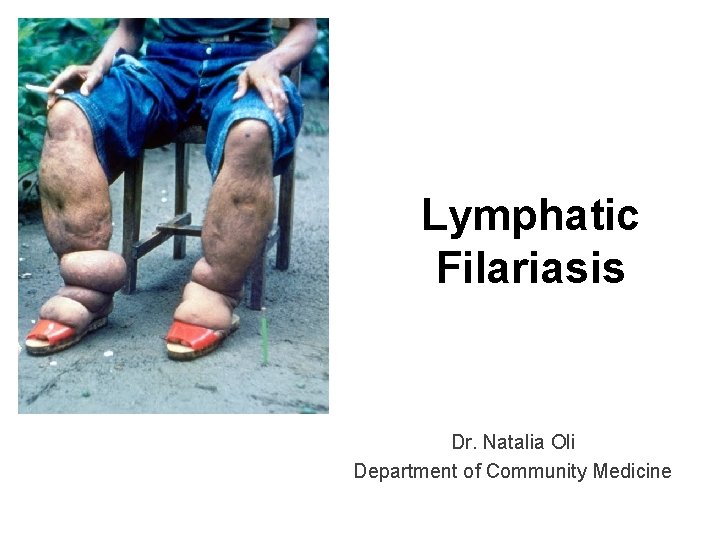
Lymphatic Filariasis Dr Natalia Oli Department of Community

- Slides: 33
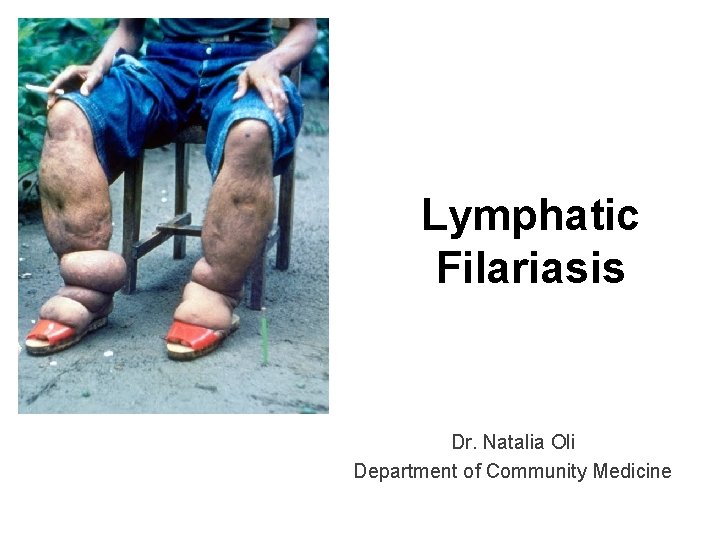
Lymphatic Filariasis Dr. Natalia Oli Department of Community Medicine
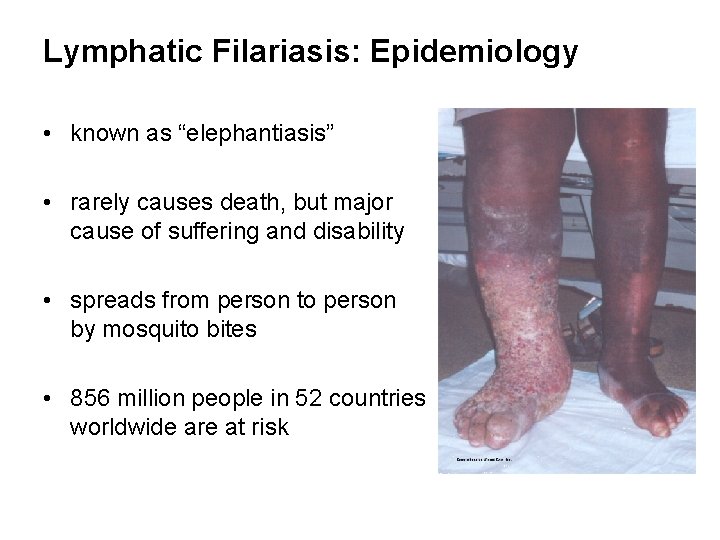
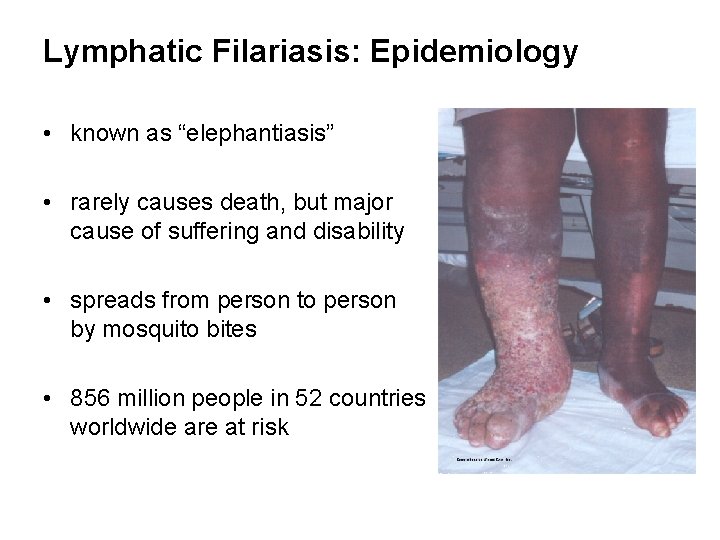
Lymphatic Filariasis: Epidemiology • known as “elephantiasis” • rarely causes death, but major cause of suffering and disability • spreads from person to person by mosquito bites • 856 million people in 52 countries worldwide are at risk
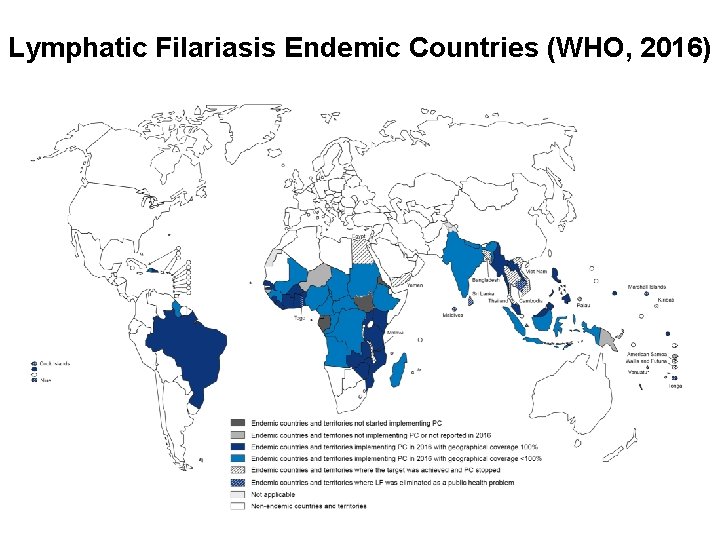
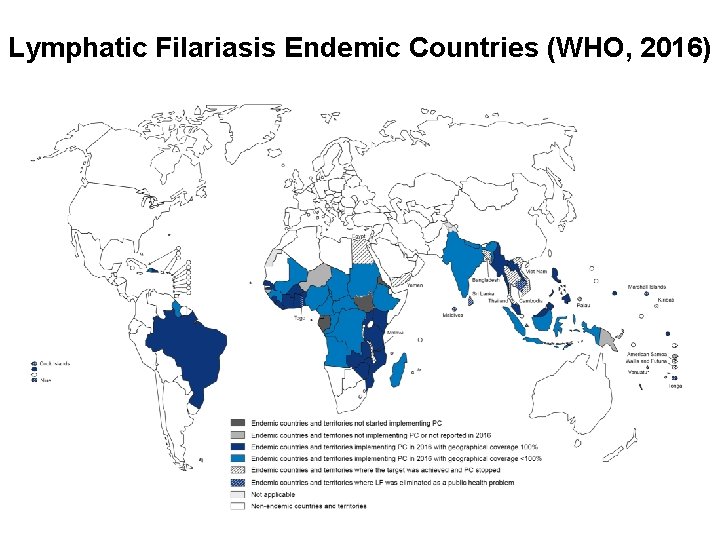
Lymphatic Filariasis Endemic Countries (WHO, 2016)
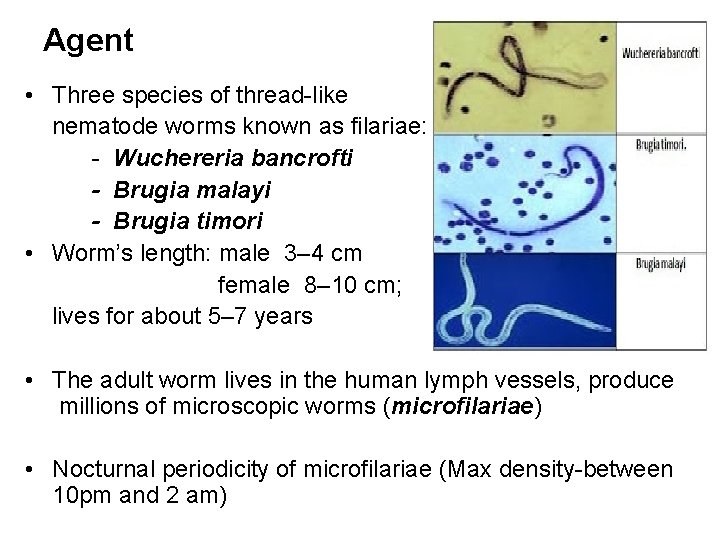
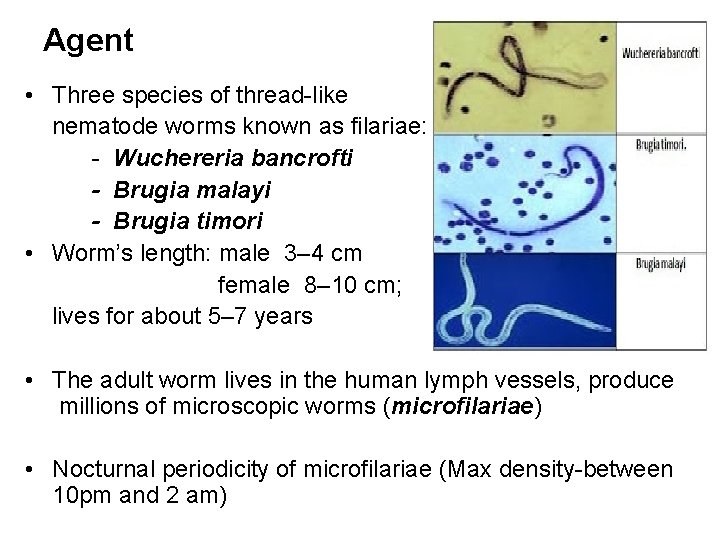
Agent • Three species of thread-like nematode worms known as filariae: - Wuchereria bancrofti - Brugia malayi - Brugia timori • Worm’s length: male 3– 4 cm female 8– 10 cm; lives for about 5– 7 years • The adult worm lives in the human lymph vessels, produce millions of microscopic worms (microfilariae) • Nocturnal periodicity of microfilariae (Max density-between 10 pm and 2 am)
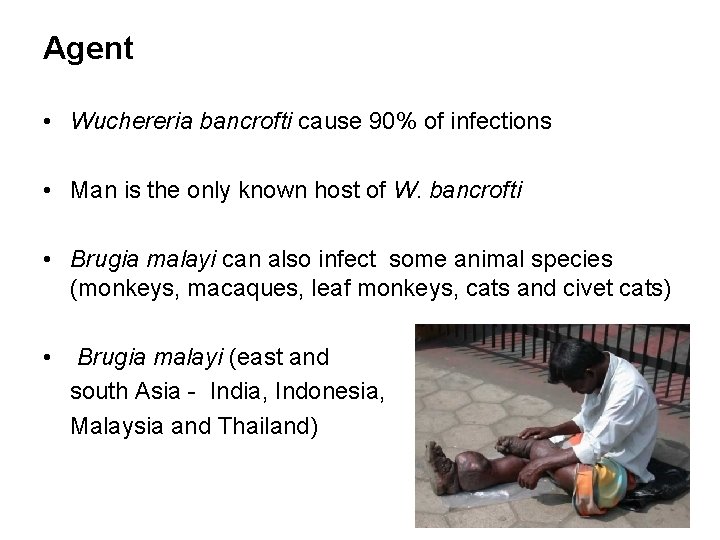
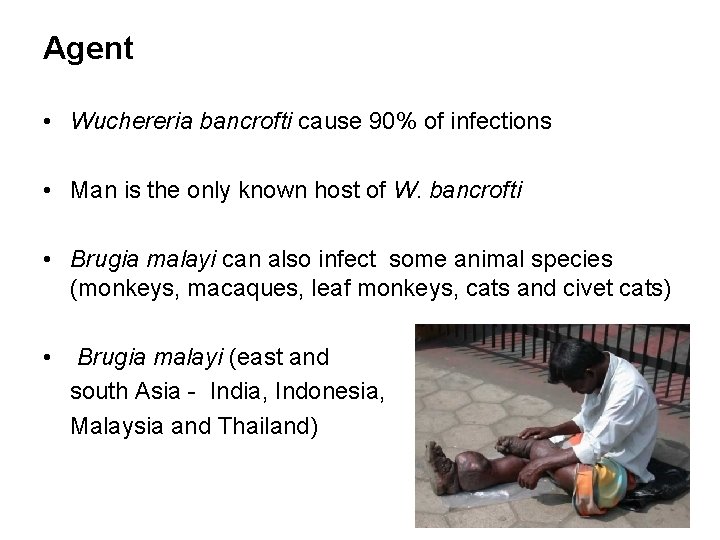
Agent • Wuchereria bancrofti cause 90% of infections • Man is the only known host of W. bancrofti • Brugia malayi can also infect some animal species (monkeys, macaques, leaf monkeys, cats and civet cats) • Brugia malayi (east and south Asia - India, Indonesia, Malaysia and Thailand)
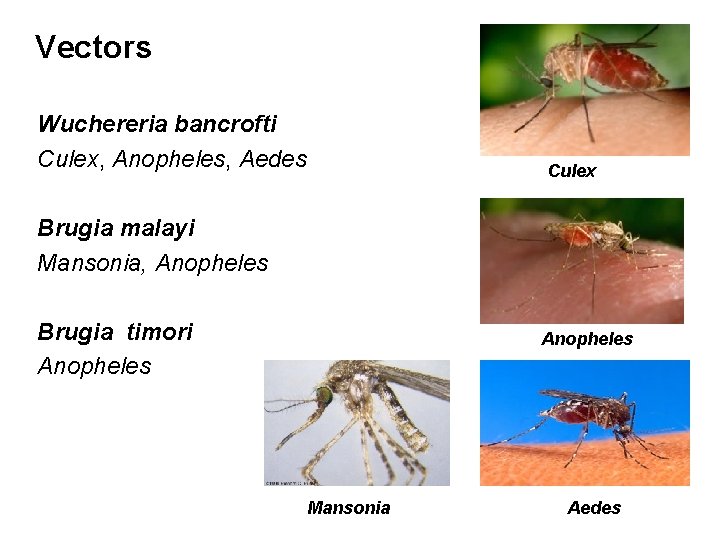
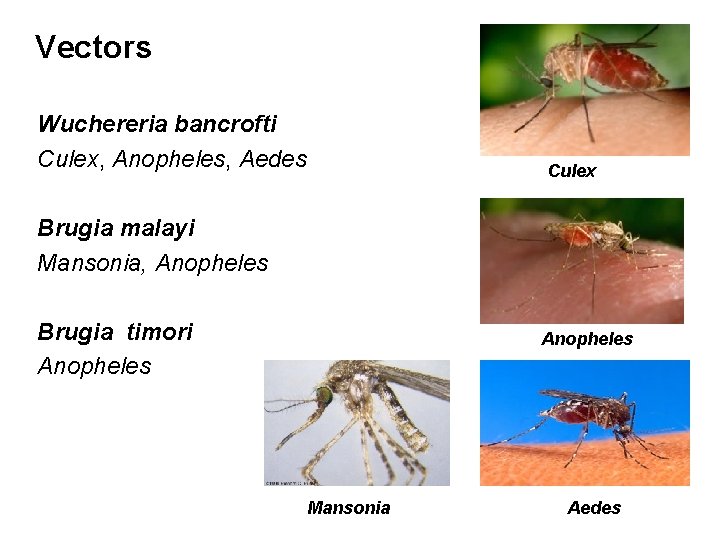
Vectors Wuchereria bancrofti Culex, Anopheles, Aedes Culex Brugia malayi Mansonia, Anopheles Brugia timori Anopheles Mansonia Aedes
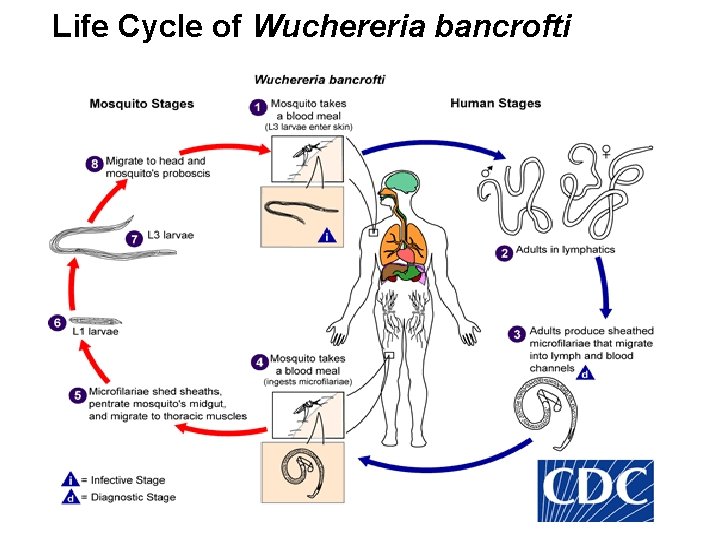
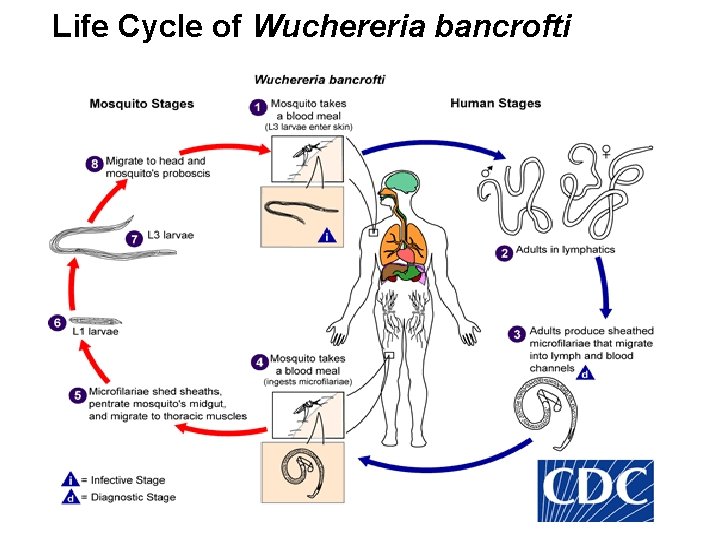
Life Cycle of Wuchereria bancrofti
Host factors • Man – natural host • Age – all age (6 months) Max: 20 -30 years, then decline • Sex – higher in men • Migration – leading to extension of infection to nonendemic areas • Immunity – may develop after long year of exposure (Basis of immunity-not known)
Social and Environmental Factors • Climate is an important factor which influences: - The breeding of mosquitoes - Longevity (optimum temperature 20 -300 C and humidity 70%) - The development of parasite in the vector • Associated with urbanization, poverty, industrialization, illiteracy and poor sanitation • Sanitation, town planning, sewage and drainage
Transmission in a community is influenced by: • the number of infected persons (prevalence) • the density of microfilaria in the blood of infected persons • the density of vector mosquitoes • characteristics of the vector that affect development of infective larvae • frequency of human-vector contact
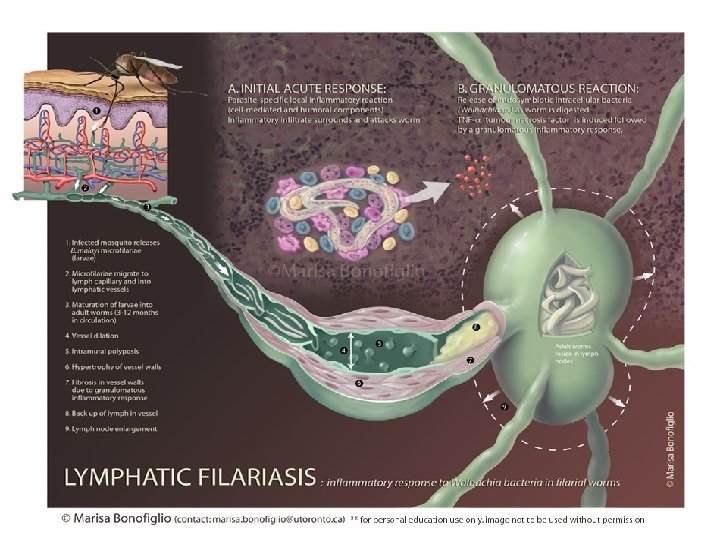
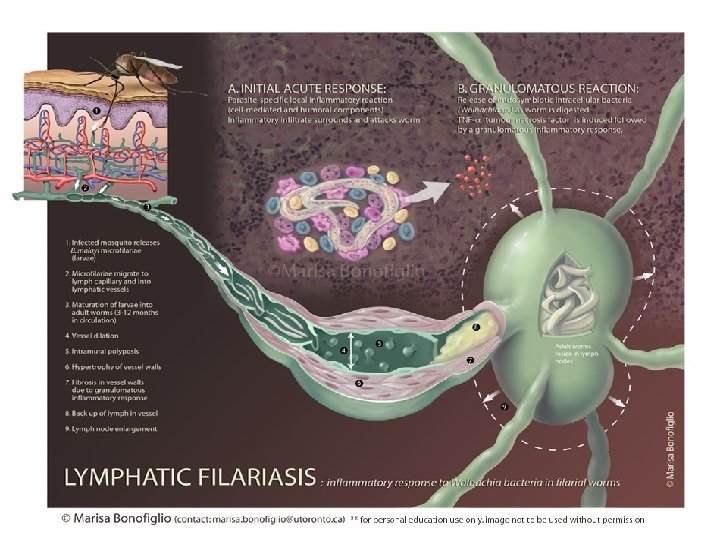
Clinical manifestations 1) Majority of infected people are asymptomatic - have circulating microfilariae - important source of infection - may have subclinical lymphatic damage and as many as 40% have kidney damage, with proteinuria and haematuria 2) Acute: attacks of ‘filarial fever’ - pain and inflammation of lymph nodes and ducts related to bacterial and fungal super infections of the tissue that are already compromised lymphatic function - fever, nausea
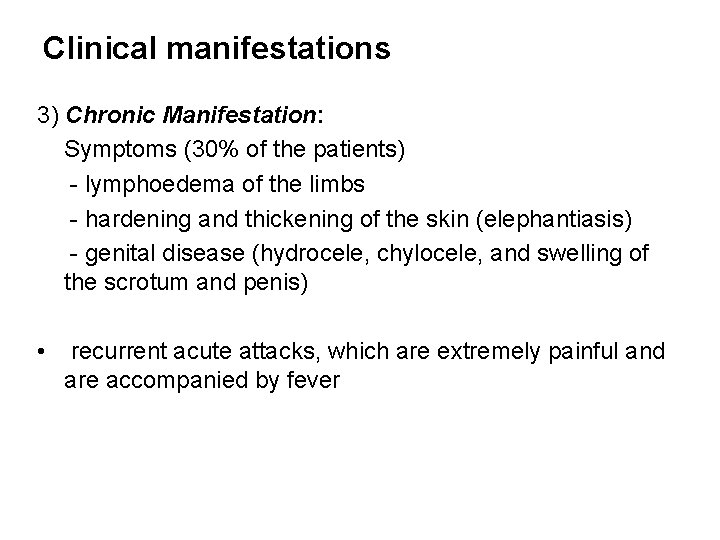
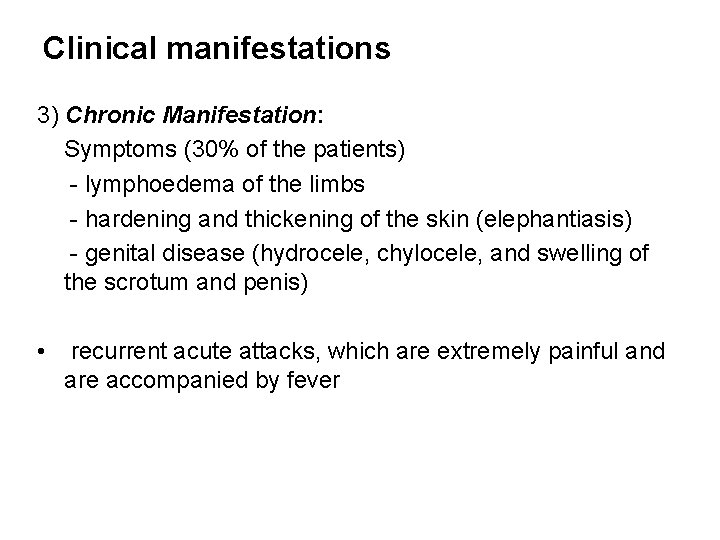
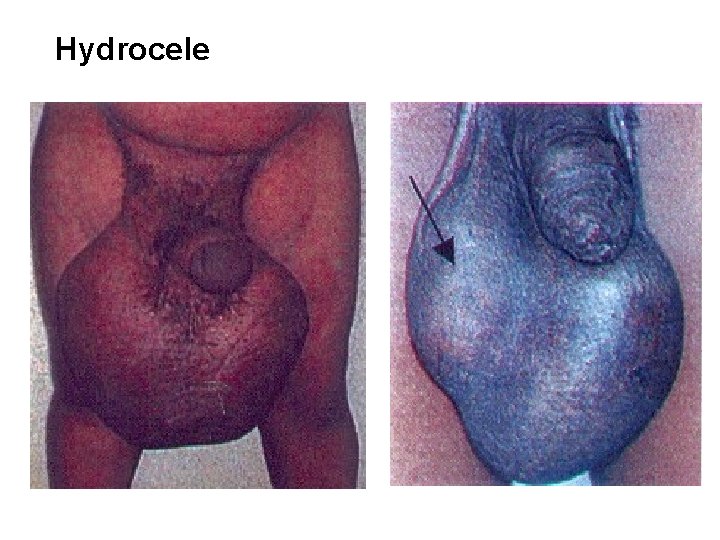
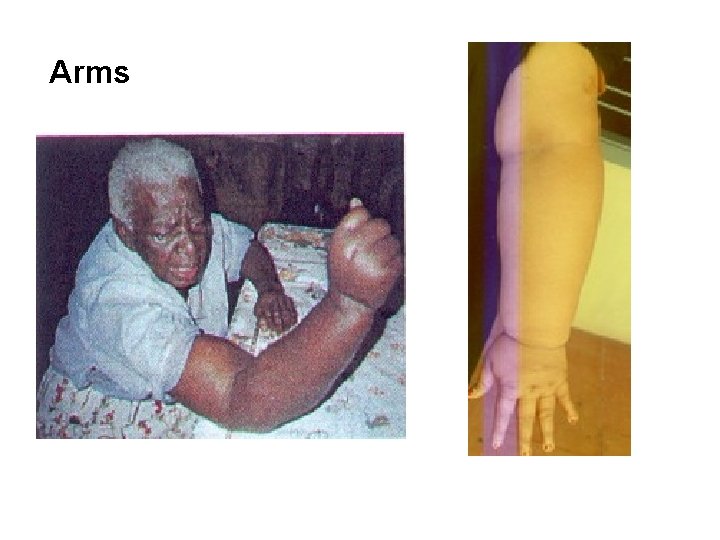
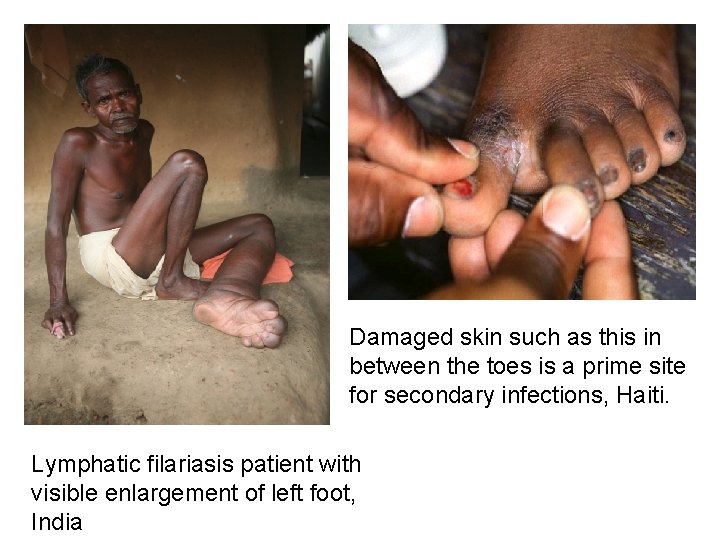
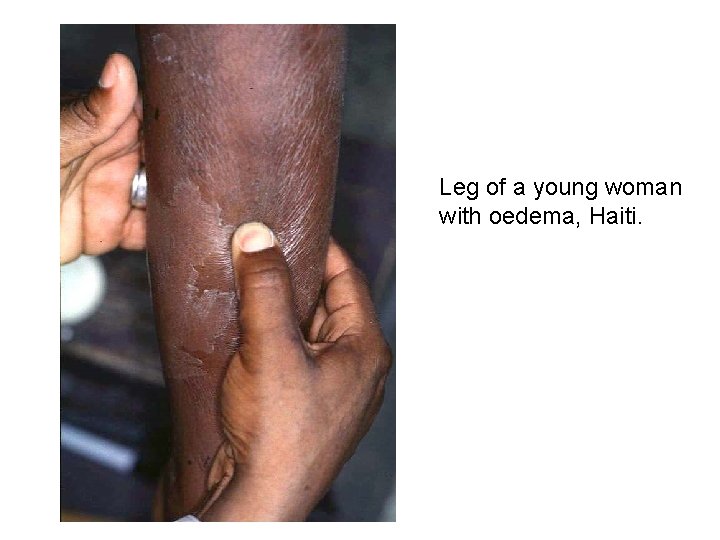
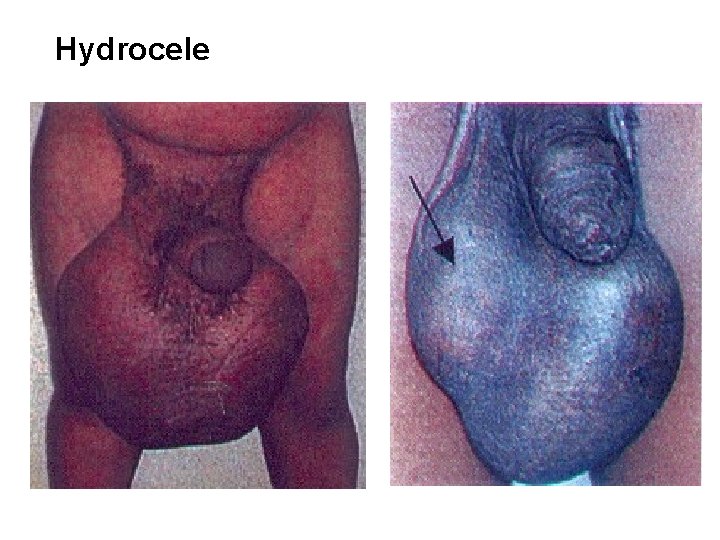
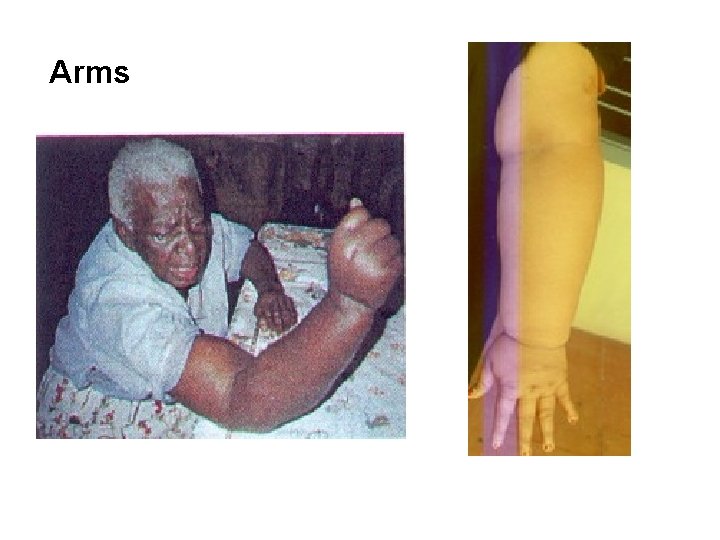
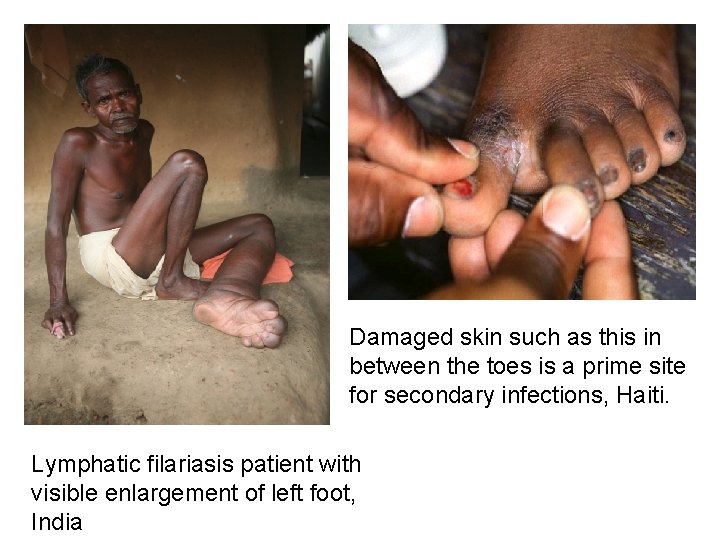
Clinical manifestations 3) Chronic Manifestation: Symptoms (30% of the patients) - lymphoedema of the limbs - hardening and thickening of the skin (elephantiasis) - genital disease (hydrocele, chylocele, and swelling of the scrotum and penis) • recurrent acute attacks, which are extremely painful and are accompanied by fever
Hydrocele

Legs
Arms
Damaged skin such as this in between the toes is a prime site for secondary infections, Haiti. Lymphatic filariasis patient with visible enlargement of left foot, India
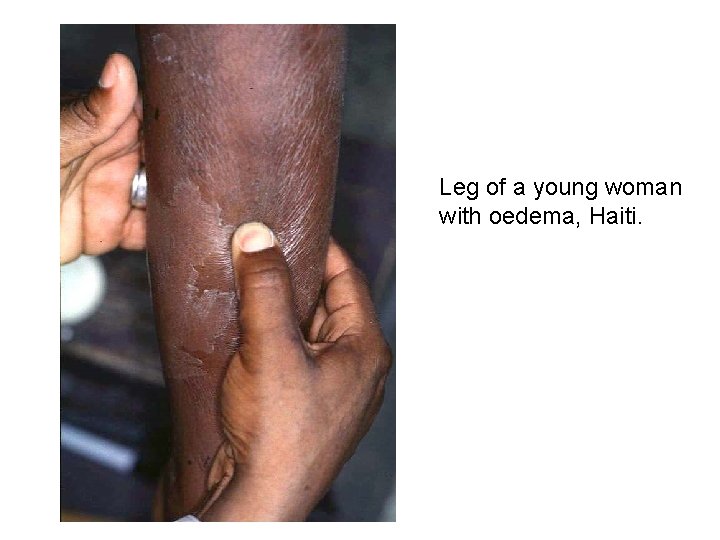
Leg of a young woman with oedema, Haiti.
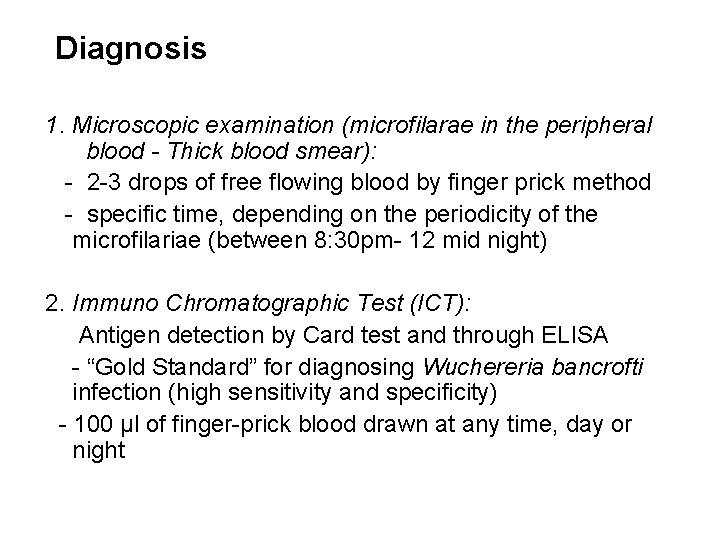
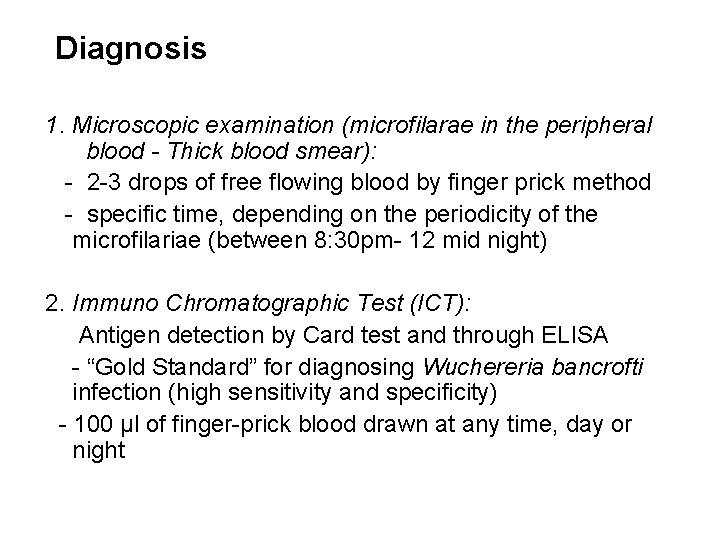
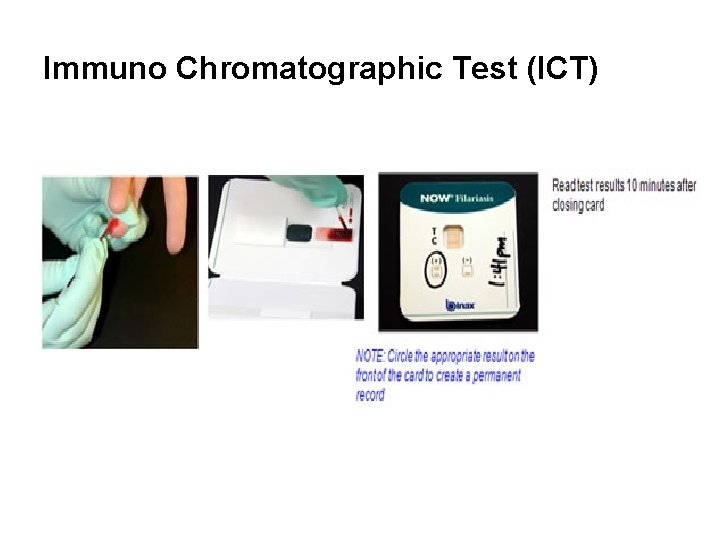
Diagnosis 1. Microscopic examination (microfilarae in the peripheral blood - Thick blood smear): - 2 -3 drops of free flowing blood by finger prick method - specific time, depending on the periodicity of the microfilariae (between 8: 30 pm- 12 mid night) 2. Immuno Chromatographic Test (ICT): Antigen detection by Card test and through ELISA - “Gold Standard” for diagnosing Wuchereria bancrofti infection (high sensitivity and specificity) - 100 μl of finger-prick blood drawn at any time, day or night
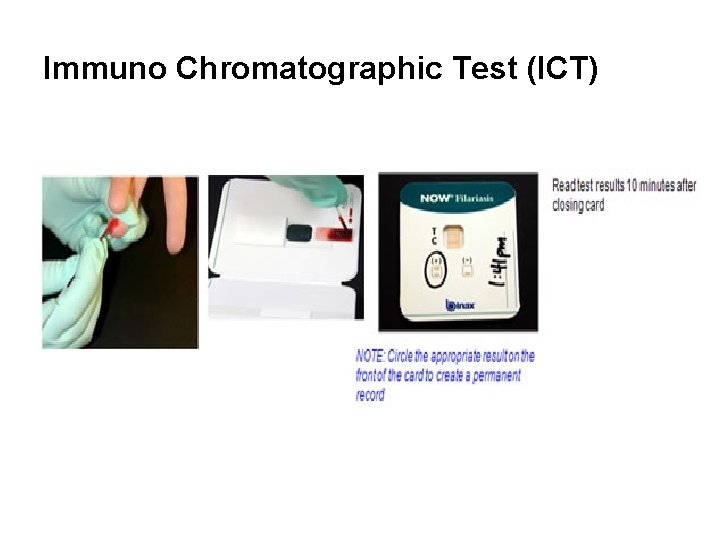
Immuno Chromatographic Test (ICT)
Lymphatic Filariasis Elimination Strategy • Global Programme to Eliminate Lymphatic Filariasis (GPELF) was launched in 2000 - interrupting the transmission cycle - control morbidity (relief of suffering)
Lymphatic Filariasis Elimination Strategy • Mass Drug Administration (MDA) – preventive chemotherapy: - combined dose of 2 medicines given annually to an entire at-risk population in the following way: Albendazole (400 mg) Diethylcarbamazine citrate (DEC) (6 mg/kg) - at least 5 rounds are recommended in the community to stop transmission
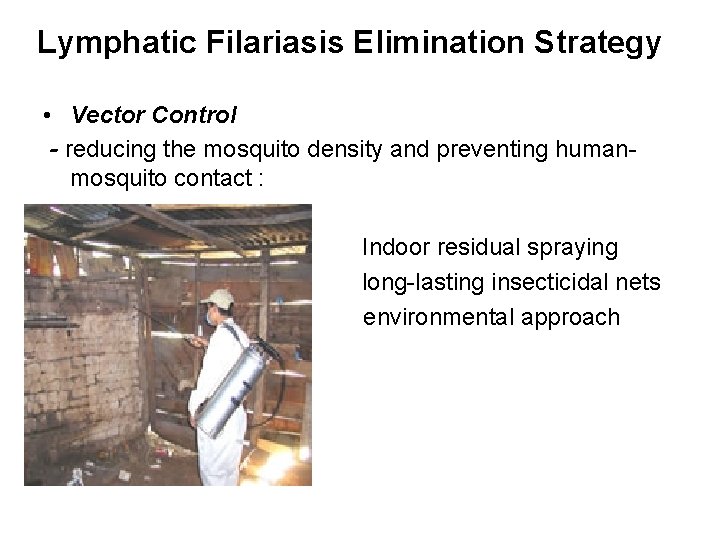
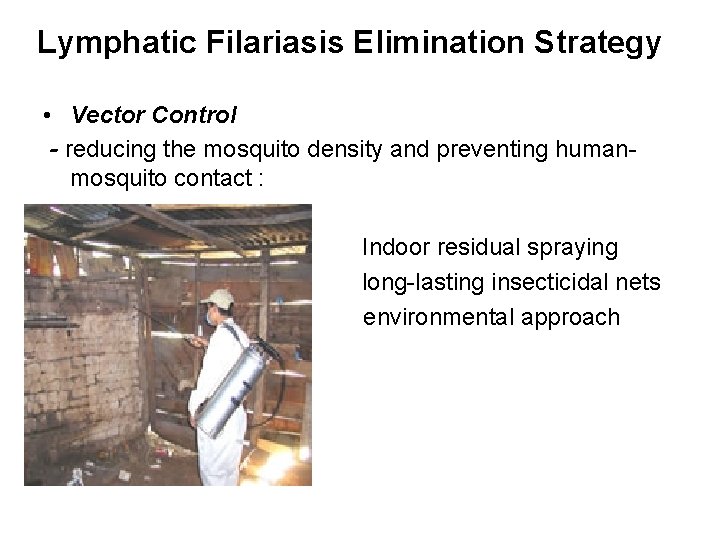
Lymphatic Filariasis Elimination Strategy • Vector Control - reducing the mosquito density and preventing humanmosquito contact : Indoor residual spraying long-lasting insecticidal nets environmental approach
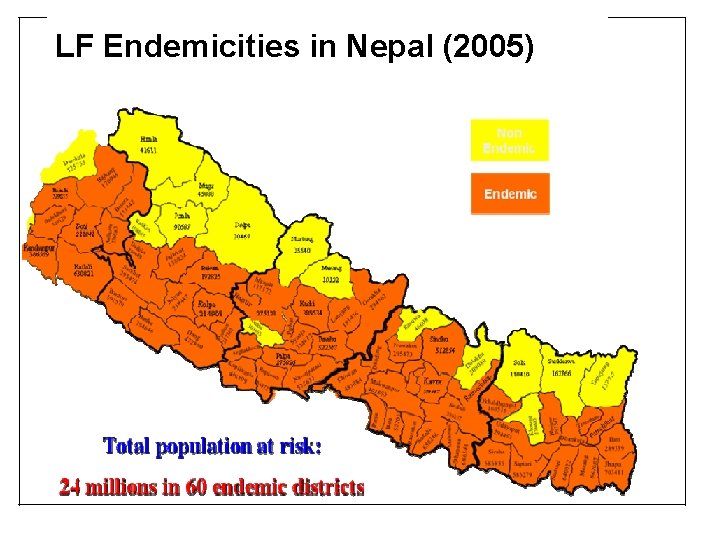
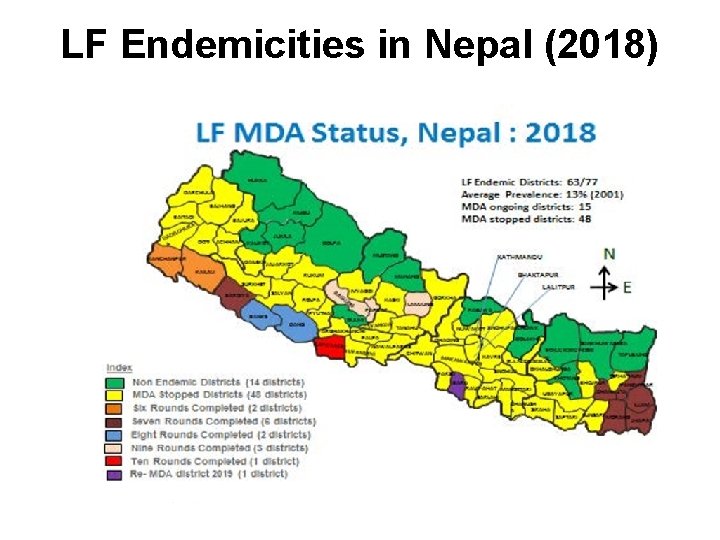
Situation in Nepal • Agent - Wuchereria bancrofti (only recorded parasite in Nepal) • Vector - The mosquito, Culex quinquefasciatus • 13% average prevalence of LF infection in the country, ranging from <1% to 39% • Nepal conducted LF mapping in 2001 and 2005 (Immunochromatography Test card), remapping - 2012 61 districts were mapped as endemic for LF • More LF cases are seen in the Terai than in the Hills
National Plan of Action (2003‐ 2020 AD) for the Elimination of Lymphatic Filariasis • Epidemiology and Disease Control Division under the Department of Health Services Goal: People of Nepal no longer suffer from LF Objectives: • To eliminate LF as a public health problem by 2020 • To interrupt the transmission of Lymphatic Filariasis • To reduce and prevent morbidity • To provide de‐worming benefit through use of Albendazole to endemic community especially to the children • To reduce mosquito vectors
National Plan of Action (2003‐ 2020 AD) for the Elimination of Lymphatic Filariasis Target: • To scale up MDA to all LF endemic districts by 2014 • To achieve <1% prevalence (microfilaraemia rate) in all endemic districts after 6 years of MDA by 2018
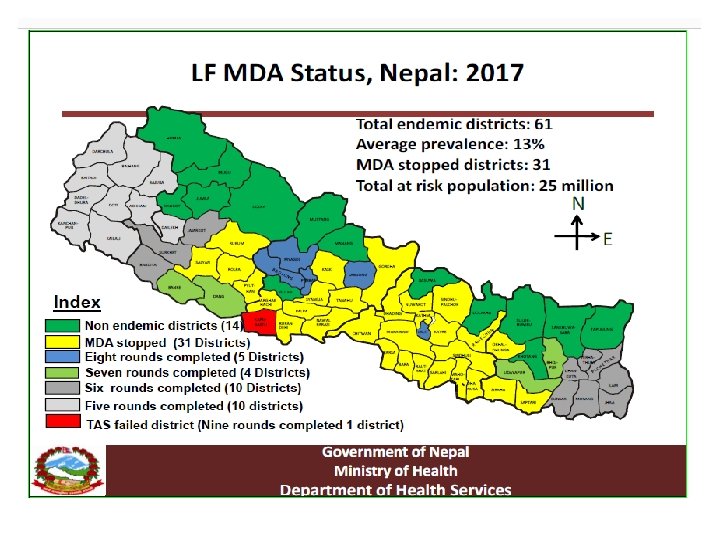
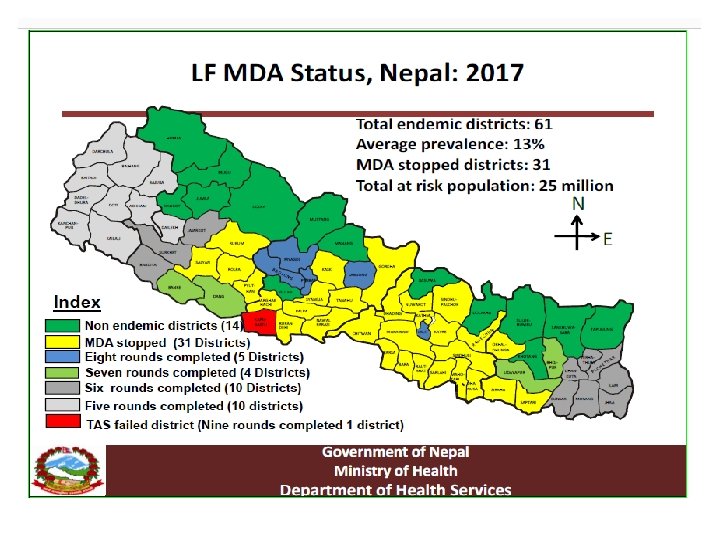
Lymphatic Filariasis: national major activities Mass Drug Administration (MDA) • Was started in Parsa district in 2003 • Gradually scaled up to all endemic districts achieving 100% geographical coverage by 2013 • MDA has been stopped (phased out) in 20 districts ( post MDA surveillance initiated in 5 districts) by 2015 year • All endemic districts completed the recommended six rounds of MDA by 2018.
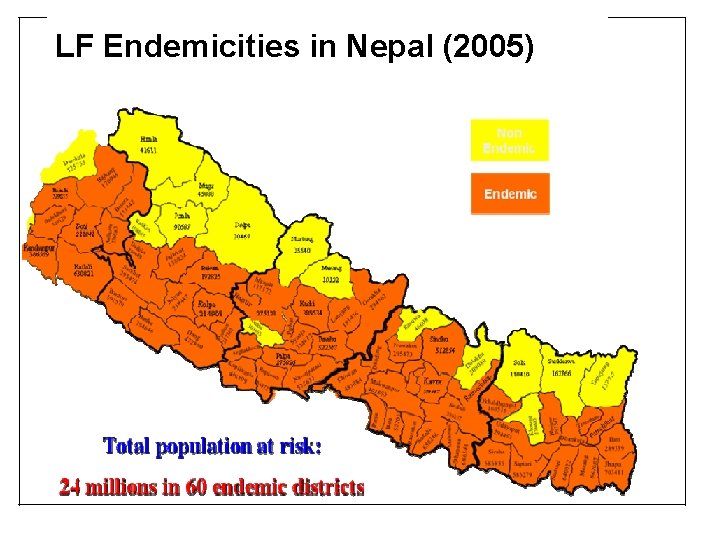
LF Endemicities in Nepal (2005)
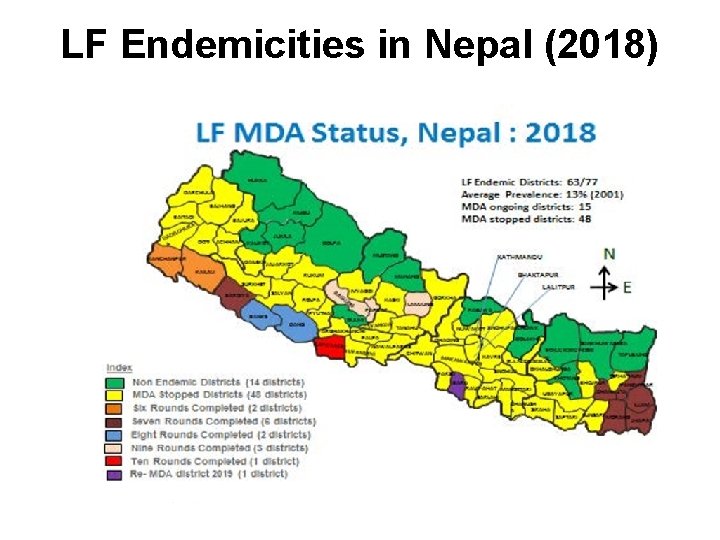
LF Endemicities in Nepal (2018)
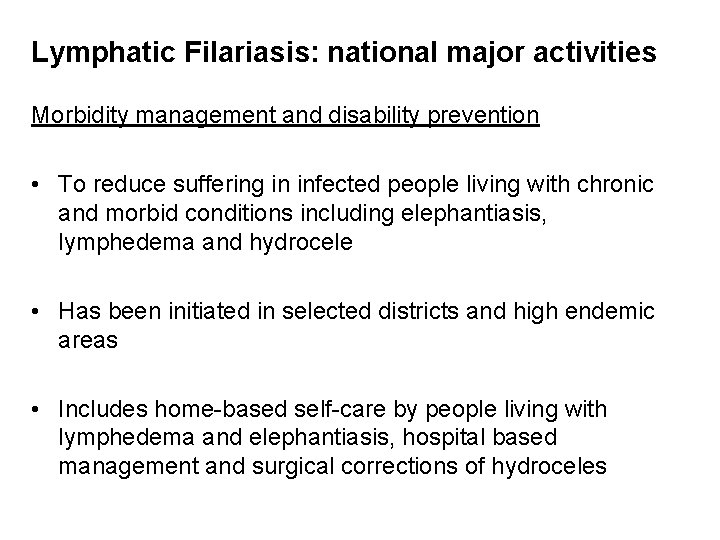
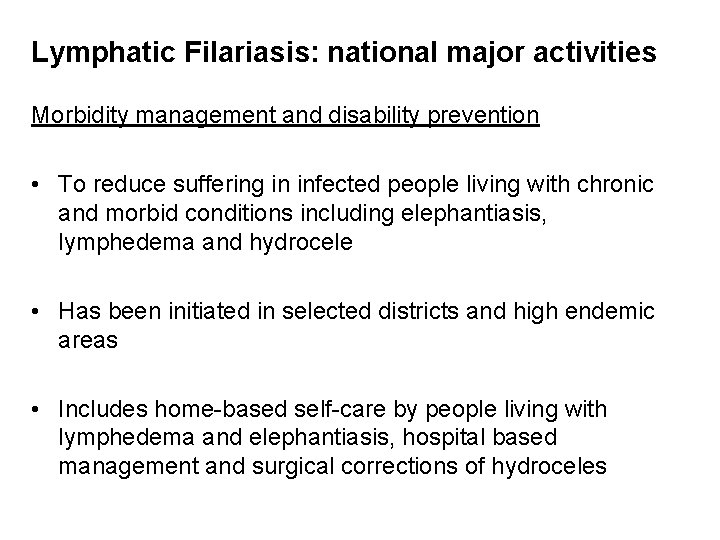
Lymphatic Filariasis: national major activities Morbidity management and disability prevention • To reduce suffering in infected people living with chronic and morbid conditions including elephantiasis, lymphedema and hydrocele • Has been initiated in selected districts and high endemic areas • Includes home-based self-care by people living with lymphedema and elephantiasis, hospital based management and surgical corrections of hydroceles
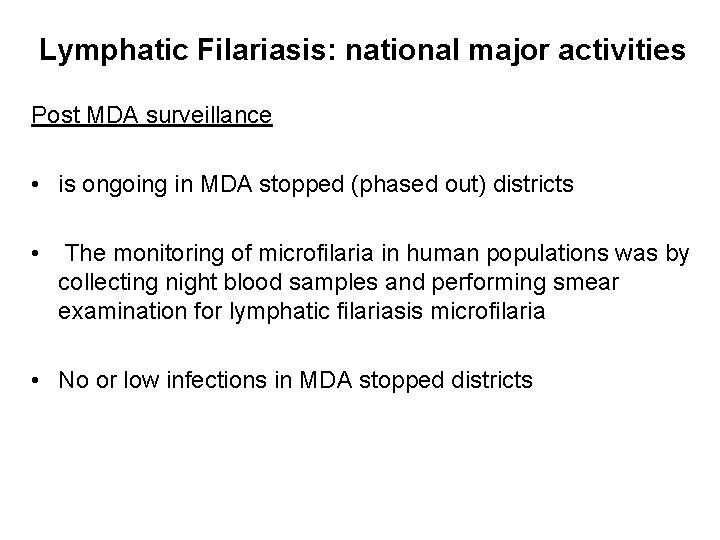
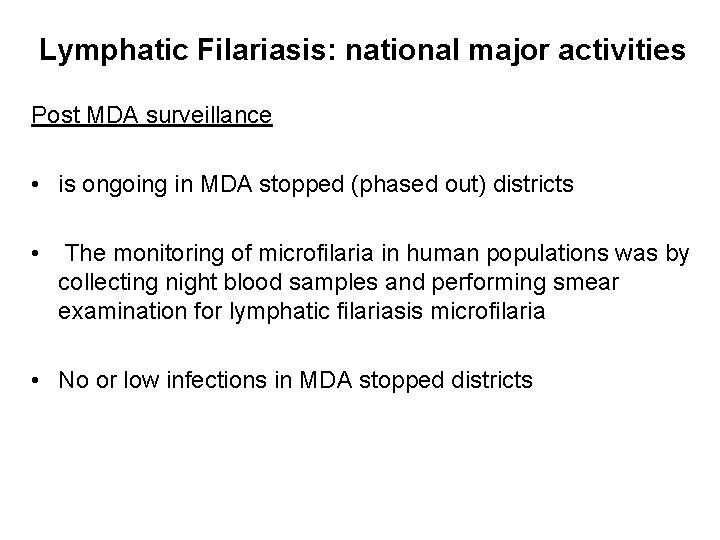
Lymphatic Filariasis: national major activities Post MDA surveillance • is ongoing in MDA stopped (phased out) districts • The monitoring of microfilaria in human populations was by collecting night blood samples and performing smear examination for lymphatic filariasis microfilaria • No or low infections in MDA stopped districts
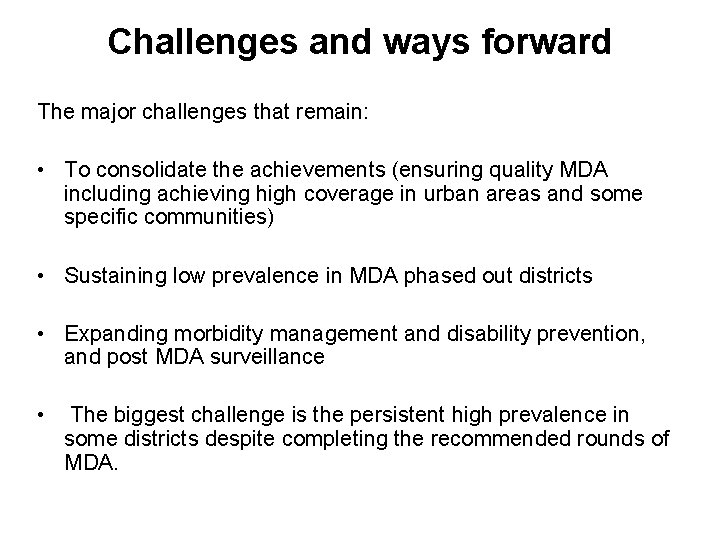
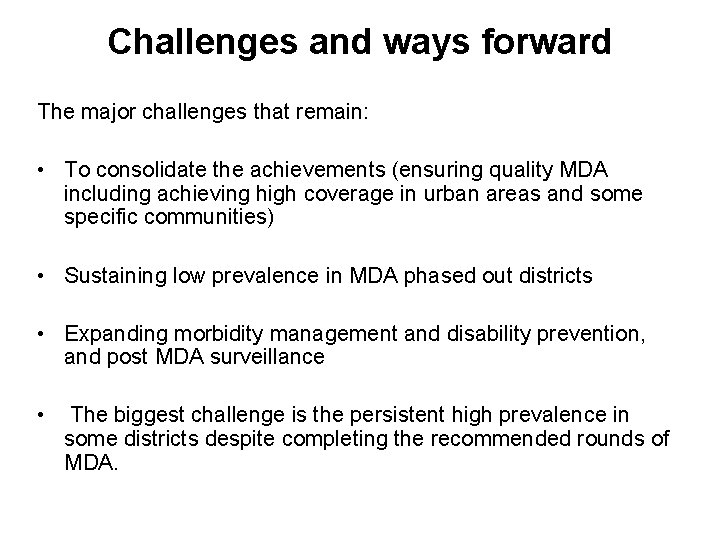
Challenges and ways forward The major challenges that remain: • To consolidate the achievements (ensuring quality MDA including achieving high coverage in urban areas and some specific communities) • Sustaining low prevalence in MDA phased out districts • Expanding morbidity management and disability prevention, and post MDA surveillance • The biggest challenge is the persistent high prevalence in some districts despite completing the recommended rounds of MDA.