Lymph Nodes Differential Diagnosis in Ultrasound Imaging p


- Slides: 58
Lymph Nodes Differential Diagnosis in Ultrasound Imaging p 199 -222 Presented by Intern郭婉吟
Outline • • • Introduction Topography Sonographic parameter for assessment Peripheral lymph nodes Abdominal lymph nodes
Introduction • Essential barrier of the secondary immune system • Diameter: 0. 2 cm ~ 2. 5 cm Ø Functional state Ø Age of the patient • Assessment of possible malignancy: Ø Clinical picture Ø Ultrasound findings • Differential diagnosis of LAP
Differential diagnosis of LAP Infectious disease ► ► ► * • • Viral infection Infectious mononucleosis (EBV), cytomegalic inclusion disease, infectious hepatitis, AIDS, rubella, human herpesvirus 3 (varicella zoster) Bacterial infection Streptococci, staphylococci, salmonellae, Tropheryma whippelii (Whipple disease), Francisella tularensis (tularemia) Mycotic infection Histoplasmosis, coccidioidomycosis, blastomycosis Chlamydial infection Lymphogranuloma venereum, cat scratch disease, trachoma Mycobacterial infection Toxoplasmosis, trypanosomosis, microfilariae Spirochetosis Syphilis, leptospirosis Malignancy • • • Hodgkin disease, non Hodgkin lymphoma, chronic lymphocytic leukemia, acute lympho cytic leukemia Myelogenous leukemia (chloromas = extramedullary manifestation of myelogenous leu kosis): acute myelogenous leukemia, blast crisis in chronic myelogenous leukemia Metastasis of epithelial or mesenchymal tumors Immunological disease • • Rheumatoid arthritis Systemic lupus erythematosus Dermatomyositis Allergic reaction to drugs such as phenytoin, hydralazine, allopurinol Other • • Sarcoidosis Lipid storage disease (Caucher disease, Niemann Pick disease)
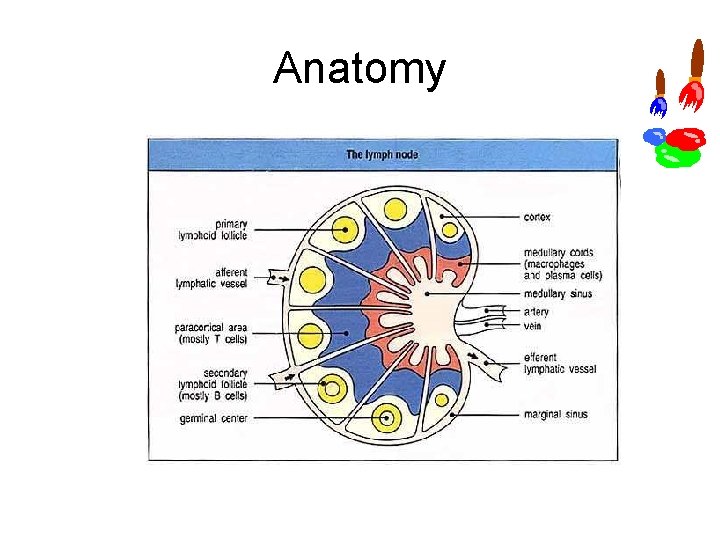
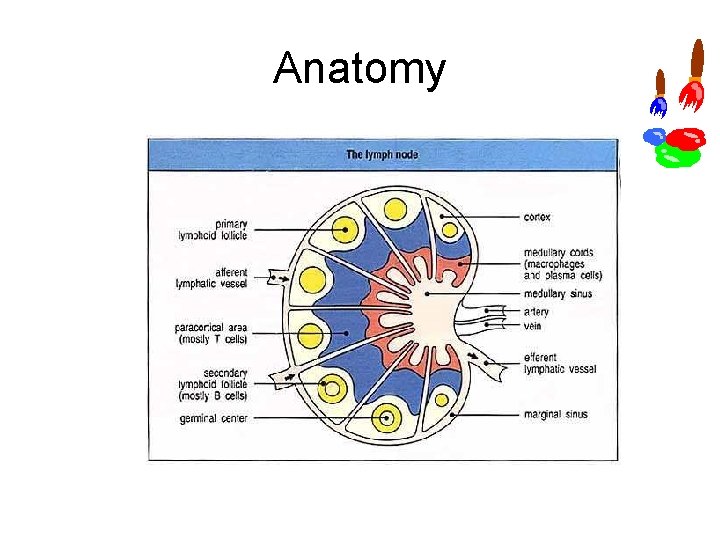
Anatomy
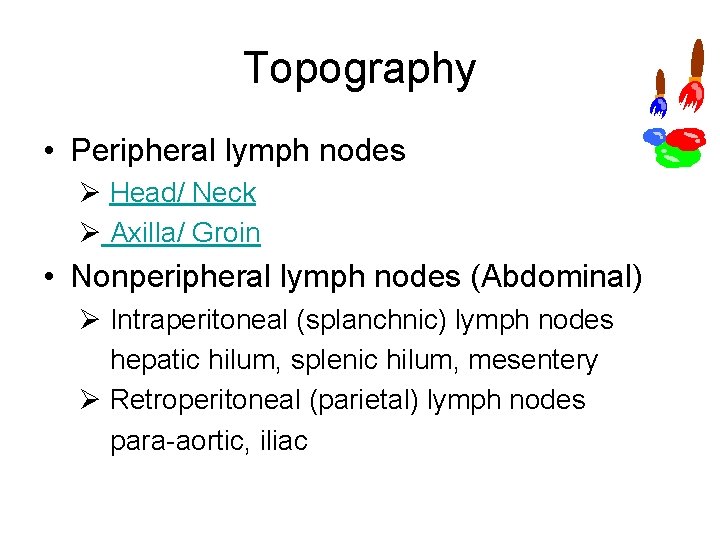
Topography • Peripheral lymph nodes Ø Head/ Neck Ø Axilla/ Groin • Nonperipheral lymph nodes (Abdominal) Ø Intraperitoneal (splanchnic) lymph nodes hepatic hilum, splenic hilum, mesentery Ø Retroperitoneal (parietal) lymph nodes para aortic, iliac
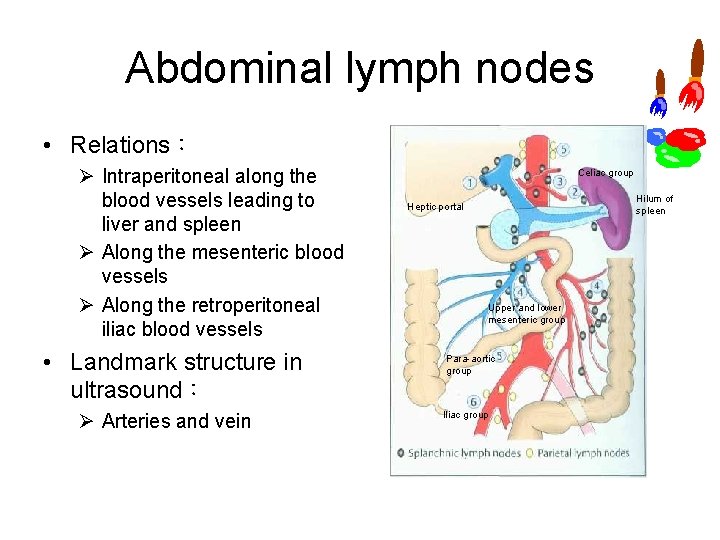
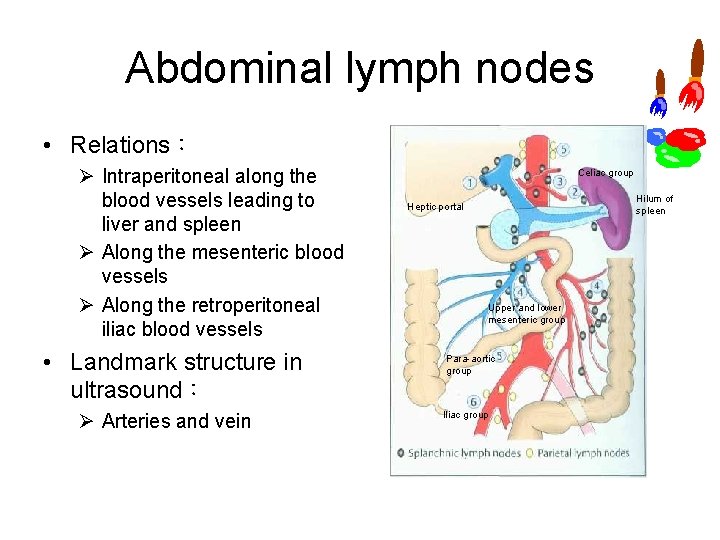
Abdominal lymph nodes • Relations: Ø Intraperitoneal along the blood vessels leading to liver and spleen Ø Along the mesenteric blood vessels Ø Along the retroperitoneal iliac blood vessels • Landmark structure in ultrasound: Ø Arteries and vein Celiac group Hilum of spleen Heptic portal Upper and lower mesenteric group Para aortic group Iliac group
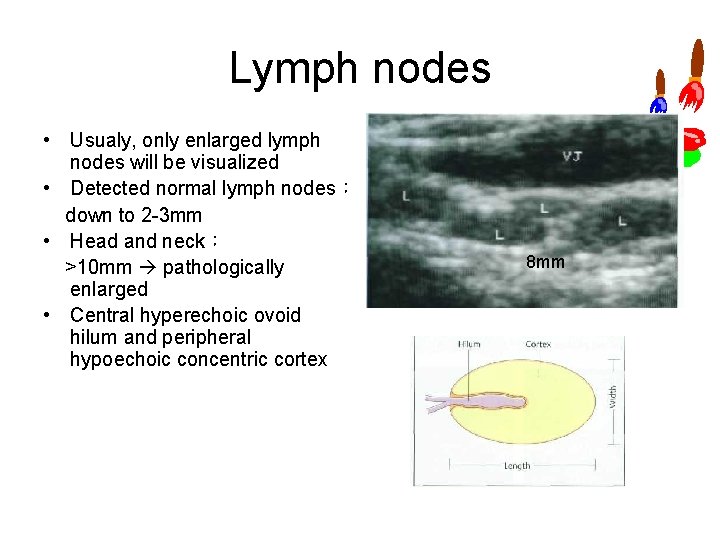
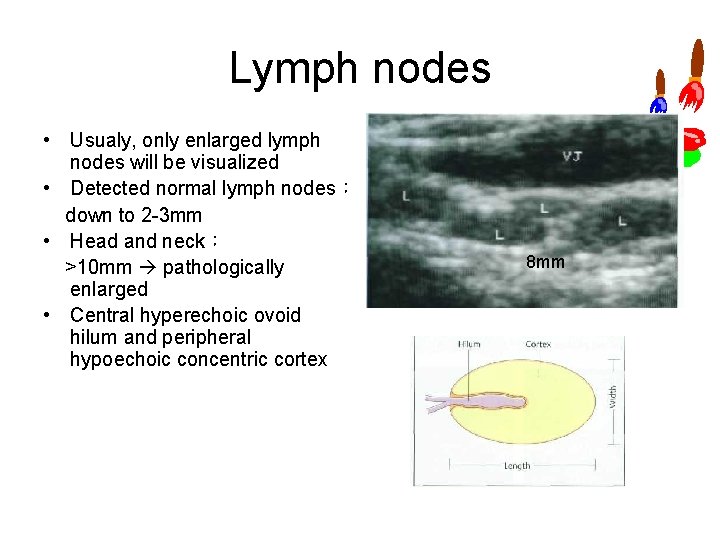
Lymph nodes • Usualy, only enlarged lymph nodes will be visualized • Detected normal lymph nodes: down to 2 3 mm • Head and neck: >10 mm pathologically enlarged • Central hyperechoic ovoid hilum and peripheral hypoechoic concentric cortex 8 mm
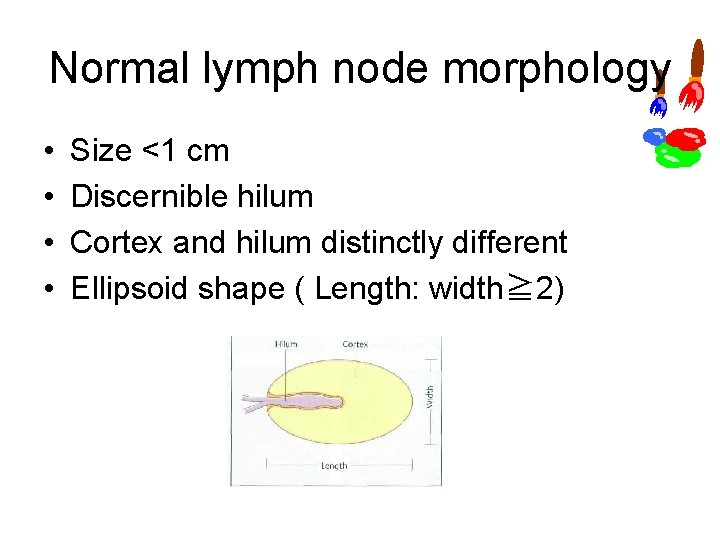
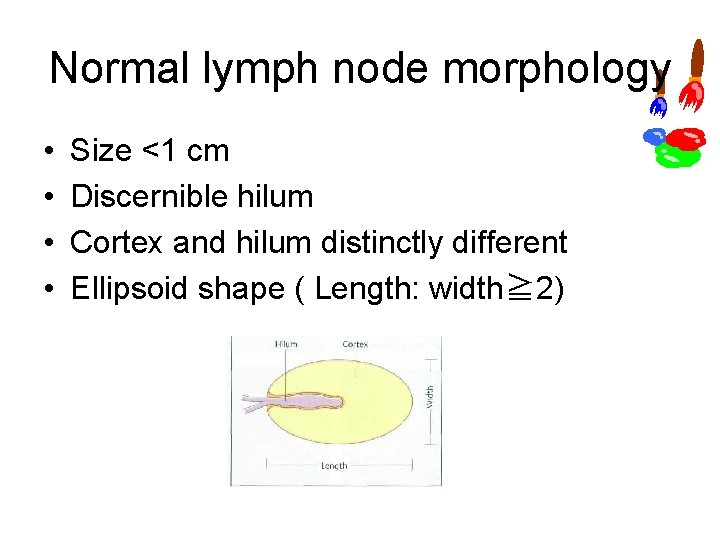
Normal lymph node morphology • • Size <1 cm Discernible hilum Cortex and hilum distinctly different Ellipsoid shape ( Length: width≧ 2)
Sonographic parameters for lymph node assessment l • • • Location Region involved Pattern of involvement Morphology Size Shape Delineation from adjacent tissue Structural parameters Hilar sign Echogenicity Homogeneity Vascularization Concentration of blood vessels Pattern of vascularization Flow parameters
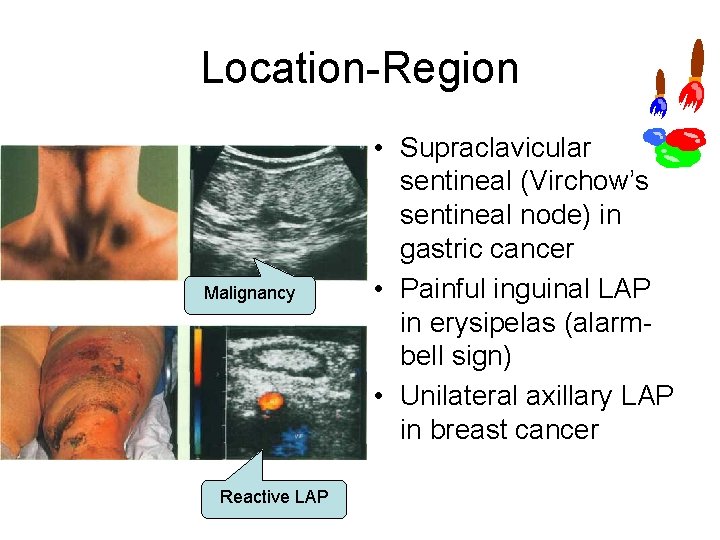
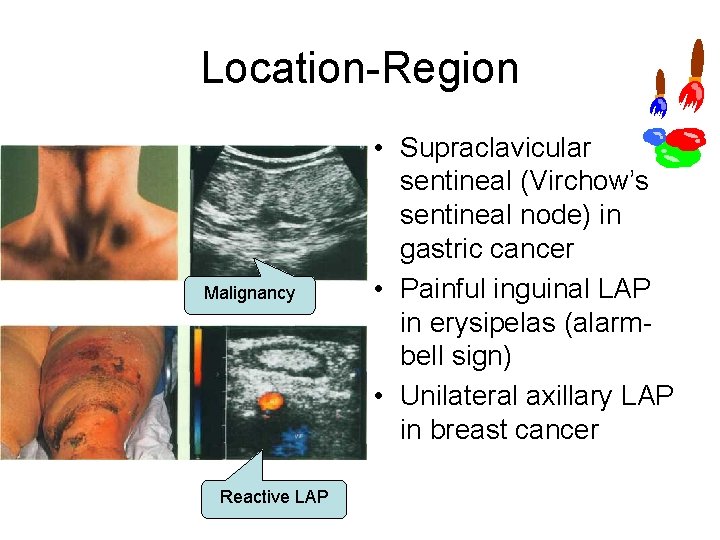
Location Region Malignancy Reactive LAP • Supraclavicular sentineal (Virchow’s sentineal node) in gastric cancer • Painful inguinal LAP in erysipelas (alarm bell sign) • Unilateral axillary LAP in breast cancer
Location Pattern • Localized or generally spread • Relation with the blood vessels – Vascular invasion: Contact between the tumor and the vascular wall > 3. 5 cm or >1/2 the circumference
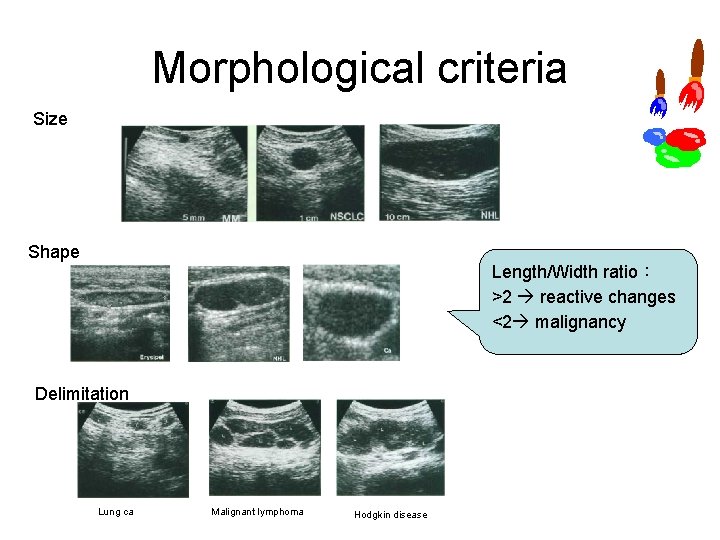
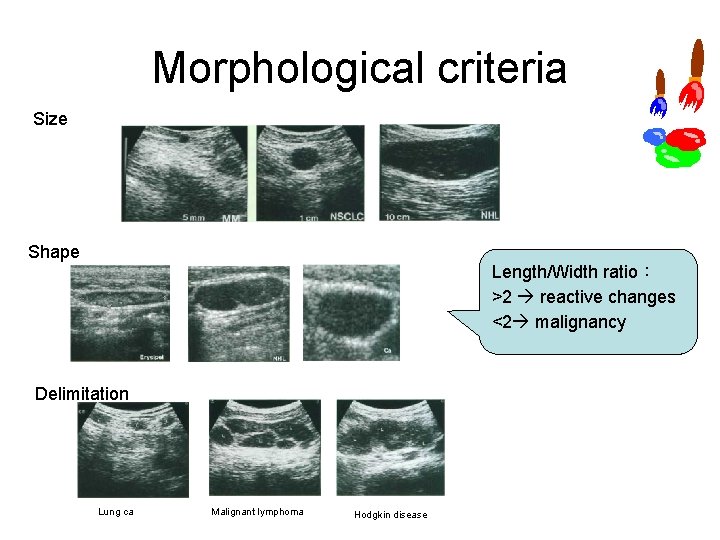
Morphological criteria Size Shape Length/Width ratio: >2 reactive changes <2 malignancy Delimitation Lung ca Malignant lymphoma Hodgkin disease

Structural parameters • Hilar sign:indicative of malignant LAP • Echogenicity: Ø Malignant lymphoma hypoechoic Ø Cancer metastasis, chronic inflammation or regression scars hyperechoic Malignant lymphoma Ovarian cancer CLL
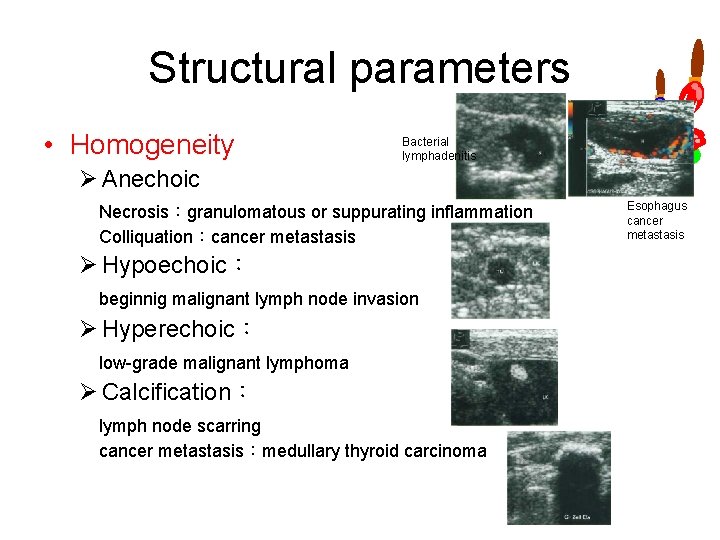
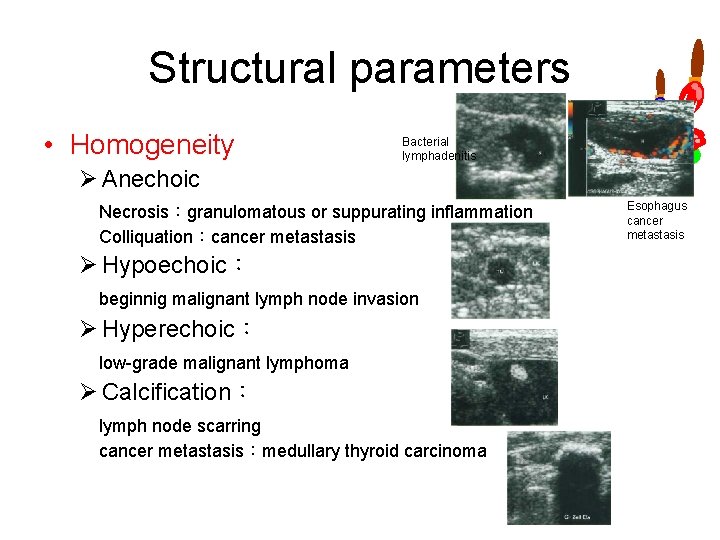
Structural parameters • Homogeneity Bacterial lymphadenitis Ø Anechoic Necrosis:granulomatous or suppurating inflammation Colliquation:cancer metastasis Ø Hypoechoic: beginnig malignant lymph node invasion Ø Hyperechoic: low grade malignant lymphoma Ø Calcification: lymph node scarring cancer metastasis:medullary thyroid carcinoma Esophagus cancer metastasis
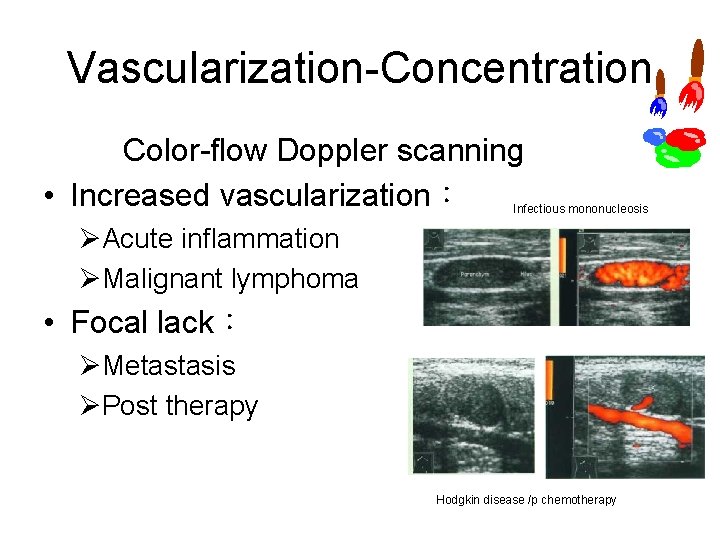
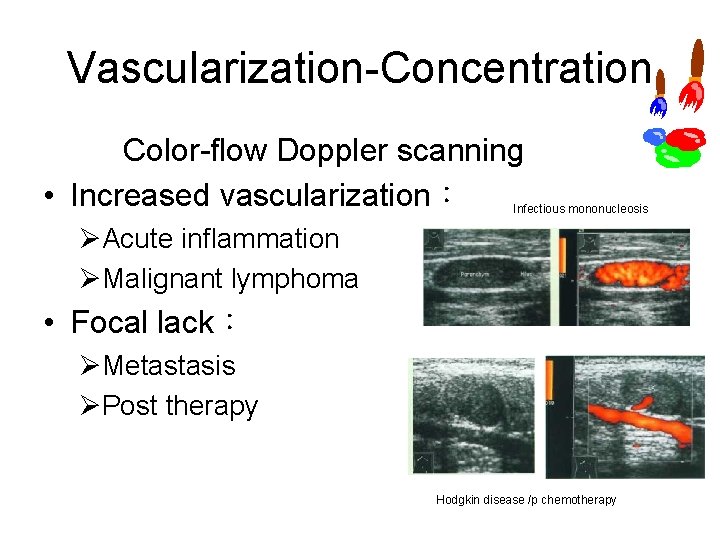
Vascularization Concentration Color flow Doppler scanning • Increased vascularization: Infectious mononucleosis ØAcute inflammation ØMalignant lymphoma • Focal lack: ØMetastasis ØPost therapy Hodgkin disease /p chemotherapy
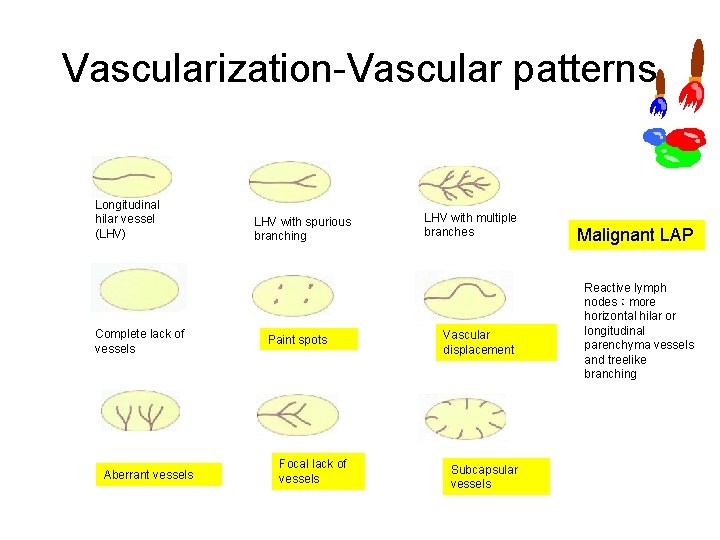
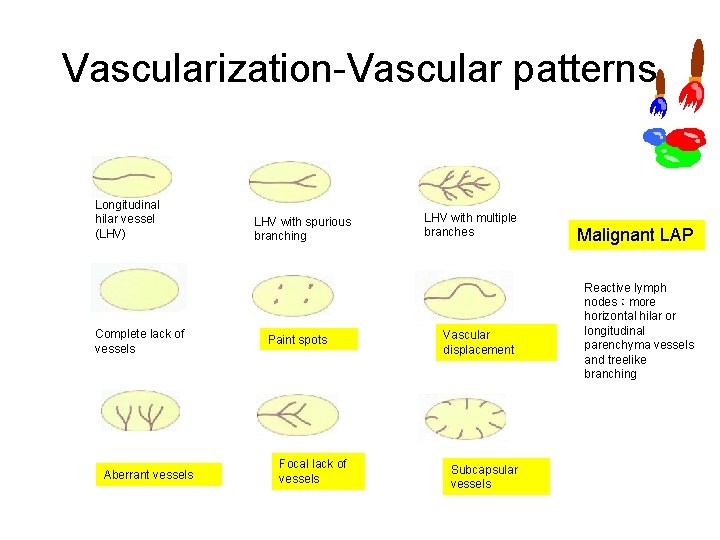
Vascularization Vascular patterns Longitudinal hilar vessel (LHV) Complete lack of vessels Aberrant vessels LHV with spurious branching Paint spots Focal lack of vessels LHV with multiple branches Vascular displacement Subcapsular vessels Malignant LAP Reactive lymph nodes:more horizontal hilar or longitudinal parenchyma vessels and treelike branching
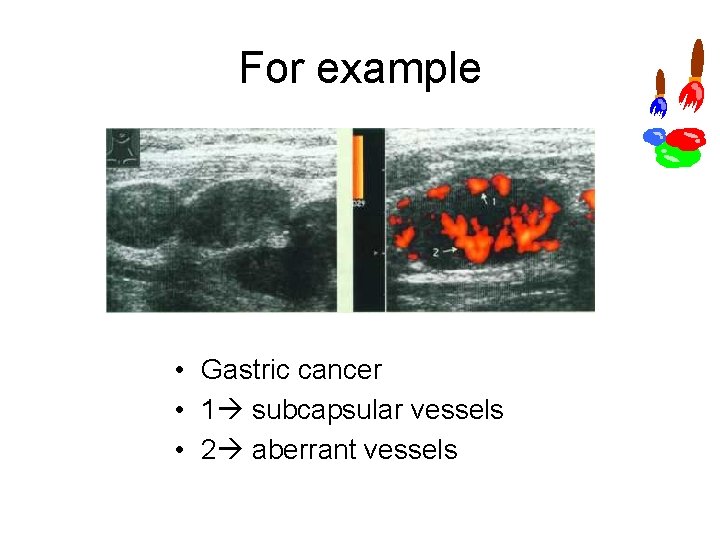
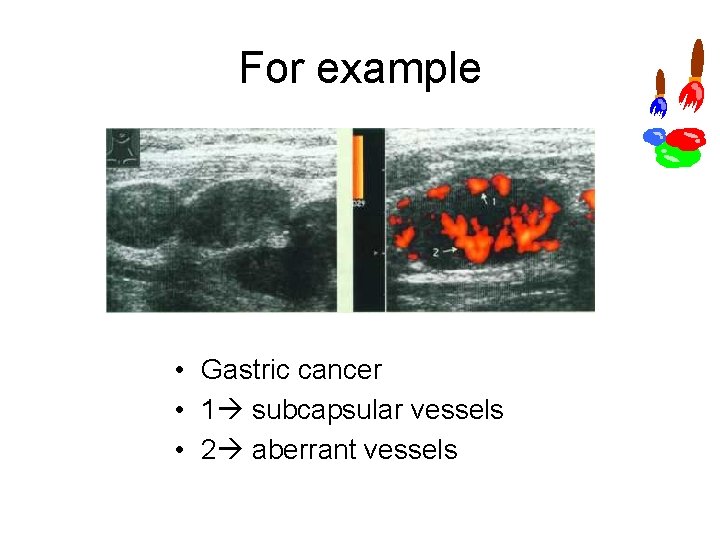
For example • Gastric cancer • 1 subcapsular vessels • 2 aberrant vessels
Vascularization Flow parameters • Resistance index (RI) • Pulsatility index (PI) RI > 85:lymph node invaded by metastasis
Abdominal lymph nodes • Sonographic parameters of the vascularization are difficult to obtain. • Differential diagnosis: location and morphology • In most cases, impossible to demonstrate the hilum.
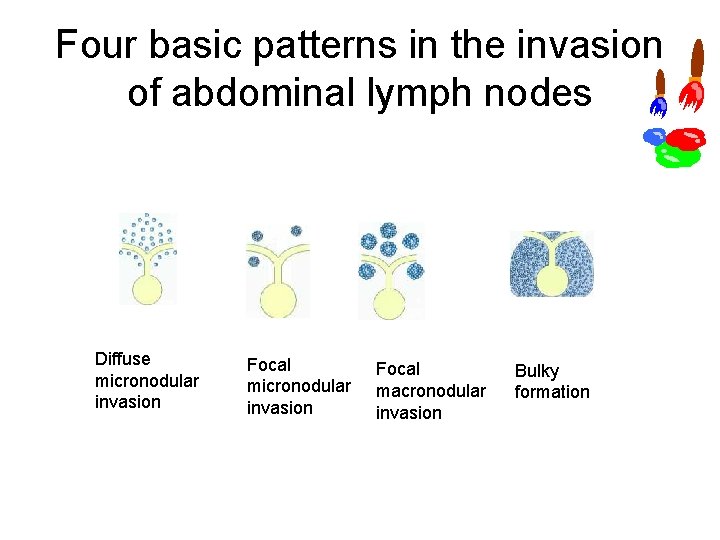
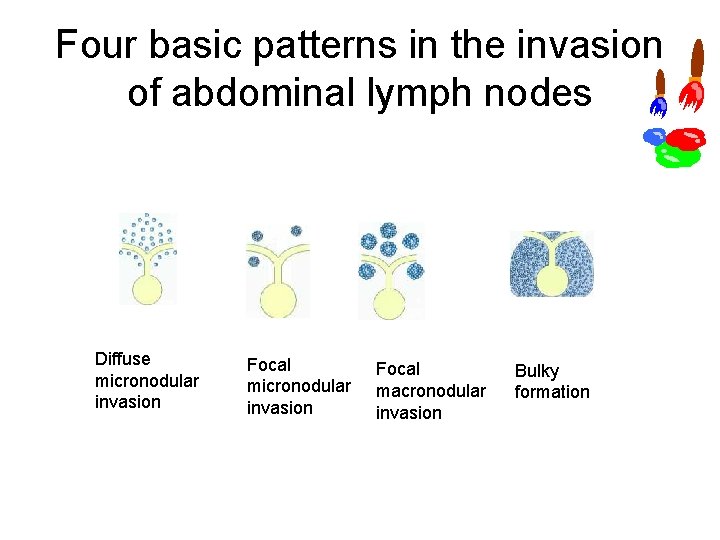
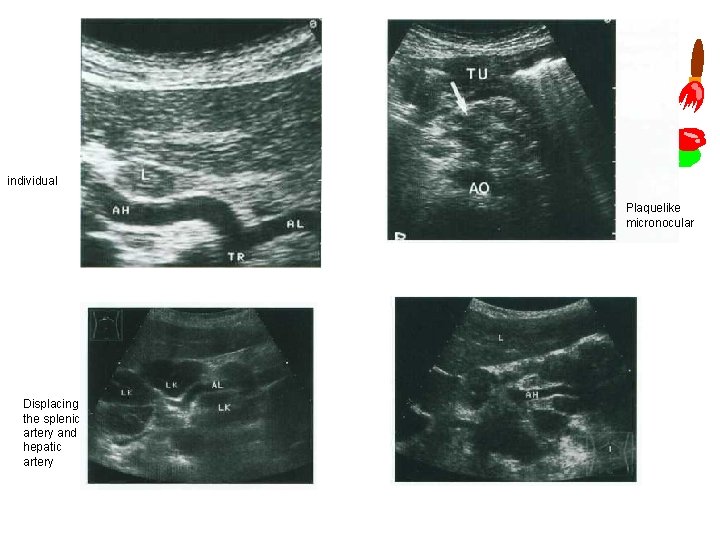
Four basic patterns in the invasion of abdominal lymph nodes Diffuse micronodular invasion Focal macronodular invasion Bulky formation
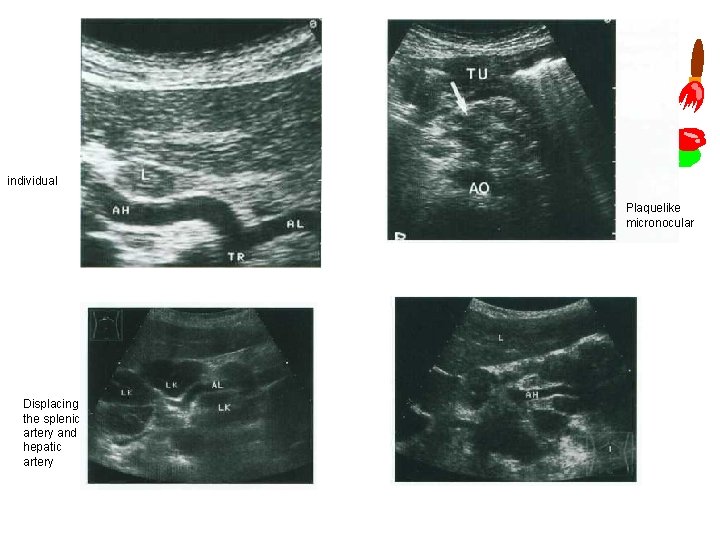
individual Plaquelike micronocular Displacing the splenic artery and hepatic artery
Disadvantages • • • Only enlarged lymph nodes will be detected. Specificity is rather low in lumbar and iliac lymph nodes. Intestinal gas can limit the usefulness of the study. Misdiagnosis is possible in solitary lympho mas. It requires substantial experience of the operator in terms of technique and assessment.
Peripheral lymph nodes • Head / Neck • Extremities (Axilla, Groin) Inflammatory lymph nodes Metastases Malignant lymphoma Other structures
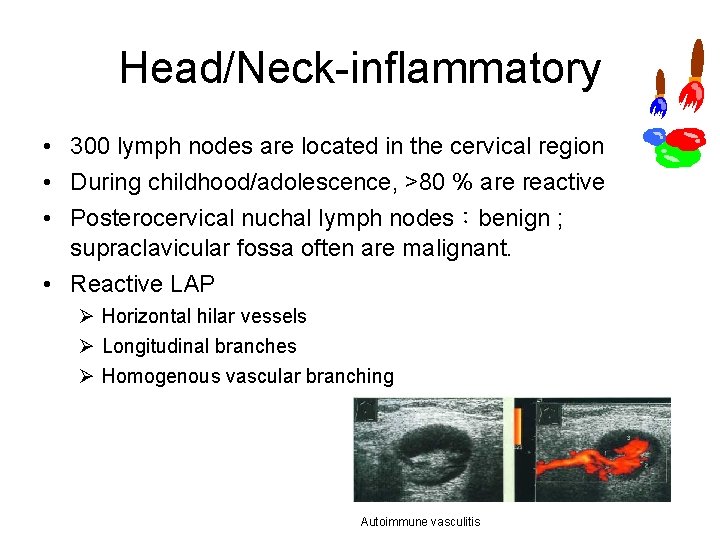
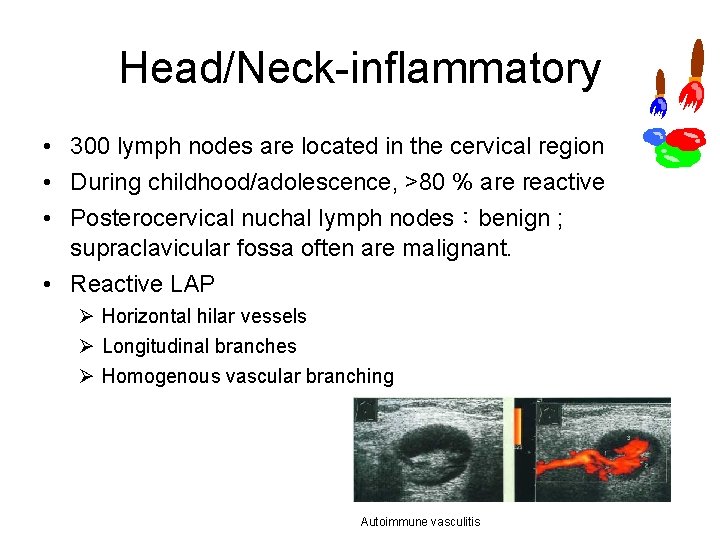
Head/Neck inflammatory • 300 lymph nodes are located in the cervical region • During childhood/adolescence, >80 % are reactive • Posterocervical nuchal lymph nodes:benign ; supraclavicular fossa often are malignant. • Reactive LAP Ø Horizontal hilar vessels Ø Longitudinal branches Ø Homogenous vascular branching Autoimmune vasculitis
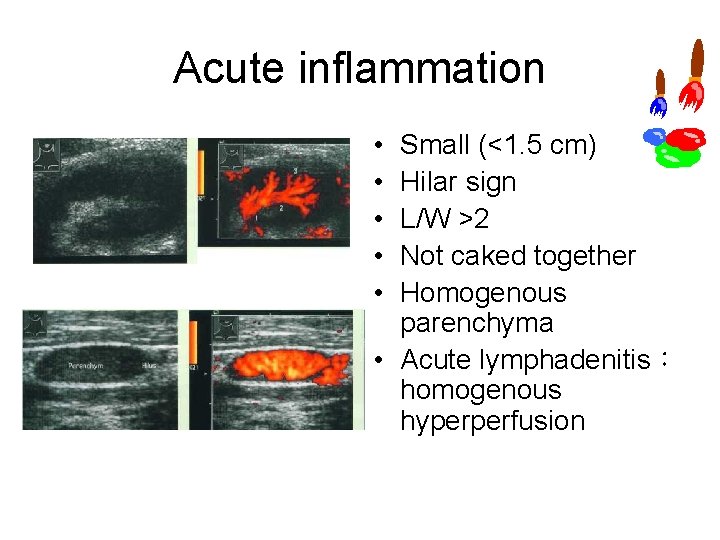
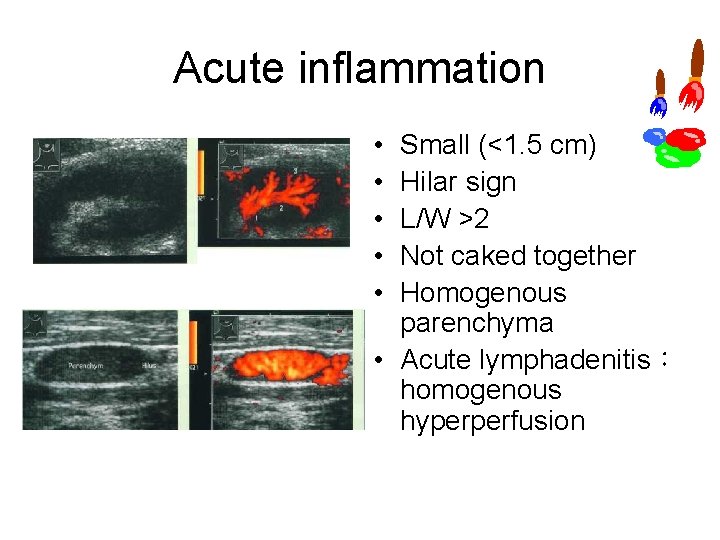
Acute inflammation • • • Small (<1. 5 cm) Hilar sign L/W >2 Not caked together Homogenous parenchyma • Acute lymphadenitis: homogenous hyperperfusion
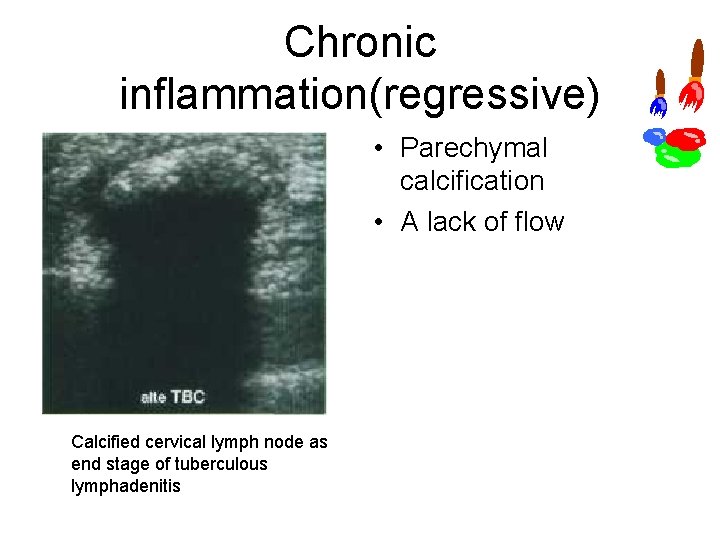
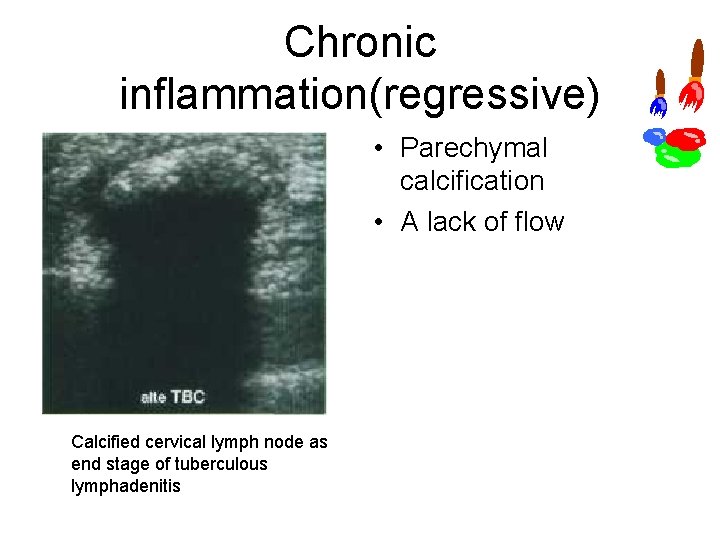
Chronic inflammation(regressive) • Parechymal calcification • A lack of flow Calcified cervical lymph node as end stage of tuberculous lymphadenitis
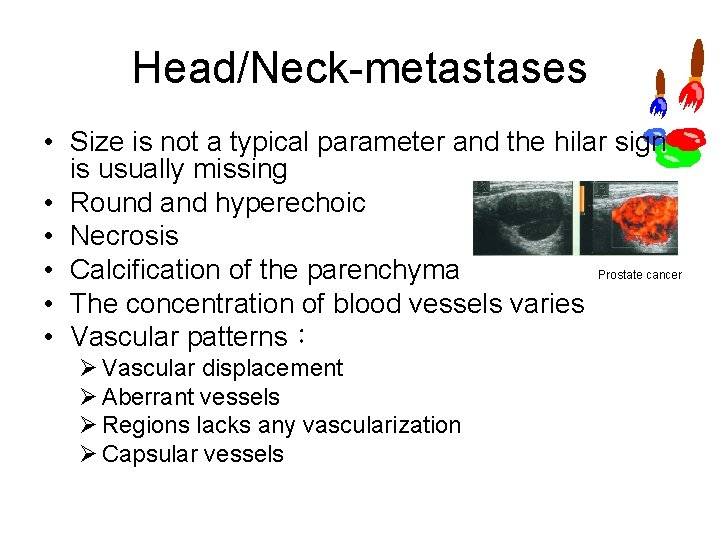
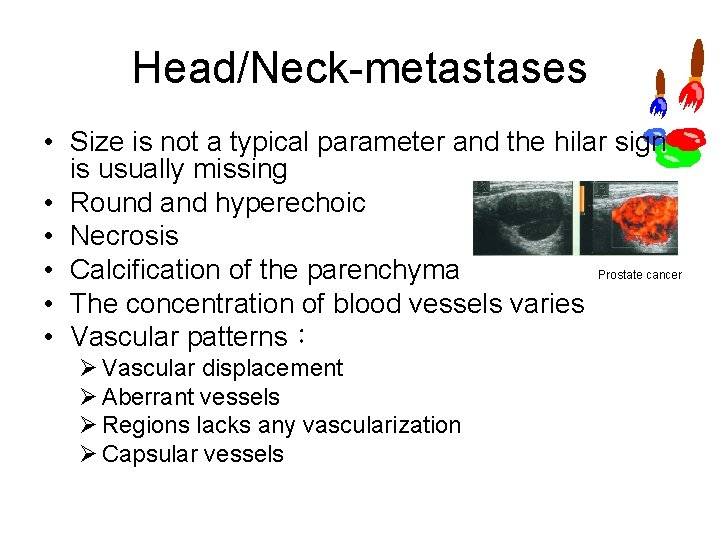
Head/Neck metastases • Size is not a typical parameter and the hilar sign is usually missing • Round and hyperechoic • Necrosis Prostate cancer • Calcification of the parenchyma • The concentration of blood vessels varies • Vascular patterns: Ø Vascular displacement Ø Aberrant vessels Ø Regions lacks any vascularization Ø Capsular vessels
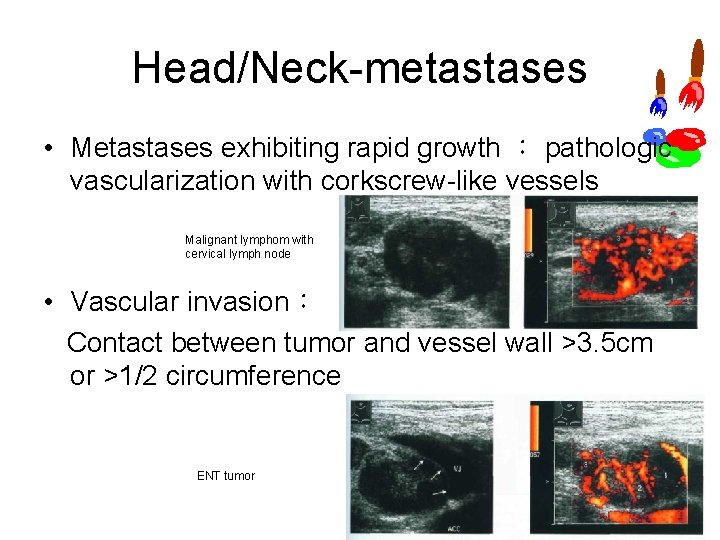
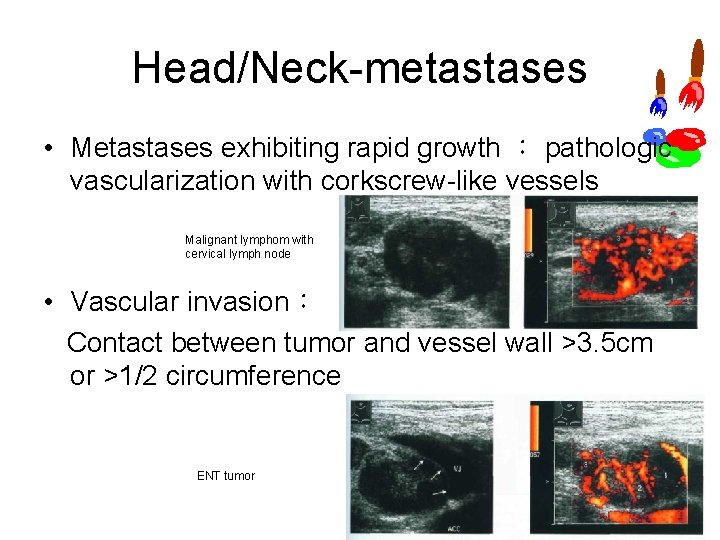
Head/Neck metastases • Metastases exhibiting rapid growth : pathologic vascularization with corkscrew like vessels Malignant lymphom with cervical lymph node • Vascular invasion: Contact between tumor and vessel wall >3. 5 cm or >1/2 circumference ENT tumor
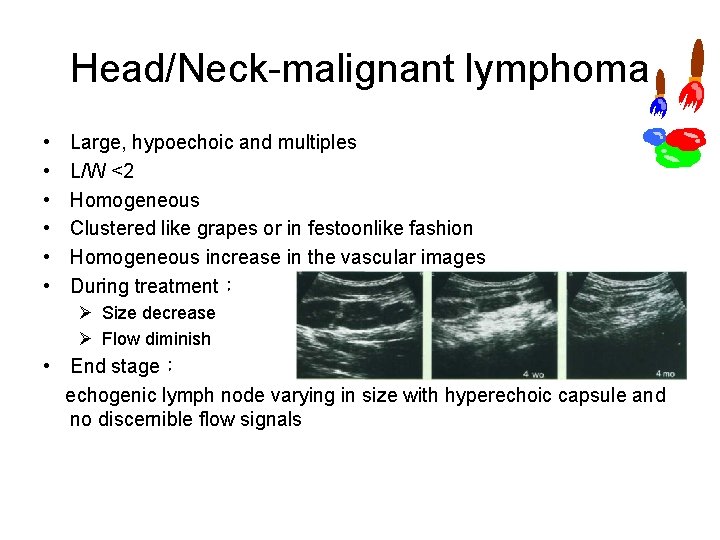
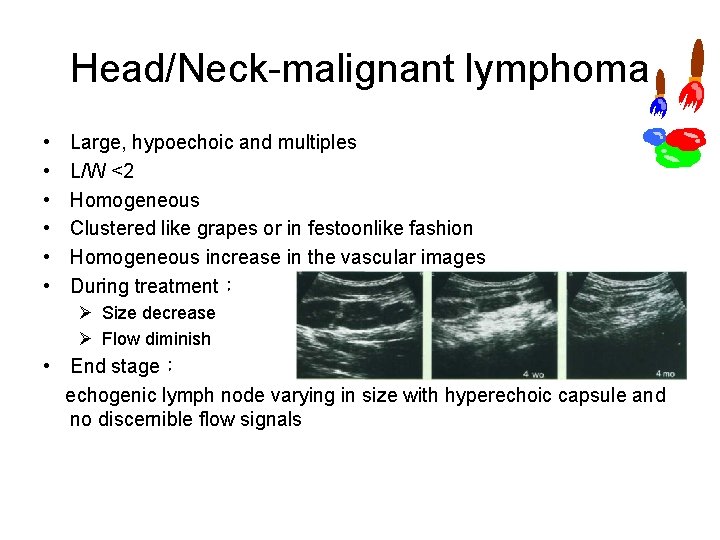
Head/Neck malignant lymphoma • • • Large, hypoechoic and multiples L/W <2 Homogeneous Clustered like grapes or in festoonlike fashion Homogeneous increase in the vascular images During treatment: Ø Size decrease Ø Flow diminish • End stage: echogenic lymph node varying in size with hyperechoic capsule and no discernible flow signals
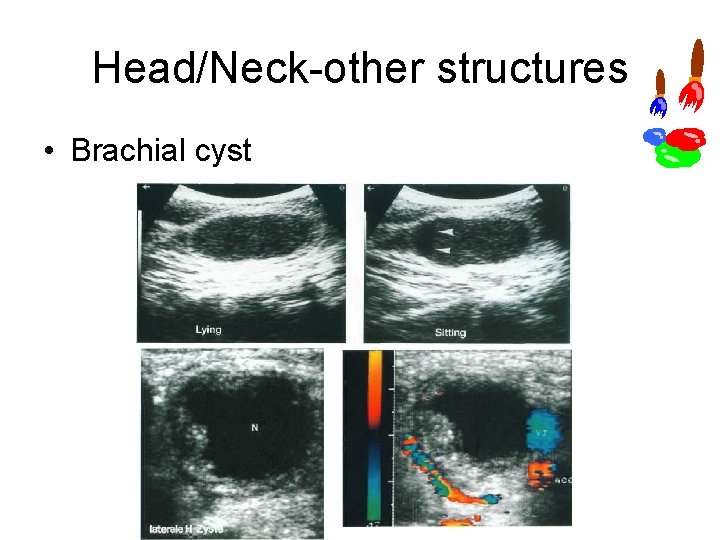
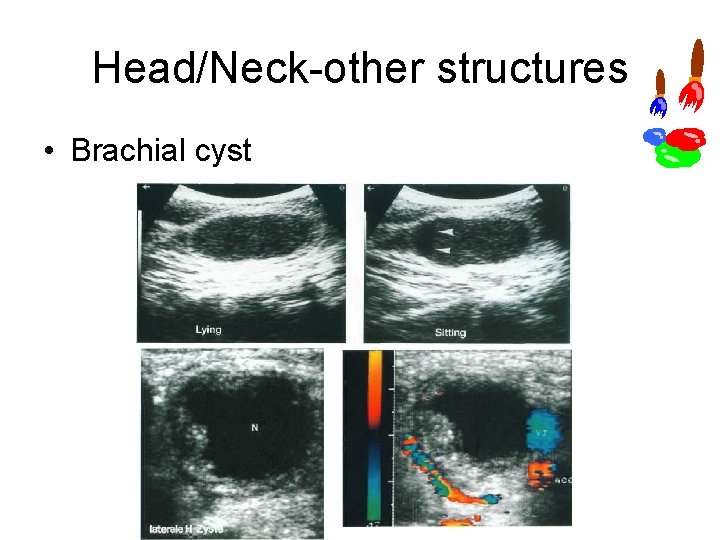
Head/Neck other structures • Brachial cyst
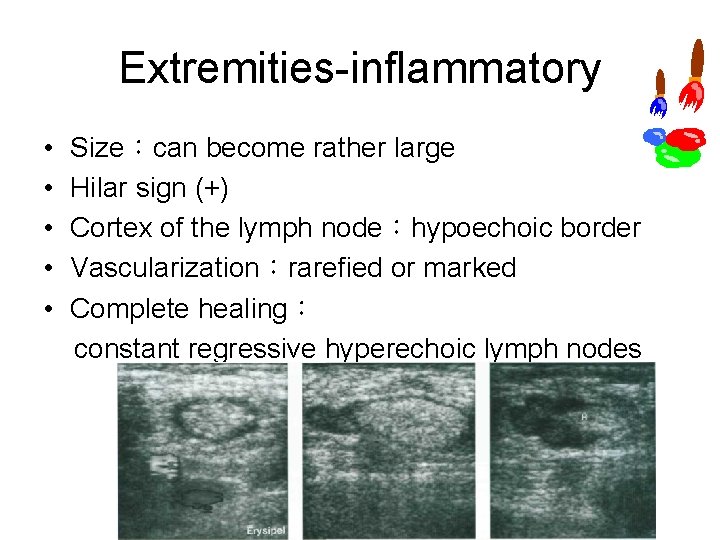
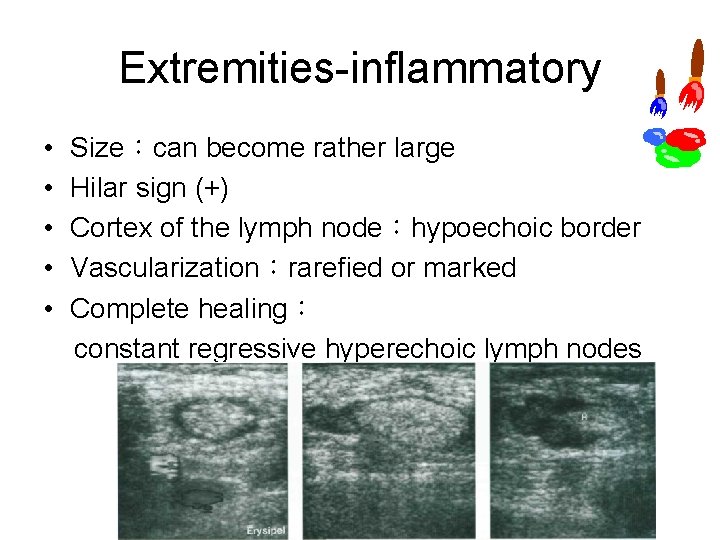
Extremities inflammatory • • • Size:can become rather large Hilar sign (+) Cortex of the lymph node:hypoechoic border Vascularization:rarefied or marked Complete healing: constant regressive hyperechoic lymph nodes
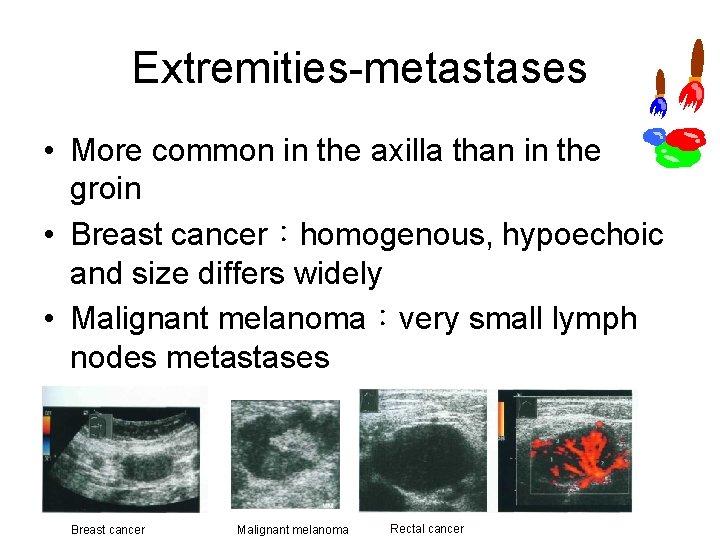
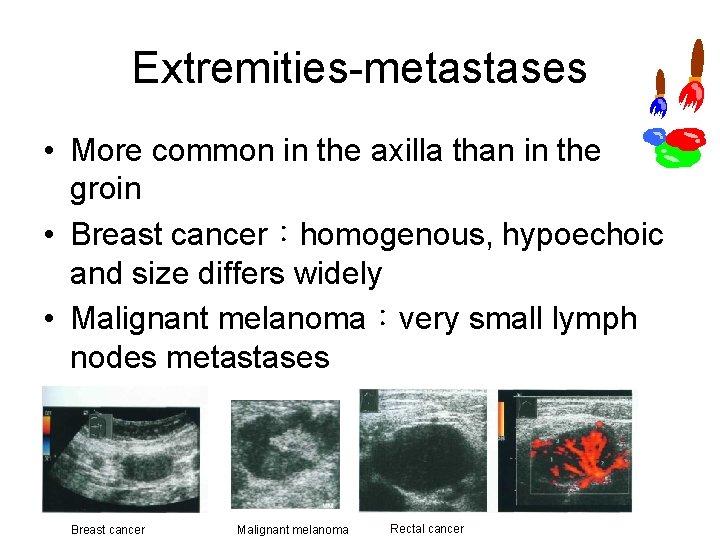
Extremities metastases • More common in the axilla than in the groin • Breast cancer:homogenous, hypoechoic and size differs widely • Malignant melanoma:very small lymph nodes metastases Breast cancer Malignant melanoma Rectal cancer
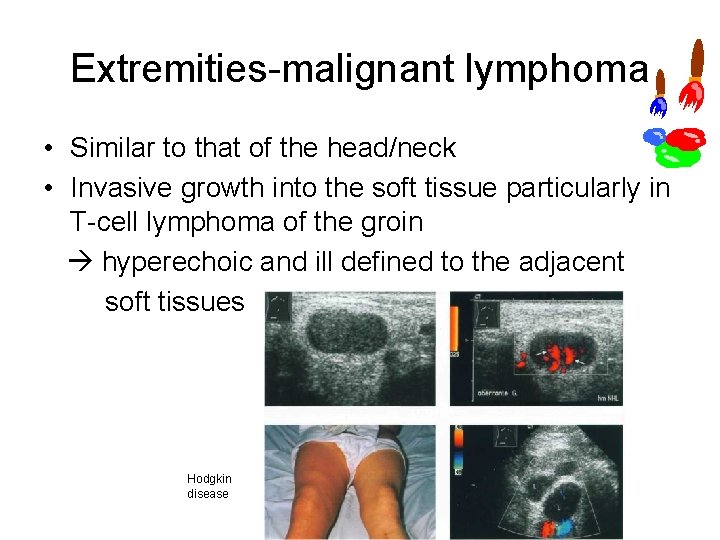
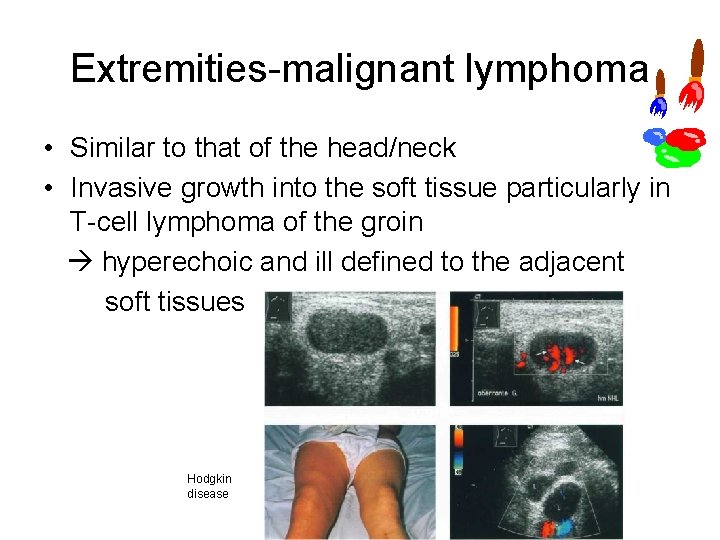
Extremities malignant lymphoma • Similar to that of the head/neck • Invasive growth into the soft tissue particularly in T cell lymphoma of the groin hyperechoic and ill defined to the adjacent soft tissues Hodgkin disease
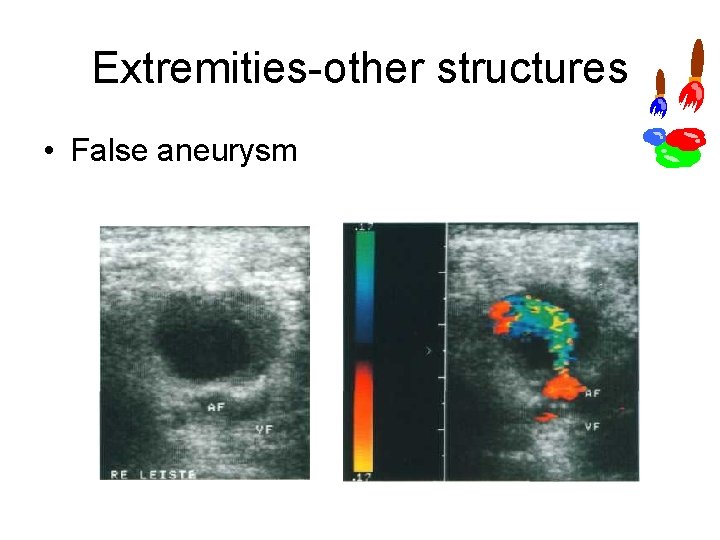
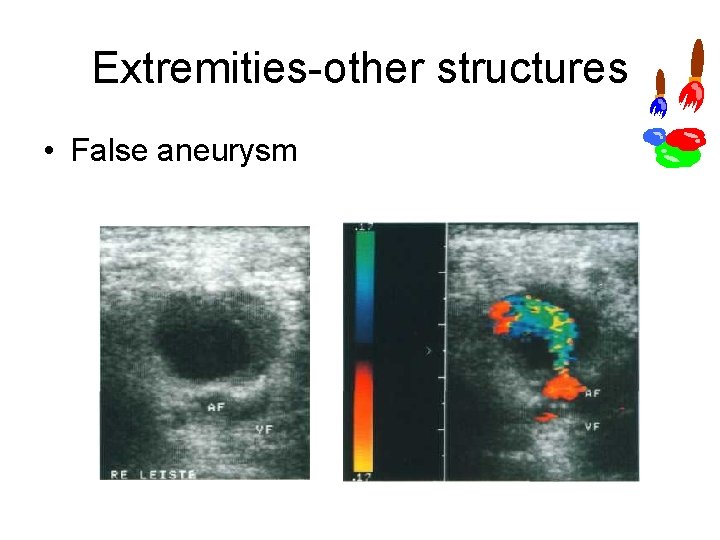
Extremities other structures • False aneurysm
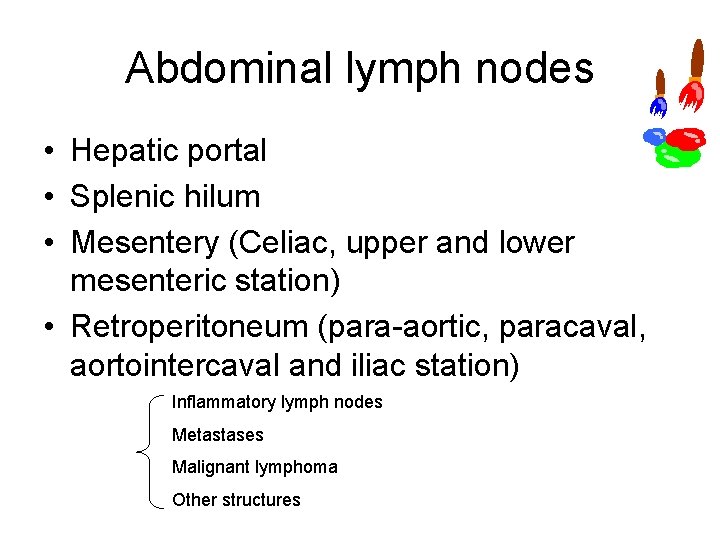
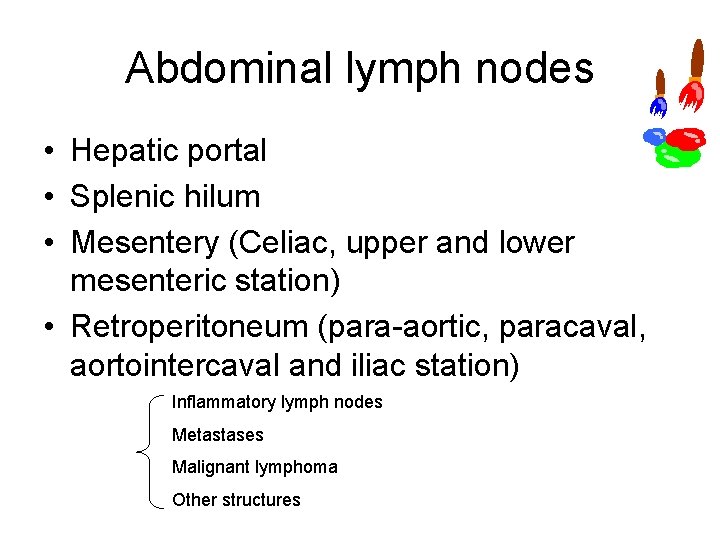
Abdominal lymph nodes • Hepatic portal • Splenic hilum • Mesentery (Celiac, upper and lower mesenteric station) • Retroperitoneum (para aortic, paracaval, aortointercaval and iliac station) Inflammatory lymph nodes Metastases Malignant lymphoma Other structures
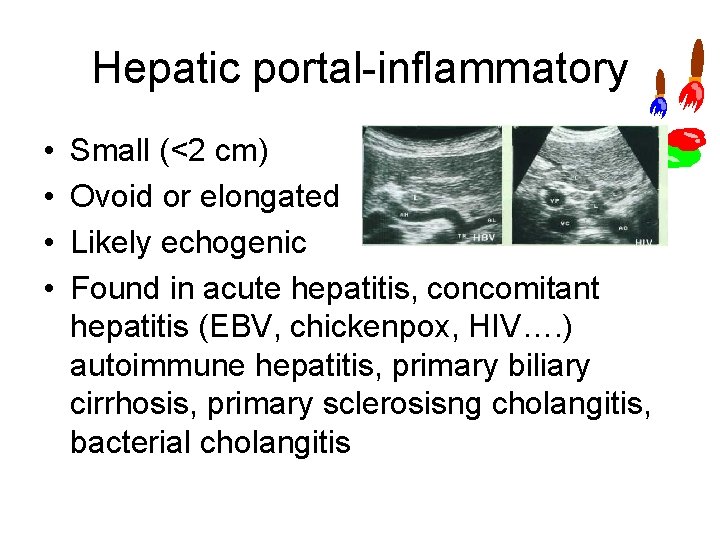
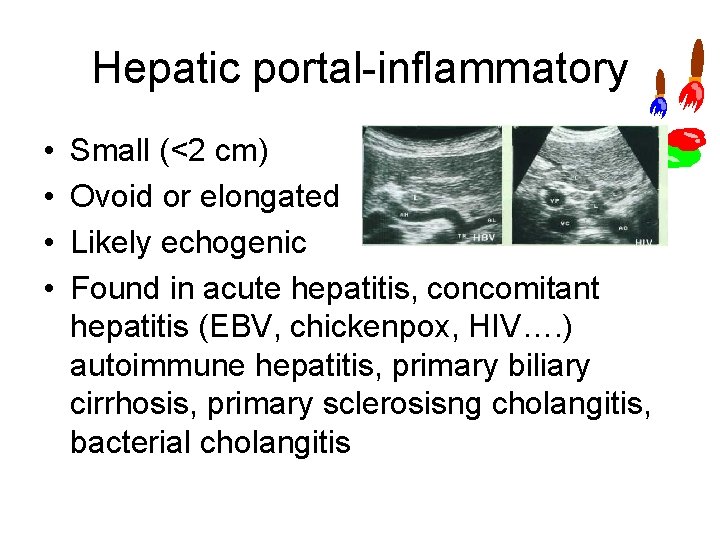
Hepatic portal inflammatory • • Small (<2 cm) Ovoid or elongated Likely echogenic Found in acute hepatitis, concomitant hepatitis (EBV, chickenpox, HIV…. ) autoimmune hepatitis, primary biliary cirrhosis, primary sclerosisng cholangitis, bacterial cholangitis
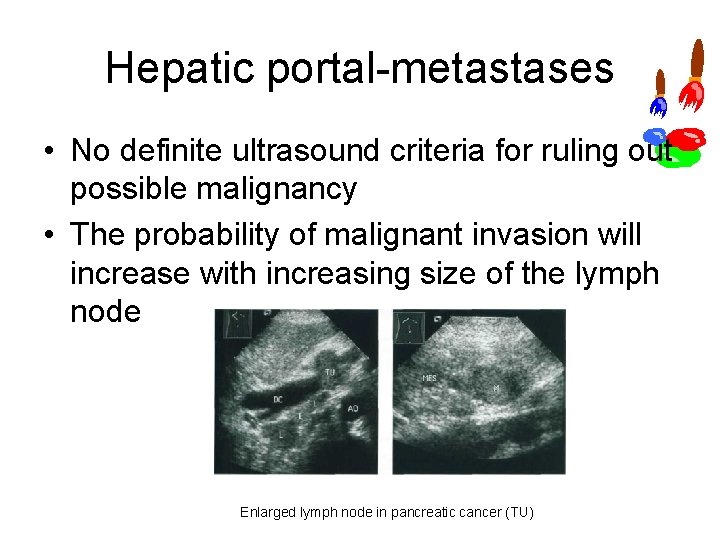
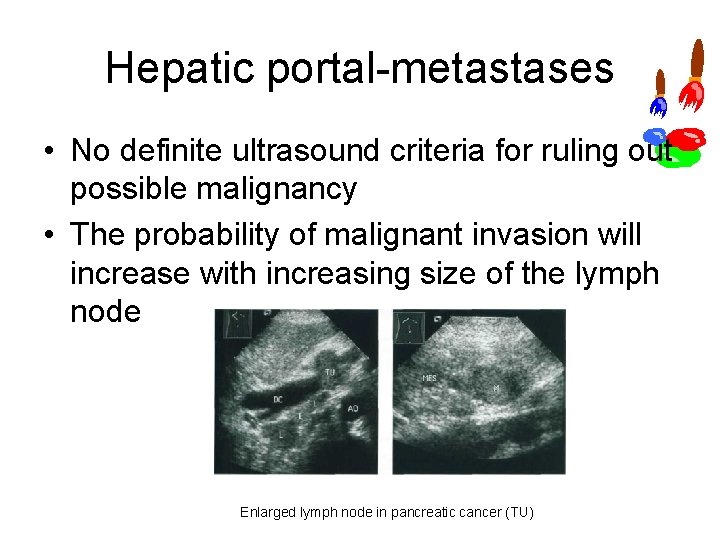
Hepatic portal metastases • No definite ultrasound criteria for ruling out possible malignancy • The probability of malignant invasion will increase with increasing size of the lymph node Enlarged lymph node in pancreatic cancer (TU)
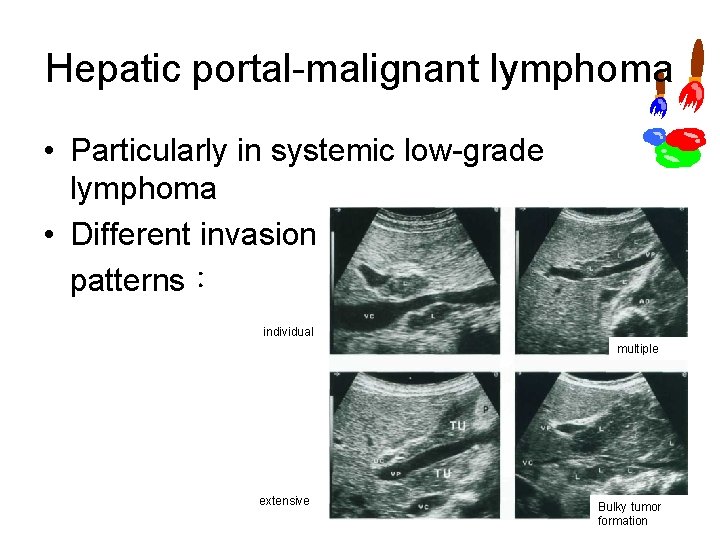
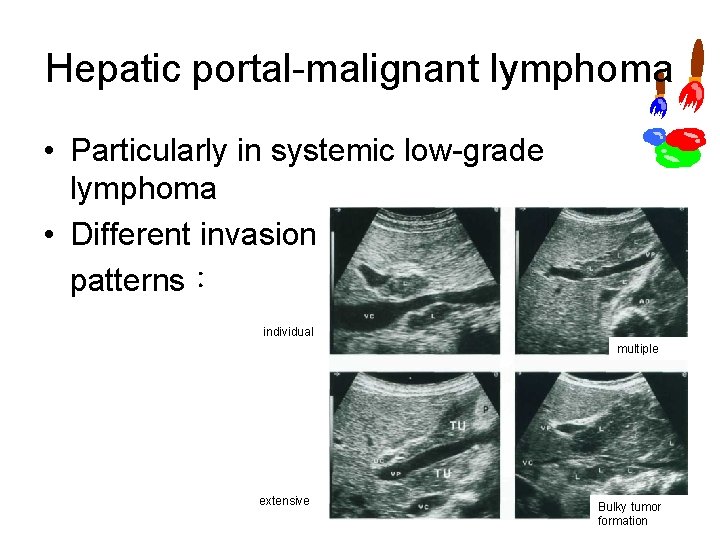
Hepatic portal malignant lymphoma • Particularly in systemic low grade lymphoma • Different invasion patterns: individual multiple extensive Bulky tumor formation
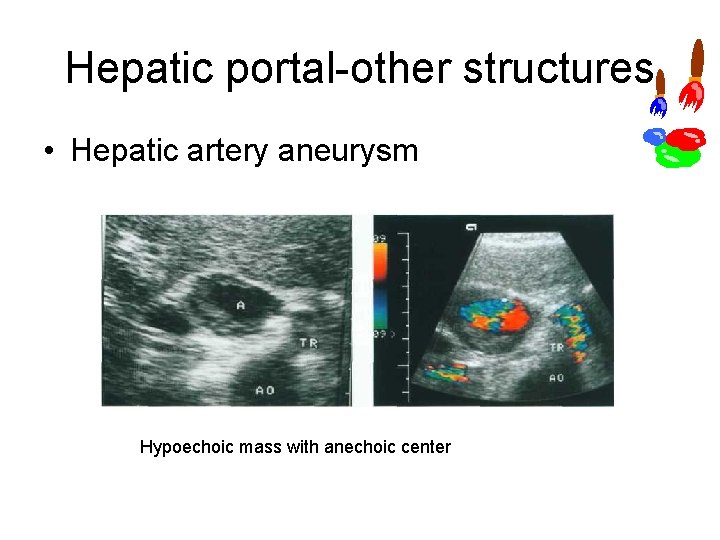
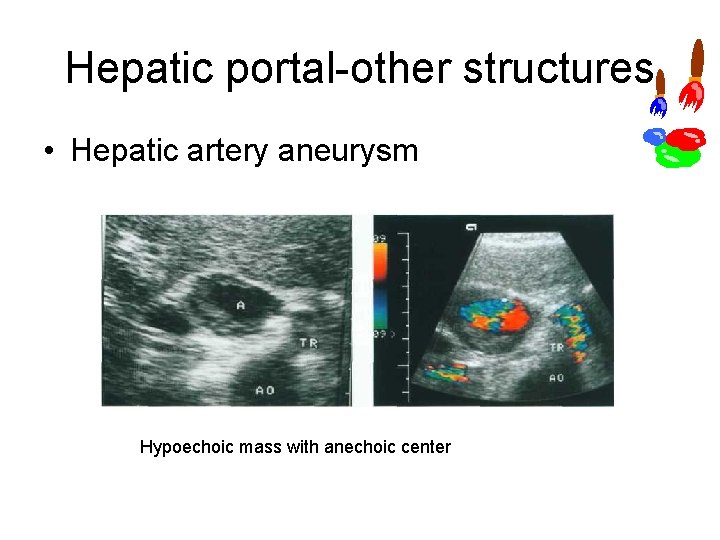
Hepatic portal other structures • Hepatic artery aneurysm Hypoechoic mass with anechoic center
Splenic hilum inflammatory • Reactive lymphadenitis of lymph nodes is almost never seen
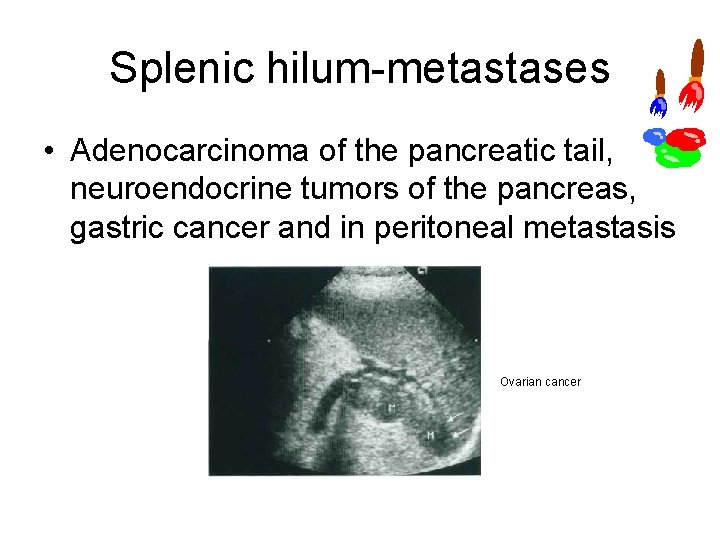
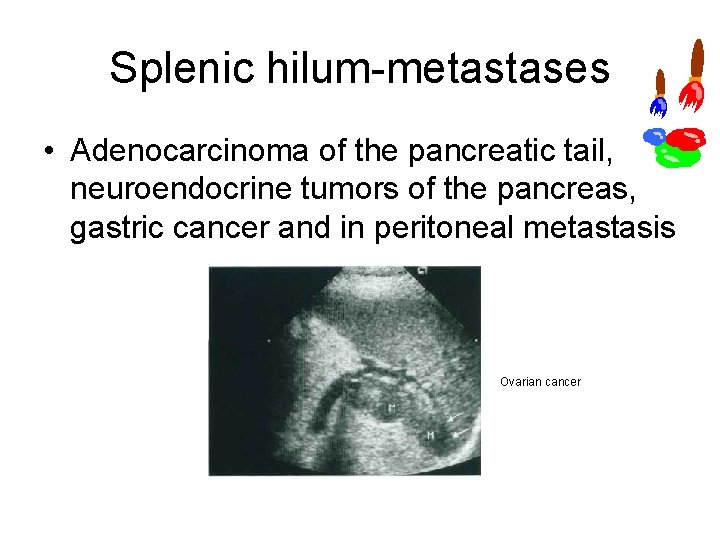
Splenic hilum metastases • Adenocarcinoma of the pancreatic tail, neuroendocrine tumors of the pancreas, gastric cancer and in peritoneal metastasis Ovarian cancer
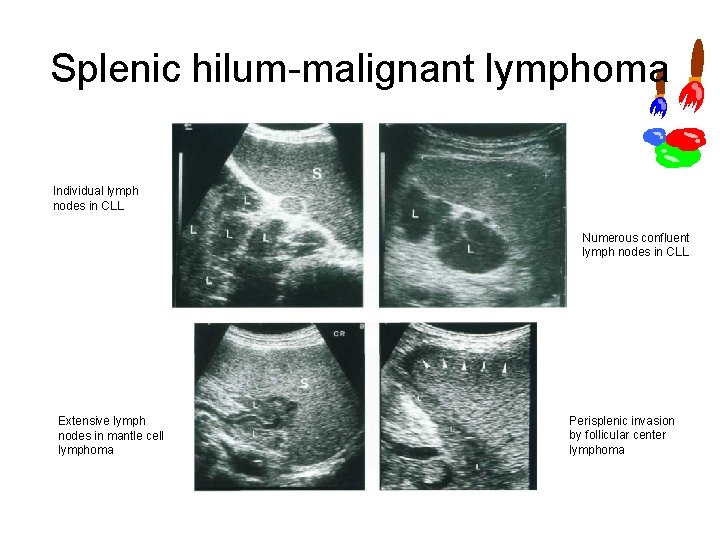
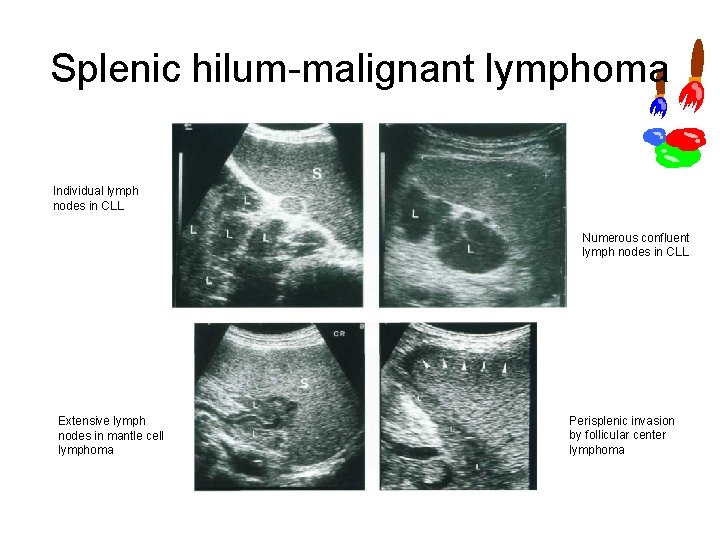
Splenic hilum malignant lymphoma Individual lymph nodes in CLL Numerous confluent lymph nodes in CLL Extensive lymph nodes in mantle cell lymphoma Perisplenic invasion by follicular center lymphoma
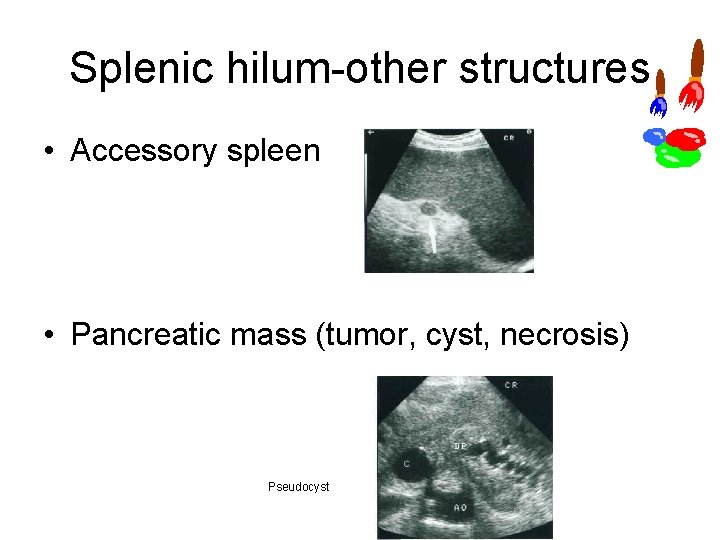
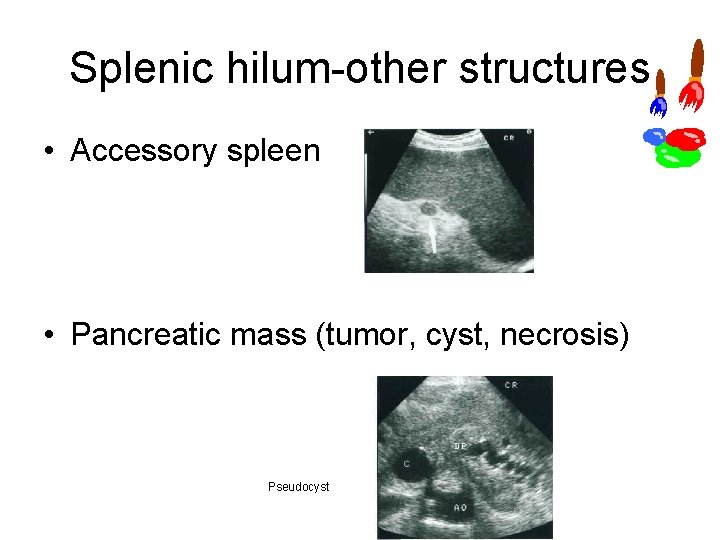
Splenic hilum other structures • Accessory spleen • Pancreatic mass (tumor, cyst, necrosis) Pseudocyst
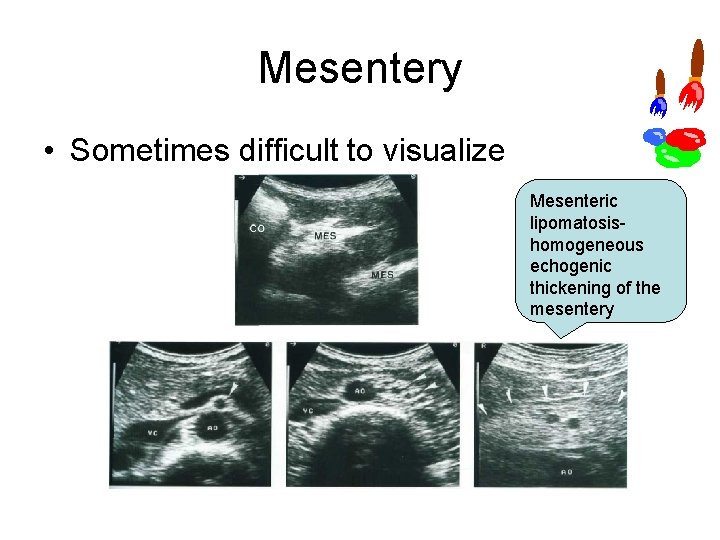
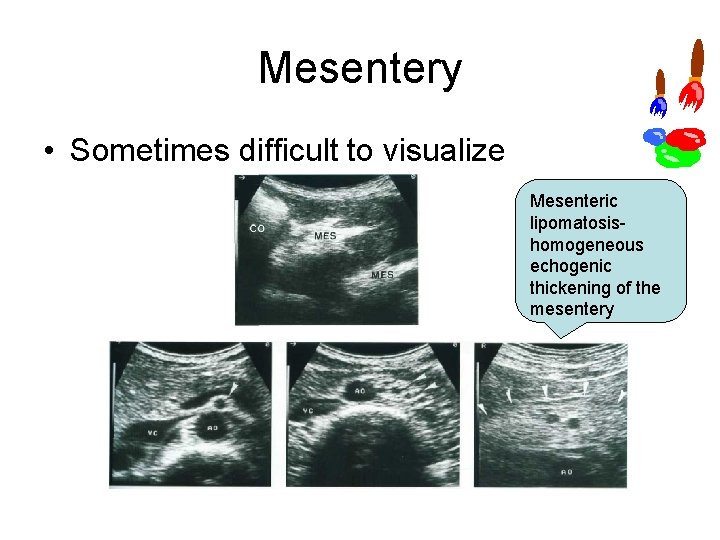
Mesentery • Sometimes difficult to visualize Mesenteric lipomatosis homogeneous echogenic thickening of the mesentery
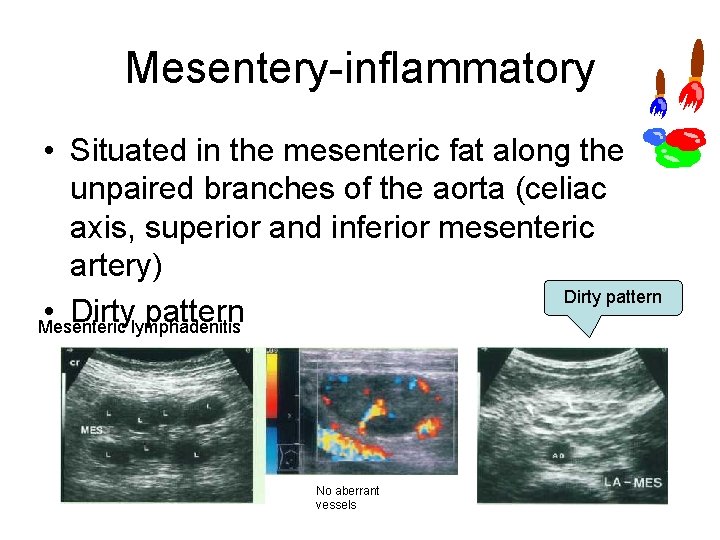
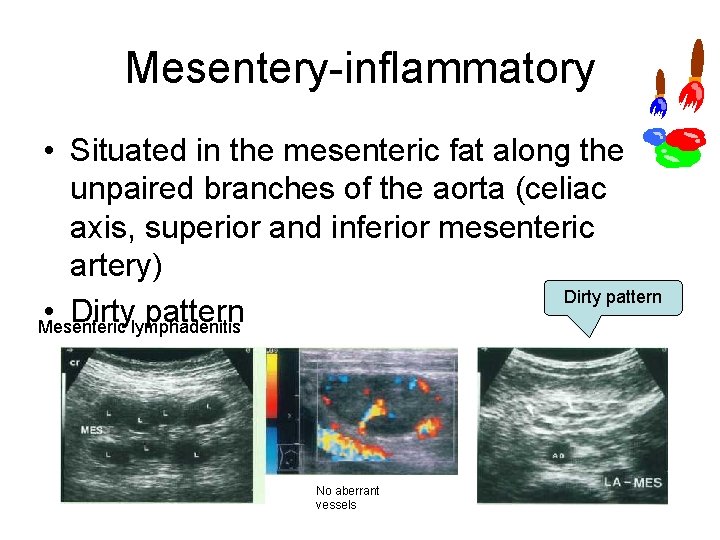
Mesentery inflammatory • Situated in the mesenteric fat along the unpaired branches of the aorta (celiac axis, superior and inferior mesenteric artery) Dirty pattern • Dirty pattern Mesenteric lymphadenitis No aberrant vessels
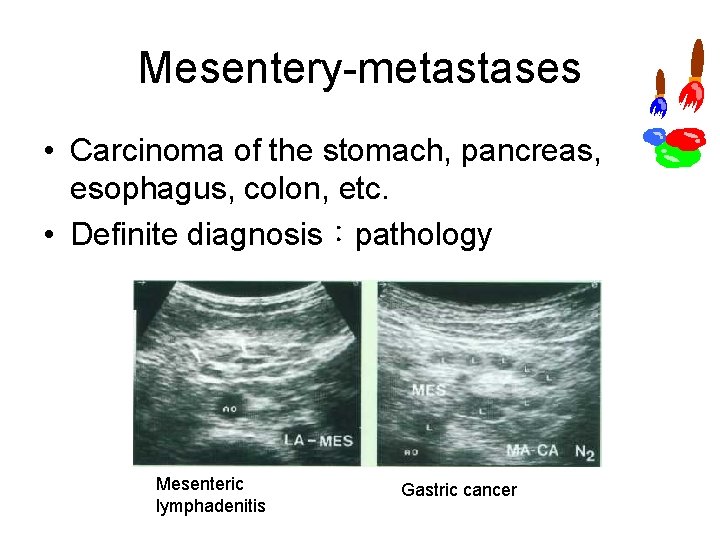
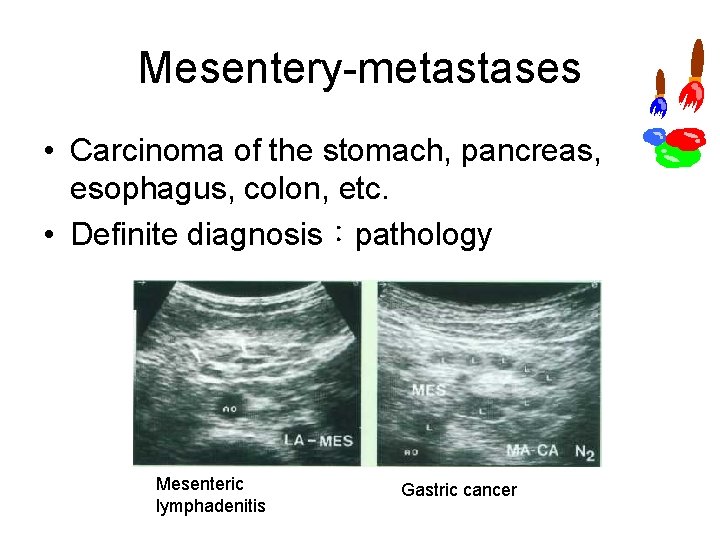
Mesentery metastases • Carcinoma of the stomach, pancreas, esophagus, colon, etc. • Definite diagnosis:pathology Mesenteric lymphadenitis Gastric cancer
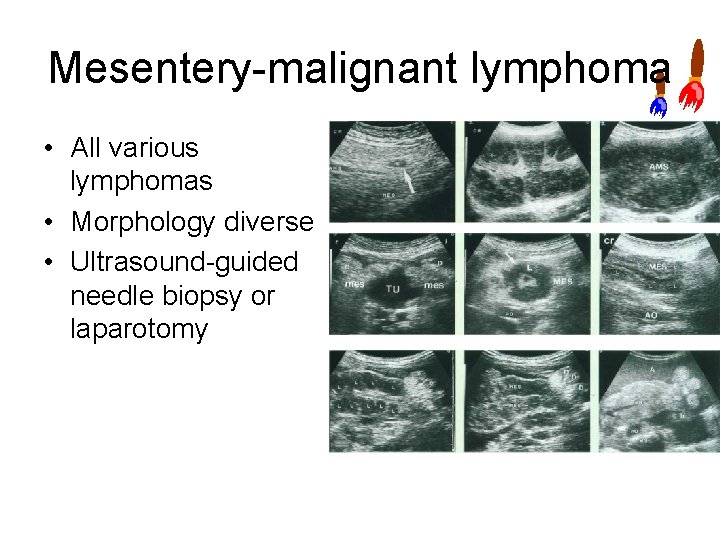
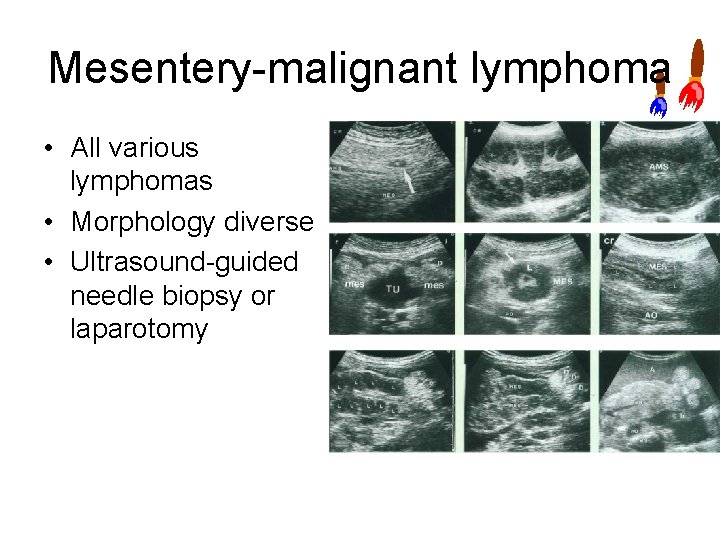
Mesentery malignant lymphoma • All various lymphomas • Morphology diverse • Ultrasound guided needle biopsy or laparotomy
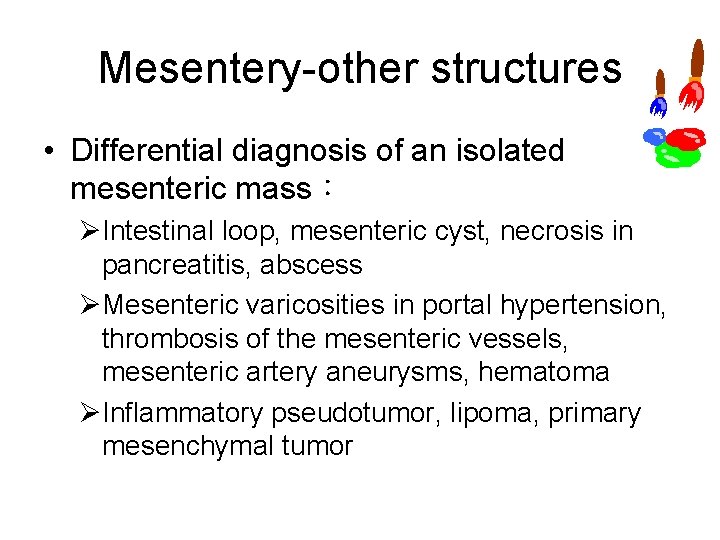
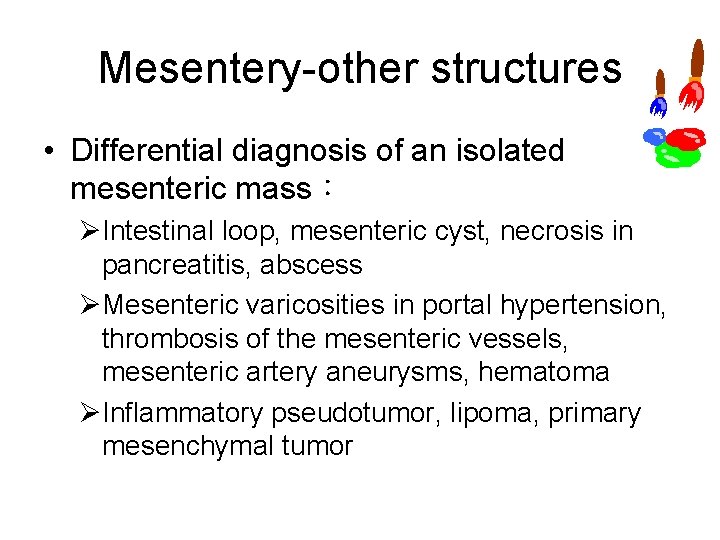
Mesentery other structures • Differential diagnosis of an isolated mesenteric mass: ØIntestinal loop, mesenteric cyst, necrosis in pancreatitis, abscess ØMesenteric varicosities in portal hypertension, thrombosis of the mesenteric vessels, mesenteric artery aneurysms, hematoma ØInflammatory pseudotumor, lipoma, primary mesenchymal tumor
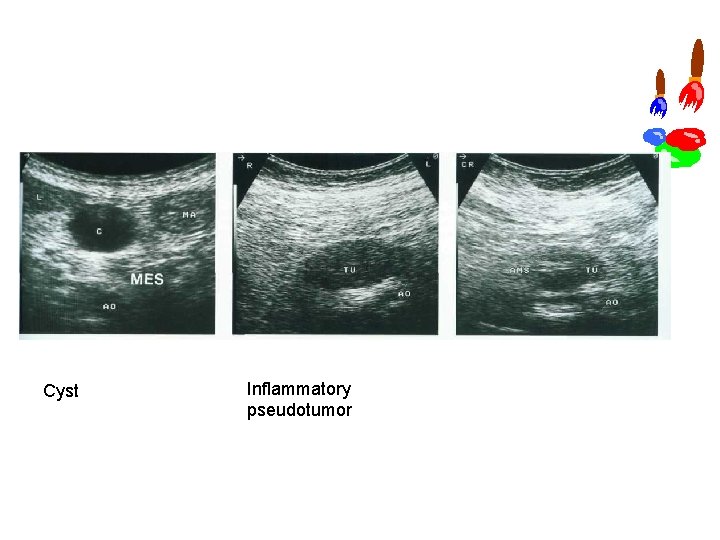
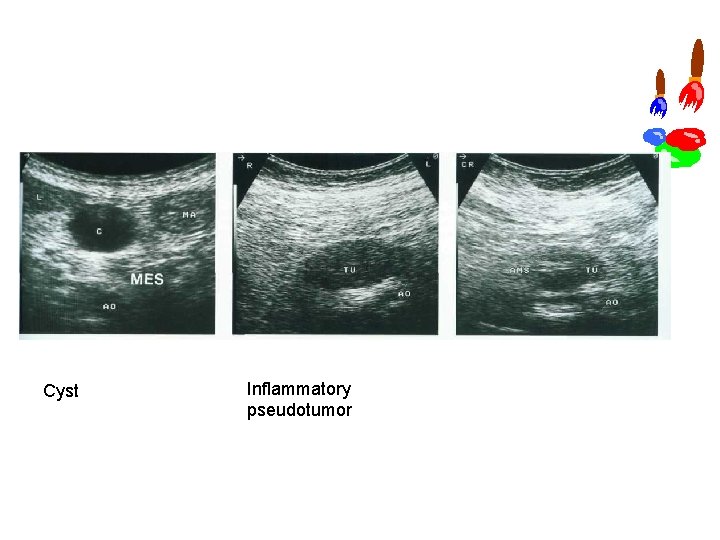
Cyst Inflammatory pseudotumor
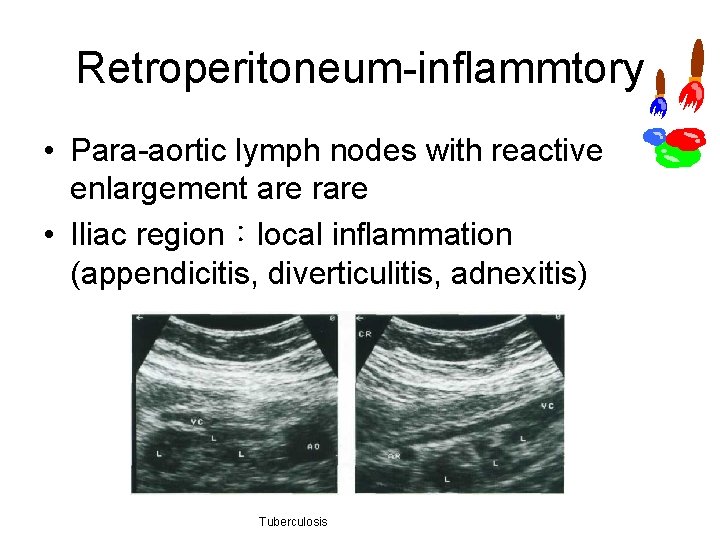
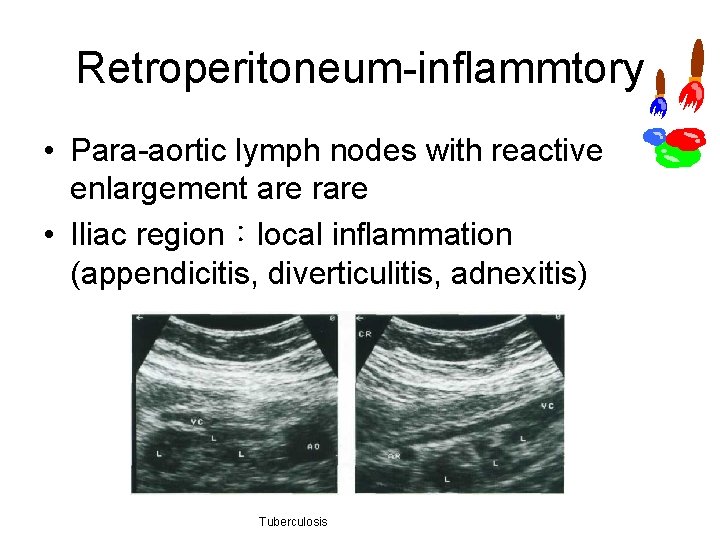
Retroperitoneum inflammtory • Para aortic lymph nodes with reactive enlargement are rare • Iliac region:local inflammation (appendicitis, diverticulitis, adnexitis) Tuberculosis
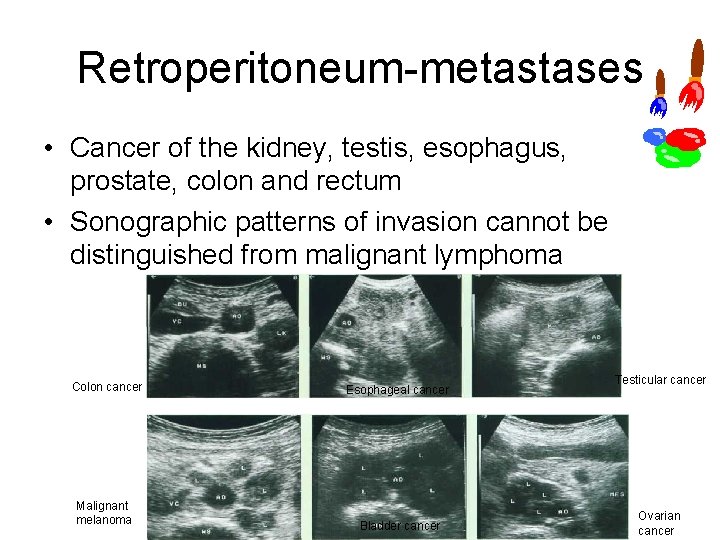
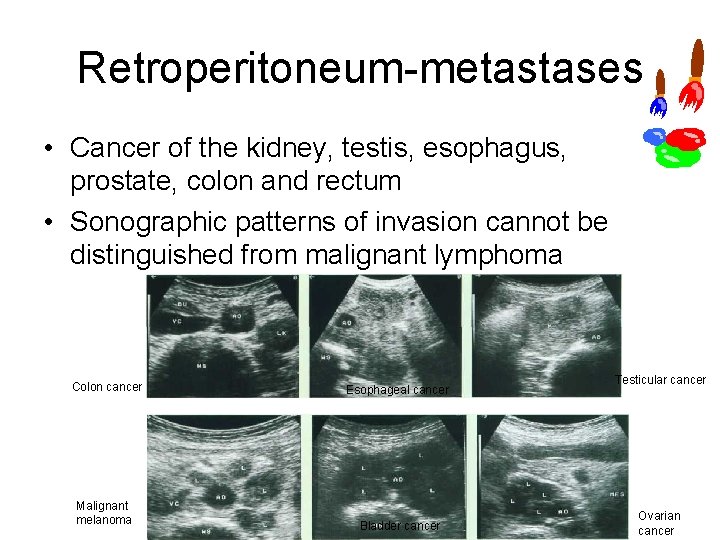
Retroperitoneum metastases • Cancer of the kidney, testis, esophagus, prostate, colon and rectum • Sonographic patterns of invasion cannot be distinguished from malignant lymphoma Colon cancer Esophageal cancer Malignant melanoma Bladder cancer Testicular cancer Ovarian cancer
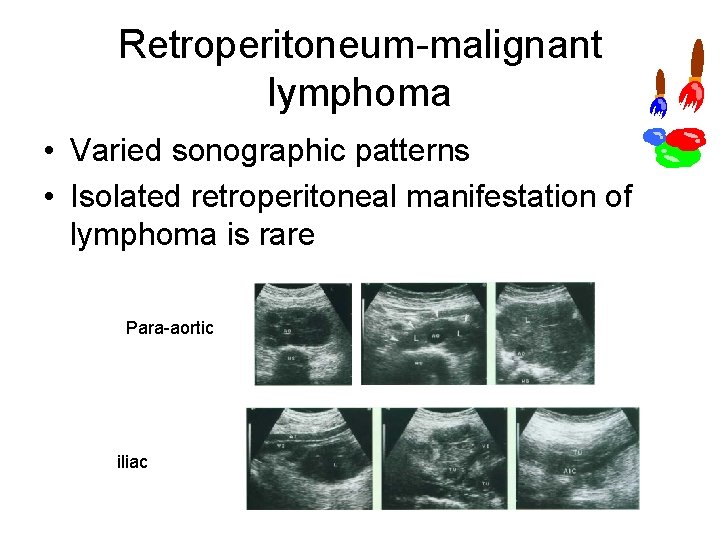
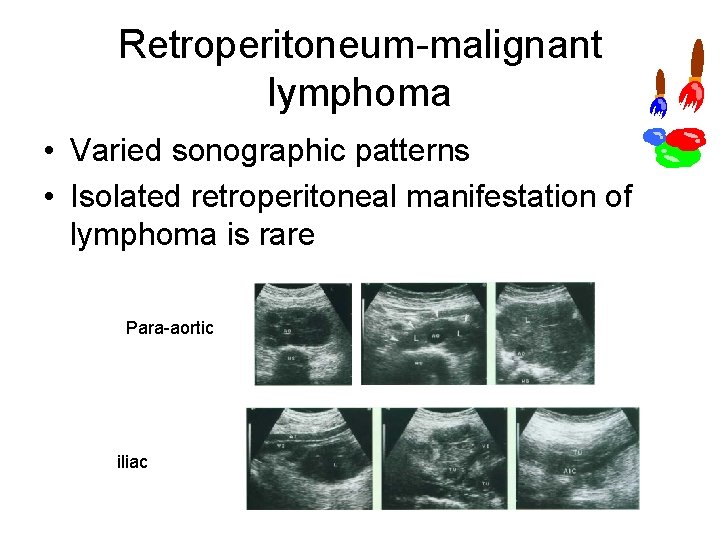
Retroperitoneum malignant lymphoma • Varied sonographic patterns • Isolated retroperitoneal manifestation of lymphoma is rare Para aortic iliac
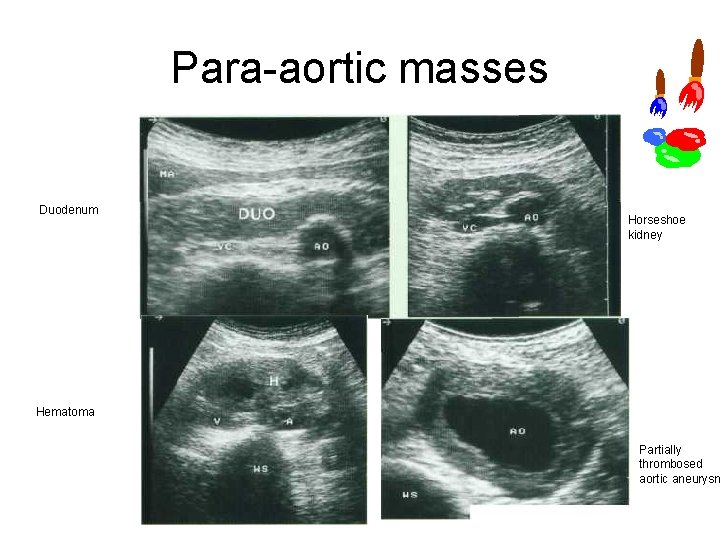
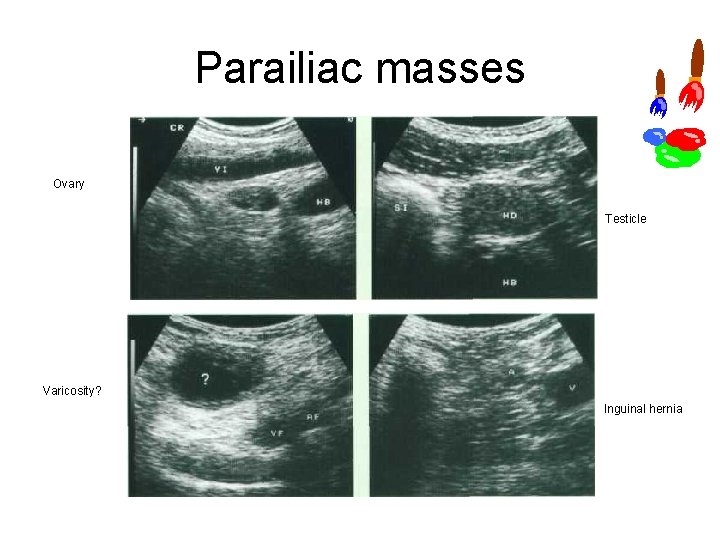
Retroperitoneum other structures • Local retroperitoneal tumor formations: ØPara aortic region:crura of diaphragm, abscess, aortic aneurysm, horseshoe kidney, horizontal part of the duodenum, hematoma, primarily retroperitoneal tumors ØIliac region:ovary, undescended testis, lymphocele, hematoma, abscess
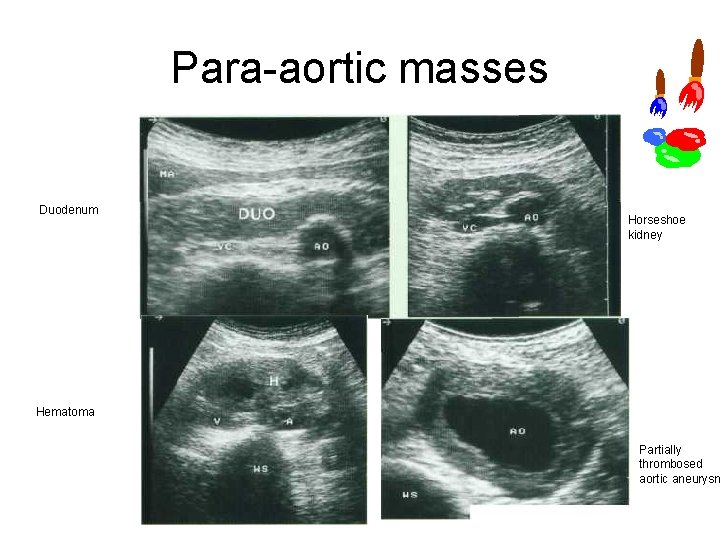
Para aortic masses Duodenum Horseshoe kidney Hematoma Partially thrombosed aortic aneurysm
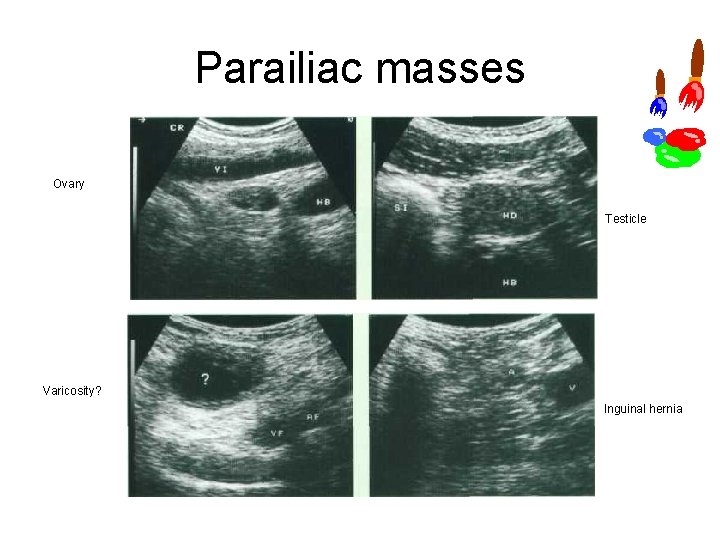
Parailiac masses Ovary Testicle Varicosity? Inguinal hernia

Thank you for your attention
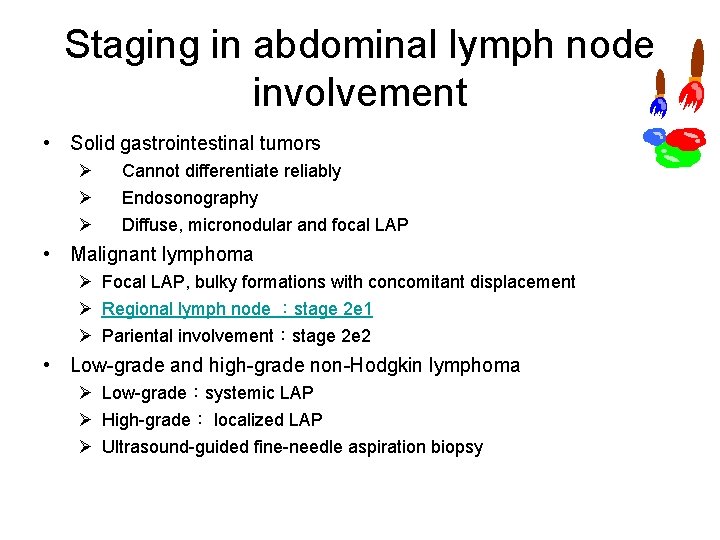
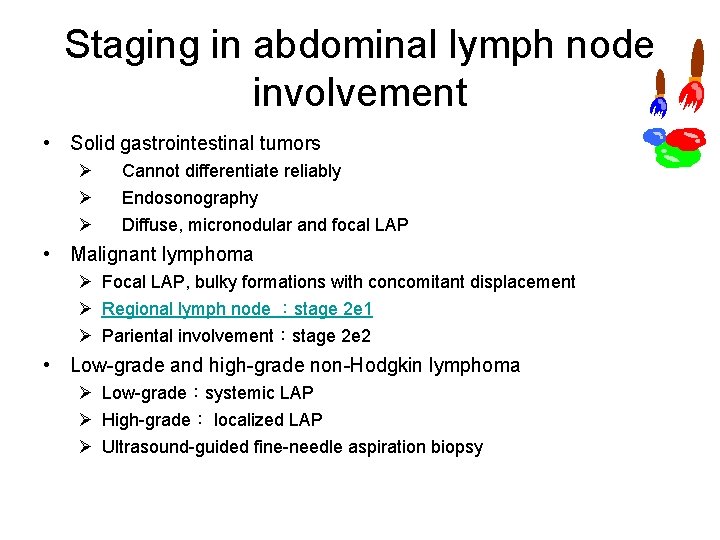
Staging in abdominal lymph node involvement • Solid gastrointestinal tumors Ø Ø Ø Cannot differentiate reliably Endosonography Diffuse, micronodular and focal LAP • Malignant lymphoma Ø Focal LAP, bulky formations with concomitant displacement Ø Regional lymph node :stage 2 e 1 Ø Pariental involvement:stage 2 e 2 • Low grade and high grade non Hodgkin lymphoma Ø Low grade:systemic LAP Ø High grade: localized LAP Ø Ultrasound guided fine needle aspiration biopsy