Malaria national guidelines VARIABLE RESISTANCE PATTERN ACROSS WORLD
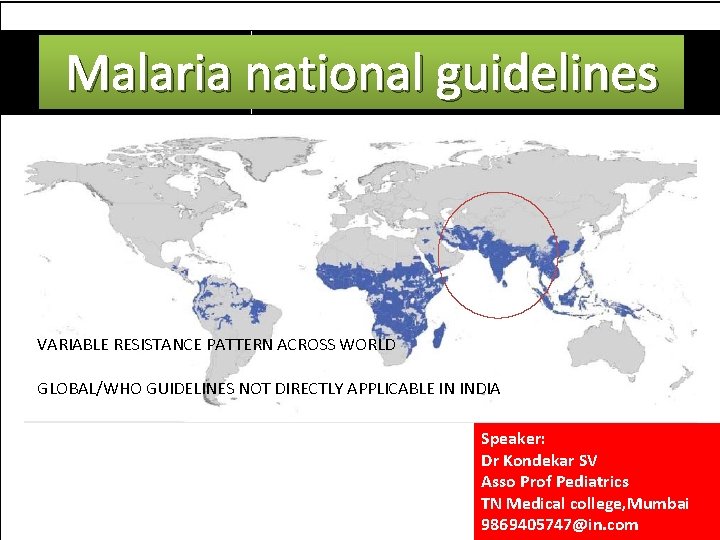
Malaria national guidelines VARIABLE RESISTANCE PATTERN ACROSS WORLD GLOBAL/WHO GUIDELINES NOT DIRECTLY APPLICABLE IN INDIA Speaker: Dr Kondekar SV Asso Prof Pediatrics TN Medical college, Mumbai 9869405747@in. com
FIRST IN 2009, UPDATED 2010 WHO FUNDED REVISED NATIONAL POLICY BY MINISTRY OF HEALTH AND FAMILY WELFARE BRAIN STORMING MEETINGS NATION WIDE EXPERTS NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 2
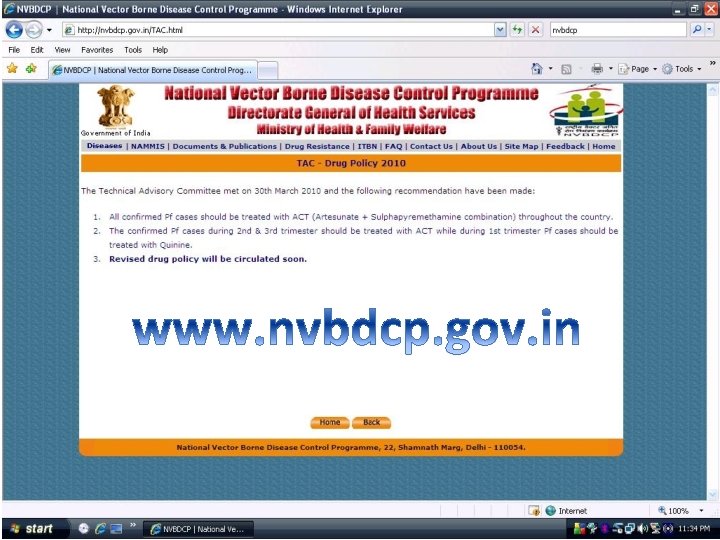
NVBDCP 2010 ALL CONFIRMED CASES OF PF SHOULD BE TREATED WITH ACT +SP NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 3
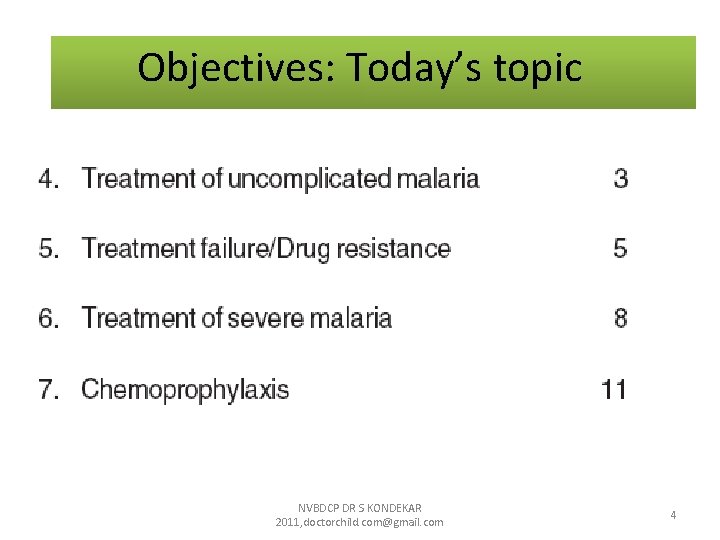
Objectives: Today’s topic NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 4
WHY GUIDELINES • 1. 5 million confirmed cases are reported annually by the NVBDCP • about 50% are due to Plasmodium falciparum. • Malaria is curable if effective treatment is started early. • Delay in treatment may lead to serious consequences including death NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 5
WHY GUIDELINES • chloroquine-resistant PF increasing • The continued treatment of PF with chloroquine = MORE RESISTANT PF = MORE LETHAL MALARIA. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 6
WHY GUIDELINES • VARIABLE RESISTANCE PATTERN ACROSS WORLD • GLOBAL/WHO GUIDELINES NOT DIRECTLY APPLICABLE IN INDIA NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 7
SUSPECT MALARIA IF • FEVER: INTERMITTENT, PERIODIC OR CONTINUOUS • CHILLS/RIGORS • MYALGIA, BODY ACHE, HEAD ACHE, ARTHRALGIA, ANOREXIA, NAUSEA , VOMITING • RESIDING IN OR A VISIT TO – ENDEMIC AREA NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 8
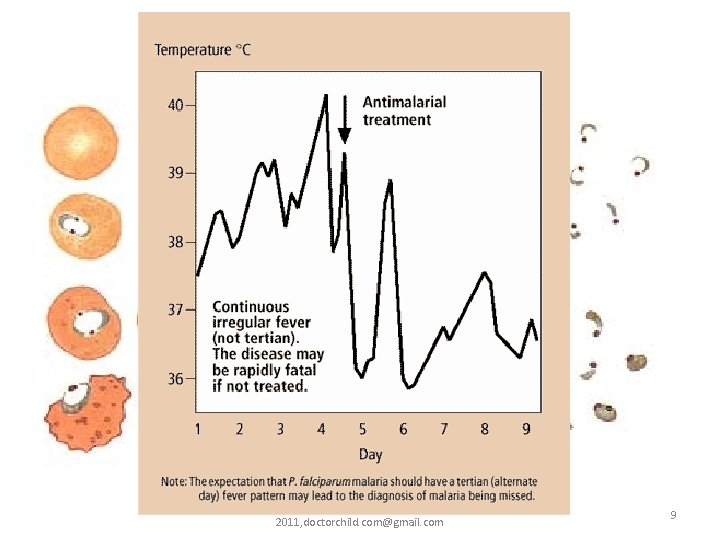
trophozites NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 9
ANY FEVER CAN BE MALARIA • The symptoms of malaria can be non-specific and mimic other diseases like viral infections, enteric fever etc. • Although malaria is known to mimic the signs and symptoms of many common infectious diseases, the other causes should also be suspected and investigated NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 10
All clinically suspected malaria cases should be investigated immediately by microscopy and/or Rapid Diagnostic Test (RDT). A MAJOR BREAKTHROUGH NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 11
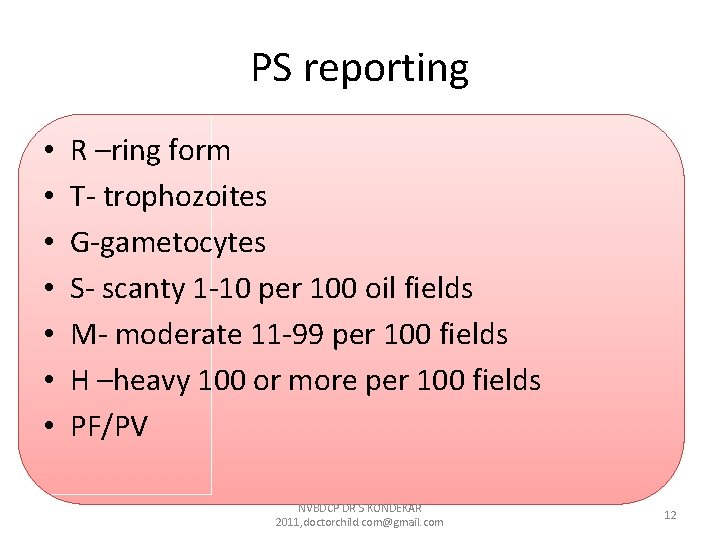
PS reporting • • R –ring form T- trophozoites G-gametocytes S- scanty 1 -10 per 100 oil fields M- moderate 11 -99 per 100 fields H –heavy 100 or more per 100 fields PF/PV NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 12
WHEN INVESTIGATIONS NOT POSSIBLE AND CLINICALLY SUSPECTED START CHQ NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 13
Early diagnosis and treatment of cases of malaria aims at • Complete cure • Prevention of progression of uncomplicated malaria to severe disease • Prevention of deaths • Interruption of transmission • Minimizing risk of selection and spread of drug resistant parasites. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 14
4. Treatment of uncomplicated malaria 4. 1 Treatment of P. vivax malaria 4. 2 Treatment of P. falciparum malaria 4. 3 Treatment of malaria in pregnancy 4. 4 Treatment of mixed infections 4. 5 Treatment based on clinical criteria without laboratory confirmation 4. 6 General recommendations for the management of uncomplicated malaria NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 15
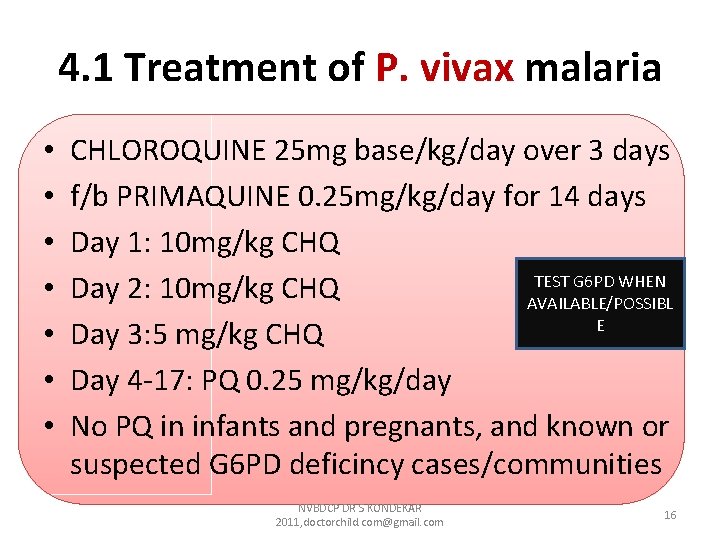
4. 1 Treatment of P. vivax malaria • • CHLOROQUINE 25 mg base/kg/day over 3 days f/b PRIMAQUINE 0. 25 mg/kg/day for 14 days Day 1: 10 mg/kg CHQ TEST G 6 PD WHEN Day 2: 10 mg/kg CHQ AVAILABLE/POSSIBL E Day 3: 5 mg/kg CHQ Day 4 -17: PQ 0. 25 mg/kg/day No PQ in infants and pregnants, and known or suspected G 6 PD deficincy cases/communities NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 16
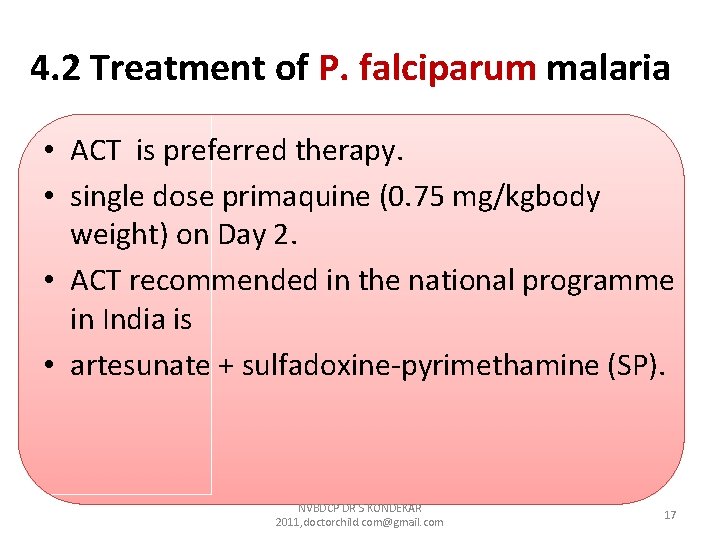
4. 2 Treatment of P. falciparum malaria • ACT is preferred therapy. • single dose primaquine (0. 75 mg/kgbody weight) on Day 2. • ACT recommended in the national programme in India is • artesunate + sulfadoxine-pyrimethamine (SP). NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 17
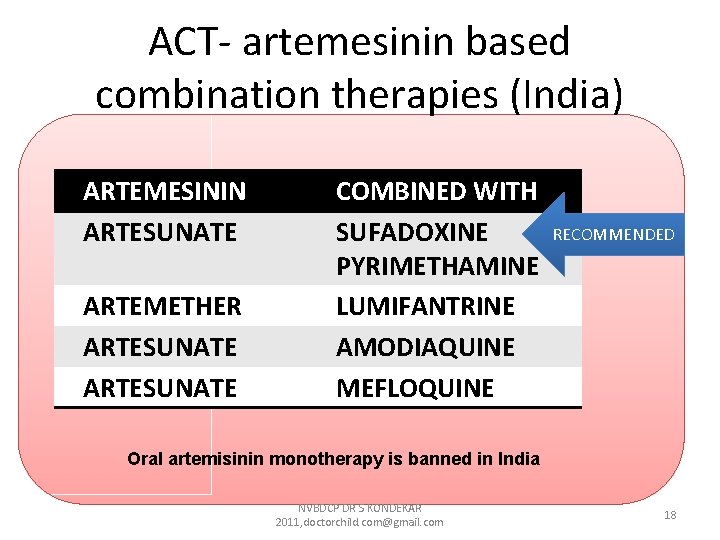
ACT- artemesinin based combination therapies (India) ARTEMESININ ARTESUNATE ARTEMETHER ARTESUNATE COMBINED WITH SUFADOXINE PYRIMETHAMINE LUMIFANTRINE AMODIAQUINE MEFLOQUINE RECOMMENDED Oral artemisinin monotherapy is banned in India NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 18
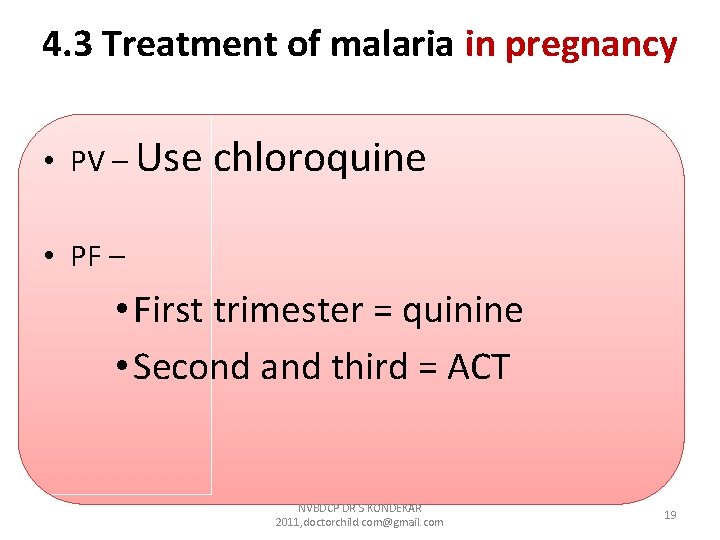
4. 3 Treatment of malaria in pregnancy • PV – Use chloroquine • PF – • First trimester = quinine • Second and third = ACT NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 19
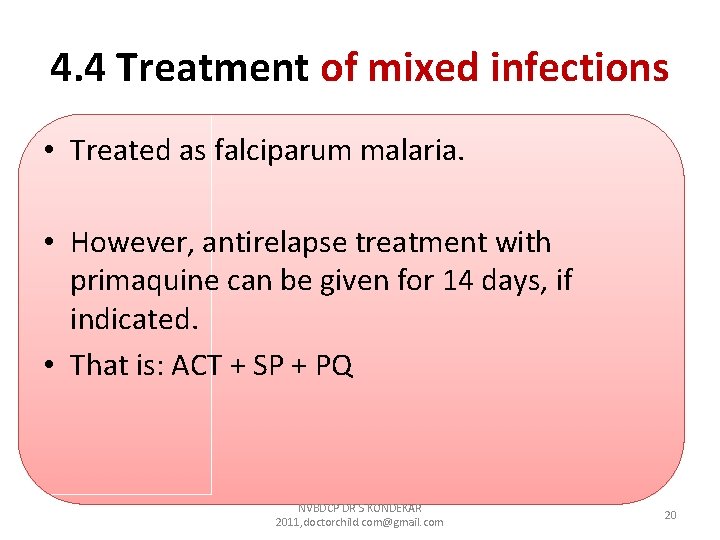
4. 4 Treatment of mixed infections • Treated as falciparum malaria. • However, antirelapse treatment with primaquine can be given for 14 days, if indicated. • That is: ACT + SP + PQ NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 20
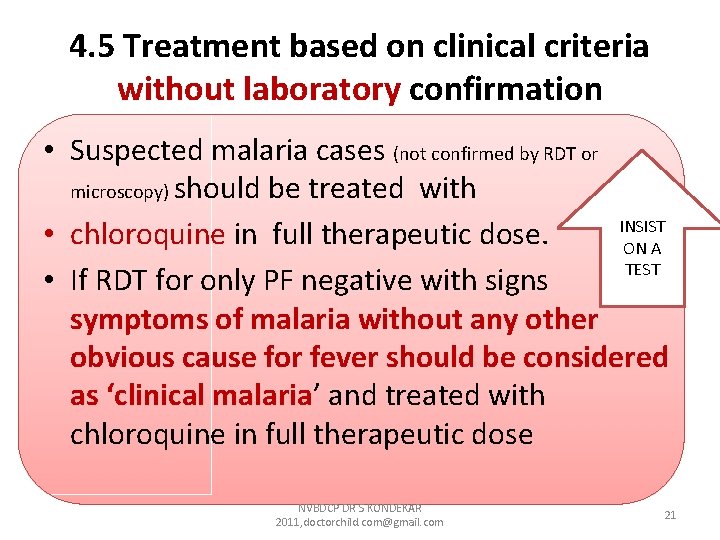
4. 5 Treatment based on clinical criteria without laboratory confirmation • Suspected malaria cases (not confirmed by RDT or microscopy) should be treated with INSIST • chloroquine in full therapeutic dose. ON A TEST • If RDT for only PF negative with signs symptoms of malaria without any other obvious cause for fever should be considered as ‘clinical malaria’ and treated with chloroquine in full therapeutic dose NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 21
4. 6 General recommendations for the management of uncomplicated malaria • Avoid starting Rx on an empty stomach. The first dose should be given under observation. • Dose repeated if vomit in 30 minutes. • Report back, if there is no improvement after 48 hours or if the situation deteriorates. • The patient should also be examined for concomitant illnesses. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 22
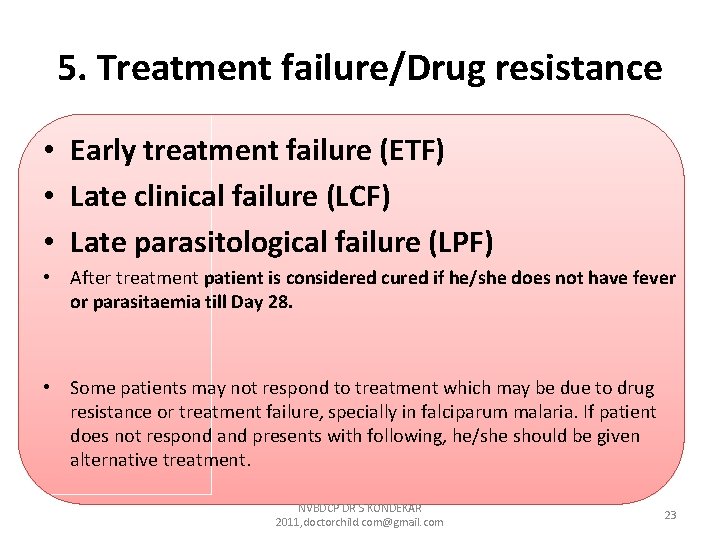
5. Treatment failure/Drug resistance • Early treatment failure (ETF) • Late clinical failure (LCF) • Late parasitological failure (LPF) • After treatment patient is considered cured if he/she does not have fever or parasitaemia till Day 28. • Some patients may not respond to treatment which may be due to drug resistance or treatment failure, specially in falciparum malaria. If patient does not respond and presents with following, he/she should be given alternative treatment. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 23
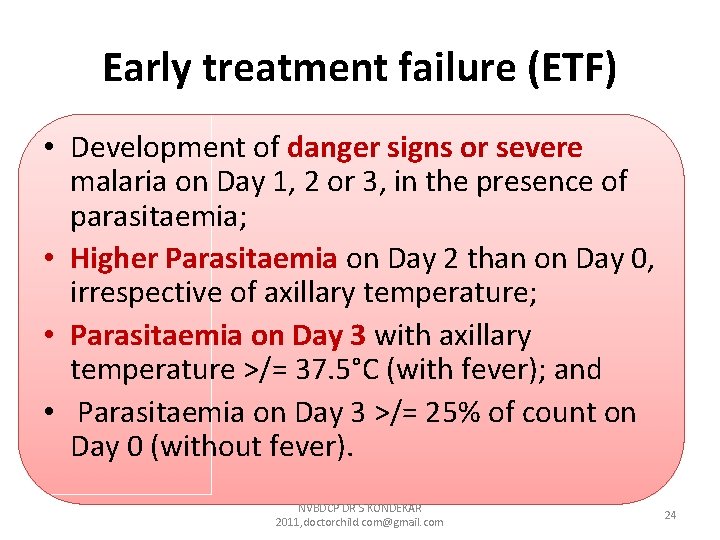
Early treatment failure (ETF) • Development of danger signs or severe malaria on Day 1, 2 or 3, in the presence of parasitaemia; • Higher Parasitaemia on Day 2 than on Day 0, irrespective of axillary temperature; • Parasitaemia on Day 3 with axillary temperature >/= 37. 5°C (with fever); and • Parasitaemia on Day 3 >/= 25% of count on Day 0 (without fever). NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 24
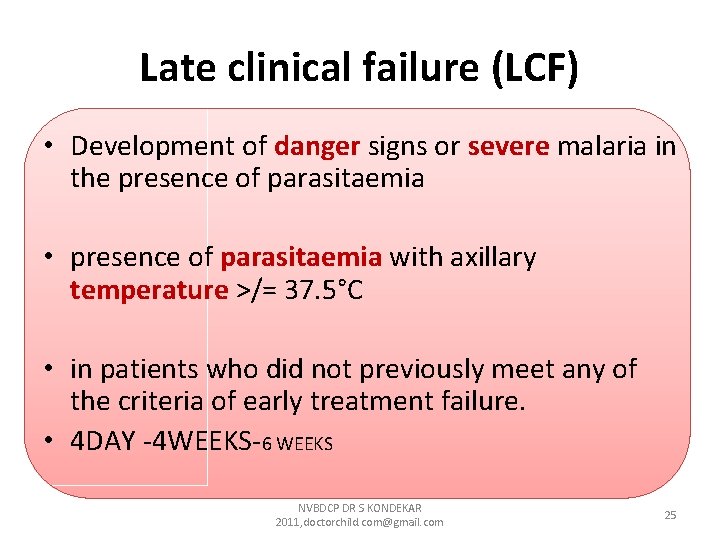
Late clinical failure (LCF) • Development of danger signs or severe malaria in the presence of parasitaemia • presence of parasitaemia with axillary temperature >/= 37. 5°C • in patients who did not previously meet any of the criteria of early treatment failure. • 4 DAY -4 WEEKS-6 WEEKS NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 25
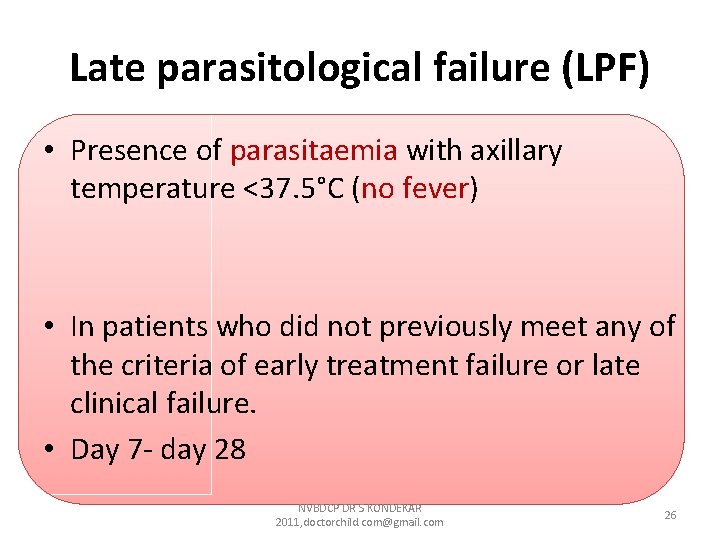
Late parasitological failure (LPF) • Presence of parasitaemia with axillary temperature <37. 5°C (no fever) • In patients who did not previously meet any of the criteria of early treatment failure or late clinical failure. • Day 7 - day 28 NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 26
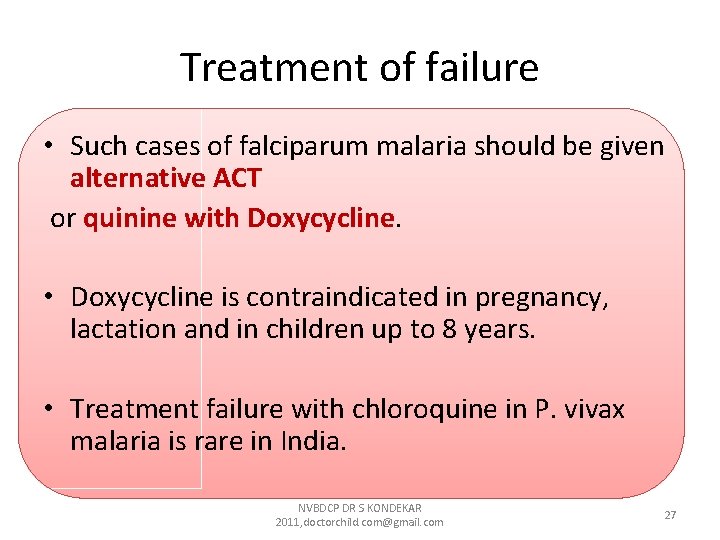
Treatment of failure • Such cases of falciparum malaria should be given alternative ACT or quinine with Doxycycline. • Doxycycline is contraindicated in pregnancy, lactation and in children up to 8 years. • Treatment failure with chloroquine in P. vivax malaria is rare in India. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 27
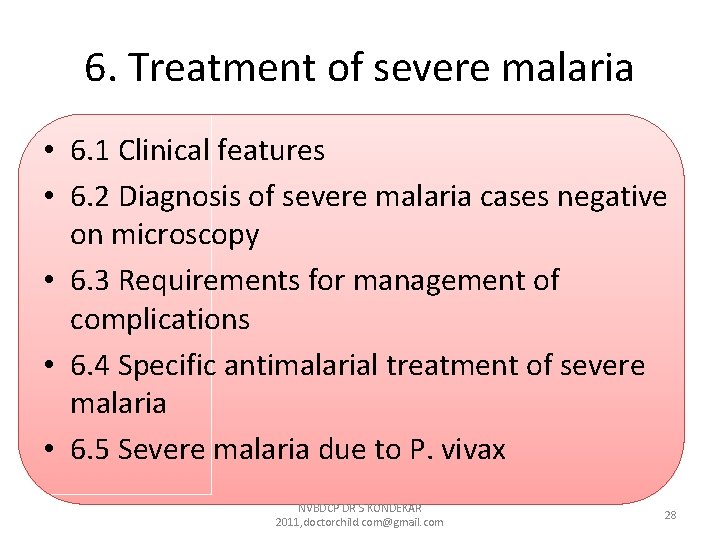
6. Treatment of severe malaria • 6. 1 Clinical features • 6. 2 Diagnosis of severe malaria cases negative on microscopy • 6. 3 Requirements for management of complications • 6. 4 Specific antimalarial treatment of severe malaria • 6. 5 Severe malaria due to P. vivax NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 28
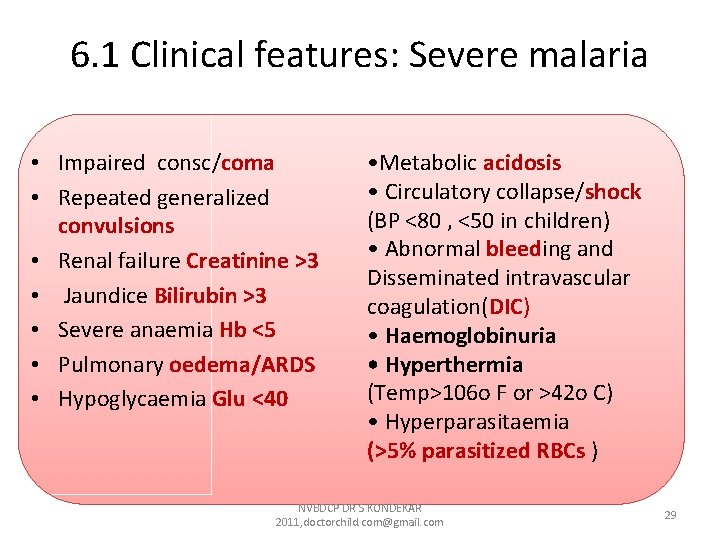
6. 1 Clinical features: Severe malaria • Impaired consc/coma • Repeated generalized convulsions • Renal failure Creatinine >3 • Jaundice Bilirubin >3 • Severe anaemia Hb <5 • Pulmonary oedema/ARDS • Hypoglycaemia Glu <40 • Metabolic acidosis • Circulatory collapse/shock (BP <80 , <50 in children) • Abnormal bleeding and Disseminated intravascular coagulation(DIC) • Haemoglobinuria • Hyperthermia (Temp>106 o F or >42 o C) • Hyperparasitaemia (>5% parasitized RBCs ) NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 29
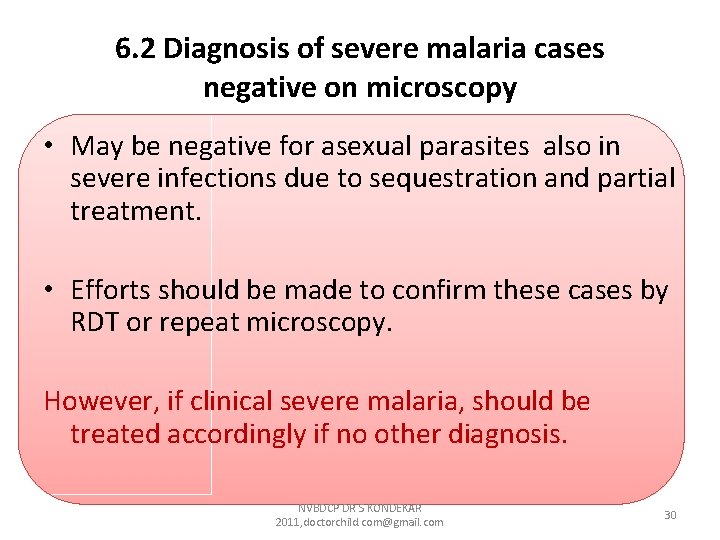
6. 2 Diagnosis of severe malaria cases negative on microscopy • May be negative for asexual parasites also in severe infections due to sequestration and partial treatment. • Efforts should be made to confirm these cases by RDT or repeat microscopy. However, if clinical severe malaria, should be treated accordingly if no other diagnosis. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 30
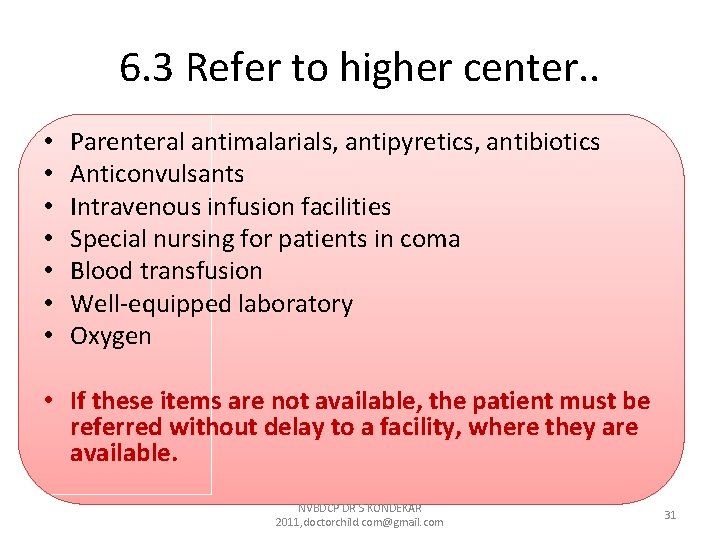
6. 3 Refer to higher center. . • • Parenteral antimalarials, antipyretics, antibiotics Anticonvulsants Intravenous infusion facilities Special nursing for patients in coma Blood transfusion Well-equipped laboratory Oxygen • If these items are not available, the patient must be referred without delay to a facility, where they are available. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 31
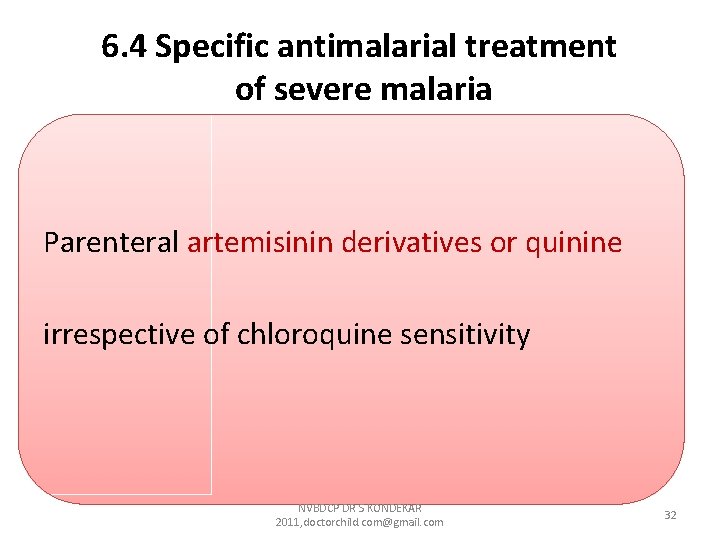
6. 4 Specific antimalarial treatment of severe malaria Parenteral artemisinin derivatives or quinine irrespective of chloroquine sensitivity NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 32
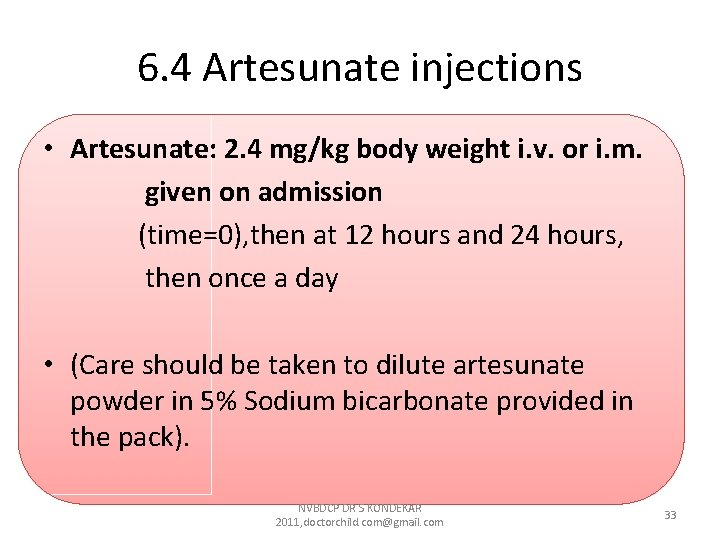
6. 4 Artesunate injections • Artesunate: 2. 4 mg/kg body weight i. v. or i. m. given on admission (time=0), then at 12 hours and 24 hours, then once a day • (Care should be taken to dilute artesunate powder in 5% Sodium bicarbonate provided in the pack). NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 33
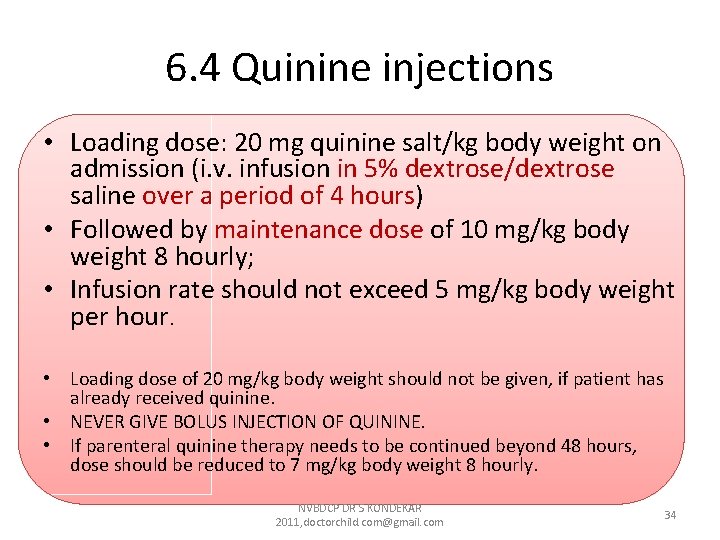
6. 4 Quinine injections • Loading dose: 20 mg quinine salt/kg body weight on admission (i. v. infusion in 5% dextrose/dextrose saline over a period of 4 hours) • Followed by maintenance dose of 10 mg/kg body weight 8 hourly; • Infusion rate should not exceed 5 mg/kg body weight per hour. • Loading dose of 20 mg/kg body weight should not be given, if patient has already received quinine. • NEVER GIVE BOLUS INJECTION OF QUININE. • If parenteral quinine therapy needs to be continued beyond 48 hours, dose should be reduced to 7 mg/kg body weight 8 hourly. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 34
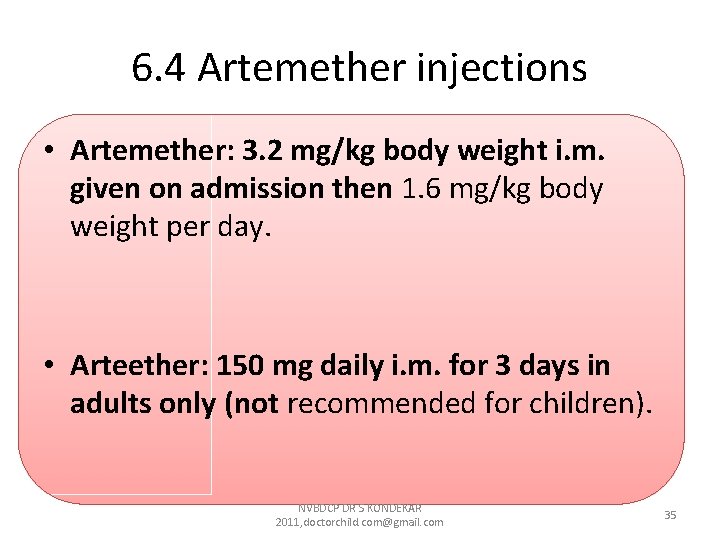
6. 4 Artemether injections • Artemether: 3. 2 mg/kg body weight i. m. given on admission then 1. 6 mg/kg body weight per day. • Arteether: 150 mg daily i. m. for 3 days in adults only (not recommended for children). NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 35
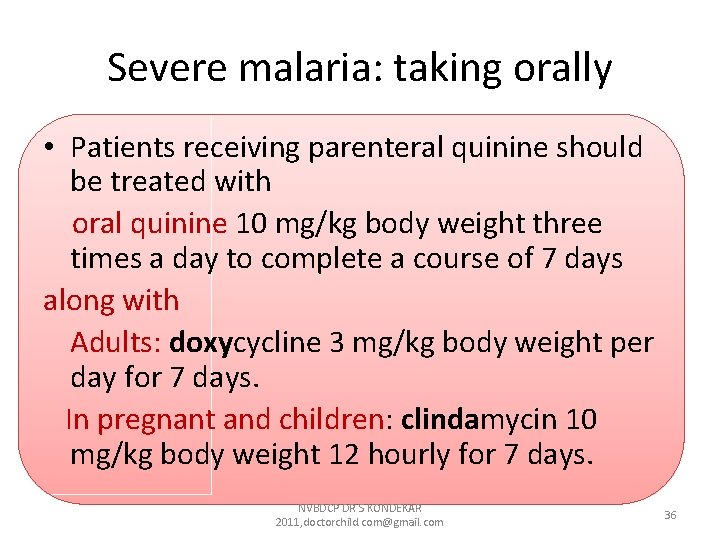
Severe malaria: taking orally • Patients receiving parenteral quinine should be treated with oral quinine 10 mg/kg body weight three times a day to complete a course of 7 days along with Adults: doxycycline 3 mg/kg body weight per day for 7 days. In pregnant and children: clindamycin 10 mg/kg body weight 12 hourly for 7 days. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 36
Severe malaria: taking orally • Patients receiving artemisinin derivatives should get full course of oral ACT. • Avoid: ACT containing mefloquine in cerebral malaria - neuropsychiatric complications. • IV better than IM. Parenteral treatment should be given for minimum of 24 hours once started. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 37
Severe malaria in pregnancy • In first trimester of pregnancy, parenteral quinine is the drug of choice. • However, if quinine is not available, artemisinin derivatives may be given to save the life of mother. • In second and third trimester, parenteral artemisinin derivatives are preferred. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 38
6. 5 Severe vivax malaria • Recent rise in such cases • Severe malaria caused by P. vivax should be treated like severe P. falciparum malaria. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 39
7. Chemoprophylaxis • 7. 1 Short-term chemoprophylaxis (less than 6 weeks) • 7. 2 Long-term chemoprophylaxis (more than 6 weeks) NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 40
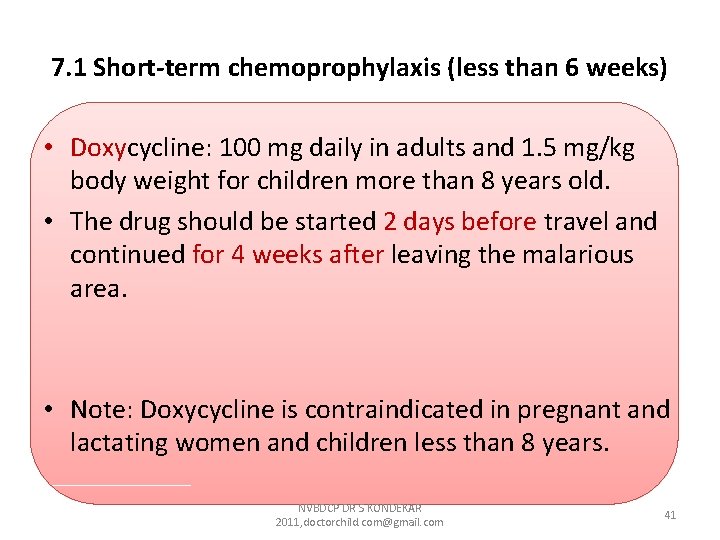
7. 1 Short-term chemoprophylaxis (less than 6 weeks) • Doxycycline: 100 mg daily in adults and 1. 5 mg/kg body weight for children more than 8 years old. • The drug should be started 2 days before travel and continued for 4 weeks after leaving the malarious area. • Note: Doxycycline is contraindicated in pregnant and lactating women and children less than 8 years. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 41
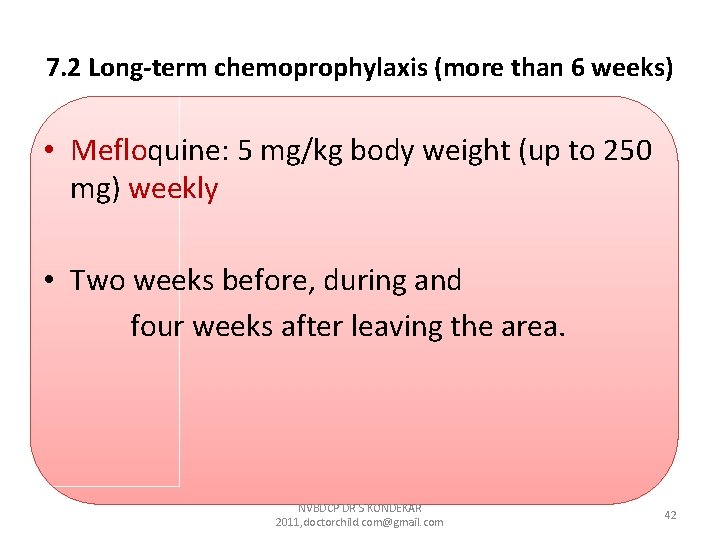
7. 2 Long-term chemoprophylaxis (more than 6 weeks) • Mefloquine: 5 mg/kg body weight (up to 250 mg) weekly • Two weeks before, during and four weeks after leaving the area. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 42
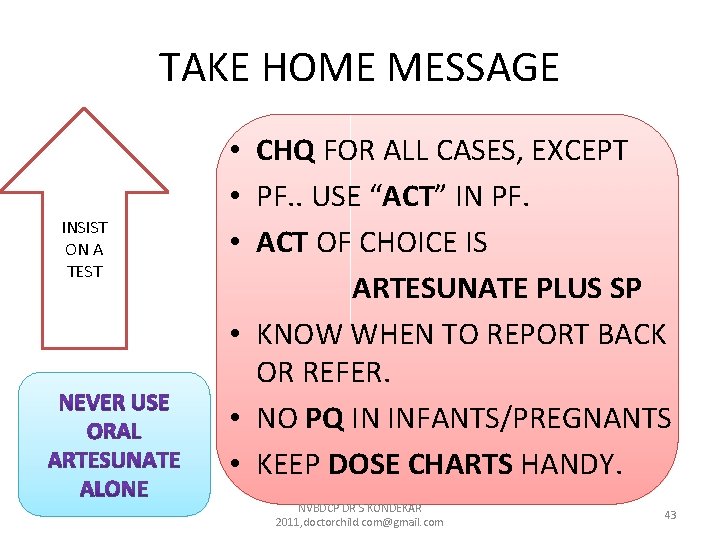
TAKE HOME MESSAGE INSIST ON A TEST • CHQ FOR ALL CASES, EXCEPT • PF. . USE “ACT” IN PF. • ACT OF CHOICE IS ARTESUNATE PLUS SP • KNOW WHEN TO REPORT BACK OR REFER. • NO PQ IN INFANTS/PREGNANTS • KEEP DOSE CHARTS HANDY. NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 43
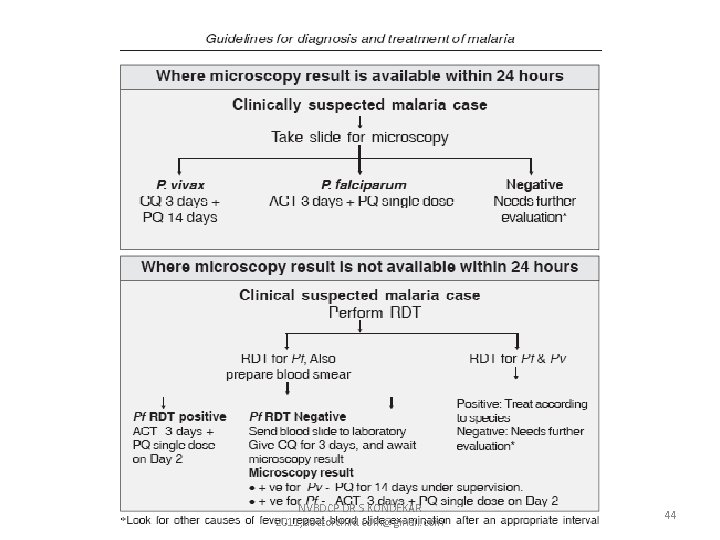
NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 44
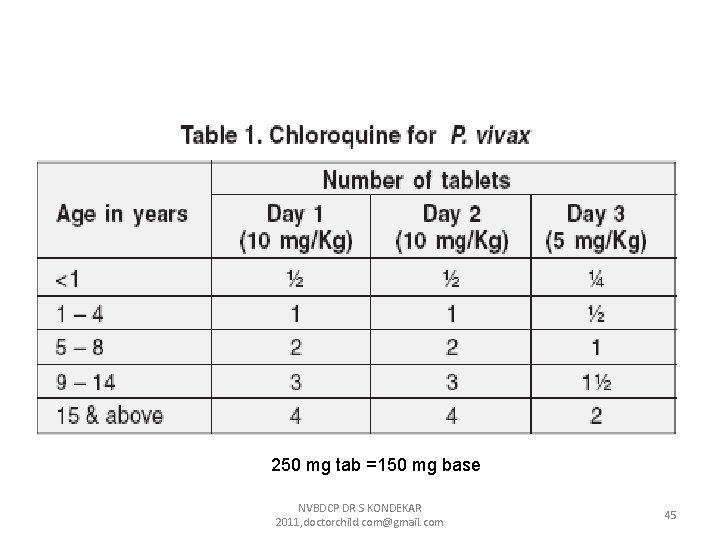
250 mg tab =150 mg base NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 45
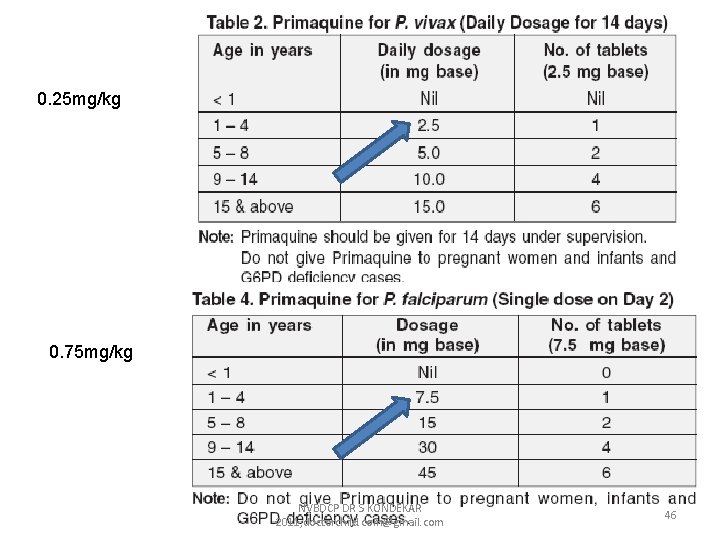
0. 25 mg/kg 0. 75 mg/kg NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 46
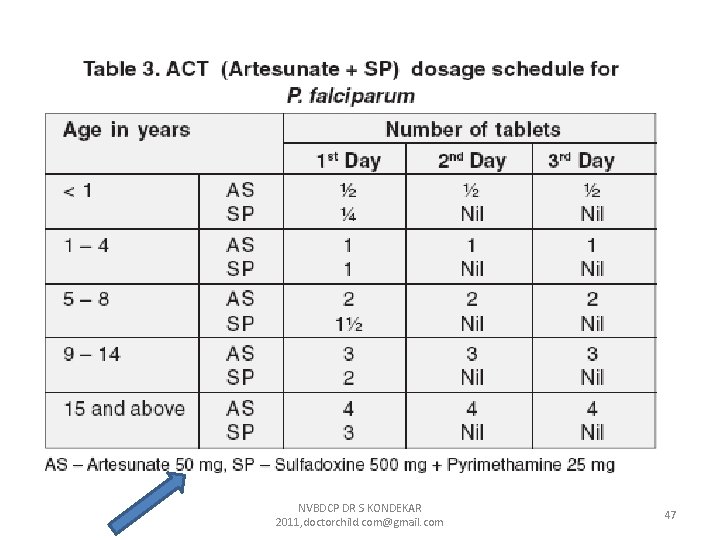
NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com 47
GUIDELINES ARE NOT RULES! BUT APPLICABLE EASILY IN MOST CASES JUDICIOUS JUDGEMENT THE MOST IMPORTANT! NVBDCP DR S KONDEKAR 2011, doctorchild. com@gmail. com Dr Kondekar SV Asso Prof Pediatrics TN Medical college, Mumbai 48 9869405747@in. com
- Slides: 48