LYME DISEASE CASSANDRA WHITE PHARMD BCACP CGP ASSISTANT
LYME DISEASE CASSANDRA WHITE, PHARMD, BCACP, CGP ASSISTANT PROFESSOR OF PHARMACY PRACTICE HUSSON UNIVERSITY SCHOOL OF PHARMACY MAINE PHARMACY ASSOCIATION FALL CONVENTION SEPTEMBER 12, 2015
OVERVIEW • Epidemiology • Disease Summary • Stages of Lyme Disease • Medications 2 • Prevention
OBJECTIVES • Recognize patients at risk for Lyme disease • Explain how the infection is transmitted and diagnosed • Differentiate three phases of Lyme disease • Use IDSA treatment guidelines to determine appropriate pharmacotherapy 3 • Relate key counseling points to Lyme disease patients
4 EPIDEMIOLOGY
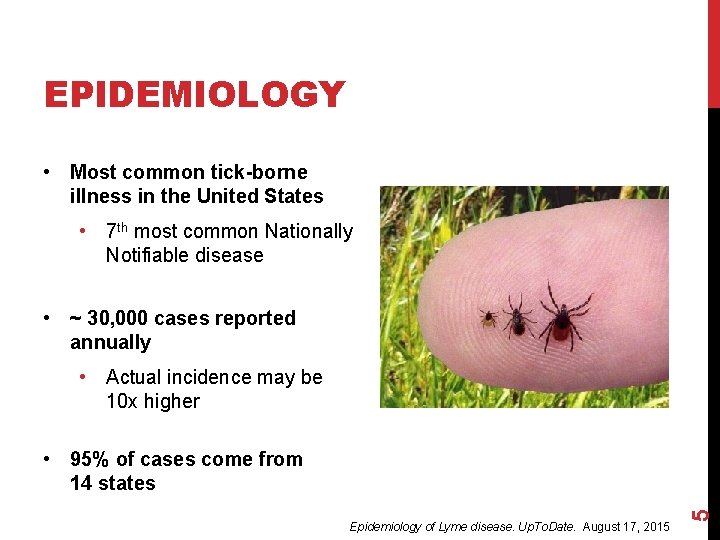
EPIDEMIOLOGY • Most common tick-borne illness in the United States • 7 th most common Nationally Notifiable disease • ~ 30, 000 cases reported annually • Actual incidence may be 10 x higher Epidemiology of Lyme disease. Up. To. Date. August 17, 2015 5 • 95% of cases come from 14 states
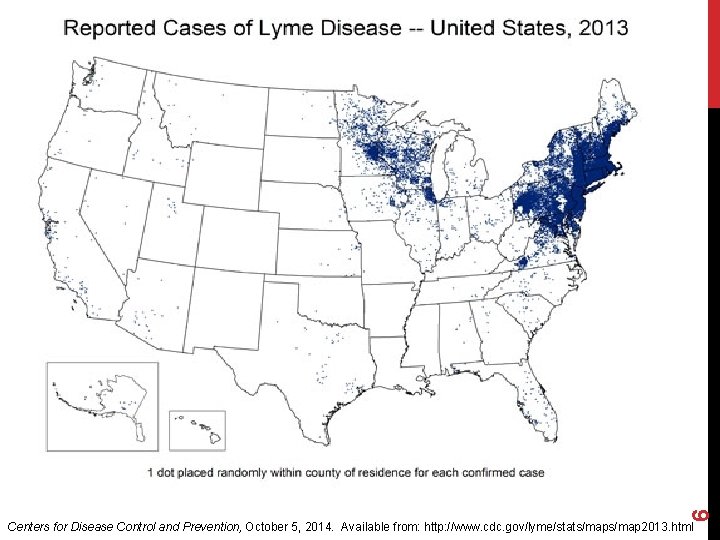
6 Centers for Disease Control and Prevention, October 5, 2014. Available from: http: //www. cdc. gov/lyme/stats/map 2013. html
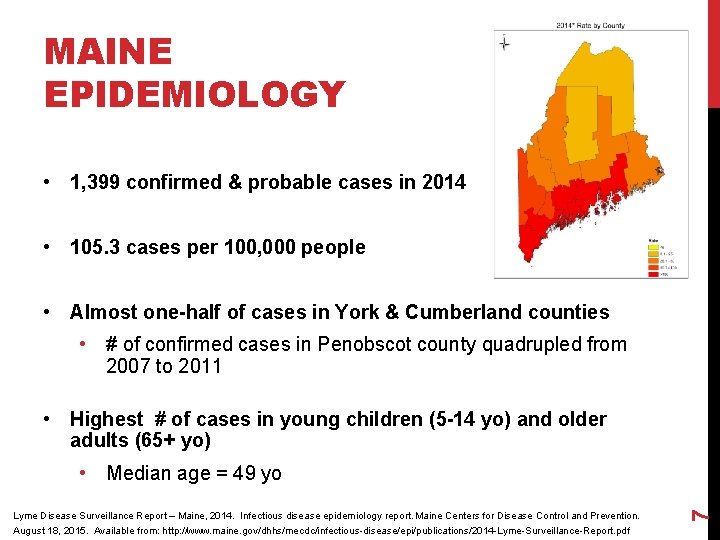
MAINE EPIDEMIOLOGY • 1, 399 confirmed & probable cases in 2014 • 105. 3 cases per 100, 000 people • Almost one-half of cases in York & Cumberland counties • # of confirmed cases in Penobscot county quadrupled from 2007 to 2011 • Highest # of cases in young children (5 -14 yo) and older adults (65+ yo) Lyme Disease Surveillance Report – Maine, 2014. Infectious disease epidemiology report. Maine Centers for Disease Control and Prevention. August 18, 2015. Available from: http: //www. maine. gov/dhhs/mecdc/infectious-disease/epi/publications/2014 -Lyme-Surveillance-Report. pdf 7 • Median age = 49 yo

8 LYME DISEASE IN MAINE Maine Centers for Disease Control and Prevention, August 18, 2015
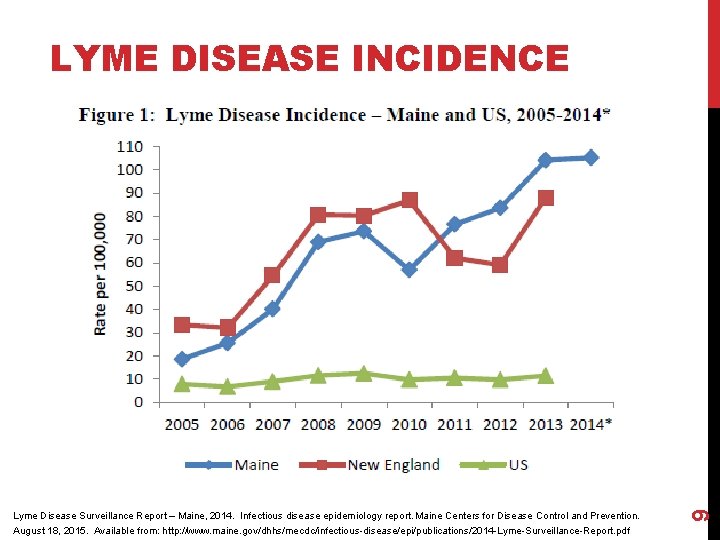
Lyme Disease Surveillance Report – Maine, 2014. Infectious disease epidemiology report. Maine Centers for Disease Control and Prevention. August 18, 2015. Available from: http: //www. maine. gov/dhhs/mecdc/infectious-disease/epi/publications/2014 -Lyme-Surveillance-Report. pdf 9 LYME DISEASE INCIDENCE
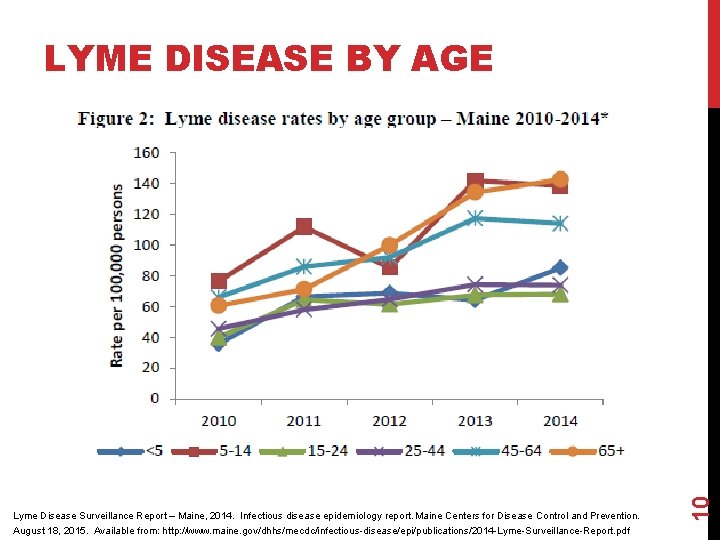
Lyme Disease Surveillance Report – Maine, 2014. Infectious disease epidemiology report. Maine Centers for Disease Control and Prevention. August 18, 2015. Available from: http: //www. maine. gov/dhhs/mecdc/infectious-disease/epi/publications/2014 -Lyme-Surveillance-Report. pdf 10 LYME DISEASE BY AGE

11 DISEASE SUMMARY
LYME DISEASE • Named for Lyme, Connecticut where it was identified in 1975 • Spirochetal infection caused by Borrelia species • Borrelia burgdorferi in the United States • Transmitted by bite of infected Ioxdes scapularis ticks (black-legged “deer” ticks) • Can involve the skin, joints, nervous system, Lyme borreliosis. Lancet. 2012; 379: 461 12 and heart
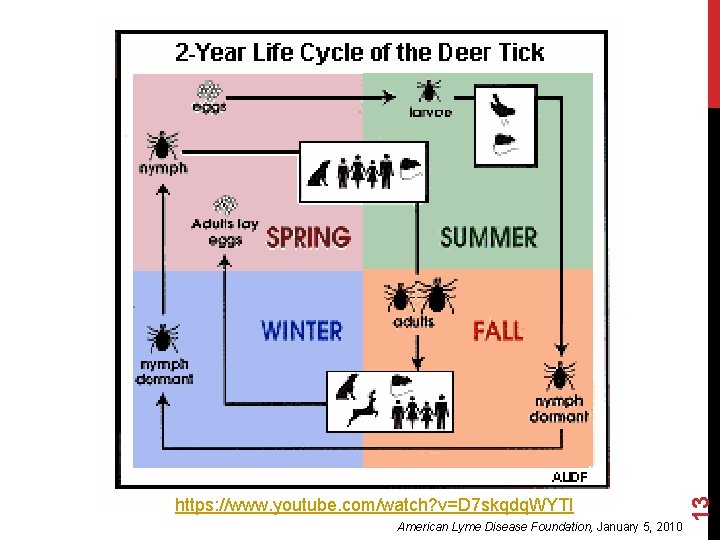
13 https: //www. youtube. com/watch? v=D 7 skqdq. WYTI American Lyme Disease Foundation, January 5, 2010
14 http: //www. tickencounter. org/prevention/lyme_disease
DIAGNOSIS • Diagnosis based on: • Signs and symptoms • A history of possible exposure to infected blacklegged ticks • Difficult to diagnose because: • Patient may be unaware of tick bite • Patient may not present with erythema migrans rash • Initial symptoms are vague and can be attributed to a variety of different causes • Serologic testing can be misleading Negative in up to 60% of patients with early infection Western Blot must be used for confirmation Centers for Disease Control and Prevention, October 5, 2014 15 • •
16
17 STAGES OF LYME DISEASE
STAGES OF LYME DISEASE • Early Localized • 3 -30 days • Early Disseminated • 3 -12 weeks • Late Disease or Chronic Disseminated 18 • > 2 months
EARLY LOCALIZED • Incubation 3 – 32 days • Erythema migrans – bull’s eye rash in ~80% of patients • Flu-like symptoms • Fever, headache, fatigue, muscle aches • Swollen lymph nodes • Approximately 50% of untreated cases will go on to disseminated disease Clinical manifestations of Lyme disease in adults. Up. To. Date. February 5, 2013 19 • Usually responds well to appropriate PO antibiotic treatment
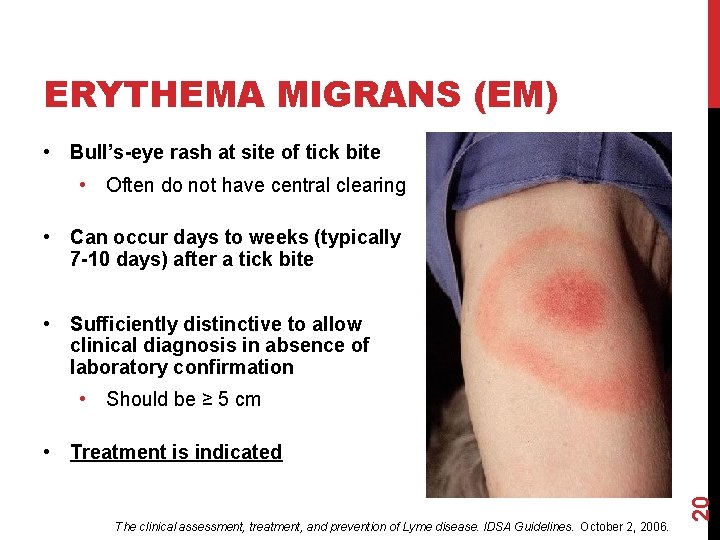
ERYTHEMA MIGRANS (EM) • Bull’s-eye rash at site of tick bite • Often do not have central clearing • Can occur days to weeks (typically 7 -10 days) after a tick bite • Sufficiently distinctive to allow clinical diagnosis in absence of laboratory confirmation • Should be ≥ 5 cm The clinical assessment, treatment, and prevention of Lyme disease. IDSA Guidelines. October 2, 2006. 20 • Treatment is indicated
EARLY DISSEMINATED • Organism spreads throughout the body by invasion • Distinct preference for skin, heart, CNS, joints, & eyes • Weeks to months after infection • Organism can persist in skin for a very long time • Characterized by multiple, often smaller EM lesions • Sign of spirochetemia Clinical manifestations of Lyme disease in adults. Up. To. Date. February 5, 2013 21 • May require IV antibiotic treatment
LATE DISEASE OR CHRONIC DISSEMINATED • Infection stimulates an immune response that leads to symptoms in various organs • Arthritis • Chronic CNS Facial palsy Meningitis Difficulty thinking Short term memory loss • Speech problems • Double / blurry vision • Tinnitus • • Seizures Mood swings Irritability Depression Disturbed sleep Personality changes OCD Anxiety Evidence-based guidelines for the treatment of Lyme disease. ILADS. 2004 22 • •
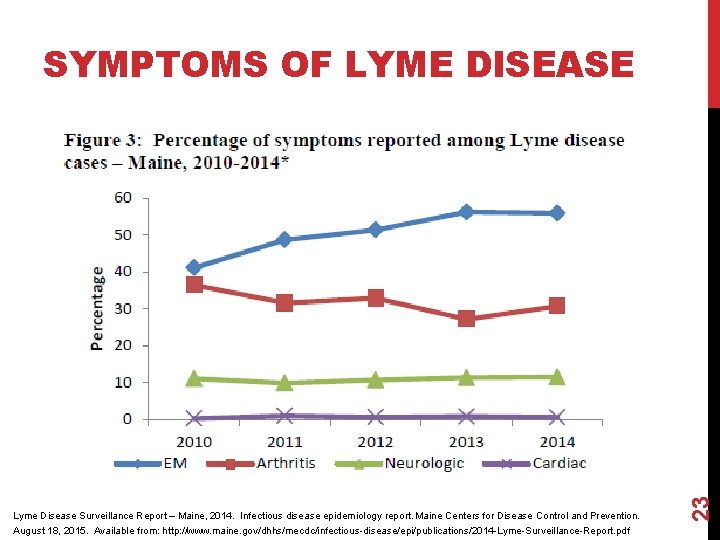
Lyme Disease Surveillance Report – Maine, 2014. Infectious disease epidemiology report. Maine Centers for Disease Control and Prevention. August 18, 2015. Available from: http: //www. maine. gov/dhhs/mecdc/infectious-disease/epi/publications/2014 -Lyme-Surveillance-Report. pdf 23 SYMPTOMS OF LYME DISEASE

24 MEDICATIONS
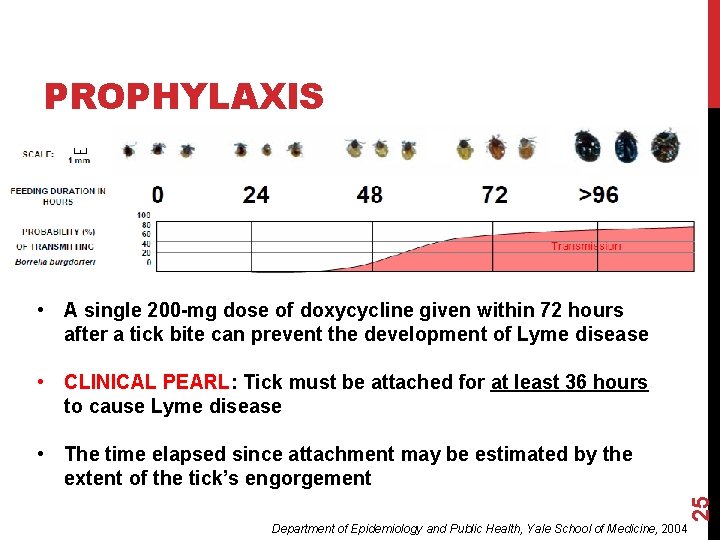
PROPHYLAXIS • A single 200 -mg dose of doxycycline given within 72 hours after a tick bite can prevent the development of Lyme disease • CLINICAL PEARL: Tick must be attached for at least 36 hours to cause Lyme disease 25 • The time elapsed since attachment may be estimated by the extent of the tick’s engorgement Department of Epidemiology and Public Health, Yale School of Medicine, 2004
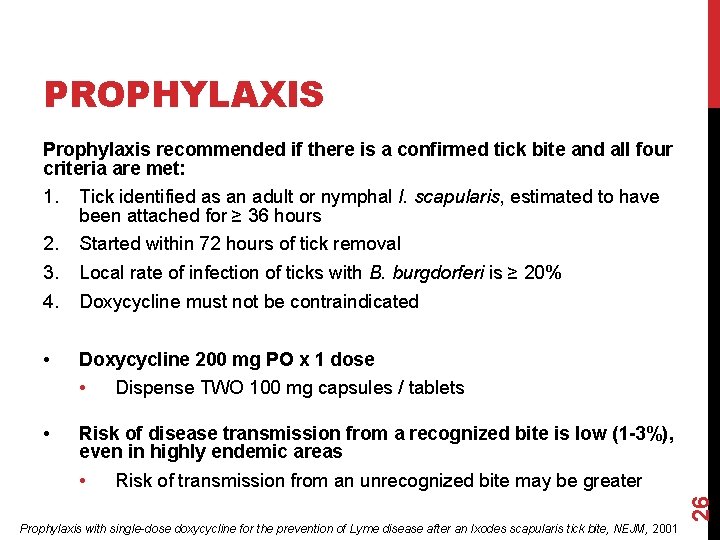
PROPHYLAXIS Prophylaxis recommended if there is a confirmed tick bite and all four criteria are met: 1. Tick identified as an adult or nymphal I. scapularis, estimated to have been attached for ≥ 36 hours 2. 3. 4. Started within 72 hours of tick removal • Doxycycline 200 mg PO x 1 dose Local rate of infection of ticks with B. burgdorferi is ≥ 20% Doxycycline must not be contraindicated • • Dispense TWO 100 mg capsules / tablets Risk of disease transmission from a recognized bite is low (1 -3%), even in highly endemic areas Risk of transmission from an unrecognized bite may be greater 26 • Prophylaxis with single-dose doxycycline for the prevention of Lyme disease after an Ixodes scapularis tick bite, NEJM, 2001
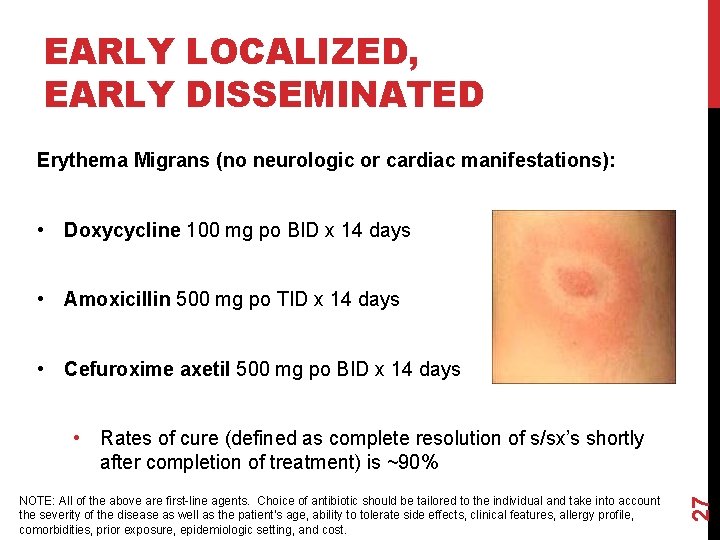
EARLY LOCALIZED, EARLY DISSEMINATED Erythema Migrans (no neurologic or cardiac manifestations): • Doxycycline 100 mg po BID x 14 days • Amoxicillin 500 mg po TID x 14 days • Cefuroxime axetil 500 mg po BID x 14 days NOTE: All of the above are first-line agents. Choice of antibiotic should be tailored to the individual and take into account the severity of the disease as well as the patient’s age, ability to tolerate side effects, clinical features, allergy profile, comorbidities, prior exposure, epidemiologic setting, and cost. 27 • Rates of cure (defined as complete resolution of s/sx’s shortly after completion of treatment) is ~90%
EARLY LOCALIZED, EARLY DISSEMINATED Lyme Meningitis or Radiculopathy: • Ceftriaxone 2 g IV daily x 14 days Lyme Carditis: • PO antibiotics as for erythema migrans x 14 days The clinical assessment, treatment, and prevention of Lyme disease. IDSA Guidelines. October 2, 2006. 28 • Ceftriaxone 2 g IV daily x 14 days for hospitalized patients
LATE DISEASE OR CHRONIC DISSEMINATED • Treatment at this stage is controversial • Ranges from months to years • Can result in treatment failure or adverse drug reactions • Many patients resort to alternative therapies 29 • Homeopathy, detoxification, nutritional therapies, etc.
LATE DISEASE OR CHRONIC DISSEMINATED Lyme Arthritis • Doxycycline 100 mg po BID x 28 days • Amoxicillin 500 mg po TID x 28 days • Cefuroxime axetil 500 mg po BID x 28 days • Ceftriaxone 2 g IV daily x 14 -28 days 30 Late Neurologic
DOXYCYCLINE • Contraindications (relative): • Pregnancy or lactation • Children < 8 years of age • Side Effects: • Nausea/Vomiting/Diarrhea • Nasopharyngitis • Counseling Points: • Administer with food to decrease GI upset • • Teach patient importance of adequate hydration Report severe diarrhea (could be C. difficile) 31 • Causes sun-sensitivity use sunscreen • May interact with oral contraceptives use additional form of birth control Micromedex 2. 0, Truven Health Analytics Inc. 2013
AMOXICILLIN • Contraindication: • Hypersensitivity (to amoxicillin or other beta-lactam) • Side Effects: • Nausea/Vomiting/Diarrhea (frequent) • Rash • Counseling Points: • Administer with food to decrease GI upset • Report severe diarrhea (could be C. difficile) 32 • May interact with oral contraceptives use additional form of birth control • Take entire prescription (remember TID dosing!) Micromedex 2. 0, Truven Health Analytics Inc. 2013
CEFUROXIME AXETIL • Contraindication: • Hypersensitivity (up to 10% cross-sensitivity with PCN) • Side Effects: • Nausea/Vomiting/Diarrhea (frequent, duration-dependent) • Vaginitis • Counseling Points: • Administer with food to increase absorption • • Bioavailability: Fasting: 37%; Following food: 52% Report severe diarrhea (could be C. difficile) 33 • May interact with oral contraceptives use additional form of birth control Micromedex 2. 0, Truven Health Analytics Inc. 2013
CEFTRIAXONE IV • Contraindication: • • Do not reconstitute or coadminister with calcium-containing solutions (C/I in neonates aged 28 days or less) Side Effects: • • Nausea/Vomiting/Diarrhea • Induration, warmth, or tightness at injection site • Thrombocytosis Counseling Points: Must be administered by qualified healthcare provider • • • Home visits or daily hospital appointments Not necessarily covered by insurance companies Local and systemic risks associated with IV therapy • Phlebitis, infiltration, infection, etc. Micromedex 2. 0, Truven Health Analytics Inc. 2013 34 •

35 PREVENTION
LYME VACCINE • A Lyme disease vaccine was discontinued in 2002 and is no longer available • “insufficient consumer demand” = poor sales 36 • New vaccines under development
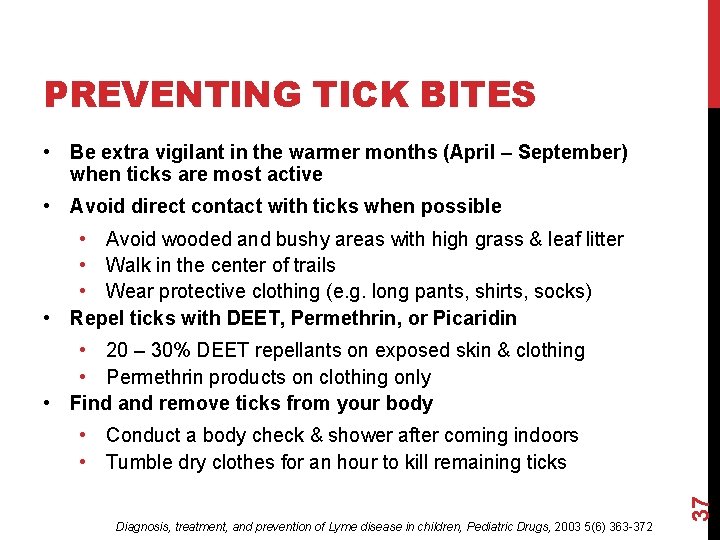
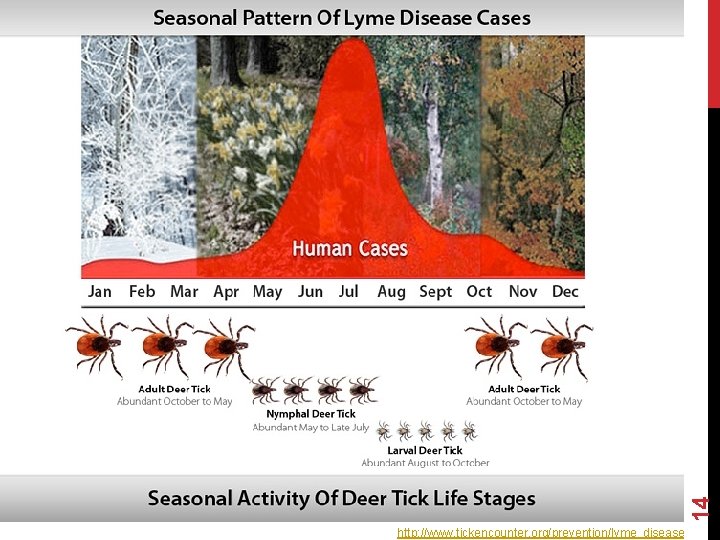
PREVENTING TICK BITES • Be extra vigilant in the warmer months (April – September) when ticks are most active • Avoid direct contact with ticks when possible • Avoid wooded and bushy areas with high grass & leaf litter • Walk in the center of trails • Wear protective clothing (e. g. long pants, shirts, socks) • Repel ticks with DEET, Permethrin, or Picaridin • 20 – 30% DEET repellants on exposed skin & clothing • Permethrin products on clothing only • Find and remove ticks from your body Diagnosis, treatment, and prevention of Lyme disease in children, Pediatric Drugs, 2003 5(6) 363 -372 37 • Conduct a body check & shower after coming indoors • Tumble dry clothes for an hour to kill remaining ticks
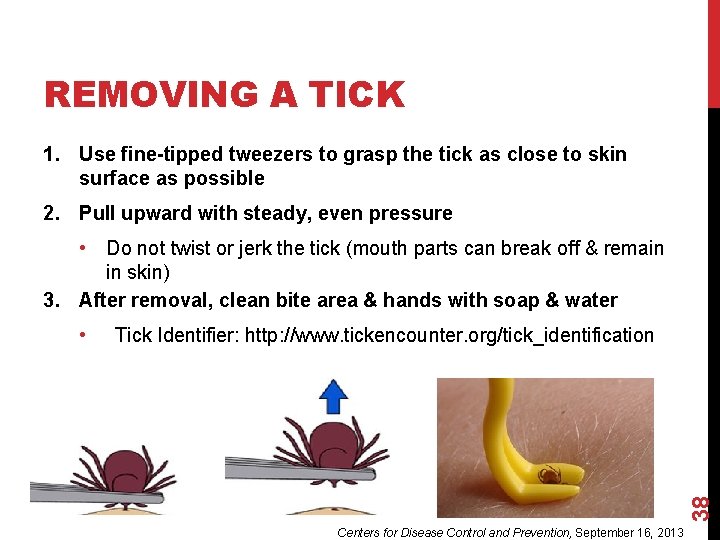
REMOVING A TICK 1. Use fine-tipped tweezers to grasp the tick as close to skin surface as possible 2. Pull upward with steady, even pressure • Do not twist or jerk the tick (mouth parts can break off & remain in skin) 3. After removal, clean bite area & hands with soap & water Tick Identifier: http: //www. tickencounter. org/tick_identification 38 • Centers for Disease Control and Prevention, September 16, 2013
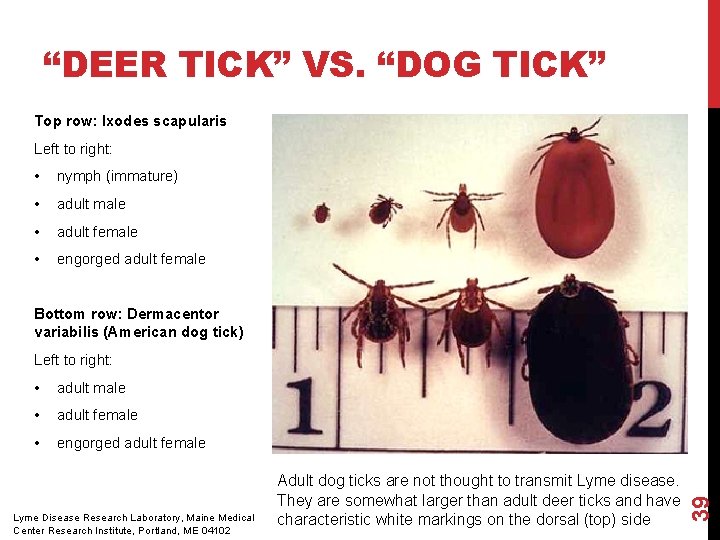
“DEER TICK” VS. “DOG TICK” Top row: Ixodes scapularis Left to right: • nymph (immature) • adult male • adult female • engorged adult female Bottom row: Dermacentor variabilis (American dog tick) Left to right: adult male • adult female • engorged adult female Lyme Disease Research Laboratory, Maine Medical Center Research Institute, Portland, ME 04102 Adult dog ticks are not thought to transmit Lyme disease. They are somewhat larger than adult deer ticks and have characteristic white markings on the dorsal (top) side 39 •
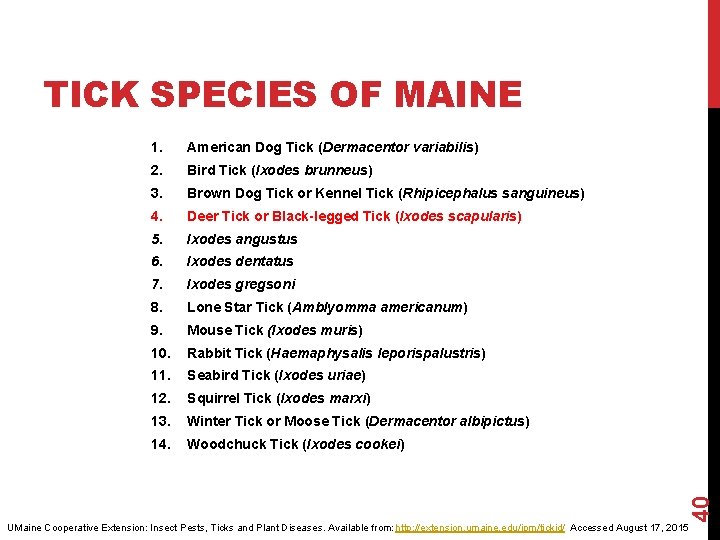
1. American Dog Tick (Dermacentor variabilis) 2. Bird Tick (Ixodes brunneus) 3. Brown Dog Tick or Kennel Tick (Rhipicephalus sanguineus) 4. Deer Tick or Black-legged Tick (Ixodes scapularis) 5. Ixodes angustus 6. Ixodes dentatus 7. Ixodes gregsoni 8. Lone Star Tick (Amblyomma americanum) 9. Mouse Tick (Ixodes muris) 10. Rabbit Tick (Haemaphysalis leporispalustris) 11. Seabird Tick (Ixodes uriae) 12. Squirrel Tick (Ixodes marxi) 13. Winter Tick or Moose Tick (Dermacentor albipictus) 14. Woodchuck Tick (Ixodes cookei) 40 TICK SPECIES OF MAINE UMaine Cooperative Extension: Insect Pests, Ticks and Plant Diseases. Available from: http: //extension. umaine. edu/ipm/tickid/ Accessed August 17, 2015
TESTING TICKS University of Maine Cooperative Extension Service • Tick identification only • • Does not currently test tick specimens for diseases November 2014: Maine voters approved a bond referendum that will enable the building of a new lab for in-state disease testing of tick specimens After proper removal: • Fill out the tick submission form from their website • Place the tick to be identified in a crush proof container with enough rubbing alcohol to cover the specimen; wrap in paper towel and place in plastic bag mail in the specimen Alternatively, you can drop the tick off in-person 41 • UMaine Cooperative Extension: Insect Pests, Ticks and Plant Diseases. Available from: http: //extension. umaine. edu/ipm/tickid/ Accessed August 17, 2015
LYME DISEASE IN THE NEWS • “Maine legislature clears way for long-term Lyme disease treatment” - Joe Lawlor, Portland Press Herald (June 2015) • A bill to shield doctors from license sanctions for prescribing long-term antibiotics becomes law without the governor’s signature. • “Maine records spike in diseases carried by ticks, not just Lyme” – Jackie Farwell, Bangor Daily News (August 2014) 42 • An emerging infection carried by the same ticks that transmit Lyme disease has sickened a record number of Mainers this year, according to the Maine Center for Disease Control and Prevention. While rarely fatal, anaplasmosis can cause serious illness if left untreated.
TICK-BORNE DISEASE • Becoming a growing veterinary problem (dogs, horses, etc. ) • Support groups available • For a list of support groups in Maine: http: //www. mainelyme. org/patient-support/support-groups/ • In addition to Lyme disease, ixodes ticks in the U. S. can transmit: Anaplasmosis Babesiosis Powassan virus 43 • • •
ANAPLASMOSIS • Human granulocytic anaplasmosis (HGA), a bacterial disease Findings that may suggest coinfection (2. 2 - 36% of ticks) with B. burgdorferi include: • • • Drug of choice: Doxycycline 100 mg BID x 10 days • • Leukopenia Thrombocytopenia High fever Abnormal liver enzyme tests 14 days for coinfection with Lyme disease 94 confirmed cases in Maine in 2013 • First detected in Maine in mid 1990 s Lyme and Other Vector-borne Disease Information. Tick Borne Diseases. Maine Medical Center Research Institute. Available from: http: //www. mmcri. org/home/web. Sub. Content. php? list=webcontentlive&id=107&cat. ID=4&sub. Cat. ID=19 Accessed 21 Aug 2015 44 •
BABESIOSIS • Parasitic disease caused by protozoa of Babesia genus • Most commonly B. microti • Invades red blood cells similar to the parasites that cause malaria • Clinical manifestations mild to severe • Fatigue, aches, fever, chills, sweating, dark urine, anemia • Two major antimicrobial regimens (7 -10 day treatment course) • Atovaquone + Azithromycin or Quinine + Clindamycin • 36 confirmed cases in Maine in 2013 First detected in a Maine tick in 2004 Lyme and Other Vector-borne Disease Information. Tick Borne Diseases. Maine Medical Center Research Institute. Available from: http: //www. mmcri. org/home/web. Sub. Content. php? list=webcontentlive&id=107&cat. ID=4&sub. Cat. ID=19 Accessed 21 Aug 2015 45 •
POWASSAN VIRUS • Serious viral infection of the brain and surrounding tissues • Fatal for 10 -15% of patients • Leaves ½ of its victims with permanent neurological damage • Early signs and symptoms include: • Headache, fever, nausea, vomiting, stiff neck, and sleepiness • No delay between tick bite and transmission of the virus • No specific treatment • Hospitalization with supportive care • Fatal, co-infected with Lyme disease and anaplasmosis • 5 total recorded cases in Maine, 60 in the U. S. over the past 10 years Lyme and Other Vector-borne Disease Information. Tick Borne Diseases. Maine Medical Center Research Institute. Available from: http: //www. mmcri. org/home/web. Sub. Content. php? list=webcontentlive&id=107&cat. ID=4&sub. Cat. ID=19 Accessed 21 Aug 2015 46 • 1 confirmed case in Maine in 2013
SUMMARY • Infected ticks can transmit Lyme disease to anyone • Most common patient characteristics: • • Live in endemic areas Ages 5 – 14 and 65+ years old Males > Females Spend ↑ amount of time outdoors in forested habitats • Nymph and adult Ioxdes scapularis ticks transmit the disease • • Nymphs = 25% infected yet 90% of all cases Transmission begins 36 hours after attachment 47 • Most likely to have illness onset in June, July, or August
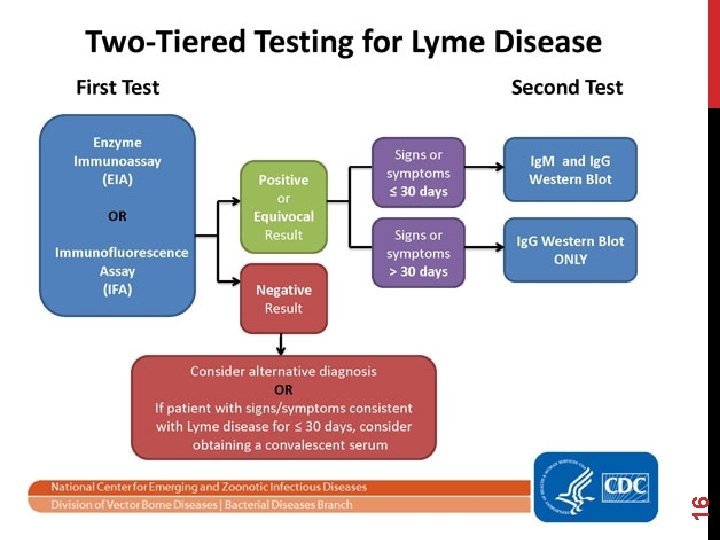
SUMMARY • Diagnosed based on signs & symptoms and history of possible tick exposure • EM rash = pathognomonic sign • Two-tiered testing using serodiagnostics • Three phases of Lyme disease: 48 • Early localized (days to weeks) • Early disseminated (weeks to months) • Late disease or chronic disseminated (months to years)
SUMMARY • Prophylaxis should be given in select patients within 72 hours after a tick bite • Doxycycline 200 mg PO x 1 dose • First-line medications for treatment include: Doxycycline PO Amoxicillin PO Cefuroxime PO Ceftriaxone IV • Depends on patient characteristics, stage, & severity of disease 49 • •
- Slides: 49