Major Histocompatibility Complex MHC What is MHC HLA
Major Histocompatibility Complex (MHC) Ø What is MHC? – – – HLA H-2 Minor histocompatibility antigens 1
Significance of the MHC role in immune response Ø role in organ transplantation Ø role in predisposition to disease Ø 2

DEFINITIONS: Histocompatibility (transplantation) antigens: Antigens on tissues and cells that determine their rejection when grafted between two genetically different individuals Major histocompatibility (MHC) antigens: Histocompatibility antigens that cause a very strong immune response and are most important in rejection MHC complex: Group of genes on a single chromosome encoding the MHC antigens HLA (human leukocyte antigens): MHC antigens of man (first detected on leukocytes) H-2 antigens: MHC antigens of mouse
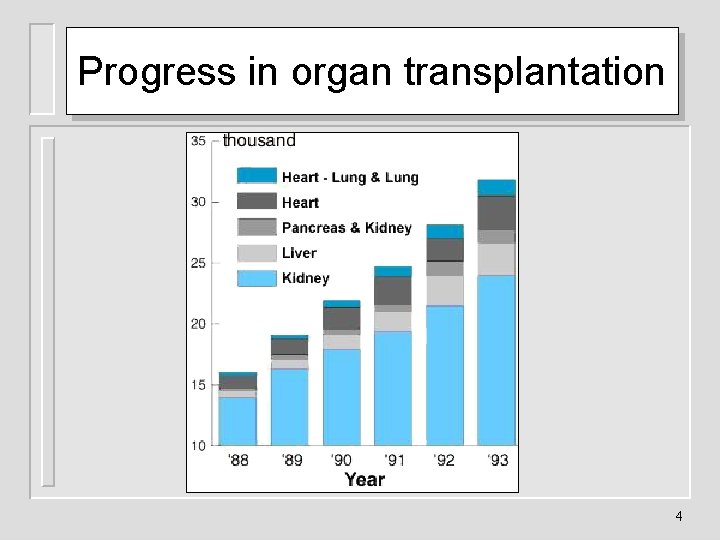
Progress in organ transplantation 4
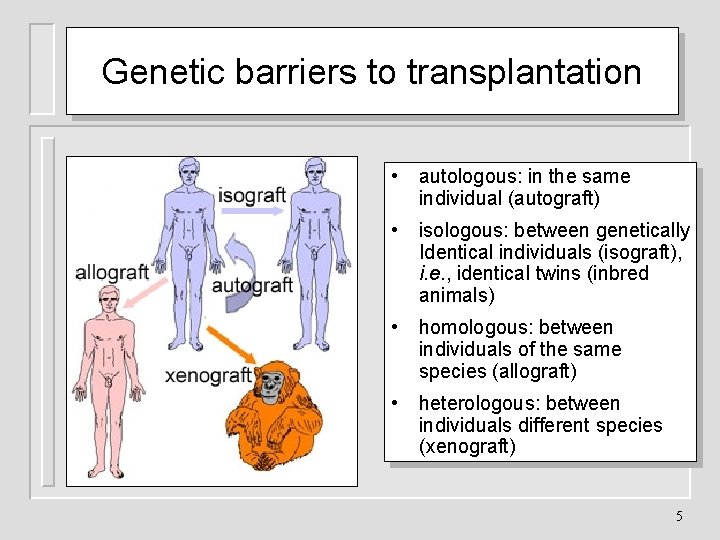
Genetic barriers to transplantation • autologous: in the same individual (autograft) • isologous: between genetically Identical individuals (isograft), i. e. , identical twins (inbred animals) • homologous: between individuals of the same species (allograft) • heterologous: between individuals different species (xenograft) 5
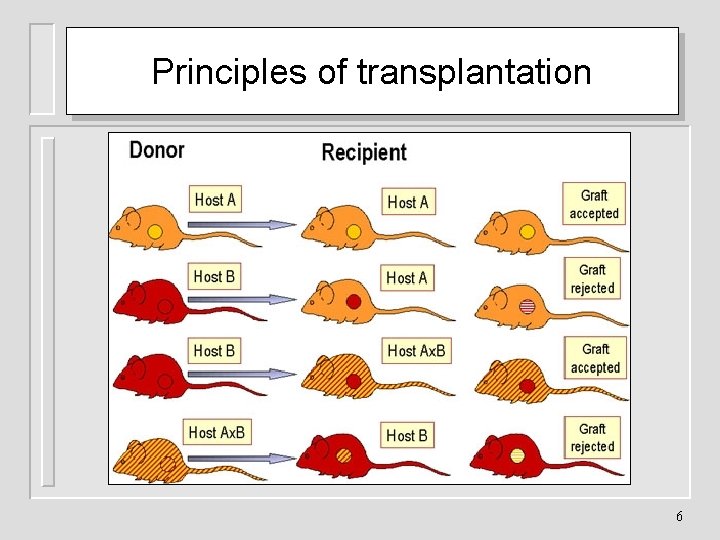
Principles of transplantation 6
Minor histocompatibility antigens and graft survival Ø minor histocompatibility antigens also cause rejection Ø The rejection time is variable but longer than that for major histocompatibility antigen Ø They have additive effects 7
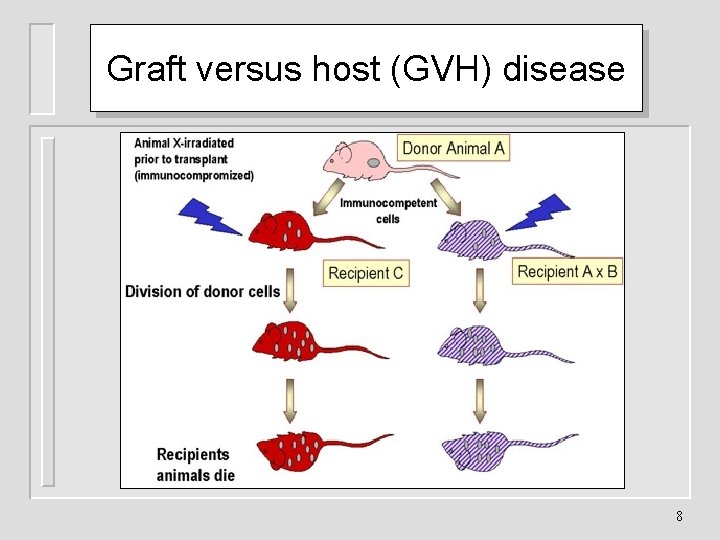
Graft versus host (GVH) disease 8

GVH disease in humans 9
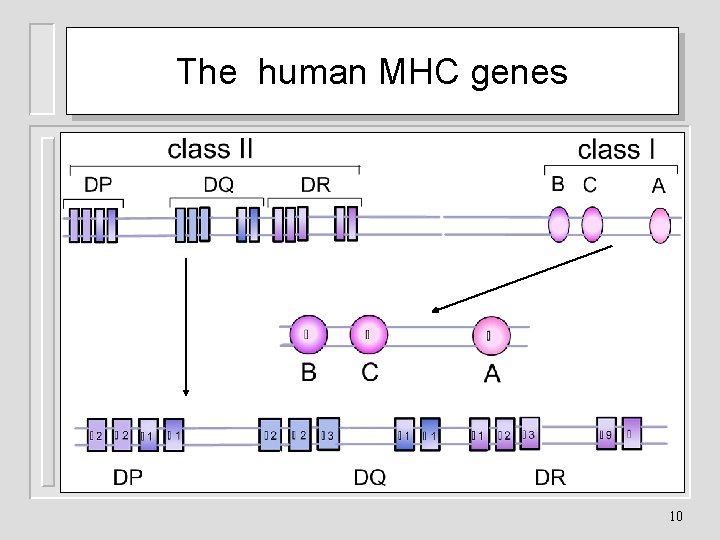
The human MHC genes 10
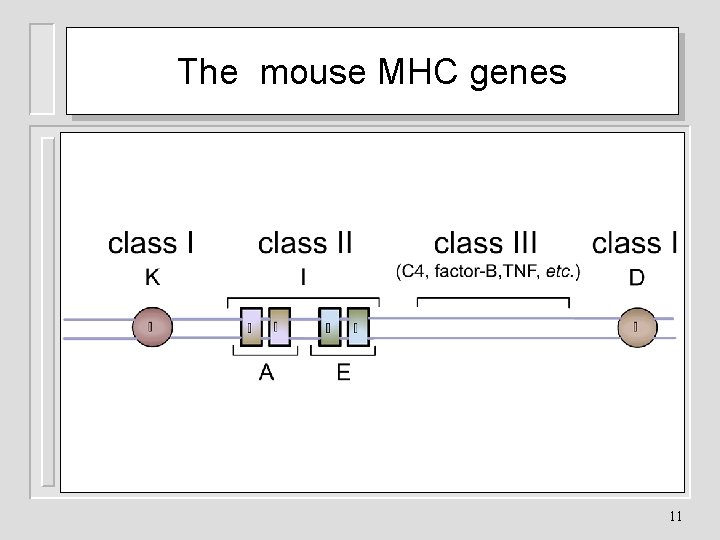
The mouse MHC genes 11
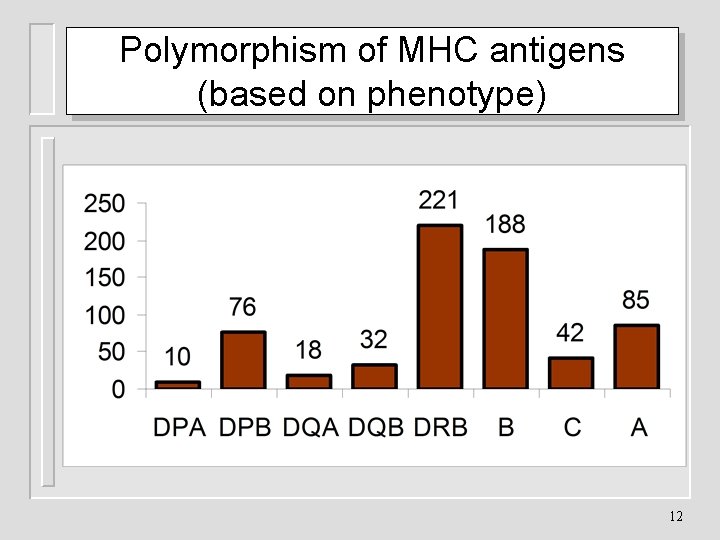
Polymorphism of MHC antigens (based on phenotype) 12
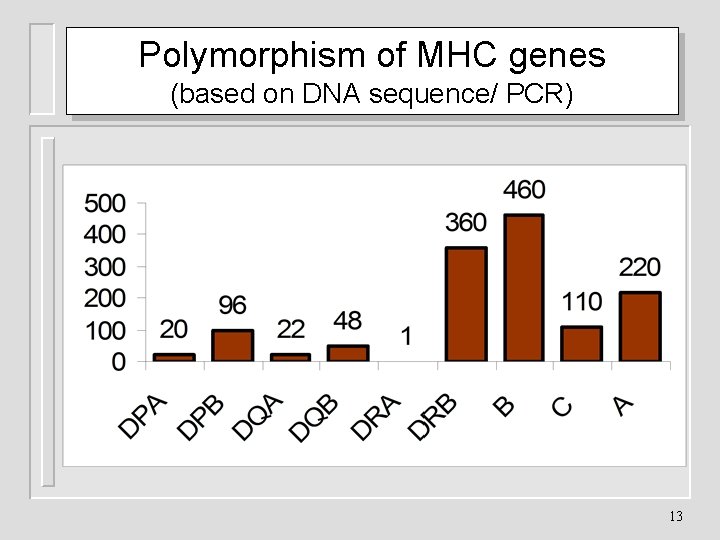
Polymorphism of MHC genes (based on DNA sequence/ PCR) 13
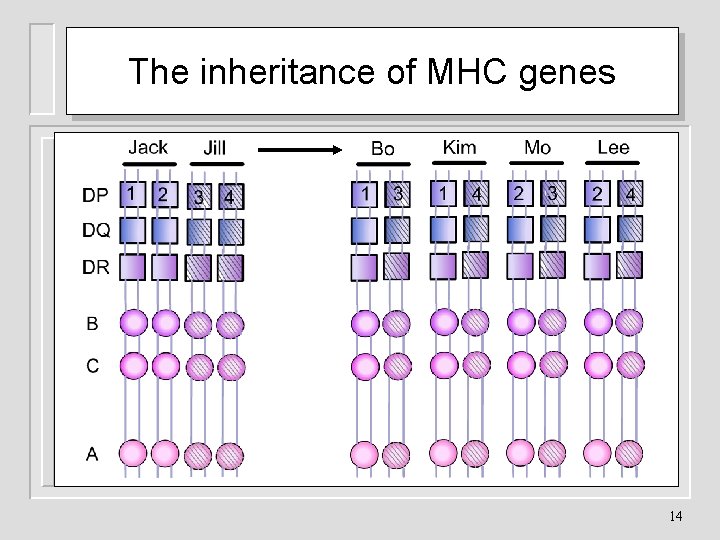
The inheritance of MHC genes 14
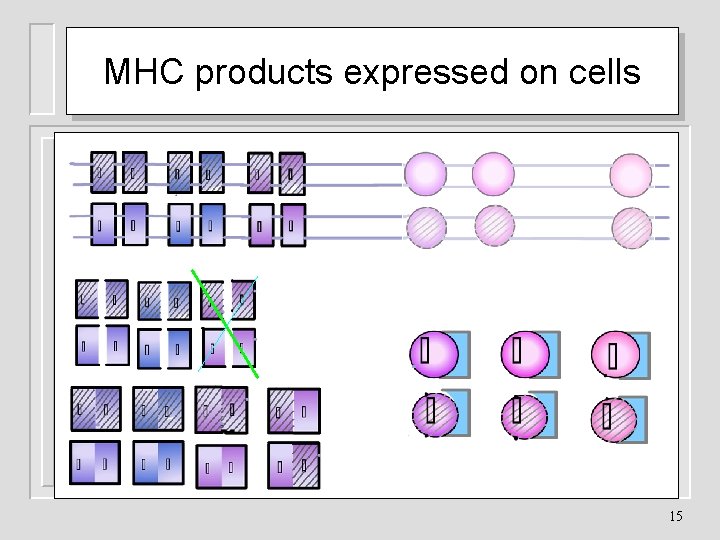
MHC products expressed on cells 15
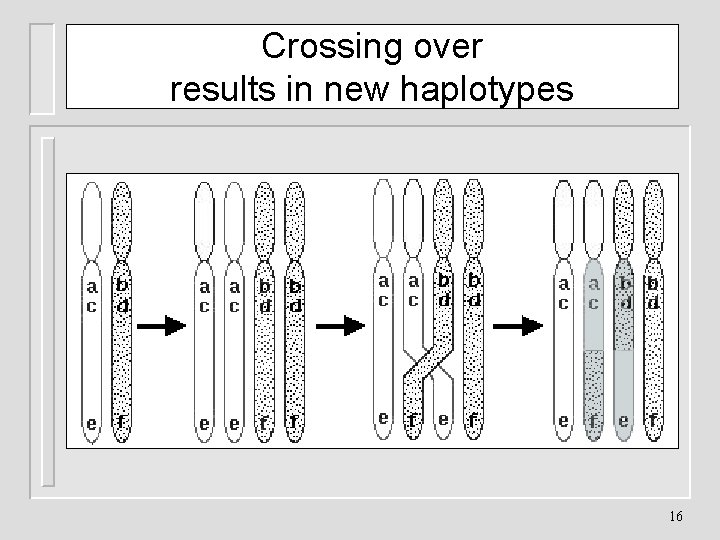
Crossing over results in new haplotypes 16
MHC products expressed on cells If Jack and Jill have four children; Bo, Kim, Mo and Lee They’ll all inherit antigens of the parental MHC Oft their haplotypes will be of the father or mother Unless during meiosis, a crossover should occur 17
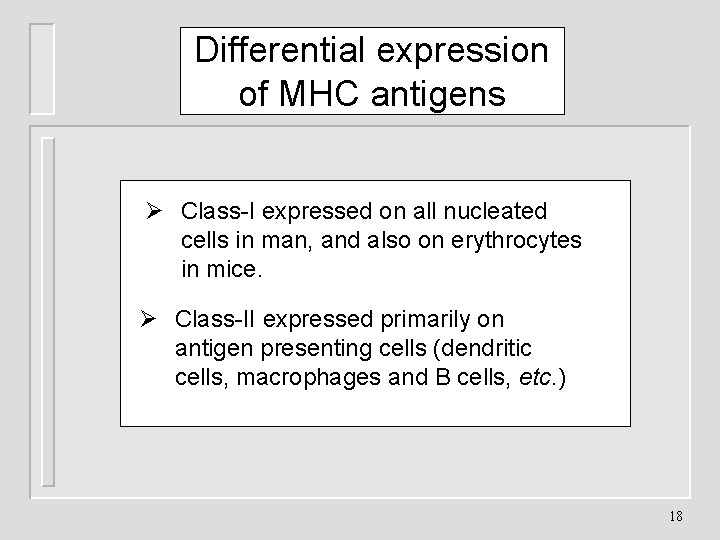
Differential expression of MHC antigens Ø Class-I expressed on all nucleated cells in man, and also on erythrocytes in mice. Ø Class-II expressed primarily on antigen presenting cells (dendritic cells, macrophages and B cells, etc. ) 18
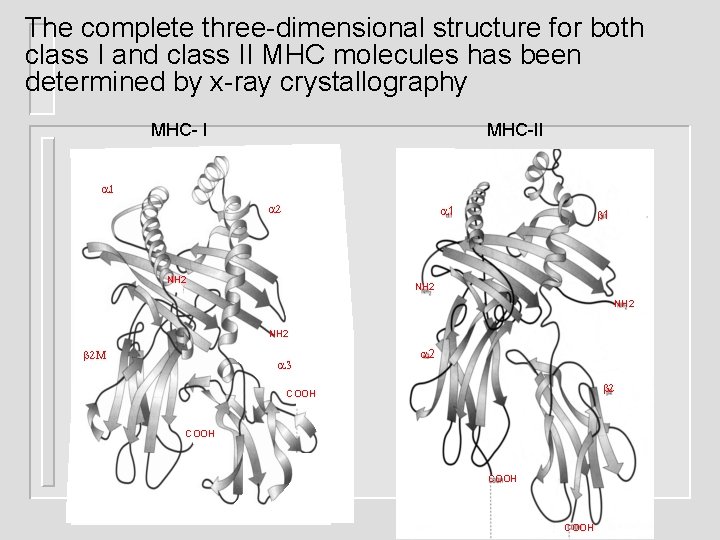
The complete three-dimensional structure for both class I and class II MHC molecules has been determined by x-ray crystallography MHC- I MHC-II 1 2 1 NH 2 2 M 3 2 2 COOH
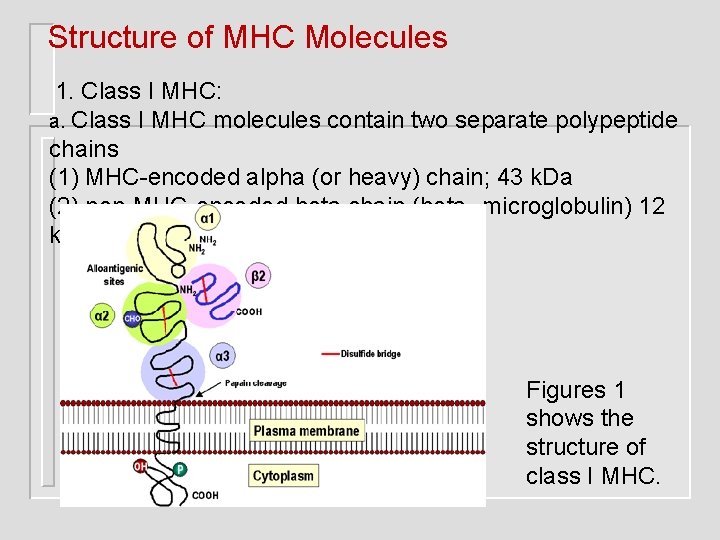
Structure of MHC Molecules 1. Class I MHC: a. Class I MHC molecules contain two separate polypeptide chains (1) MHC-encoded alpha (or heavy) chain; 43 k. Da (2) non-MHC-encoded beta chain (beta 2 microglobulin) 12 k. Da Figures 1 shows the structure of class I MHC.
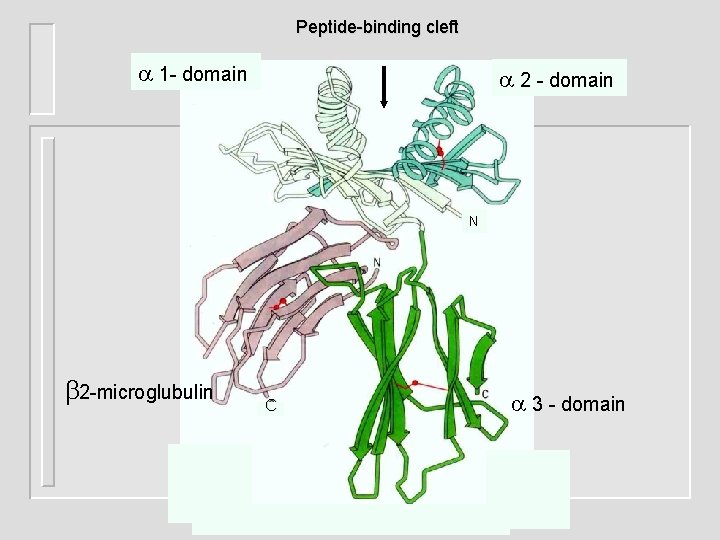
Peptide-binding cleft 1 - domain 2 - domain N 2 -microglubulin C 3 - domain
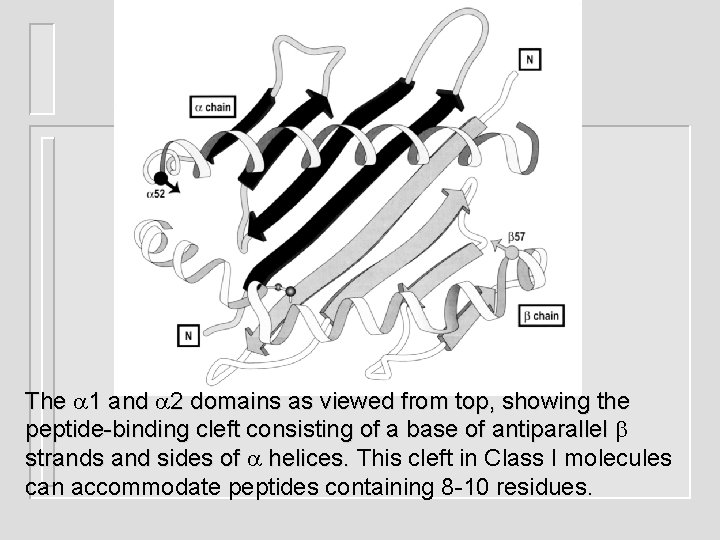
The 1 and 2 domains as viewed from top, showing the peptide-binding cleft consisting of a base of antiparallel strands and sides of helices. This cleft in Class I molecules helices. can accommodate peptides containing 8 -10 residues.
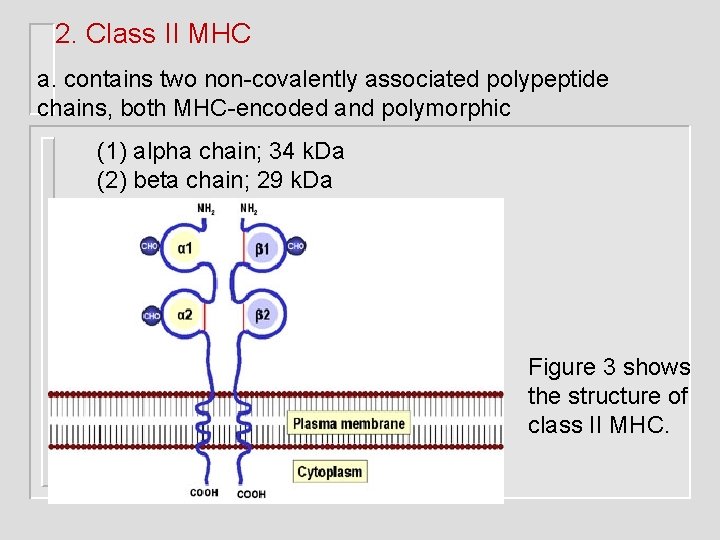
2. Class II MHC a. contains two non-covalently associated polypeptide chains, both MHC-encoded and polymorphic (1) alpha chain; 34 k. Da (2) beta chain; 29 k. Da Figure 3 shows the structure of class II MHC.
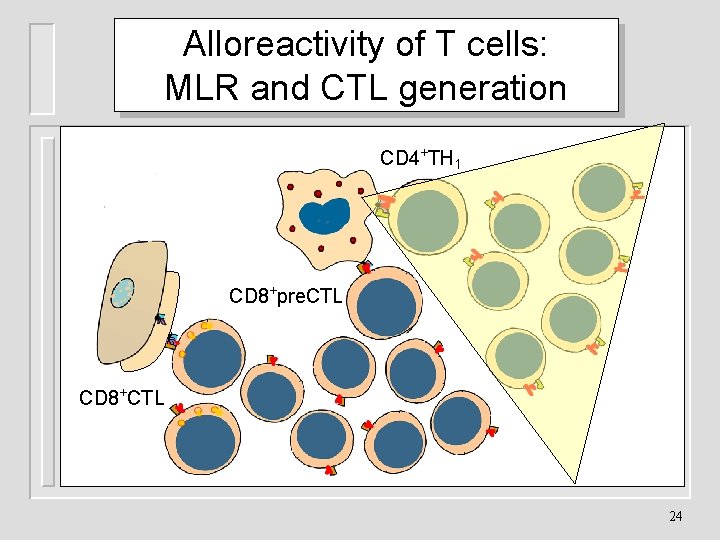
Alloreactivity of T cells: MLR and CTL generation CD 4+TH 1 CD 8+pre. CTL CD 8+CTL 24
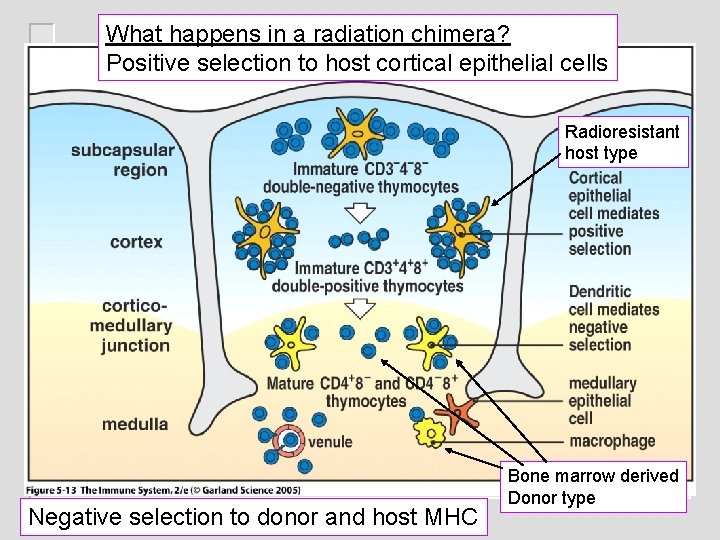
What happens in a radiation chimera? Positive selection to host cortical epithelial cells Figure 5 -13 Radioresistant host type Negative selection to donor and host MHC Bone marrow derived Donor type
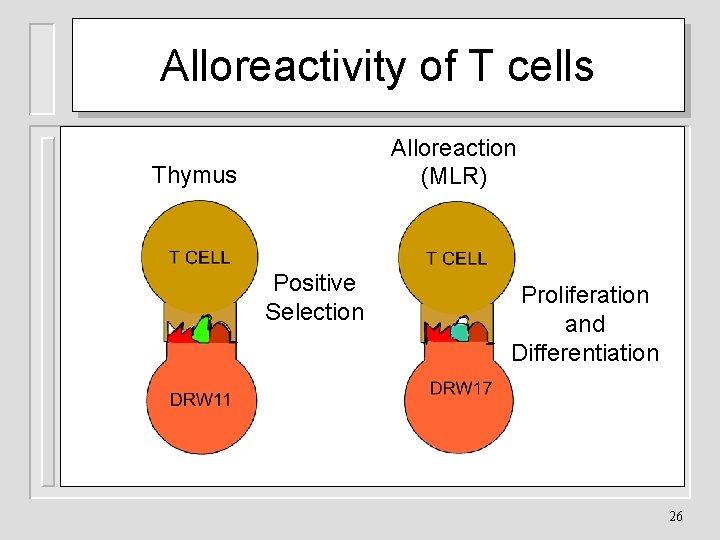
Alloreactivity of T cells Alloreaction (MLR) Thymus Positive Selection Proliferation and Differentiation 26

Mechanisms of graft rejection IL 2, TNF , IFN TNF , NO 2 Inflammation IL 2, IL 4, IL 5 IL 2, IFN lysis ADCC lysis rejection 27
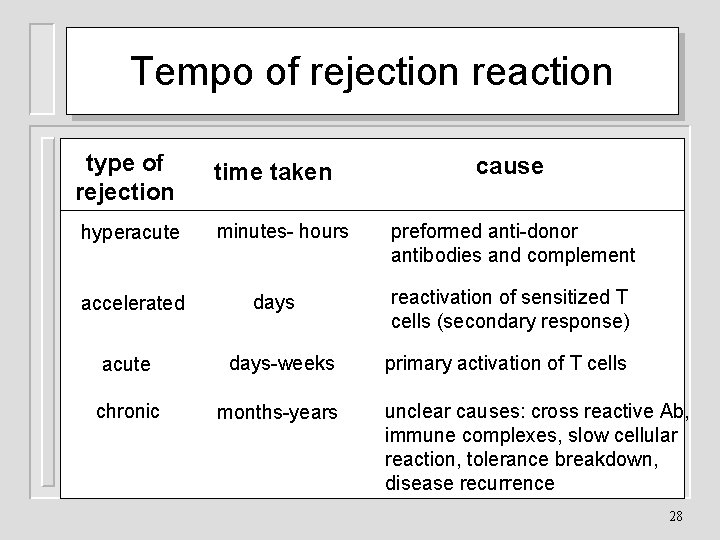
Tempo of rejection reaction type of rejection hyperacute accelerated time taken minutes- hours days acute days-weeks chronic months-years cause preformed anti-donor antibodies and complement reactivation of sensitized T cells (secondary response) primary activation of T cells unclear causes: cross reactive Ab, immune complexes, slow cellular reaction, tolerance breakdown, disease recurrence 28
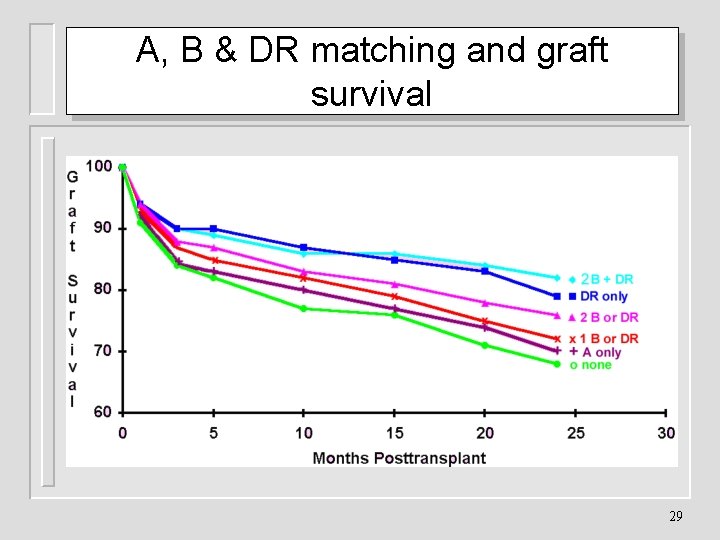
A, B & DR matching and graft survival 29
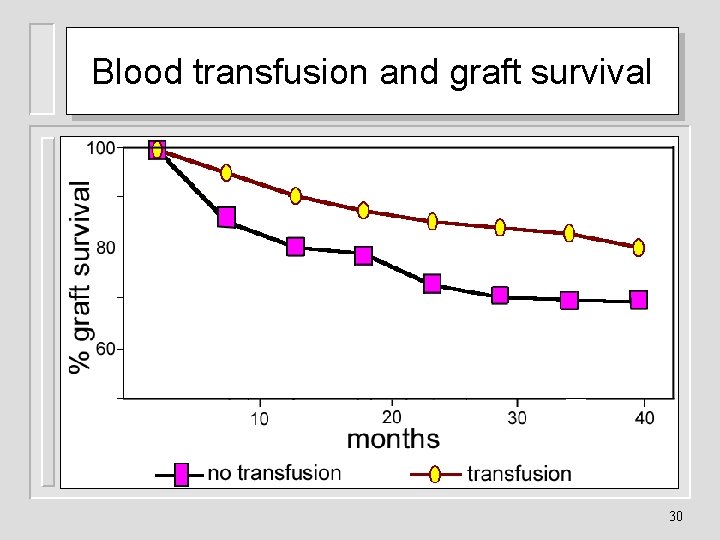
Blood transfusion and graft survival 30
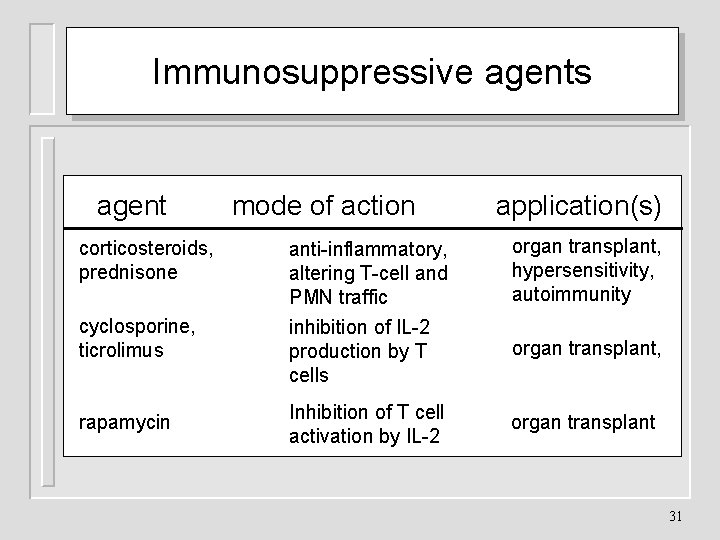
Immunosuppressive agents agent corticosteroids, prednisone cyclosporine, ticrolimus rapamycin mode of action application(s) anti-inflammatory, altering T-cell and PMN traffic inhibition of IL-2 production by T cells organ transplant, hypersensitivity, autoimmunity Inhibition of T cell activation by IL-2 organ transplant, 31
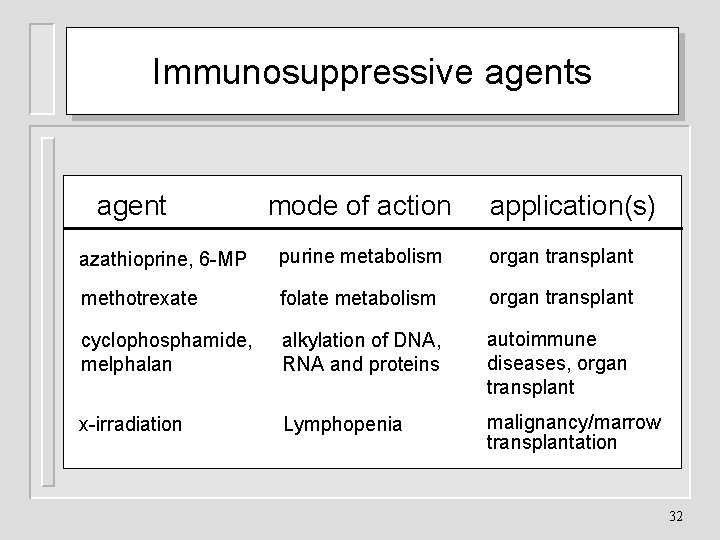
Immunosuppressive agents agent mode of action application(s) azathioprine, 6 -MP purine metabolism organ transplant methotrexate folate metabolism organ transplant cyclophosphamide, melphalan alkylation of DNA, RNA and proteins autoimmune diseases, organ transplant x-irradiation Lymphopenia malignancy/marrow transplantation 32
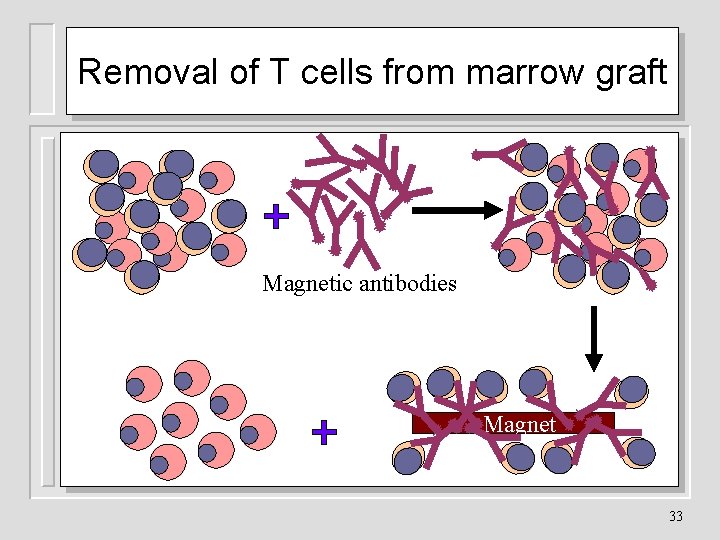
Removal of T cells from marrow graft Magnetic antibodies Magnet 33
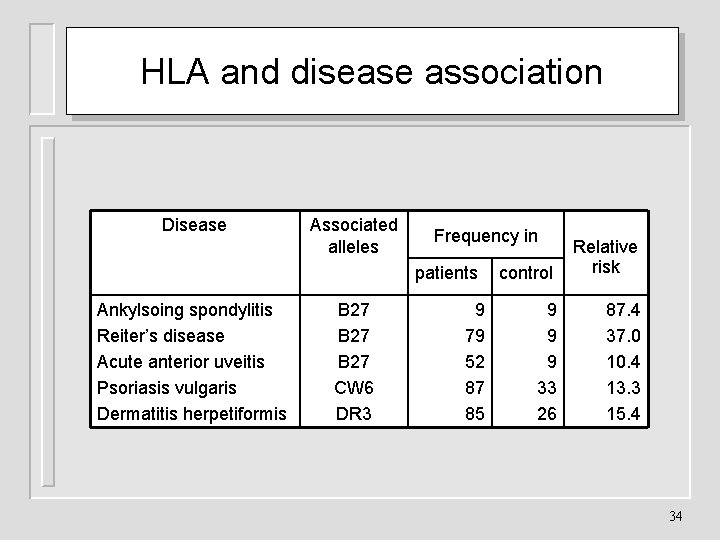
HLA and disease association Disease Associated alleles Frequency in patients Ankylsoing spondylitis Reiter’s disease Acute anterior uveitis Psoriasis vulgaris Dermatitis herpetiformis B 27 CW 6 DR 3 9 79 52 87 85 control Relative risk 9 9 9 33 26 87. 4 37. 0 10. 4 13. 3 15. 4 34
- Slides: 34