Lymphatic System and Lymphoid Organs and Tissues Lymphatic










- Slides: 131
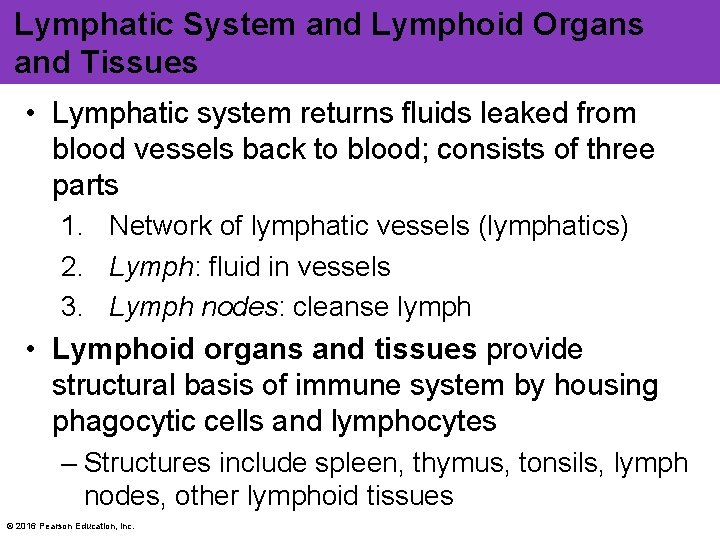
Lymphatic System and Lymphoid Organs and Tissues • Lymphatic system returns fluids leaked from blood vessels back to blood; consists of three parts 1. Network of lymphatic vessels (lymphatics) 2. Lymph: fluid in vessels 3. Lymph nodes: cleanse lymph • Lymphoid organs and tissues provide structural basis of immune system by housing phagocytic cells and lymphocytes – Structures include spleen, thymus, tonsils, lymph nodes, other lymphoid tissues © 2016 Pearson Education, Inc.
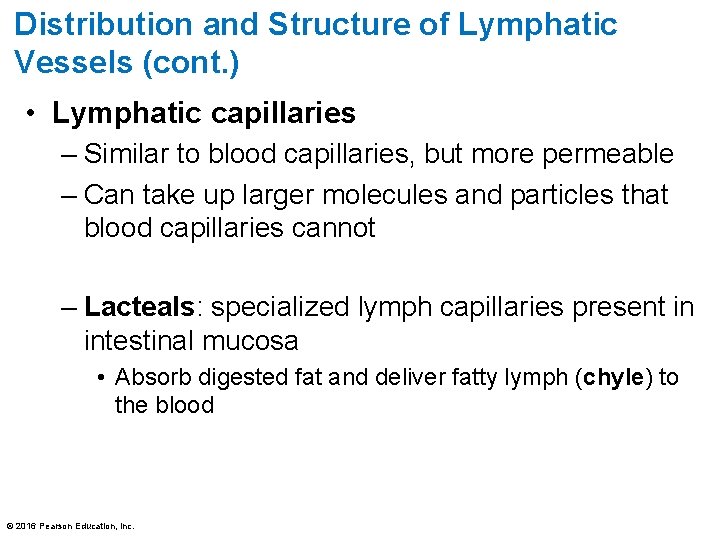
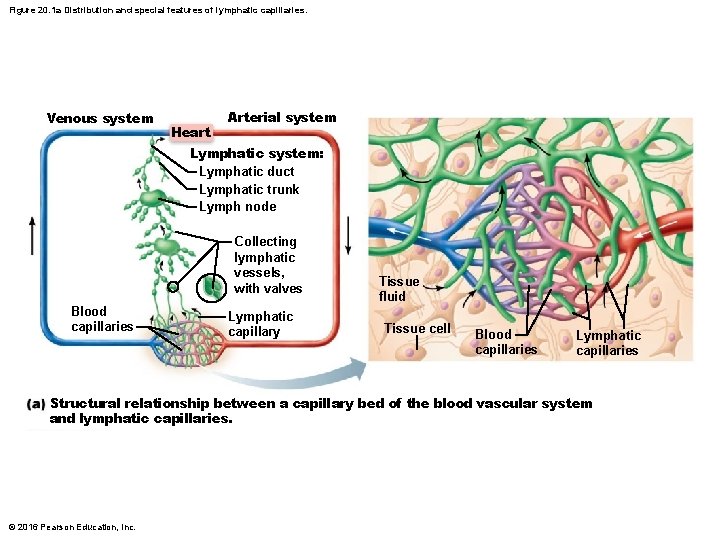
Distribution and Structure of Lymphatic Vessels (cont. ) • Lymphatic capillaries – Similar to blood capillaries, but more permeable – Can take up larger molecules and particles that blood capillaries cannot – Lacteals: specialized lymph capillaries present in intestinal mucosa • Absorb digested fat and deliver fatty lymph (chyle) to the blood © 2016 Pearson Education, Inc.
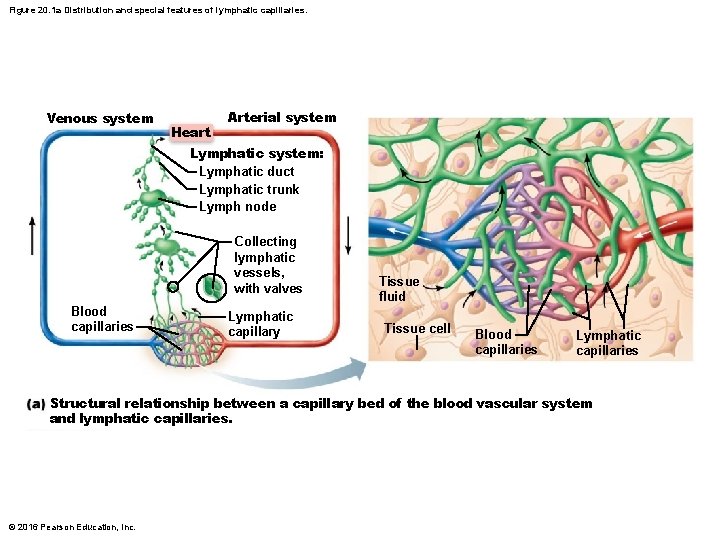
Figure 20. 1 a Distribution and special features of lymphatic capillaries. Venous system Heart Arterial system Lymphatic system: Lymphatic duct Lymphatic trunk Lymph node Collecting lymphatic vessels, with valves Blood capillaries Lymphatic capillary Tissue fluid Tissue cell Blood capillaries Lymphatic capillaries Structural relationship between a capillary bed of the blood vascular system and lymphatic capillaries. © 2016 Pearson Education, Inc.
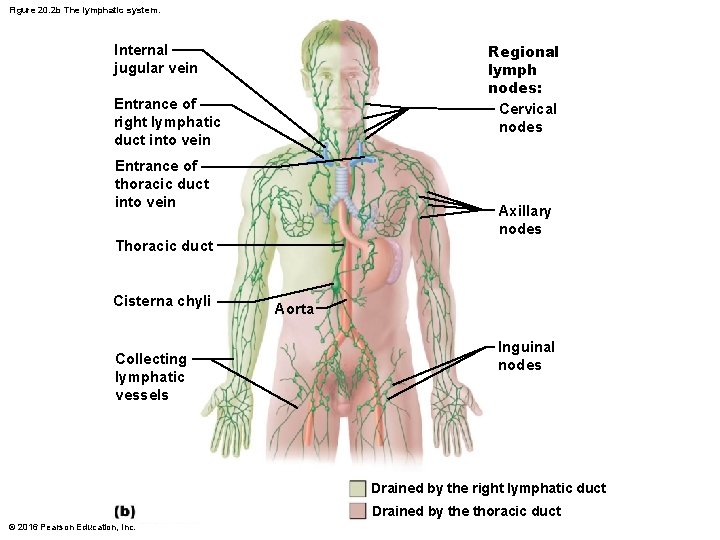
Distribution and Structure of Lymphatic Vessels (cont. ) • Larger lymphatic vessels – Lymph capillaries drain into increasingly larger vessels called collecting lymphatic vessels – Lymphatic trunks, which are formed by union of largest collecting vessels, drain large areas of body and empty into one of two large lymphatic ducts • Each duct empties lymph into venous circulation at junction of internal jugular and subclavian veins on its own side of body © 2016 Pearson Education, Inc.
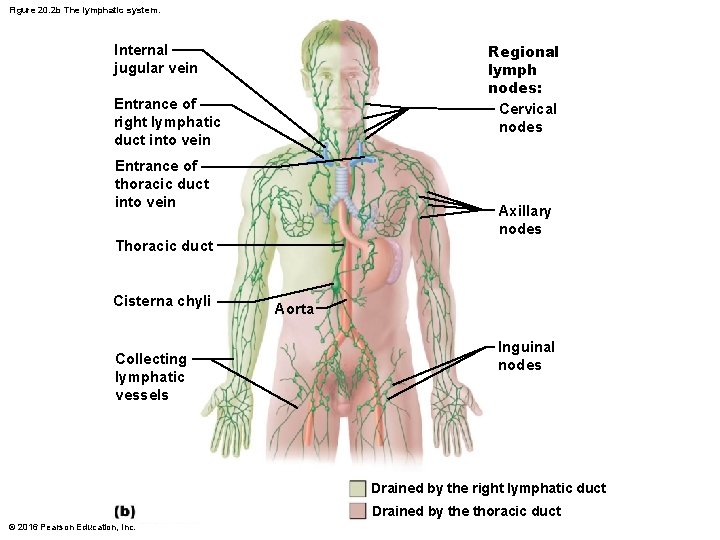
Figure 20. 2 b The lymphatic system. Regional lymph nodes: Cervical nodes Internal jugular vein Entrance of right lymphatic duct into vein Entrance of thoracic duct into vein Axillary nodes Thoracic duct Cisterna chyli Collecting lymphatic vessels ` Aorta Inguinal nodes Drained by the right lymphatic duct Drained by the thoracic duct © 2016 Pearson Education, Inc.
Lymph Transport • Lymph system is a low-pressure system like venous system • Lymph is propelled by: – Milking action of skeletal muscle – Pressure changes in thorax during breathing – Valves to prevent backflow – Pulsations of nearby arteries – Contractions of smooth muscle in walls of lymphatics © 2016 Pearson Education, Inc.
20. 2 Lymphoid Cells, Tissues, and Organs Lymphoid Cells • Lymphoid cells consist of • (1) immune system cells found in lymphoid tissue and • (2) supporting cells that form lymphoid tissue structures © 2016 Pearson Education, Inc.
Immune system cells T cells and B cells protect against antigens (anything the body perceives as foreign) • T cells: manage immune response, and some also attack and destroy infected cells • B cells: produce plasma cells, which secrete antibodies • Macrophages phagocytize foreign substances and help activate T cells • Dendritic cells capture antigens and deliver them to lymph nodes; also help activate T cells © 2016 Pearson Education, Inc.
Supporting lymphoid cell • Reticular cells produce reticular fibers called stroma in lymphoid organs – Stroma: network-like support that acts as scaffolding for immune cells © 2016 Pearson Education, Inc.
Lymphoid Tissue • Main functions of lymphoid tissue – Houses and provides proliferation sites for lymphocytes – Offers surveillance vantage points for lymphocytes and macrophages as they filter through lymph • Largely composed of reticular connective tissue, a type of loose connective tissue – Macrophages live on reticular fibers – Spaces between fibers offer a place for lymphocytes to occupy when they return from patrolling body © 2016 Pearson Education, Inc.
Two main types of lymphoid tissues 1. Diffuse lymphoid tissue: loose arrangement of lymphoid cells and some reticular fibers • Found in virtually every body organ • Larger collections in lamina propria of mucous membranes 2. Lymphoid follicles (nodules): solid, spherical bodies consisting of tightly packed lymphoid cells and reticular fibers • Contain germinal centers of proliferating B cells • May form part of larger lymphoid organs (nodes) • Isolated aggregations of Peyer’s patches and in appendix © 2016 Pearson Education, Inc.

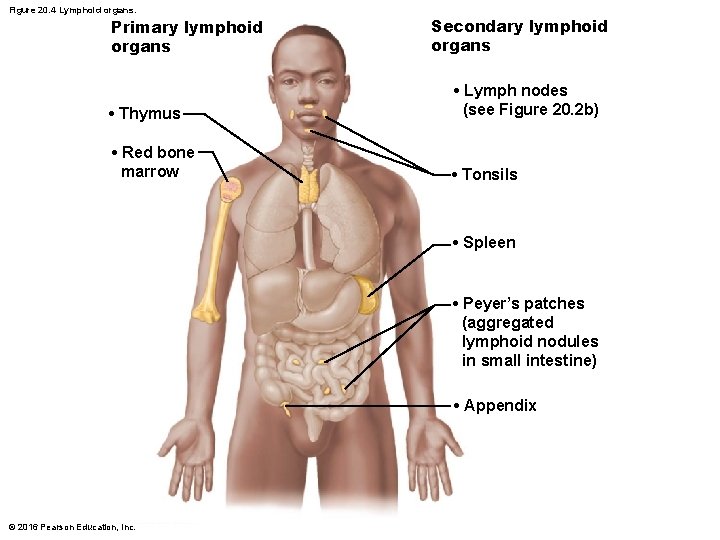
Lymphoid organs are grouped into two functional categories – Primary lymphoid organs: areas where T and B cells mature—red bone marrow and thymus • T and B cells originate in bone marrow, but only B cells matures there; T cells mature in thymus – Secondary lymphoid organs: areas where mature lymphocytes first encounter their antigen and become activated • Nodes, spleen, MALT (mucosa-associated lymphoid tissue) and diffuse lymphoid tissues © 2016 Pearson Education, Inc.
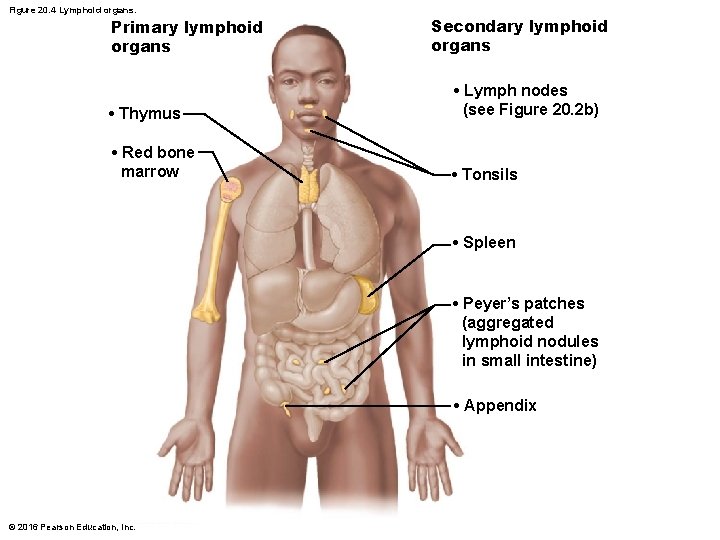
Figure 20. 4 Lymphoid organs. Primary lymphoid organs Secondary lymphoid organs • Thymus • Lymph nodes (see Figure 20. 2 b) • Red bone marrow • Tonsils • Spleen • Peyer’s patches (aggregated lymphoid nodules in small intestine) • Appendix © 2016 Pearson Education, Inc.
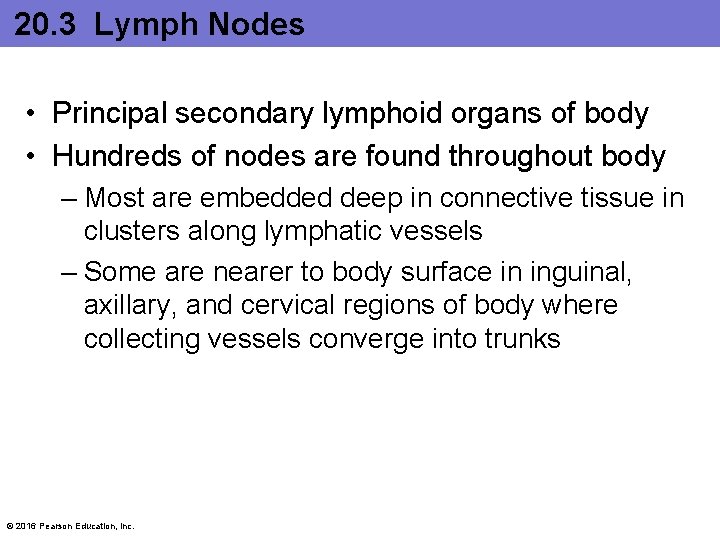
20. 3 Lymph Nodes • Principal secondary lymphoid organs of body • Hundreds of nodes are found throughout body – Most are embedded deep in connective tissue in clusters along lymphatic vessels – Some are nearer to body surface in inguinal, axillary, and cervical regions of body where collecting vessels converge into trunks © 2016 Pearson Education, Inc.

Figure 20. 2 b The lymphatic system. Regional lymph nodes: Cervical nodes Internal jugular vein Entrance of right lymphatic duct into vein Entrance of thoracic duct into vein Axillary nodes Thoracic duct Cisterna chyli Collecting lymphatic vessels ` Aorta Inguinal nodes Drained by the right lymphatic duct Drained by the thoracic duct © 2016 Pearson Education, Inc.
20. 3 Lymph Nodes (cont. ) • Two main functions of lymph nodes 1. Cleansing the lymph: act as lymph “filters” • Macrophages remove and destroy microorganisms and debris that enter lymph – Prevent unwanted substances from being delivered to blood 2. Immune system activation: offer a place for lymphocytes to become activated and mount an attack against antigens © 2016 Pearson Education, Inc.
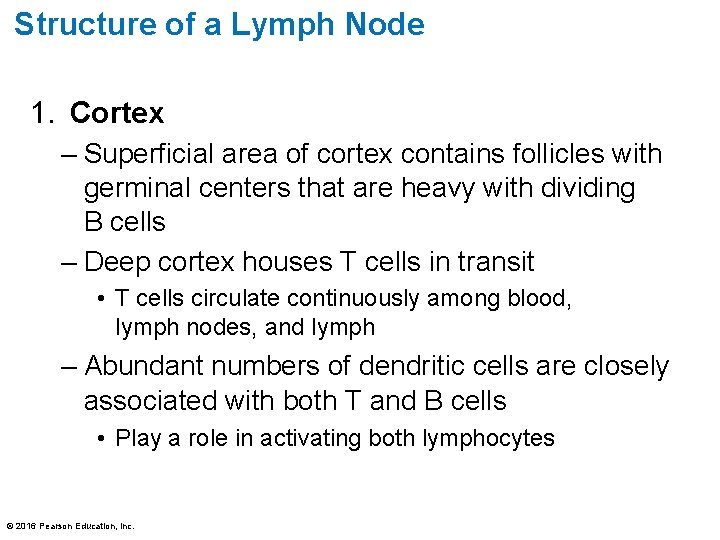
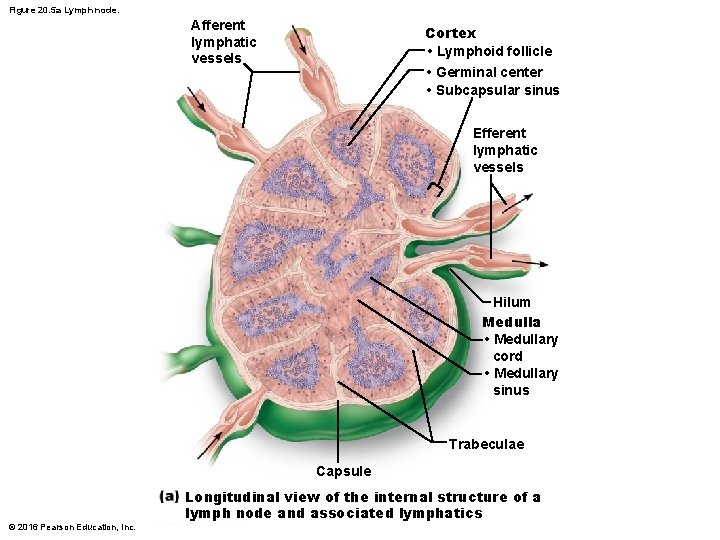
Structure of a Lymph Node 1. Cortex – Superficial area of cortex contains follicles with germinal centers that are heavy with dividing B cells – Deep cortex houses T cells in transit • T cells circulate continuously among blood, lymph nodes, and lymph – Abundant numbers of dendritic cells are closely associated with both T and B cells • Play a role in activating both lymphocytes © 2016 Pearson Education, Inc.
Structure of a Lymph Node 2. Medulla – Medullary cords extend inward from cortex and contain B cells, T cells, and plasma cells • Lymph sinuses are found throughout node – Consist of large lymphatic capillaries spanned by crisscrossing reticular fibers – Macrophages reside on fibers, checking for and phagocytizing any foreign matter © 2016 Pearson Education, Inc.
Circulation in the Lymph Nodes • Lymph enters convex side of node via afferent lymphatic vessels • Travels through large subcapsular sinus and then into smaller sinuses found throughout cortex and medulla • Lymph then enters medullary sinuses • Finally exits concave side at hilum via efferent lymphatic vessels – Presence of fewer efferent vessels causes flow to somewhat stagnate; allows lymphocytes and macrophages time to function – Lymph travels through several nodes © 2016 Pearson Education, Inc.
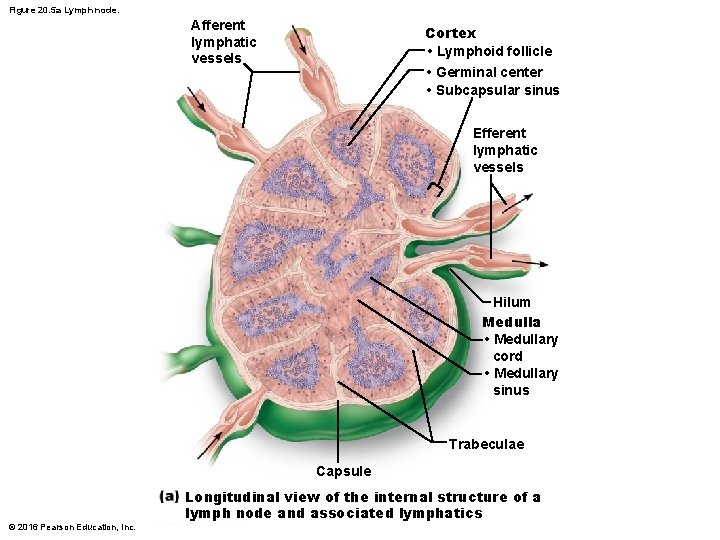
Figure 20. 5 a Lymph node. Afferent lymphatic vessels Cortex • Lymphoid follicle • Germinal center • Subcapsular sinus Efferent lymphatic vessels ` Hilum Medulla • Medullary cord • Medullary sinus Trabeculae Capsule © 2016 Pearson Education, Inc. Longitudinal view of the internal structure of a lymph node and associated lymphatics
20. 4 Spleen • Largest lymphoid organ • Functions – Site of lymphocyte proliferation and immune surveillance and response – Cleanses blood of aged blood cells and platelets; macrophages remove debris © 2016 Pearson Education, Inc.
20. 4 Spleen • Three additional functions of spleen: 1. Stores breakdown products of RBCs (e. g. , iron) for later reuse 2. Stores blood platelets and monocytes for release into blood when needed 3. May be site of fetal erythrocyte production • Histologically, consists of two components 1. White pulp 2. Red pulp © 2016 Pearson Education, Inc.
20. 4 Spleen 1. White pulp: site where immune function occurs • Contains mostly lymphocytes on reticular fibers 2. Red pulp: site where old blood cells and bloodborne pathogens are destroyed © 2016 Pearson Education, Inc.
20. 5 MALT • Mucosa-associated lymphoid tissue (MALT) – Lymphoid tissues in mucous membranes throughout body • Protects from pathogens trying to enter body • Found in mucosa of respiratory tract, genitourinary organs, and digestive tract; largest collections of MALT found in – Tonsils – Peyer’s patches – Appendix © 2016 Pearson Education, Inc.
Tonsils • Simplest lymphoid organs • Form ring of lymphatic tissue around pharynx; appear as swellings of mucosa • Named according to location © 2016 Pearson Education, Inc.

Figure 20. 7 Histology of the palatine tonsil. Pharyngeal tonsil Palatine tonsil Lingual tonsil Germinal centers in lymphoid follicles © 2016 Pearson Education, Inc. Tonsillar crypt
Tonsils • Tonsils function is to gather and remove pathogens in food or air • Contain follicles with germinal centers and scattered lymphocytes • Are not fully encapsulated • Overlying epithelium invaginates, forming tonsillar crypts – Bacteria or particulate matter enters crypts, where they are trapped and destroyed • Risky to lure bacteria into tissues, but allows immune cells to become activated and build memory cells against these potential pathogens © 2016 Pearson Education, Inc.
Peyer’s Patches • Peyer’s patches: clusters of lymphoid follicles in wall of distal portion of small intestine – Also called aggregated lymphoid nodules • Structurally similar to tonsils • Location aids in functions 1. Destroy bacteria, preventing them from breaching intestinal wall 2. Generate “memory” lymphocytes © 2016 Pearson Education, Inc.
Appendix • Appendix: offshoot of first part of large intestine • Contains a large number of lymphoid follicles • Location aids in functions (like Peyer’s patches) 1. Destroy bacteria, preventing them from breaching intestinal wall 2. Generate “memory” lymphocytes © 2016 Pearson Education, Inc.
20. 6 Thymus • Thymus: Functions as lymphoid organ where T cells mature – Most active and largest in size during childhood – Stops growing during adolescence, then gradually atrophies – Still produces immunocompetent cells, though more slowly © 2016 Pearson Education, Inc.
20. 6 Thymus • Thymus is broken into lobules that contain outer cortex and inner medulla – Cortex contains rapidly dividing lymphocytes (the bulk of thymic cells) and scattered macrophages – Medulla contains fewer lymphocytes and thymic corpuscles • Thymic corpuscles are where regulatory T cells develop – Regulatory T cells: type of T cell that helps to prevent autoimmunity © 2016 Pearson Education, Inc.
20. 6 Thymus • Thymus differs from other lymphoid organs in important ways 1. Has no follicles because it lacks B cells 2. Does not directly fight antigens • Functions strictly in T lymphocyte maturation – Contains blood thymus barrier: keeps immature T lymphocytes isolated from any antigens to prevent premature activation 3. Stroma is made up of epithelial cells, not reticular fibers • Provide environment in which T lymphocytes become immunocompetent © 2016 Pearson Education, Inc.
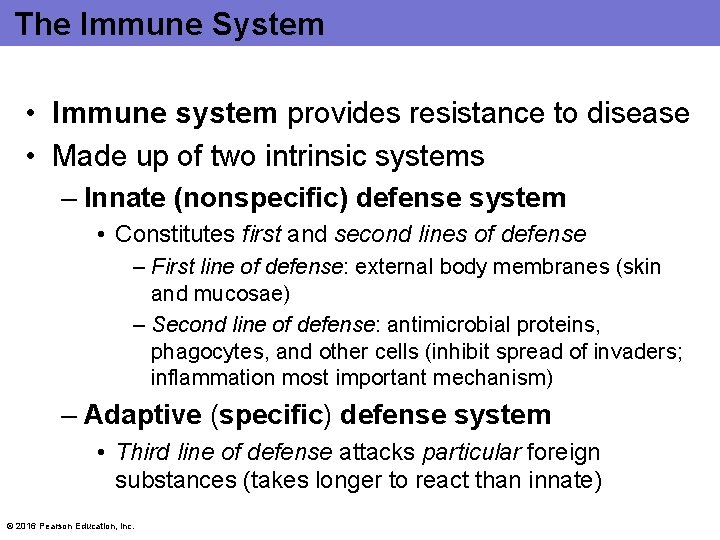
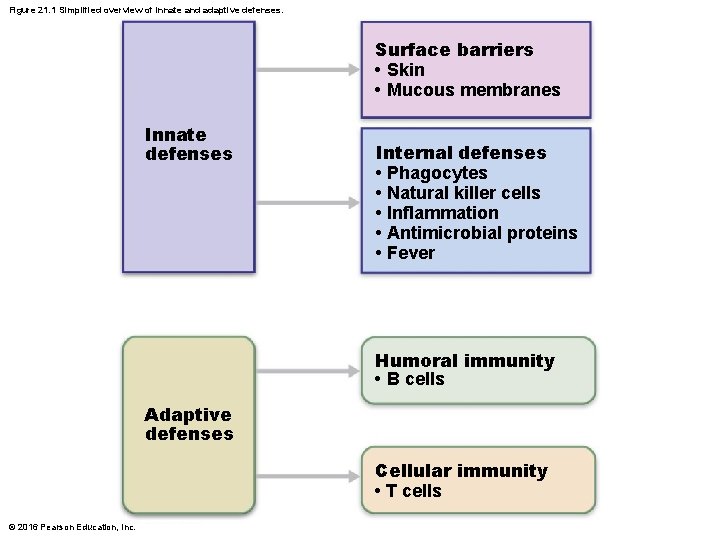
The Immune System • Immune system provides resistance to disease • Made up of two intrinsic systems – Innate (nonspecific) defense system • Constitutes first and second lines of defense – First line of defense: external body membranes (skin and mucosae) – Second line of defense: antimicrobial proteins, phagocytes, and other cells (inhibit spread of invaders; inflammation most important mechanism) – Adaptive (specific) defense system • Third line of defense attacks particular foreign substances (takes longer to react than innate) © 2016 Pearson Education, Inc.
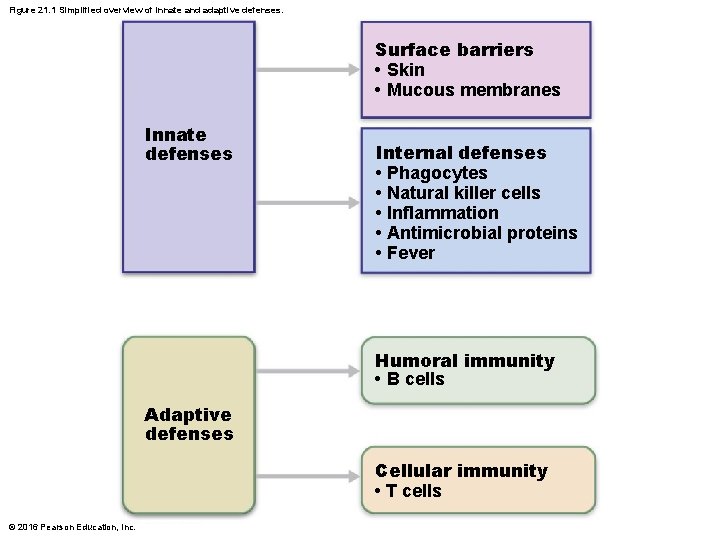
Figure 21. 1 Simplified overview of innate and adaptive defenses. Surface barriers • Skin • Mucous membranes Innate defenses Internal defenses • Phagocytes • Natural killer cells • Inflammation • Antimicrobial proteins • Fever Humoral immunity • B cells Adaptive defenses Cellular immunity • T cells © 2016 Pearson Education, Inc.
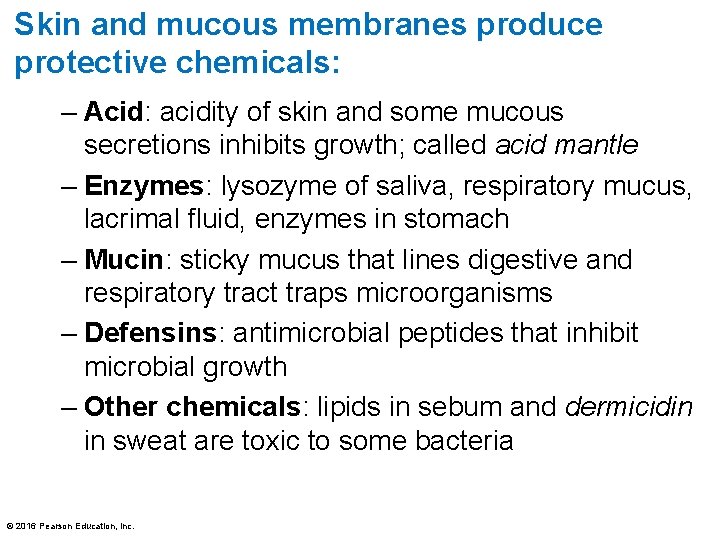
Skin and mucous membranes produce protective chemicals: – Acid: acidity of skin and some mucous secretions inhibits growth; called acid mantle – Enzymes: lysozyme of saliva, respiratory mucus, lacrimal fluid, enzymes in stomach – Mucin: sticky mucus that lines digestive and respiratory tract traps microorganisms – Defensins: antimicrobial peptides that inhibit microbial growth – Other chemicals: lipids in sebum and dermicidin in sweat are toxic to some bacteria © 2016 Pearson Education, Inc.
21. 1 First Line of Defense: Surface Barriers • Respiratory system also has modifications to stop pathogens – Mucus-coated hairs in nose trap inhaled particles – Cilia of upper respiratory tract sweep dust- and bacteria-laden mucus toward mouth • Surface barriers breached by nicks or cuts trigger the internal second line of defense that protects deeper tissues © 2016 Pearson Education, Inc.
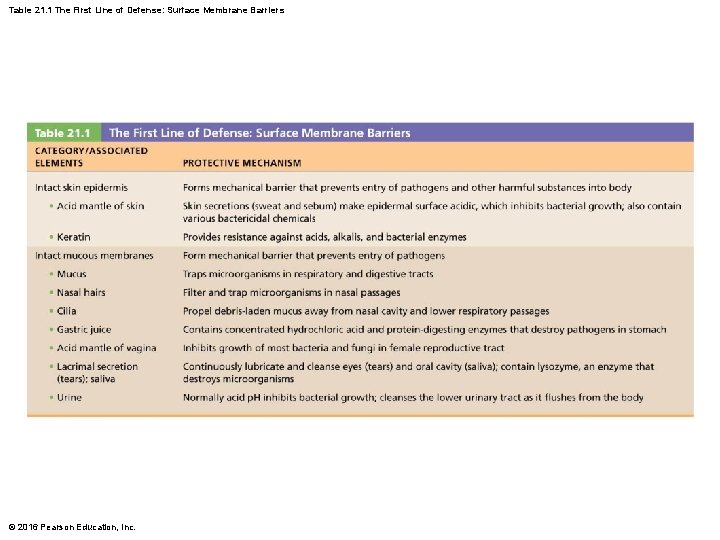
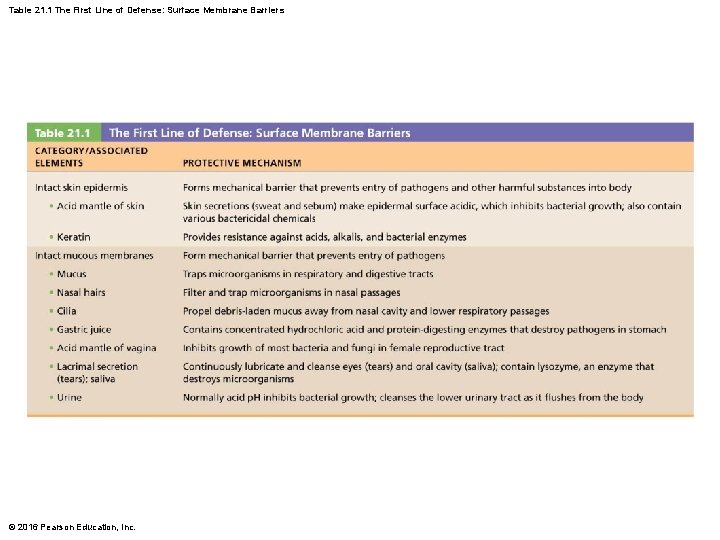
Table 21. 1 The First Line of Defense: Surface Membrane Barriers © 2016 Pearson Education, Inc.
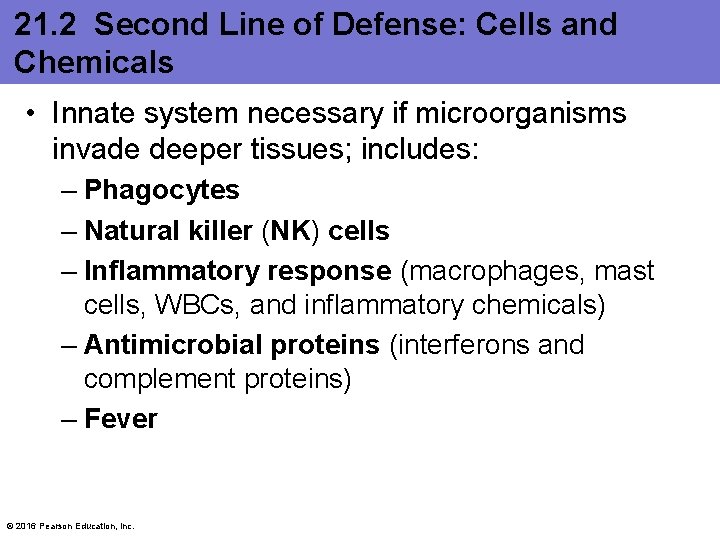
21. 2 Second Line of Defense: Cells and Chemicals • Innate system necessary if microorganisms invade deeper tissues; includes: – Phagocytes – Natural killer (NK) cells – Inflammatory response (macrophages, mast cells, WBCs, and inflammatory chemicals) – Antimicrobial proteins (interferons and complement proteins) – Fever © 2016 Pearson Education, Inc.
Phagocytes • Phagocytes: white blood cells that ingest and digest (eat) foreign invaders • Neutrophils: most abundant phagocytes, but die fighting; become phagocytic on exposure to infectious material © 2016 Pearson Education, Inc.
Phagocytes (cont. ) • Macrophages: develop from monocytes and are chief phagocytic cells; most robust phagocytic cell – Free macrophages: wander through tissue spaces; example: alveolar macrophages – Fixed macrophages: permanent residents of some organs; examples: stellate macrophages (liver) and microglia (brain) © 2016 Pearson Education, Inc.
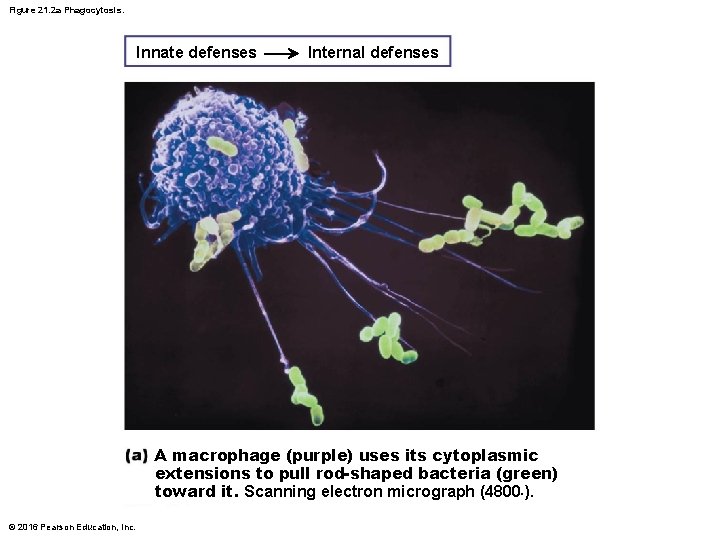
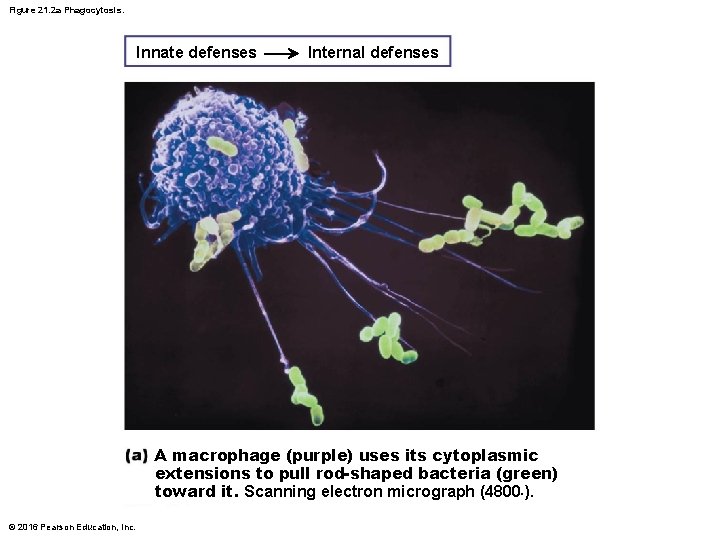
Figure 21. 2 a Phagocytosis. Innate defenses Internal defenses A macrophage (purple) uses its cytoplasmic extensions to pull rod-shaped bacteria (green) toward it. Scanning electron micrograph (4800×). © 2016 Pearson Education, Inc.
Phagocytosis Process starts when phagocyte recognizes and adheres to pathogen’s carbohydrate “signature” • Some microorganisms have external capsules that hide their surface carbohydrates, helping them evade phagocytosis – Opsonization: immune system uses antibodies or complement proteins as opsonins that coat pathogens » Act as “handles” for phagocytes to grab on to, enhancing phagocytosis © 2016 Pearson Education, Inc.
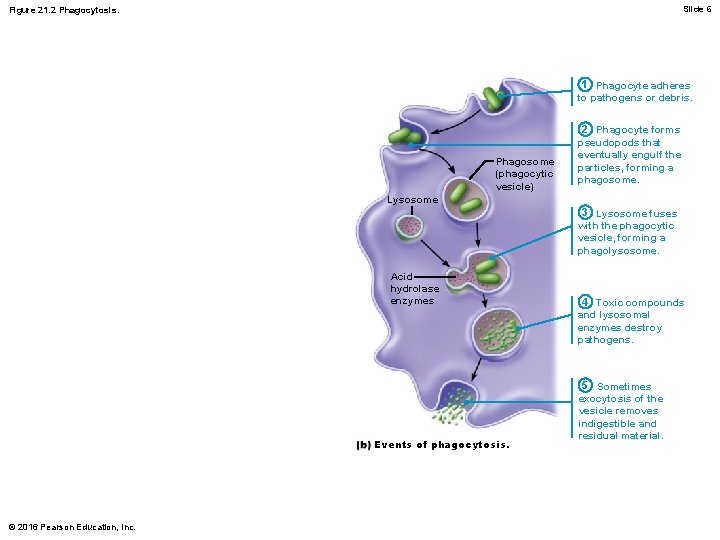
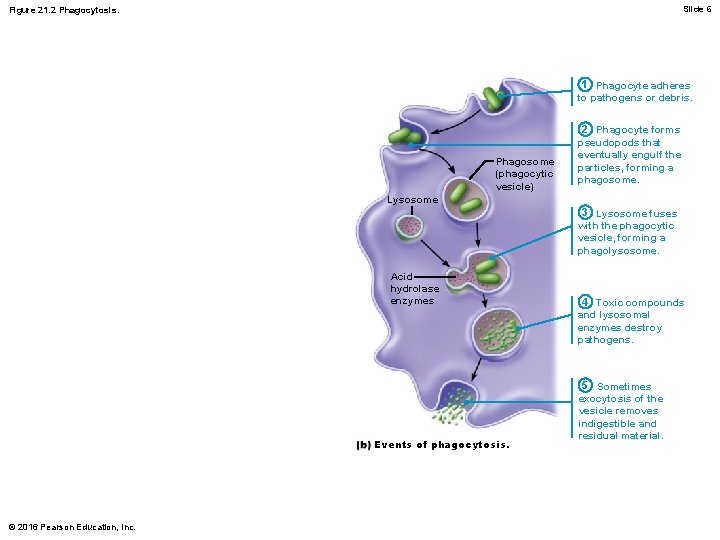
Slide 6 Figure 21. 2 Phagocytosis. 1 Phagocyte adheres to pathogens or debris. Phagosome (phagocytic vesicle) 2 Phagocyte forms pseudopods that eventually engulf the particles, forming a phagosome. Lysosome 3 Lysosome fuses with the phagocytic vesicle, forming a phagolysosome. Acid hydrolase enzymes Events of phagocytosis. © 2016 Pearson Education, Inc. 4 Toxic compounds and lysosomal enzymes destroy pathogens. 5 Sometimes exocytosis of the vesicle removes indigestible and residual material.
Phagocytes (cont. ) • Phagocytosis (cont. ) – Some pathogens are not killed with acidified lysosomal enzymes (e. g. , tuberculosis bacteria) • Helper T cells trigger macrophage to produce respiratory burst, which kills pathogens resistant to lysosomal enzymes by: – Releasing cell-killing free radicals – Producing oxidizing chemicals (e. g. , H 2 O 2) – Increasing p. H and osmolarity of phagolysosome – Defensins (in neutrophils) also help by piercing membrane of pathogen © 2016 Pearson Education, Inc.
Natural Killer (NK) Cells • Nonphagocytic, large granular lymphocytes that police blood and lymph – Can kill cancer and virus-infected cells before adaptive immune system is activated • Attack cells that lack “self” cell-surface receptors • Kill by inducing apoptosis in cancer cells and virus-infected cells • Secrete potent chemicals that enhance inflammatory response © 2016 Pearson Education, Inc.
Inflammation: Tissue Response to Injury • Inflammation is triggered whenever body tissues are injured – Injuries can be due to trauma, heat, irritating chemicals, or infections by microorganisms • Benefits of inflammation: – Prevents spread of damaging agents – Disposes of cell debris and pathogens – Alerts adaptive immune system – Sets the stage for repair © 2016 Pearson Education, Inc.
Inflammation: Tissue Response to Injury (cont. ) • Four cardinal signs of acute inflammation: 1. Redness 2. Heat 3. Swelling 4. Pain – Sometimes a fifth sign, impairment of function, is seen if movement or use of area is hampered © 2016 Pearson Education, Inc.
Inflammatory chemical release – Chemicals are released into ECF by injured tissues, immune cells, or blood proteins • Example: histamine released by mast cells is key inflammatory chemical – Macrophages and epithelial cells of boundary tissues (respiratory tissues, intestine) bear special pattern recognition receptors called “Tolllike receptors” (TLRs) • Activated TLRs trigger release of cytokines that promote inflammation © 2016 Pearson Education, Inc.
Other inflammatory mediators Kinins, prostaglandins (PGs), and complement • • All cause vasodilation of local arterioles All make capillaries leaky Many attract leukocytes to area Some have other inflammatory roles, such as triggering pain receptors, or prompting release of more inflammatory chemicals © 2016 Pearson Education, Inc.
2. Vasodilation and increased vascular permeability – Vasodilation causes hyperemia—congestion with blood—which leads to redness and heat – Increased capillary permeability causes exudate—fluid containing clotting factors and antibodies—to leak into tissue • Results in local swelling (edema) • Swelling also pushes on nerve endings, resulting in pain © 2016 Pearson Education, Inc.
Vasodilation and increased vascular permeability – Pain can also result from release of toxins from bacteria or released prostaglandins and kinins – Benefits of edema • Surge of fluid in tissue sweeps foreign material into lymphatic vessels for processing in lymph nodes • Delivers clotting proteins and complement to area – Clotting factors form fibrin mesh that acts as scaffold for repair » Mesh also isolates injured area so invaders cannot spread © 2016 Pearson Education, Inc.
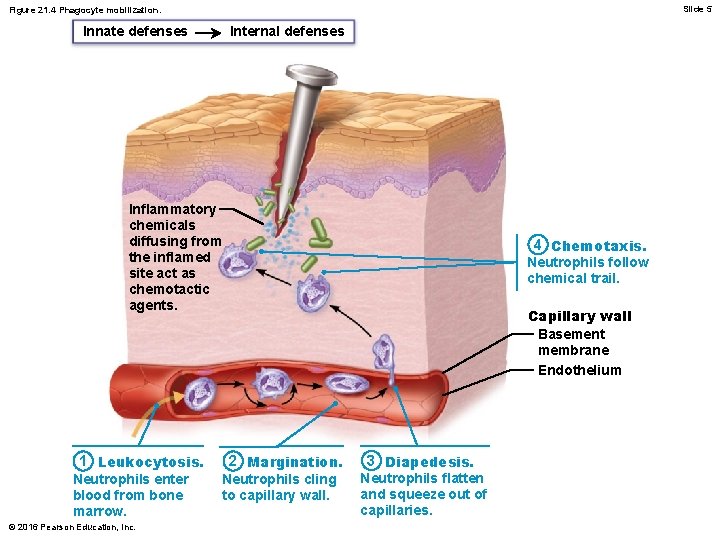
Phagocyte mobilization – Neutrophils flood area first; macrophages follow – If inflammation is due to pathogens, complement is activated; adaptive immunity elements arrive © 2016 Pearson Education, Inc.
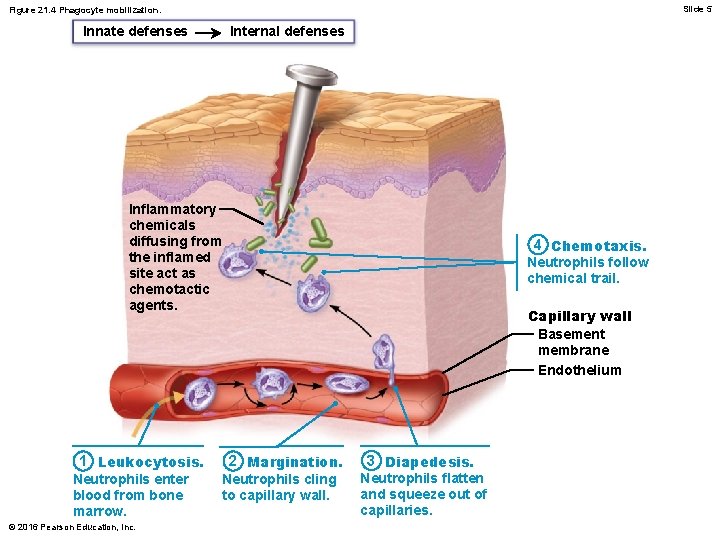
Slide 5 Figure 21. 4 Phagocyte mobilization. Innate defenses Internal defenses Inflammatory chemicals diffusing from the inflamed site act as chemotactic agents. 1 Leukocytosis. Neutrophils enter blood from bone marrow. © 2016 Pearson Education, Inc. 4 Chemotaxis. Neutrophils follow chemical trail. Capillary wall Basement membrane Endothelium 2 Margination. Neutrophils cling to capillary wall. 3 Diapedesis. Neutrophils flatten and squeeze out of capillaries.
Antimicrobial Proteins • Antimicrobial proteins enhance innate defense by: – Attacking microorganisms directly, or – Hindering microorganisms’ ability to reproduce • Most important antimicrobial proteins – Interferons – Complement proteins © 2016 Pearson Education, Inc.
Interferons – Interferons (IFN): family of immune modulating proteins – Cells infected with viruses can secrete IFNs that “warn” healthy neighboring cells • IFNs enter neighboring cells, stimulating production of proteins that block viral reproduction and degrade viral RNA – IFNs activate NK cells and macrophages, so they indirectly fight cancer – Artificial IFNs are used to treat disorders such as hepatitis C, genital warts, and multiple sclerosis © 2016 Pearson Education, Inc.

Slide 6 Figure 21. 5 The interferon mechanism against viruses. Internal defenses Innate defenses Virus Viral nucleic acid 1 Virus enters cell. New viruses 5 Antiviral proteins block viral reproduction. 2 Interferon genes switch on. Antiviral m. RNA DNA Nucleus m. RNA for interferon 3 Cell produces interferon molecules. Interferon Host cell 1 Infected by virus; makes interferon; is killed by virus © 2016 Pearson Education, Inc. Interferon receptor 4 Interferon binding stimulates cell to turn on genes for antiviral proteins. Host cell 2 Binds interferon from cell 1; interferon induces synthesis of protective proteins
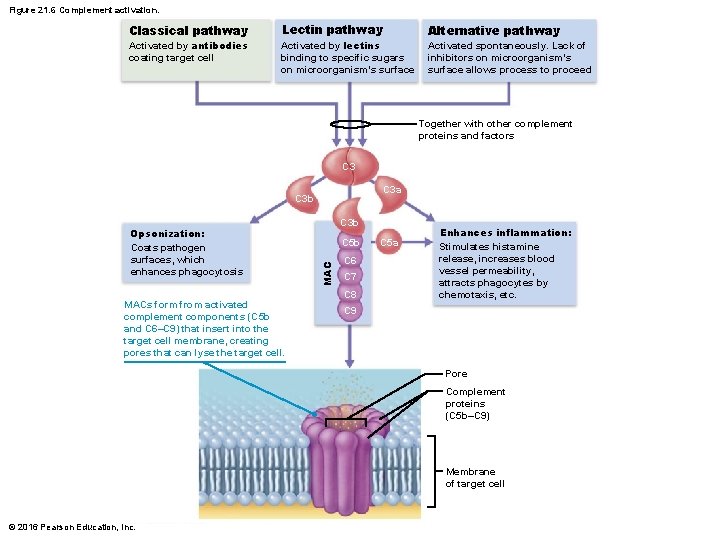
Complement – Provides major mechanism for destroying foreign substances – Activation enhances inflammation and also directly destroys bacteria • Enhances both innate and adaptive defenses © 2016 Pearson Education, Inc.
Activation of complement (3 possibilities) 1. Classical pathway – Antibodies first bind to invading organisms and then bind to complement components, activating them » Double binding called complement fixation – Once initial complement proteins are activated, an activation cascade is triggered © 2016 Pearson Education, Inc.
Activation of complement (3 possibilities) 2. Lectin pathway – Lectins are produced by innate system to recognize foreign invaders – When lectin is bound to specific sugars on foreign invaders, it can also bind activate complement 3. Alternative pathway – Complement cascade is activated spontaneously when certain complement factors bind directly to foreign invader » Lack of inhibitors on microorganism’s surface allows process to proceed © 2016 Pearson Education, Inc.
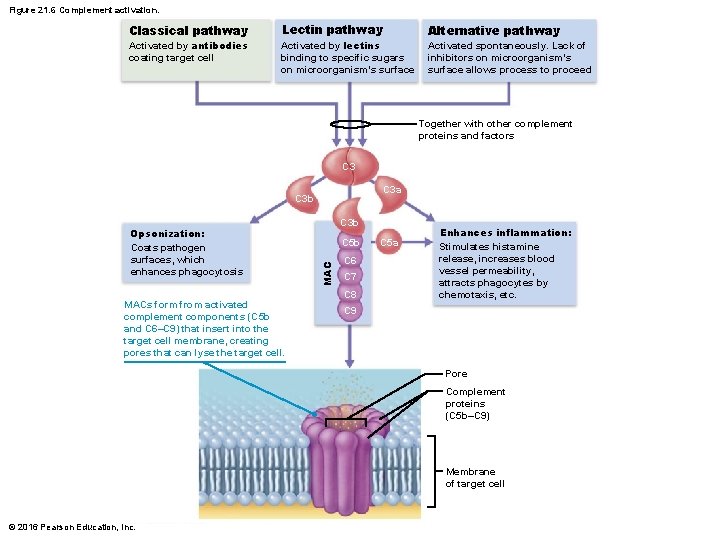
Figure 21. 6 Complement activation. Classical pathway Activated by antibodies coating target cell Lectin pathway Activated by lectins binding to specific sugars on microorganism’s surface Alternative pathway Activated spontaneously. Lack of inhibitors on microorganism’s surface allows process to proceed Together with other complement proteins and factors C 3 a C 3 b MACs form from activated complement components (C 5 b and C 6–C 9) that insert into the target cell membrane, creating pores that can lyse the target cell. C 3 b C 5 b MAC Opsonization: Coats pathogen surfaces, which enhances phagocytosis C 6 C 7 C 8 C 5 a Enhances inflammation: Stimulates histamine release, increases blood vessel permeability, attracts phagocytes by chemotaxis, etc. C 9 Pore Complement proteins (C 5 b–C 9) Membrane of target cell © 2016 Pearson Education, Inc.
Fever – Abnormally high body temperature that is systemic response to invading microorganisms – Leukocytes and macrophages exposed to foreign substances secrete pyrogens – Pyrogens act on body’s thermostat in hypothalamus, raising body temperature – Benefits of moderate fever • Causes liver and spleen to sequester iron and zinc (needed by microorganisms) • Increases metabolic rate, which increases rate of repair © 2016 Pearson Education, Inc.
Adaptive Defenses • Adaptive immune system is a specific defensive system that eliminates almost any pathogen or abnormal cell in body • Activities – Amplifies inflammatory response – Activates complement • Shortcoming: must be primed by initial exposure to specific foreign substance – Priming takes time © 2016 Pearson Education, Inc.
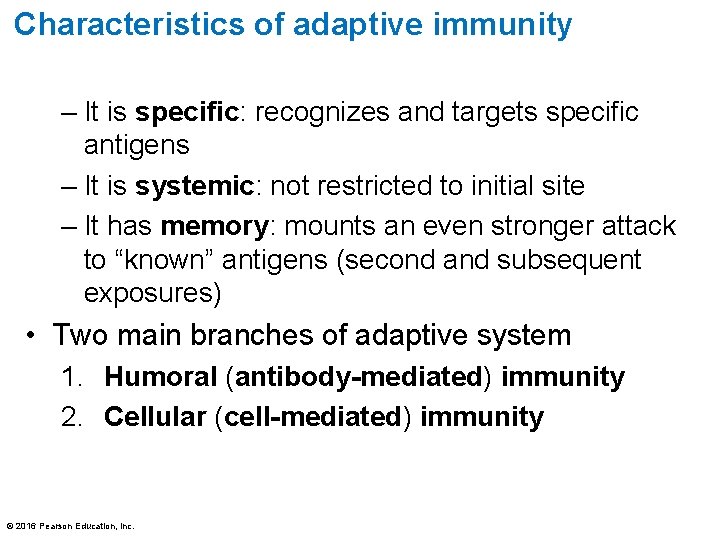
Characteristics of adaptive immunity – It is specific: recognizes and targets specific antigens – It is systemic: not restricted to initial site – It has memory: mounts an even stronger attack to “known” antigens (second and subsequent exposures) • Two main branches of adaptive system 1. Humoral (antibody-mediated) immunity 2. Cellular (cell-mediated) immunity © 2016 Pearson Education, Inc.
Humoral immunity – Antibodies, produced by lymphocytes, circulate freely in body fluids – Bind temporarily to target cell • Temporarily inactivate • Mark for destruction by phagocytes or complement – Humoral immunity has extracellular targets © 2016 Pearson Education, Inc.
Cellular Immunity – Lymphocytes act against target cell • Directly—by killing infected cells • Indirectly—by releasing chemicals that enhance inflammatory response; or activating other lymphocytes or macrophages – Cellular immunity has cellular targets © 2016 Pearson Education, Inc.
Antigens • Antigens: substances that can mobilize adaptive defenses and provoke an immune response • Targets of all adaptive immune responses • Most are large, complex molecules not normally found in body (nonself) © 2016 Pearson Education, Inc.
Complete Antigens • Complete antigens have two important functional properties: – Immunogenicity: ability to stimulate proliferation of specific lymphocytes – Reactivity: ability to react with activated lymphocytes and antibodies released by immunogenic reactions – Examples: foreign proteins, polysaccharides, lipids, and nucleic acids; seen on many foreign invaders such as pollen and microorganisms © 2016 Pearson Education, Inc.
Haptens • Incomplete antigens, also called haptens, involve molecules too small to be seen so are not immunogenic by themselves • May become immunogenic if hapten attaches to body’s own proteins – Combination of protein and hapten is then seen as foreign and causes immune system to mount attack that is harmful to person because it attacks self-proteins as well as hapten – Examples: poison ivy, animal dander, detergents, and cosmetics © 2016 Pearson Education, Inc.

Antigenic Determinants • Antigenic determinants: parts of antigen that antibodies or lymphocyte receptors bind to • Most naturally occurring antigens have numerous antigenic determinants that: – Mobilize several different lymphocyte populations – Form different kinds of antibodies against them • Large, chemically simple molecules (such as plastics) have little or no immunogenicity © 2016 Pearson Education, Inc.
Self-Antigens: MHC Proteins • Self-antigens: all cells are covered with variety of proteins located on surface that are not antigenic to self, but may be antigenic to others in transfusions or grafts • One set of important self-proteins are group of glycoproteins called MHC proteins – Coded by genes of major histocompatibility complex (MHC) and unique to each individual • T lymphocytes can recognize only antigens that are presented on MHC proteins © 2016 Pearson Education, Inc.
Lymphocytes and Antigen-Presenting Cells • Adaptive immune system involves three crucial types of cells – Two types of lymphocytes • B lymphocytes (B cells)—humoral immunity • T lymphocytes (T cells)—cellular immunity – Antigen-presenting cells (APCs) • Do not respond to specific antigens • Play essential auxiliary roles in immunity © 2016 Pearson Education, Inc.
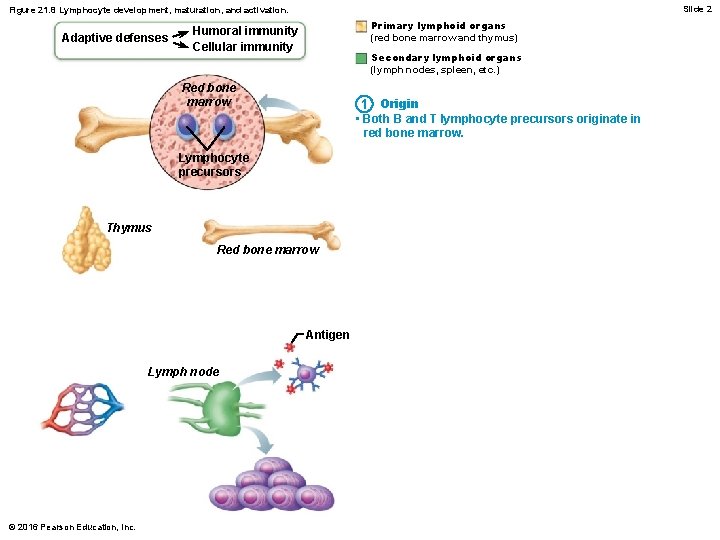
Lymphocytes • Lymphocyte development, maturation, and activation – T and B lymphocytes share common development and steps in their life cycles – Five general steps: 1. Origin: both lymphocytes originate in red bone marrow © 2016 Pearson Education, Inc.
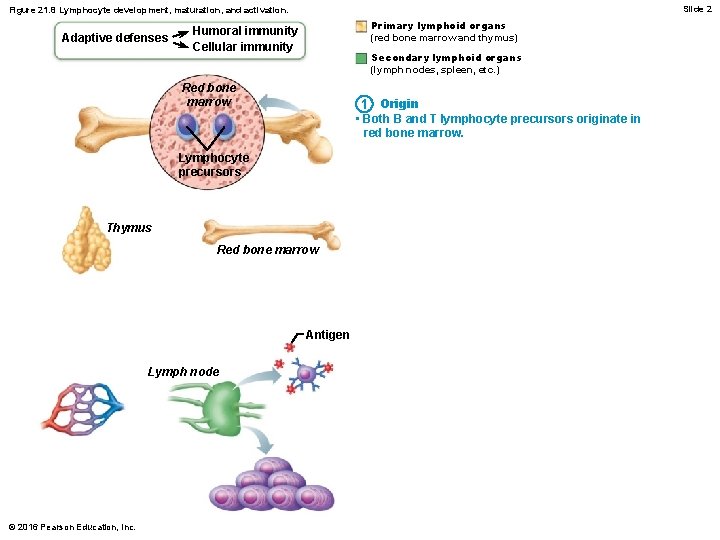
Slide 2 Figure 21. 8 Lymphocyte development, maturation, and activation. Adaptive defenses Primary lymphoid organs (red bone marrow and thymus) Humoral immunity Cellular immunity Secondary lymphoid organs (lymph nodes, spleen, etc. ) Red bone marrow 1 Origin • Both B and T lymphocyte precursors originate in red bone marrow. Lymphocyte precursors Thymus Red bone marrow Antigen Lymph node © 2016 Pearson Education, Inc.
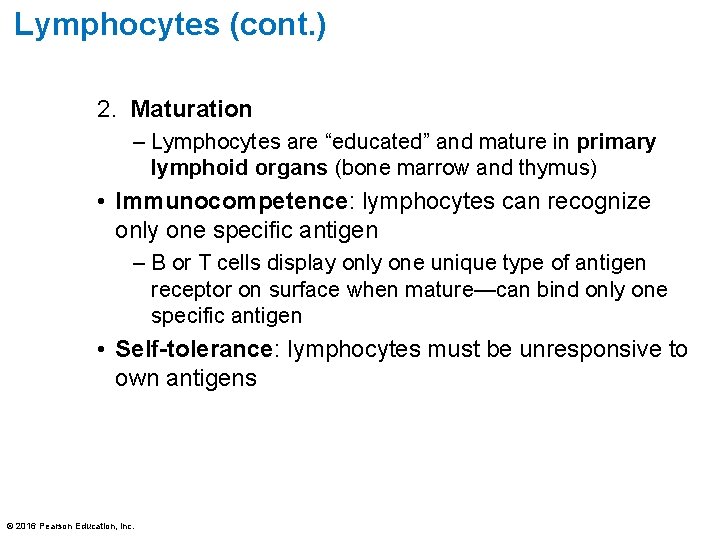
Lymphocytes (cont. ) 2. Maturation – Lymphocytes are “educated” and mature in primary lymphoid organs (bone marrow and thymus) • Immunocompetence: lymphocytes can recognize only one specific antigen – B or T cells display only one unique type of antigen receptor on surface when mature—can bind only one specific antigen • Self-tolerance: lymphocytes must be unresponsive to own antigens © 2016 Pearson Education, Inc.
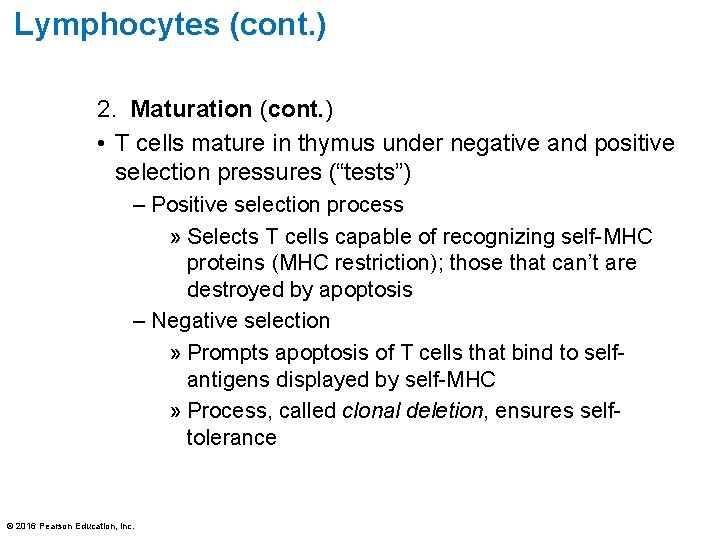
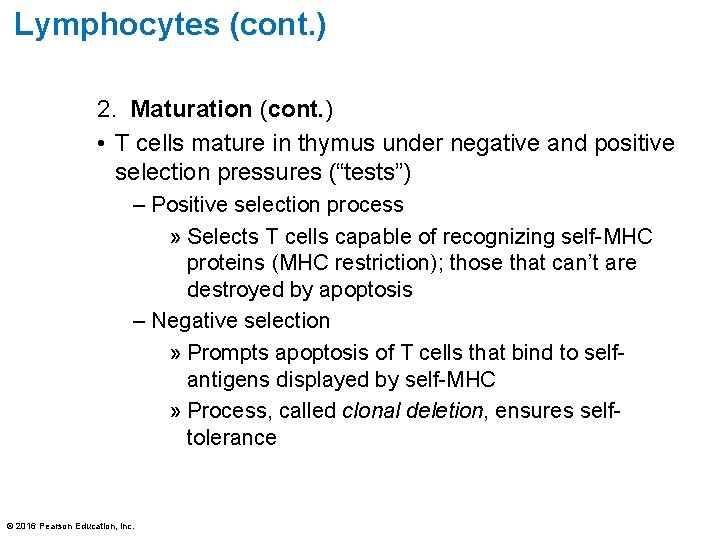
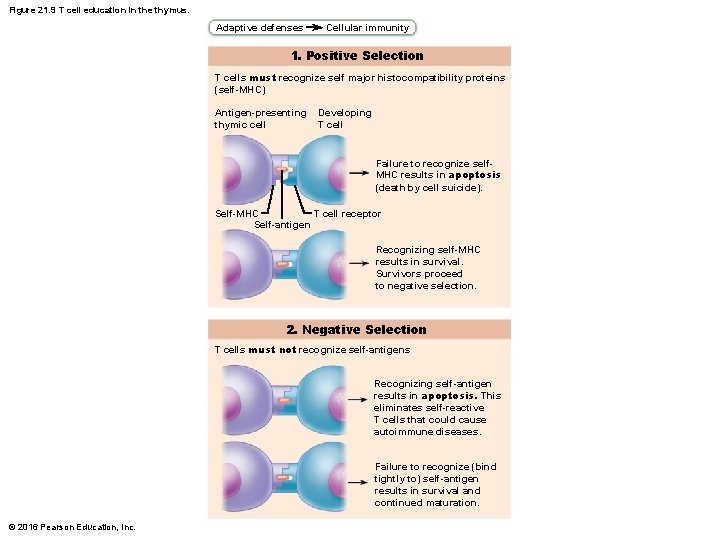
Lymphocytes (cont. ) 2. Maturation (cont. ) • T cells mature in thymus under negative and positive selection pressures (“tests”) – Positive selection process » Selects T cells capable of recognizing self-MHC proteins (MHC restriction); those that can’t are destroyed by apoptosis – Negative selection » Prompts apoptosis of T cells that bind to selfantigens displayed by self-MHC » Process, called clonal deletion, ensures selftolerance © 2016 Pearson Education, Inc.
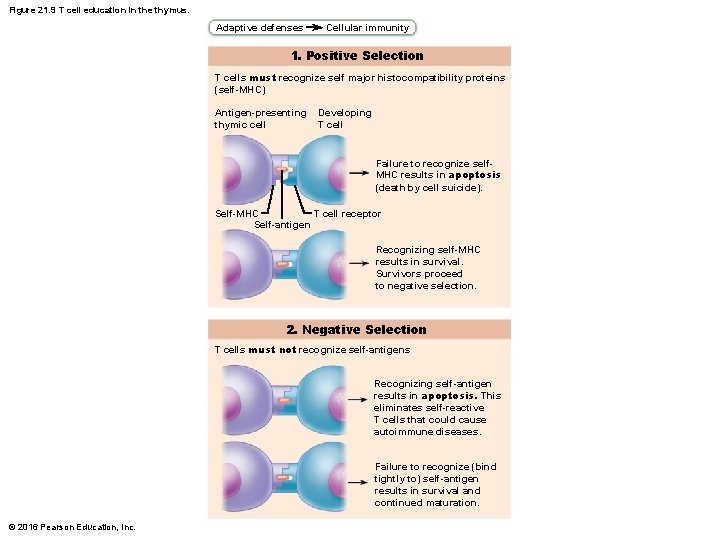
Figure 21. 9 T cell education in the thymus. Adaptive defenses Cellular immunity 1. Positive Selection T cells must recognize self major histocompatibility proteins (self-MHC) Antigen-presenting thymic cell Developing T cell Failure to recognize self. MHC results in apoptosis (death by cell suicide). Self-MHC T cell receptor Self-antigen Recognizing self-MHC results in survival. Survivors proceed to negative selection. 2. Negative Selection T cells must not recognize self-antigens Recognizing self-antigen results in apoptosis. This eliminates self-reactive T cells that could cause autoimmune diseases. Failure to recognize (bind tightly to) self-antigen results in survival and continued maturation. © 2016 Pearson Education, Inc.
Lymphocytes (cont. ) 2. Maturation (cont. ) • B cells mature in red bone marrow – Not as much known about process of B cell maturation – Only immunocompetent B cells are allowed to mature – Those that are self-reactive are eliminated by apoptosis (clonal deletion) © 2016 Pearson Education, Inc.
Lymphocytes (cont. ) 3. Seeding secondary lymphoid organs and circulation • Immunocompetent B and T cells not yet exposed to antigen are called naive • Exported from primary lymphoid organs (bone marrow and thymus) to “seed” secondary lymphoid organs (lymph nodes, spleen, etc. ) – Increases chance of encounter with antigen © 2016 Pearson Education, Inc.
Lymphocytes (cont. ) 4. Antigen encounter and activation • Naive lymphocyte’s first encounter with antigen triggers lymphocyte to develop further • Lymphocyte is selected to differentiate into active cell by binding to its specific antigen – Referred to as clonal selection • If correct signals are present, lymphocyte will complete its differentiation into active cell © 2016 Pearson Education, Inc.
Lymphocytes (cont. ) 5. Proliferation and differentiation • Once selected and activated, lymphocyte proliferates – Forms army of exact copies of itself – Referred to as clones • Most clones become effector cells that fight infections • A few remain as memory cells – Able to respond to same antigen more quickly second time it is encountered • B and T memory cells and effector T cells circulate continuously © 2016 Pearson Education, Inc.

Slide 6 Figure 21. 8 Lymphocyte development, maturation, and activation. Adaptive defenses Primary lymphoid organs (red bone marrow and thymus) Humoral immunity Cellular immunity Secondary lymphoid organs (lymph nodes, spleen, etc. ) Red bone marrow 1 Origin • Both B and T lymphocyte precursors originate in red bone marrow. Lymphocyte precursors 2 Maturation • Lymphocyte precursors destined to become T cells migrate (in blood) to the thymus and mature there. • B cells mature in the bone marrow. • During maturation lymphocytes develop immunocompetence and self-tolerance. Thymus Red bone marrow 3 Seeding secondary lymphoid organs and circulation • Immunocompetent but still naive lymphocytes leave thymus and bone marrow. • They “seed” the secondary lymphoid organs and Antigen circulate through blood and lymph. Lymph node 4 Antigen encounter and activation • When a lymphocyte’s antigen receptors bind its antigen, that lymphocyte can be activated. 5 Proliferation and differentiation • Activated lymphocytes proliferate (multiply) and then differentiate into effector cells and memory cells. • Memory cells and effector T cells circulate continuously in the blood and lymph and throughout the secondary lymphoid organs. © 2016 Pearson Education, Inc.
Antigen-Presenting Cells (APCs) • Engulf antigens and present fragments of antigens to T cells for recognition • Major types – Dendritic cells – Macrophages – B cells © 2016 Pearson Education, Inc.
Antigen-Presenting Cells (APCs) • Dendritic cells – Found in connective tissues and epidermis • Act as mobile sentinels of boundary tissues – Phagocytize pathogens that enter tissues, then enter lymphatics to present antigens to T cells in lymph node • Most effective antigen presenter known • Key link between innate and adaptive immunity © 2016 Pearson Education, Inc.
Antigen-Presenting Cells (APCs) • Macrophages – Widely distributed in connective tissues and lymphoid organs – Present antigens to T cells, which not only activates T cell, but also further activates macrophage • Activated macrophage becomes voracious phagocytic killer • Also trigger powerful inflammatory responses and recruit additional defenses © 2016 Pearson Education, Inc.

Antigen-Presenting Cells (APCs) • B lymphocytes – Do not activate naive T cells – Present antigens to helper T cell to assist their own activation © 2016 Pearson Education, Inc.
21. 5 Humoral Immune Response • When B cell encounters target antigen, it provokes humoral immune response – Antibodies specific for that particular antigen are then produced © 2016 Pearson Education, Inc.
Activation and Differentiation of B Cells • B cells are activated when antigens bind to surface receptors, cross-linking them • Triggers receptor-mediated endocytosis of cross -linked antigen-receptor complexes (clonal selection), leading to proliferation and differentiation of B cell into effector cells © 2016 Pearson Education, Inc.
Activation and Differentiation of B Cells • Most clone cells become plasma cells, antibody -secreting effector cells – Secrete specific antibodies and then die – Antibodies circulate in blood or lymph, binding to free antigens, marking them for destruction by innate or other adaptive mechanisms © 2016 Pearson Education, Inc.

Figure 21. 11 -1 Clonal selection of a B cell. Adaptive defenses Humoral immunity Antigen Primary response (initial encounter with antigen) Activated B cells Plasma cells (effector B cells) Secreted antibody molecules © 2016 Pearson Education, Inc. Proliferation to form a clone Antigen binding to a receptor on a specific B lymphocyte (B lymphocytes with noncomplementary receptors remain inactive) Memory B cell— primed to respond to same antigen
Activation and Differentiation of B Cells (cont. ) • Clone cells that do not become plasma cells become memory cells – Provide immunological memory – Mount an immediate response to future exposures to same antigen © 2016 Pearson Education, Inc.
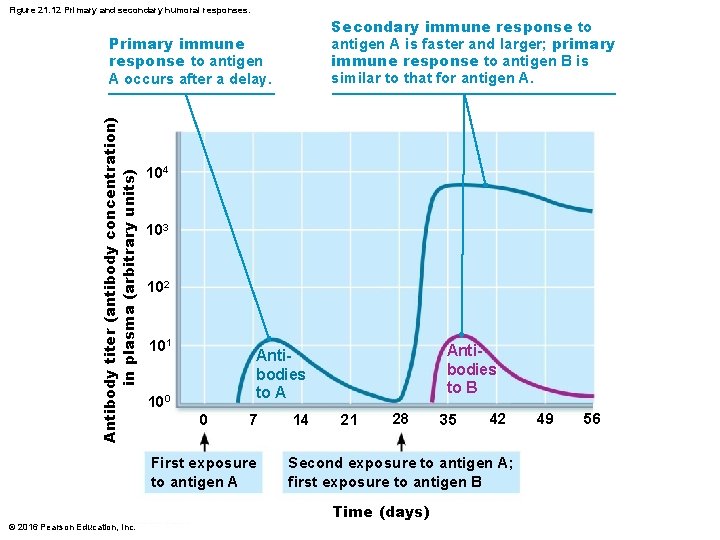
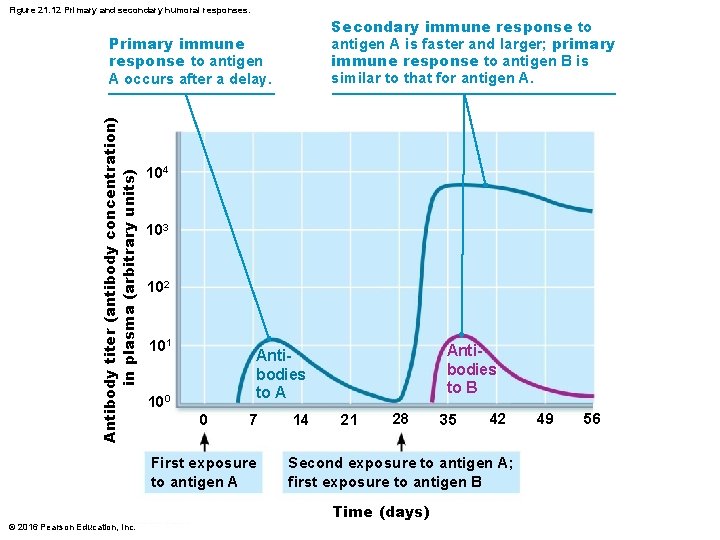
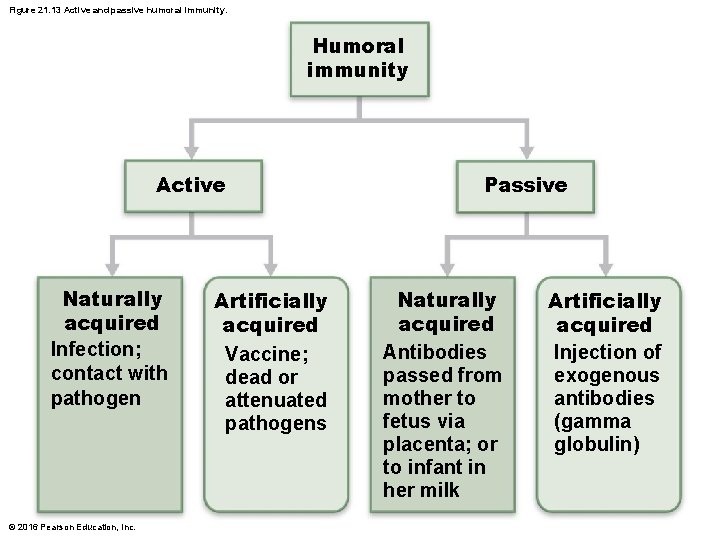
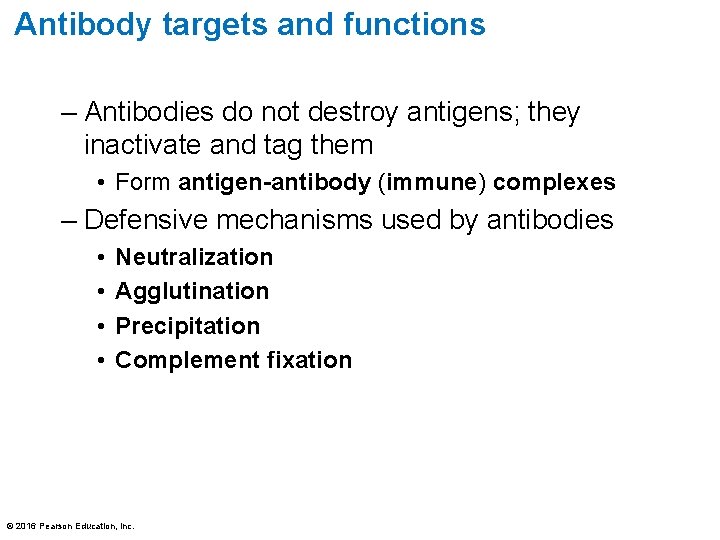
Figure 21. 12 Primary and secondary humoral responses. Secondary immune response to antigen A is faster and larger; primary immune response to antigen B is similar to that for antigen A. Antibody titer (antibody concentration) in plasma (arbitrary units) Primary immune response to antigen A occurs after a delay. 104 103 102 101 Antibodies to B Antibodies to A 100 0 7 First exposure to antigen A 14 21 28 42 Second exposure to antigen A; first exposure to antigen B Time (days) © 2016 Pearson Education, Inc. 35 49 56
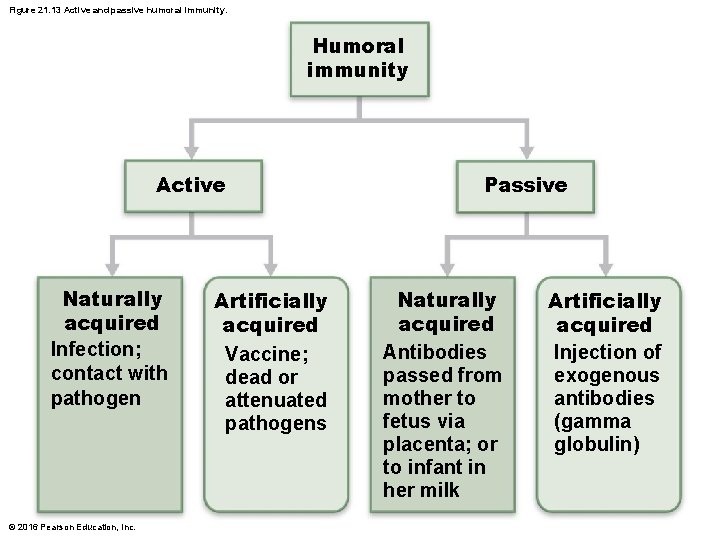
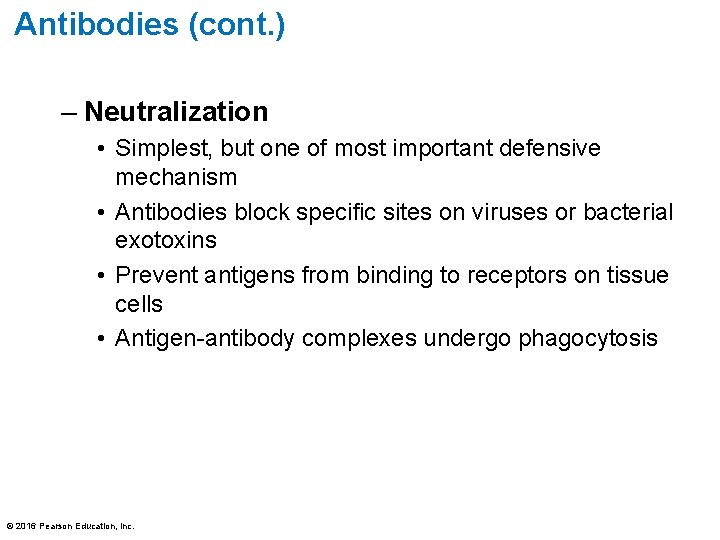
Figure 21. 13 Active and passive humoral immunity. Humoral immunity Active Naturally acquired Infection; contact with pathogen © 2016 Pearson Education, Inc. Artificially acquired Vaccine; dead or attenuated pathogens Passive Naturally acquired Antibodies passed from mother to fetus via placenta; or to infant in her milk Artificially acquired Injection of exogenous antibodies (gamma globulin)
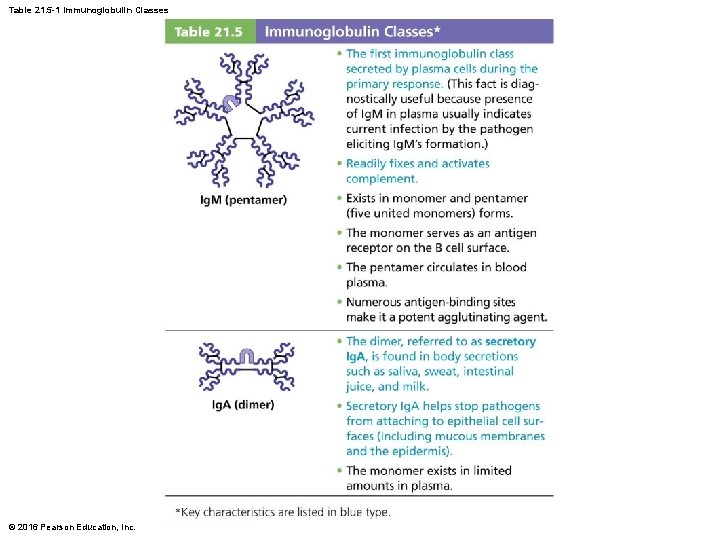
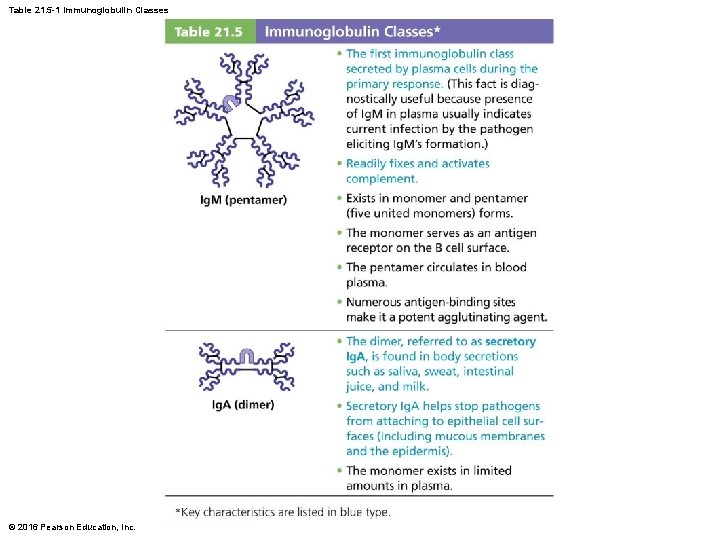
Table 21. 5 -1 Immunoglobulin Classes © 2016 Pearson Education, Inc.
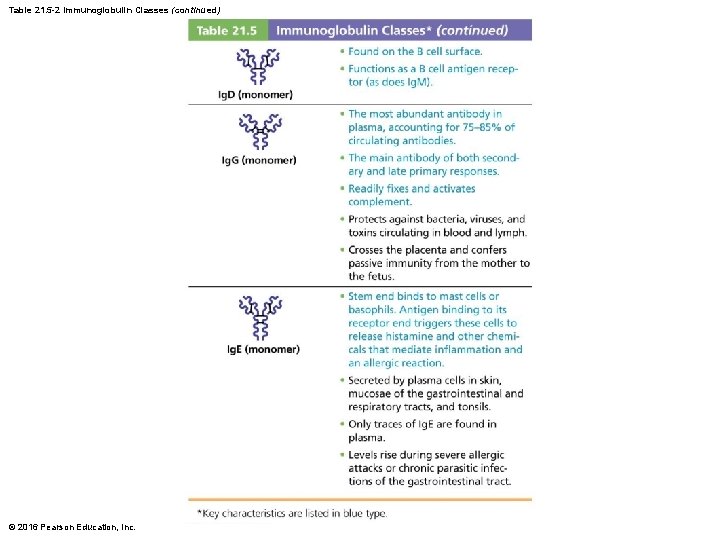
Table 21. 5 -2 Immunoglobulin Classes (continued) © 2016 Pearson Education, Inc.
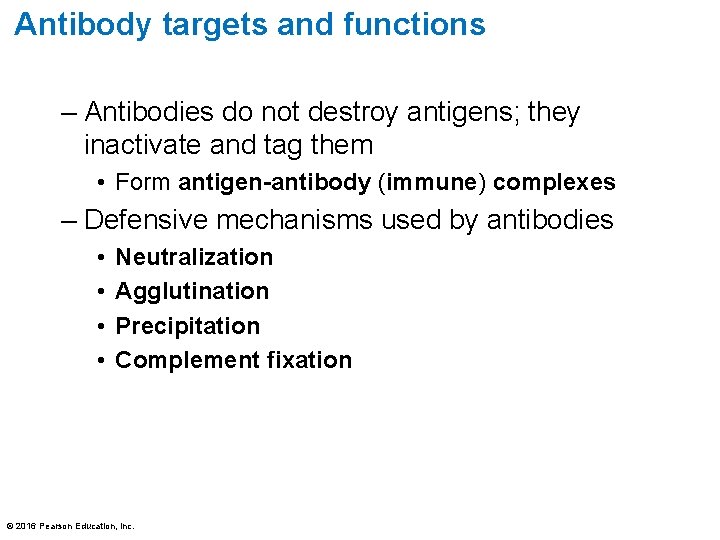
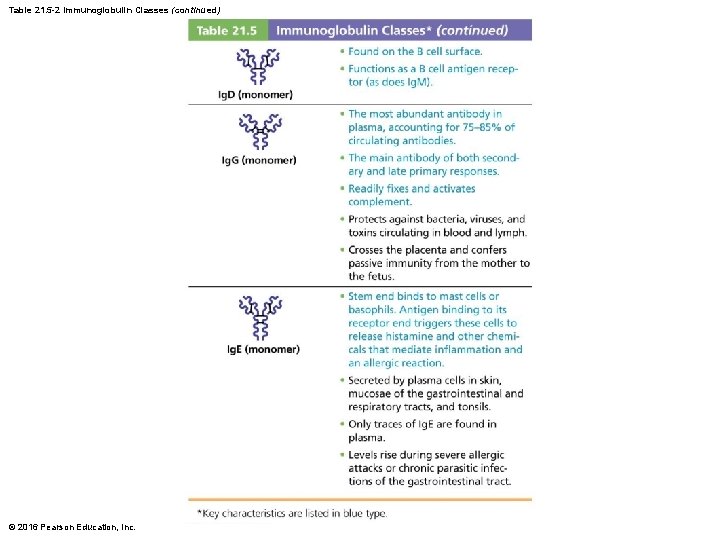
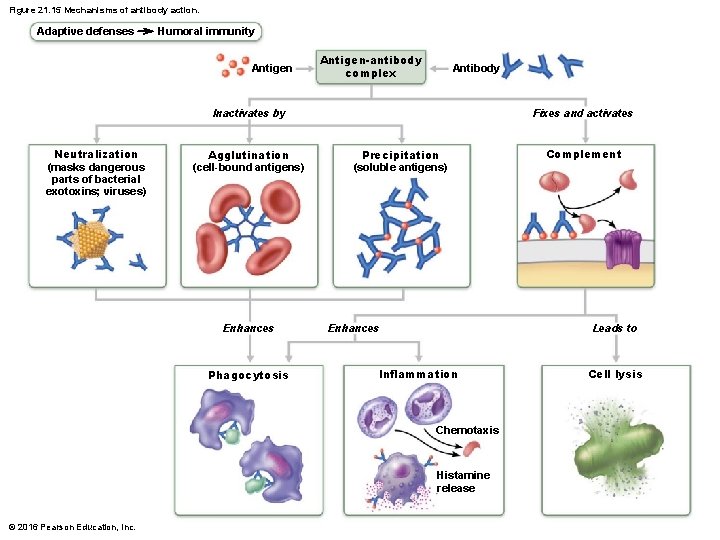
Antibody targets and functions – Antibodies do not destroy antigens; they inactivate and tag them • Form antigen-antibody (immune) complexes – Defensive mechanisms used by antibodies • • Neutralization Agglutination Precipitation Complement fixation © 2016 Pearson Education, Inc.
Antibodies (cont. ) – Neutralization • Simplest, but one of most important defensive mechanism • Antibodies block specific sites on viruses or bacterial exotoxins • Prevent antigens from binding to receptors on tissue cells • Antigen-antibody complexes undergo phagocytosis © 2016 Pearson Education, Inc.
Antibodies (cont. ) – Agglutination • Antibodies can bind same determinant on two different antigens at the same time – Each antibody has two arms, each containing a variable region capable of binding to one antigen • Allows for antigen-antibody complexes to become cross-linked into large lattice-like clumps – Process referred to as agglutination » Example: clumping of mismatched blood cells © 2016 Pearson Education, Inc.
Antibodies (cont. ) – Precipitation • Soluble molecules (instead of cells) are cross-linked into complexes • Complexes precipitate out of solution • Precipated complexes are easier for phagocytes to engulf © 2016 Pearson Education, Inc.
Antibodies (cont. ) – Complement fixation and activation • Main antibody defense against cellular antigens (bacteria, mismatched RBCs) • When several antibodies are bound close together on same antigen, complement-binding sites on their stem regions are aligned – Alignment triggers complement fixation, which leads to cell lysis, as well as other complement functions » Example: amplification of inflammatory response, opsonization © 2016 Pearson Education, Inc.
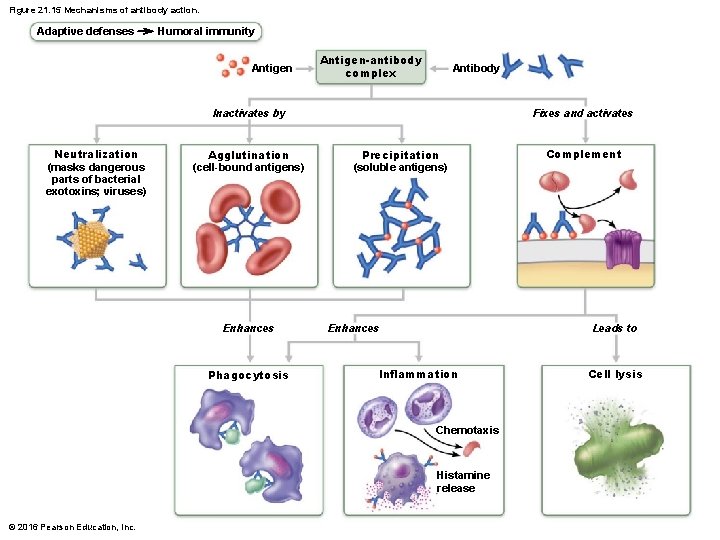
Figure 21. 15 Mechanisms of antibody action. Adaptive defenses Humoral immunity Antigen-antibody complex Antibody Inactivates by Neutralization (masks dangerous parts of bacterial exotoxins; viruses) Agglutination (cell-bound antigens) Enhances Phagocytosis Fixes and activates Precipitation (soluble antigens) Enhances Leads to Inflammation Chemotaxis Histamine release © 2016 Pearson Education, Inc. Complement Cell lysis
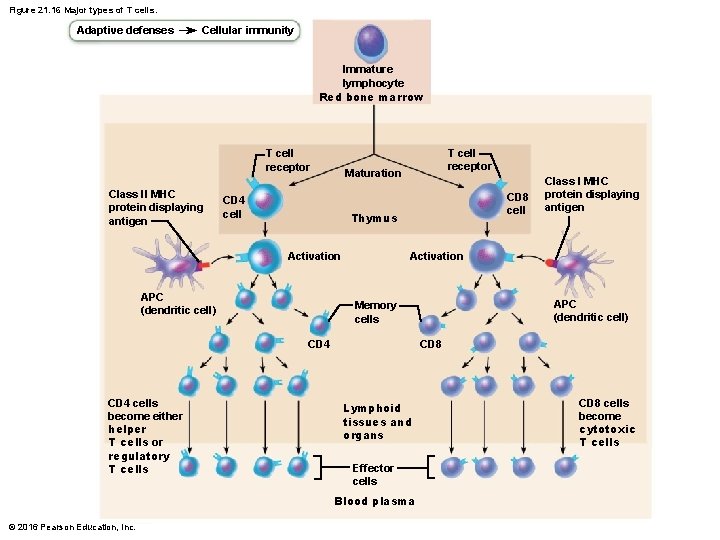
21. 6 Cellular Immune Response • T cells provide defense against intracellular antigens – Example: cells infected with viruses or bacteria, cancerous or abnormal cells, foreign (transplanted) cells • Some T cells directly kill cells; others release chemicals that regulate immune response © 2016 Pearson Education, Inc.
21. 6 Cellular Immune Response • T cells are more complex than B cells both in classification and function • Two populations of T cells are based on which cell differentiation glycoprotein receptors are displayed on their surface – CD 4 cells usually become helper T cells (TH) that can activate B cells, other T cells, and macrophages; direct adaptive immune response • Some become regulatory T cells, which moderate immune response – Can also become memory T cells © 2016 Pearson Education, Inc.
21. 6 Cellular Immune Response – CD 8 cells become cytotoxic T cells (TC) that are capable of destroying cells harboring foreign antigens • Also become memory T cells • Helper, cytotoxic, and regulatory T cells are activated T cells • Naive T cells are simply termed CD 4 or CD 8 cells © 2016 Pearson Education, Inc.
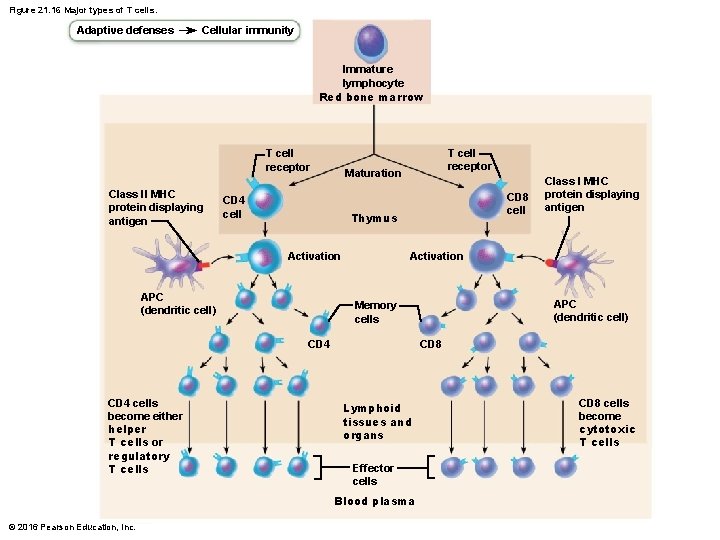
Figure 21. 16 Major types of T cells. Adaptive defenses Cellular immunity Immature lymphocyte Red bone marrow T cell receptor Class II MHC protein displaying antigen T cell receptor Maturation CD 4 cell CD 8 cell Thymus Activation APC (dendritic cell) CD 8 Lymphoid tissues and organs Effector cells Blood plasma © 2016 Pearson Education, Inc. APC (dendritic cell) Memory cells CD 4 cells become either helper T cells or regulatory T cells Class I MHC protein displaying antigen CD 8 cells become cytotoxic T cells
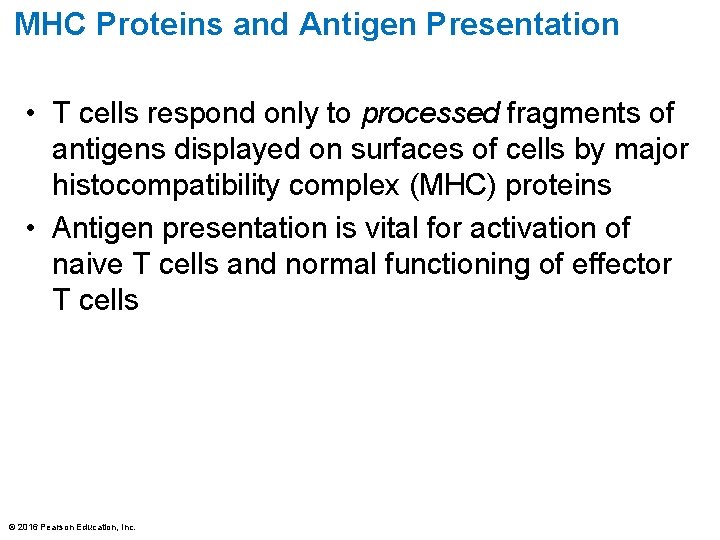
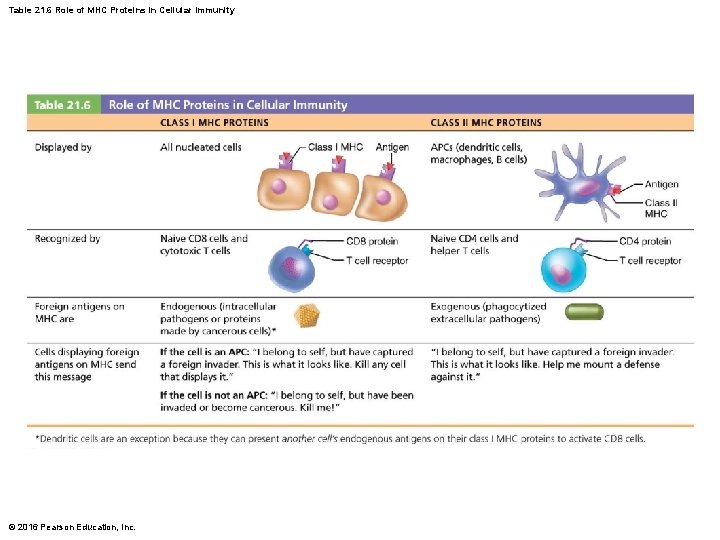
MHC Proteins and Antigen Presentation • T cells respond only to processed fragments of antigens displayed on surfaces of cells by major histocompatibility complex (MHC) proteins • Antigen presentation is vital for activation of naive T cells and normal functioning of effector T cells © 2016 Pearson Education, Inc.
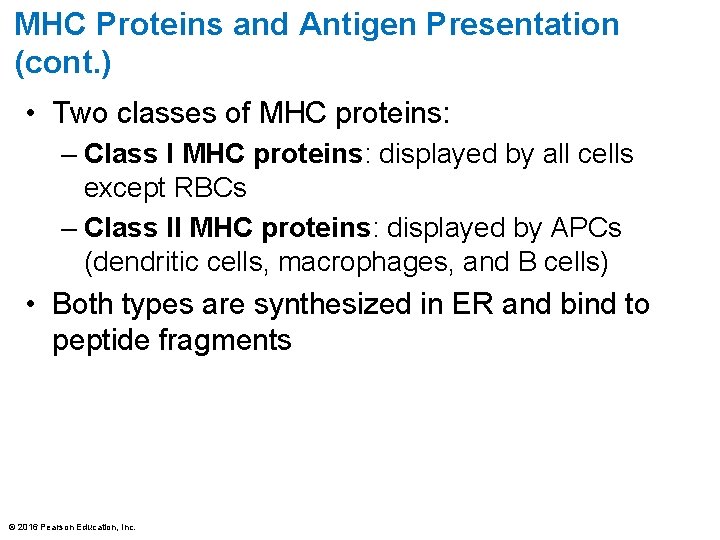
MHC Proteins and Antigen Presentation (cont. ) • Two classes of MHC proteins: – Class I MHC proteins: displayed by all cells except RBCs – Class II MHC proteins: displayed by APCs (dendritic cells, macrophages, and B cells) • Both types are synthesized in ER and bind to peptide fragments © 2016 Pearson Education, Inc.

MHC Proteins and Antigen Presentation (cont. ) • Class I MHC proteins – Class I MHC crucial for CD 8 cell activation • Act as antigen holders; form “self” part that T cells recognize • Inform cytotoxic T cells of microorganisms hiding in cells (cytotoxic T cells ignore displayed self-antigens) © 2016 Pearson Education, Inc.
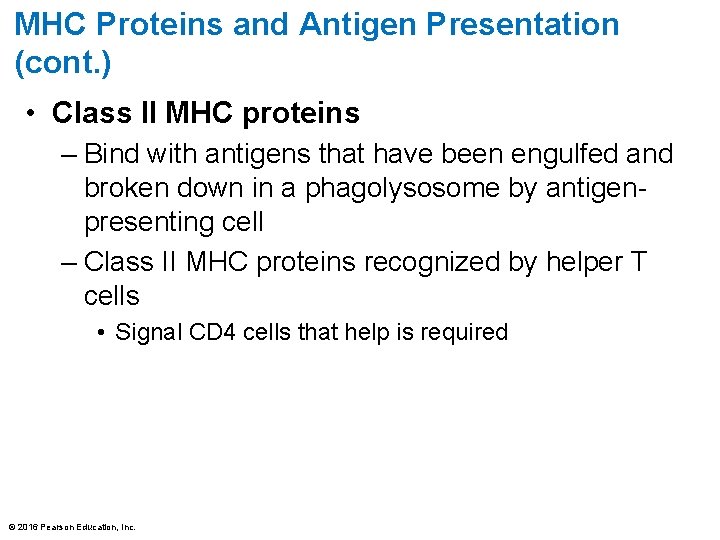
MHC Proteins and Antigen Presentation (cont. ) • Class II MHC proteins – Bind with antigens that have been engulfed and broken down in a phagolysosome by antigenpresenting cell – Class II MHC proteins recognized by helper T cells • Signal CD 4 cells that help is required © 2016 Pearson Education, Inc.
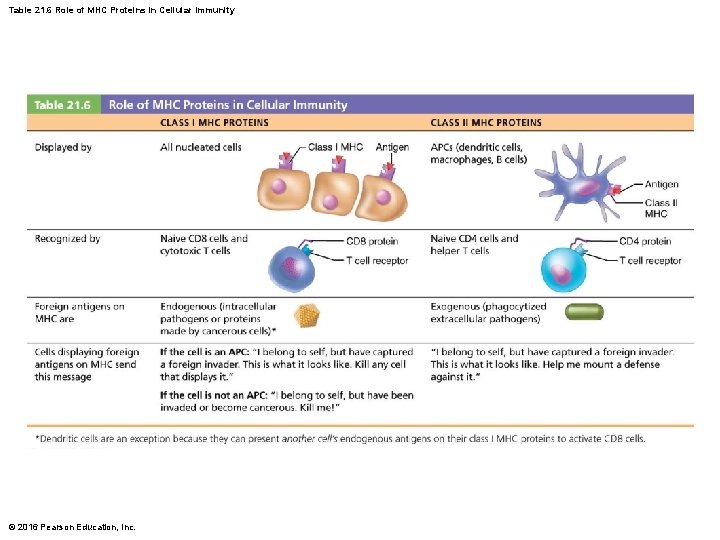
Table 21. 6 Role of MHC Proteins in Cellular Immunity © 2016 Pearson Education, Inc.
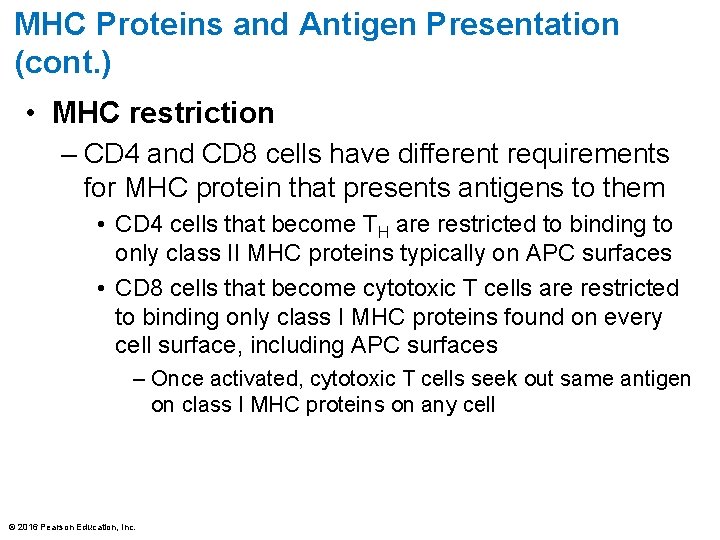
MHC Proteins and Antigen Presentation (cont. ) • MHC restriction – CD 4 and CD 8 cells have different requirements for MHC protein that presents antigens to them • CD 4 cells that become TH are restricted to binding to only class II MHC proteins typically on APC surfaces • CD 8 cells that become cytotoxic T cells are restricted to binding only class I MHC proteins found on every cell surface, including APC surfaces – Once activated, cytotoxic T cells seek out same antigen on class I MHC proteins on any cell © 2016 Pearson Education, Inc.
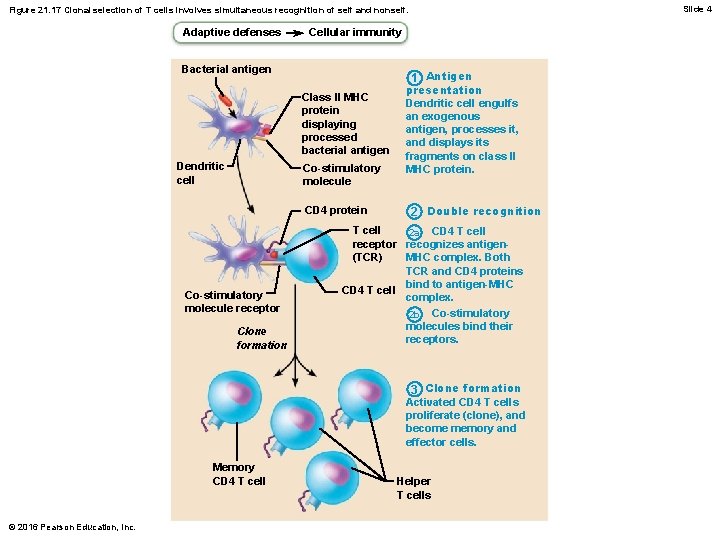
Activation and Differentiation of T cells • T cells can be activated only when antigen is presented to them • Activation is a two-step process 1. Antigen binding 2. Co-stimulation • Both occur on surface of same APC • Both are required for clonal selection of T cell © 2016 Pearson Education, Inc.
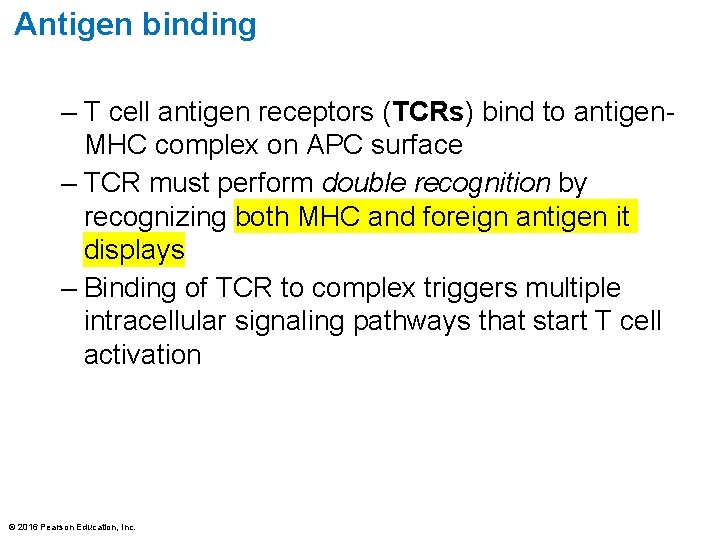
Antigen binding – T cell antigen receptors (TCRs) bind to antigen. MHC complex on APC surface – TCR must perform double recognition by recognizing both MHC and foreign antigen it displays – Binding of TCR to complex triggers multiple intracellular signaling pathways that start T cell activation © 2016 Pearson Education, Inc.

Co-stimulation – Complete T cell activation requires T cell to also bind to one or more co-stimulatory signals on surface of APC – Two-step process is a safeguard against unwanted T cell activation © 2016 Pearson Education, Inc.
Proliferation and differentiation – T cells that are activated enlarge and proliferate in response to cytokines • Differentiate and perform functions according to their T cell class – Primary T cell response peaks within a week – T cell apoptosis occurs between days 7 and 30 • Activated T cells are a hazard because they produce large amounts of inflammatory cytokines and could result in hyperplasia or cancer if not cleared from system – Memory T cells remain and mediate secondary responses © 2016 Pearson Education, Inc.
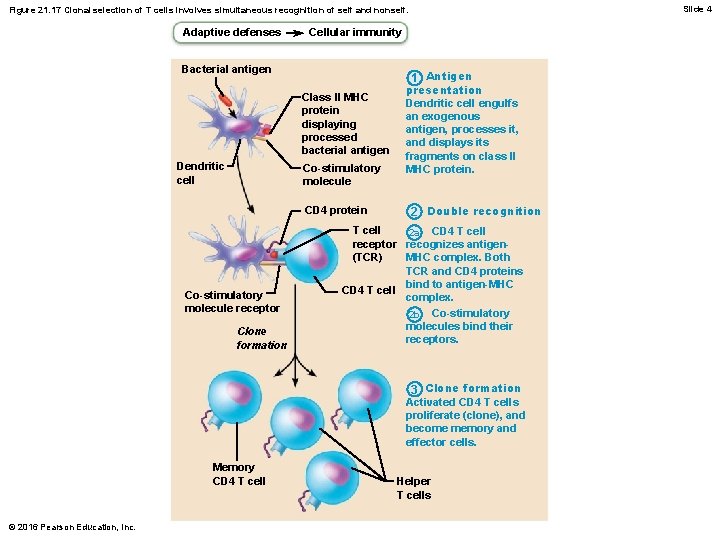
Slide 4 Figure 21. 17 Clonal selection of T cells involves simultaneous recognition of self and nonself. Adaptive defenses Cellular immunity Bacterial antigen Class l. I MHC protein displaying processed bacterial antigen Dendritic cell Co-stimulatory molecule CD 4 protein Co-stimulatory molecule receptor Clone formation 1 Antigen presentation Dendritic cell engulfs an exogenous antigen, processes it, and displays its fragments on class II MHC protein. 2 Double recognition T cell 2 a CD 4 T cell receptor recognizes antigen(TCR) MHC complex. Both TCR and CD 4 proteins bind to antigen-MHC CD 4 T cell complex. 2 b Co-stimulatory molecules bind their receptors. 3 Clone formation Activated CD 4 T cells proliferate (clone), and become memory and effector cells. Memory CD 4 T cell © 2016 Pearson Education, Inc. Helper T cells
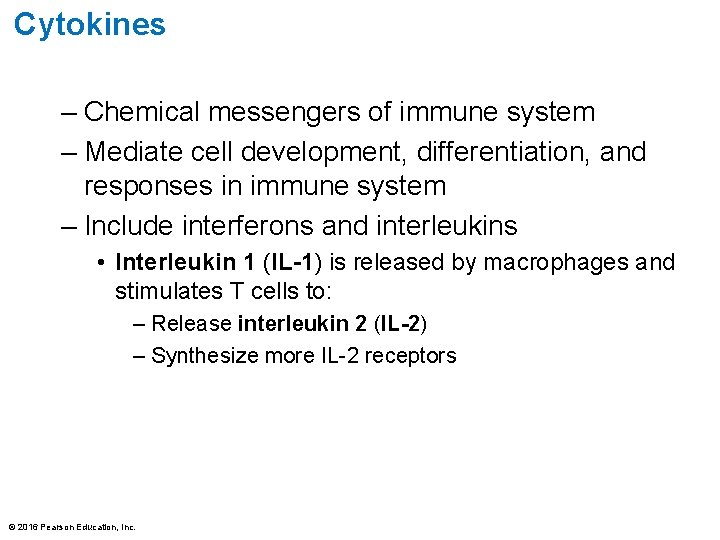
Cytokines – Chemical messengers of immune system – Mediate cell development, differentiation, and responses in immune system – Include interferons and interleukins • Interleukin 1 (IL-1) is released by macrophages and stimulates T cells to: – Release interleukin 2 (IL-2) – Synthesize more IL-2 receptors © 2016 Pearson Education, Inc.
Cytokines • IL-2 is a key growth factor, acting on same cells that release it and other T cells • Encourages activated T cells to divide rapidly – Other cytokines amplify and regulate innate and adaptive responses • Example: gamma interferon—enhances killing power of macrophages © 2016 Pearson Education, Inc.
Roles of Specific Effector T Cells • Helper T (TH) cells – Play central role in adaptive immune response – Activate both humoral and cellular arms – Once primed by APC presentation of antigen, helper T cells: • Help activate B cells and other T cells • Induce T and B cell proliferation • Secrete cytokines that recruit other immune cells • Without TH, there is no immune response © 2016 Pearson Education, Inc.
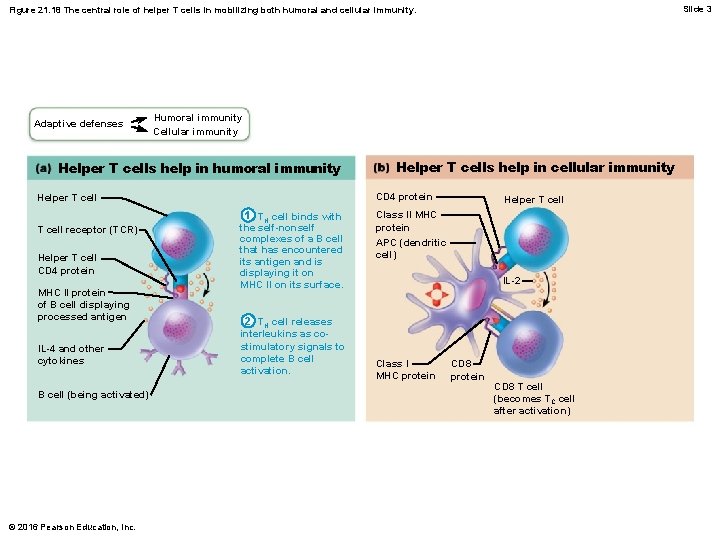
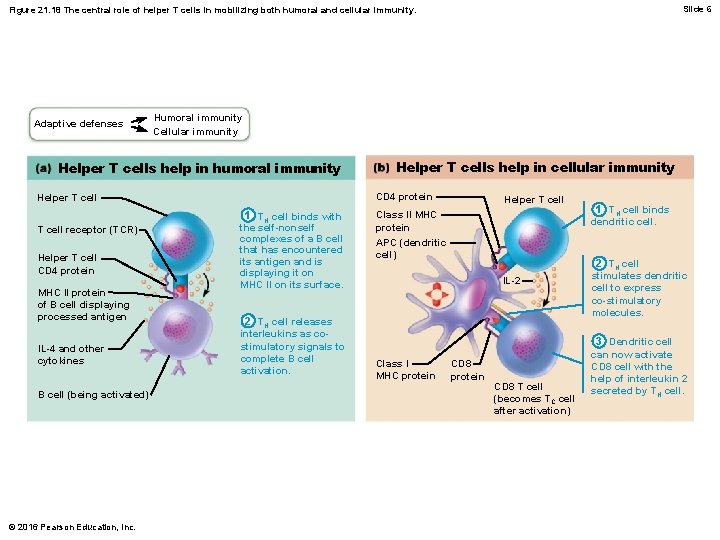
Activation of B cells • Helper T cells interact directly with B cells displaying antigen fragments bound to MHC II receptors • Stimulate B cells to divide more rapidly and begin antibody formation • B cells may be activated without TH cells by binding to T cell–independent antigens – Response is weak and short-lived • Most antigens are T cell–dependent antigens that require TH co-stimulation to activate B cells © 2016 Pearson Education, Inc.
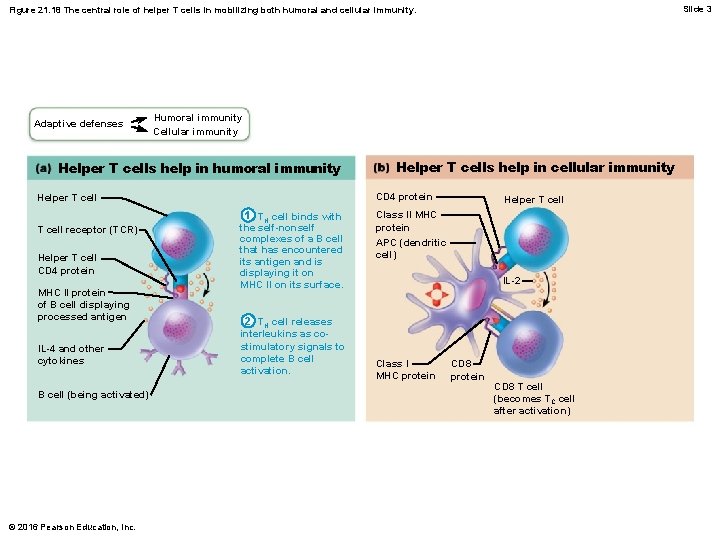
Slide 3 Figure 21. 18 The central role of helper T cells in mobilizing both humoral and cellular immunity. Adaptive defenses Humoral immunity Cellular immunity Helper T cells help in humoral immunity CD 4 protein Helper T cell receptor (TCR) Helper T cell CD 4 protein MHC II protein of B cell displaying processed antigen IL-4 and other cytokines B cell (being activated) © 2016 Pearson Education, Inc. Helper T cells help in cellular immunity 1 TH cell binds with the self-nonself complexes of a B cell that has encountered its antigen and is displaying it on MHC II on its surface. 2 TH cell releases interleukins as costimulatory signals to complete B cell activation. Helper T cell Class II MHC protein APC (dendritic cell) IL-2 Class I MHC protein CD 8 T cell (becomes TC cell after activation)
Activation of CD 8 cells • CD 8 cells require TH cell to become activated into destructive cytotoxic T cells • Cause dendritic cells to express co-stimulatory molecules required for CD 8 cell activation © 2016 Pearson Education, Inc.
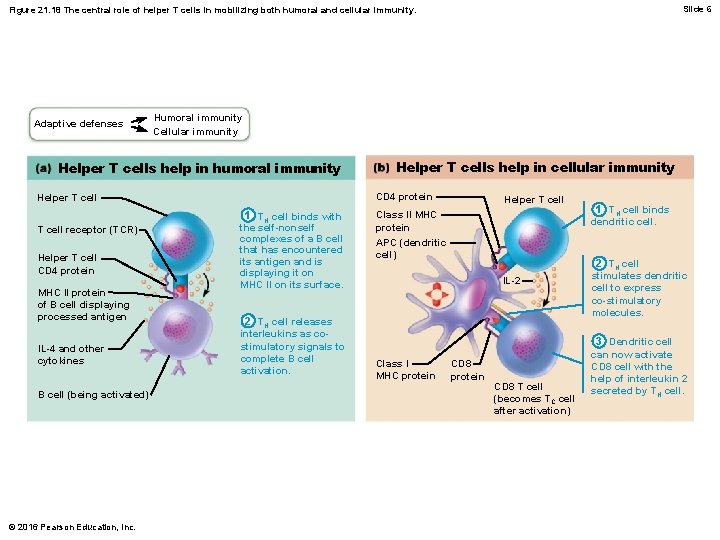
Slide 6 Figure 21. 18 The central role of helper T cells in mobilizing both humoral and cellular immunity. Adaptive defenses Humoral immunity Cellular immunity Helper T cells help in humoral immunity CD 4 protein Helper T cell receptor (TCR) Helper T cell CD 4 protein MHC II protein of B cell displaying processed antigen IL-4 and other cytokines B cell (being activated) © 2016 Pearson Education, Inc. Helper T cells help in cellular immunity 1 TH cell binds with the self-nonself complexes of a B cell that has encountered its antigen and is displaying it on MHC II on its surface. 2 TH cell releases interleukins as costimulatory signals to complete B cell activation. Helper T cell Class II MHC protein APC (dendritic cell) IL-2 Class I MHC protein CD 8 T cell (becomes TC cell after activation) 1 TH cell binds dendritic cell. 2 TH cell stimulates dendritic cell to express co-stimulatory molecules. 3 Dendritic cell can now activate CD 8 cell with the help of interleukin 2 secreted by TH cell.
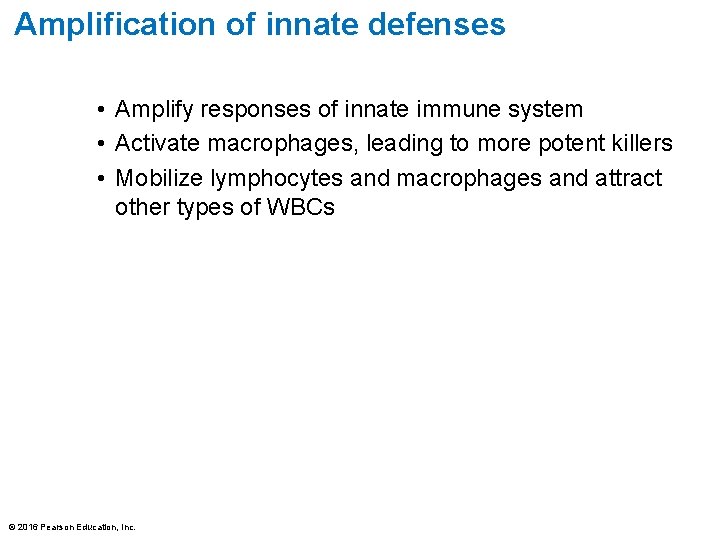
Amplification of innate defenses • Amplify responses of innate immune system • Activate macrophages, leading to more potent killers • Mobilize lymphocytes and macrophages and attract other types of WBCs © 2016 Pearson Education, Inc.
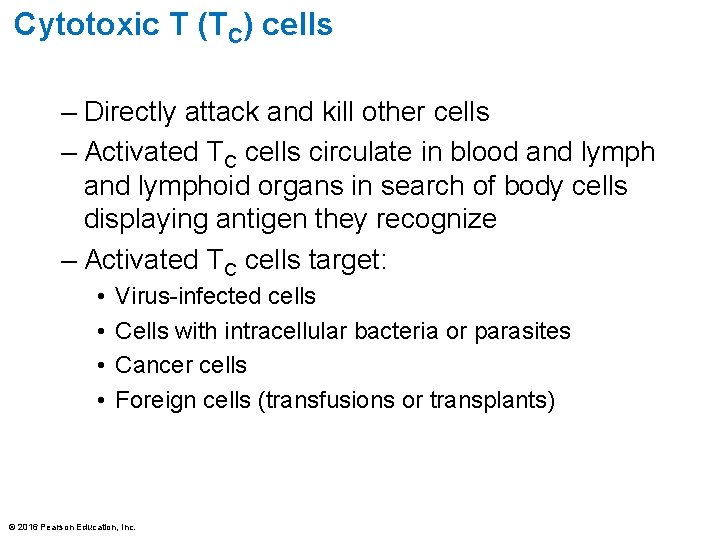
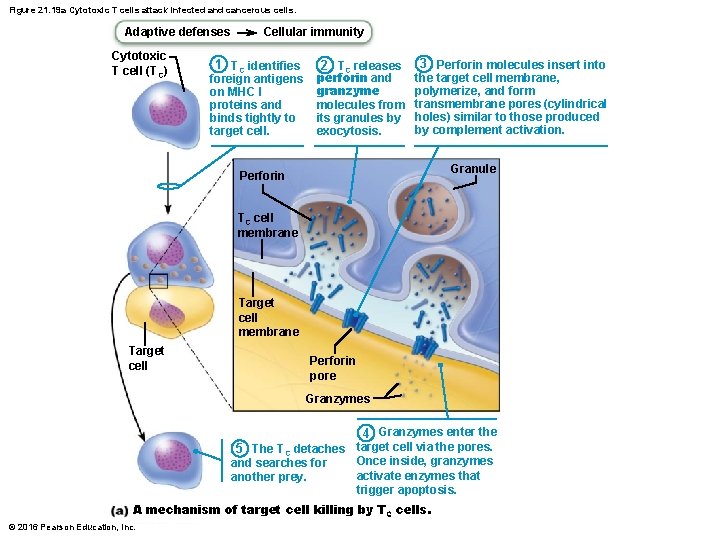
Cytotoxic T (TC) cells – Directly attack and kill other cells – Activated TC cells circulate in blood and lymphoid organs in search of body cells displaying antigen they recognize – Activated TC cells target: • • Virus-infected cells Cells with intracellular bacteria or parasites Cancer cells Foreign cells (transfusions or transplants) © 2016 Pearson Education, Inc.
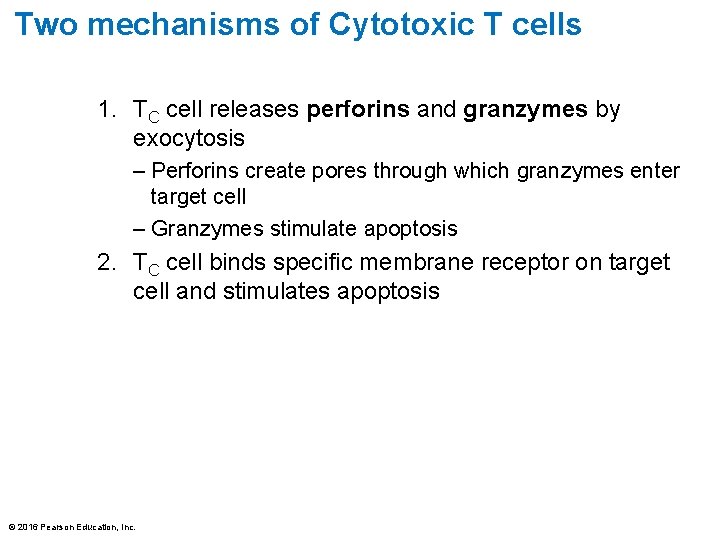
Two mechanisms of Cytotoxic T cells 1. TC cell releases perforins and granzymes by exocytosis – Perforins create pores through which granzymes enter target cell – Granzymes stimulate apoptosis 2. TC cell binds specific membrane receptor on target cell and stimulates apoptosis © 2016 Pearson Education, Inc.
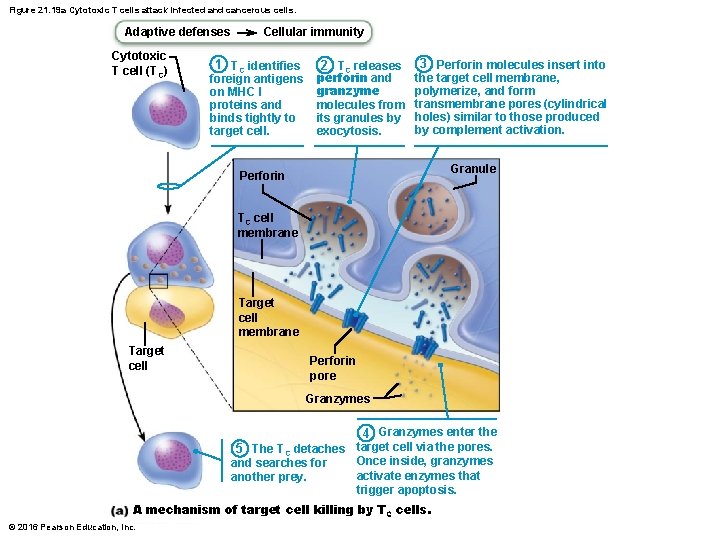
Figure 21. 19 a Cytotoxic T cells attack infected and cancerous cells. Adaptive defenses Cytotoxic T cell (TC) Cellular immunity 1 TC identifies foreign antigens on MHC I proteins and binds tightly to target cell. 2 TC releases perforin and granzyme molecules from its granules by exocytosis. 3 Perforin molecules insert into the target cell membrane, polymerize, and form transmembrane pores (cylindrical holes) similar to those produced by complement activation. Granule Perforin TC cell membrane Target cell Perforin pore Granzymes 4 Granzymes enter the target cell via the pores. 5 The TC detaches Once inside, granzymes and searches for activate enzymes that another prey. trigger apoptosis. A mechanism of target cell killing by T C cells. © 2016 Pearson Education, Inc.
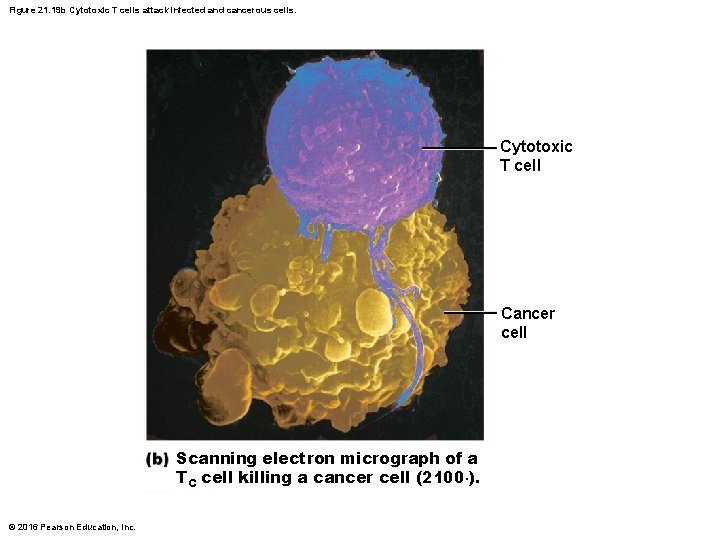
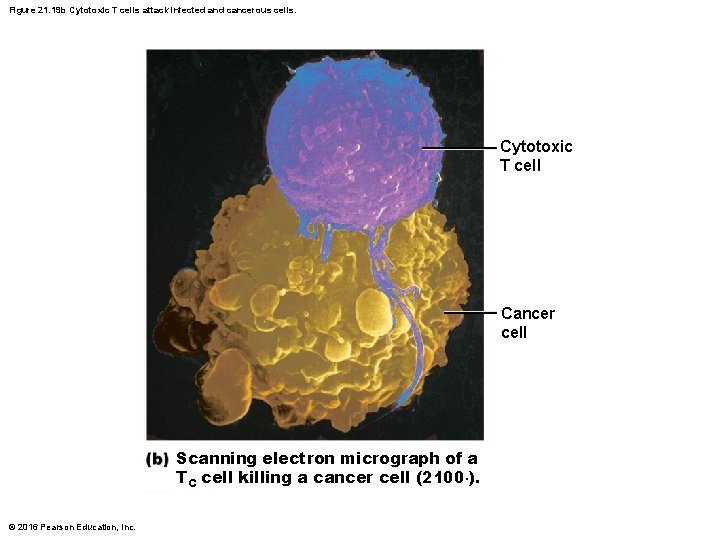
Figure 21. 19 b Cytotoxic T cells attack infected and cancerous cells. Cytotoxic T cell Cancer cell Scanning electron micrograph of a TC cell killing a cancer cell (2100×). © 2016 Pearson Education, Inc.
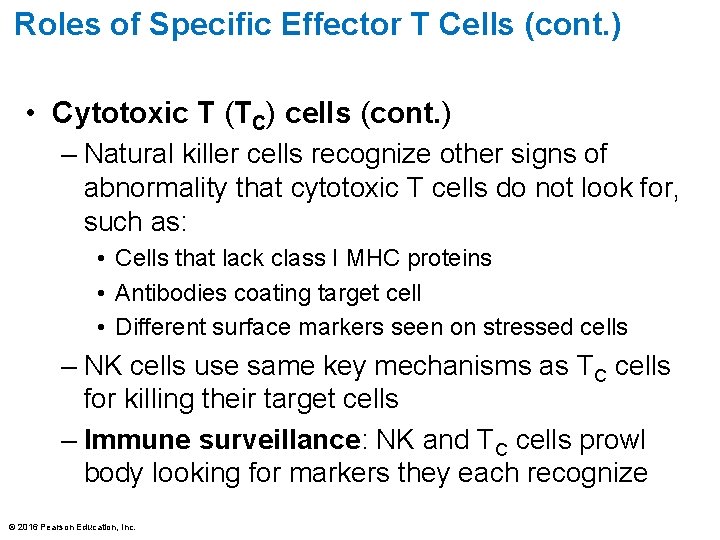
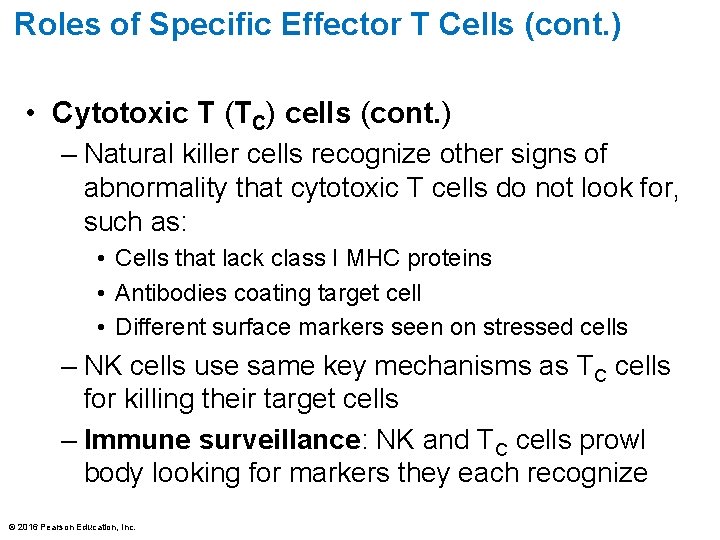
Roles of Specific Effector T Cells (cont. ) • Cytotoxic T (TC) cells (cont. ) – Natural killer cells recognize other signs of abnormality that cytotoxic T cells do not look for, such as: • Cells that lack class I MHC proteins • Antibodies coating target cell • Different surface markers seen on stressed cells – NK cells use same key mechanisms as TC cells for killing their target cells – Immune surveillance: NK and TC cells prowl body looking for markers they each recognize © 2016 Pearson Education, Inc.
Roles of Specific Effector T Cells (cont. ) • Regulatory T (TReg) cells – Dampen immune response by direct contact or by secreting inhibitory cytokines such as IL-10 and transforming growth factor beta (TGF- ) – Important in preventing autoimmune reactions • Suppress self-reactive lymphocytes in periphery (outside lymphoid organs) • Research into using them to induce tolerance to transplanted tissue © 2016 Pearson Education, Inc.
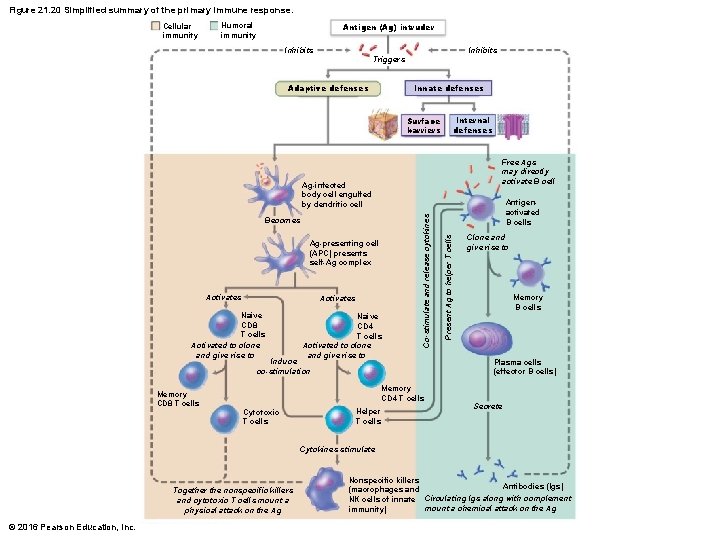
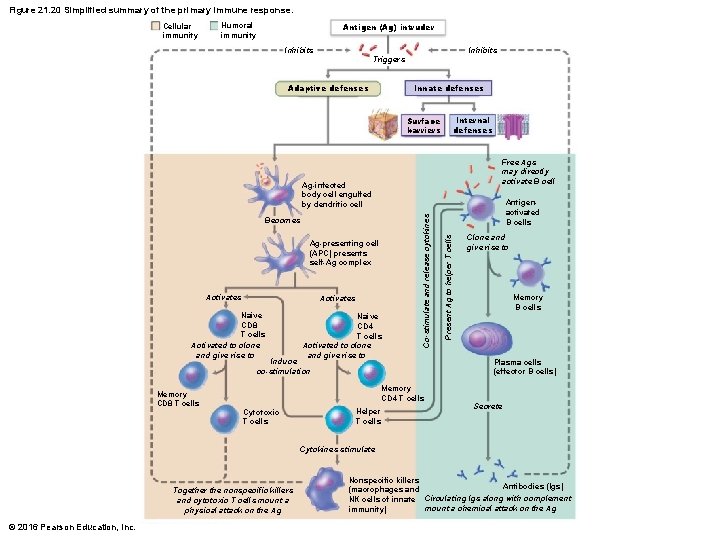
Figure 21. 20 Simplified summary of the primary immune response. Cellular immunity Antigen (Ag) intruder Humoral immunity Inhibits Triggers Innate defenses Adaptive defenses Internal defenses Surface barriers Free Ags may directly activate B cell Ag-presenting cell (APC) presents self-Ag complex Activates Naive CD 8 T cells Activated to clone and give rise to Naive CD 4 T cells Activated to clone and give rise to Induce co-stimulation Memory CD 8 T cells Memory CD 4 T cells Cytotoxic T cells Helper T cells Antigenactivated B cells Present Ag to helper T cells Becomes Co-stimulate and release cytokines Ag-infected body cell engulfed by dendritic cell Clone and give rise to Memory B cells Plasma cells (effector B cells) Secrete Cytokines stimulate Together the nonspecific killers and cytotoxic T cells mount a physical attack on the Ag © 2016 Pearson Education, Inc. Nonspecific killers Antibodies (Igs) (macrophages and NK cells of innate Circulating lgs along with complement mount a chemical attack on the Ag immunity)
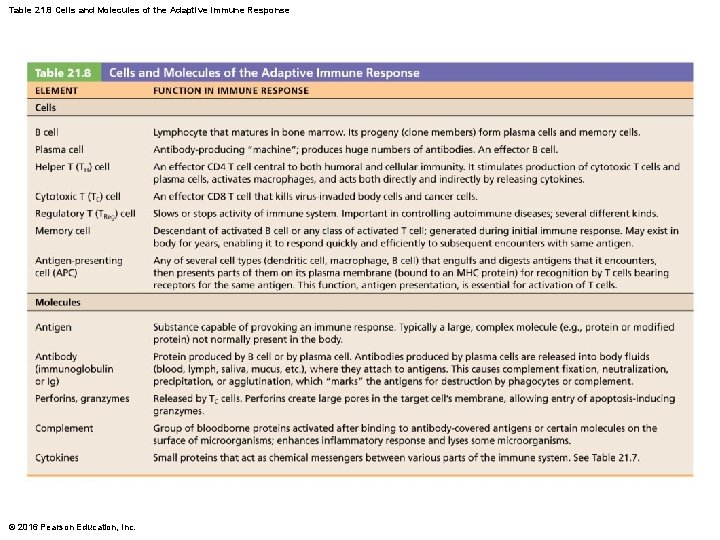
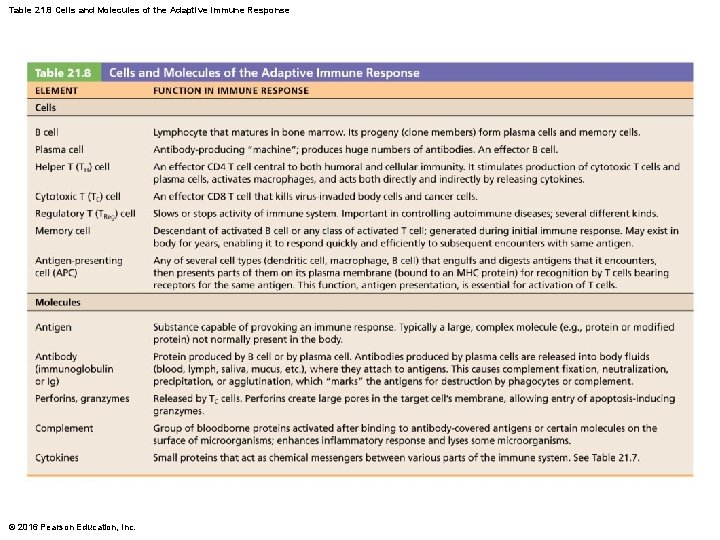
Table 21. 8 Cells and Molecules of the Adaptive Immune Response © 2016 Pearson Education, Inc.