (lack of intake and diversified food) MALNUTRITION : Term for bad nutritional status Definition: situation when the body does not receive the sufficient quantity and/or quality of nutrients. 05 December 2020 6

Food intake § Food intake depends on different factors: • Availability of the food — For example: food available in the market • Accessibility of the food — For example: cost of the food in the market § Possible influences? ? • Harvest, price, soil, culture/beliefs, etc 05 December 2020 7
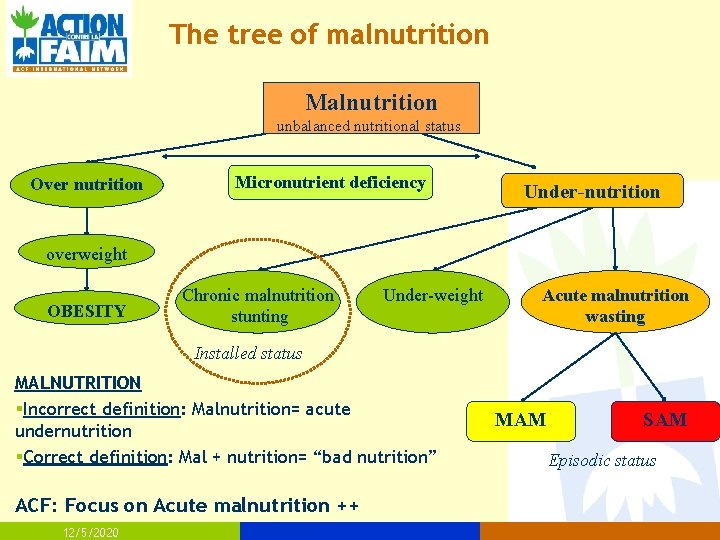
The tree of malnutrition Malnutrition unbalanced nutritional status Over nutrition Micronutrient deficiency Under-nutrition overweight OBESITY Chronic malnutrition stunting Under-weight Acute malnutrition wasting Installed status MALNUTRITION §Incorrect definition: Malnutrition= acute undernutrition §Correct definition: Mal + nutrition= “bad nutrition” ACF: Focus on Acute malnutrition ++ 12/5/2020 MAM SAM Episodic status
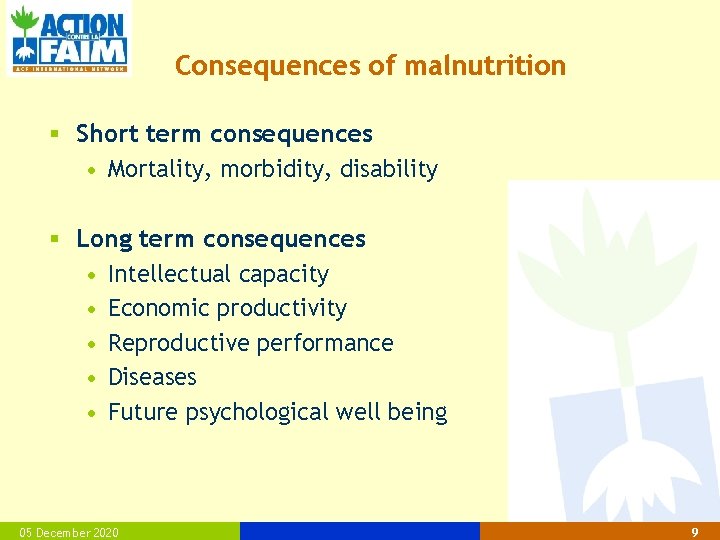
Consequences of malnutrition § Short term consequences • Mortality, morbidity, disability § Long term consequences • Intellectual capacity • Economic productivity • Reproductive performance • Diseases • Future psychological well being 05 December 2020 9
Consequences and risks of malnutrition. . . Lowered resistance to disease Even not dangerous disease becomes dangerous Increased risk of mortality Learning difficulties Reduced physical activity 05 December 2020 10
Acute Malnutrition § Acute Malnutrition = DISEASE § Acute malnutrition • Sudden deprivation / Short-term process • Sudden weight loss • More vulnerable population : Children 659 months and PLW • Consequences if no treatment : DEATH 05 December 2020 11
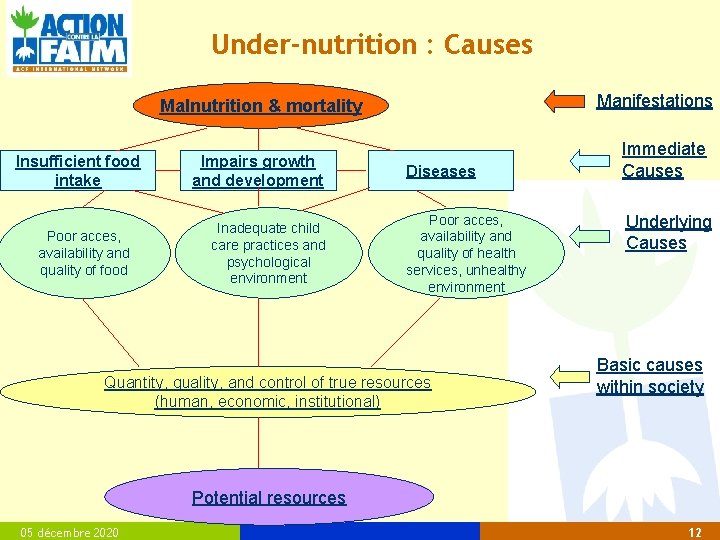
Under-nutrition : Causes Manifestations Malnutrition & mortality Insufficient food intake Poor acces, availability and quality of food Impairs growth and development Inadequate child care practices and psychological environment Diseases Poor acces, availability and quality of health services, unhealthy environment Quantity, quality, and control of true resources (human, economic, institutional) Immediate Causes Underlying Causes Basic causes within society Potential resources 05 décembre 2020 12
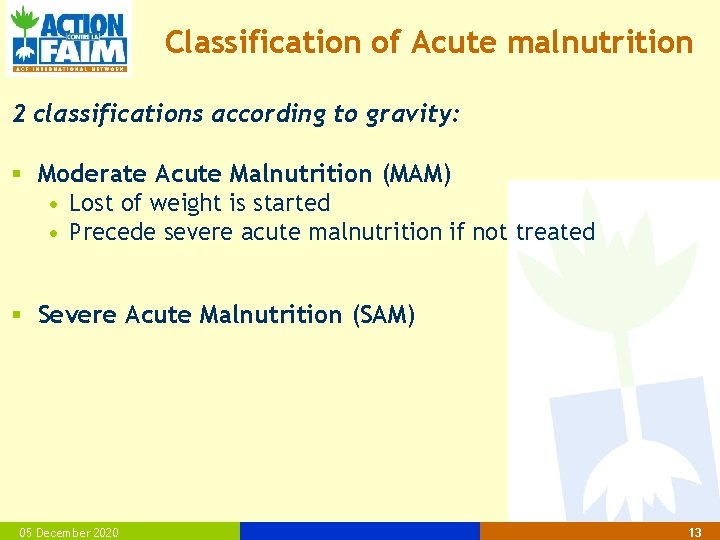
Classification of Acute malnutrition 2 classifications according to gravity: § Moderate Acute Malnutrition (MAM) • Lost of weight is started • Precede severe acute malnutrition if not treated § Severe Acute Malnutrition (SAM) 05 December 2020 13
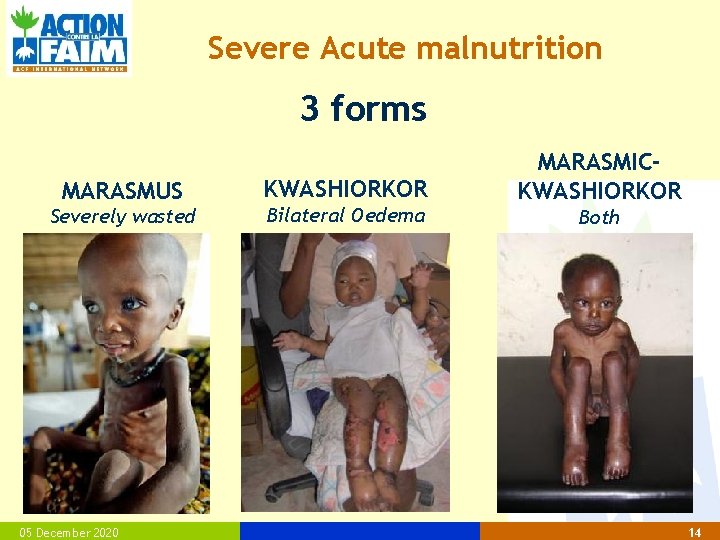
Severe Acute malnutrition 3 forms MARASMUS Severely wasted 05 December 2020 KWASHIORKOR Bilateral Oedema MARASMICKWASHIORKOR Both 14
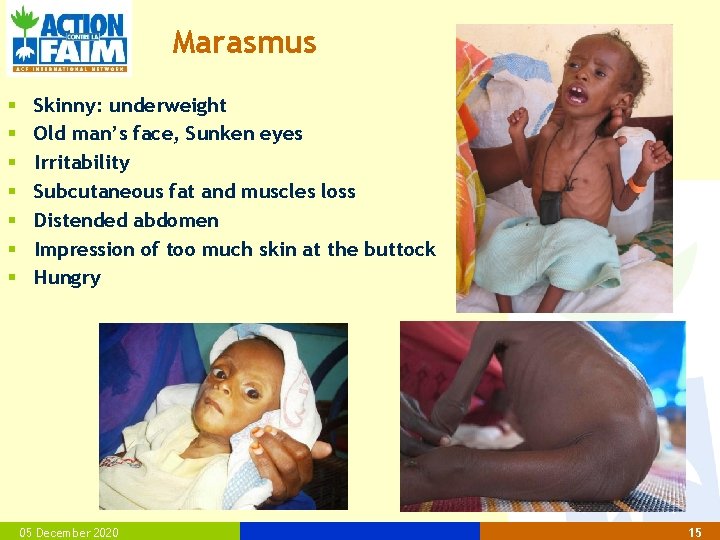
Marasmus § § § § Skinny: underweight Old man’s face, Sunken eyes Irritability Subcutaneous fat and muscles loss Distended abdomen Impression of too much skin at the buttock Hungry 05 December 2020 15
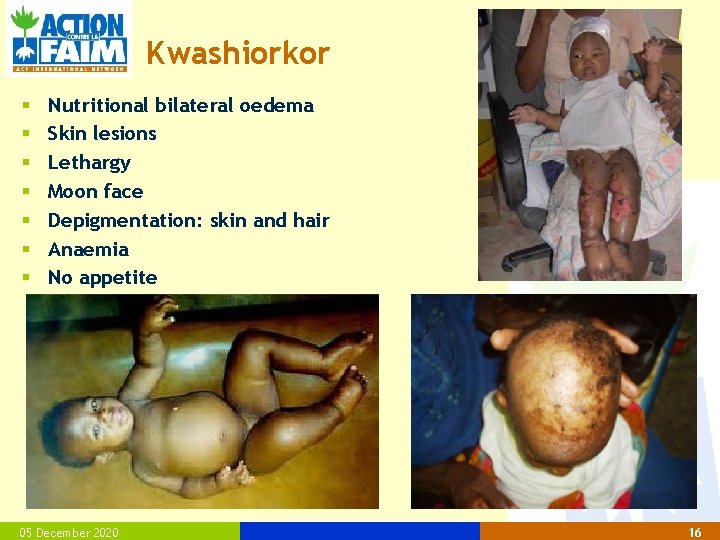
Kwashiorkor § § § § Nutritional bilateral oedema Skin lesions Lethargy Moon face Depigmentation: skin and hair Anaemia No appetite 05 December 2020 16
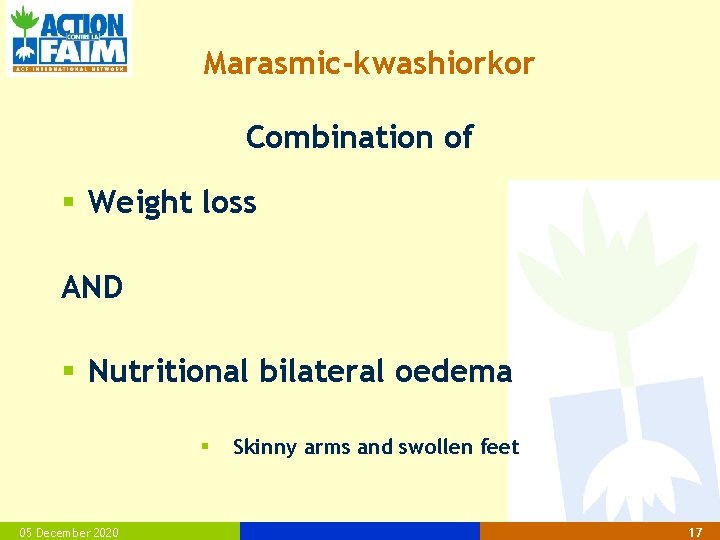
Marasmic-kwashiorkor Combination of § Weight loss AND § Nutritional bilateral oedema § 05 December 2020 Skinny arms and swollen feet 17
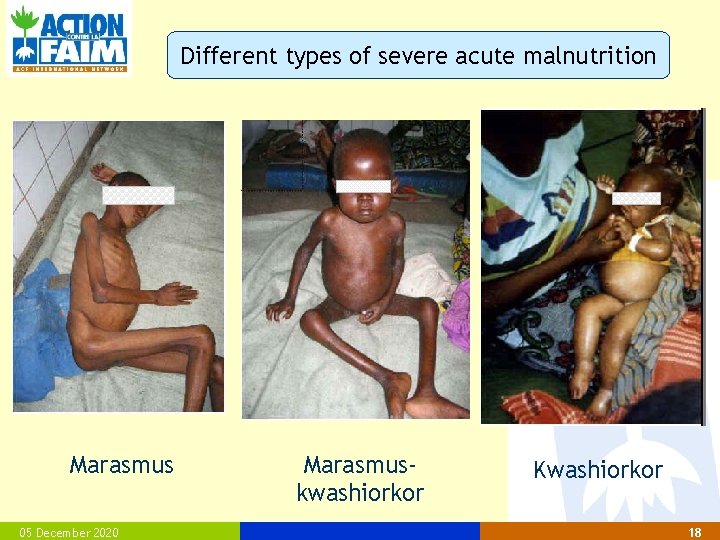
Different types of severe acute malnutrition Marasmus 05 December 2020 Marasmuskwashiorkor Kwashiorkor 18
Acute malnutrition § How can we measure it ? ? 12/5/2020
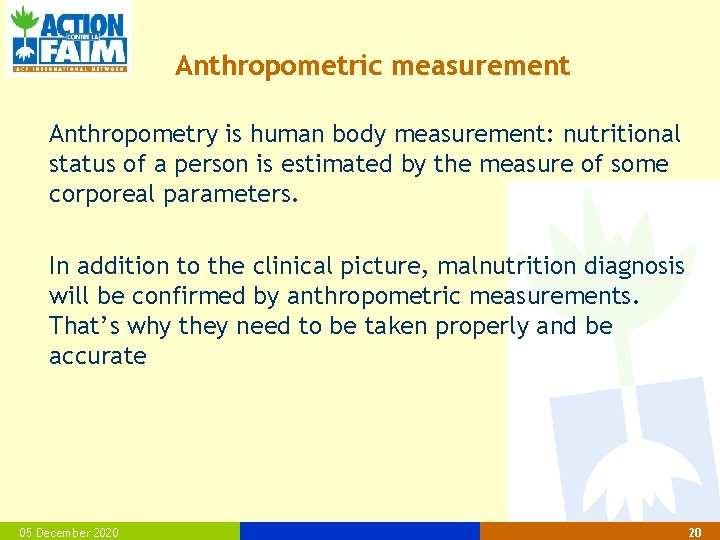
Anthropometric measurement Anthropometry is human body measurement: nutritional status of a person is estimated by the measure of some corporeal parameters. In addition to the clinical picture, malnutrition diagnosis will be confirmed by anthropometric measurements. That’s why they need to be taken properly and be accurate 05 December 2020 20
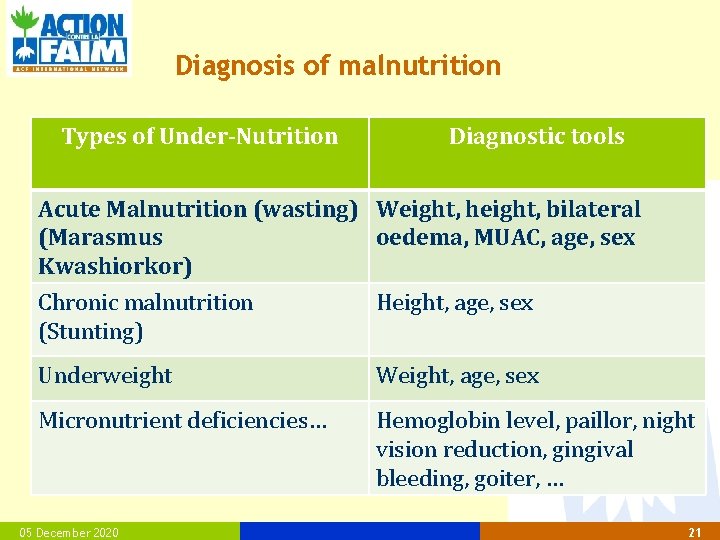
Diagnosis of malnutrition Types of Under-Nutrition Diagnostic tools Acute Malnutrition (wasting) Weight, height, bilateral (Marasmus oedema, MUAC, age, sex Kwashiorkor) Chronic malnutrition (Stunting) Height, age, sex Underweight Weight, age, sex Micronutrient deficiencies… Hemoglobin level, paillor, night vision reduction, gingival bleeding, goiter, … 05 December 2020 21
Anthropometric measurements What is necessary to do a good anthropometric measurement? § Good measurement equipment § Standardized measurement procedure § Well trained personnel § … 05 December 2020 22
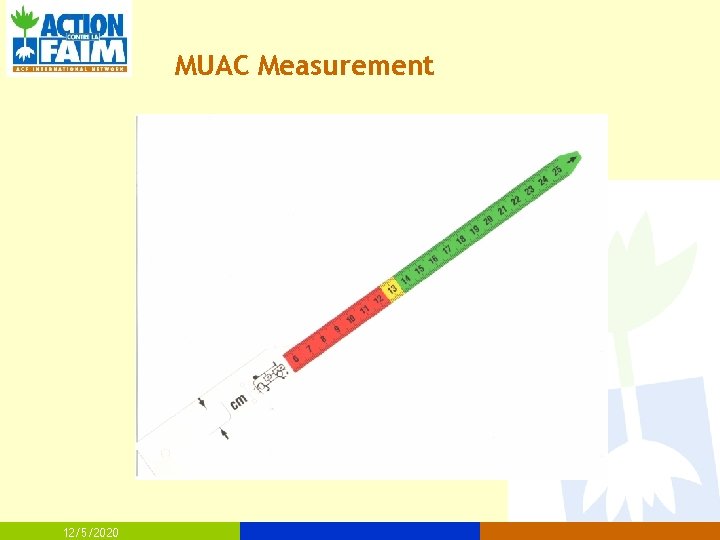
MUAC Measurement 12/5/2020
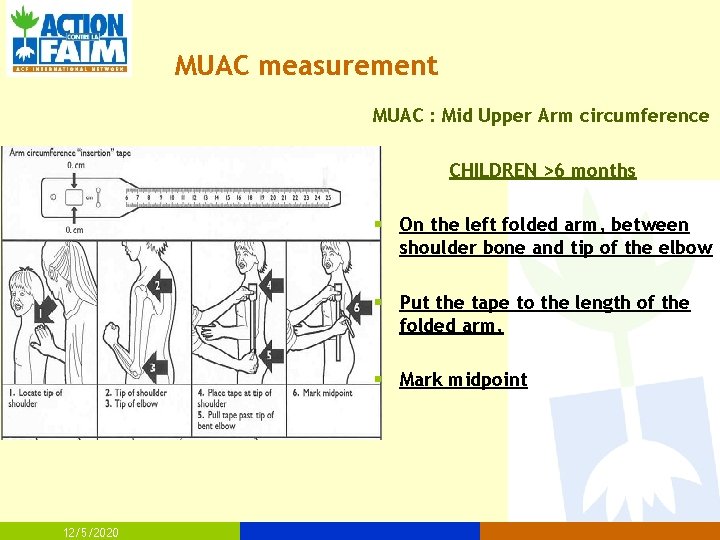
MUAC measurement MUAC : Mid Upper Arm circumference CHILDREN >6 months § On the left folded arm, between shoulder bone and tip of the elbow § Put the tape to the length of the folded arm, § Mark midpoint 12/5/2020
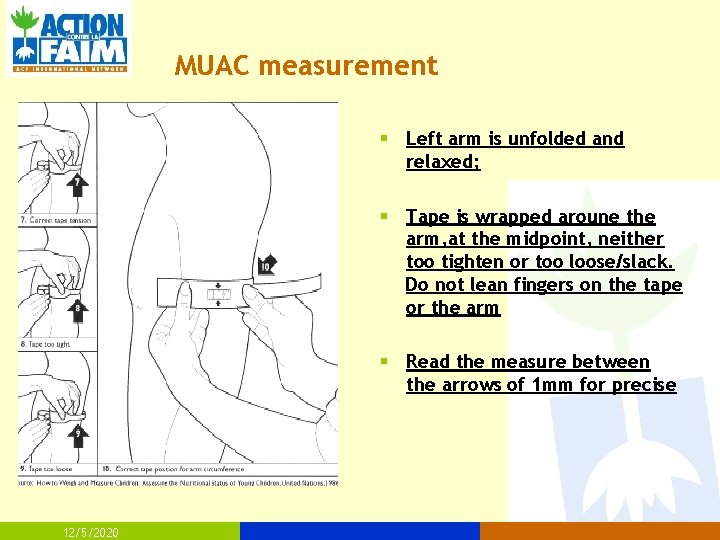
MUAC measurement § Left arm is unfolded and relaxed; § Tape is wrapped aroune the arm, at the midpoint, neither too tighten or too loose/slack. Do not lean fingers on the tape or the arm § Read the measure between the arrows of 1 mm for precise 12/5/2020
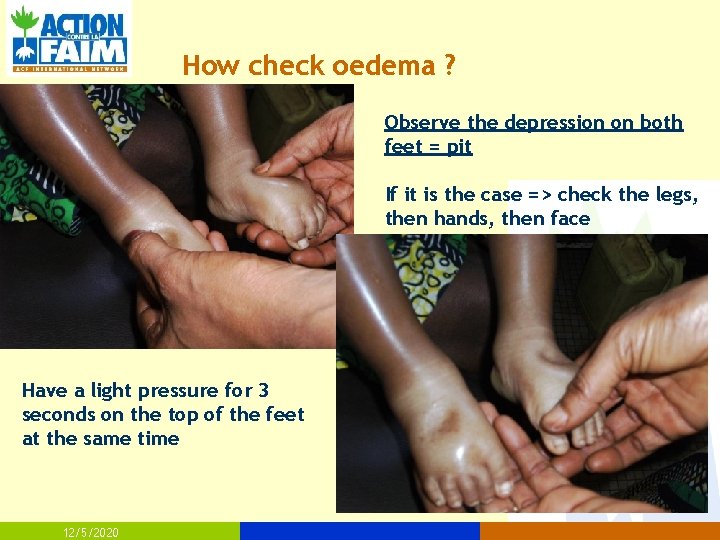
How check oedema ? Observe the depression on both feet = pit If it is the case => check the legs, then hands, then face Have a light pressure for 3 seconds on the top of the feet at the same time 12/5/2020
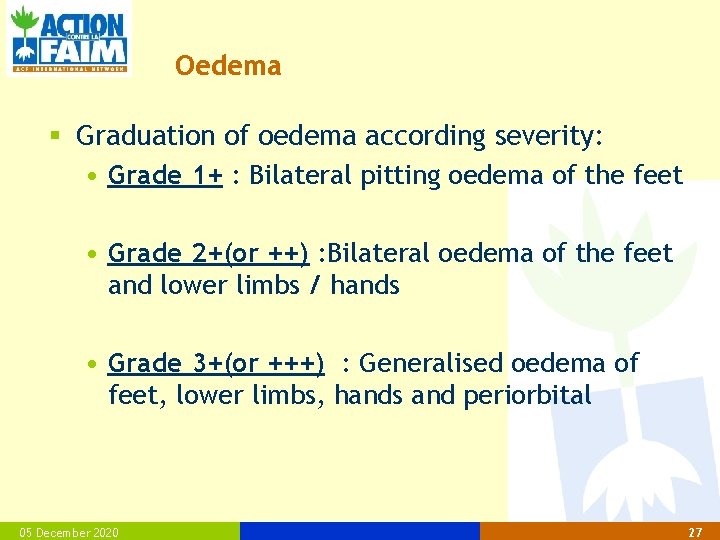
Oedema § Graduation of oedema according severity: • Grade 1+ : Bilateral pitting oedema of the feet • Grade 2+(or ++) : Bilateral oedema of the feet and lower limbs / hands • Grade 3+(or +++) : Generalised oedema of feet, lower limbs, hands and periorbital 05 December 2020 27
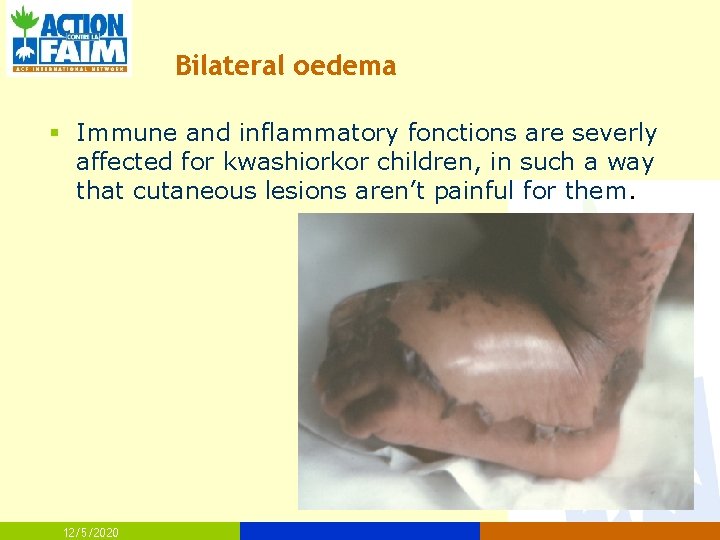
Bilateral oedema § Immune and inflammatory fonctions are severly affected for kwashiorkor children, in such a way that cutaneous lesions aren’t painful for them. 12/5/2020
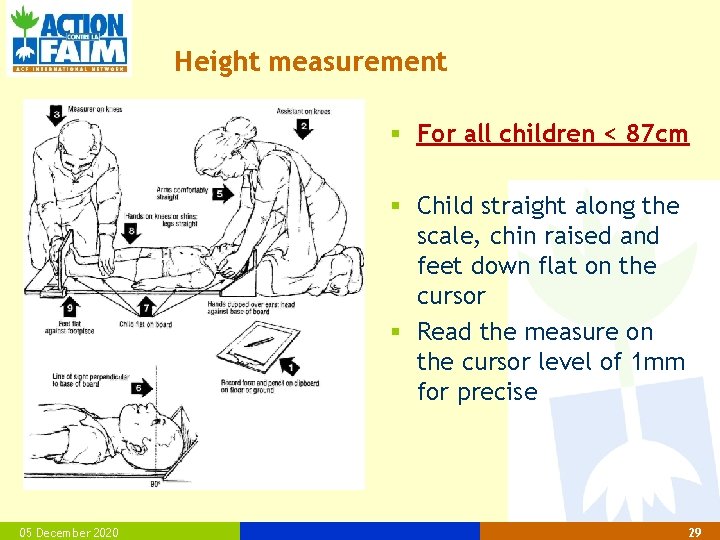
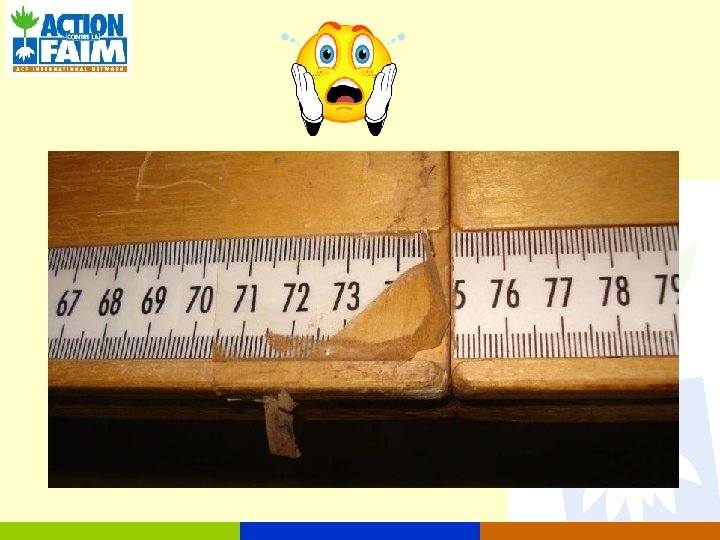
Height measurement § For all children < 87 cm § Child straight along the scale, chin raised and feet down flat on the cursor § Read the measure on the cursor level of 1 mm for precise 05 December 2020 29
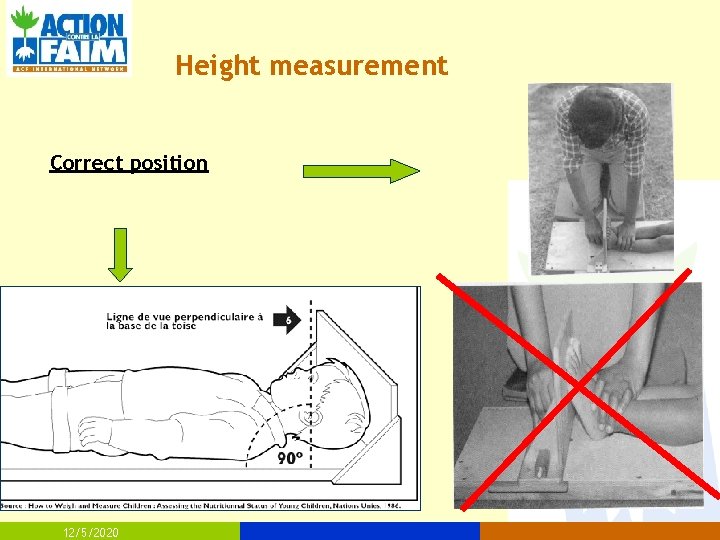
Height measurement Correct position 12/5/2020
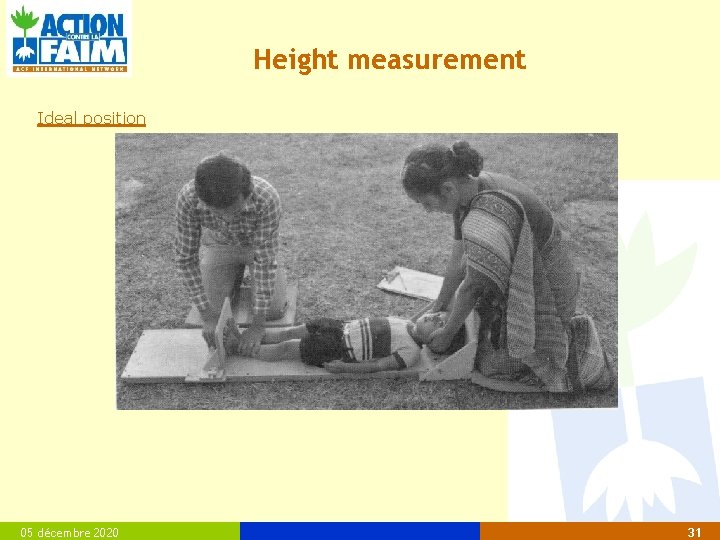
Height measurement Ideal position 05 décembre 2020 31
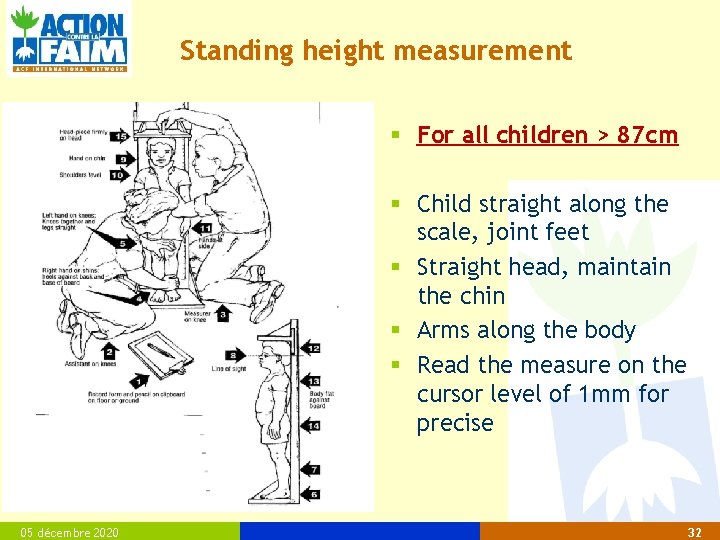
Standing height measurement § For all children > 87 cm § Child straight along the scale, joint feet § Straight head, maintain the chin § Arms along the body § Read the measure on the cursor level of 1 mm for precise 05 décembre 2020 32
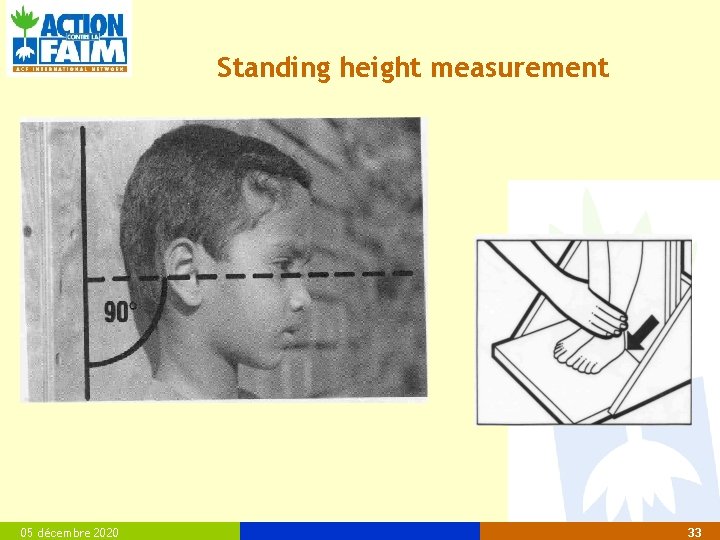
Standing height measurement 05 décembre 2020 33
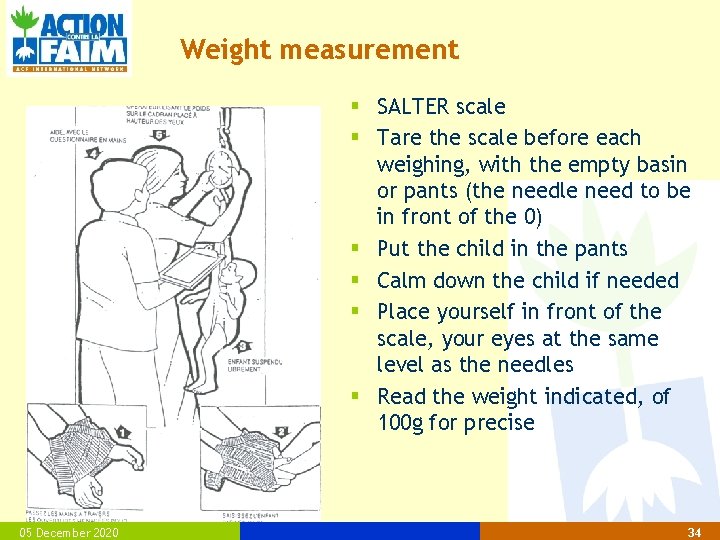
Weight measurement § SALTER scale § Tare the scale before each weighing, with the empty basin or pants (the needle need to be in front of the 0) § Put the child in the pants § Calm down the child if needed § Place yourself in front of the scale, your eyes at the same level as the needles § Read the weight indicated, of 100 g for precise 05 December 2020 34
What are the common mistakes? 05 December 2020 35







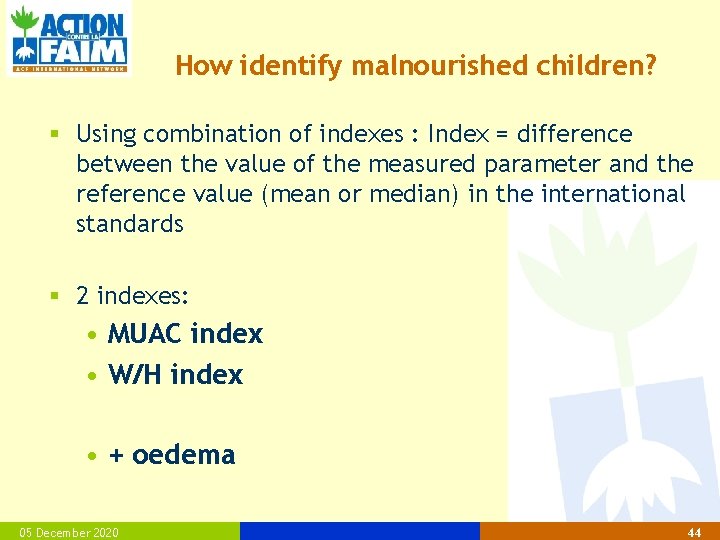
How identify malnourished children? § Using combination of indexes : Index = difference between the value of the measured parameter and the reference value (mean or median) in the international standards § 2 indexes: • MUAC index • W/H index • + oedema 05 December 2020 44
Weight for Height § Emaciated child has a lower weight than a « standard » child, who has the same Height and Sex. § Weight for Height (W/H) measure the child’s corpulence. § Weight gain is sensitive to the actual situation. § So W/H reflects a recent situation. § It is a reliable and admitted. § Doesnt require age estimation § It is used for show recent food or health situation. 05 décembre 2020 45
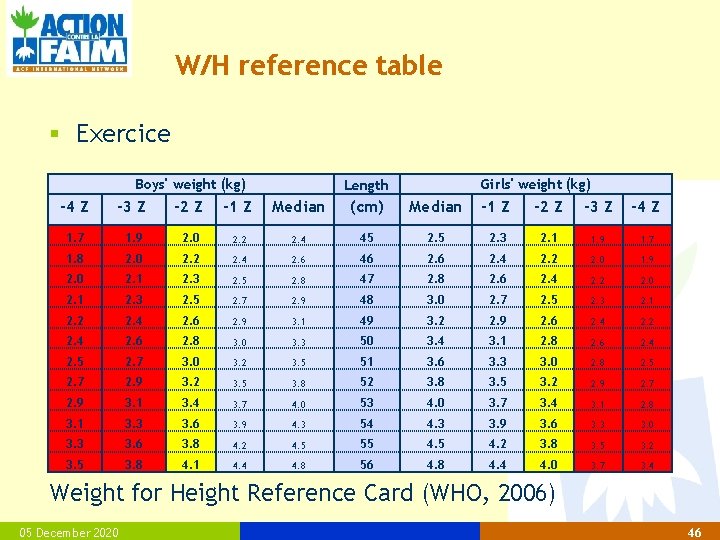
W/H reference table § Exercice Boys' weight (kg) -4 Z -3 Z 1. 7 1. 9 2. 0 2. 2 1. 8 2. 0 2. 2 2. 0 2. 1 Girls' weight (kg) Length -2 Z -1 Z Median (cm) Median -1 Z -2 Z -3 Z -4 Z 2. 4 45 2. 3 2. 1 1. 9 1. 7 2. 4 2. 6 46 2. 4 2. 2 2. 0 1. 9 2. 3 2. 5 2. 8 47 2. 8 2. 6 2. 4 2. 2 2. 0 2. 3 2. 5 2. 7 2. 9 48 3. 0 2. 7 2. 5 2. 3 2. 1 2. 2 2. 4 2. 6 2. 9 3. 1 49 3. 2 2. 9 2. 6 2. 4 2. 2 2. 4 2. 6 2. 8 3. 0 3. 3 50 3. 4 3. 1 2. 8 2. 6 2. 4 2. 5 2. 7 3. 0 3. 2 3. 5 51 3. 6 3. 3 3. 0 2. 8 2. 5 2. 7 2. 9 3. 2 3. 5 3. 8 52 3. 8 3. 5 3. 2 2. 9 2. 7 2. 9 3. 1 3. 4 3. 7 4. 0 53 4. 0 3. 7 3. 4 3. 1 2. 8 3. 1 3. 3 3. 6 3. 9 4. 3 54 4. 3 3. 9 3. 6 3. 3 3. 0 3. 3 3. 6 3. 8 4. 2 4. 5 55 4. 2 3. 8 3. 5 3. 2 3. 5 3. 8 4. 1 4. 4 4. 8 56 4. 8 4. 4 4. 0 3. 7 3. 4 Weight for Height Reference Card (WHO, 2006) 05 December 2020 46
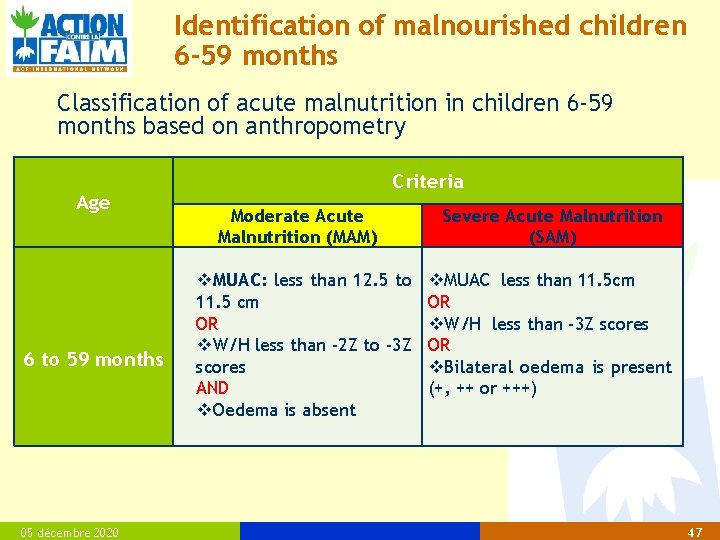
Identification of malnourished children 6 -59 months Classification of acute malnutrition in children 6 -59 months based on anthropometry Age 6 to 59 months 05 décembre 2020 Criteria Moderate Acute Malnutrition (MAM) MUAC: less than 12. 5 to 11. 5 cm OR W/H less than -2 Z to -3 Z scores AND Oedema is absent Severe Acute Malnutrition (SAM) MUAC less than 11. 5 cm OR W/H less than -3 Z scores OR Bilateral oedema is present (+, ++ or +++) 47
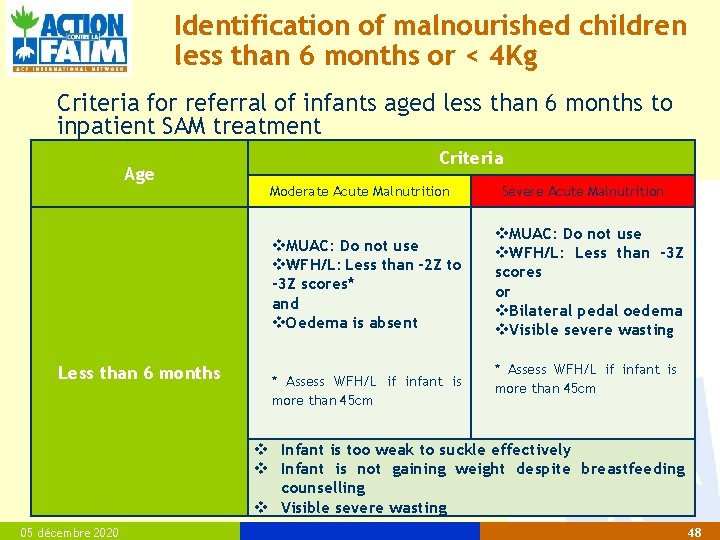
Identification of malnourished children less than 6 months or < 4 Kg Criteria for referral of infants aged less than 6 months to inpatient SAM treatment Age Less than 6 months Criteria Moderate Acute Malnutrition Severe Acute Malnutrition MUAC: Do not use WFH/L: Less than -2 Z to -3 Z scores* and Oedema is absent MUAC: Do not use WFH/L: Less than -3 Z scores or Bilateral pedal oedema Visible severe wasting * Assess WFH/L if infant is more than 45 cm Infant is too weak to suckle effectively Infant is not gaining weight despite breastfeeding counselling Visible severe wasting 05 décembre 2020 48
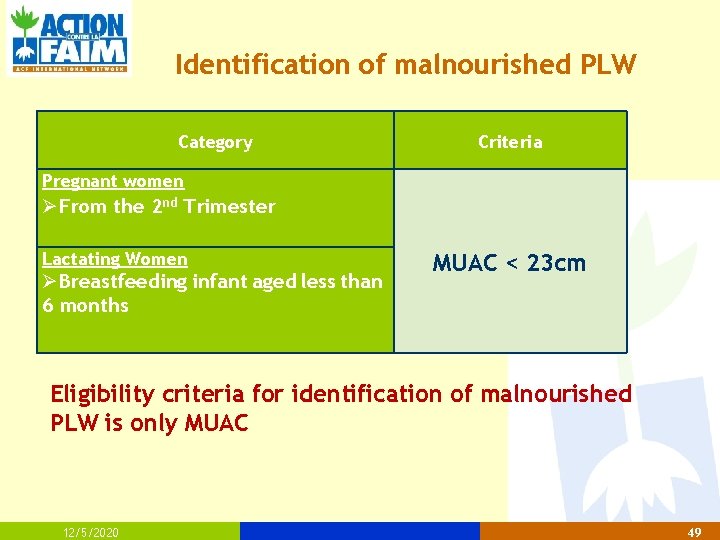
Identification of malnourished PLW Category Criteria Pregnant women From the 2 nd Trimester Lactating Women Breastfeeding infant aged less than 6 months MUAC < 23 cm Eligibility criteria for identification of malnourished PLW is only MUAC 12/5/2020 49
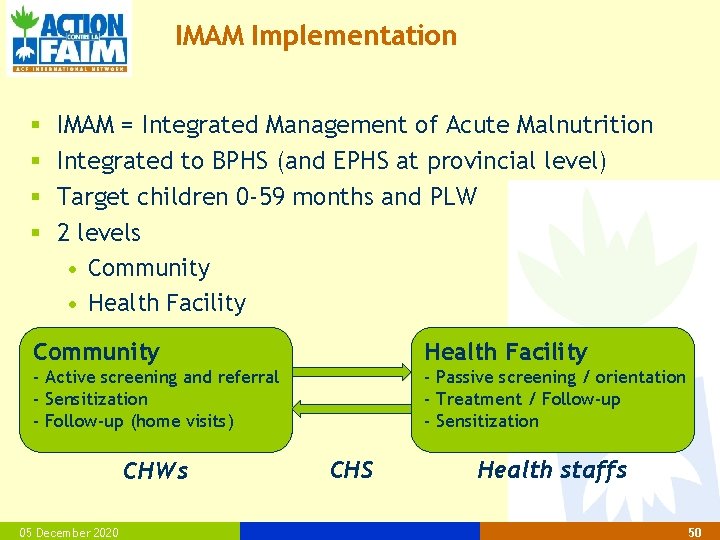
IMAM Implementation § § IMAM = Integrated Management of Acute Malnutrition Integrated to BPHS (and EPHS at provincial level) Target children 0 -59 months and PLW 2 levels • Community • Health Facility Community Health Facility - Active screening and referral - Sensitization - Follow-up (home visits) - Passive screening / orientation - Treatment / Follow-up - Sensitization CHWs 05 December 2020 CHS Health staffs 50

IMAM Implementation : COMMUNITY Goals of community outreach 1. Maximize coverage and access 2. Maximize the timeliness of treatment 3. Maximize compliance with treatment 05 December 2020 51
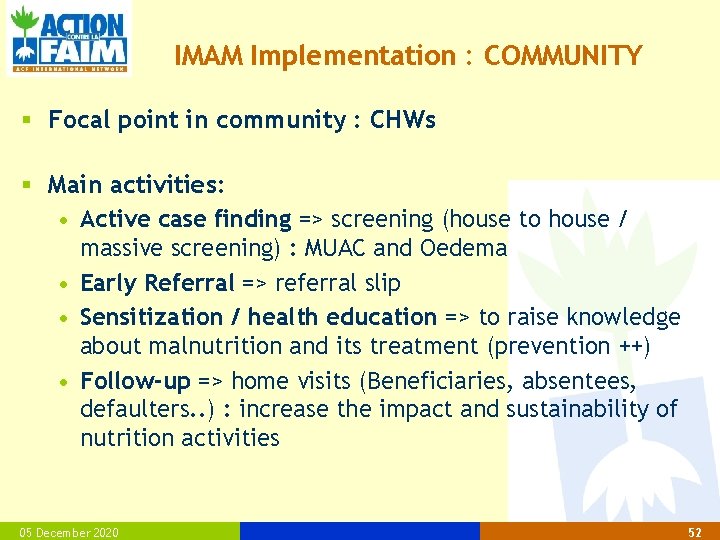
IMAM Implementation : COMMUNITY § Focal point in community : CHWs § Main activities: • Active case finding => screening (house to house / massive screening) : MUAC and Oedema • Early Referral => referral slip • Sensitization / health education => to raise knowledge about malnutrition and its treatment (prevention ++) • Follow-up => home visits (Beneficiaries, absentees, defaulters. . ) : increase the impact and sustainability of nutrition activities 05 December 2020 52
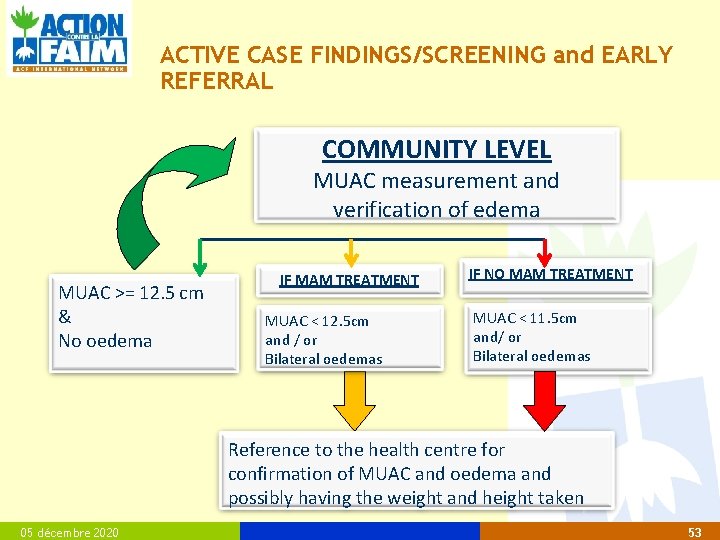
ACTIVE CASE FINDINGS/SCREENING and EARLY REFERRAL COMMUNITY LEVEL MUAC measurement and verification of edema MUAC >= 12. 5 cm & No oedema IF MAM TREATMENT MUAC < 12. 5 cm and / or Bilateral oedemas IF NO MAM TREATMENT MUAC < 11. 5 cm and/ or Bilateral oedemas Reference to the health centre for confirmation of MUAC and oedema and possibly having the weight and height taken 05 décembre 2020 53
IT IS ALSO… § The HOME VISITS for the high-risk cases Non-response/ absents/ defaulters of the program… § AWARENESS SESSIONS/SENSITIZATION/HEALTH EDUCATION Nutrition, health, hygiene promotion. . . 05 décembre 2020 © ACF, Christina Lionnet - Tchad 54
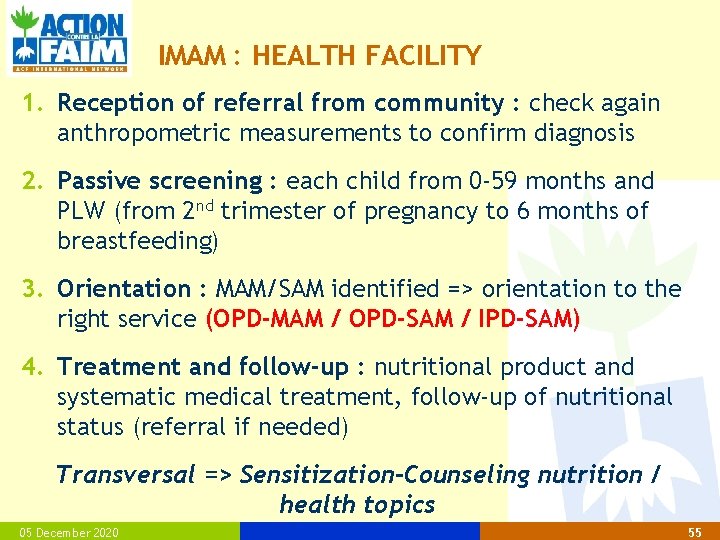
IMAM : HEALTH FACILITY 1. Reception of referral from community : check again anthropometric measurements to confirm diagnosis 2. Passive screening : each child from 0 -59 months and PLW (from 2 nd trimester of pregnancy to 6 months of breastfeeding) 3. Orientation : MAM/SAM identified => orientation to the right service (OPD-MAM / OPD-SAM / IPD-SAM) 4. Treatment and follow-up : nutritional product and systematic medical treatment, follow-up of nutritional status (referral if needed) Transversal => Sensitization-Counseling nutrition / health topics 05 December 2020 55
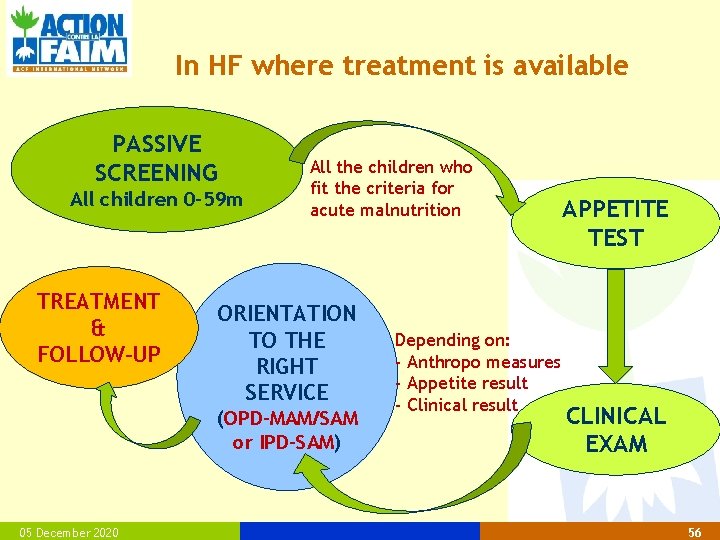
In HF where treatment is available PASSIVE SCREENING All children 0 -59 m TREATMENT & FOLLOW-UP All the children who fit the criteria for acute malnutrition ORIENTATION TO THE RIGHT SERVICE (OPD-MAM/SAM or IPD-SAM) 05 December 2020 Depending on: - Anthropo measures - Appetite result - Clinical result APPETITE TEST CLINICAL EXAM 56
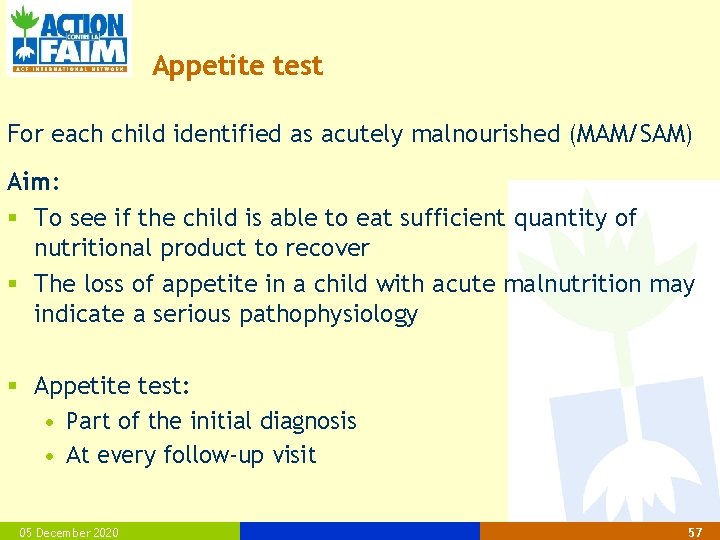
Appetite test For each child identified as acutely malnourished (MAM/SAM) Aim: § To see if the child is able to eat sufficient quantity of nutritional product to recover § The loss of appetite in a child with acute malnutrition may indicate a serious pathophysiology § Appetite test: • Part of the initial diagnosis • At every follow-up visit 05 December 2020 57
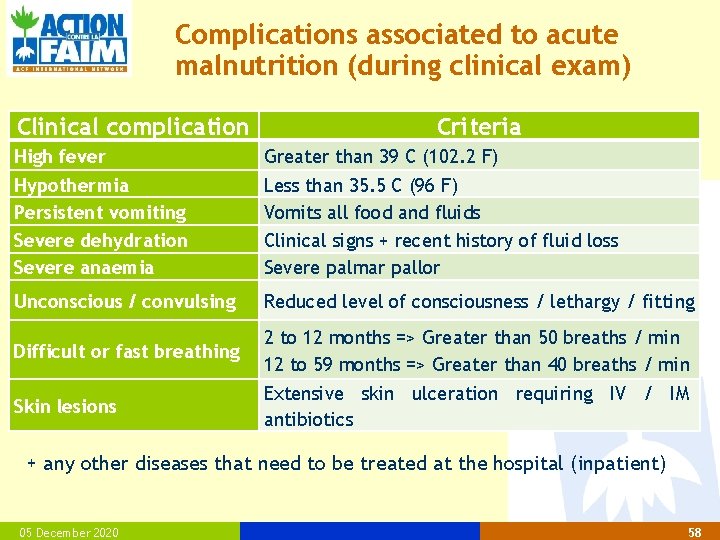
Complications associated to acute malnutrition (during clinical exam) Clinical complication Criteria High fever Greater than 39 C (102. 2 F) Hypothermia Persistent vomiting Severe dehydration Severe anaemia Less than 35. 5 C (96 F) Vomits all food and fluids Clinical signs + recent history of fluid loss Severe palmar pallor Unconscious / convulsing Reduced level of consciousness / lethargy / fitting Difficult or fast breathing 2 to 12 months => Greater than 50 breaths / min 12 to 59 months => Greater than 40 breaths / min Skin lesions Extensive skin ulceration requiring IV / IM antibiotics + any other diseases that need to be treated at the hospital (inpatient) 05 December 2020 58
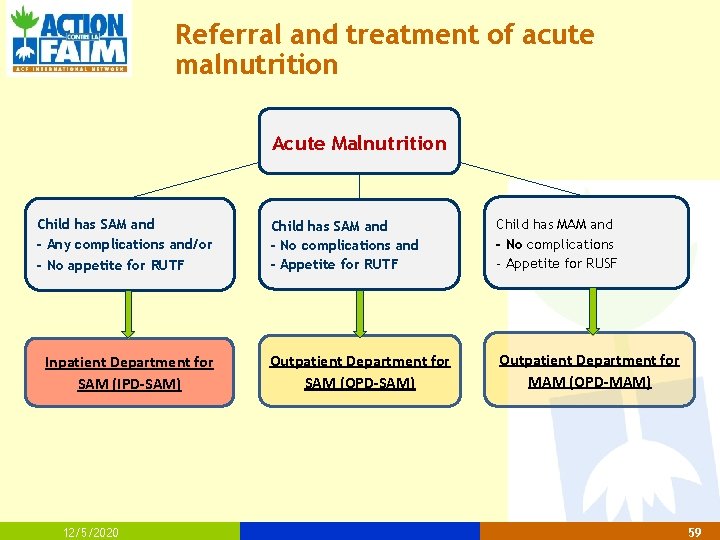
Referral and treatment of acute malnutrition Acute Malnutrition Child has SAM and - Any complications and/or - No appetite for RUTF Inpatient Department for SAM (IPD-SAM) 12/5/2020 Child has SAM and - No complications and - Appetite for RUTF Child has MAM and - No complications - Appetite for RUSF Outpatient Department for SAM (OPD-SAM) Outpatient Department for MAM (OPD-MAM) 59

60
- Slides: 60