LUNG CANCER Marianna Strakhan MD Attending Physician Department

- Slides: 29
LUNG CANCER Marianna Strakhan, MD Attending Physician Department of Hematology/Oncology Jacobi Medical Center Bronx, NY March 30, 2010
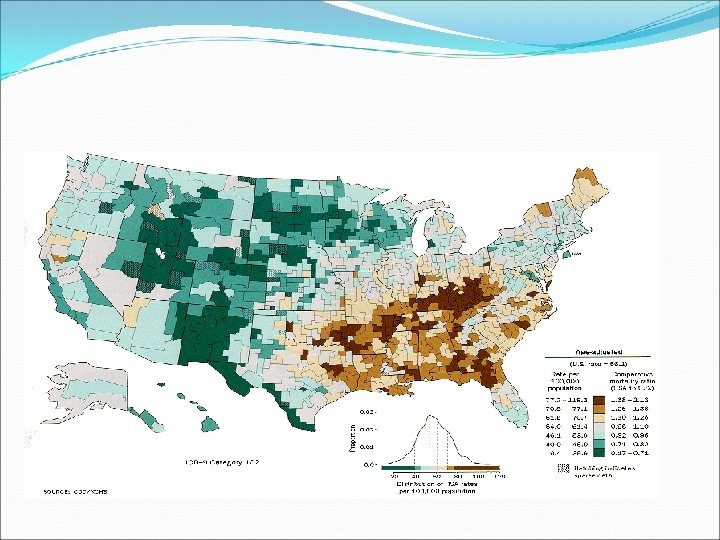
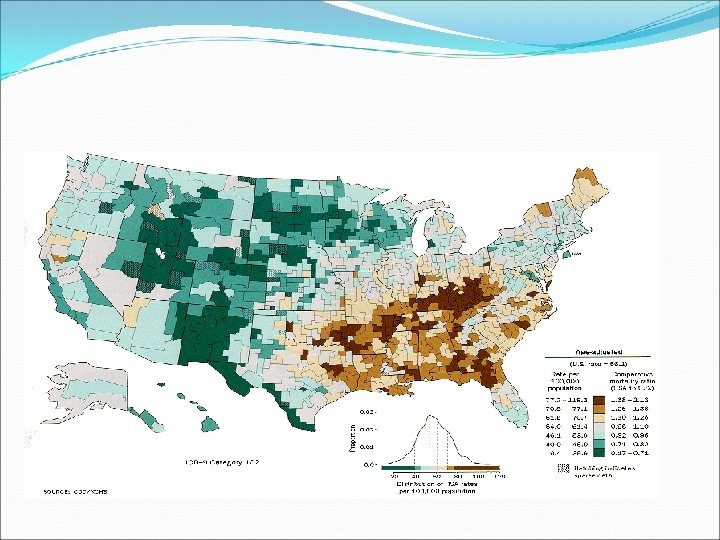
Incidence 2 nd most common type of malignancy in the U. S. among both men and women Most common form of cancer mortality in the U. S. in both men and women In 2007 – approximately 215, 000 new cases of Lung cancer were diagnosed in the U. S, with 162, 000 deaths Between 1990 and 2003 – incidence of lung cancer have remained stable in men, however in women, incidence increased by 60% (incidence in African american females being partially higher than white females). **Incidence increase is seen among large portion of never-smokers, healthy, and active women)
Incidence Although deaths have begun decreasing in MEN (likely due to decrease in smoking), mortality in WOMEN has reached a plateau Almost ½ of all cancer deaths now occur in women 10 – 15% of lung cancer victims are non-smokers. Among that group, women are 2 -3 x more likely than men to get the disease
Incidence Median age of diagnosis is 66 y. o. in both women and men. More of the patients <50 y. o. at time of diagnosis were women In women, 45% of all lung cancers were adenocarcinoma, followed by 22% small cell cancer, 21% squamous cell, rest as other subtypes (in men, squamous subtype is most common, followed by adeno, followed by small cell)
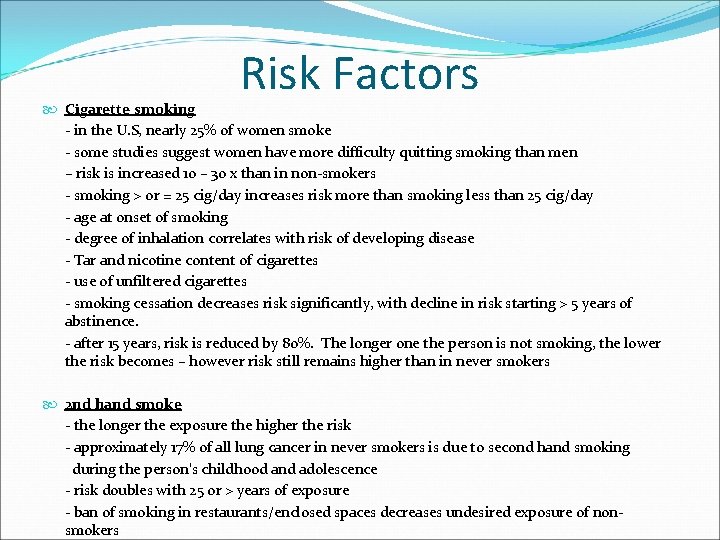
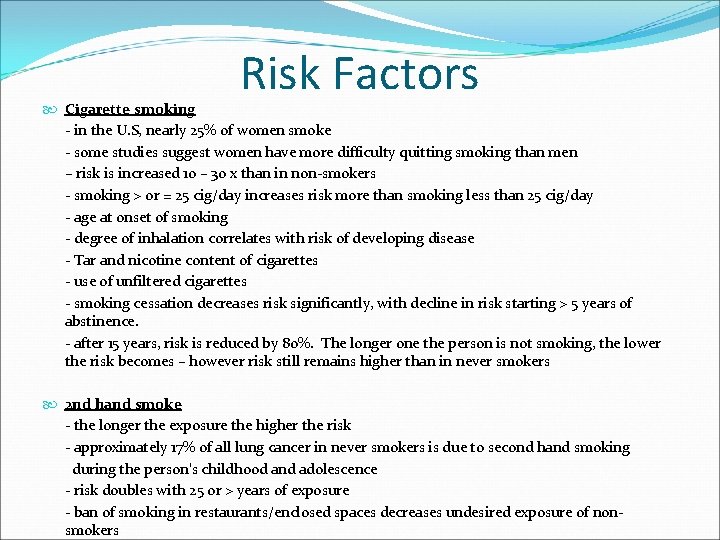
Risk Factors Cigarette smoking - in the U. S, nearly 25% of women smoke - some studies suggest women have more difficulty quitting smoking than men – risk is increased 10 – 30 x than in non-smokers - smoking > or = 25 cig/day increases risk more than smoking less than 25 cig/day - age at onset of smoking - degree of inhalation correlates with risk of developing disease - Tar and nicotine content of cigarettes - use of unfiltered cigarettes - smoking cessation decreases risk significantly, with decline in risk starting > 5 years of abstinence. - after 15 years, risk is reduced by 80%. The longer one the person is not smoking, the lower the risk becomes – however risk still remains higher than in never smokers 2 nd hand smoke - the longer the exposure the higher the risk - approximately 17% of all lung cancer in never smokers is due to second hand smoking during the person’s childhood and adolescence - risk doubles with 25 or > years of exposure - ban of smoking in restaurants/enclosed spaces decreases undesired exposure of nonsmokers
Risk Factors Asbestos Radon Arsenic Ionizing radiation Polycyclic aromatic hydrocarbons Nickel Pulmonary Fibrosis HIV infection Family History Beta Carotene (initially used for chemoprevention, noted to be associated with higher risk of lung cancer in smokers) Race (African Americans and Hawaiians have higher risk of lung cancer incidence among persons who smoke <30 cig/day, no difference between the races among persons smoking >30 cig/day)
Risk Factors *Lung cancer in women is a biologically and genetically different disease than in men: Genes that cause women to be more vulnerable to the harmful effects of tobacco smoke Differences in how the chemicals in tobacco are metabolized (broken down) by the body Changes to genes that control cell growth, which may result in the development of cancer A decreased ability of the body to repair damaged DNA, as DNA damage can promote the development of cancer Hormones, such as estrogen, which could directly or indirectly affect cancer growth
Signs and Symptoms Cough Hemoptysis Dyspnea Chest Pain Hoarseness (due to involvement of recurrent laryngeal nerve) SVC syndrome (dilated neck veins, facial edema) – due to pressure on SVC by the tumor Pancoast’s syndrome – pain in shoulder or arm, Horner’s syndrome (miosis, ptosis, anhidrosis), atrophy of hand muscles Weight loss Paraneoplastic syndromes -example: Hypercalcemia in Squamous cell ca SIADH in Small Cell Ca
SVC Syndrome Etiology: -result of compression of SVC by either malignancy (RUL mass) or thrombosis (mainly due to use of intravascular device) -most common etiology is lung cancer -may also be due to infections (TB, etc. . ) or hematological malignancies such as lymphoma/leukemia Signs/Symptoms: -symptoms may develop over weeks or longer -increased venous pressure leads to edema of head, neck and arms -headache -cyanosis -cough, dyspnea -dysphasia, stridor
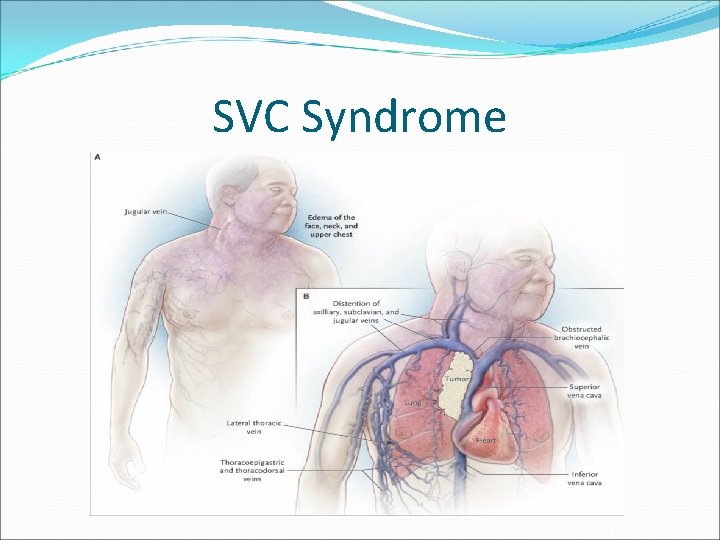
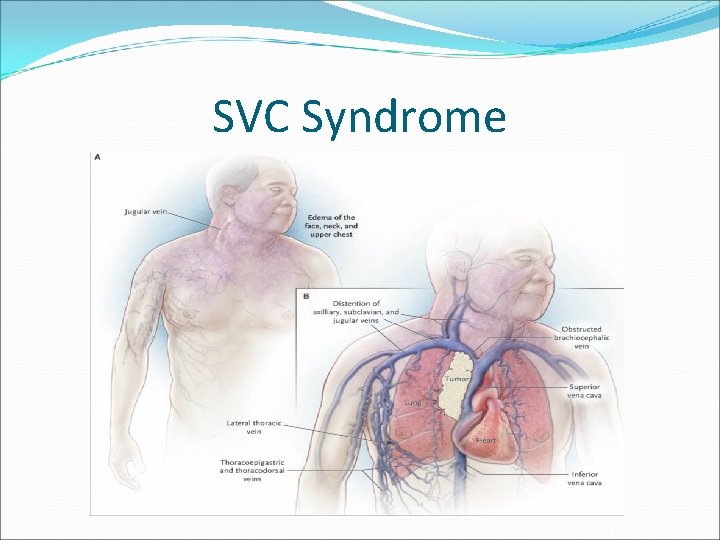
SVC Syndrome

SVC Syndrome
SVC Syndrome Diagnosis -CXR (mediastinal widening, mediastinal mass) -CT neck/chest -ultrasound/doppler to r/o thrombosis of SVC Treatment -Oxygen -elevation of the upper body -diuretics, fluid restriction -anticoagulation if thrombosis -biopsy – obtain pathology prior to treatment -*chemotherapy -radiation therapy -steroids (benefits unproven) -endovascular stents (if conventional therapy unsuccessful) Prognosis -patients with malignant obstruction of SVC have Overall survival of <7 months
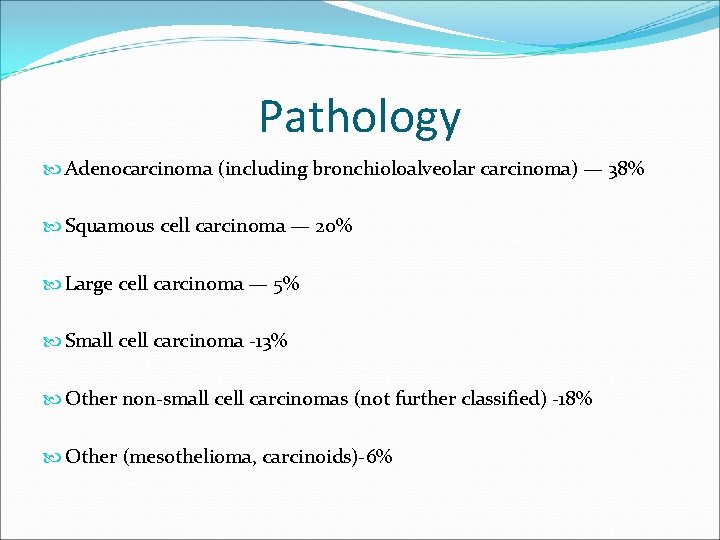
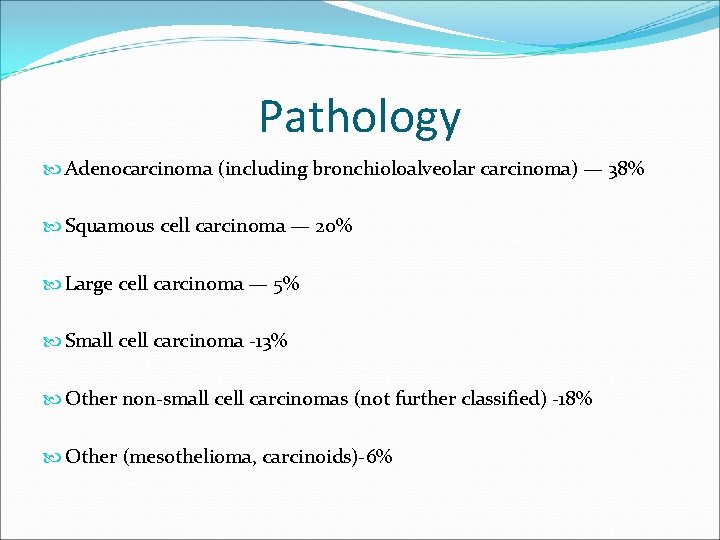
Pathology Adenocarcinoma (including bronchioloalveolar carcinoma) — 38% Squamous cell carcinoma — 20% Large cell carcinoma — 5% Small cell carcinoma -13% Other non-small cell carcinomas (not further classified) -18% Other (mesothelioma, carcinoids)-6%
NSC Lung Cancer Adenocarcinoma -Bronchioloalveolar subtype (more common in never smokers and women) Squamous cell Carcinoma -Centrally located -Often cavitates Large Cell Carcinoma *prognosis is similar among the subtypes
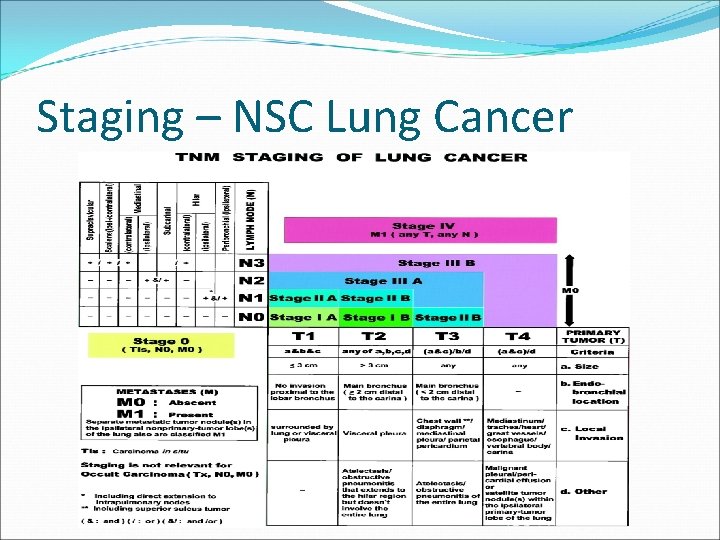
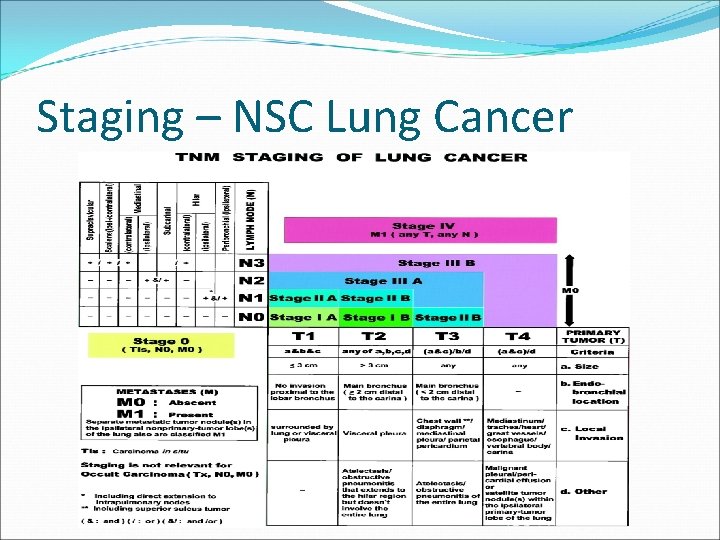
Staging – NSC Lung Cancer
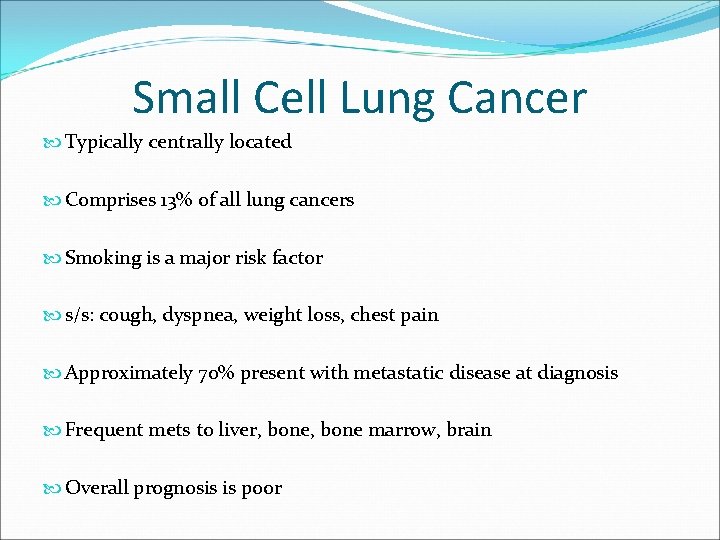
Small Cell Lung Cancer Typically centrally located Comprises 13% of all lung cancers Smoking is a major risk factor s/s: cough, dyspnea, weight loss, chest pain Approximately 70% present with metastatic disease at diagnosis Frequent mets to liver, bone marrow, brain Overall prognosis is poor
Staging – Small Cell Lung Cancer Limited Stage -disease confined to ipsilateral hemithorax -confined to a single radiotherapy port Extensive Stage -evidence of disease outside of ipsilateral hemithorax -disease which can not be covered by a single radiotherapy port
Mesothelioma Rare type of cancer Almost always caused by exposure to asbestos Malignant cells develop in the mesothelium– the lining of the body’s organs (example: pleura) There is no association between mesothelioma and smoking, although smoking greatly increases risk of asbestos induced cancer
Screening NO SCREENING TEST (CXR, CT, OR SPUTUM CYTOLOGY) HAS BEEN SHOWN TO REDUCE MORTALITY FROM LUNG CANCER
Diagnosis History and Physical Laboratory studies Radiographic Imaging (CT, PET, bone scan) Tissue sampling
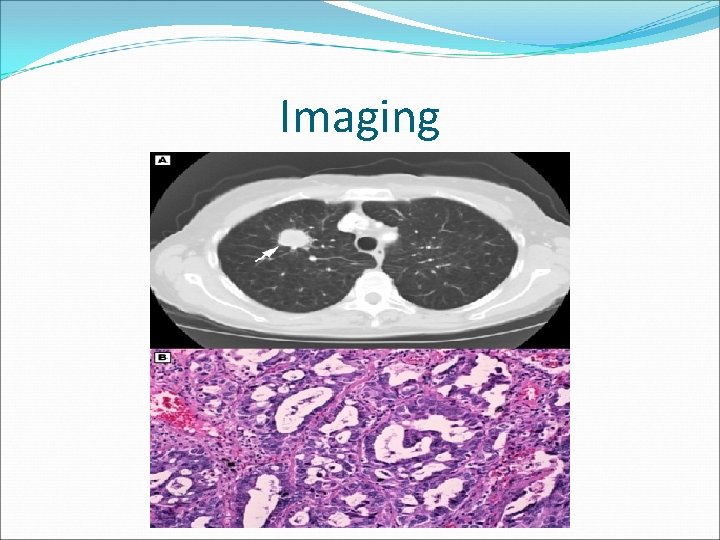
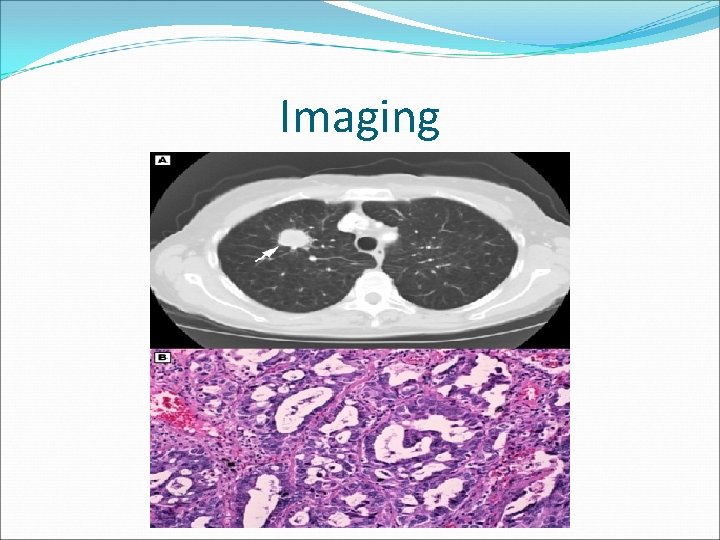
Imaging
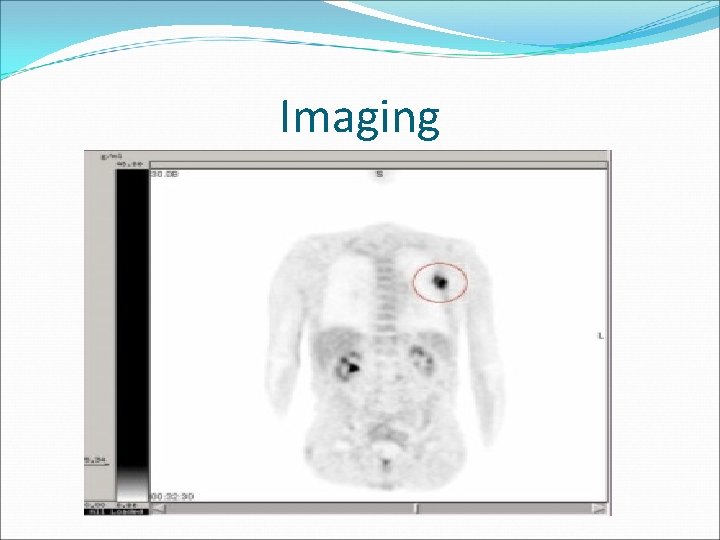
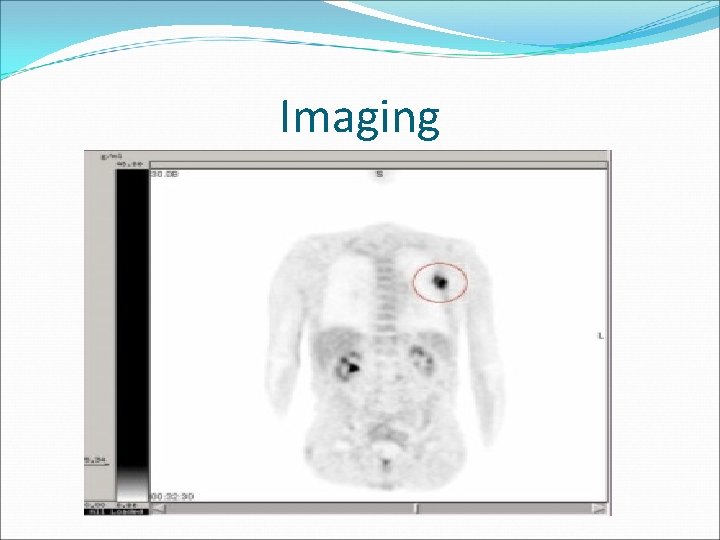
Imaging
Treatment Approach to treatment is multifactorial Depends on: 1. type of cancer (Non-small cell including subtype or small cell) 2. stage of disease 3. patient’s age 4. performance status 5. patient’s smoking status 6. patient’s preference Options include: 1. Surgery 2. Radiation therapy 3. Chemotherapy 4. Combination of above
Pharmacology Chemotherapy side –effects Carboplatin – neuropathy, renal toxicity Cisplatin – neuropathy, renal toxicity, renal wasting of electrolytes, hearing loss Paclitaxel – neuropathy, allergic reactions to cremaphor (preservative), chest pain, fluid retention Navelbine – neurotoxicity, cytopenias, fatigue * all – cytopenias, nausea/vomiting, hair loss, fatigue
IPASS Study EGFR inhibitor (Iressa in Europe, oral form -Tarceva in U. S. ) Compared with standard chemotherapy (Carbo/Taxol) Found that in women, Asian descent, non-smokers, with adenocarcinoma, with EGFR mutation – PFS >3 x higher with EGFR inhibitor than with standard chemotherapy.
Prognosis NSC Lung Cancer: 5 year overall survival: -Stage I – 50 -60% -Stage IV – 1% -Stage IV disease median survival 9 months Small Cell Lung Cancer: 5 year overall survival: -Limited disease – 20% -Extensive disease - <1%
Prognosis stage specific survival rates are better in women than in men in both NSC and small cell lung cancer women who underwent surgical resection of disease had longer O. S. than men with same stage and surgery
THANK YOU