MALARIA URINARY TRACT INFECTION AND CHEST INFECTION IN









- Slides: 54
MALARIA, URINARY TRACT INFECTION AND CHEST INFECTION IN PREGNANCY MUSA MARENA
MALARIA IN PREGNANCY
Clinical Significance n n n Commonest parasitic disease in man P falciparum , most virulence and most common in sub-Saharan Africa. P falciparum attacks red cells of all ages, therefore anaemia +++. (c. f others)

Malaria risk. Malaria is Hyper endemic in Ghana – Transmission is throughout the year. n Malaria endemicity can be classified as n n Stable- transmitted throughout the year but may have seasonal variation. Adults less likely to get severe disease due to acquisition of some immunity. n Unstable – intermittent transmission, variable epidemics. Poor immunity against malaria. n Malaria-free – Low transmission of malaria, no immunity among population. Prone to severe disease. n ** Note: Ghana is stable
MALARIA IN PREGNANCY LEARNING OBJECTIVEAt the end of this lecture, students will be able to: n n Identify the group of people at highest risk of malaria infection. List the effects of malaria on pregnant women and their unborn babies. Describe the control strategies for malaria in pregnancy and understand the rationale for IPT(malaria prevention) Learn the case –management of un/complicated malaria
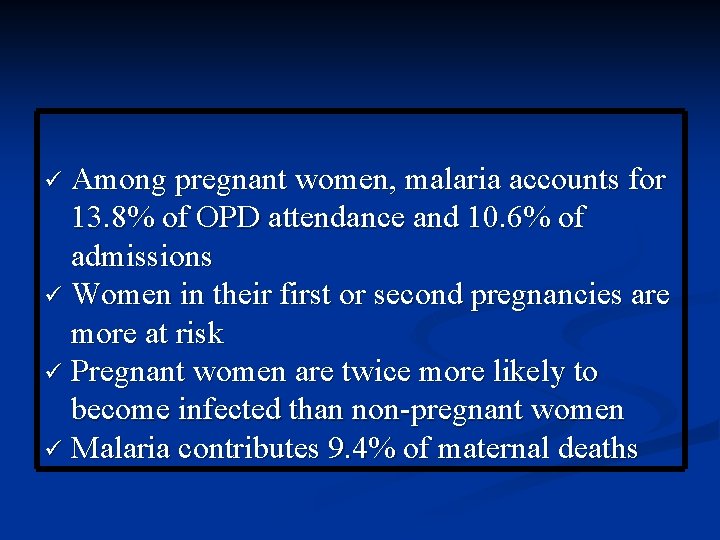
Among pregnant women, malaria accounts for 13. 8% of OPD attendance and 10. 6% of admissions Women in their first or second pregnancies are more at risk Pregnant women are twice more likely to become infected than non-pregnant women Malaria contributes 9. 4% of maternal deaths
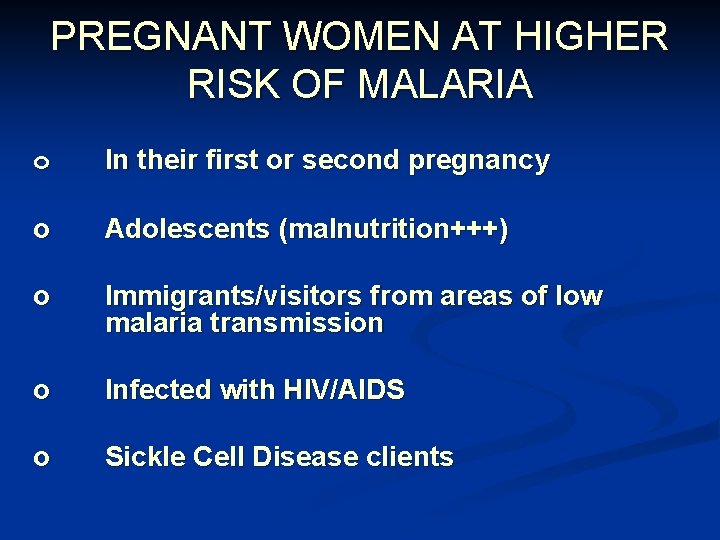
PREGNANT WOMEN AT HIGHER RISK OF MALARIA o In their first or second pregnancy o Adolescents (malnutrition+++) o Immigrants/visitors from areas of low malaria transmission o Infected with HIV/AIDS o Sickle Cell Disease clients

Immunity to Malaria Acquired immunity n Depends on Ø Effectiveness of individual’s immune response Ø Intensity of transmission of malaria in woman’s residential area (stable/unstable) Ø How regularly the woman is personally exposed to the parasite n Adults indigenous to endemic areas → partial immunity through recurrent n
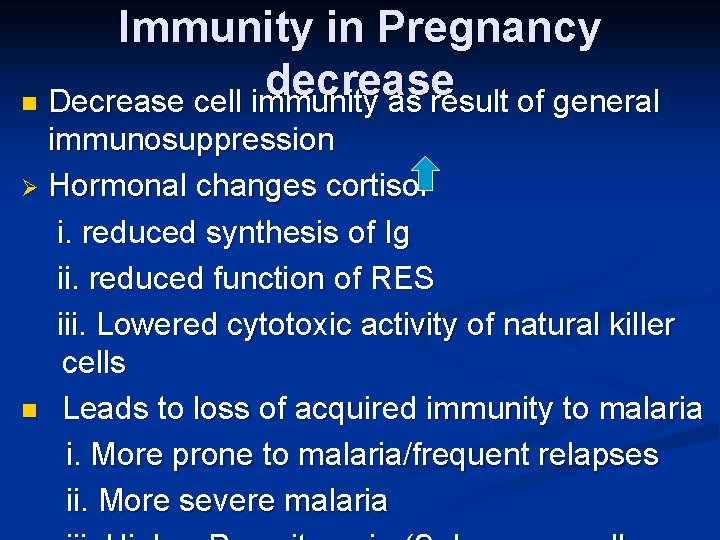
Immunity in Pregnancy decrease n Decrease cell immunity as result of general immunosuppression Ø Hormonal changes cortisol i. reduced synthesis of Ig ii. reduced function of RES iii. Lowered cytotoxic activity of natural killer cells n Leads to loss of acquired immunity to malaria i. More prone to malaria/frequent relapses ii. More severe malaria
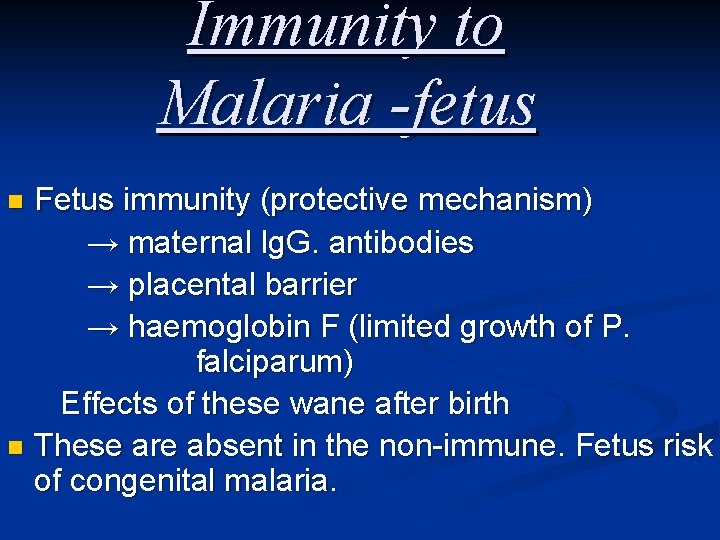
Immunity to Malaria -fetus Fetus immunity (protective mechanism) → maternal lg. G. antibodies → placental barrier → haemoglobin F (limited growth of P. falciparum) Effects of these wane after birth n These are absent in the non-immune. Fetus risk of congenital malaria. n
Effect of Pregnancy on Malaria More frequent and severe malarial attacks n Immunosuppression n Pregnant women found to attract mosquito(A gambiae) > non-pregnant counterparts ( possibly-hormonal, increased release of carbon dioxide and increased body surface temperature) More frequent in primigravida and young because of n n less repeated parasitisation Higher level of cortisol

EFFECT OF MALARIA ON PREGNANT WOMAN 1. 2. 3. 4. Maternal anaemia Puerperal pyrexia Complicated malaria (severe malaria) Spontaneous abortion and its complication/ preterm birth/IUGR/SB 5. Placental infection/Fetal anaemia/rarely congenital malaria
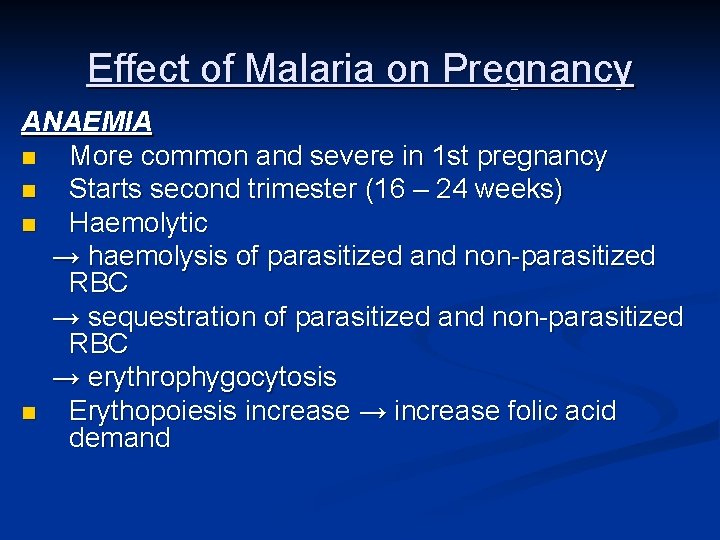
Effect of Malaria on Pregnancy ANAEMIA n More common and severe in 1 st pregnancy n Starts second trimester (16 – 24 weeks) n Haemolytic → haemolysis of parasitized and non-parasitized RBC → sequestration of parasitized and non-parasitized RBC → erythrophygocytosis n Erythopoiesis increase → increase folic acid demand
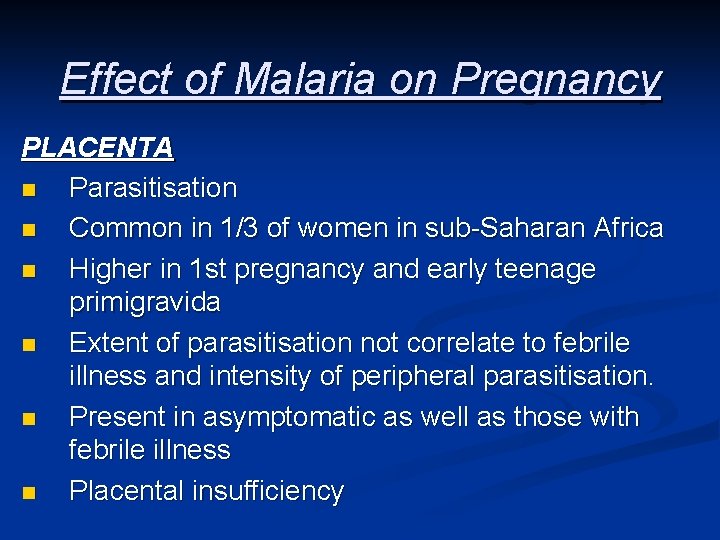
Effect of Malaria on Pregnancy PLACENTA n Parasitisation n Common in 1/3 of women in sub-Saharan Africa n Higher in 1 st pregnancy and early teenage primigravida n Extent of parasitisation not correlate to febrile illness and intensity of peripheral parasitisation. n Present in asymptomatic as well as those with febrile illness n Placental insufficiency

Effect of Malaria on Pregnancy FETUS 1. Intra uterine growth restriction (IUGR) and low birth weight Mediated through n Anaemia n Placental parasitisation - inflammatory reaction - reduces rate of gaseous exchange and nutrient transfer - also placental damage by type -1 cytokines (from immune response) • Surveysthe – birth weight 150 – 200 g lower for babies born to mothers with placental malaria. n
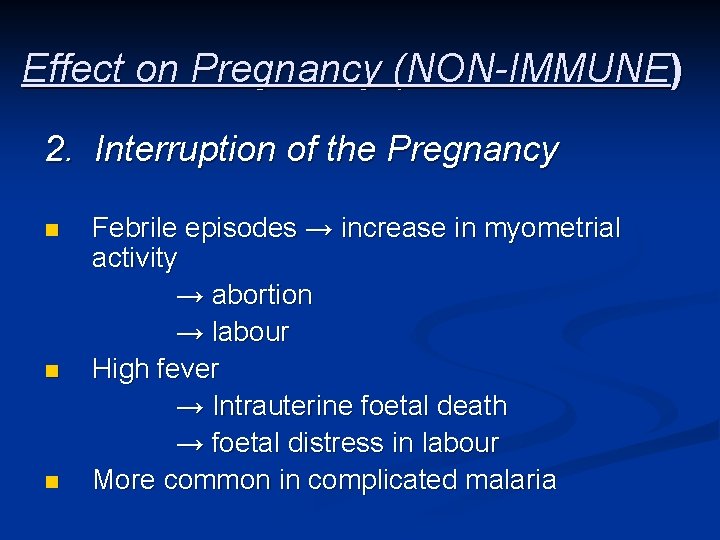
Effect on Pregnancy (NON-IMMUNE) 2. Interruption of the Pregnancy n n n Febrile episodes → increase in myometrial activity → abortion → labour High fever → Intrauterine foetal death → foetal distress in labour More common in complicated malaria
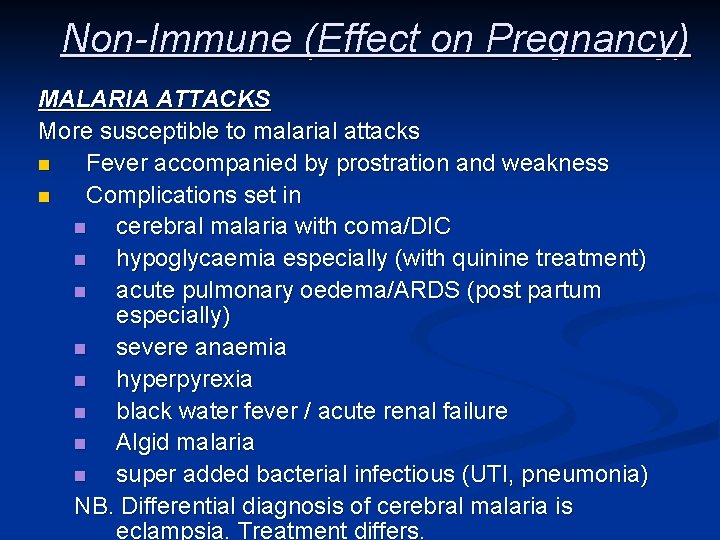
Non-Immune (Effect on Pregnancy) MALARIA ATTACKS More susceptible to malarial attacks n Fever accompanied by prostration and weakness n Complications set in n cerebral malaria with coma/DIC n hypoglycaemia especially (with quinine treatment) n acute pulmonary oedema/ARDS (post partum especially) n severe anaemia n hyperpyrexia n black water fever / acute renal failure n Algid malaria n super added bacterial infectious (UTI, pneumonia) NB. Differential diagnosis of cerebral malaria is eclampsia. Treatment differs.
STRATEGY FOR CONTROLLING MALARIA(W H O) 1. Use of insecticide-treated nets (ITNs), Repellant and aero spray 2. Use of Intermittent Preventive Treatment (IPT) 3. Public education/ Environmental hygiene 4. Case Management of malaria illness
WHAT IS IPT? n Intermittent preventive treatment (IPT) is based on the use of anti-malarial drugs given in treatment doses at predefined intervals after quickening to clear a presumed burden of malaria parasites.
WHY IPT? n Intermittent preventive treatment (IPT) of malaria during pregnancy is based on the assumption that every pregnant woman living in areas of high malaria transmission has malaria parasites in her blood or placenta, whether or not she has symptoms of malaria.

IPT is important because many pregnant women can have malaria parasites without symptoms. TARGET GROUP IPT is given to all asymptomatic pregnant women who report at the antenatal clinic in the second or third trimester but more especially: n n n Those of low gravidity (i. e. primigravida and secundigravida) Those infected with HIV Adolescents and youth (10 - 24 years) Sickle Cell Disease patients Those with unexplained anaemia
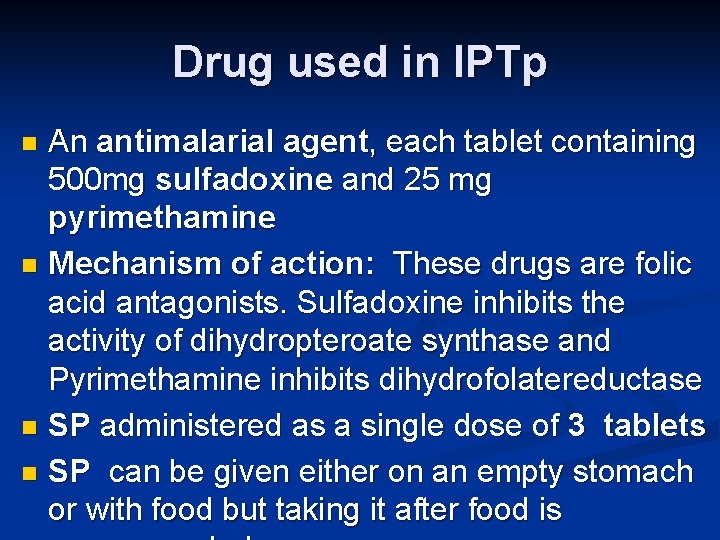
Drug used in IPTp An antimalarial agent, each tablet containing 500 mg sulfadoxine and 25 mg pyrimethamine n Mechanism of action: These drugs are folic acid antagonists. Sulfadoxine inhibits the activity of dihydropteroate synthase and Pyrimethamine inhibits dihydrofolatereductase n SP administered as a single dose of 3 tablets n SP can be given either on an empty stomach or with food but taking it after food is n
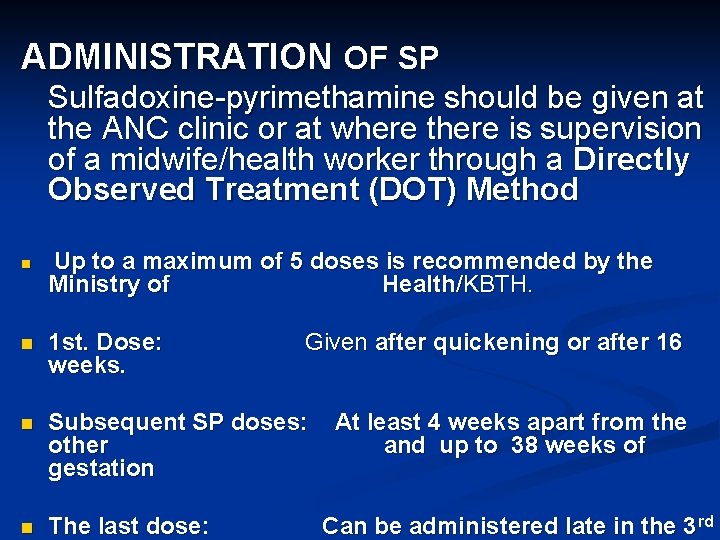
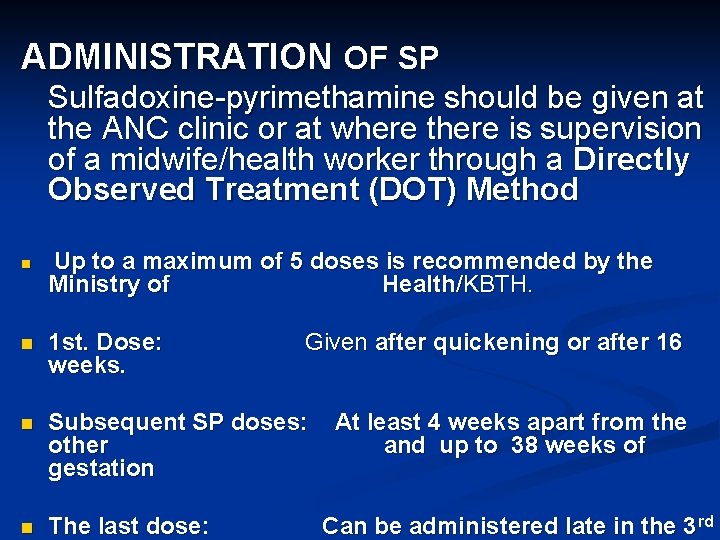
ADMINISTRATION OF SP Sulfadoxine-pyrimethamine should be given at the ANC clinic or at where there is supervision of a midwife/health worker through a Directly Observed Treatment (DOT) Method n Up to a maximum of 5 doses is recommended by the Ministry of Health /KBTH. n 1 st. Dose: weeks. Given after quickening or after 16 n Subsequent SP doses: other gestation n The last dose: At least 4 weeks apart from the and up to 38 weeks of Can be administered late in the 3 rd
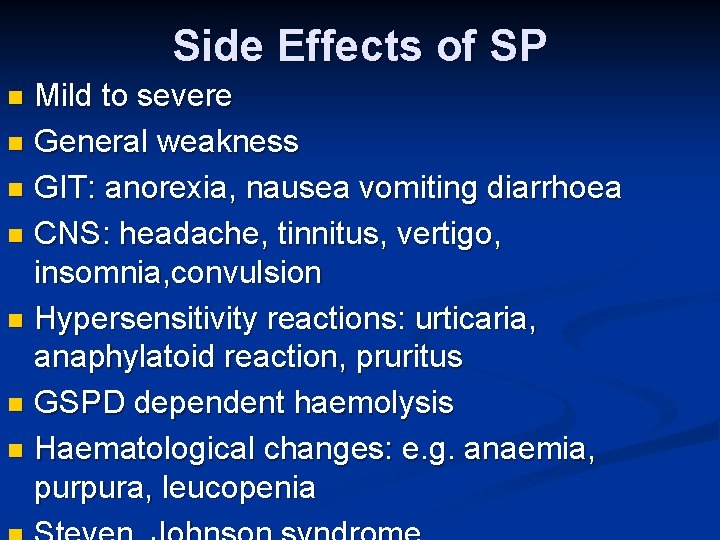
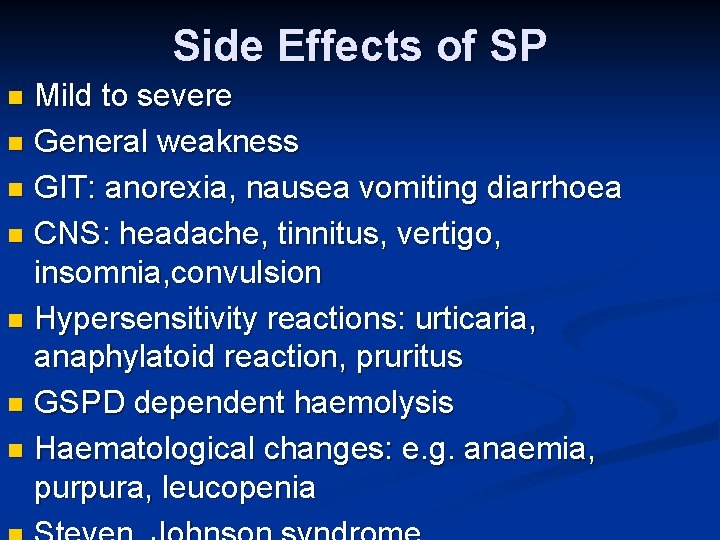
Side Effects of SP Mild to severe n General weakness n GIT: anorexia, nausea vomiting diarrhoea n CNS: headache, tinnitus, vertigo, insomnia, convulsion n Hypersensitivity reactions: urticaria, anaphylatoid reaction, pruritus n GSPD dependent haemolysis n Haematological changes: e. g. anaemia, purpura, leucopenia n
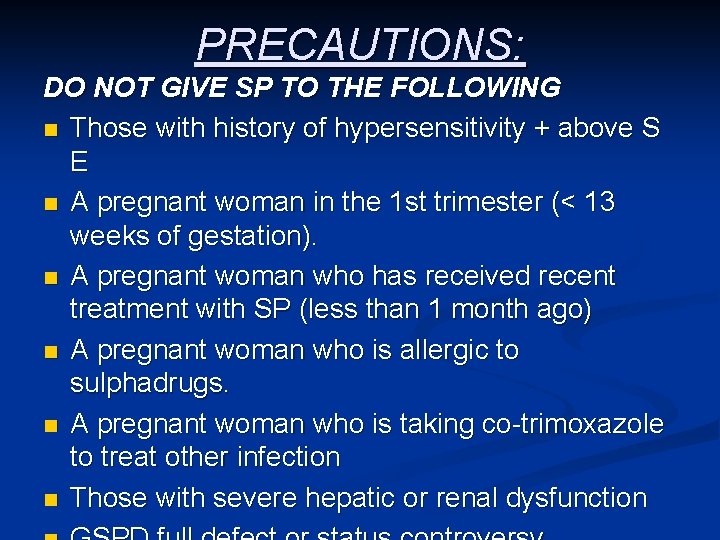
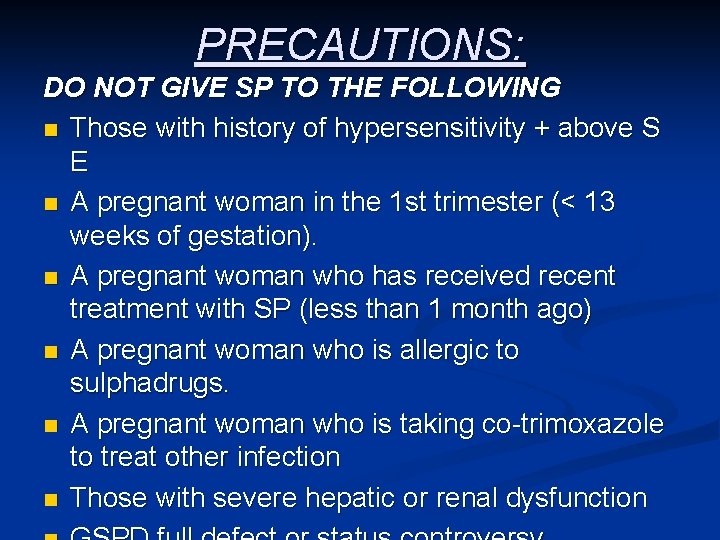
PRECAUTIONS: DO NOT GIVE SP TO THE FOLLOWING n Those with history of hypersensitivity + above S E n A pregnant woman in the 1 st trimester (< 13 weeks of gestation). n A pregnant woman who has received recent treatment with SP (less than 1 month ago) n A pregnant woman who is allergic to sulphadrugs. n A pregnant woman who is taking co-trimoxazole to treat other infection n Those with severe hepatic or renal dysfunction
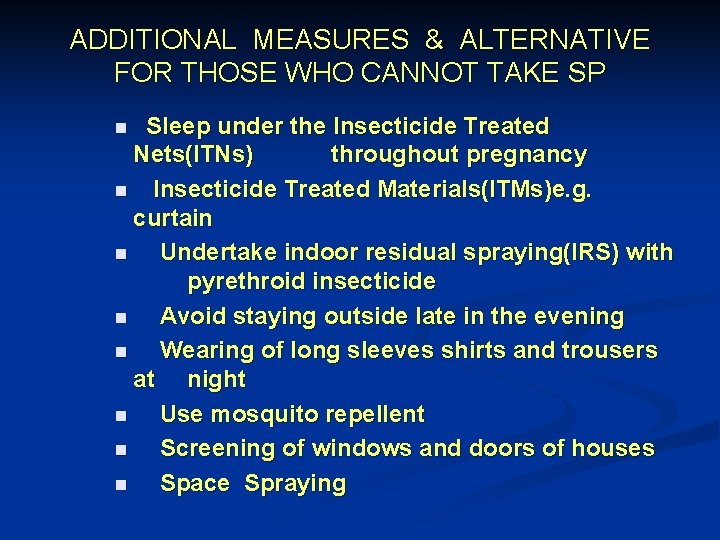
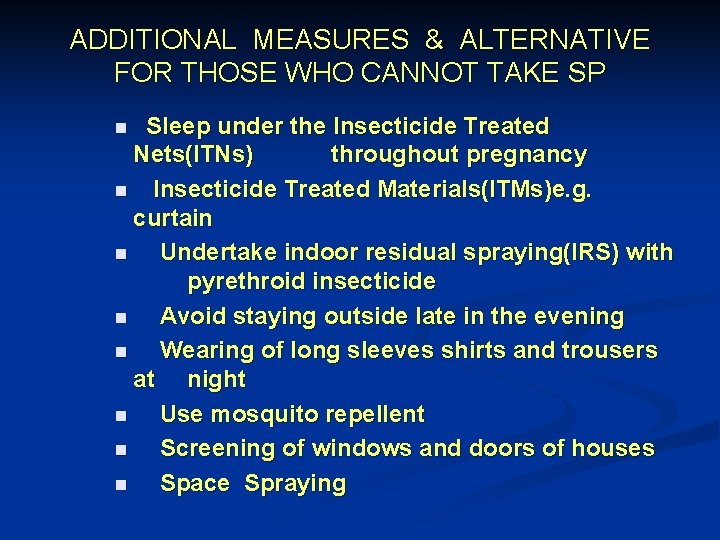
ADDITIONAL MEASURES & ALTERNATIVE FOR THOSE WHO CANNOT TAKE SP Sleep under the Insecticide Treated Nets(ITNs) throughout pregnancy n Insecticide Treated Materials(ITMs)e. g. curtain n Undertake indoor residual spraying(IRS) with pyrethroid insecticide n Avoid staying outside late in the evening n Wearing of long sleeves shirts and trousers at night n Use mosquito repellent n Screening of windows and doors of houses n Space Spraying n
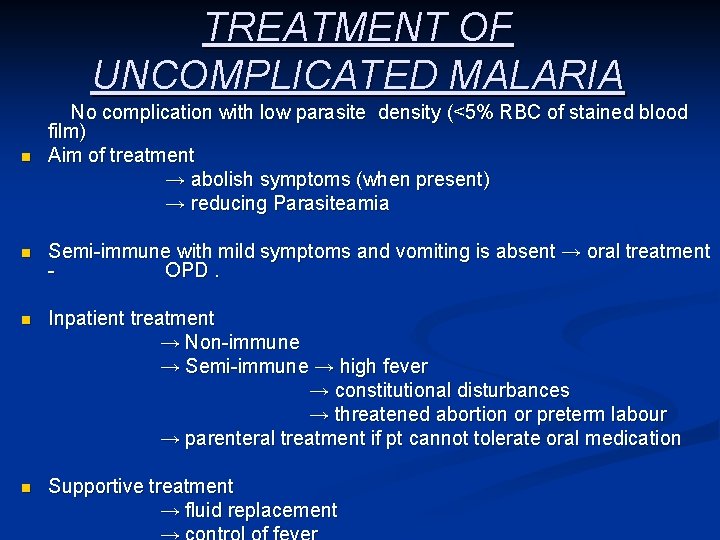
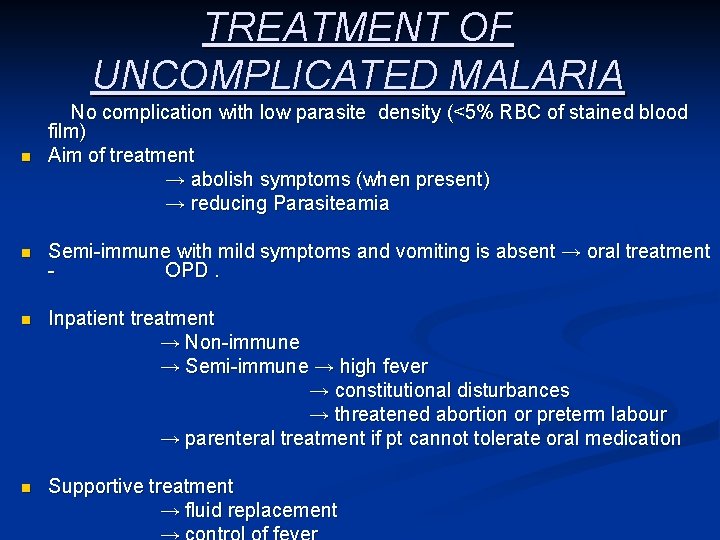
TREATMENT OF UNCOMPLICATED MALARIA n No complication with low parasite density (<5% RBC of stained blood film) Aim of treatment → abolish symptoms (when present) → reducing Parasiteamia n Semi-immune with mild symptoms and vomiting is absent → oral treatment OPD. n Inpatient treatment → Non-immune → Semi-immune → high fever → constitutional disturbances → threatened abortion or preterm labour → parenteral treatment if pt cannot tolerate oral medication n Supportive treatment → fluid replacement
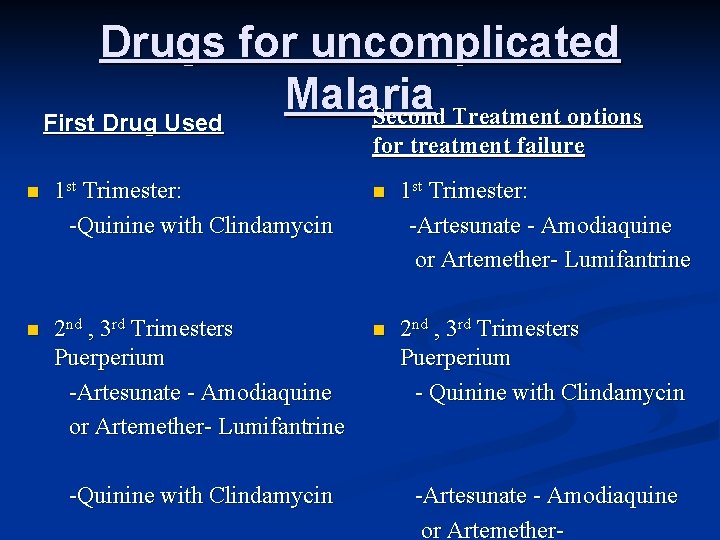
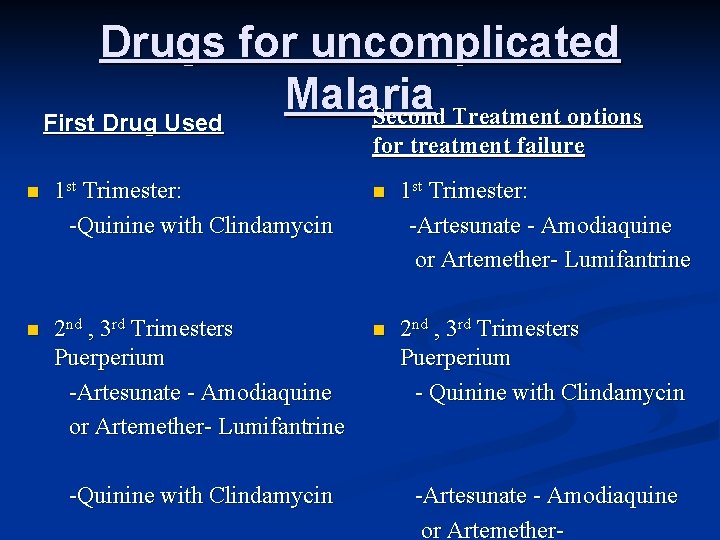
Drugs for uncomplicated Malaria Second Treatment options First Drug Used for treatment failure n 1 st Trimester: -Quinine with Clindamycin n 1 st Trimester: -Artesunate - Amodiaquine or Artemether- Lumifantrine n 2 nd , 3 rd Trimesters Puerperium - Quinine with Clindamycin -Artesunate - Amodiaquine or Artemether-
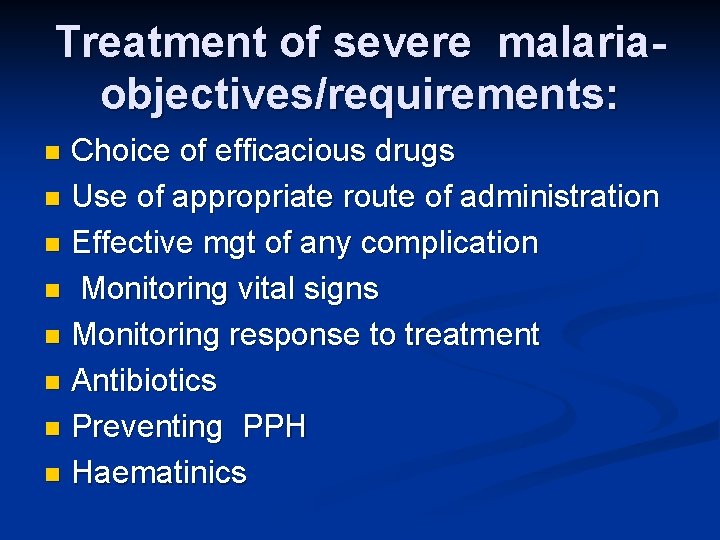
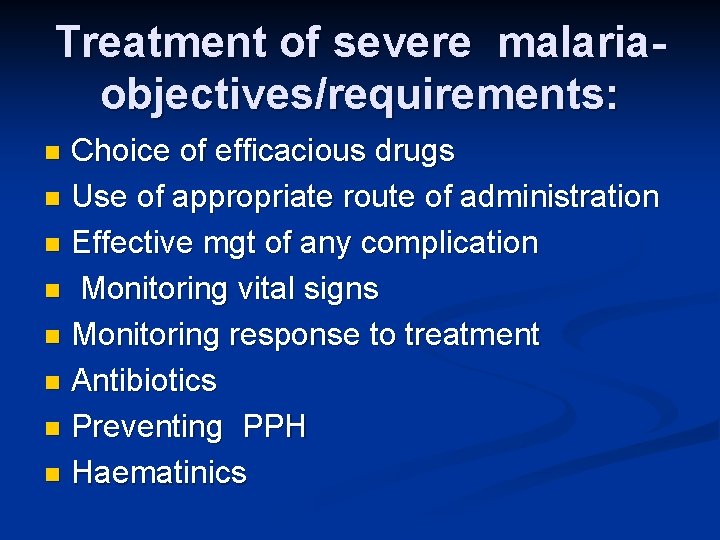
Treatment of severe malariaobjectives/requirements: Choice of efficacious drugs n Use of appropriate route of administration n Effective mgt of any complication n Monitoring vital signs n Monitoring response to treatment n Antibiotics n Preventing PPH n Haematinics n
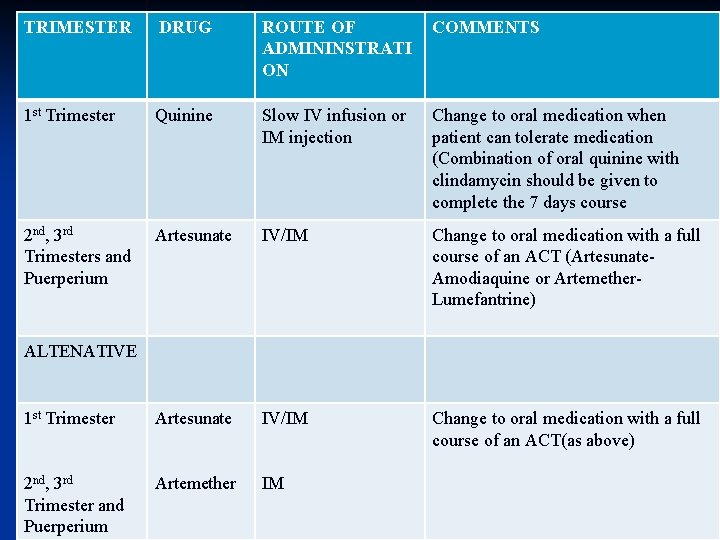
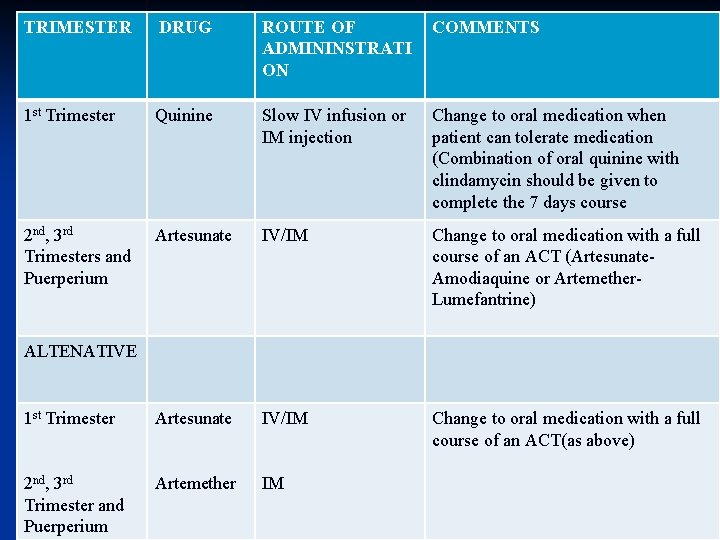
TRIMESTER DRUG ROUTE OF ADMININSTRATI ON COMMENTS 1 st Trimester Quinine Slow IV infusion or IM injection Change to oral medication when patient can tolerate medication (Combination of oral quinine with clindamycin should be given to complete the 7 days course 2 nd, 3 rd Trimesters and Puerperium Artesunate IV/IM Change to oral medication with a full course of an ACT (Artesunate. Amodiaquine or Artemether. Lumefantrine) 1 st Trimester Artesunate IV/IM Change to oral medication with a full course of an ACT(as above) 2 nd, 3 rd Trimester and Puerperium Artemether IM ALTENATIVE
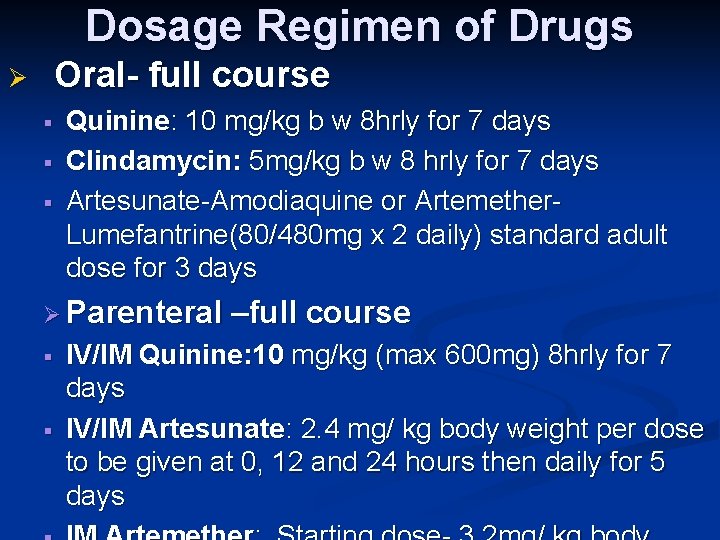
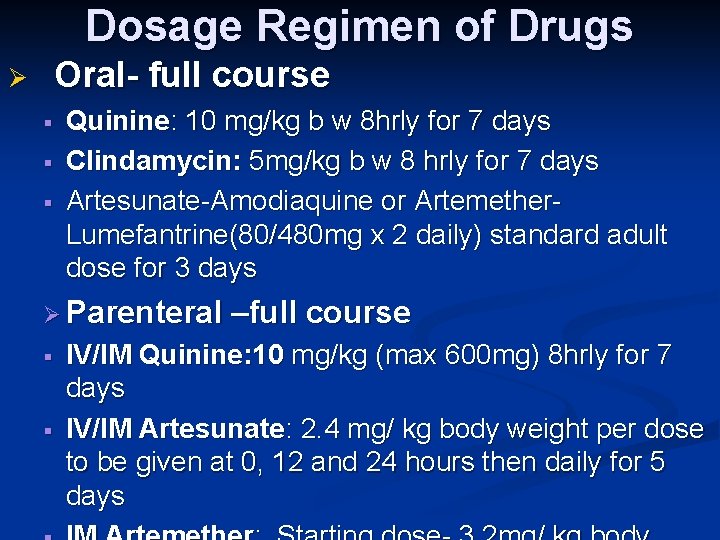
Dosage Regimen of Drugs Oral- full course Ø § § § Quinine: 10 mg/kg b w 8 hrly for 7 days Clindamycin: 5 mg/kg b w 8 hrly for 7 days Artesunate-Amodiaquine or Artemether. Lumefantrine(80/480 mg x 2 daily) standard adult dose for 3 days Ø Parenteral § § –full course IV/IM Quinine: 10 mg/kg (max 600 mg) 8 hrly for 7 days IV/IM Artesunate: 2. 4 mg/ kg body weight per dose to be given at 0, 12 and 24 hours then daily for 5 days
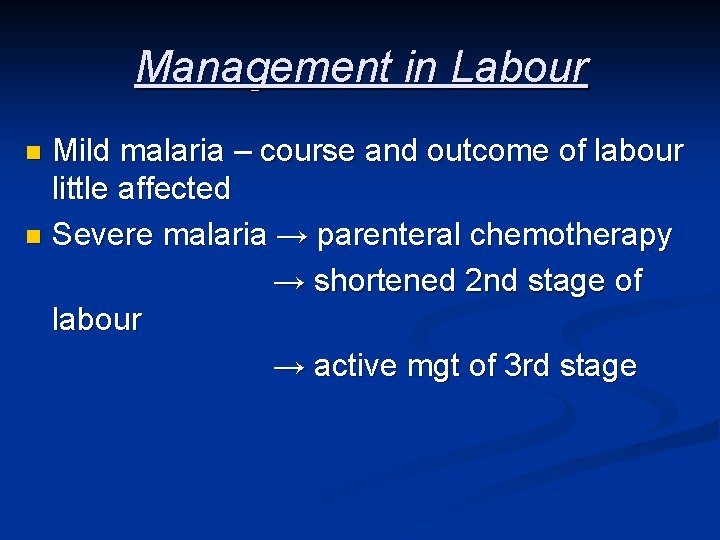
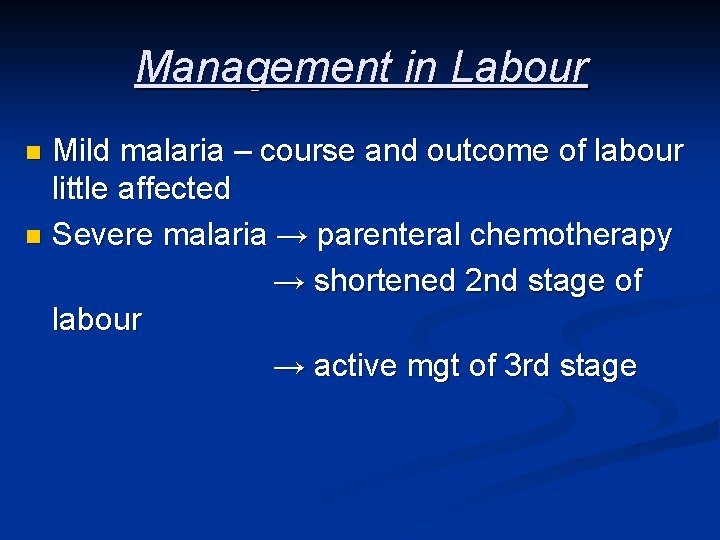
Management in Labour Mild malaria – course and outcome of labour little affected n Severe malaria → parenteral chemotherapy → shortened 2 nd stage of labour → active mgt of 3 rd stage n

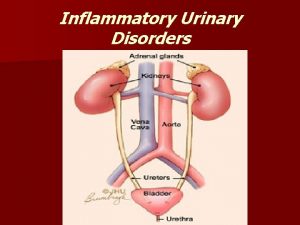
URINARY TRACT INFECTION
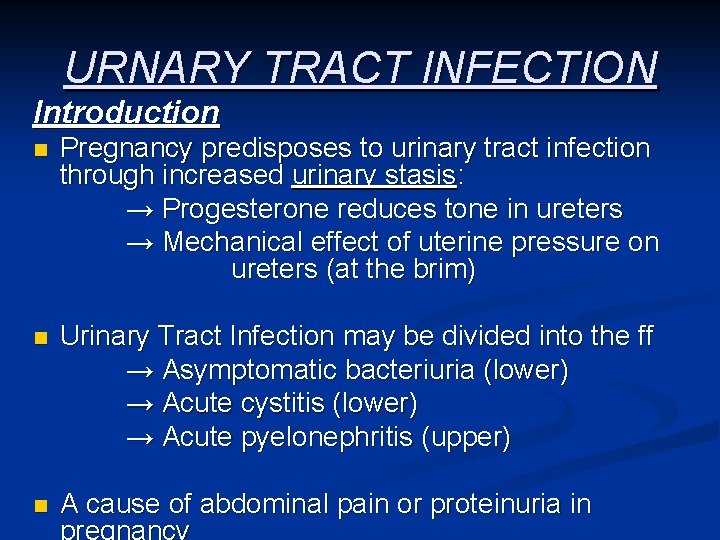
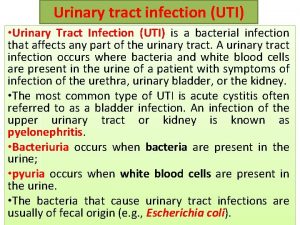
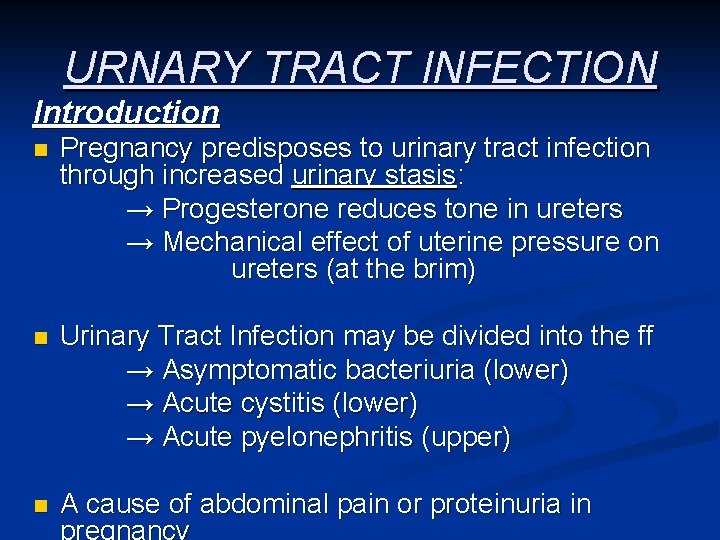
URNARY TRACT INFECTION Introduction n Pregnancy predisposes to urinary tract infection through increased urinary stasis: → Progesterone reduces tone in ureters → Mechanical effect of uterine pressure on ureters (at the brim) n Urinary Tract Infection may be divided into the ff → Asymptomatic bacteriuria (lower) → Acute cystitis (lower) → Acute pyelonephritis (upper) n A cause of abdominal pain or proteinuria in
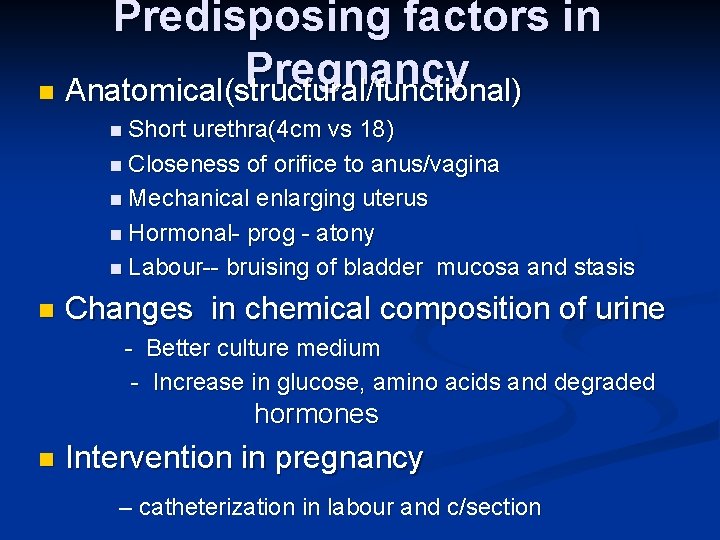
Predisposing factors in Pregnancy n Anatomical(structural/functional) n Short urethra(4 cm vs 18) n Closeness of orifice to anus/vagina n Mechanical enlarging uterus n Hormonal- prog - atony n Labour-- bruising of bladder mucosa and stasis n Changes in chemical composition of urine - Better culture medium - Increase in glucose, amino acids and degraded hormones n Intervention in pregnancy – catheterization in labour and c/section
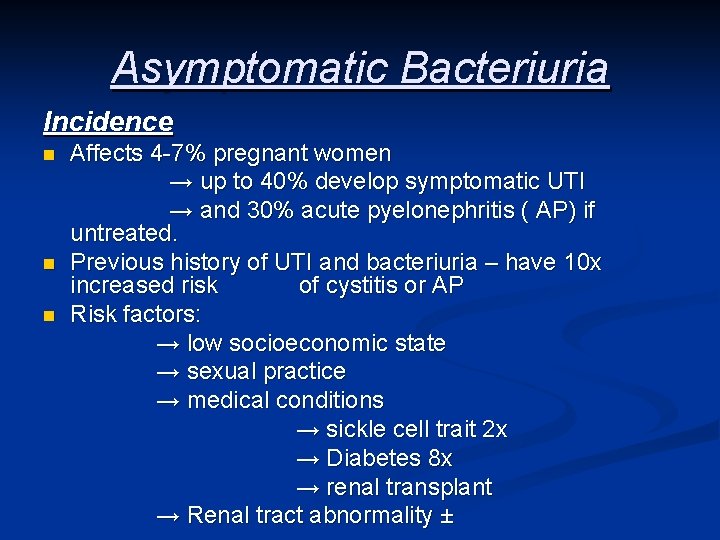
Asymptomatic Bacteriuria Incidence n n n Affects 4 -7% pregnant women → up to 40% develop symptomatic UTI → and 30% acute pyelonephritis ( AP) if untreated. Previous history of UTI and bacteriuria – have 10 x increased risk of cystitis or AP Risk factors: → low socioeconomic state → sexual practice → medical conditions → sickle cell trait 2 x → Diabetes 8 x → renal transplant → Renal tract abnormality ±
Asymptomatic Bacteriuria Definition n Presence of actively multiplying bacteria in the urinary tract excluding the distal urethra in a patient without obvious symptoms.
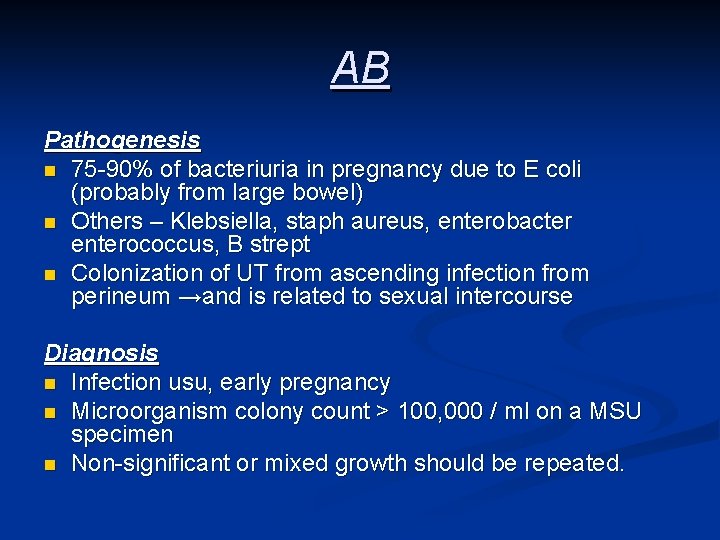
AB Pathogenesis n 75 -90% of bacteriuria in pregnancy due to E coli (probably from large bowel) n Others – Klebsiella, staph aureus, enterobacter enterococcus, B strept n Colonization of UT from ascending infection from perineum →and is related to sexual intercourse Diagnosis n Infection usu, early pregnancy n Microorganism colony count > 100, 000 / ml on a MSU specimen n Non-significant or mixed growth should be repeated.
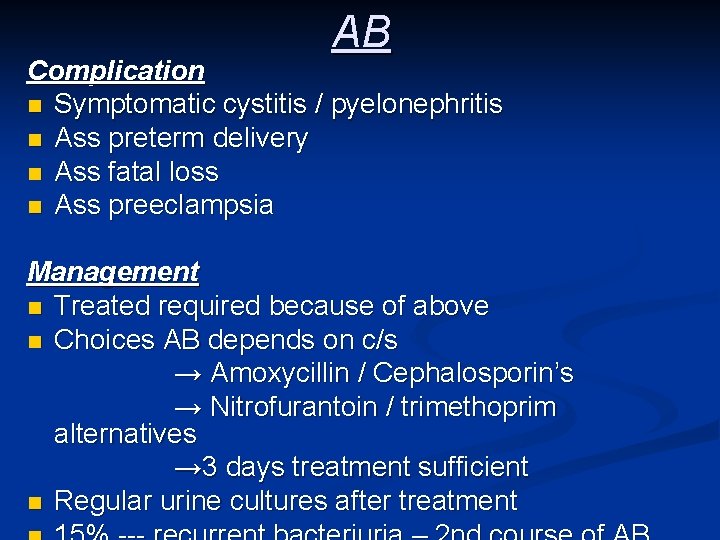
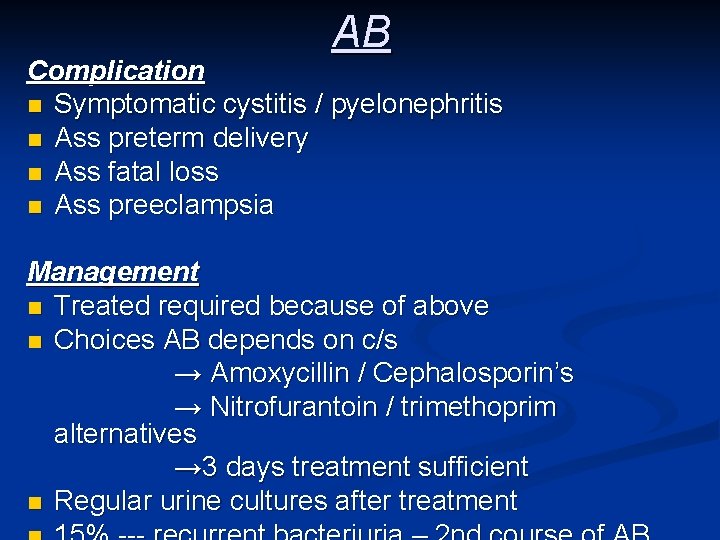
AB Complication n Symptomatic cystitis / pyelonephritis n Ass preterm delivery n Ass fatal loss n Ass preeclampsia Management n Treated required because of above n Choices AB depends on c/s → Amoxycillin / Cephalosporin’s → Nitrofurantoin / trimethoprim alternatives → 3 days treatment sufficient n Regular urine cultures after treatment
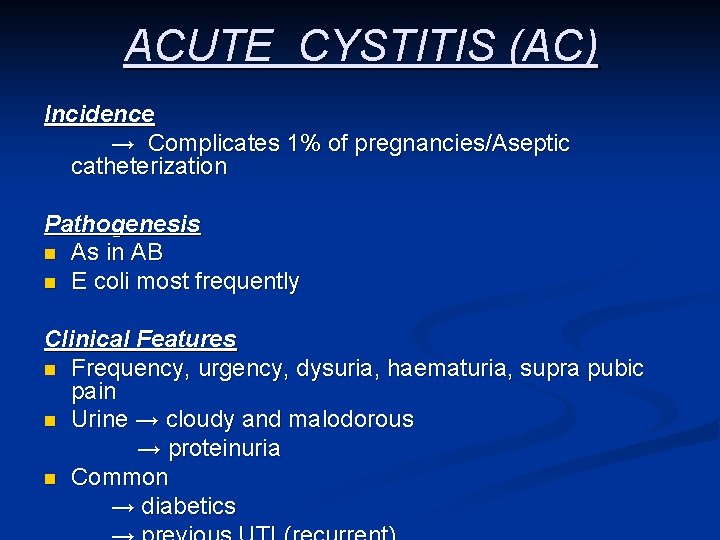
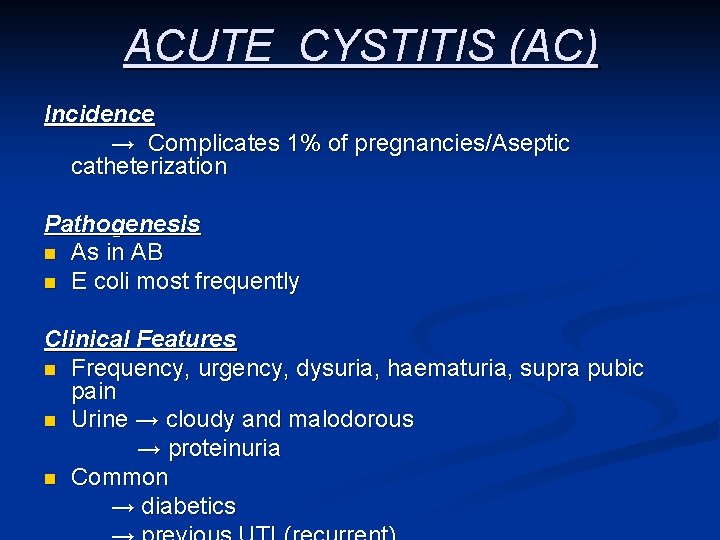
ACUTE CYSTITIS (AC) Incidence → Complicates 1% of pregnancies/Aseptic catheterization Pathogenesis n As in AB n E coli most frequently Clinical Features n Frequency, urgency, dysuria, haematuria, supra pubic pain n Urine → cloudy and malodorous → proteinuria n Common → diabetics
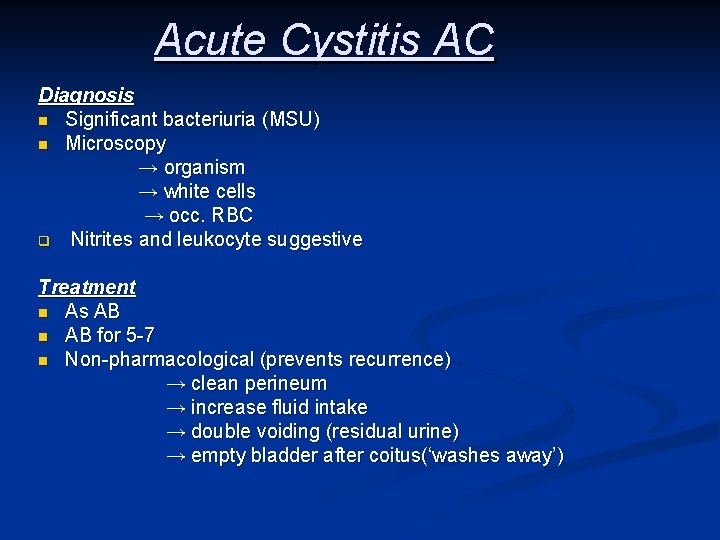
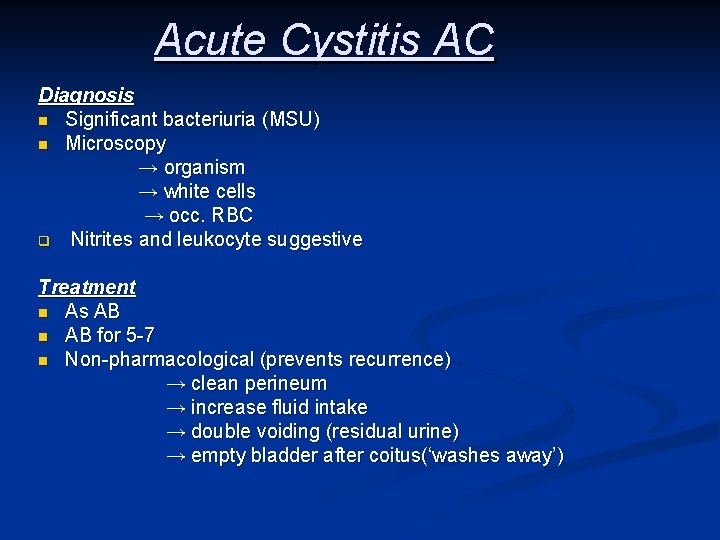
Acute Cystitis AC Diagnosis n Significant bacteriuria (MSU) n Microscopy → organism → white cells → occ. RBC q Nitrites and leukocyte suggestive Treatment n As AB n AB for 5 -7 n Non-pharmacological (prevents recurrence) → clean perineum → increase fluid intake → double voiding (residual urine) → empty bladder after coitus(‘washes away’)
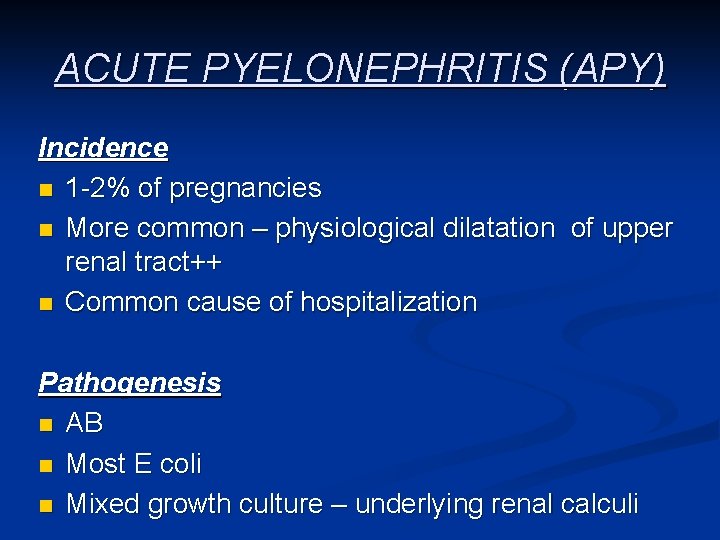
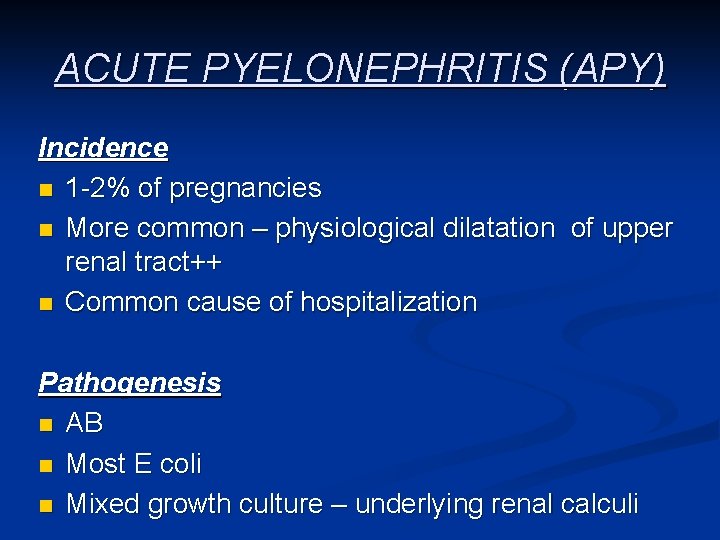
ACUTE PYELONEPHRITIS (APY) Incidence n 1 -2% of pregnancies n More common – physiological dilatation of upper renal tract++ n Common cause of hospitalization Pathogenesis n AB n Most E coli n Mixed growth culture – underlying renal calculi
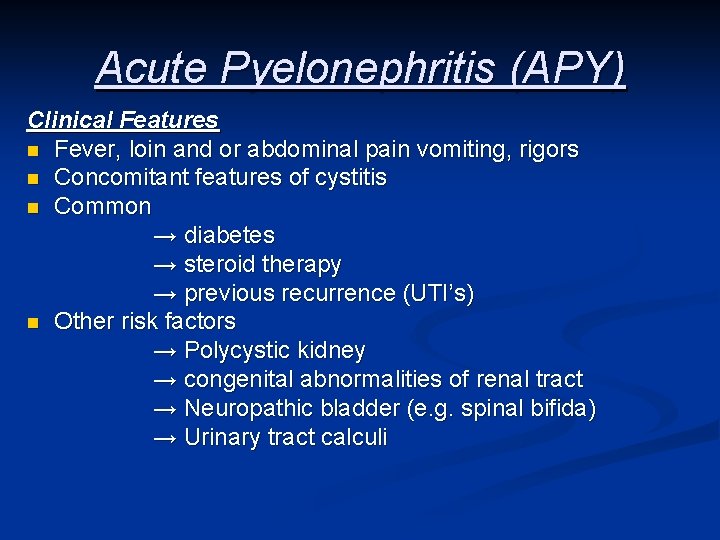
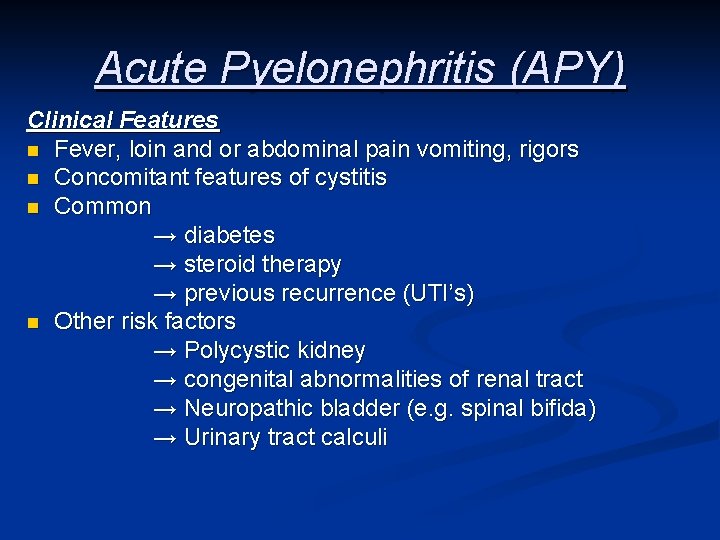
Acute Pyelonephritis (APY) Clinical Features n Fever, loin and or abdominal pain vomiting, rigors n Concomitant features of cystitis n Common → diabetes → steroid therapy → previous recurrence (UTI’s) n Other risk factors → Polycystic kidney → congenital abnormalities of renal tract → Neuropathic bladder (e. g. spinal bifida) → Urinary tract calculi
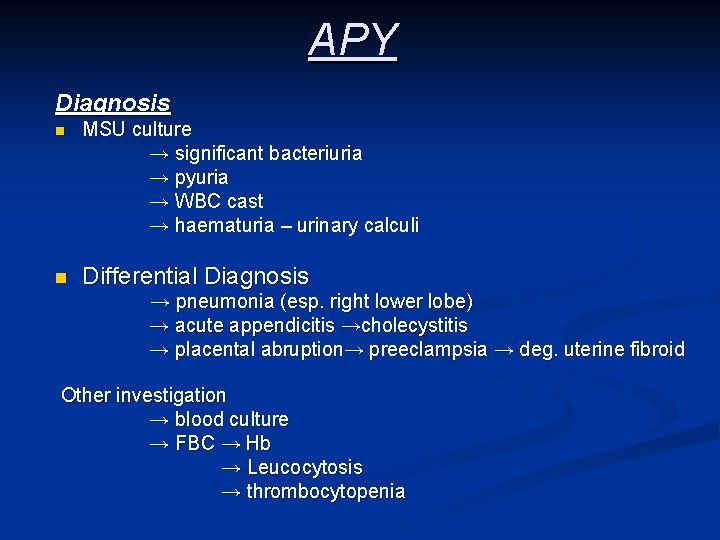
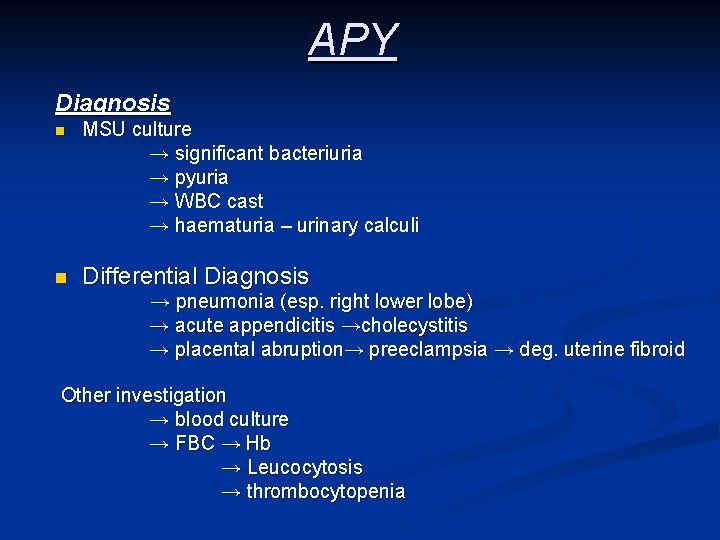
APY Diagnosis n MSU culture → significant bacteriuria → pyuria → WBC cast → haematuria – urinary calculi n Differential Diagnosis → pneumonia (esp. right lower lobe) → acute appendicitis →cholecystitis → placental abruption→ preeclampsia → deg. uterine fibroid Other investigation → blood culture → FBC → Hb → Leucocytosis → thrombocytopenia

APY Complication Effect on Pregnancy n Risk of premature labour (pyrexia), PROM n Foetal tachycardia n Low birth weight / prematurity n Hypertension n Anaemia → marrow suppression → erythrocyte destruction → decreases rbc production Others n Bacterial endotoxemia n Endotoxic shock n Renal insufficiency –oliguria and failure n Pulmonary dysfunction (cough → ARDS) n CNS-confusion/hypothalmic dysfunction
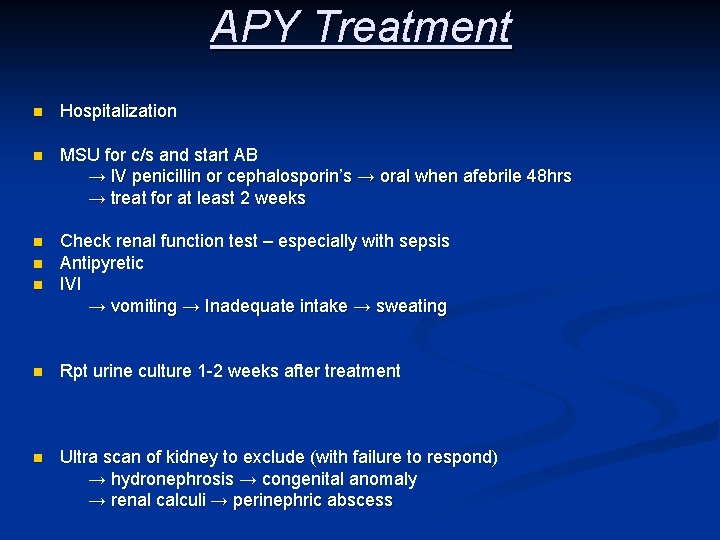
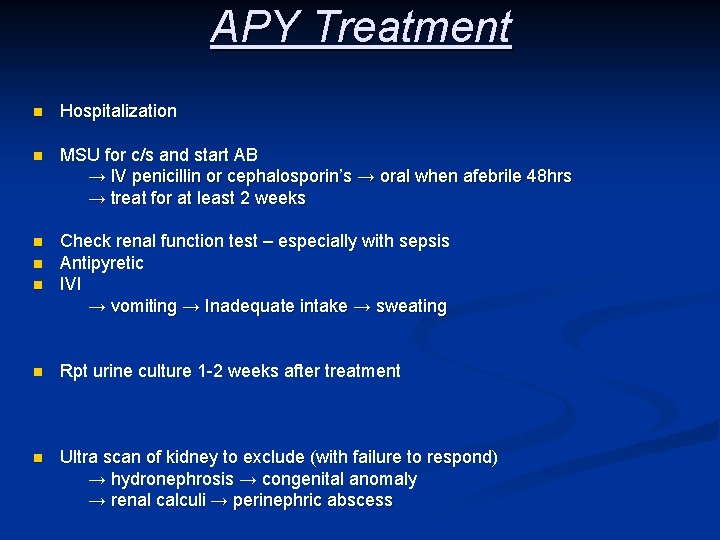
APY Treatment n Hospitalization n MSU for c/s and start AB → IV penicillin or cephalosporin’s → oral when afebrile 48 hrs → treat for at least 2 weeks n Check renal function test – especially with sepsis Antipyretic IVI → vomiting → Inadequate intake → sweating n n n Rpt urine culture 1 -2 weeks after treatment n Ultra scan of kidney to exclude (with failure to respond) → hydronephrosis → congenital anomaly → renal calculi → perinephric abscess
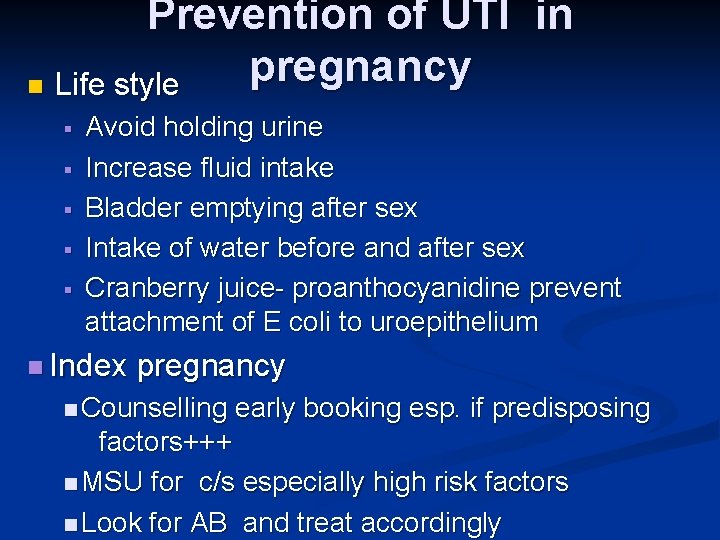
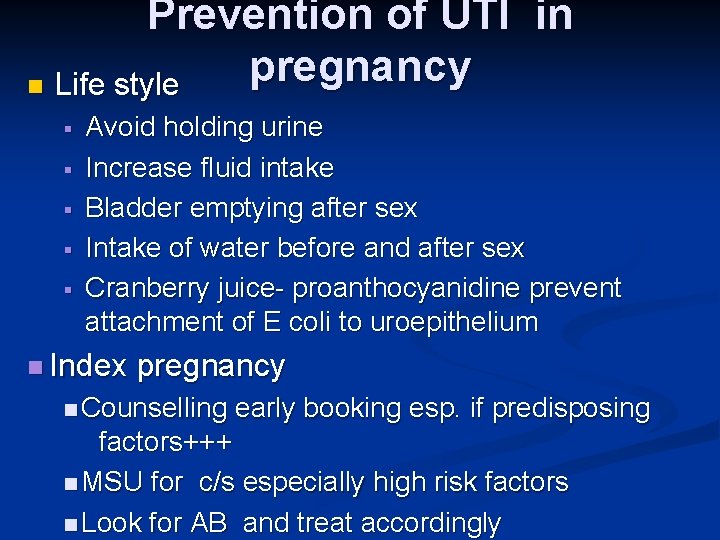
Prevention of UTI in pregnancy n Life style § § § Avoid holding urine Increase fluid intake Bladder emptying after sex Intake of water before and after sex Cranberry juice- proanthocyanidine prevent attachment of E coli to uroepithelium n Index pregnancy n Counselling early booking esp. if predisposing factors+++ n MSU for c/s especially high risk factors n Look for AB and treat accordingly

CHEST INFECTION
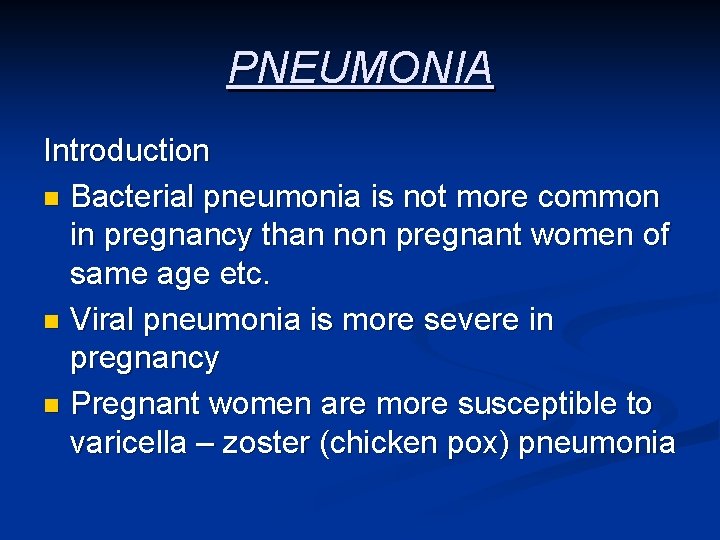
PNEUMONIA Introduction n Bacterial pneumonia is not more common in pregnancy than non pregnant women of same age etc. n Viral pneumonia is more severe in pregnancy n Pregnant women are more susceptible to varicella – zoster (chicken pox) pneumonia
PNEUMONIA Pathogenesis n Bacterial → Strept pneumoniae ( > 50% of cases) → Haemophilus influenza (community acquired chronic bronchitis) → Staphylococcus (ass. with influenza → Legionella (institutional) n Viral → Influenza A → Varicella – zoster n Others → Mycoplasma pneumoniae (community acquired) → Pneumocystis carinii (ass. with HIV)
PNEUMONIA Clinical Features Symptoms n Cough (often dry at first) n Fever n Rigors n Breathlessness n Pleuritic pain Signs n Fever n Purulent sputum n Coarse crackles n Signs of consolidation
PNEUMONIA Management Principles n Adequate oxygenation - oximeter n Adequate hydration – fever n Physiotherapy – secretions n Antibiotics – IV or oral, depending on severity → PCN or cephalosporin → Azithromycin → Duration 7 days Adverse Clinical Features n Respiration rate ≥ 30 pm n Hypoxaemia oxygen sat < 92% n Hypotension – systolic BP < 90 mm Hg n Bilateral or multilobe involvement in Cx. R
PNEUMONIA Effect of Pregnancy on Pneumonia n No effect Effect of Pneumonia on Pregnant n Preterm labour n Perinatal mortalities < 10% if delivered during the acute state Complication n Poor outcome if > 2 lobes etc n Hypoalbuminenia, septicaemia n Progress to ARDS – 70% mortality n Bacteremia → 25% of patients n Empyema and respiratory failure

THANK YOU Happy New Year
 Urinary tract infection
Urinary tract infection Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Nursing management for urinary tract infection
Nursing management for urinary tract infection Uti symptoms
Uti symptoms Urinary tract obstruction
Urinary tract obstruction Urinary bladder
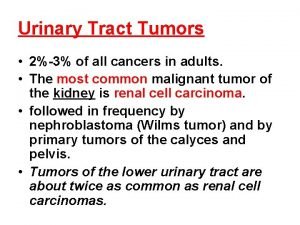
Urinary bladder Tumor in the urinary tract
Tumor in the urinary tract Pyramidal vs extrapyramidal lesions
Pyramidal vs extrapyramidal lesions Dorsal reticulospinal tract
Dorsal reticulospinal tract Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Lrti
Lrti Sexually transmitted diseases
Sexually transmitted diseases Thick and thin malaria smear
Thick and thin malaria smear Facultad de ciencias de la salud uma
Facultad de ciencias de la salud uma Malaria and dengue
Malaria and dengue Malaria and dengue
Malaria and dengue Enlargement of a lymphoid organ in the luq
Enlargement of a lymphoid organ in the luq Cause of splenomegaly in malaria
Cause of splenomegaly in malaria Dot
Dot Etiology of malaria
Etiology of malaria Obat malaria dhp
Obat malaria dhp Maurer dots
Maurer dots Malaria prophylaxis
Malaria prophylaxis Apicomplex
Apicomplex Piremetamina
Piremetamina Applique forms malaria
Applique forms malaria Imep full form in malaria
Imep full form in malaria Malaria in uganda facts
Malaria in uganda facts Icd 10 malaria falciparum
Icd 10 malaria falciparum Complicated malaria
Complicated malaria Malaria in pregnancy definition
Malaria in pregnancy definition Malaria in pregnancy definition
Malaria in pregnancy definition Emerging infectious diseases
Emerging infectious diseases Makalah surveilans malaria
Makalah surveilans malaria Tuberculosis cutanea
Tuberculosis cutanea Plasmodium vivax forma infectante
Plasmodium vivax forma infectante Malaria references
Malaria references Malaria life cycle
Malaria life cycle Plasmodium sp doença
Plasmodium sp doença History of malaria
History of malaria Falciparum
Falciparum Malaria sequestration
Malaria sequestration Malaria sequestration
Malaria sequestration Black water malaria
Black water malaria Sporontocides
Sporontocides Malaria
Malaria Plazmodium malaria
Plazmodium malaria Causative agent malaria
Causative agent malaria Burdenworld
Burdenworld Ookinite
Ookinite Icd 10 malaria tropika
Icd 10 malaria tropika Algid malaria
Algid malaria Malaria costa rica
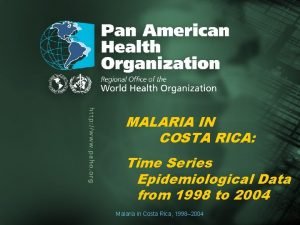
Malaria costa rica Malaria life cycle
Malaria life cycle