Lung Cancer Overview A Slide Presentation for Oncology

- Slides: 35
Lung Cancer Overview A Slide Presentation for Oncology Nurses
Lung Cancer: What is it? n n Uncontrolled growth of malignant cells in one or both lungs and tracheo-bronchial tree Arises from protective or ciliated cells in the bronchial epithelium Begins as a result of repeated carcinogenic irritation causing increased rates of cell replication Proliferation of abnormal cells leads to hyperplasia, dysplasia or carcinoma in situ
Lung Cancer: Incidence in US n n n 173, 770 new cases yearly (2004 statistics) 160, 440 deaths yearly (2004 statistics) More deaths from lung cancer than prostate, breast and colorectal cancers combined Closely correlated with smoking patterns Decreasing incidence and deaths in men; continued increase in women Incidence and mortality rates higher for African Americans than white Americans
Lung Cancer in Women n n Incidence (80, 660 new cases in 2004) Account for 12 percent of all new cases Deaths increased 150% between 1974 and 1994 (68, 510 in 2004) More deaths from lung cancer than breast, ovarian and uterine cancers combined Women are more susceptible to tobacco effects - 1. 5 times more likely to develop lung cancer than men with same smoking habits
Lung Cancer: What Causes It? Smoking n Radiation Exposure n Environmental/ Occupational Exposure n Asbestos n Radon n Passive smoke n
Lung Cancer: Smoking Facts n n n Tobacco use is the leading cause of lung cancer 87% of lung cancers are related to smoking Risk related to: n n n amount smoked (pack years- # cigs/day x # yrs) age of smoking onset product smoked (tar/nicotine content, filters) depth of inhalation gender
Lung Cancer: Screening n n n No proven effective screening tool Chest X-ray commonly used Clinical trials: n n n Low dose spiral chest CT scan Sputum analysis Chest X-ray
Lung Cancer: Clinical Presentation Local Symptoms n n n cough dyspnea hemoptysis recurrent infections chest pain
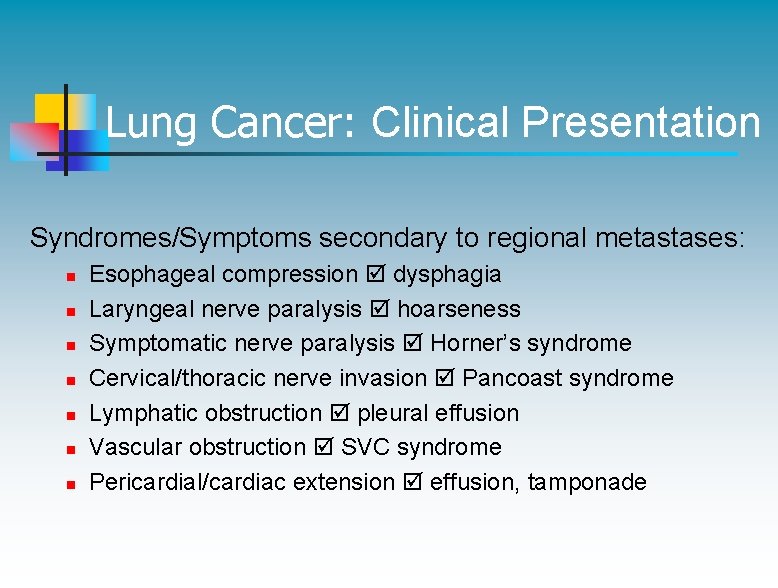
Lung Cancer: Clinical Presentation Syndromes/Symptoms secondary to regional metastases: n n n n Esophageal compression dysphagia Laryngeal nerve paralysis hoarseness Symptomatic nerve paralysis Horner’s syndrome Cervical/thoracic nerve invasion Pancoast syndrome Lymphatic obstruction pleural effusion Vascular obstruction SVC syndrome Pericardial/cardiac extension effusion, tamponade
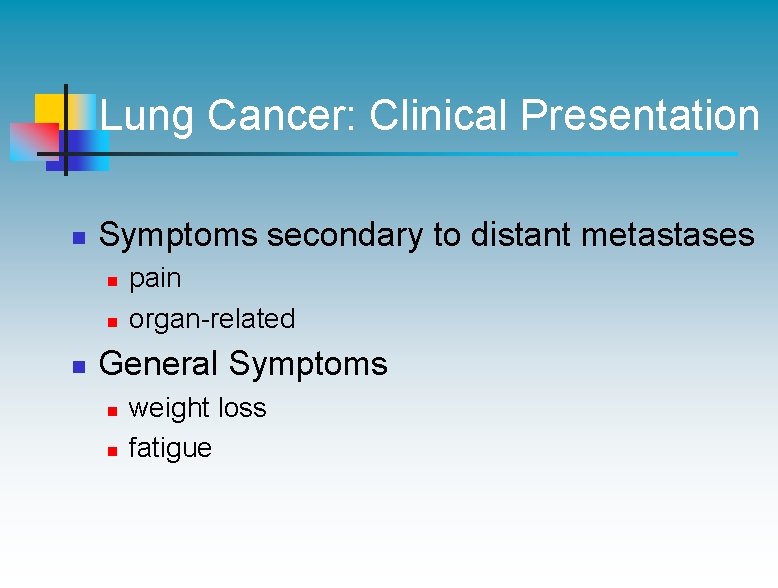
Lung Cancer: Clinical Presentation n Symptoms secondary to distant metastases n n n pain organ-related General Symptoms n n weight loss fatigue
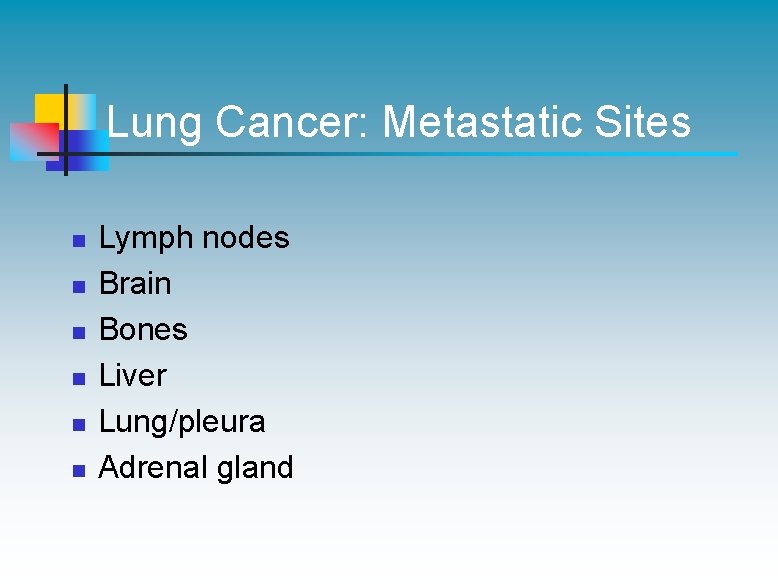
Lung Cancer: Metastatic Sites n n n Lymph nodes Brain Bones Liver Lung/pleura Adrenal gland
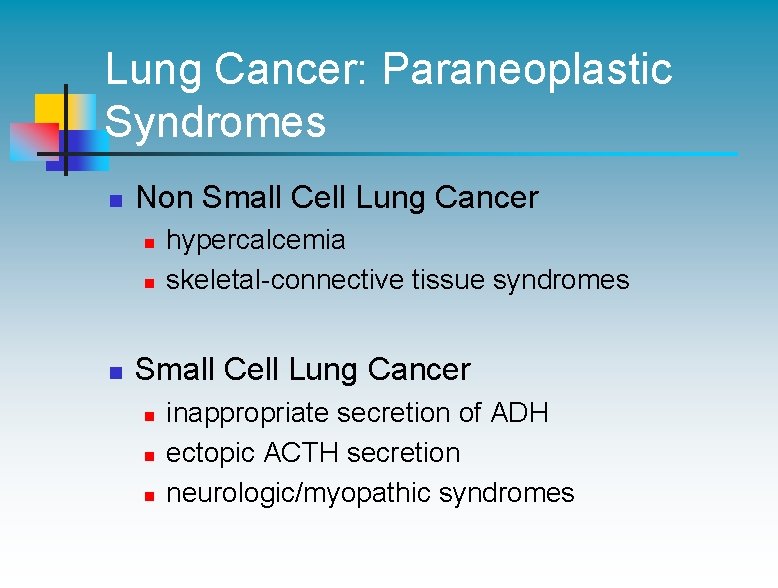
Lung Cancer: Paraneoplastic Syndromes n Non Small Cell Lung Cancer n n n hypercalcemia skeletal-connective tissue syndromes Small Cell Lung Cancer n n n inappropriate secretion of ADH ectopic ACTH secretion neurologic/myopathic syndromes
Lung Cancer: Diagnosis n n History and Physical exam Diagnostic tests n n n Chest x-ray Biopsy (bronchoscopy, needle biopsy, surgery) Staging tests n n CT chest/abdomen Bone scan Bone marrow aspiration PET scan
Lung Cancer: Prognostic Factors n Stage at diagnosis n Performance status
Lung Cancer: Cell Types Non Small Cell Lung Cancer (NSCLC) Small Cell Lung Cancer (SCLC)
Non Small Cell Lung Cancer (NSCLC) n n 80% of all lung cancers Better survival rates when found in early stages
NSCLC: Histologic Cell Types n Adenocarcinoma n Squamous Cell Carcinoma n Large Cell Carcinoma
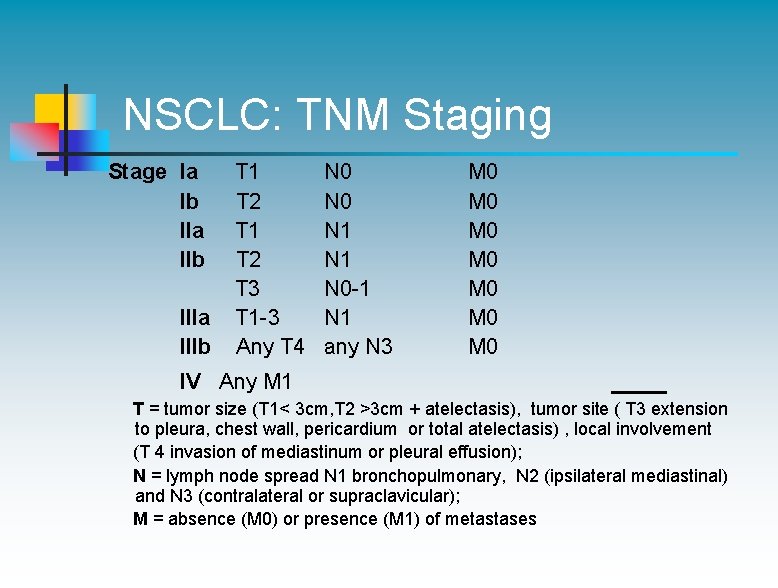
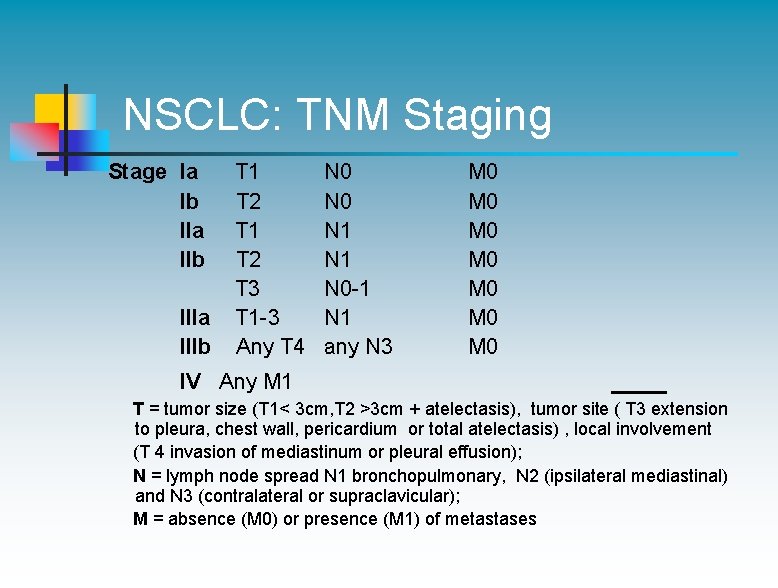
NSCLC: TNM Staging Stage Ia T 1 Ib T 2 IIa T 1 IIb T 2 T 3 IIIa T 1 -3 IIIb Any T 4 IV Any M 1 N 0 N 1 N 0 -1 N 1 any N 3 M 0 M 0 T = tumor size (T 1< 3 cm, T 2 >3 cm + atelectasis), tumor site ( T 3 extension to pleura, chest wall, pericardium or total atelectasis) , local involvement (T 4 invasion of mediastinum or pleural effusion); N = lymph node spread N 1 bronchopulmonary, N 2 (ipsilateral mediastinal) and N 3 (contralateral or supraclavicular); M = absence (M 0) or presence (M 1) of metastases
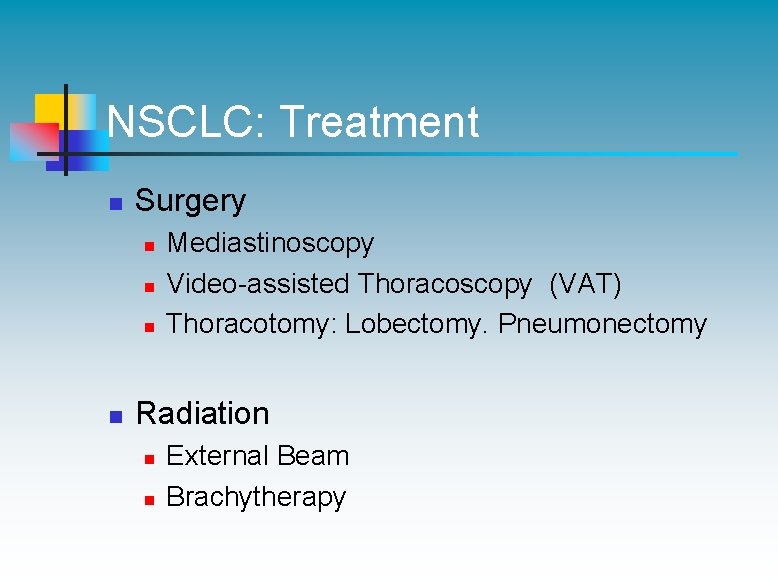
NSCLC: Treatment n Surgery n n Mediastinoscopy Video-assisted Thoracoscopy (VAT) Thoracotomy: Lobectomy. Pneumonectomy Radiation n n External Beam Brachytherapy
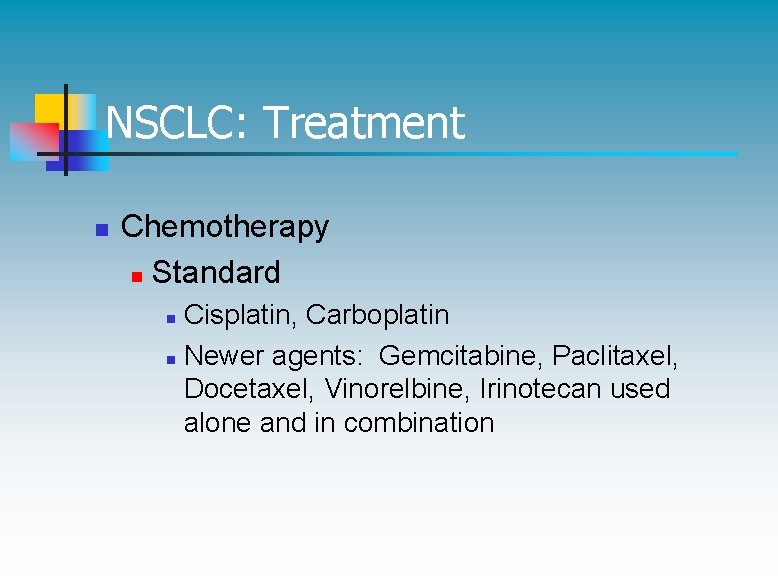
NSCLC: Treatment n Chemotherapy n Standard Cisplatin, Carboplatin n Newer agents: Gemcitabine, Paclitaxel, Docetaxel, Vinorelbine, Irinotecan used alone and in combination n
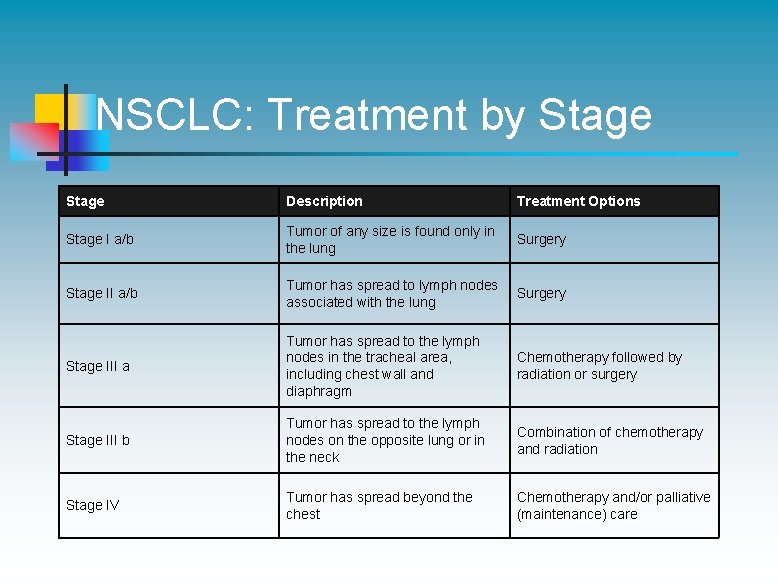
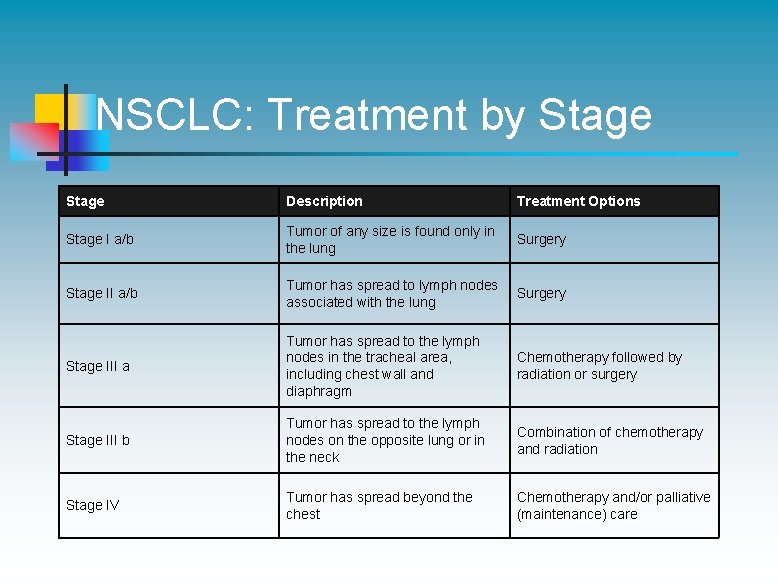
NSCLC: Treatment by Stage Description Treatment Options Stage I a/b Tumor of any size is found only in the lung Surgery Stage II a/b Tumor has spread to lymph nodes associated with the lung Surgery Stage III a Tumor has spread to the lymph nodes in the tracheal area, including chest wall and diaphragm Chemotherapy followed by radiation or surgery Stage III b Tumor has spread to the lymph nodes on the opposite lung or in the neck Combination of chemotherapy and radiation Stage IV Tumor has spread beyond the chest Chemotherapy and/or palliative (maintenance) care
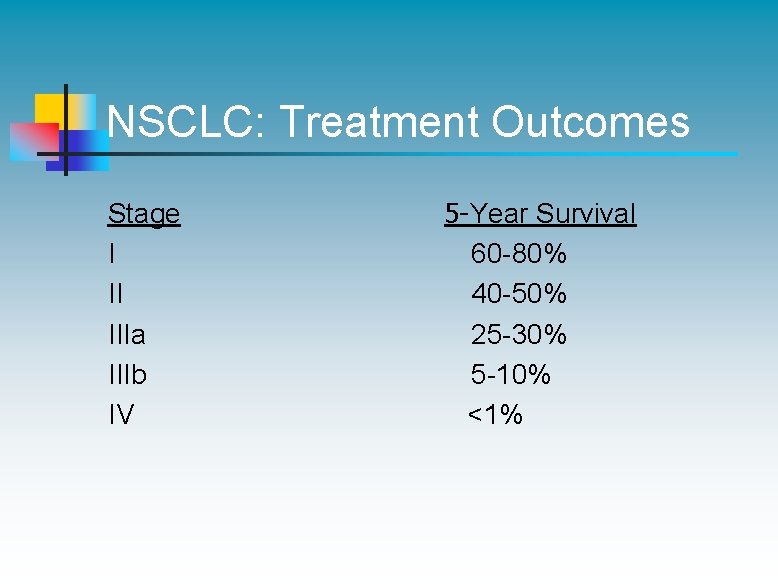
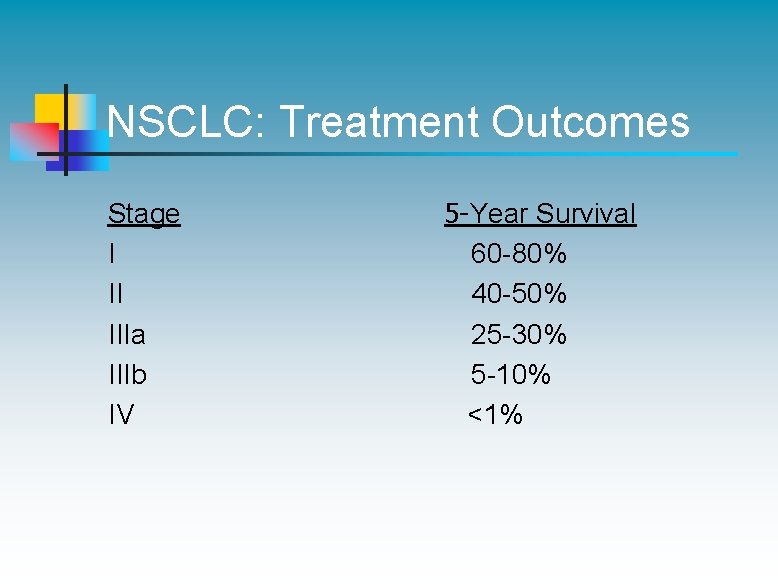
NSCLC: Treatment Outcomes Stage I II IIIa IIIb IV 5 -Year Survival 60 -80% 40 -50% 25 -30% 5 -10% <1%
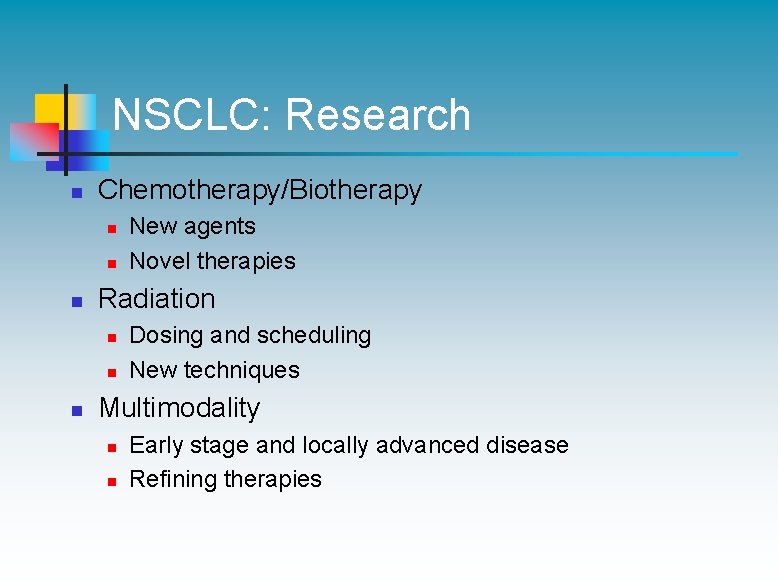
NSCLC: Research n Chemotherapy/Biotherapy n n n Radiation n New agents Novel therapies Dosing and scheduling New techniques Multimodality n n Early stage and locally advanced disease Refining therapies
Small Cell Lung Cancer (SCLC) n n Most aggressive lung cancer Responsive to chemotherapy and radiation but recurrence rate is high even in early stage
SCLC: Cell Types n Oat Cell n Intermediate n Combined
SCLC: Staging n Limited Stage Defined as tumor involvement of one lung, the mediastinum and ipsilateral and/or contralateral supraclavicular lymph nodes or disease that can be encompassed in a single radiotherapy port. n Extensive Stage Defined as tumor that has spread beyond one lung, mediastinum, and supraclavicular lymph nodes. Common distant sites of metastases are the adrenals, bone, liver, bone marrow, and brain.
SCLC: Treatment n Limited Disease n n Chemotherapy Concomitant Radiation Prophylactic Cranial Irradiation Extensive Disease n n Chemotherapy Palliative radiation
SCLC: Treatment n Chemotherapy: n n Most commonly used initial regimen: Cisplatin or Carboplatin plus Etoposide x 4 -6 cycles Newer agents under evaluation: Topotecan, Paclitaxel, Docetaxel, Irinotecan, Gemcitabine
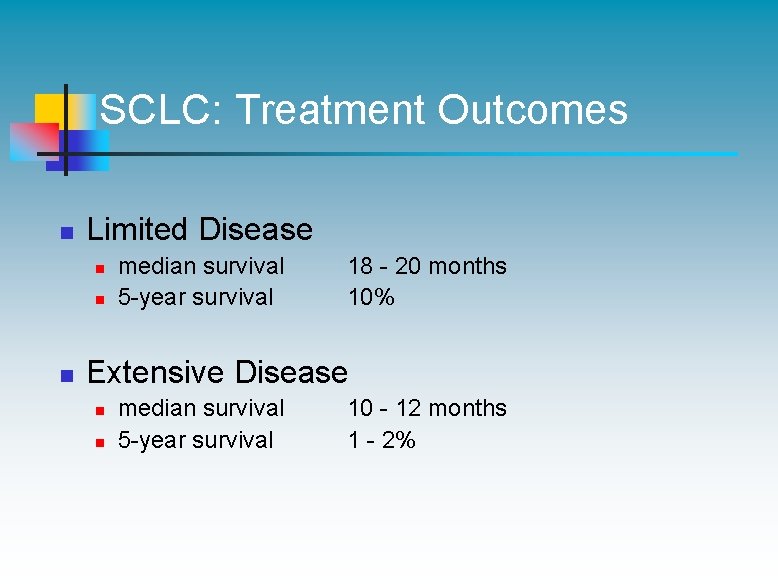
SCLC: Treatment Outcomes n Limited Disease n n n median survival 5 -year survival 18 - 20 months 10% Extensive Disease n n median survival 5 -year survival 10 - 12 months 1 - 2%

SCLC: Research Goal: To improve disease-free interval and length of survival n n New agents Vaccines Radiation schedules Prophylactic Cranial Irradiation
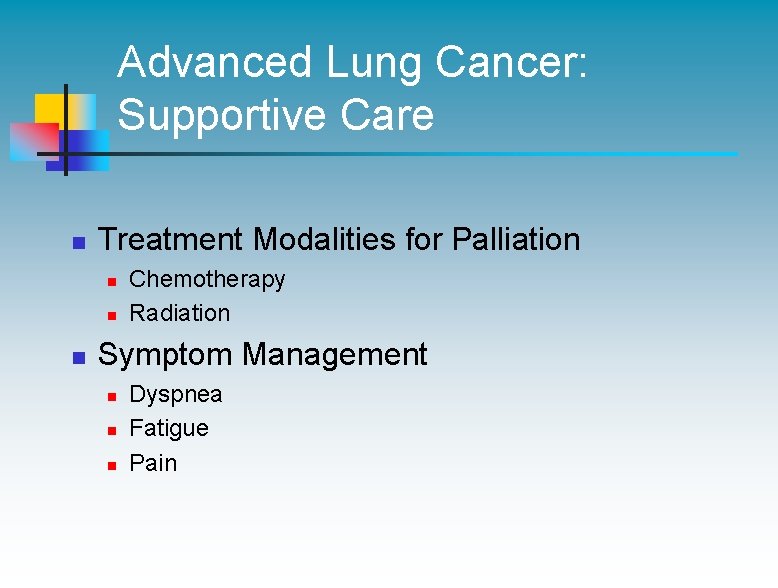
Advanced Lung Cancer: Supportive Care n Treatment Modalities for Palliation n Chemotherapy Radiation Symptom Management n n n Dyspnea Fatigue Pain
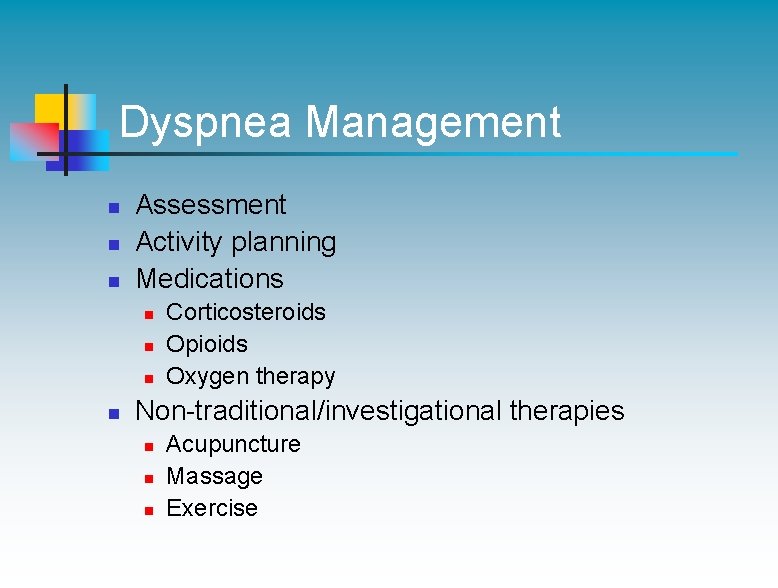
Dyspnea Management n n n Assessment Activity planning Medications n n Corticosteroids Opioids Oxygen therapy Non-traditional/investigational therapies n n n Acupuncture Massage Exercise
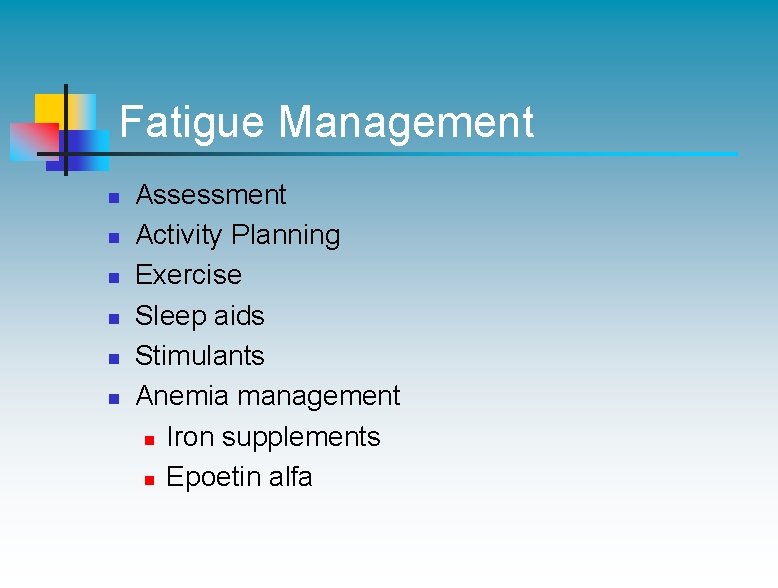
Fatigue Management n n n Assessment Activity Planning Exercise Sleep aids Stimulants Anemia management n Iron supplements n Epoetin alfa
Pain Management n n Assessment Medications: n n Opioids NSAIDS Corticosteroids Nonpharmacologic Interventions: n n Heat/cold Topical agents Massage Behavioral Therapy
Lung Cancer: Conclusions n n n Smoking cessation is essential for prevention of lung cancer. New screening tools offer promise for detection of early lung tumors. Clinical trials are testing promising new treatments. New treatments offer improved efficacy and fewer side effects. Treatment can palliate symptoms and improve quality of life.