Malaria An Overview of Lifecycle Morphology and Clinical



- Slides: 39
Malaria An Overview of Life-cycle, Morphology and Clinical Picture
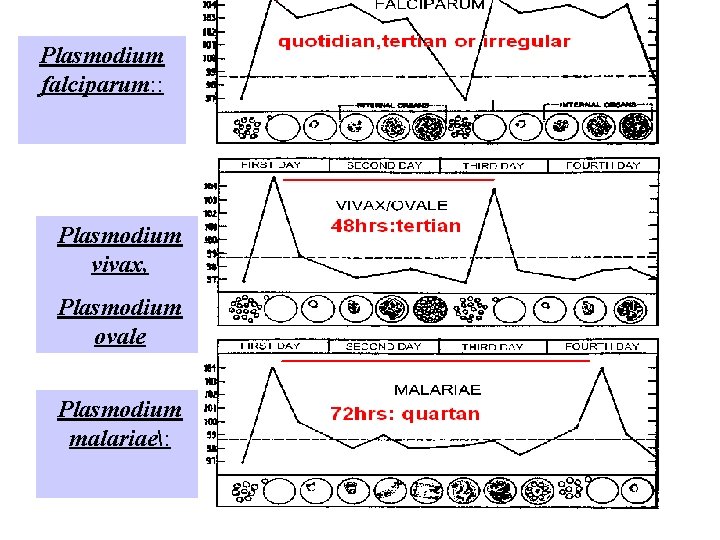
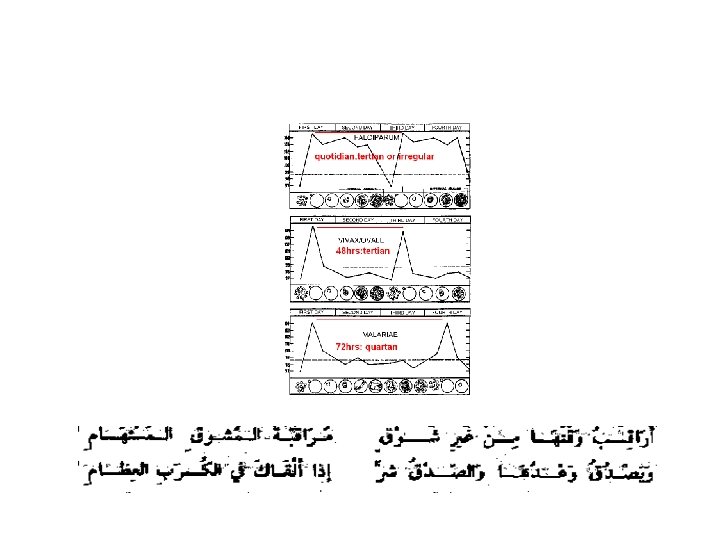
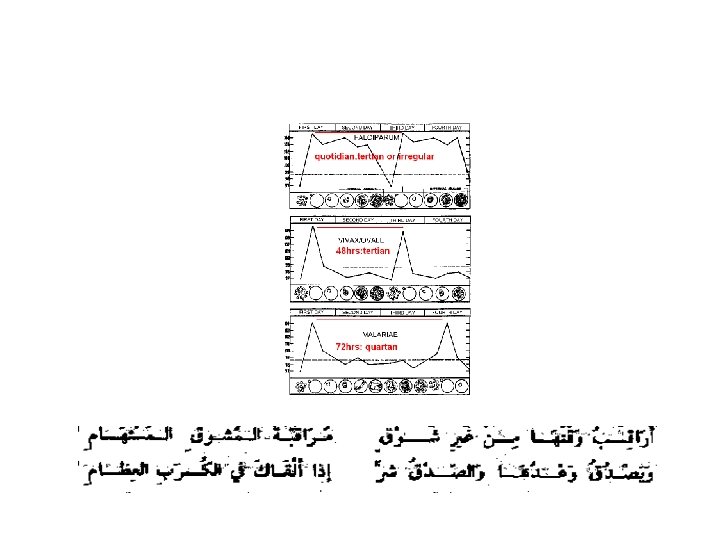
Malaria Species Four species of malaria : – Plasmodium falciparum: malignant tertian malaria – Plasmodium vivax: benign tertian malaria – Plasmodium ovale : benign tertian malaria – Plasmodium malariae: quartan malaria
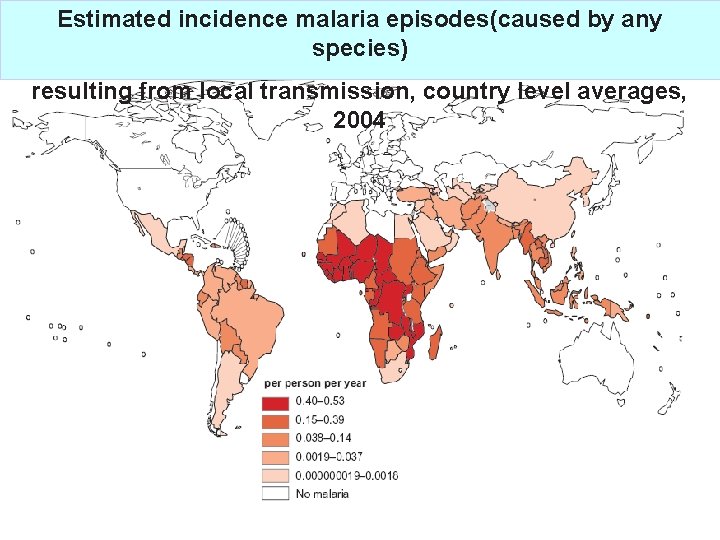
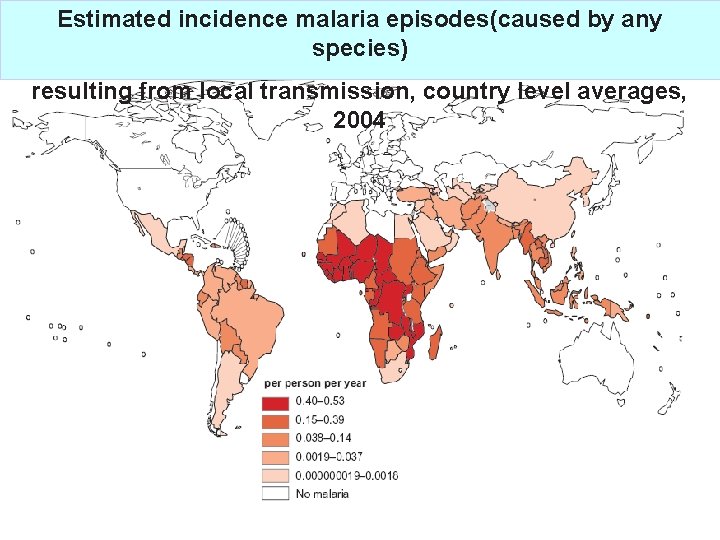
Estimated incidence malaria episodes(caused by any species) resulting from local transmission, country level averages, 2004
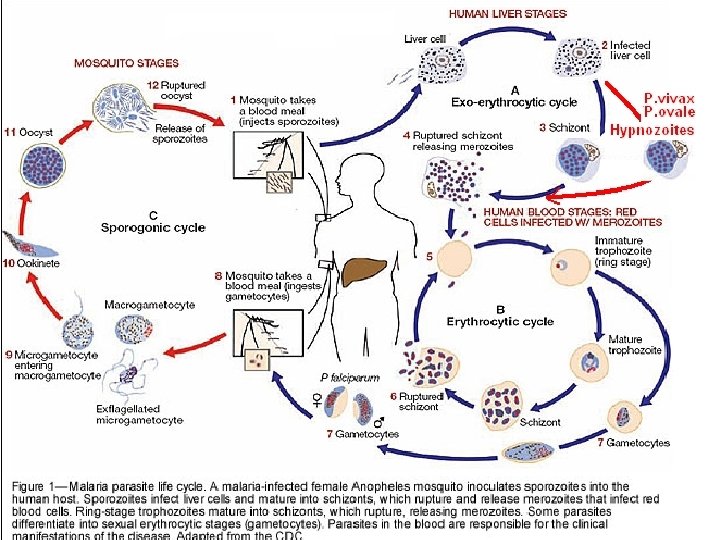
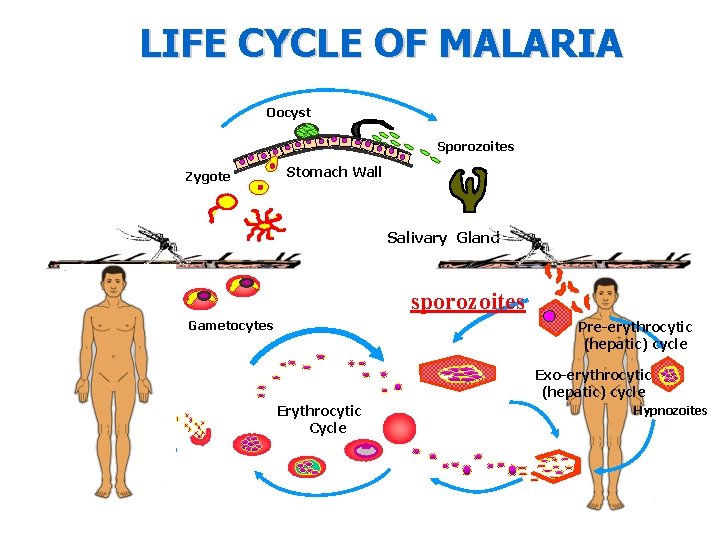
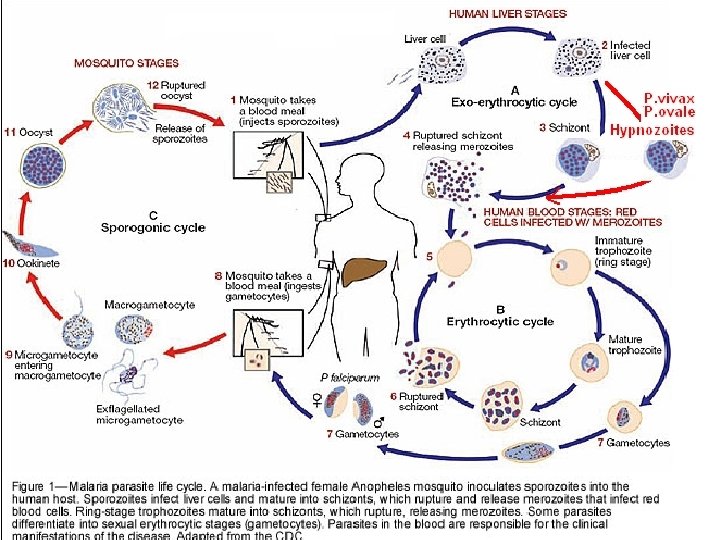
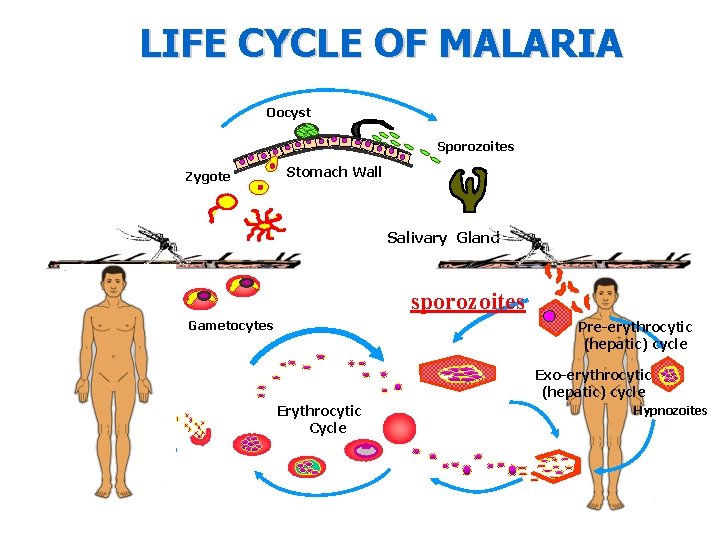
LIFE CYCLE OF MALARIA Oocyst Sporozoites Zygote Stomach Wall Salivary Gland sporozoites Gametocytes Pre-erythrocytic (hepatic) cycle Exo-erythrocytic (hepatic) cycle Erythrocytic Cycle Hypnozoites
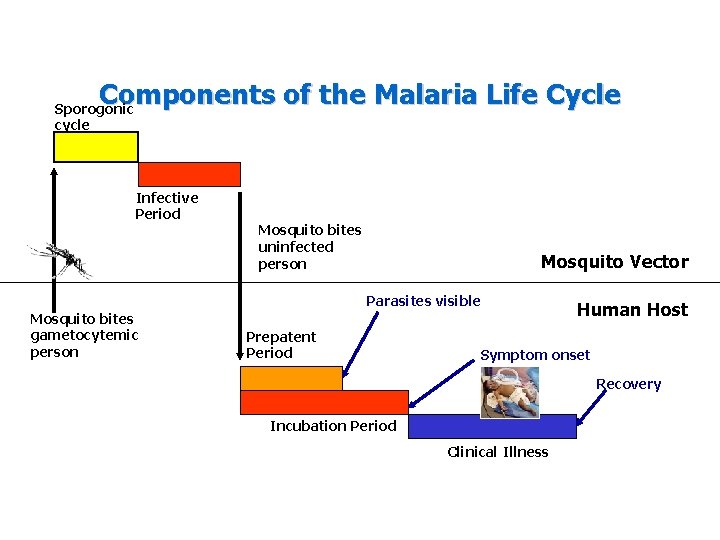
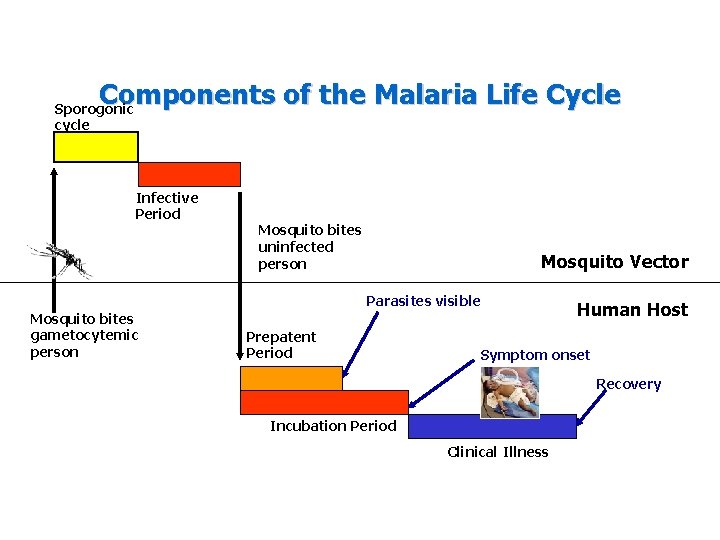
Components of the Malaria Life Cycle Sporogonic cycle Infective Period Mosquito bites uninfected person Mosquito Vector Parasites visible Mosquito bites gametocytemic person Prepatent Period Human Host Symptom onset Recovery Incubation Period Clinical Illness
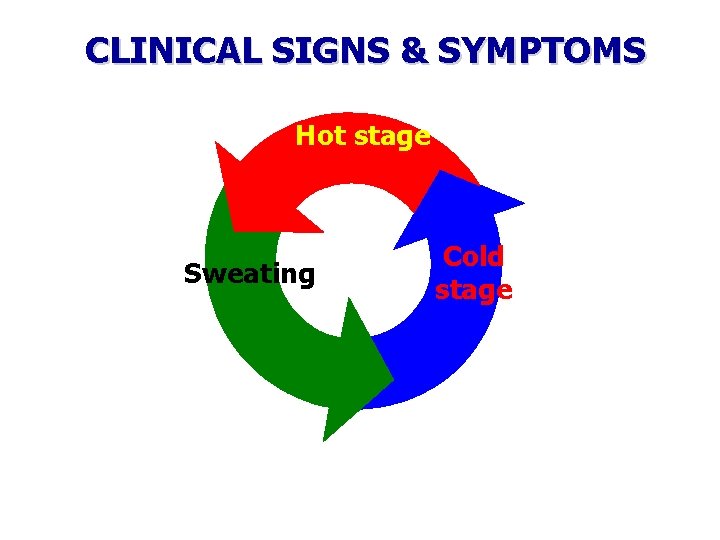
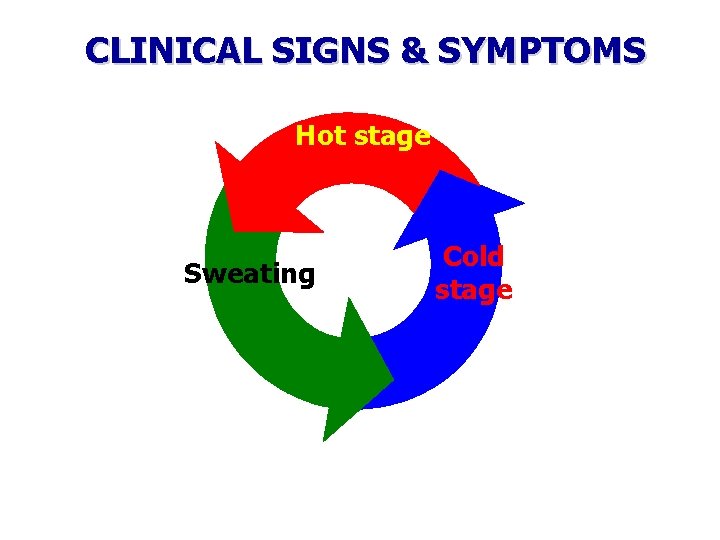
CLINICAL SIGNS & SYMPTOMS Hot stage Sweating Cold stage
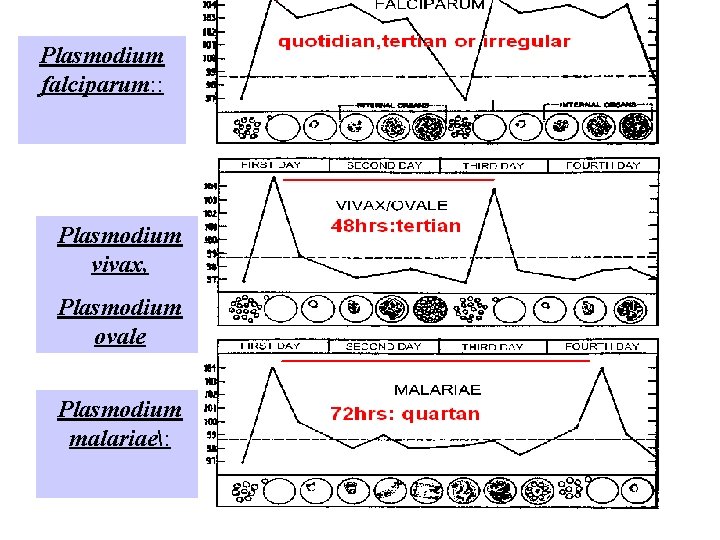
Plasmodium falciparum: : Plasmodium vivax, Plasmodium ovale Plasmodium malariae:
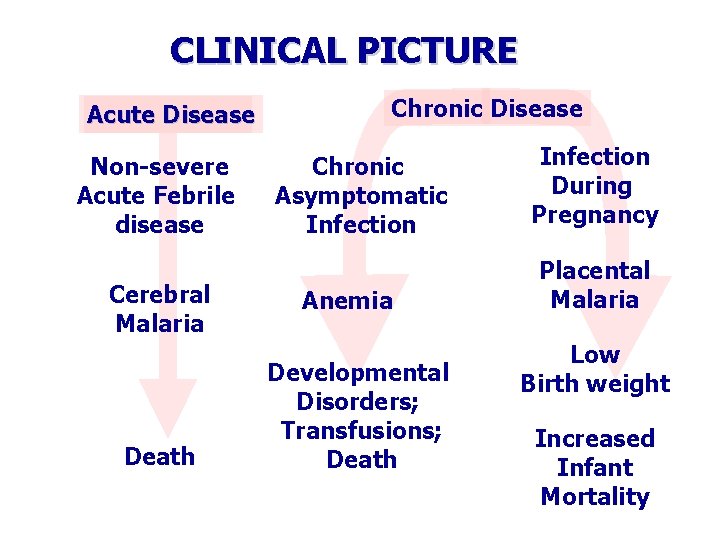
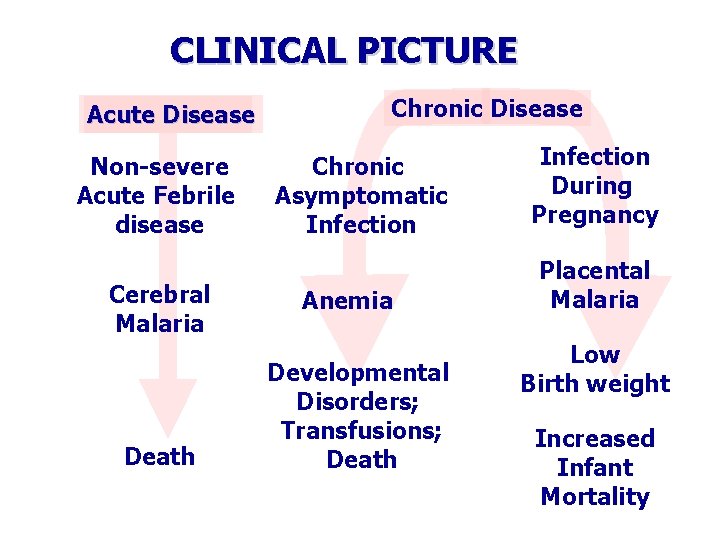
CLINICAL PICTURE Acute Disease Non-severe Acute Febrile disease Cerebral Malaria Death Chronic Disease Chronic Asymptomatic Infection Anemia Developmental Disorders; Transfusions; Death Infection During Pregnancy Placental Malaria Low Birth weight Increased Infant Mortality
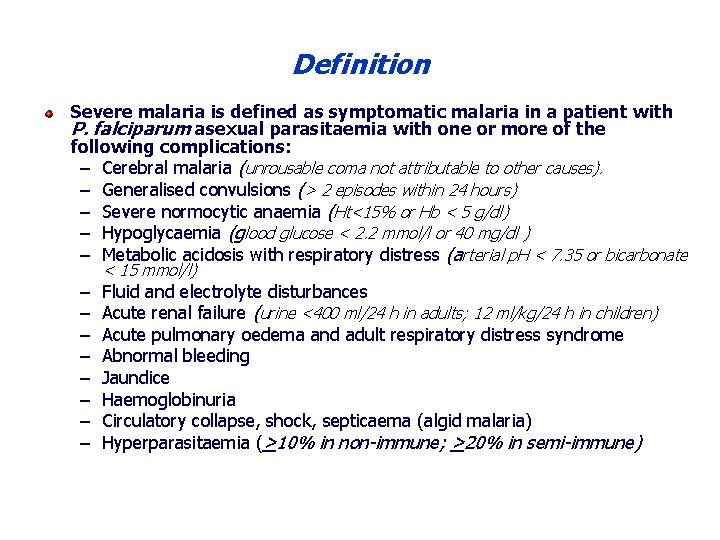
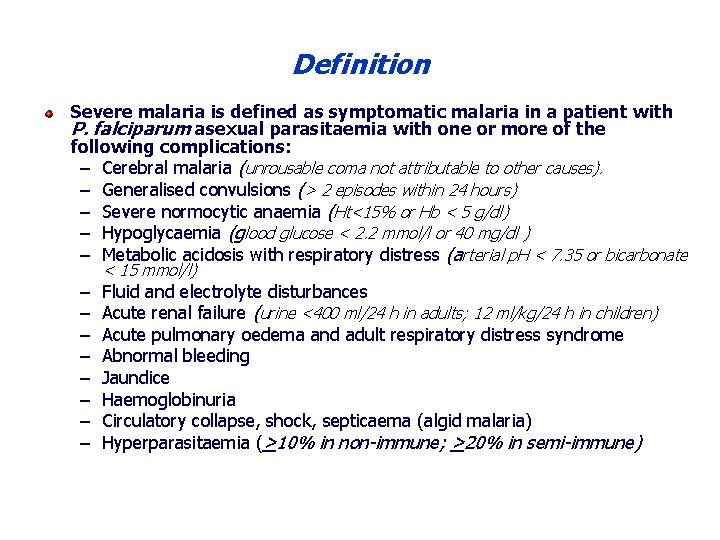
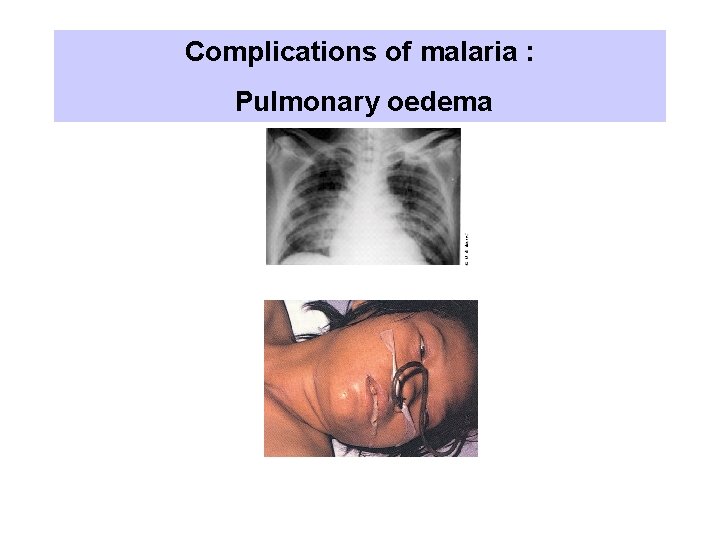
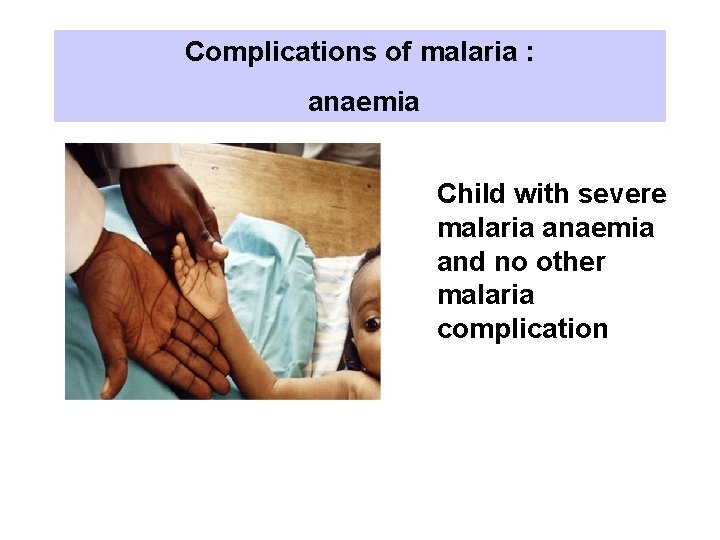
Definition Severe malaria is defined as symptomatic malaria in a patient with P. falciparum asexual parasitaemia with one or more of the following complications: – Cerebral malaria (unrousable coma not attributable to other causes). – Generalised convulsions (> 2 episodes within 24 hours) – Severe normocytic anaemia (Ht<15% or Hb < 5 g/dl) – Hypoglycaemia (glood glucose < 2. 2 mmol/l or 40 mg/dl ) – Metabolic acidosis with respiratory distress (arterial p. H < 7. 35 or bicarbonate – – – – < 15 mmol/l) Fluid and electrolyte disturbances Acute renal failure (urine <400 ml/24 h in adults; 12 ml/kg/24 h in children) Acute pulmonary oedema and adult respiratory distress syndrome Abnormal bleeding Jaundice Haemoglobinuria Circulatory collapse, shock, septicaema (algid malaria) Hyperparasitaemia (>10% in non-immune; >20% in semi-immune)
Definition Uncomplicated malaria is defined as: Symptomatic infection with malaria parasitemia without signs of severity and/or evidence of vital organ dysfunction.
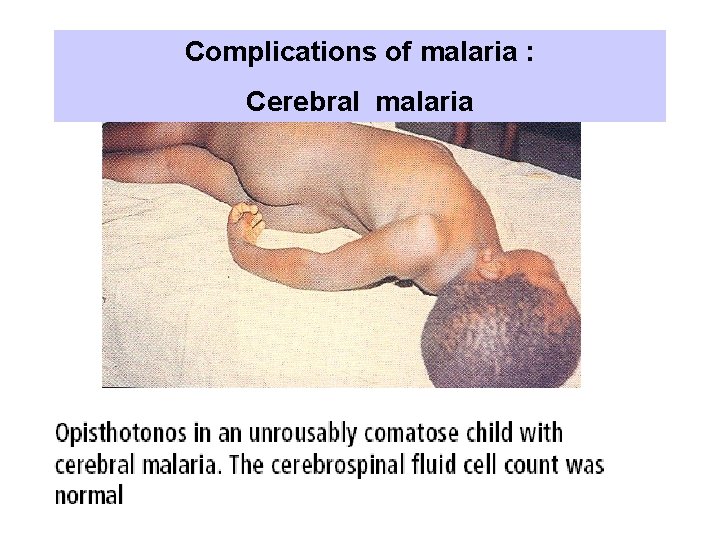
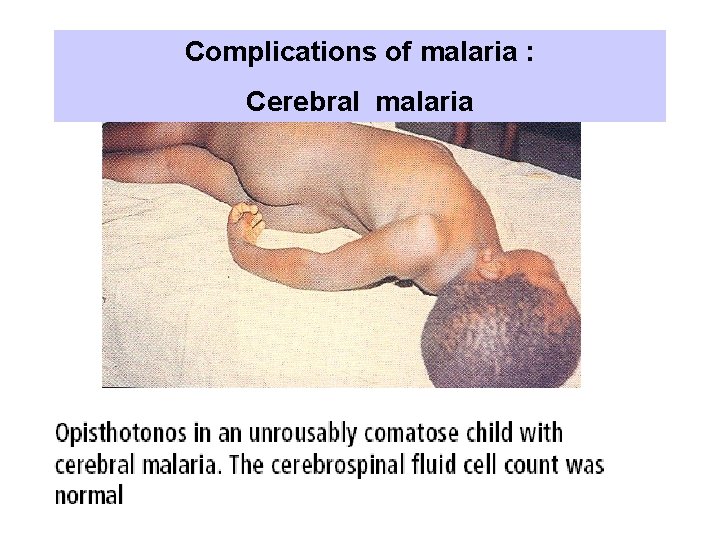
Complications of malaria : Cerebral malaria
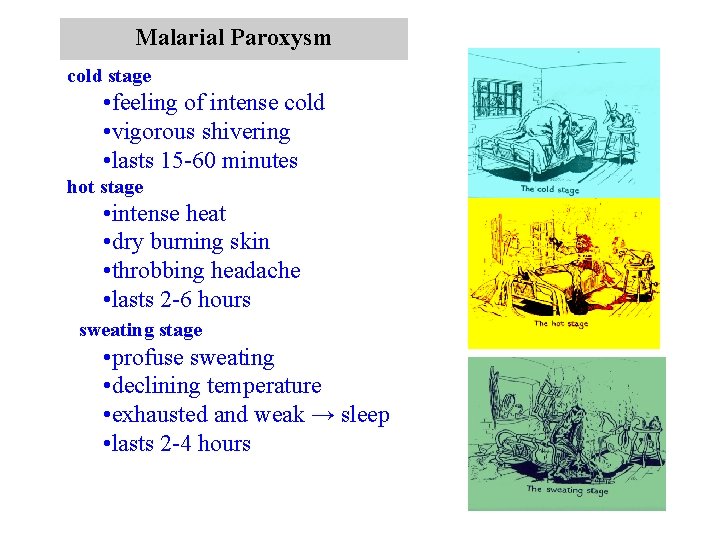
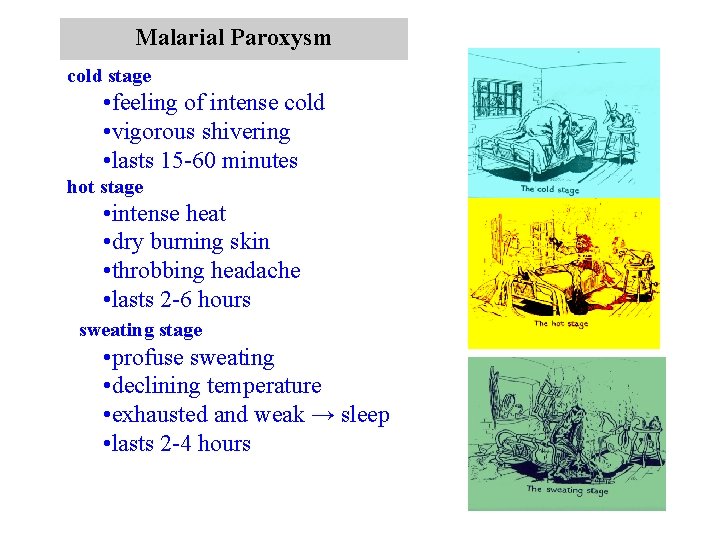
Malarial Paroxysm cold stage • feeling of intense cold • vigorous shivering • lasts 15 -60 minutes hot stage • intense heat • dry burning skin • throbbing headache • lasts 2 -6 hours sweating stage • profuse sweating • declining temperature • exhausted and weak → sleep • lasts 2 -4 hours

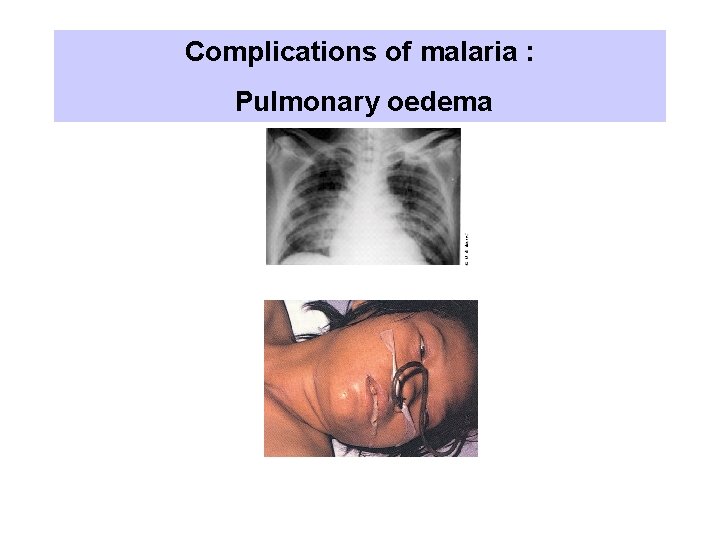
Complications of malaria : Pulmonary oedema
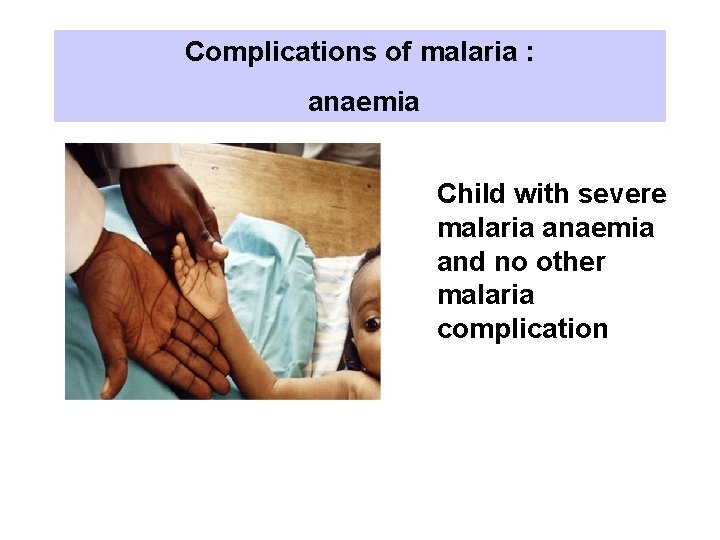
Complications of malaria : anaemia Child with severe malaria anaemia and no other malaria complication

Child with severe malaria anaemia in conjunction with acidosis and respiratory distress
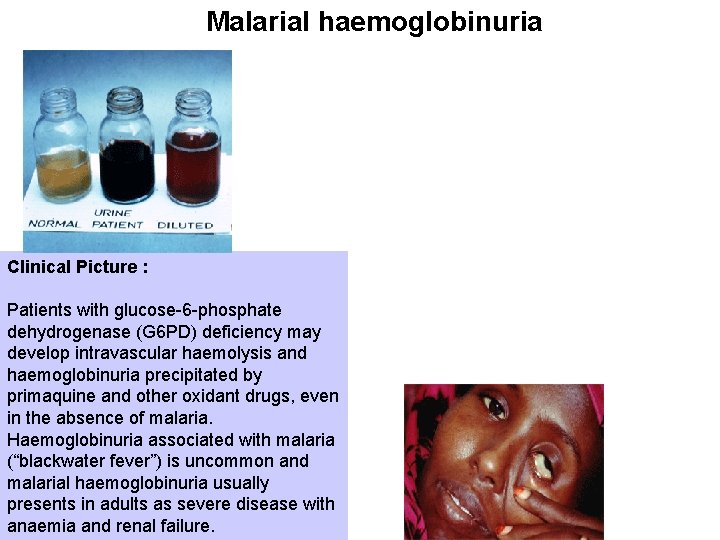
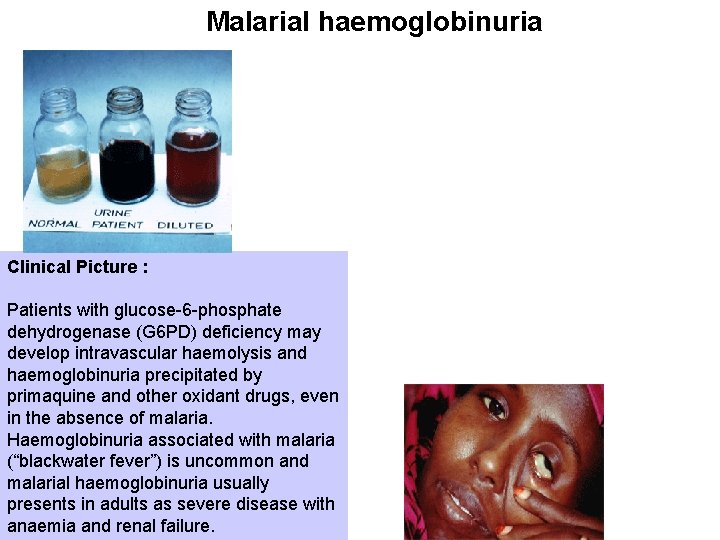
Malarial haemoglobinuria Clinical Picture : Patients with glucose-6 -phosphate dehydrogenase (G 6 PD) deficiency may develop intravascular haemolysis and haemoglobinuria precipitated by primaquine and other oxidant drugs, even in the absence of malaria. Haemoglobinuria associated with malaria (“blackwater fever”) is uncommon and malarial haemoglobinuria usually presents in adults as severe disease with anaemia and renal failure.
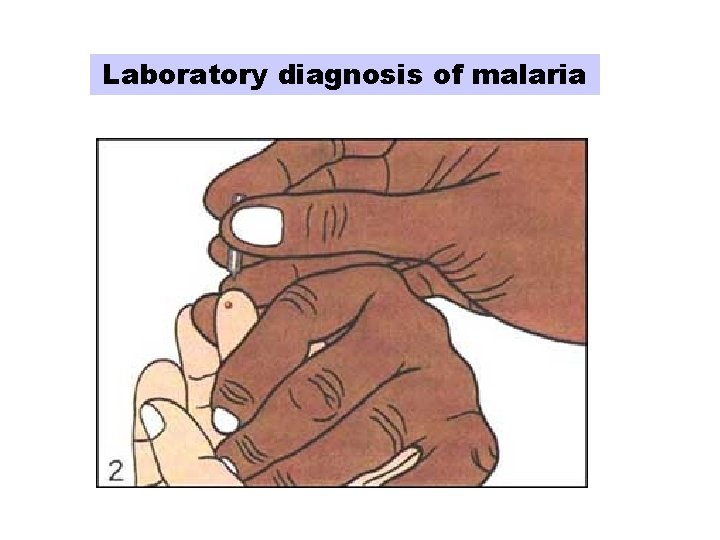
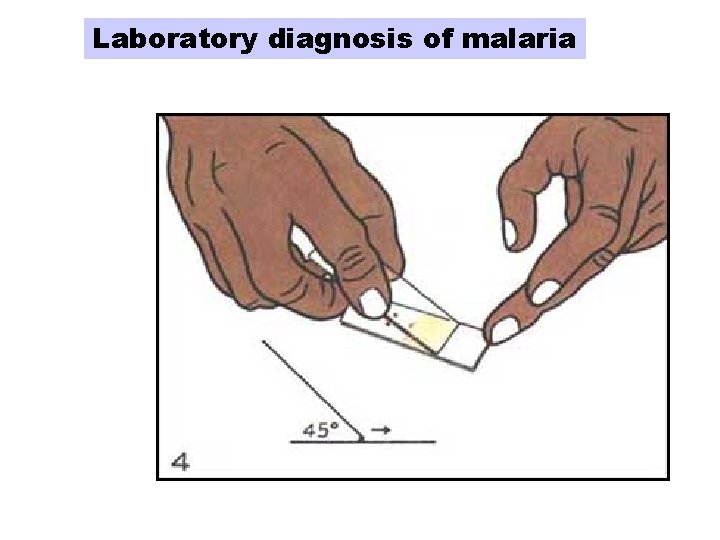
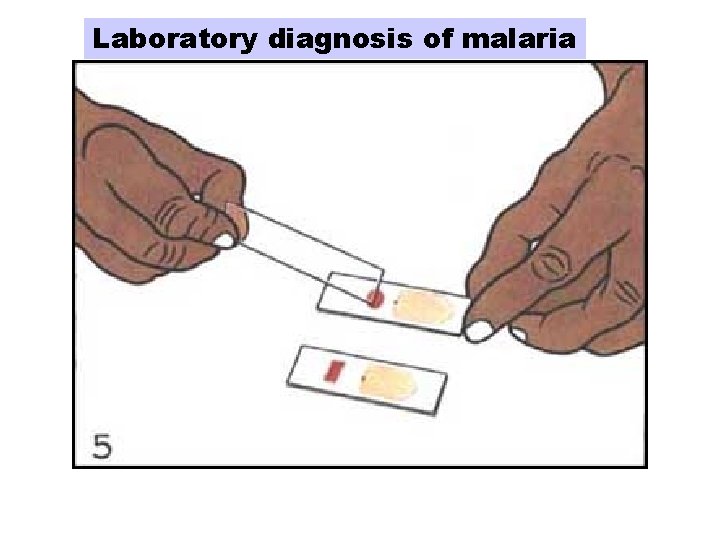
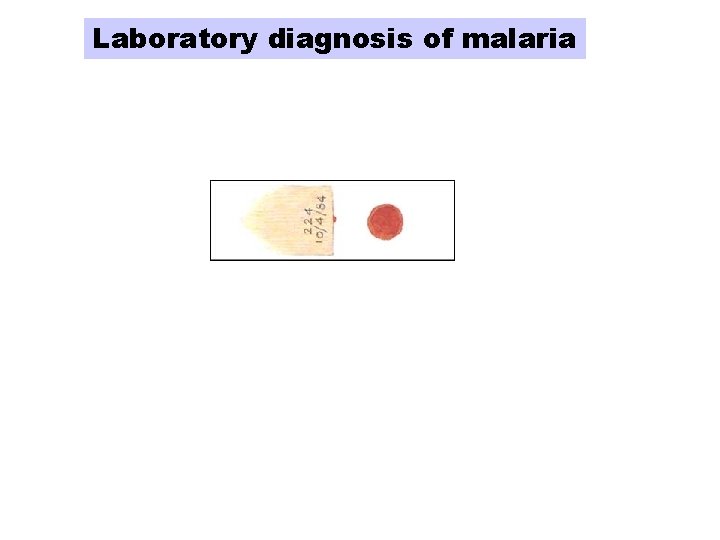
Laboratory diagnosis of malaria
Laboratory diagnosis of malaria
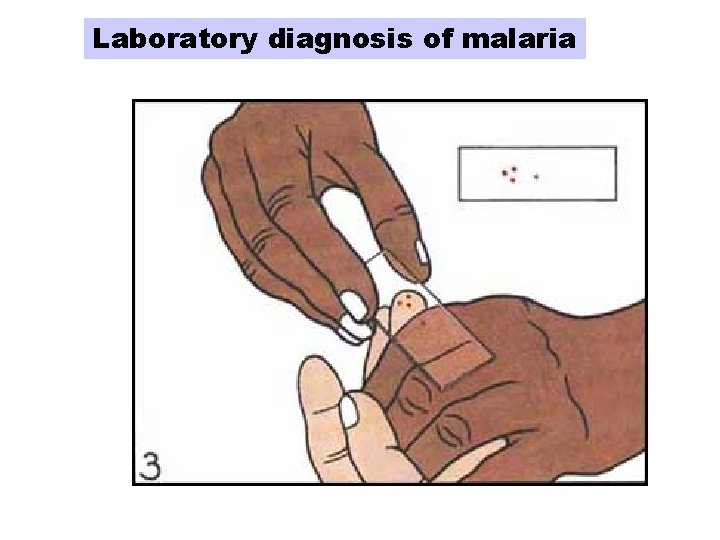
Laboratory diagnosis of malaria
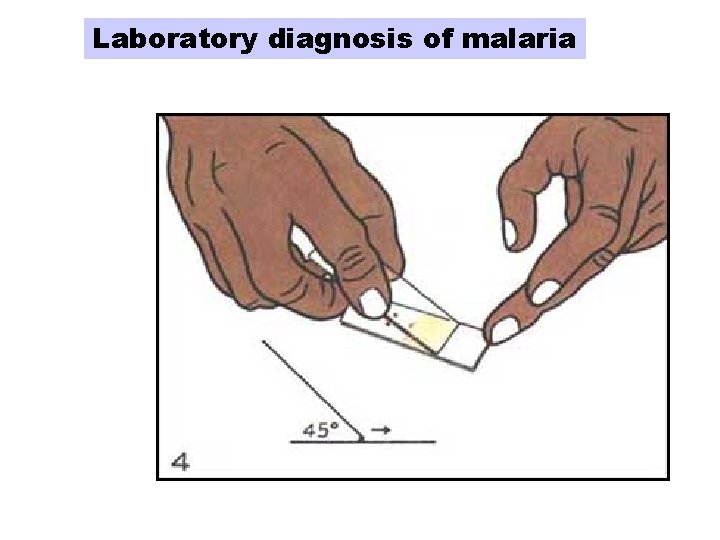
Laboratory diagnosis of malaria
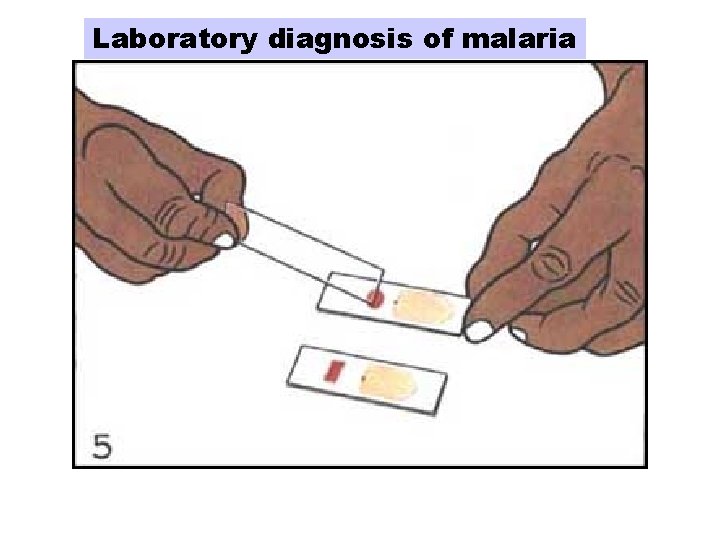
Laboratory diagnosis of malaria

Laboratory diagnosis of malaria
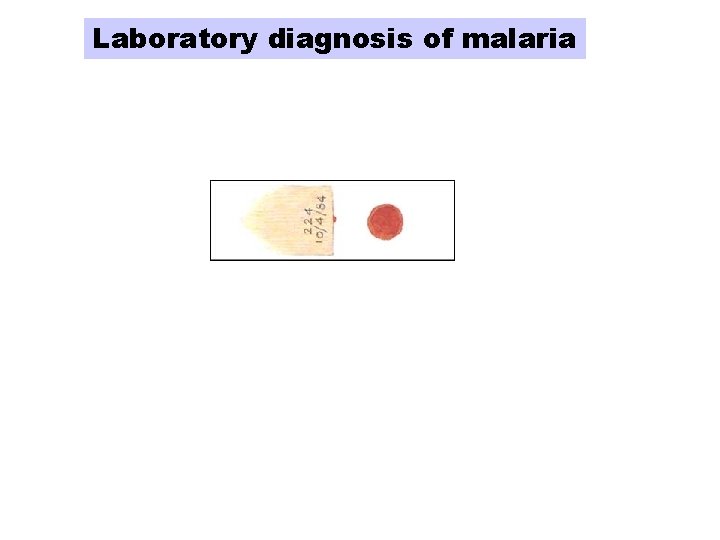
Laboratory diagnosis of malaria
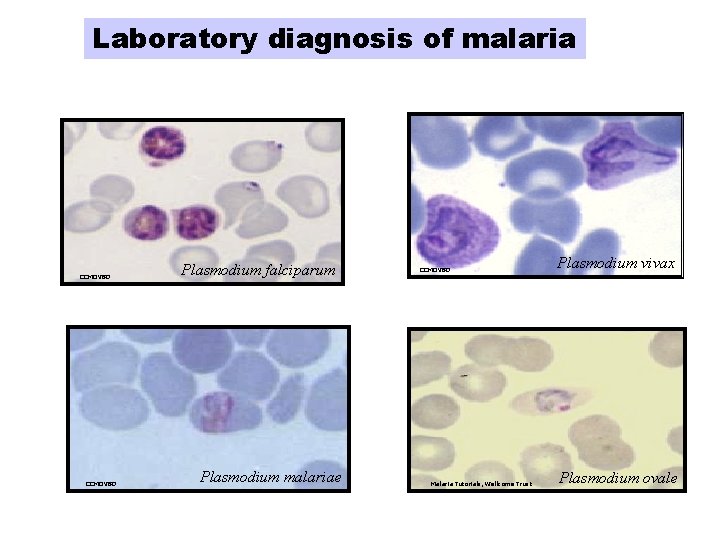
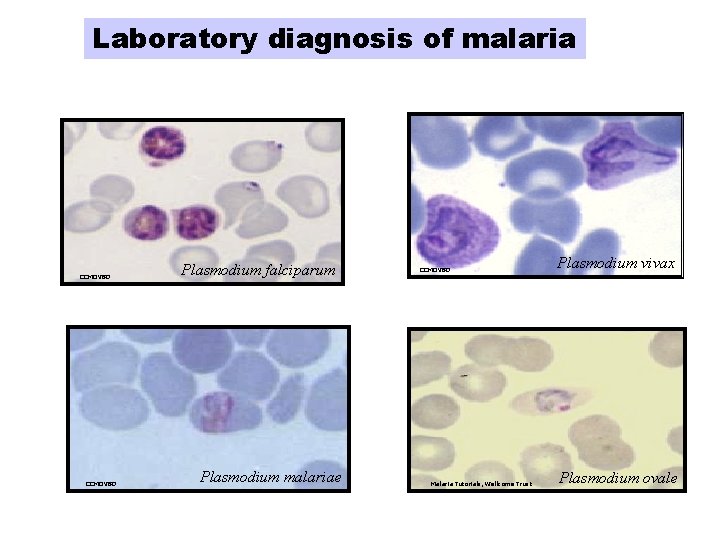
Laboratory diagnosis of malaria CCMOVBD Plasmodium falciparum Plasmodium malariae CCMOVBD Malaria Tutorials, Wellcome Trust Plasmodium vivax Plasmodium ovale
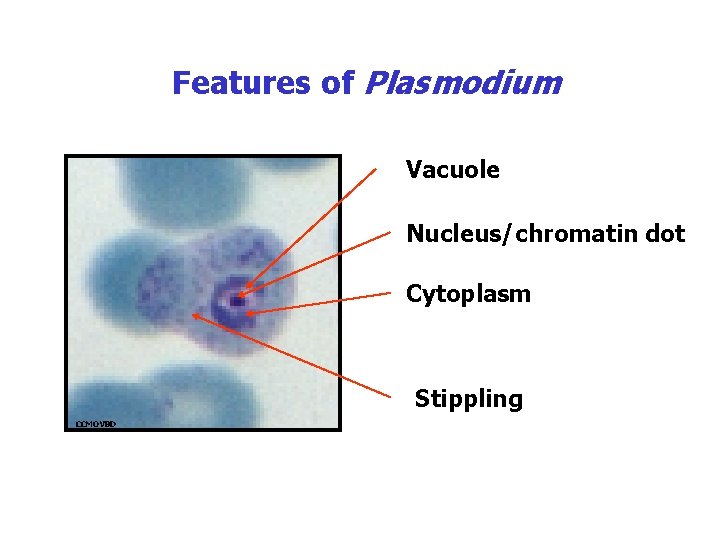
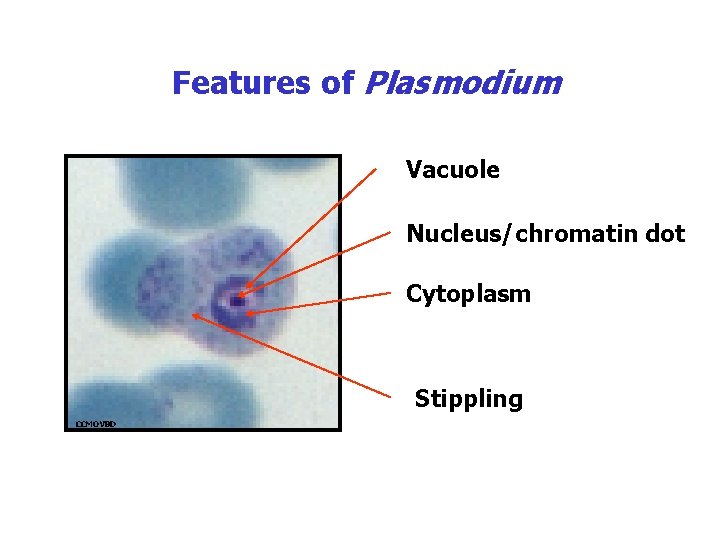
Features of Plasmodium Vacuole Nucleus/chromatin dot Cytoplasm Stippling CCMOVBD
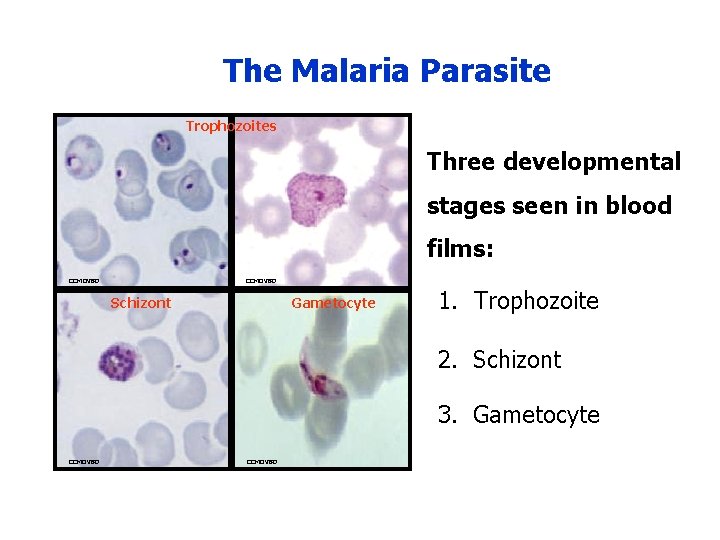
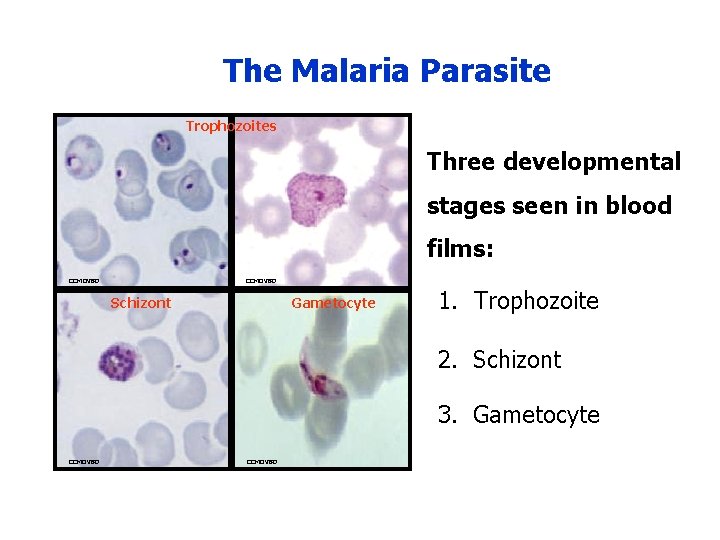
The Malaria Parasite Trophozoites Three developmental stages seen in blood films: CCMOVBD Schizont Gametocyte 1. Trophozoite 2. Schizont 3. Gametocyte CCMOVBD
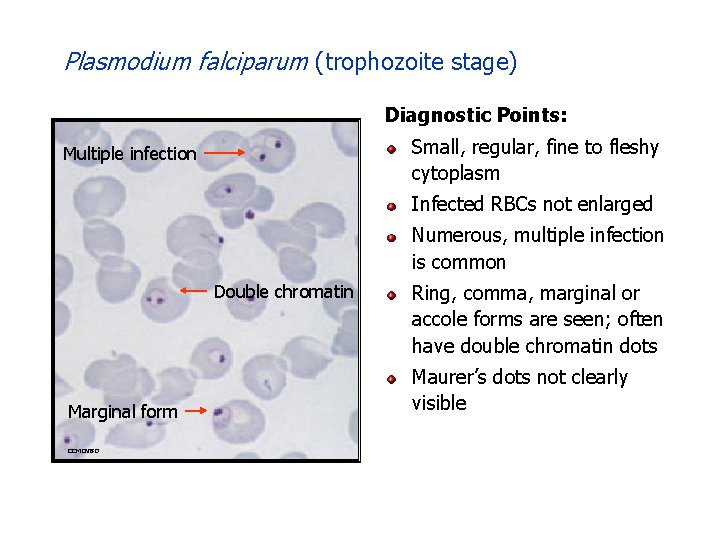
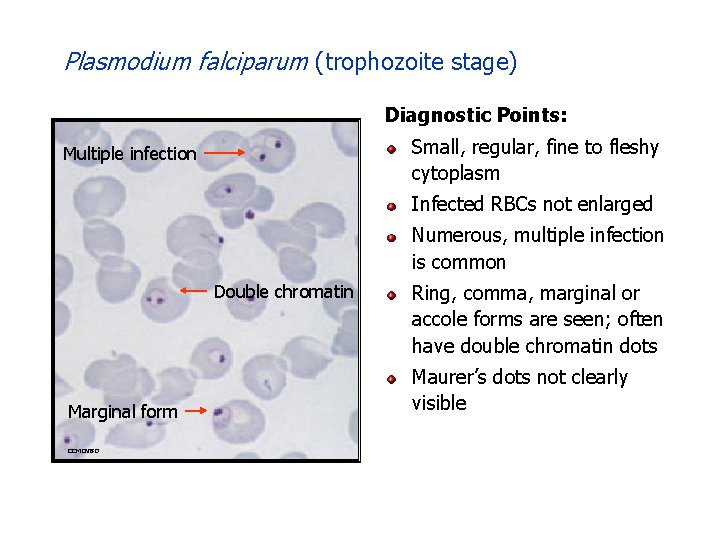
Plasmodium falciparum (trophozoite stage) Diagnostic Points: Small, regular, fine to fleshy cytoplasm Multiple infection Infected RBCs not enlarged Numerous, multiple infection is common Double chromatin Marginal form CCMOVBD Ring, comma, marginal or accole forms are seen; often have double chromatin dots Maurer’s dots not clearly visible
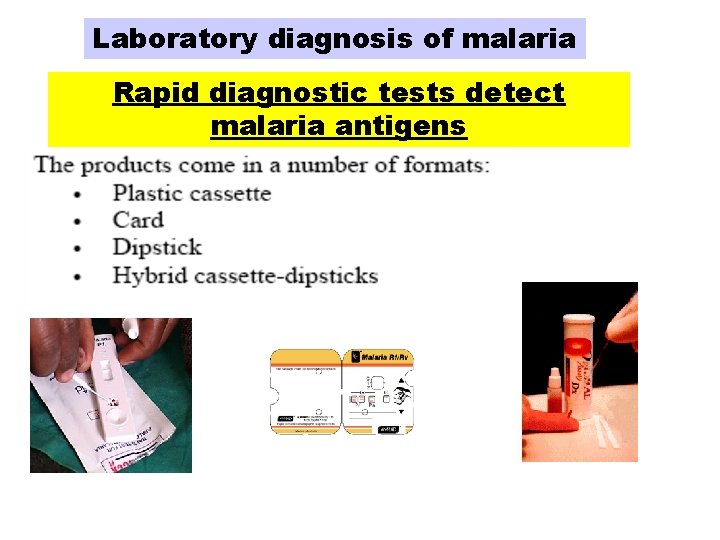
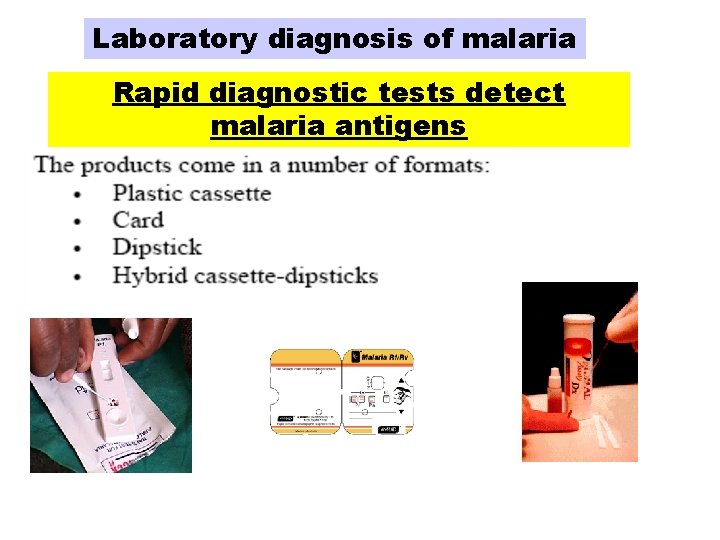
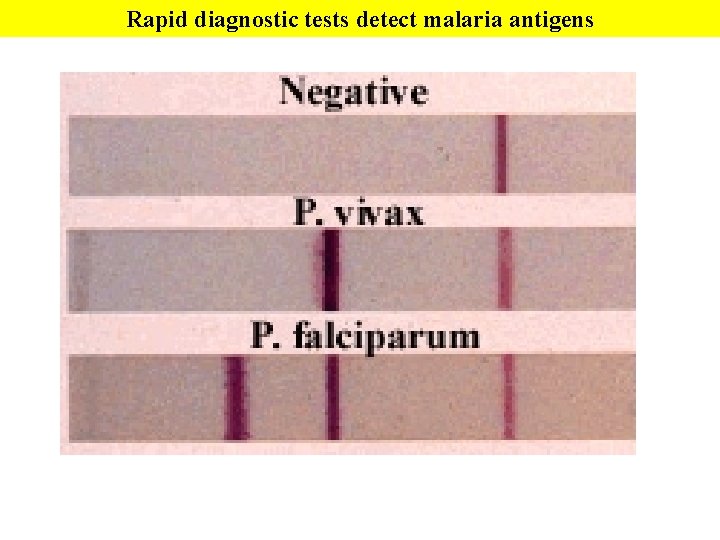
Laboratory diagnosis of malaria Rapid diagnostic tests detect malaria antigens
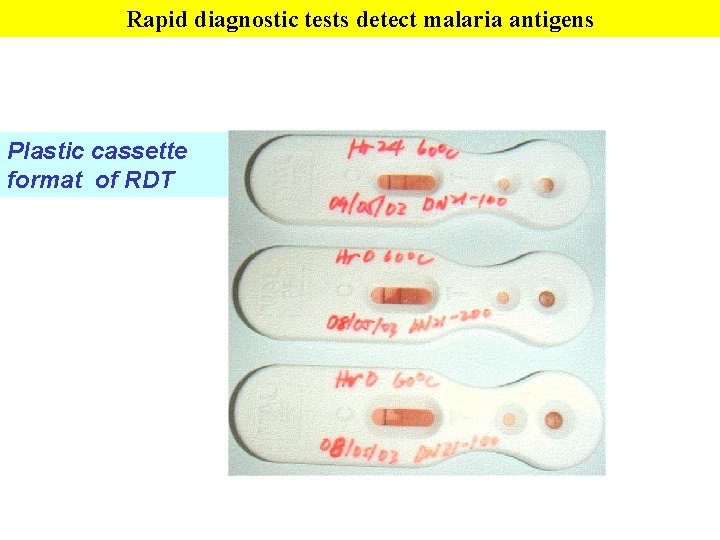
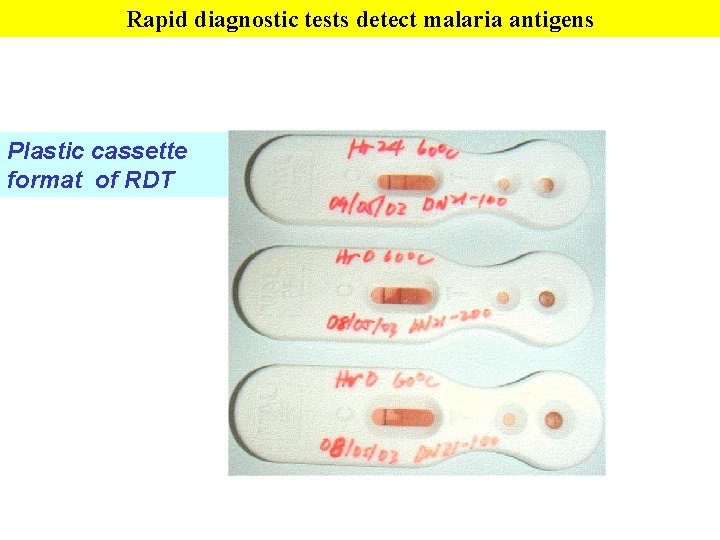
Rapid diagnostic tests detect malaria antigens Plastic cassette format of RDT
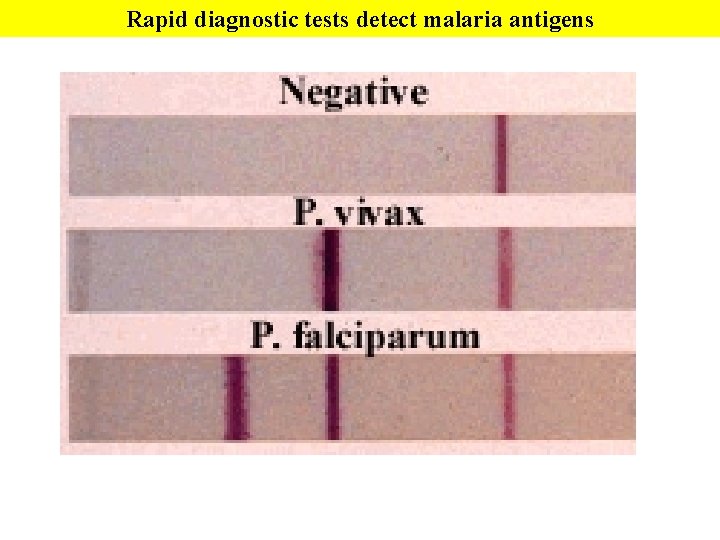
Rapid diagnostic tests detect malaria antigens
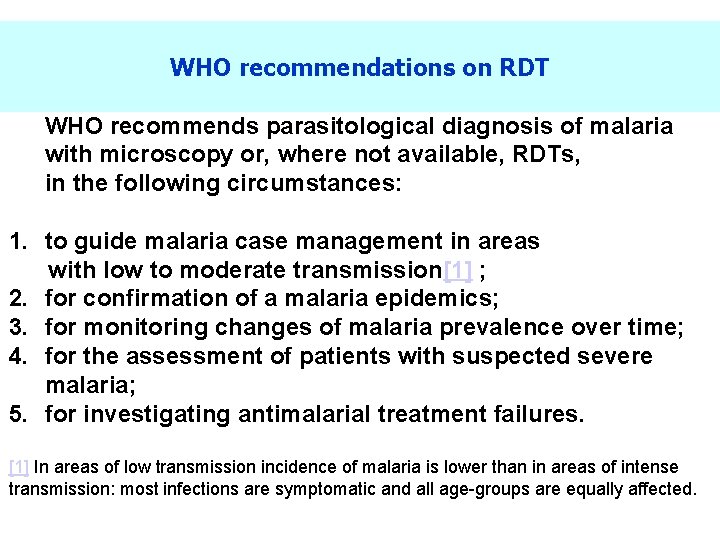
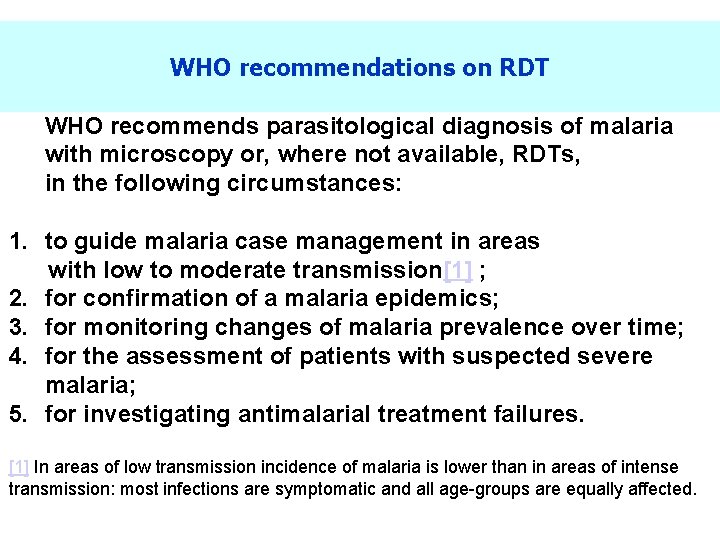
WHO recommendations on RDT WHO recommends parasitological diagnosis of malaria with microscopy or, where not available, RDTs, in the following circumstances: 1. to guide malaria case management in areas with low to moderate transmission[1] ; 2. for confirmation of a malaria epidemics; 3. for monitoring changes of malaria prevalence over time; 4. for the assessment of patients with suspected severe malaria; 5. for investigating antimalarial treatment failures. [1] In areas of low transmission incidence of malaria is lower than in areas of intense transmission: most infections are symptomatic and all age-groups are equally affected.
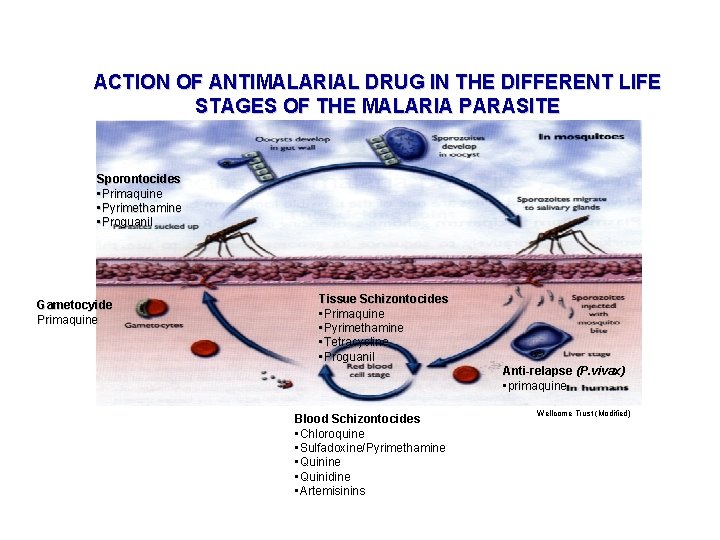
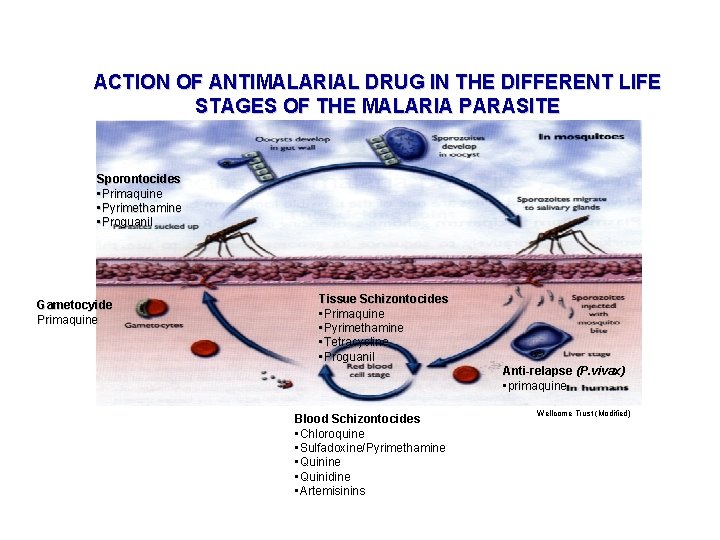
ACTION OF ANTIMALARIAL DRUG IN THE DIFFERENT LIFE STAGES OF THE MALARIA PARASITE Sporontocides • Primaquine • Pyrimethamine • Proguanil Gametocyide Primaquine Tissue Schizontocides • Primaquine • Pyrimethamine • Tetracycline • Proguanil Anti-relapse (P. vivax) • primaquine Blood Schizontocides • Chloroquine • Sulfadoxine/Pyrimethamine • Quinidine • Artemisinins Wellcome Trust (Modified)