Major Case Study Heart Failure and Left Ventricular


- Slides: 35
Major Case Study: Heart Failure and Left Ventricular Assistive Device as a Destination Therapy January th 29 , 2013 By: Rachael Woods; dietetic intern By: Rachael Woods: Dietetic Intern S
Purpose of the Study S Case was intriguing S Nutritional implications for left ventricular assistive devices (LVAD) are not well known among RD’s
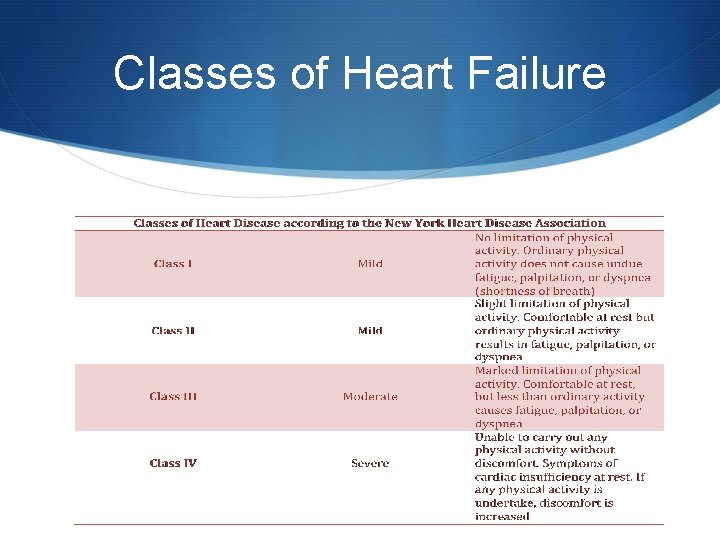
About A. S. S 71 y/o retired Caucasian male S Catholic S 113. 90 kg (250. 6 lb) S 182. 88 cm (72 in) S BMI: 36. 1 S IBW: 80. 9 kg S %IBW: 141% S Admitted with Heart Failure class III Stage IV (D) for LVAD placement
A. S. ’s Past Medical History S Congestive heart failure (heart failure) class III, stage IV (D) S Cardiomyopathy S Coronary artery disease S Chronic kidney disease S Throat and prostate cancer with radiation S Hypertension
PMH Continued S Gastritis S Atrial fibrillation S Right bundle branch block S Ischemic heart disease S History of myocardial infarction S Surgeries performed prior to admission: pacemaker placement and stented coronary artery
Heart Failure and it’s Causes S Occurs when the heart is unable to pump blood at the rate sufficient to meet the metabolic demands of the tissues or can only do so at an elevated filling pressure S 3 leading causes: coronary artery disease, high blood pressure and diabetes S Other causes: cardiomyopathy, heart valve disease, arrhythmias and congenital defects S A. S. ’s was caused by a myocardial infarction in the 1990’s
Nutrition History S Limits sodium and fat intake at home; does not follow a particular diet S Wife does grocery shopping and prepares meals S Meals are eaten at a dining room table where a television set is visible S Eat out 1 -2 x’s per week S Does not engage in physical activity regularly S Participated in Weight Watchers 1 year ago; lost 55 lbs
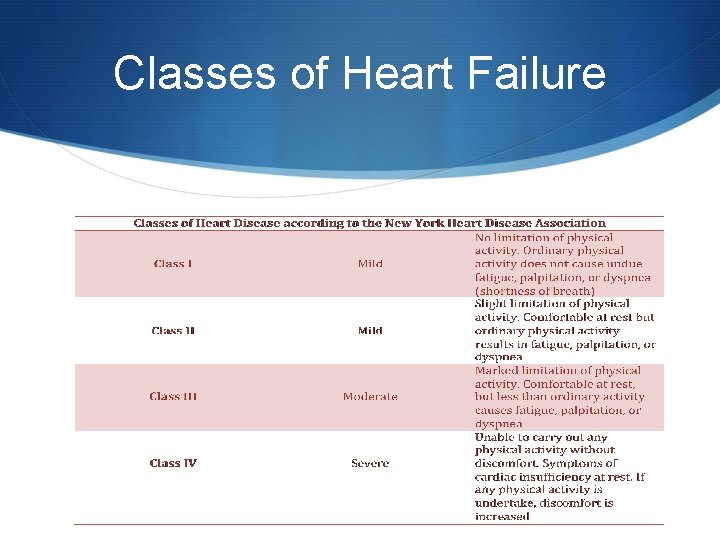
Classes of Heart Failure
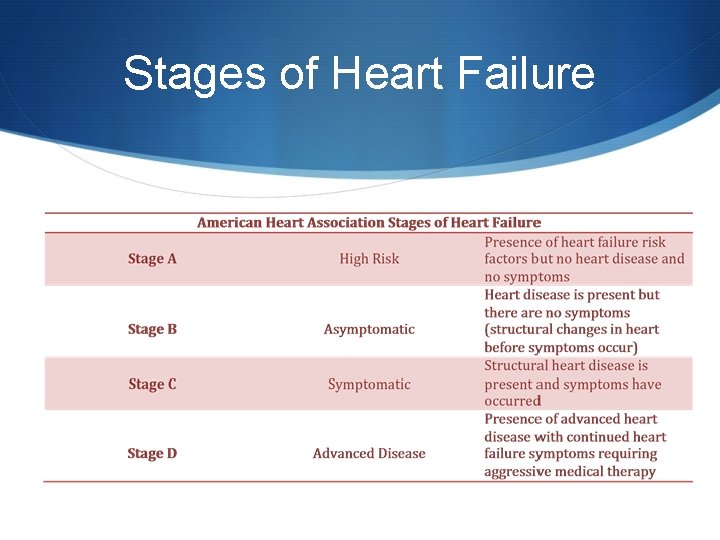
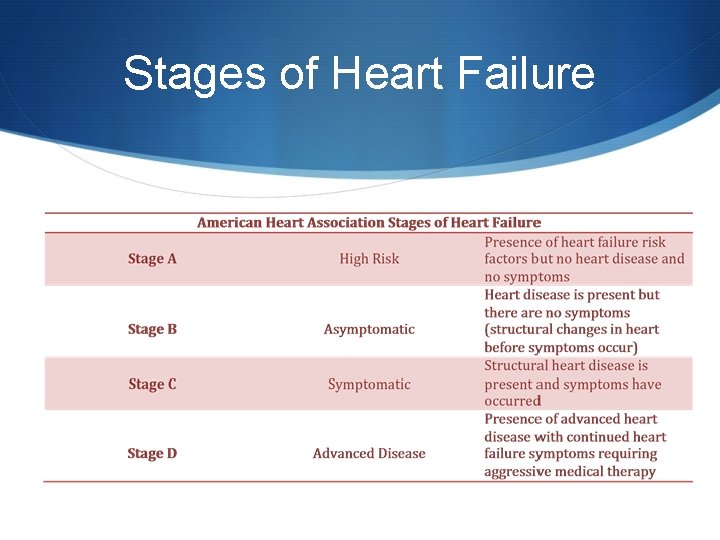
Stages of Heart Failure
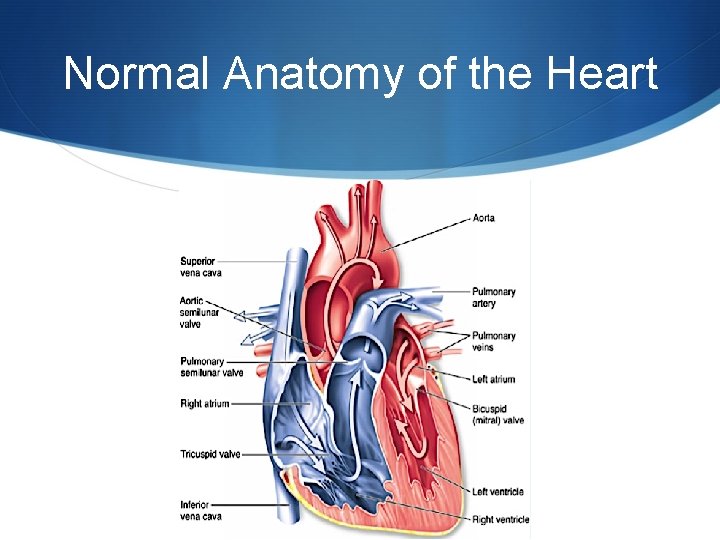
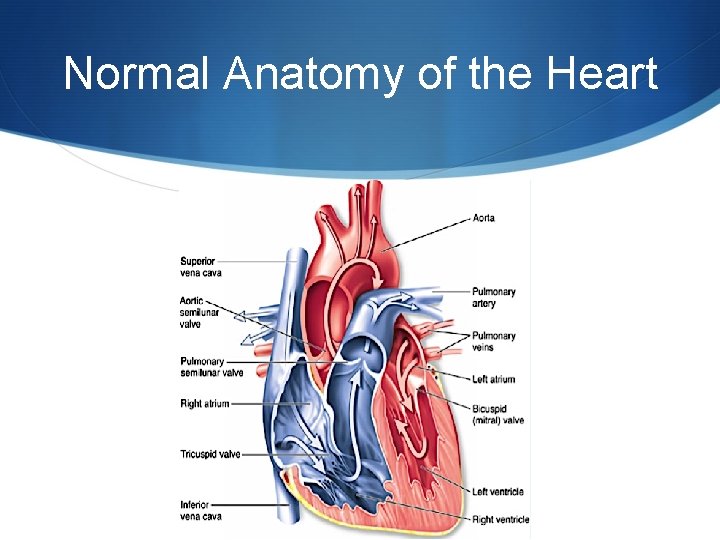
Normal Anatomy of the Heart
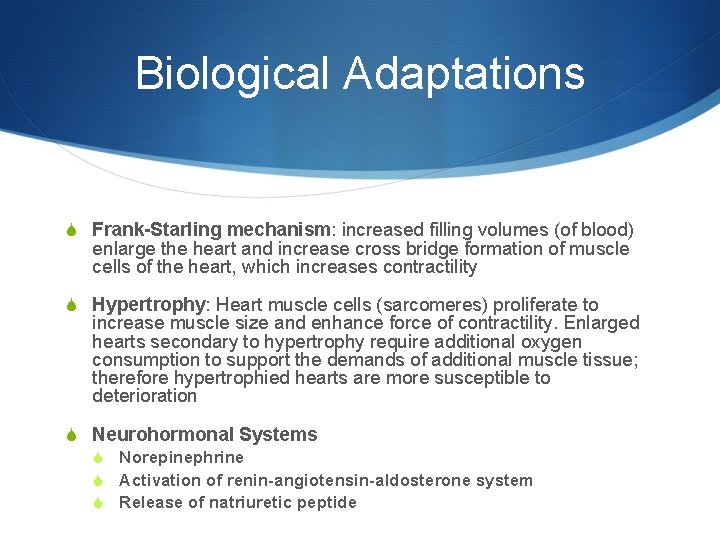
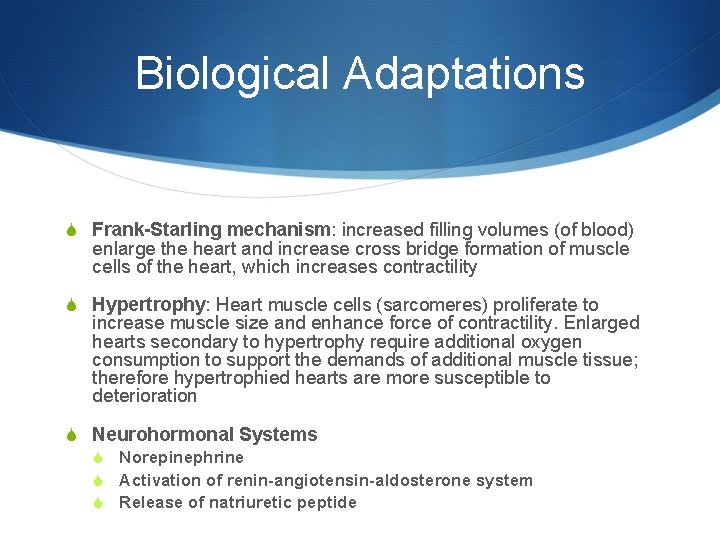
Biological Adaptations S Frank-Starling mechanism: increased filling volumes (of blood) enlarge the heart and increase cross bridge formation of muscle cells of the heart, which increases contractility S Hypertrophy: Heart muscle cells (sarcomeres) proliferate to increase muscle size and enhance force of contractility. Enlarged hearts secondary to hypertrophy require additional oxygen consumption to support the demands of additional muscle tissue; therefore hypertrophied hearts are more susceptible to deterioration S Neurohormonal Systems S Norepinephrine S Activation of renin-angiotensin-aldosterone system S Release of natriuretic peptide
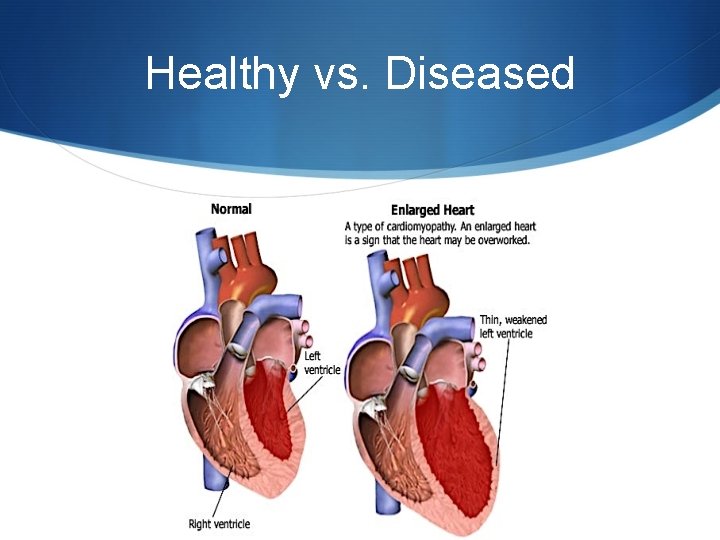
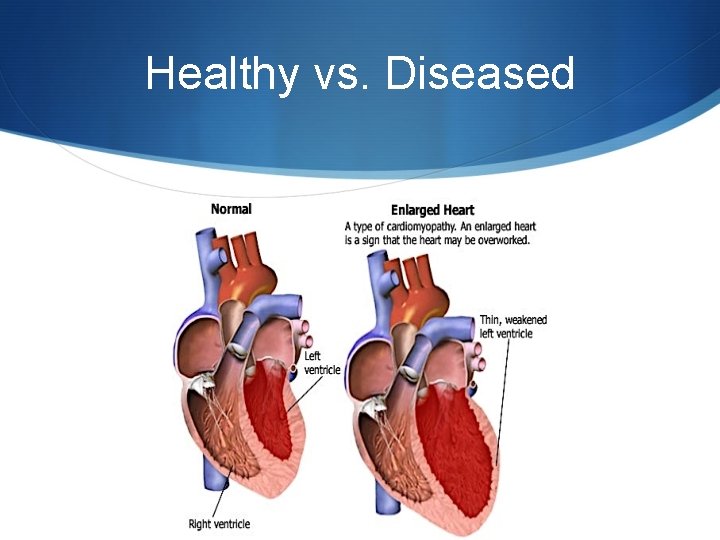
Healthy vs. Diseased
Nutrition/Medical Interventions S Heart healthy diet (such as the TLC diet)* S Physical activity S Medications (5 classes)* S ACE inhibitors & Angiotension receptor blockers S Beta-Blockers* S Diuretics* S Aldosterone receptor antagonists* S Nitrates

Surgical Interventions S Pacemaker Implantations* S Implantable Cardioverter Defibrillators S Coronary Artery Bypass Grafts S LVAD implantation* S Heart Transplant
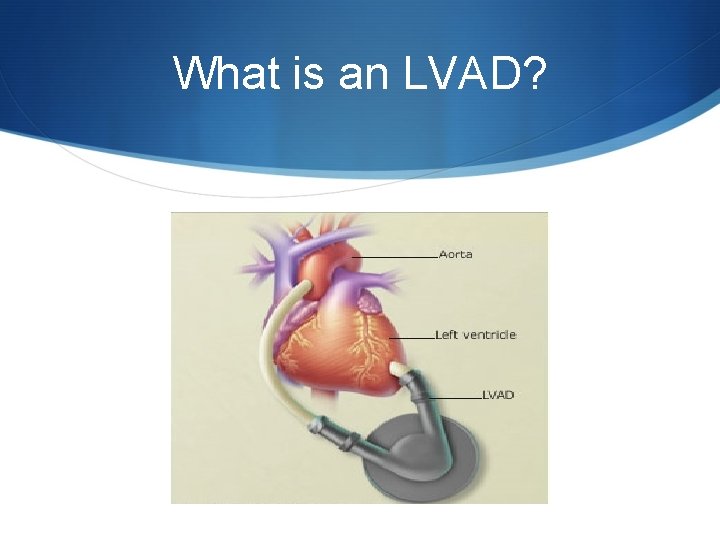
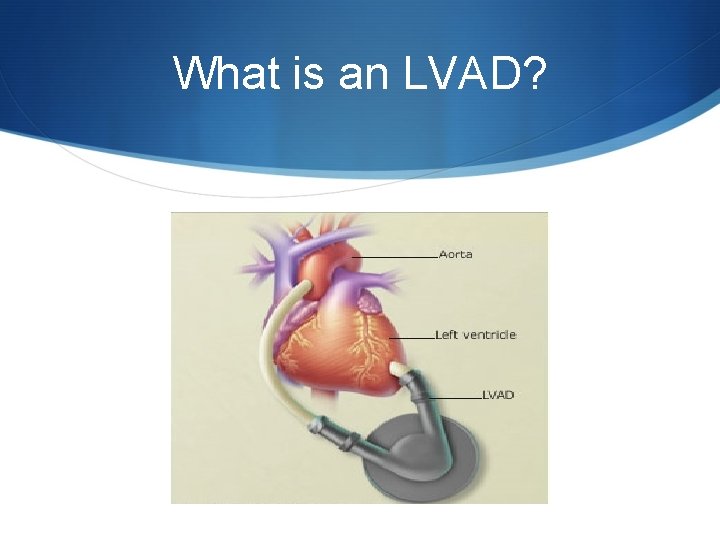
What is an LVAD?
LVAD: Heart Mate II S LVAD Video
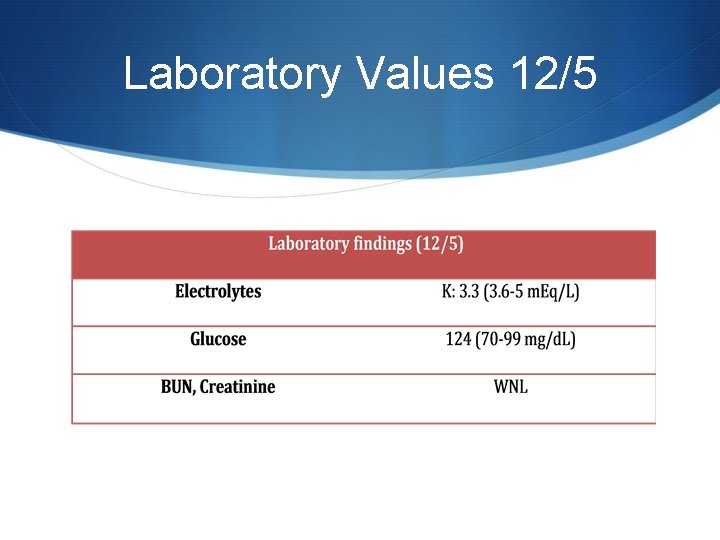
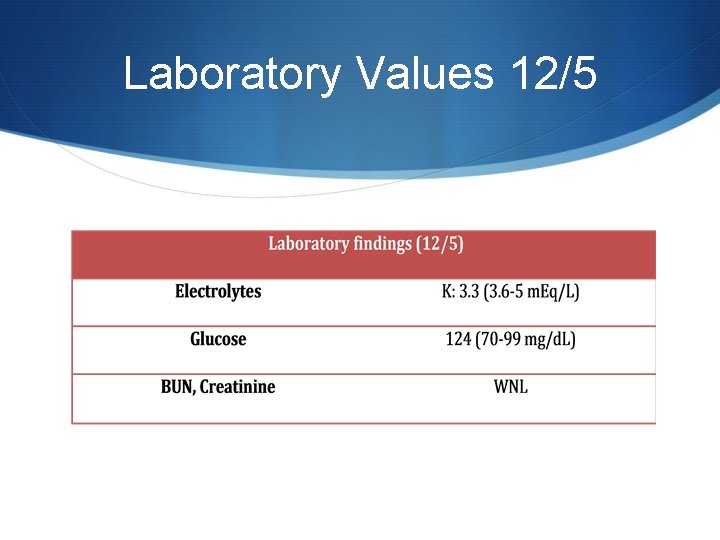
Laboratory Values 12/5
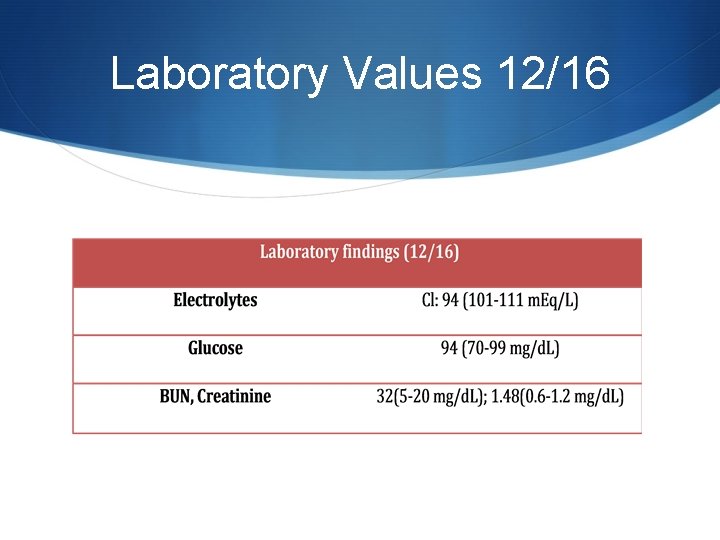
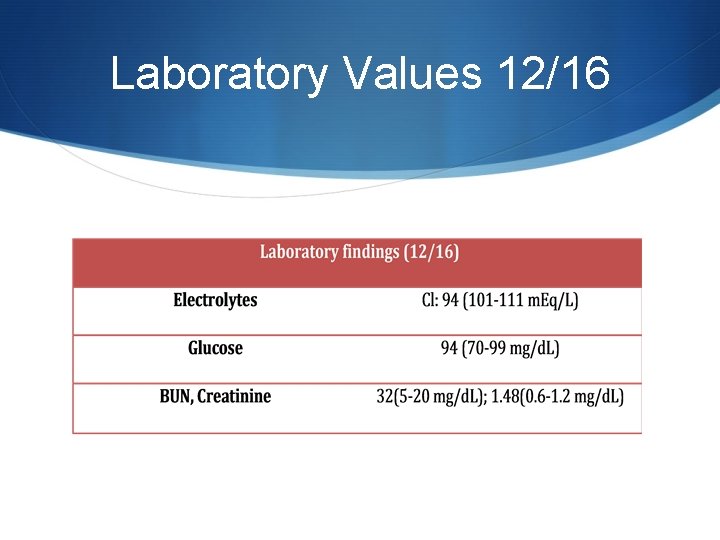
Laboratory Values 12/16

Medications S Albuterol S Lactobacillus Acidophillus S Amiodarone S Pantoprazole S Bumetanide S Ranolazine S Carvedilol S Spironolactone S Docusate-Senna S Coumadin S Humulin S Humalog
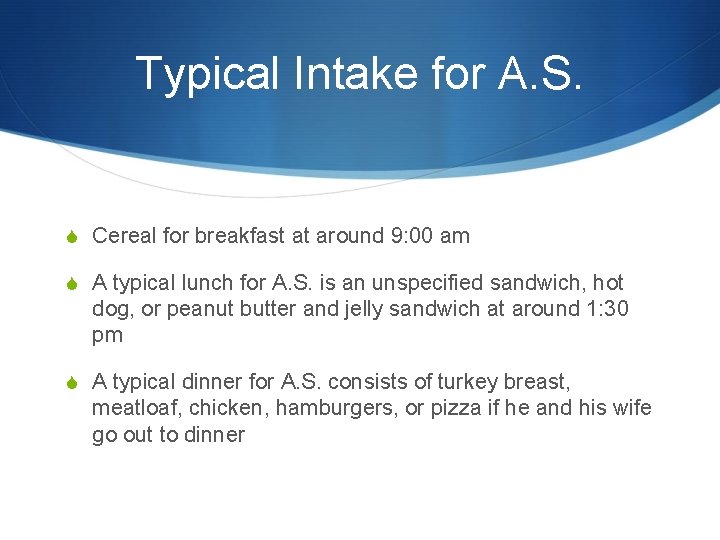
Typical Intake for A. S. S Cereal for breakfast at around 9: 00 am S A typical lunch for A. S. is an unspecified sandwich, hot dog, or peanut butter and jelly sandwich at around 1: 30 pm S A typical dinner for A. S. consists of turkey breast, meatloaf, chicken, hamburgers, or pizza if he and his wife go out to dinner
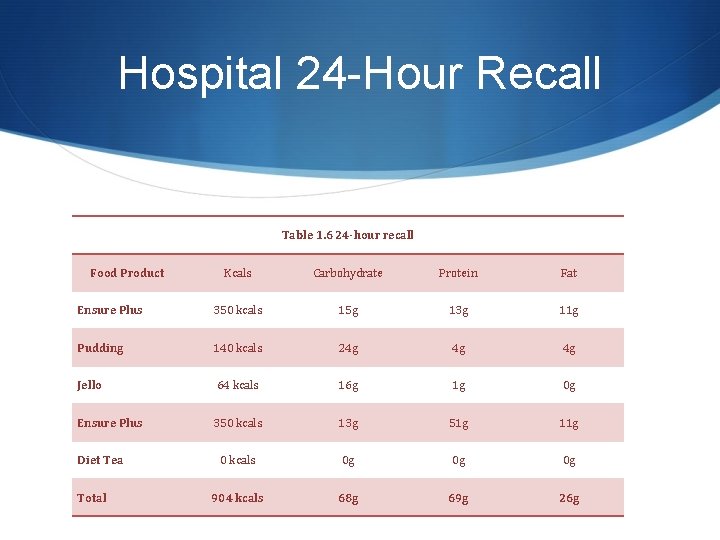
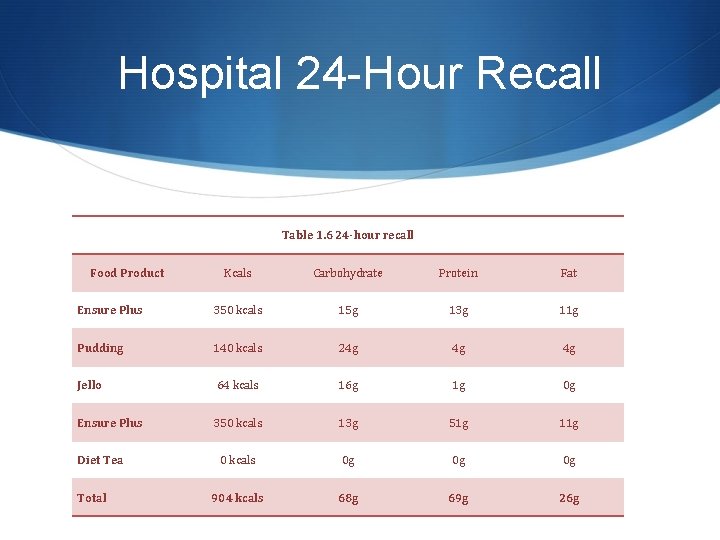
Hospital 24 -Hour Recall Table 1. 6 24 -hour recall Food Product Kcals Carbohydrate Protein Fat Ensure Plus 350 kcals 15 g 13 g 11 g Pudding 140 kcals 24 g 4 g 4 g Jello 64 kcals 16 g 1 g 0 g Ensure Plus 350 kcals 13 g 51 g 11 g 0 kcals 0 g 0 g 0 g 904 kcals 68 g 69 g 26 g Diet Tea Total
Nutrition Care Process: Assessment S At the time of A. S. ’s first visit, he was on a full liquid diet and was eating roughly 25% of his meals due to his lack of interest in the foods being served
Nutrition Care Process: Diagnosis S At the time of A. S. ’s first visit, his diagnosis was: S Inadequate protein energy intake related to decreased ability to consume sufficient protein and energy as evidenced by intake less than recommended needs S This diagnosis was formulated on the premises of the full liquid diet that was only fractionally consumed
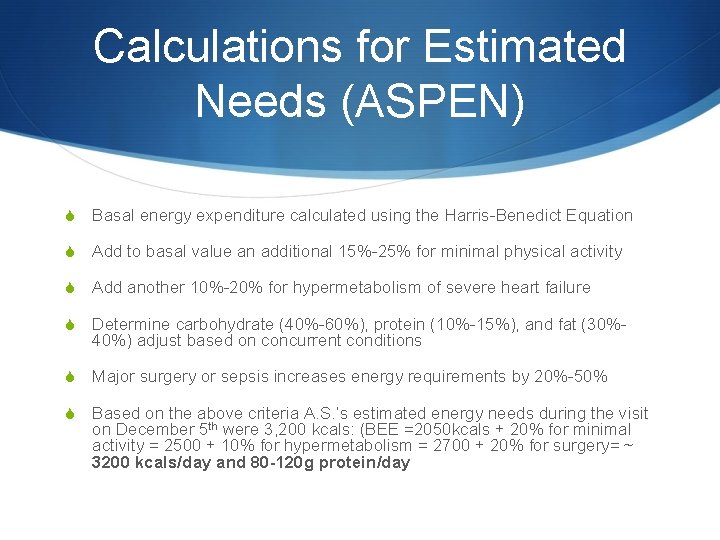
Calculations for Estimated Needs (ASPEN) S Basal energy expenditure calculated using the Harris-Benedict Equation S Add to basal value an additional 15%-25% for minimal physical activity S Add another 10%-20% for hypermetabolism of severe heart failure S Determine carbohydrate (40%-60%), protein (10%-15%), and fat (30%40%) adjust based on concurrent conditions S Major surgery or sepsis increases energy requirements by 20%-50% S Based on the above criteria A. S. ’s estimated energy needs during the visit on December 5 th were 3, 200 kcals: (BEE =2050 kcals + 20% for minimal activity = 2500 + 10% for hypermetabolism = 2700 + 20% for surgery= ~ 3200 kcals/day and 80 -120 g protein/day
Nutrition Care Process: Intervention S The importance of adequate calories and protein consumption for wound healing was discussed since he was only consuming ~25% of each meal S The topic of fat, sodium, and fluid restriction were not discussed at the time because A. S. was on a full liquid diet
Nutrition Care Process: Monitoring/Evaulation S Follow up visit was scheduled
Nutrition Care Process: Assessment S At the time of A. S. ’s second visit, A. S. ’s diet was advanced to a Solid Regular Coumadin/Warfarin Cardiac diet with Wolk Shake TID S A. S. was much more receptive to this diet than the previously prescribed diet consuming 100%
Nutrition Care Process: Diagnosis S During the second visit of the study A. S. did not have any acute nutrition related problems and so a formal nutrition diagnosis was not made secondary to 100% food/beverage intake and 100% Wolk Shake intake TID
Nutrition Care Process: Intervention/Monitoring/Evalua tion S No intervention, monitoring criteria, or evaluation was formulated as a formal diagnosis was not made
Observable Physiological and Psychological advancements S A. S. was feeling lethargic, experiencing shortness of breath and was not able to carry on the daily activities of life prior to surgery S A few days post surgery A. S. was not ambulating and appeared to be very tired and frail. His wife was present in the room and was able to assist with the interview process. Throughout A. S. ’s stay at the hospital, his physical and psychological changes were evident; with each visit, his physical and mental status greatly improved. S The second time A. S. was seen, he was able to answer all of his questions himself, and was ambulating. As the visits continued, A. S. became more talkative and began telling more personal stories about his life; such as the hardships he faced struggling with heart failure until he had the LVAD placement, rather than just talking about his eating patterns.
Medical Prognosis S Based on A. S. ’s length of stay at the hospital and the physiological and psychological advancements that were observed, it appears that the prognosis for A. S. is quite good S The most common complications post LVAD implantations are infection and sepsis (18%-59% of recipients) S Stroke is another common risk factor associated with LVAD therapy; the risk increases as long as the device remains in the patient’s body
Nutritional Prognosis S With increasing BMI, the risk for mortality decreases (good for A. S. as his BMI was 36. 1) post LVAD implantation S Metabolites such as glucose and lactate will restore to normal levels post LVAD implantation S Changes in myocardial metabolism occur in heart failure, resulting in decreased amino acid levels in cardiac tissues; LVAD therapy does not allow for the recovery of these amino acid stores
References S Web. MD. Heart Failure Health Center. Available at: http: //www. webmd. com/heartdisease/heart-failure/left-ventricular-assist-device. Accessed January 2 nd, 2014. S Fregmen BF, Frucht SS. Medical Terminology: A Living Language. 4 th ed. Upper Saddle River, NJ: Pearson; 2009: 132 -137. S Tool Loop. Veins in the Cardiovascular System. Available at: http: //www. tooloop. com/veins-in-the-cardiovascular-system/. Accessed January 9 th, 2014. S Kumar V, Abbas AK, Fausto N, Aster JC. Pathologic Basis of Disease. 8 th ed. Philadelphia, PA: Sunders Elsevier; 2010: 533 -537. S National Heart, Lung, and Blood Institute. What is Heart Failure? Available at: http: //www. nhlbi. nih. gov/health-topics/hf/. Updated January 9 th 2012. Accessed January 9 th, 2014.
References continued S Emory Healthcare. Heart Failure Stages & Functional Classifications. Available at: http: //www. emoryhealthcare. org/heart-failure/learn-aboutheart-failure/stages-classification. html. Accessed January 11 th 2014. S Heart Failure Society of America. Questions About HF. Available at: http: //www. abouthf. org/questions_stages. htm. Accessed January 11 th, 2014. S Schwartz DB, Di. Maria, RA. The A. S. P. E. N. Nutrition Support Core Curriculum a Case-Based Approach-The Adult Patient. 1 st ed. Silver Spring, MD: American Society for Parenteral and Enteral Nutrition; 2007: 495 -501. S Mahan KL, Escott-Stump S, Raymond, JL. Krause’s Food and the Nutrition Care Process. 13 th ed. St. Louis, MO: Elsevier Saunders; 2012: 194; 897. S Mayo Clinic. Diseases and Conditions. Available at: http: //www. mayoclinic. org/diseases-conditions/diabetes/expertblog/diabetes-blog/BGP-20056560. Accessed January 11 th, 2014
References continued S Mayo Clinic: Mayo Medical Laboratories. Test ID: Cl. Available at: http: //www. mayomedicallaboratories. com/test-catalog/Clinical+and+Interpretive/8460. Accessed January 11 th, 2014. S Rizzieri, A. , Verheijde, J. , Rady, M. , & Mc. Gregor, J. (2008). Ethical challenges with the left ventricular assist device as a destination therapy. Available at http: //www. ncbi. nih. gov/pmc/articles/PMC 2527574/. Accessed December 17 th, 2013. S American Dietetic Association. Nutrition Care Manual®. Heart Failure: Nutrition Prescription. http: //nutritioncaremanual. org/topic. Accessed December 17 th, 2013. S Medline Plus Trusted Health Information for You. Drugs, Supplements, and Herbal Information. Available at: http: //www. nlm. nih. gov/medlineplus/druginformation. html. Accessed January 9 th, 2014. S Florida Hospital. Enteral Nutrition Formulary. 2013 S Weitzel LB, Ambardekar AV, Brieke A, Cleveland JC, Serkova NJ, Wischmeyer PE, Lowes BD. Left Ventricular Assist Device Effects on Metabolic Substrates in the Failing Heart. April 2013; 8(4): 1 -6