MACRA Using Data to Capture the Quality Mark





- Slides: 25
MACRA: Using Data to Capture the Quality Mark Blessing, CPA, FHFMA, Managing Director Zach Remmich, Managing Consultant
Roadmap 1 2 3 2 MACRA Overview Key Elements Affecting Reimbursement in Value-Based Environment Engaging Physicians Using Data Analytics

WHY MACRA IS IMPORTANT 3 Ø Eliminated sustainable growth rate (“doc fix”): Ø Locks clinician payment rates at near zero growth Ø Phased out current Medicare physician payment programs: Ø Physician Quality Reporting System; Value-Based Modifier, Meaningful Use Ø Created two new physician incentive programs: Ø Merit-based Incentive Payment System (MIPS) Ø Advanced Alternative Payment Models (Adv APMs) – MACRA term Ø Program incentivizes participation in value-based, coordinated care models requiring EHR utilization
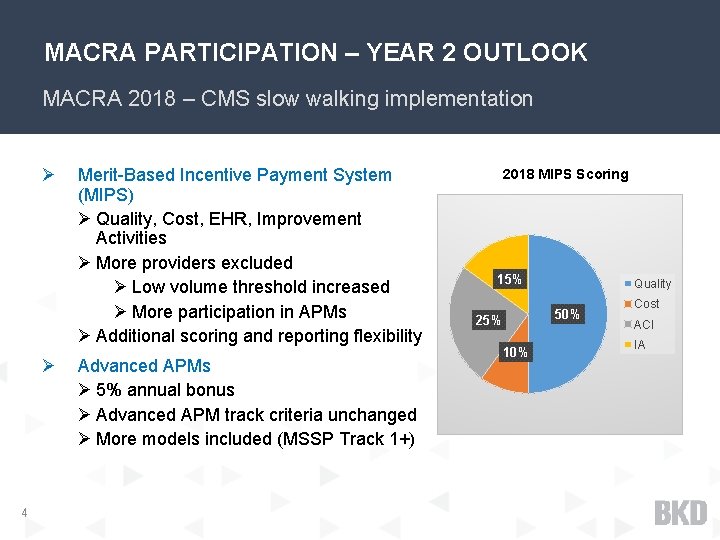
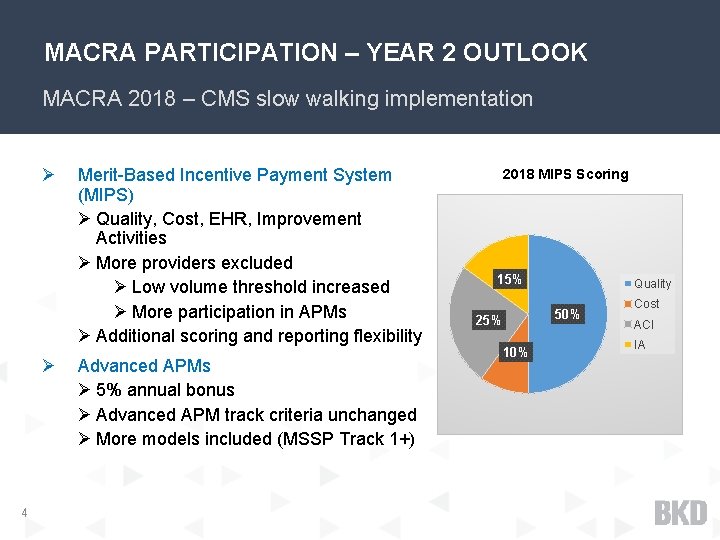
MACRA PARTICIPATION – YEAR 2 OUTLOOK MACRA 2018 – CMS slow walking implementation Ø Ø 4 Merit-Based Incentive Payment System (MIPS) Ø Quality, Cost, EHR, Improvement Activities Ø More providers excluded Ø Low volume threshold increased Ø More participation in APMs Ø Additional scoring and reporting flexibility Advanced APMs Ø 5% annual bonus Ø Advanced APM track criteria unchanged Ø More models included (MSSP Track 1+) 2018 MIPS Scoring 15% Quality 50% 25% 10% Cost ACI IA
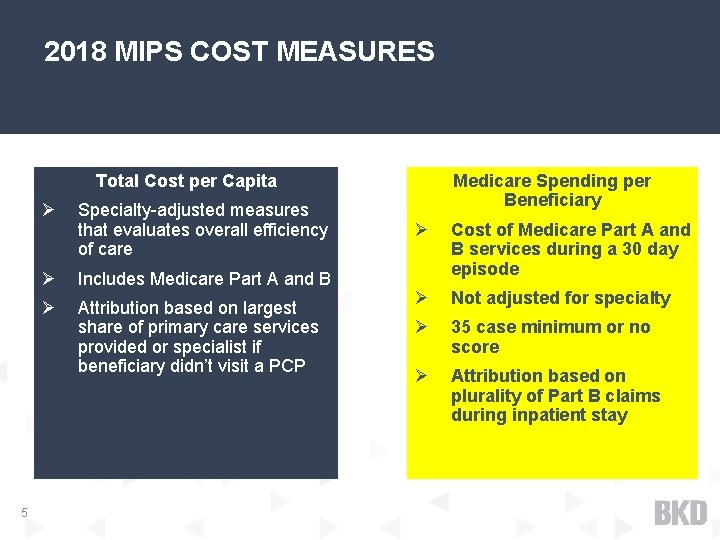
2018 MIPS COST MEASURES Medicare Spending per Beneficiary Total Cost per Capita 5 Ø Specialty-adjusted measures that evaluates overall efficiency of care Ø Includes Medicare Part A and B Ø Attribution based on largest share of primary care services provided or specialist if beneficiary didn’t visit a PCP Ø Cost of Medicare Part A and B services during a 30 day episode Ø Not adjusted for specialty Ø 35 case minimum or no score Ø Attribution based on plurality of Part B claims during inpatient stay
MACRA IMPLICATIONS Ø MACRA five-year reimbursement risk on stand-alone basis likely less than cost of infrastructure required to fully maximize reimbursement effect Ø Efforts to maximize MACRA reimbursement effect could have opposite (& potentially more material) downstream reimbursement effects for various providers in FFS environment Ø Practices need the necessary infrastructure & expertise to manage data reporting, care coordination & clinical outcomes before taking on payment risk Ø Total cost of care management for Medicare beneficiaries likely to be a significant differentiator 6
KEY ELEMENTS AFFECTING REIMBURSEMENT IN VALUE-BASED ENVIRONMENT 7
HISTORIC: FEE FOR SERVICE REIMBURSEMENT Ø Clinical procedure performed = add’l reimbursement Ø Profitability considerations: Ø Add’l expense of procedure offset by add’l reimbursement Ø Since reimbursements typically exceed direct expense of procedure, performing MORE procedures &/or HIGHER INTENSITY procedures helps cover indirect (overhead) costs Ø CPT procedural code drives reimbursement as opposed to ICD-10 diagnosis codes Ø Medicare DRG reimbursement is largest historic example of non-FFS reimbursement – what was its effect? Ø Significantly reduced average lengths of stay Ø Significantly increased diagnosis coding efforts 8
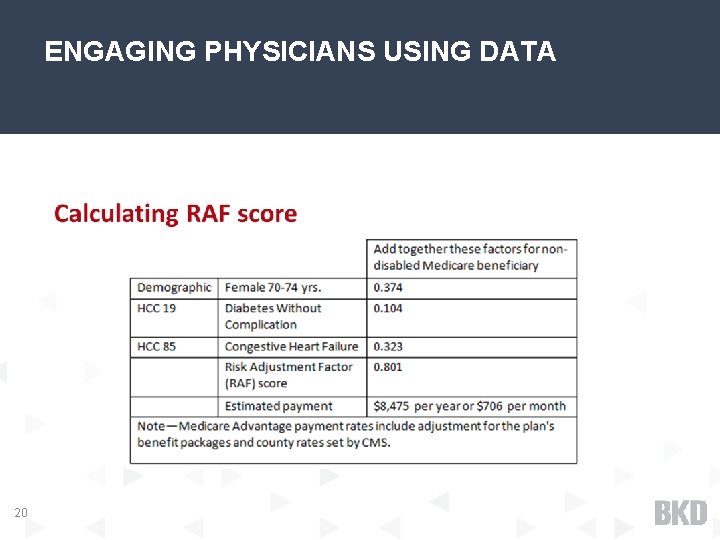
VALUE BASED REIMBURSEMENT Ø Patient episode = additional reimbursement Ø Patient episode definitions vary greatly, but basic way to define: Ø For Primary Care, attributed beneficiary total care for medical issues (Capitation) Ø For Specialists, referred beneficiary total expenditures for a specific issue, for a specific time after an initiating event (Bundle) Ø Reimbursement adjustments for “Value”: Ø Patient HCC Score: Higher score, higher reimbursement (“sicker”) Ø Quality & Outcomes: Higher score, higher reimbursement (“better care”) 9
VALUE BASED REIMBURSEMENT Continued… Ø Profitability considerations: Ø Clinical procedure performed – no additional reimbursement Ø Since no additional reimbursement, performing FEWER procedures &/or LOWER INTENSITY procedures helps profitability because of saved direct costs for procedures Ø ICD-10 diagnosis codes drive reimbursement as opposed to CPT procedural codes because of effect on HCC Score 10
HOW ARE CLINICIANS BEING AFFECTED Ø Different flavors of CMS initiatives Ø Accountable Care Organizations (ACO) Ø MACRA Ø Bundle programs (BPCI; Comprehensive Joint Replacement, etc. ) Ø Medical Home models Ø Many others Ø Commercial insurers are beginning to come along with Medicare 11
HOW ARE CLINICIANS BEING AFFECTED Continued… Ø New abilities become more important to profitability as VB reimbursement percent of business grows: Ø Diagnosis coding (HCC code effect) Ø Management of episode claim costs across all providers Ø Management of quality & outcome measures Ø What are organizations doing to develop & implement the above abilities? Ø Case management (control episode costs for high expense patients) Ø Clinical protocol development (control episode costs) Ø Coding initiatives such as AWV process (properly reflect HCC Scores) 12
ENGAGING PHYSICIANS USING DATA ANALYTICS 13

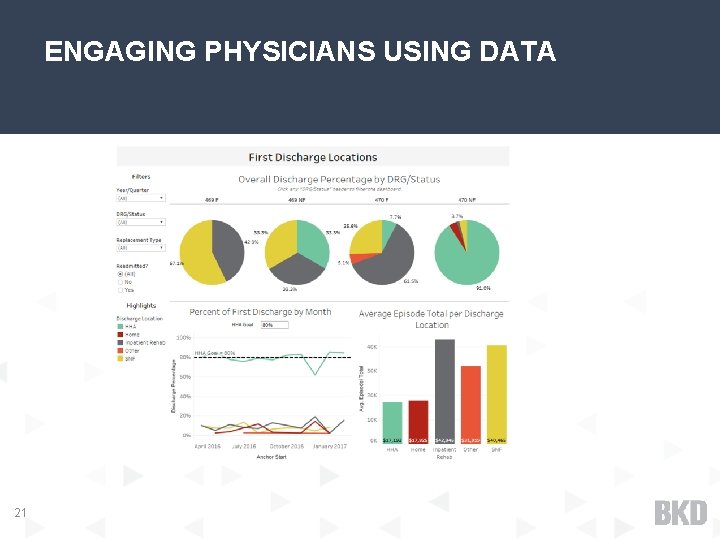
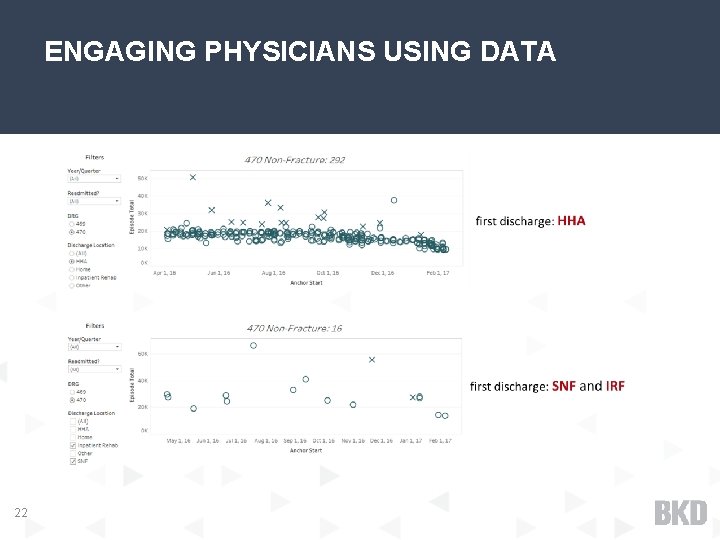
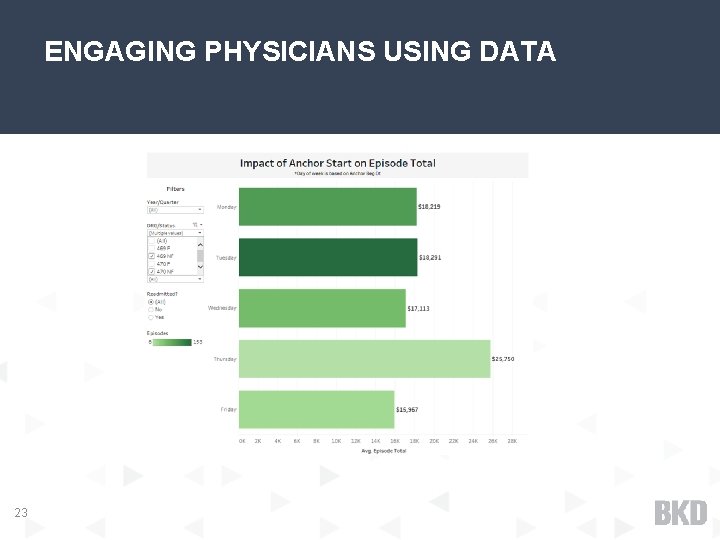
ENGAGING PHYSICIANS USING DATA 14 Ø The transition from FFS to value-based care can be summed up in two words: risk transfer Ø Multiple ways payers are transferring risk to providers: Ø Episodes of care (bundled payments) Ø ACO/MSSP Ø Hospitals must begin to think like insurance companies in terms of managing risk

ENGAGING PHYSICIANS USING DATA 15 Ø Clinical decision making becomes key financial driver- new business model Ø Standardize care, lower unwarranted variations, focus on complications and readmissions, drive down cost (Medicare and internal) Ø Must have management systems in place to gather, analyze and share data with physicians Ø Physician salary constitutes 20% of health care spending but the decisions they make influence an additional 60% of spending¹ Ø What about small, rural hospitals with only one specialist? Incenting n=1
DEVELOPING A PHYSICIAN COLLABORATOR STRATEGY 16 Ø Analyzing data for variation and impact Ø Identify high-level systemic care redesign needs Ø Identify collaborator quality guidelines Ø Integrate leadership physicians in strategy process Ø Gauge current level of interest Ø Consider how their practice will be affected Ø Evaluate potential internal cost savings Ø Compliance (FMV, Stark, IRS excess benefit)
ENGAGING PHYSICIANS Challenges you may face Ø Ø Ø Development challenges (Multi-group, employed and independent) Consensus on protocols and standardization Skepticism in data and measurement Concern with clinical decision making Perception of profit-sharing Lack of trust Establishing trust with physicians “Above all, success in business requires two things: a winning competitive strategy, and superb organizational execution. Distrust is the enemy of both. I submit that while high trust won't necessarily rescue a poor strategy, low trust will almost always derail a good one. ” Stephen MR Covey, The Speed of Trust 17
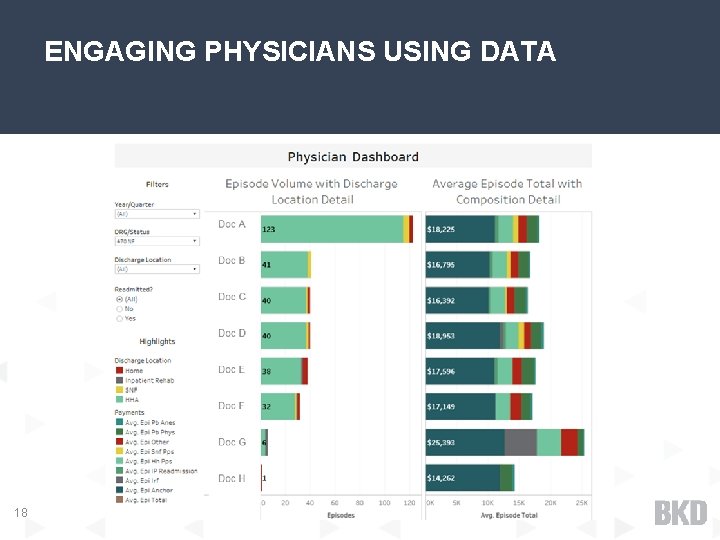
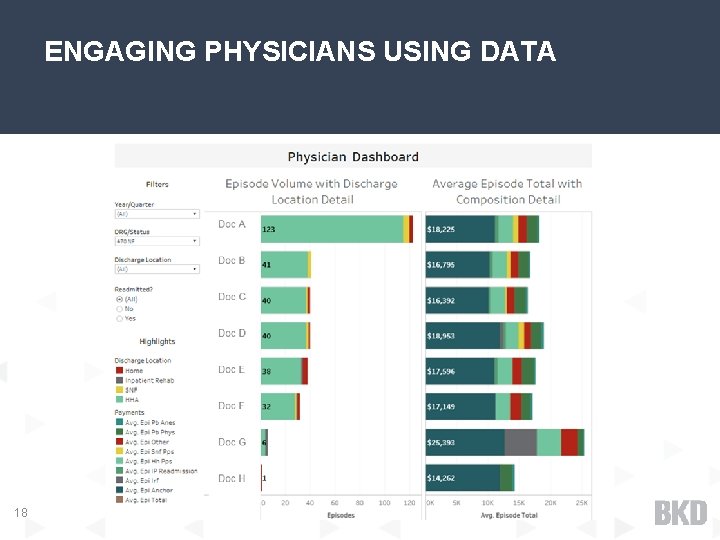
ENGAGING PHYSICIANS USING DATA 18
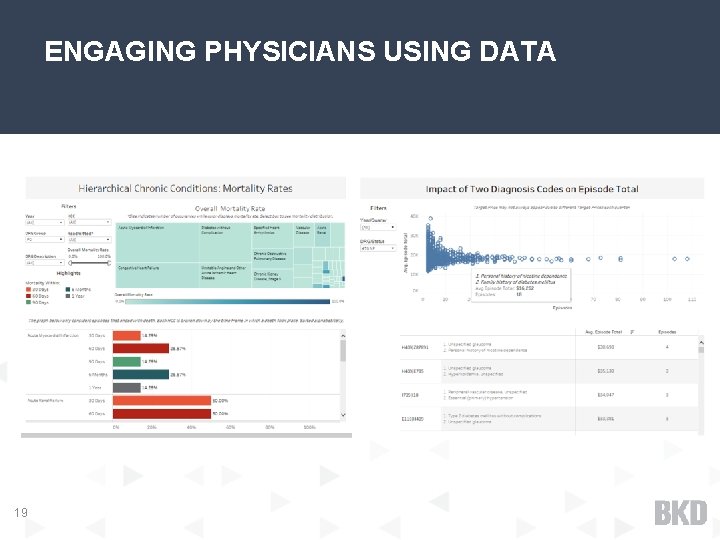
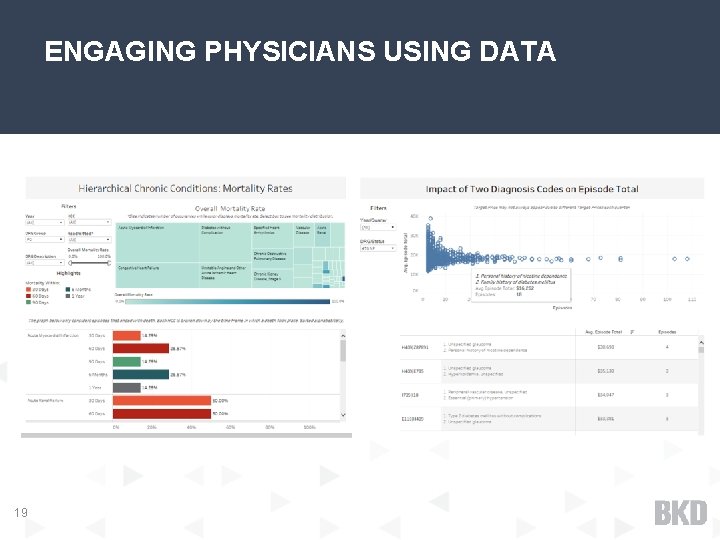
ENGAGING PHYSICIANS USING DATA 19
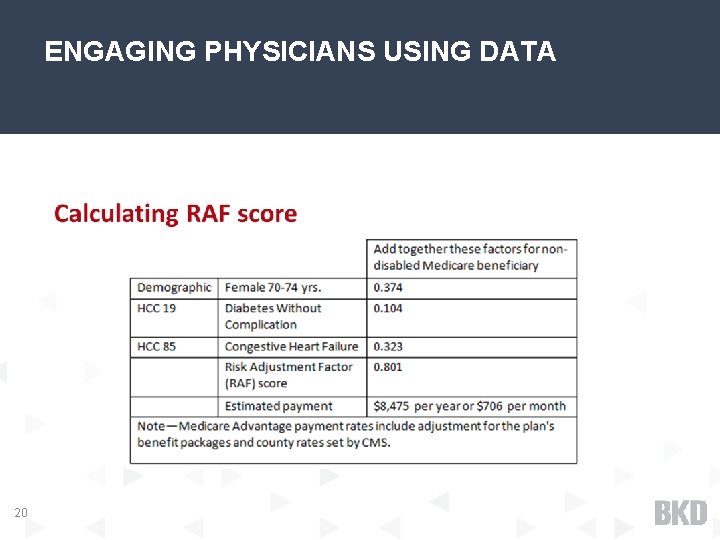
ENGAGING PHYSICIANS USING DATA 20
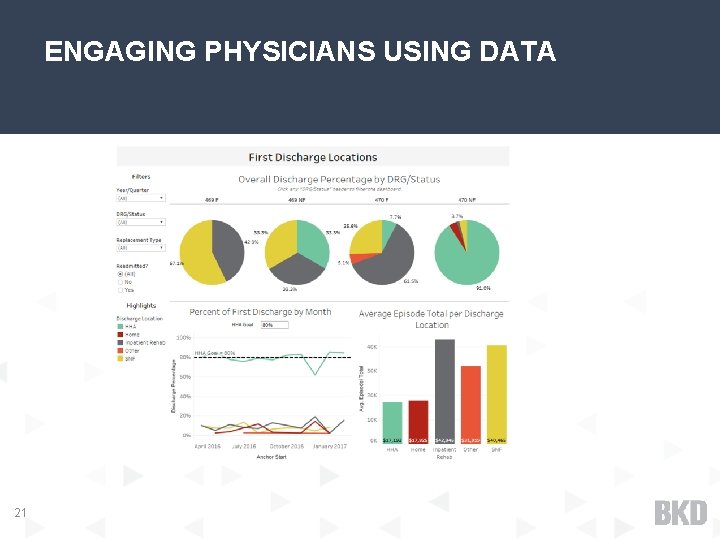
ENGAGING PHYSICIANS USING DATA 21
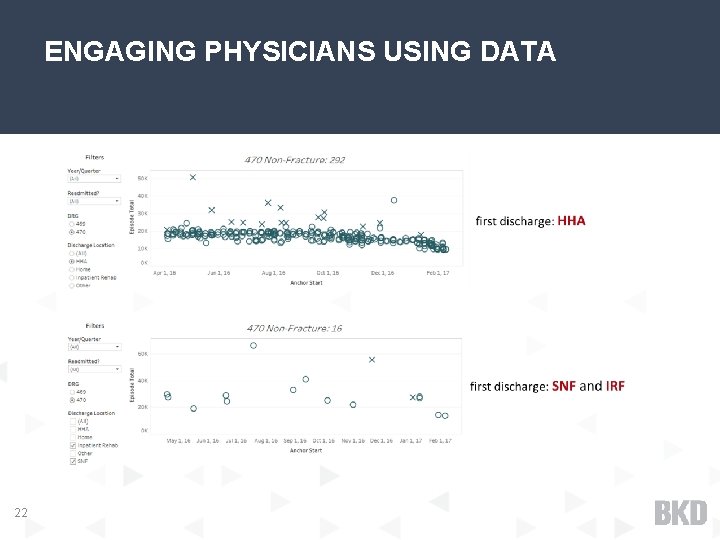
ENGAGING PHYSICIANS USING DATA 22
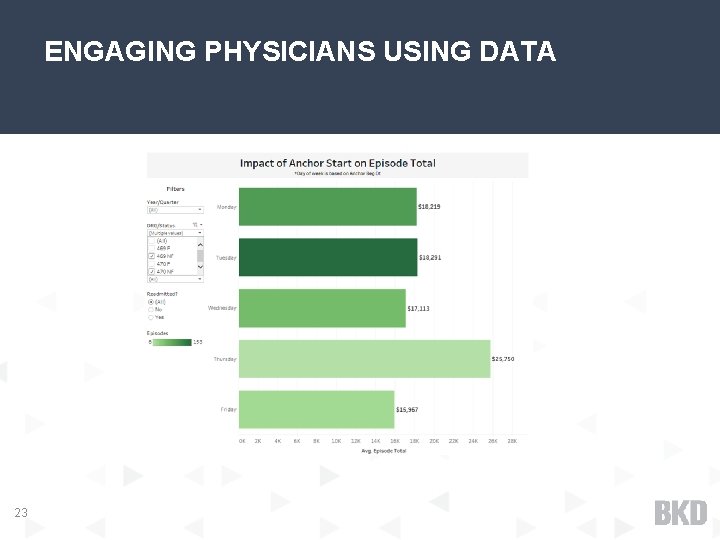
ENGAGING PHYSICIANS USING DATA 23

ENGAGING PHYSICIANS WITH DATA 24

25