MACRA Info Session 11 CMS Measure Development Education










- Slides: 29

MACRA Info Session #11 CMS Measure Development Education & Outreach Merit-based Incentive Payment System (MIPS): An Overview from CMS Presenters: Susan Arday, CMS Sophia Sugumar, CMS Dan Riner, CMS August 7, 2019 2: 00 -3: 00 pm ET
Vision and Goals: MACRA Info Sessions • An ongoing process to engage the public in quality measure development. • Elicit feedback that will help CMS design resources that can help all of those interested in healthcare quality improvement better understand the goals of quality measurement. • Education • Outreach • Dedicated Websites • Measure Development Roadmaps • Listserv opportunities 2

THE MERIT-BASED INCENTIVE PAYMENT SYSTEM: ANNUAL CALL FOR QUALITY MEASURES August 7, 2019 CMS/CCSQ/QMVIG: Sophia Sugumar Susan Arday Dan Riner
Today’s Webinar Topics • Introduction to the Merit-based Incentive Payment System (MIPS) • Overview of Existing MIPS Quality Measures • How New Quality Measures are Implemented in MIPS • QCDR Measures Compared to MIPS Quality Measures • Public Reporting on Physician Compare 4

INTRODUCTION TO THE MERIT-BASED INCENTIVE PAYMENT SYSTEM (MIPS) 5
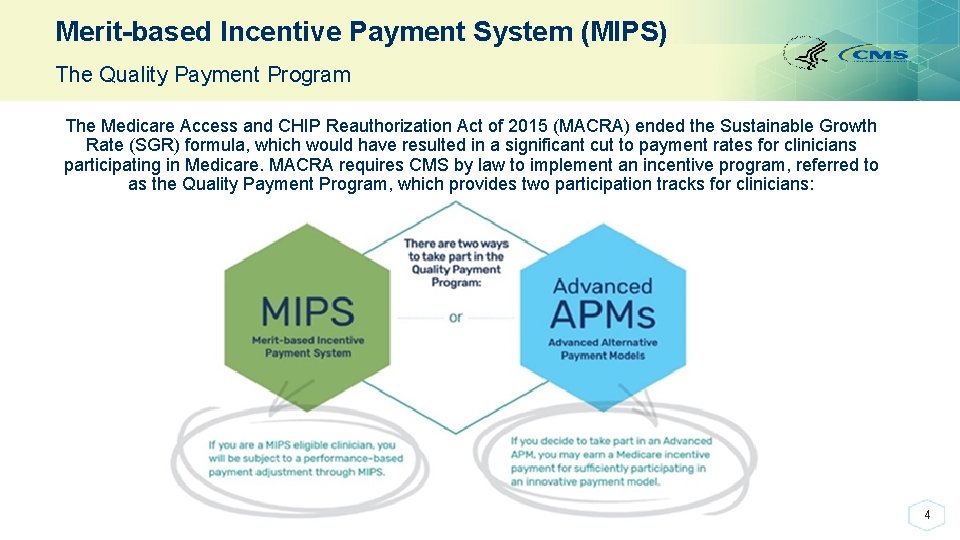
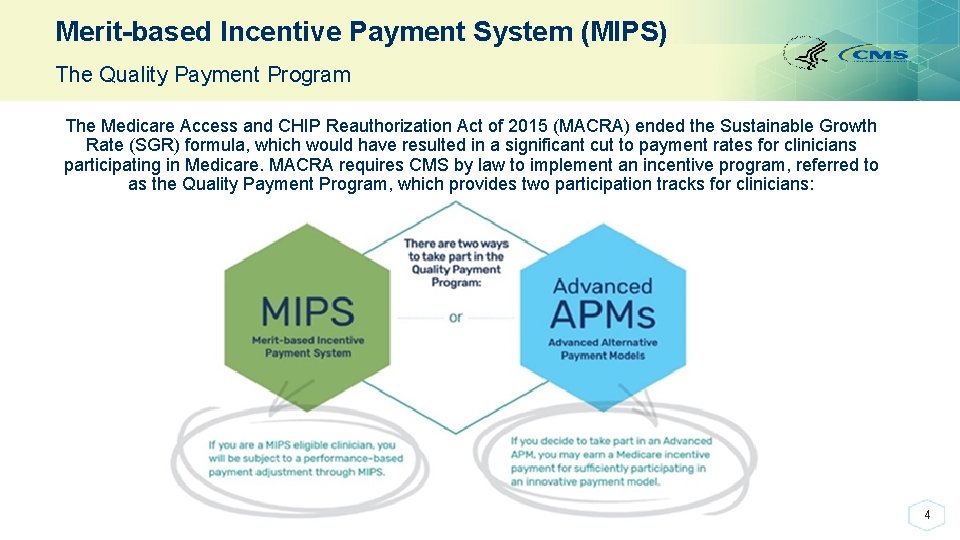
Merit-based Incentive Payment System (MIPS) The Quality Payment Program The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ended the Sustainable Growth Rate (SGR) formula, which would have resulted in a significant cut to payment rates for clinicians participating in Medicare. MACRA requires CMS by law to implement an incentive program, referred to as the Quality Payment Program, which provides two participation tracks for clinicians: 4
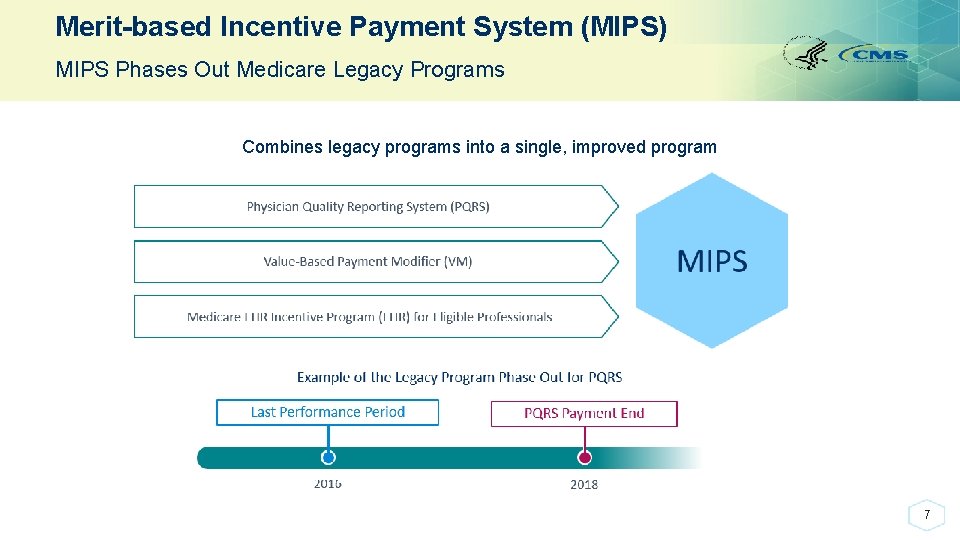
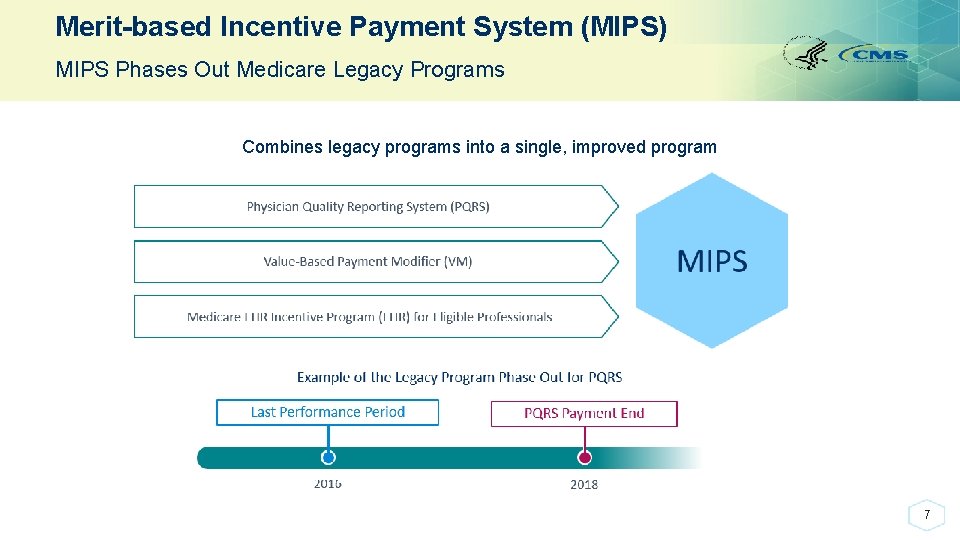
Merit-based Incentive Payment System (MIPS) MIPS Phases Out Medicare Legacy Programs Combines legacy programs into a single, improved program 7
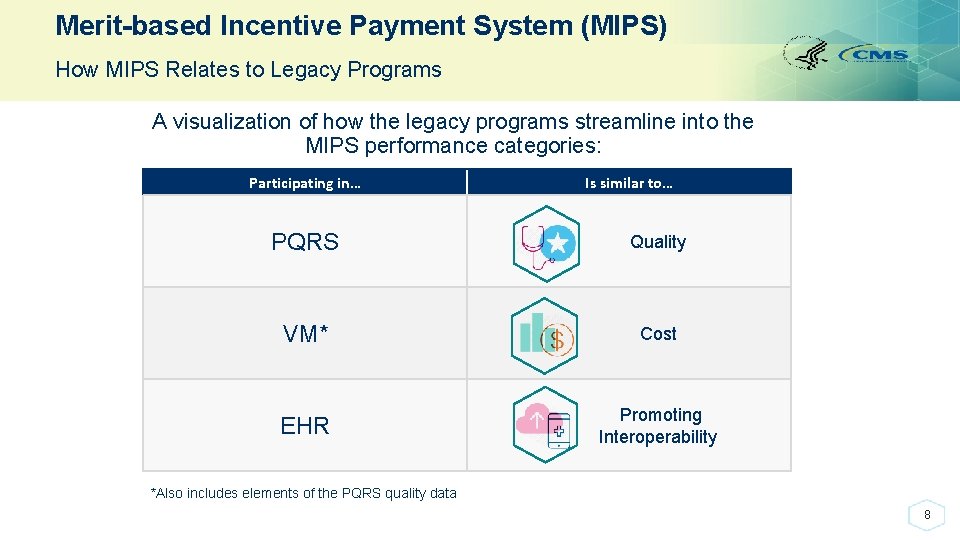
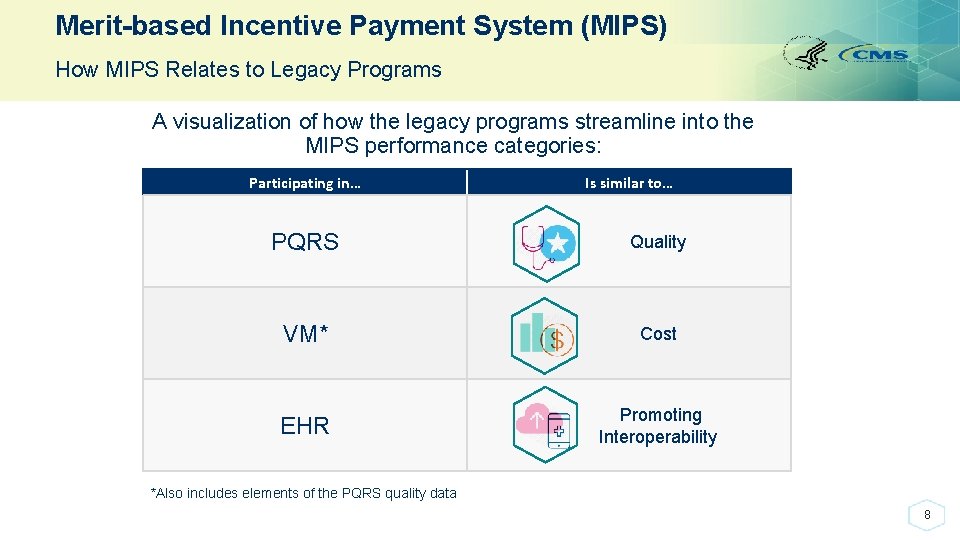
Merit-based Incentive Payment System (MIPS) How MIPS Relates to Legacy Programs A visualization of how the legacy programs streamline into the MIPS performance categories: Participating in… Is similar to… PQRS Quality VM* Cost EHR Promoting Interoperability *Also includes elements of the PQRS quality data 8

Merit-based Incentive Payment System (MIPS) What is the Merit-based Incentive Payment System? Performance Categories* • Moves Medicare Part B clinicians to a performance-based payment system • Provides clinicians with flexibility to choose the activities and measures that are most meaningful to their practice • Reporting standards align with Advanced APMs wherever possible *Weights assigned to each category based on a 1 to 100 point scale; the weights can be adjusted in certain circumstances. These weights are effective for Performance Year 2019. 9
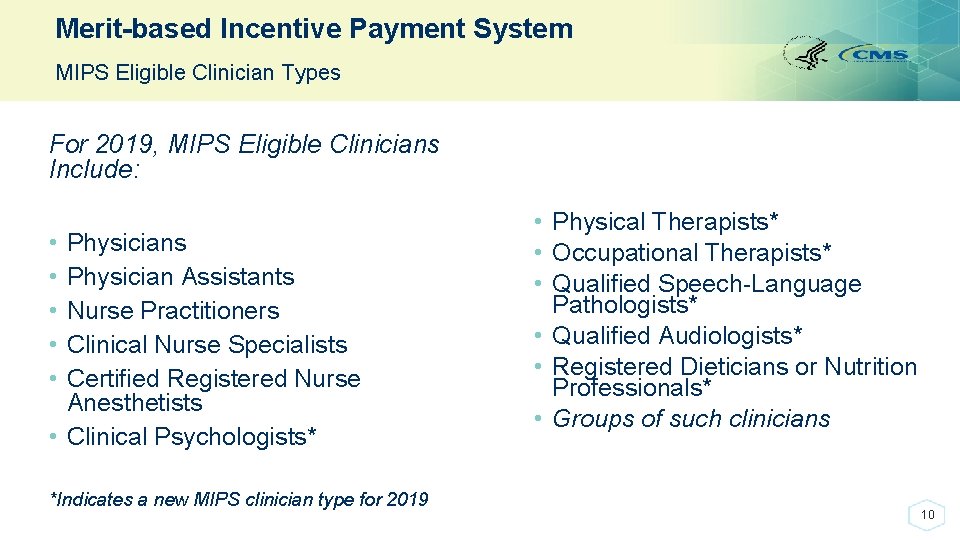
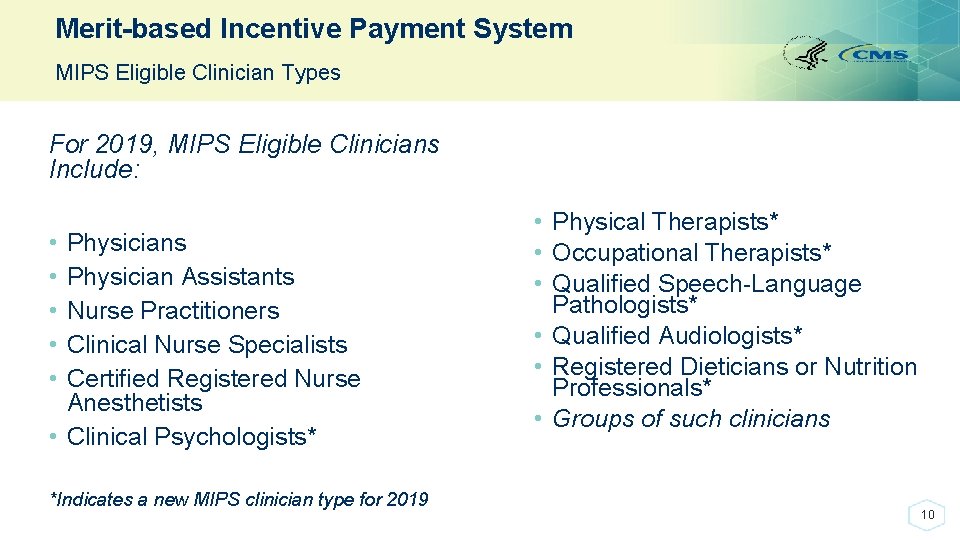
Merit-based Incentive Payment System MIPS Eligible Clinician Types For 2019, MIPS Eligible Clinicians Include: • • • Physicians Physician Assistants Nurse Practitioners Clinical Nurse Specialists Certified Registered Nurse Anesthetists • Clinical Psychologists* *Indicates a new MIPS clinician type for 2019 • Physical Therapists* • Occupational Therapists* • Qualified Speech-Language Pathologists* • Qualified Audiologists* • Registered Dieticians or Nutrition Professionals* • Groups of such clinicians 10
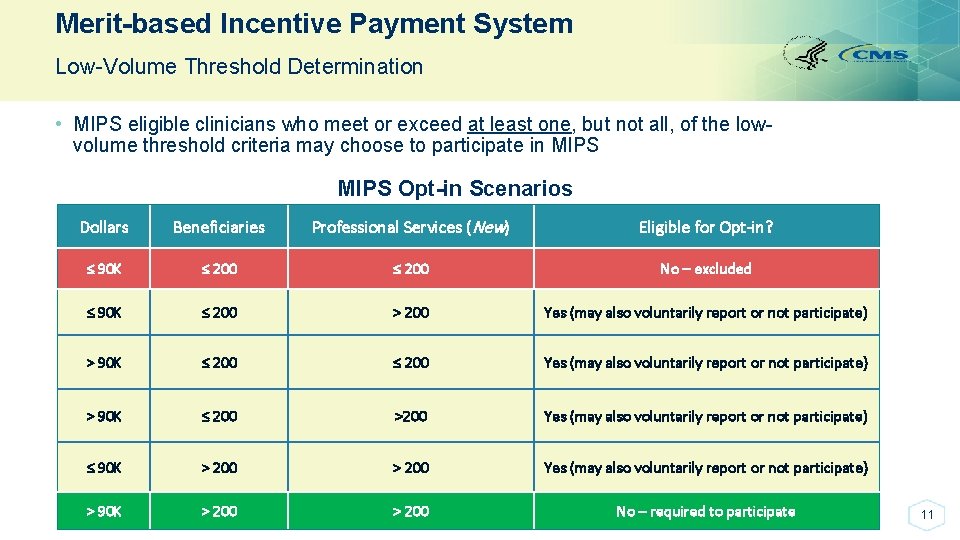
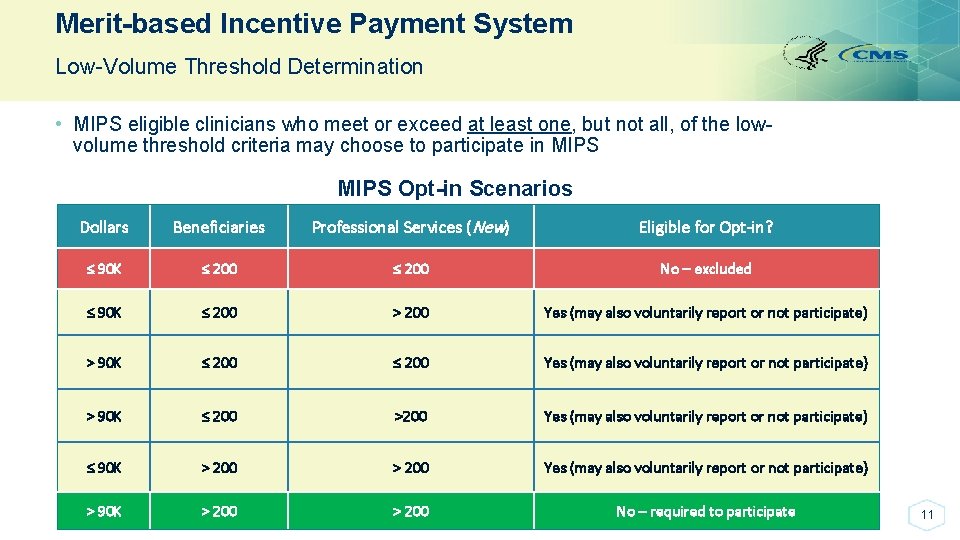
Merit-based Incentive Payment System Low-Volume Threshold Determination • MIPS eligible clinicians who meet or exceed at least one, but not all, of the lowvolume threshold criteria may choose to participate in MIPS Opt-in Scenarios Dollars Beneficiaries Professional Services (New) Eligible for Opt-in? ≤ 90 K ≤ 200 No – excluded ≤ 90 K ≤ 200 > 200 Yes (may also voluntarily report or not participate) > 90 K ≤ 200 >200 Yes (may also voluntarily report or not participate) ≤ 90 K > 200 Yes (may also voluntarily report or not participate) > 90 K > 200 No – required to participate 11

2019 CALL FOR QUALITY MEASURES 12
How Do Quality Measures Enter MIPS? Annual Call for Quality Measures • The Annual Call Quality Measures process allows organizations such as professional associations and medical societies, to identify and submit measures for consideration for the Quality performance category in MIPS. 13
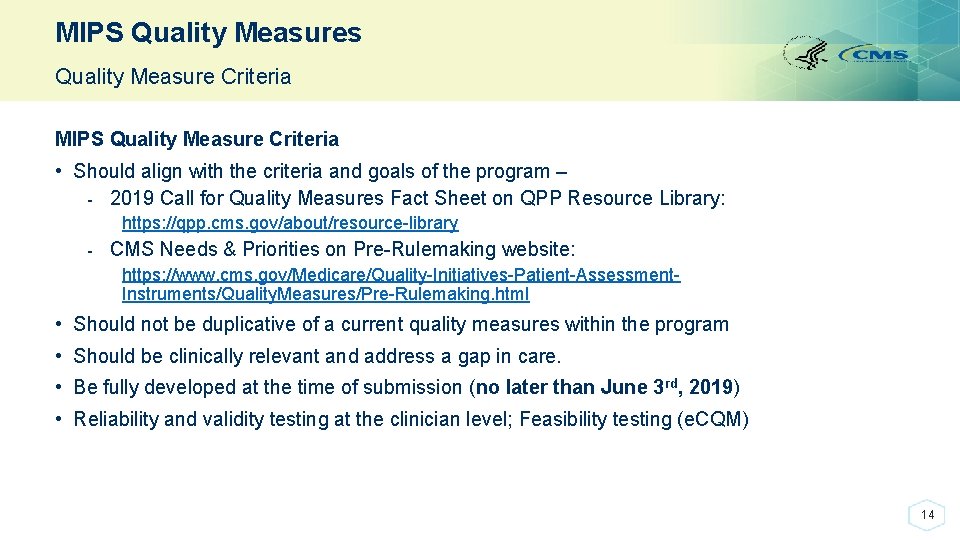
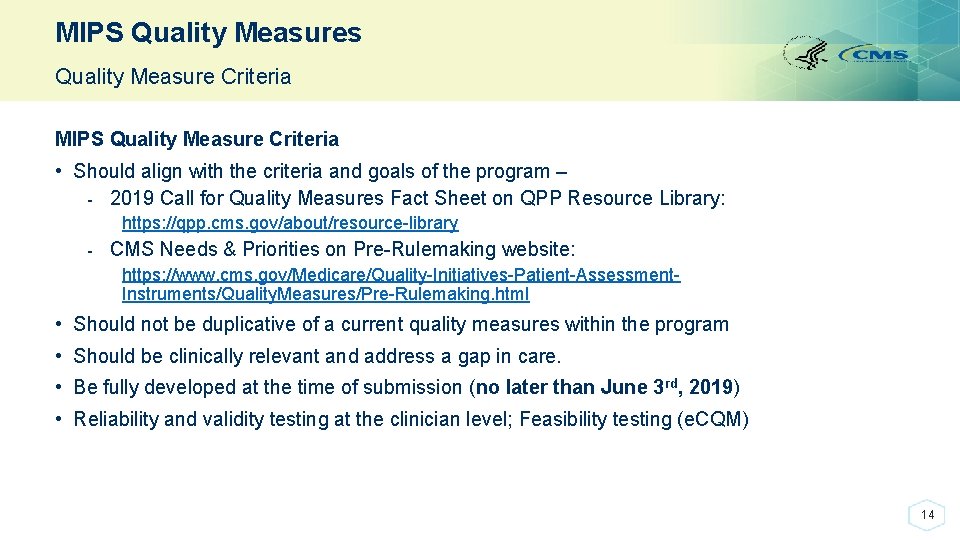
MIPS Quality Measures Quality Measure Criteria MIPS Quality Measure Criteria • Should align with the criteria and goals of the program – - 2019 Call for Quality Measures Fact Sheet on QPP Resource Library: https: //qpp. cms. gov/about/resource-library - CMS Needs & Priorities on Pre-Rulemaking website: https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/Quality. Measures/Pre-Rulemaking. html • Should not be duplicative of a current quality measures within the program • Should be clinically relevant and address a gap in care. • Be fully developed at the time of submission (no later than June 3 rd, 2019) • Reliability and validity testing at the clinician level; Feasibility testing (e. CQM) 14
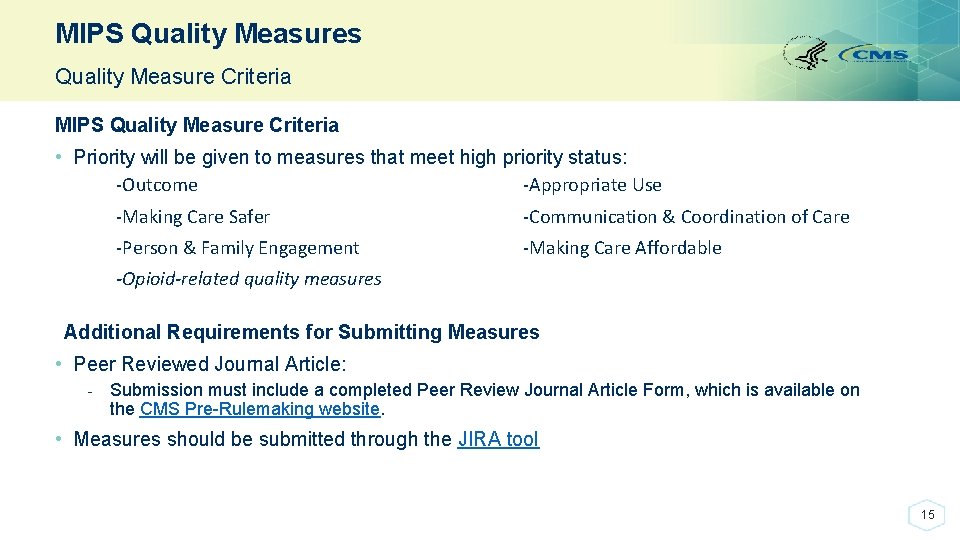
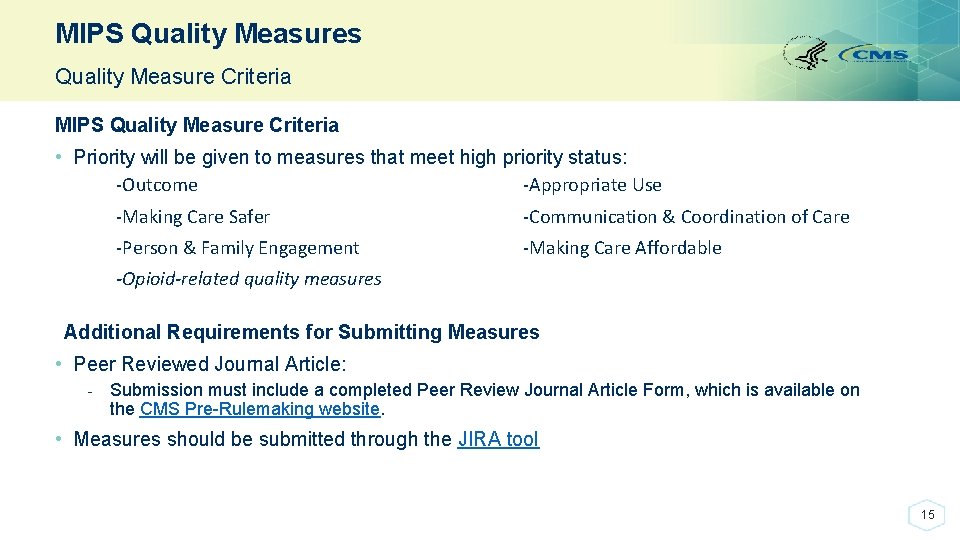
MIPS Quality Measures Quality Measure Criteria MIPS Quality Measure Criteria • Priority will be given to measures that meet high priority status: -Outcome -Appropriate Use -Making Care Safer -Communication & Coordination of Care -Person & Family Engagement -Making Care Affordable -Opioid-related quality measures Additional Requirements for Submitting Measures • Peer Reviewed Journal Article: - Submission must include a completed Peer Review Journal Article Form, which is available on the CMS Pre-Rulemaking website. • Measures should be submitted through the JIRA tool 15

MIPS Quality Measures Call for Measures/ MUD List • Measures that are submitted to the Call for Quality Measures but are not ready for implementation may be added to the MUD (Measures Under Development) List. - These measures are populated using measure developer submissions to the MIDS Resource Library and measures submitted for consideration in the pre-rulemaking process, but have not been accepted into a program at this time. - https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/Quality. Measures/CMS-Measures-Inventory. html • Current MIPS quality measures are resubmitted through the Call for Measures if the measure owner/steward suggests: - Expanding the measure into other CMS programs that follow the pre-rulemaking process, - Expanding a measure to another collection type (i. e. e. CQM) and significant changes to the measure, - Sensitive or controversial changes in clinical guidelines/technologies/intent of a measure at CMS’ discretion, or - Changes to the level of analysis (i. e. from facility to clinician level) 16
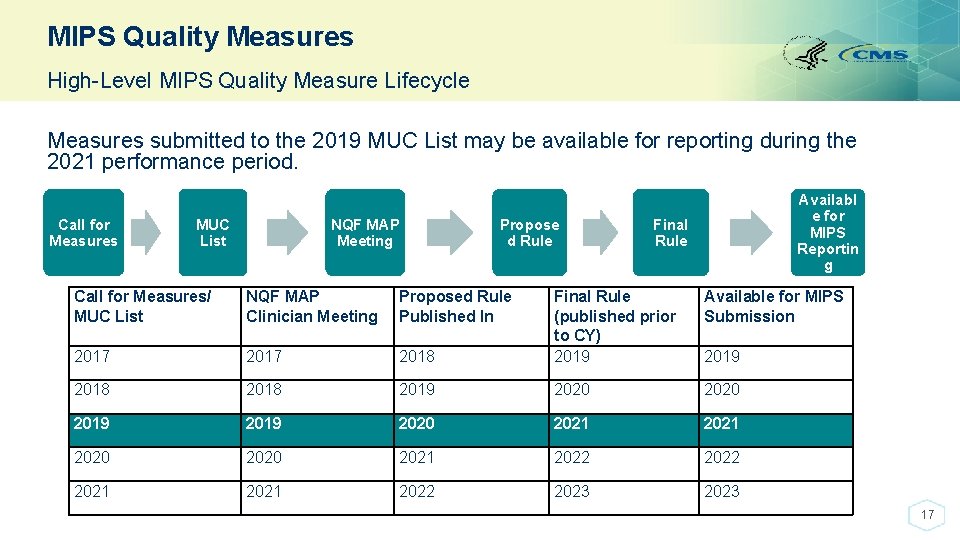
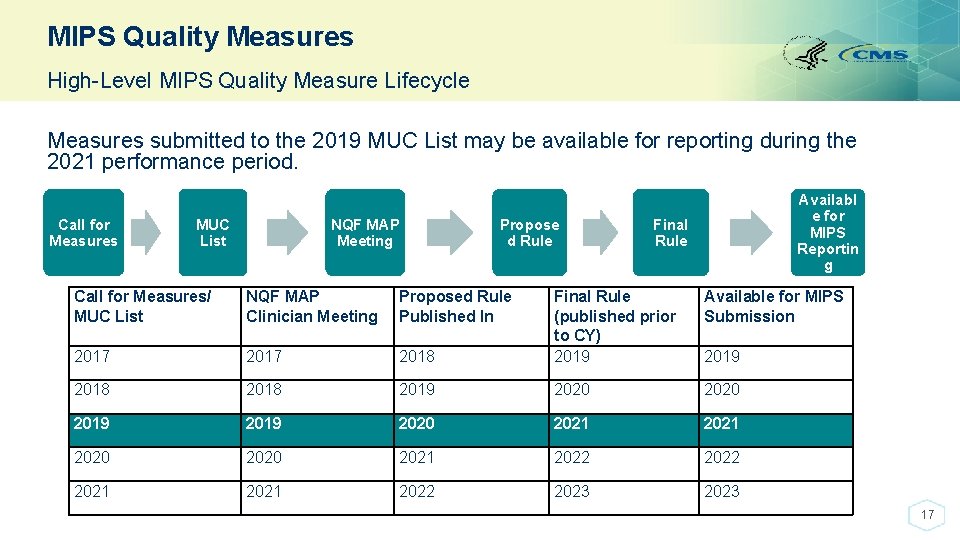
MIPS Quality Measures High-Level MIPS Quality Measure Lifecycle Measures submitted to the 2019 MUC List may be available for reporting during the 2021 performance period. Call for Measures NQF MAP Meeting MUC List Propose d Rule Call for Measures/ MUC List NQF MAP Clinician Meeting Proposed Rule Published In 2017 2018 Availabl e for MIPS Reportin g Final Rule Available for MIPS Submission 2018 Final Rule (published prior to CY) 2019 2018 2019 2020 2021 2020 2021 2022 2023 2019 17
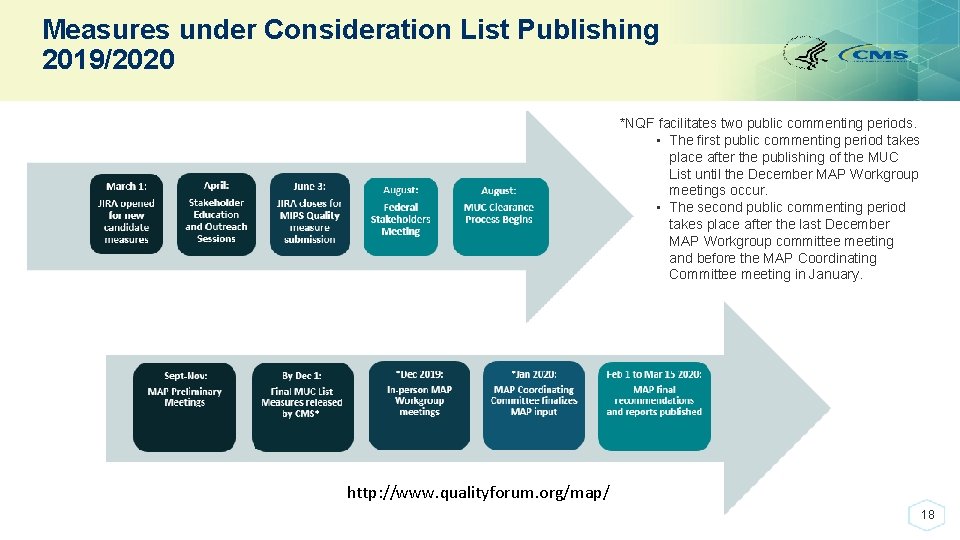
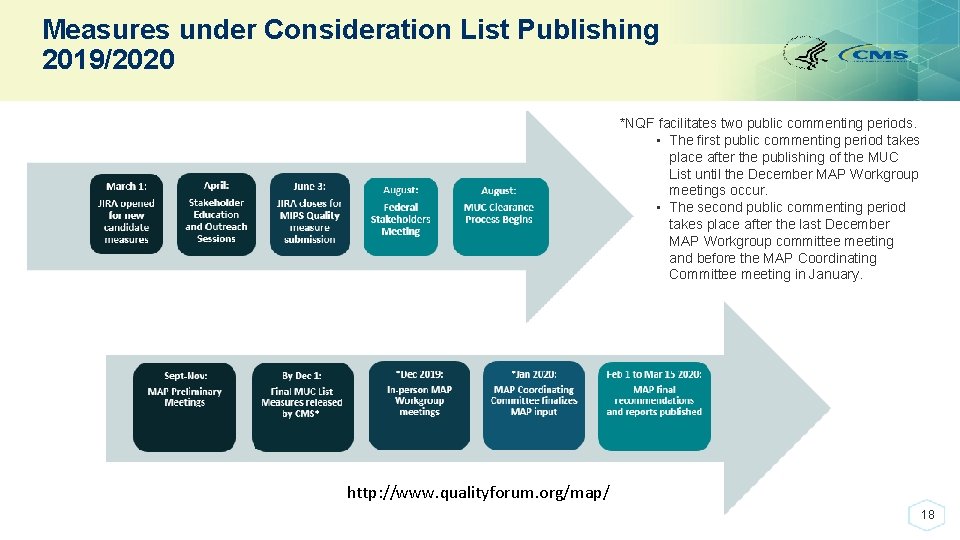
Measures under Consideration List Publishing 2019/2020 *NQF facilitates two public commenting periods. • The first public commenting period takes place after the publishing of the MUC List until the December MAP Workgroup meetings occur. • The second public commenting period takes place after the last December MAP Workgroup committee meeting and before the MAP Coordinating Committee meeting in January. http: //www. qualityforum. org/map/ 18

QCDR (QUALIFIED CLINICAL DATA REGISTRY) MEASURES: LIFECYCLE, CRITERIA, CHALLENGES/LIMITATIONS & BENEFITS 19
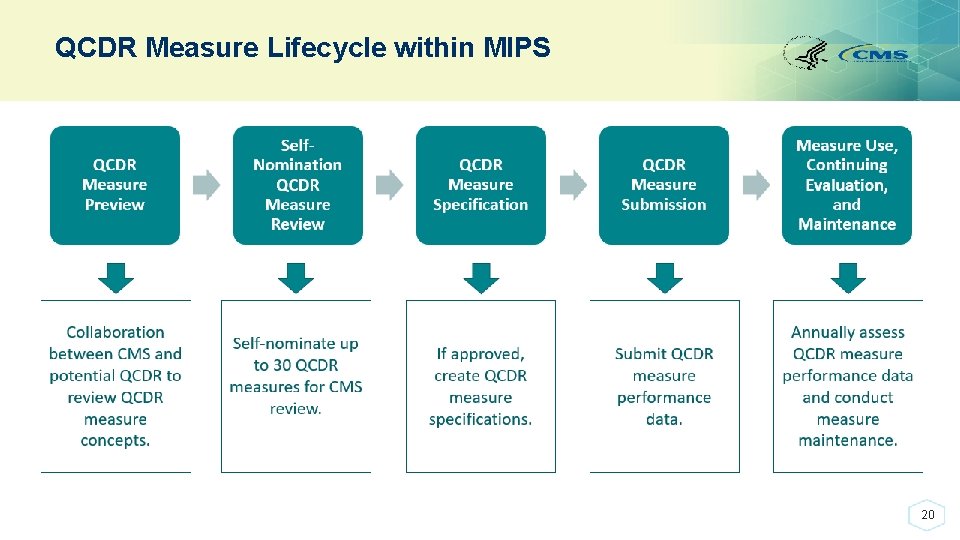
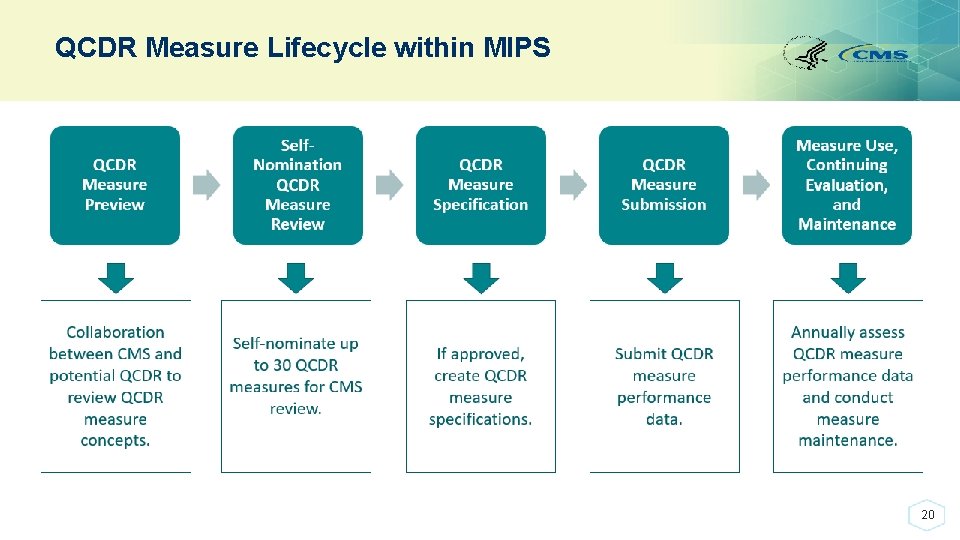
QCDR Measure Lifecycle within MIPS 20
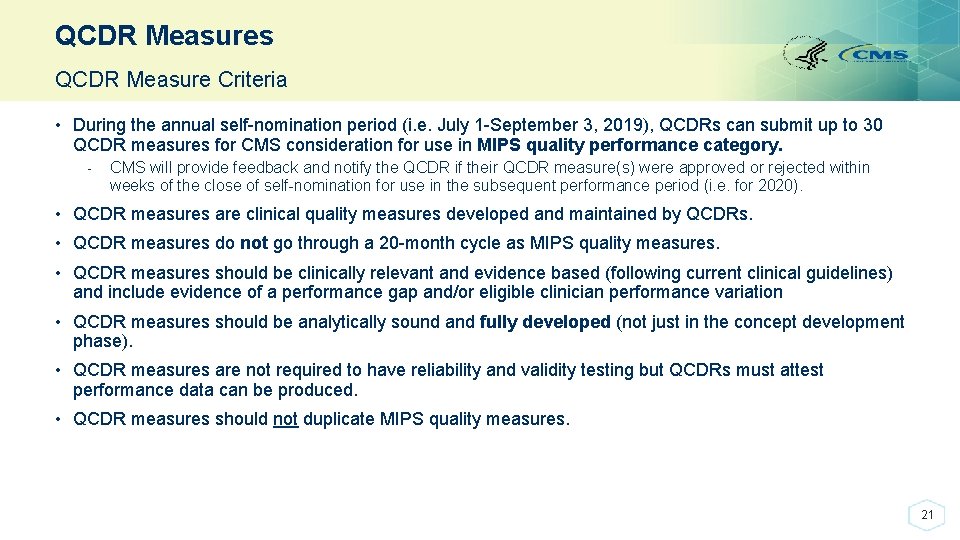
QCDR Measures QCDR Measure Criteria • During the annual self-nomination period (i. e. July 1 -September 3, 2019), QCDRs can submit up to 30 QCDR measures for CMS consideration for use in MIPS quality performance category. - CMS will provide feedback and notify the QCDR if their QCDR measure(s) were approved or rejected within weeks of the close of self-nomination for use in the subsequent performance period (i. e. for 2020). • QCDR measures are clinical quality measures developed and maintained by QCDRs. • QCDR measures do not go through a 20 -month cycle as MIPS quality measures. • QCDR measures should be clinically relevant and evidence based (following current clinical guidelines) and include evidence of a performance gap and/or eligible clinician performance variation • QCDR measures should be analytically sound and fully developed (not just in the concept development phase). • QCDR measures are not required to have reliability and validity testing but QCDRs must attest performance data can be produced. • QCDR measures should not duplicate MIPS quality measures. 21

QCDR Measures Compared to MIPS Quality Measures for 2019 MIPS Quality Measures QCDR Measures 257 Quality Measures for PY 2019 752 QCDR measures for PY 2019 Submitted through the Annual Call for Quality Measures for use by eligible clinicians, group practices, registries and QCDRs Submitted by QCDRs during the QCDR selfnomination process for use by QCDRs Any organization may submit an unlimited number of measures Limited to QCDRs who may submit up to 30 measures annually for consideration Reviewed by the MAP following the Call for Quality Measures submissions if added to the MUC List Not reviewed by the MAP Must be fully developed, clinically relevant and evidence based with adequate reliability, validity testing and performance data Must be fully developed, clinically relevant and evidence based with performance gap information Included in the Proposed Rule the following year for Included in the program for the following year (selfthe next year’s program (20 -month cycle) nomination/measure submissions occur July 1, 2019 – September 3, 2019) for 2020 22
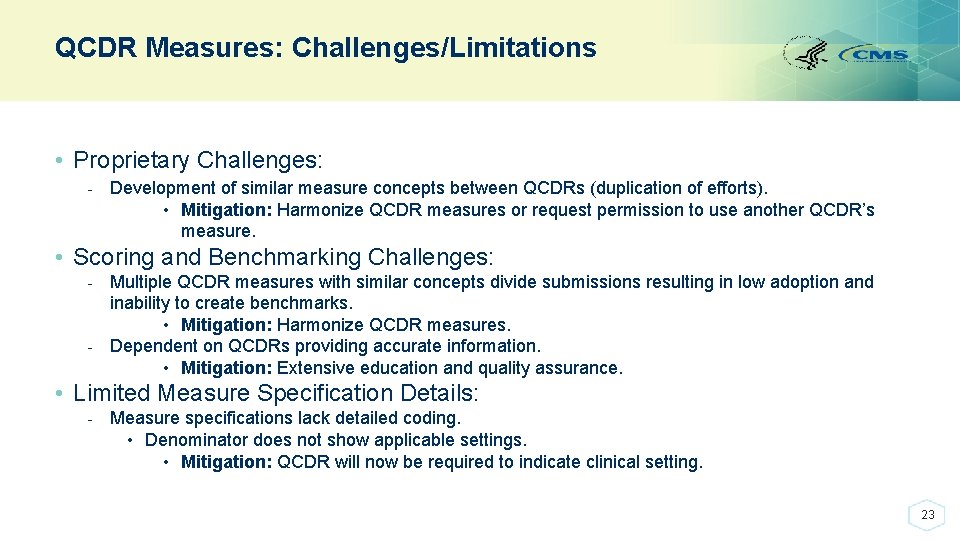
QCDR Measures: Challenges/Limitations • Proprietary Challenges: - Development of similar measure concepts between QCDRs (duplication of efforts). • Mitigation: Harmonize QCDR measures or request permission to use another QCDR’s measure. • Scoring and Benchmarking Challenges: - Multiple QCDR measures with similar concepts divide submissions resulting in low adoption and inability to create benchmarks. • Mitigation: Harmonize QCDR measures. - Dependent on QCDRs providing accurate information. • Mitigation: Extensive education and quality assurance. • Limited Measure Specification Details: - Measure specifications lack detailed coding. • Denominator does not show applicable settings. • Mitigation: QCDR will now be required to indicate clinical setting. 23
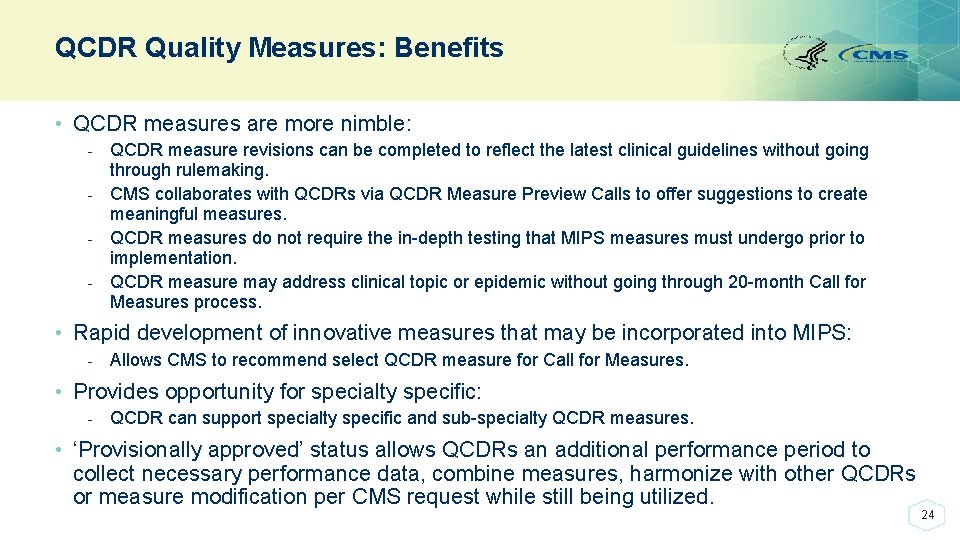
QCDR Quality Measures: Benefits • QCDR measures are more nimble: - QCDR measure revisions can be completed to reflect the latest clinical guidelines without going through rulemaking. - CMS collaborates with QCDRs via QCDR Measure Preview Calls to offer suggestions to create meaningful measures. - QCDR measures do not require the in-depth testing that MIPS measures must undergo prior to implementation. - QCDR measure may address clinical topic or epidemic without going through 20 -month Call for Measures process. • Rapid development of innovative measures that may be incorporated into MIPS: - Allows CMS to recommend select QCDR measure for Call for Measures. • Provides opportunity for specialty specific: - QCDR can support specialty specific and sub-specialty QCDR measures. • ‘Provisionally approved’ status allows QCDRs an additional performance period to collect necessary performance data, combine measures, harmonize with other QCDRs or measure modification per CMS request while still being utilized. 24

PUBLIC REPORTING ON PHYSICIAN COMPARE 25
Public Reporting on Physician Compare • The 2017 Quality Payment Program performance data was available for preview in late 2018 and will be publicly reported on Physician Compare in July 2019. - This includes MIPS and QCDR quality measures, and CAHPS for MIPS summary survey measures; advancing care information attestations and measures; and performance category and final scores. • Data must meet the established public reporting requirements to be included on Physician Compare. Data must be statistically valid, reliable, and accurate; be comparable across submission mechanisms; and meet the minimum reliability threshold. - To be included on the public-facing profile pages, data must also resonate with patients and caregivers, as shown through user testing. 26
Public Reporting on Physician Compare • The 2019 Quality Payment Program performance data will be available for public reporting on Physician Compare in late 2020. This includes MIPS, APMs and other information as required by the MACRA. • For more information, visit the Physician Compare CMS website: https: //www. cms. gov/medicare/quality-initiatives-patient-assessmentinstruments/physician-compare-initiative/ 27
Additional Materials and Support Rule Making and Call for Measures Information: • https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/Quality. Measures/Pre-Rule-Making. html 2019 Call for Quality Measures Resource Materials: • https: //qpp. cms. gov/about/resource-library General Questions • Contact the Quality Payment Program Service Center by: - Email: qpp@cms. hhs. gov - Phone: 1 -866 -288 -8292 (TTY: 1 -877 -715 -6222) 28

29