Malaria Blood Smear Remains the gold standard for
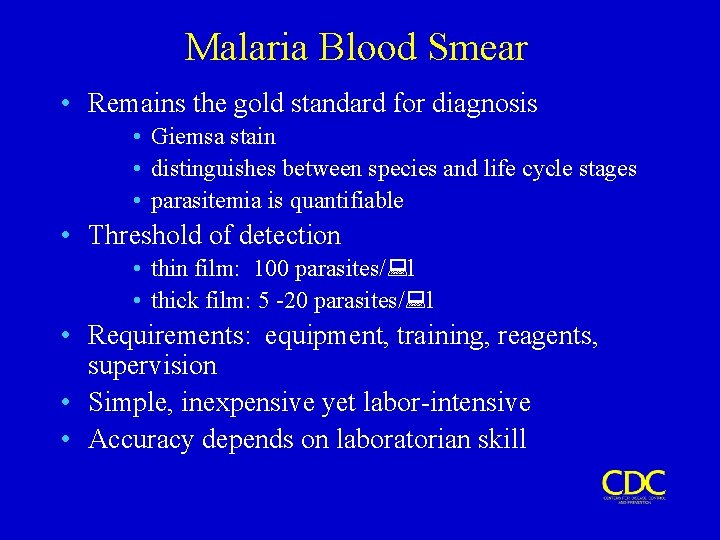
Malaria Blood Smear • Remains the gold standard for diagnosis • Giemsa stain • distinguishes between species and life cycle stages • parasitemia is quantifiable • Threshold of detection • thin film: 100 parasites/ l • thick film: 5 -20 parasites/ l • Requirements: equipment, training, reagents, supervision • Simple, inexpensive yet labor-intensive • Accuracy depends on laboratorian skill
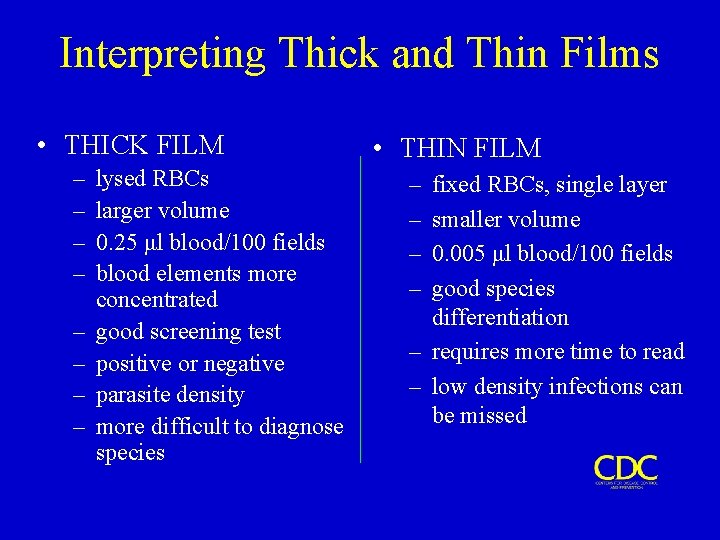
Interpreting Thick and Thin Films • THICK FILM – – – – lysed RBCs larger volume 0. 25 μl blood/100 fields blood elements more concentrated good screening test positive or negative parasite density more difficult to diagnose species • THIN FILM – – fixed RBCs, single layer smaller volume 0. 005 μl blood/100 fields good species differentiation – requires more time to read – low density infections can be missed
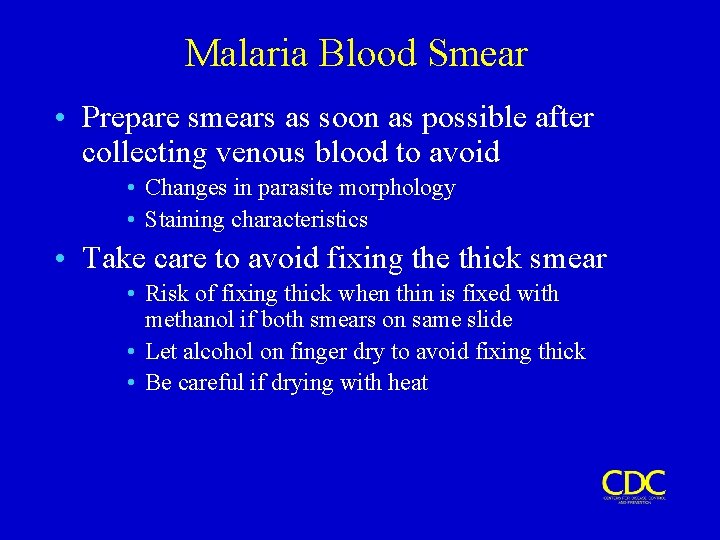
Malaria Blood Smear • Prepare smears as soon as possible after collecting venous blood to avoid • Changes in parasite morphology • Staining characteristics • Take care to avoid fixing the thick smear • Risk of fixing thick when thin is fixed with methanol if both smears on same slide • Let alcohol on finger dry to avoid fixing thick • Be careful if drying with heat
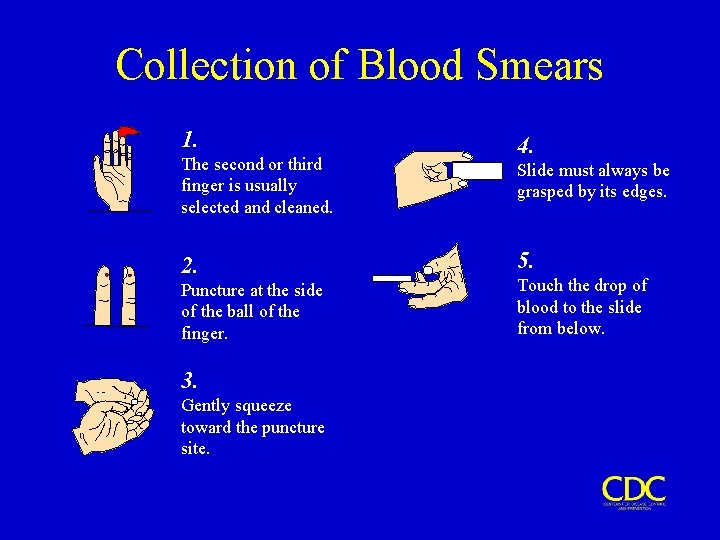
Collection of Blood Smears 1. The second or third finger is usually selected and cleaned. 2. Puncture at the side of the ball of the finger. 3. Gently squeeze toward the puncture site. 4. Slide must always be grasped by its edges. 5. Touch the drop of blood to the slide from below.
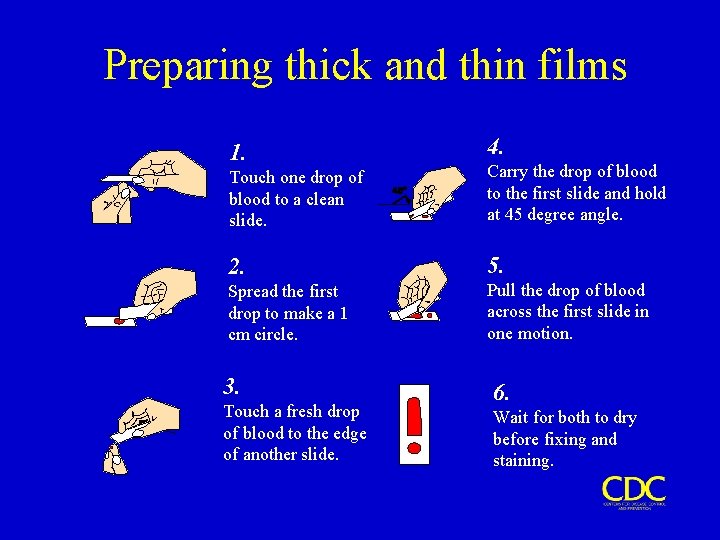
Preparing thick and thin films 1. 4. Touch one drop of blood to a clean slide. Carry the drop of blood to the first slide and hold at 45 degree angle. 2. 5. Spread the first drop to make a 1 cm circle. Pull the drop of blood across the first slide in one motion. 3. Touch a fresh drop of blood to the edge of another slide. 6. Wait for both to dry before fixing and staining.
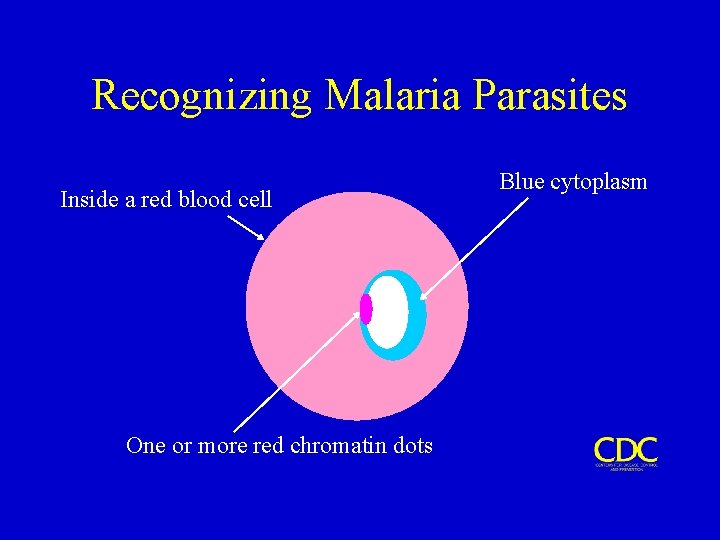
Recognizing Malaria Parasites Inside a red blood cell One or more red chromatin dots Blue cytoplasm
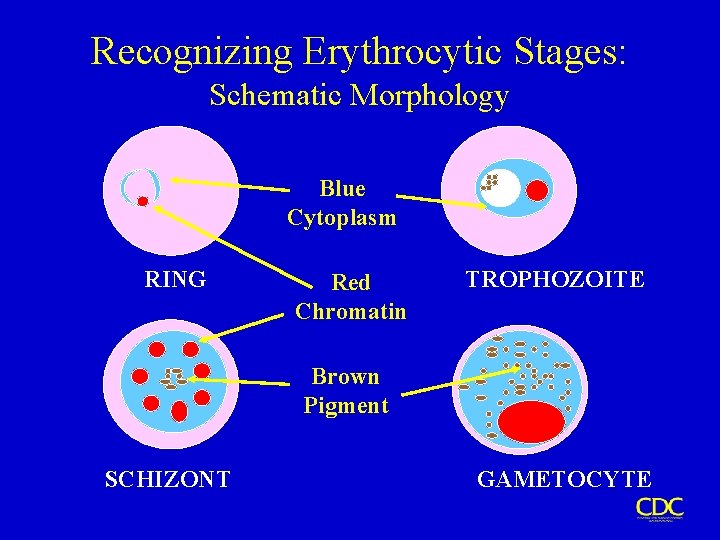
Recognizing Erythrocytic Stages: Schematic Morphology Blue Cytoplasm RING Red Chromatin TROPHOZOITE Brown Pigment SCHIZONT GAMETOCYTE
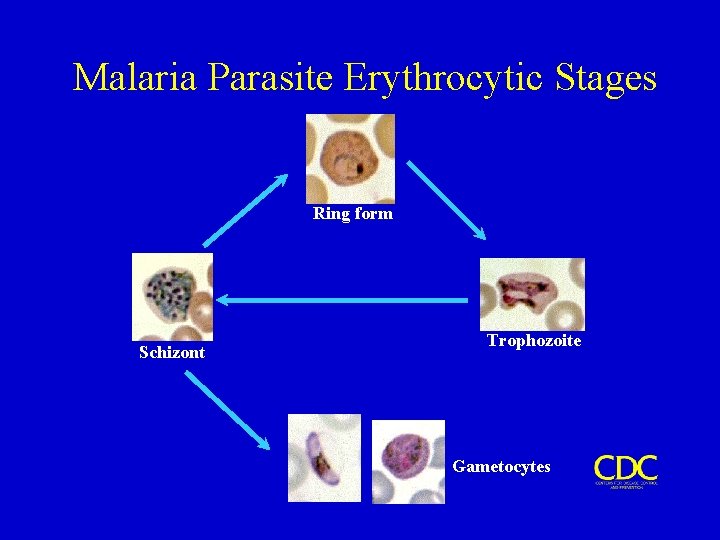
Malaria Parasite Erythrocytic Stages Ring form Schizont Trophozoite Gametocytes
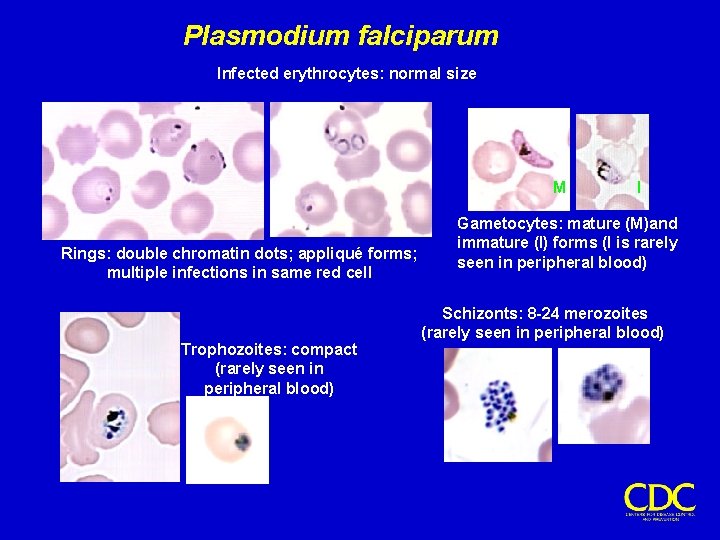
Plasmodium falciparum Infected erythrocytes: normal size M Rings: double chromatin dots; appliqué forms; multiple infections in same red cell Trophozoites: compact (rarely seen in peripheral blood) I Gametocytes: mature (M)and immature (I) forms (I is rarely seen in peripheral blood) Schizonts: 8 -24 merozoites (rarely seen in peripheral blood)
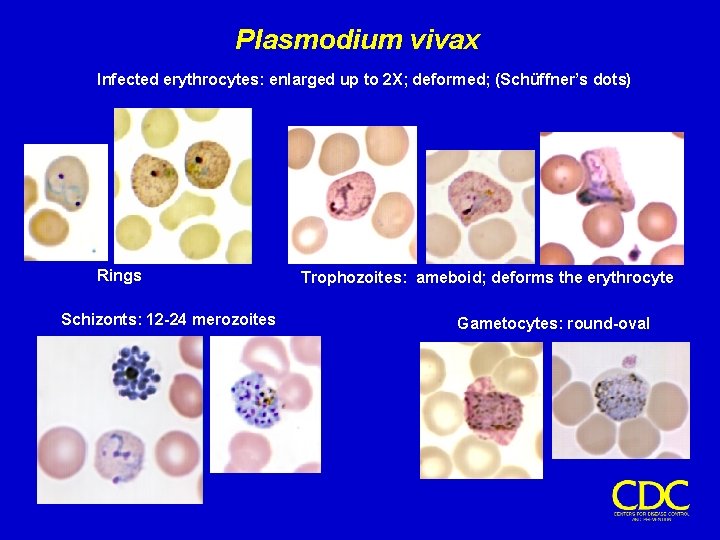
Plasmodium vivax Infected erythrocytes: enlarged up to 2 X; deformed; (Schüffner’s dots) Rings Schizonts: 12 -24 merozoites Trophozoites: ameboid; deforms the erythrocyte Gametocytes: round-oval
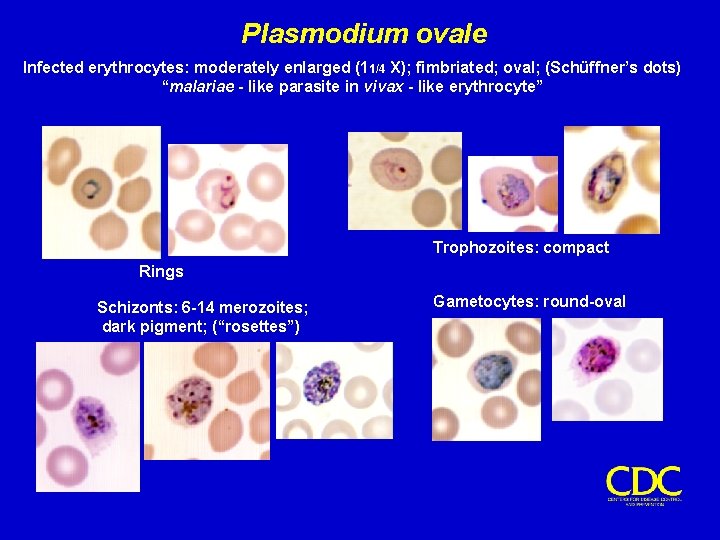
Plasmodium ovale Infected erythrocytes: moderately enlarged (11/4 X); fimbriated; oval; (Schüffner’s dots) “malariae - like parasite in vivax - like erythrocyte” Trophozoites: compact Rings Schizonts: 6 -14 merozoites; dark pigment; (“rosettes”) Gametocytes: round-oval
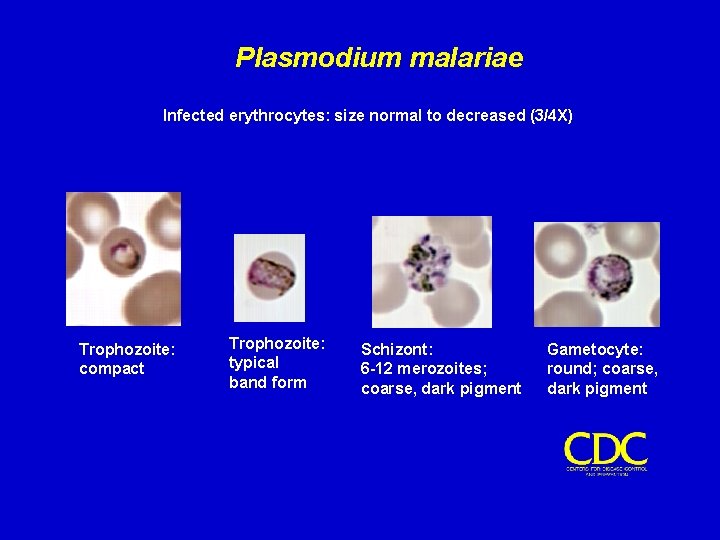
Plasmodium malariae Infected erythrocytes: size normal to decreased (3/4 X) Trophozoite: compact Trophozoite: typical band form Schizont: 6 -12 merozoites; coarse, dark pigment Gametocyte: round; coarse, dark pigment
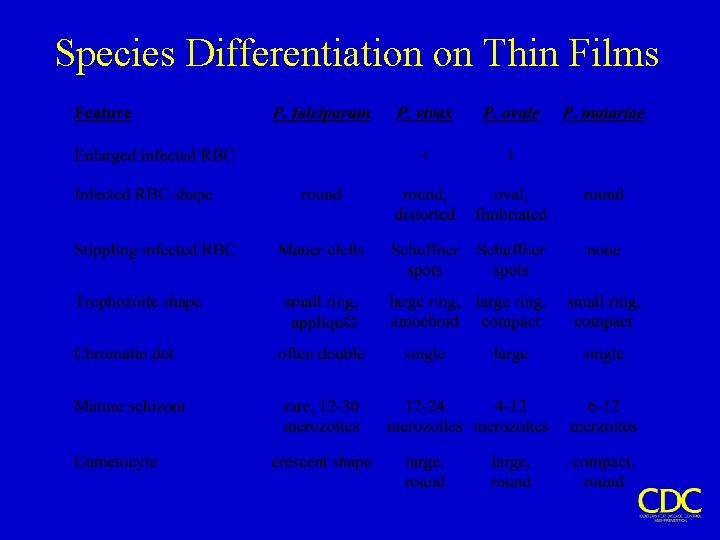
Species Differentiation on Thin Films
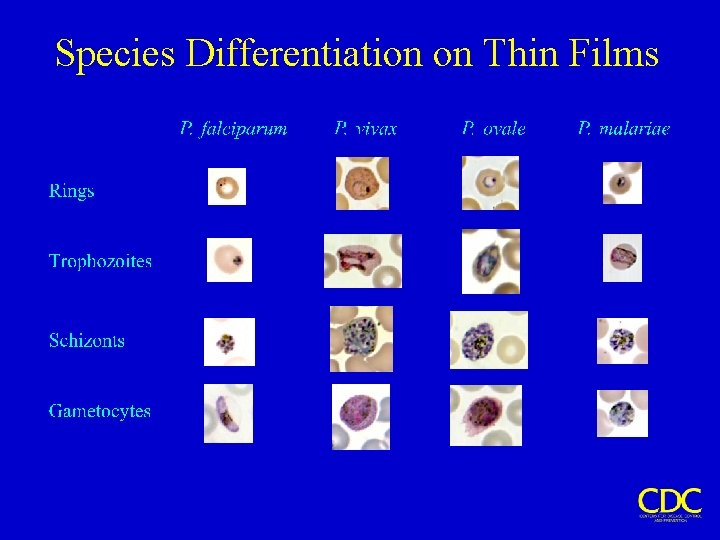
Species Differentiation on Thin Films
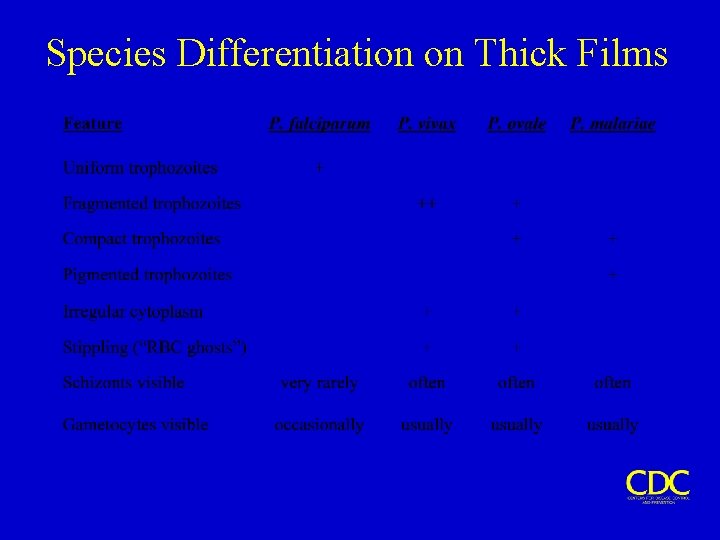
Species Differentiation on Thick Films
- Slides: 15