Lumbar puncture Bone marrow aspiration Dr M Torfehnezhad

Lumbar puncture &Bone marrow aspiration Dr. M. Torfehnezhad Pediatrician
Cardinal Symptoms of Cancer in Children Unusual mass or swelling Unexplained paleness & loss of energy Sudden tendency to bruise Persistent, localized pain or limping Prolonged, unexplained fever/illness Frequent headaches, often with vomiting Sudden eye or vision changes Excessive, rapid weight loss
Common Forms of Childhood Cancer Leukemia Lymphoma Brain & CNS tumors Bone Solid tumors Soft tissue tumors
Diagnostic Tests Lumbar puncture Bone marrow aspiration Bone marrow biopsy Radiographic examinations CT MRI Ultrasound Biopsy of tumor
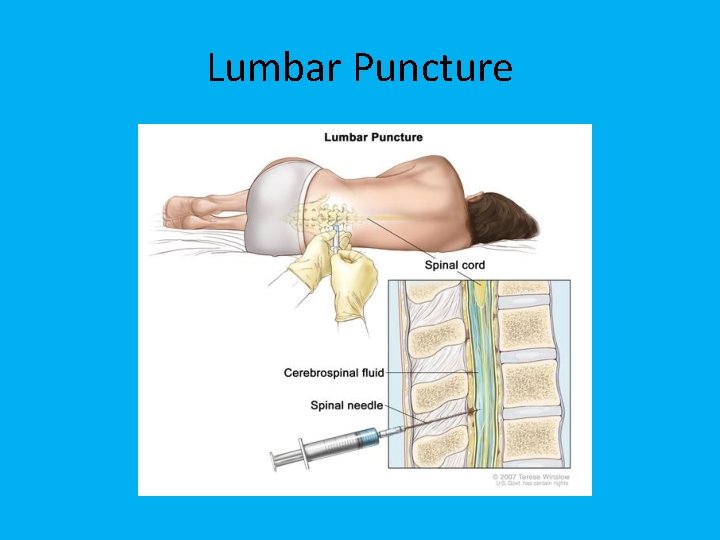
Lumbar Puncture
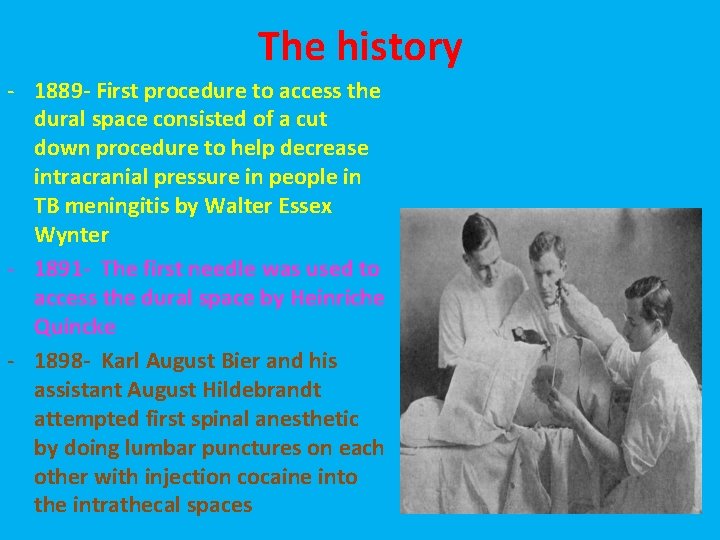
The history - 1889 - First procedure to access the dural space consisted of a cut down procedure to help decrease intracranial pressure in people in TB meningitis by Walter Essex Wynter - 1891 - The first needle was used to access the dural space by Heinriche Quincke - 1898 - Karl August Bier and his assistant August Hildebrandt attempted first spinal anesthetic by doing lumbar punctures on each other with injection cocaine into the intrathecal spaces
Indications for Lumbar Puncture • Diagnosis of central nervous system (CNS) infection • Diagnosis of subarachnoid hemorrhage (SAH) • Evaluation and diagnosis of demylinating or inflammatory CNS processes • Infusion of anesthetic, chemotherapy, or contrast agents into the spinal canal • Treatment of idiopathic intracranial hypertension
– Diagnostic Test for infectious and noninfectious neurologic conditions – Rarely diagnostic as a single agent – Combine with history, physical and selected lab tests
Contraindications • Skin infection near site of LP • Suspicion of intracranial pressure due to cerebral mass • Uncorrected coagulopathy • Acute spinal cord trauma
Contraindications - Elevated Intracranial pressure- head trauma, Intracranial mass (especially in the posterior fossa) - Cutaneous infection overlying the site - Noncommunicating hydrocephalus - Coagulopathy (thrombocytopenia is relative contraindication though no trials show increased risk of bleeding)
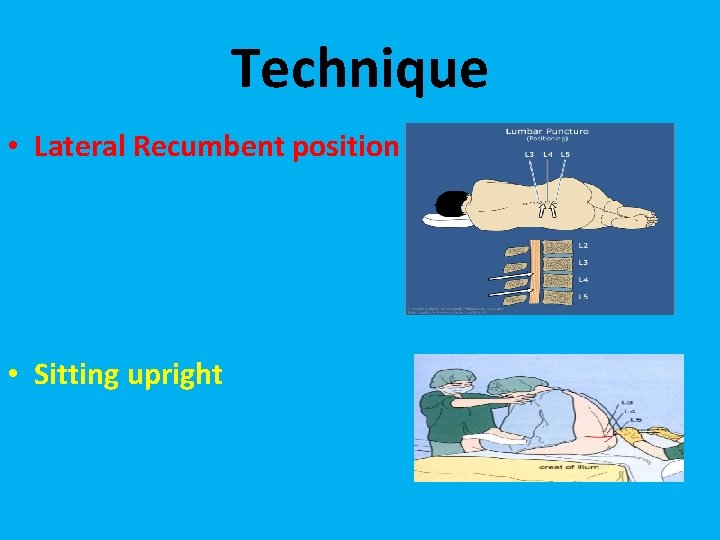
Technique • Lateral Recumbent position • Sitting upright
Procedure • Determine correct level of entry • Highest points of the iliac crests should be identified and palpated • Direct line joining the crests identifies L 4 • Spinous processes L 3, L 4, and L 5 can be directly palpated • Goal: Subarachnoid space at L 3/4 or L 4/5
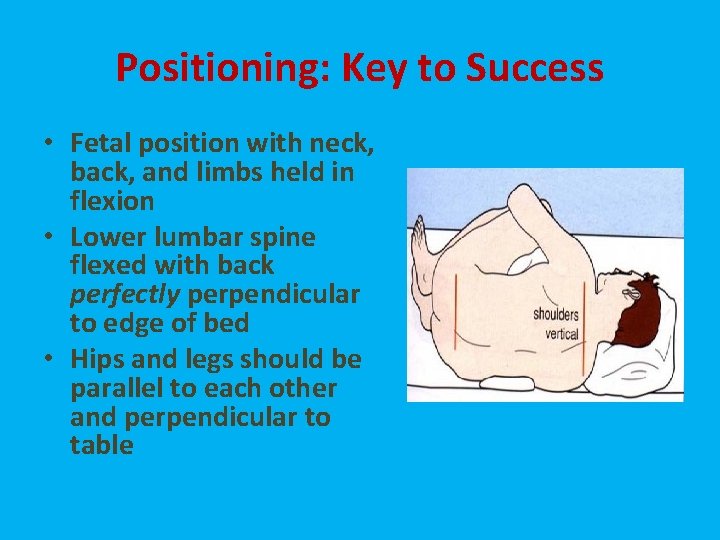
Positioning: Key to Success • Fetal position with neck, back, and limbs held in flexion • Lower lumbar spine flexed with back perfectly perpendicular to edge of bed • Hips and legs should be parallel to each other and perpendicular to table
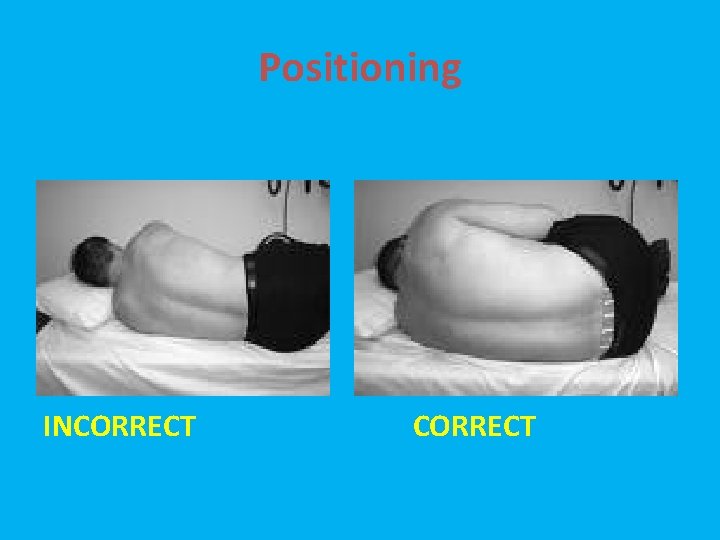
Positioning INCORRECT
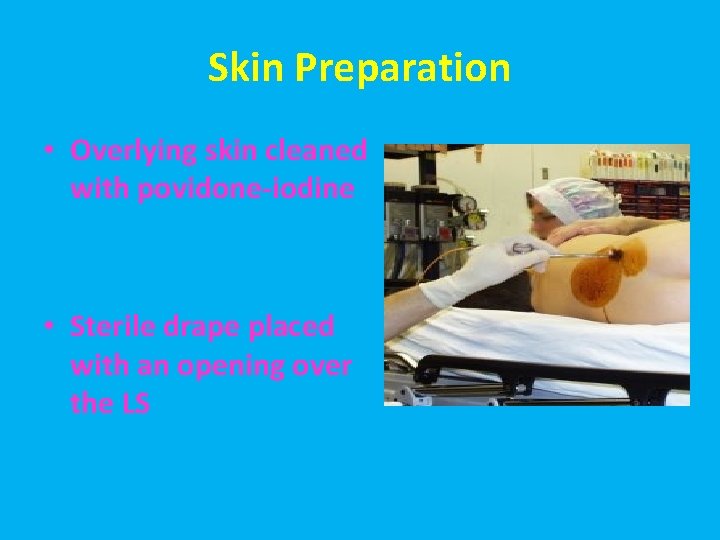
Skin Preparation • Overlying skin cleaned with povidone-iodine • Sterile drape placed with an opening over the LS
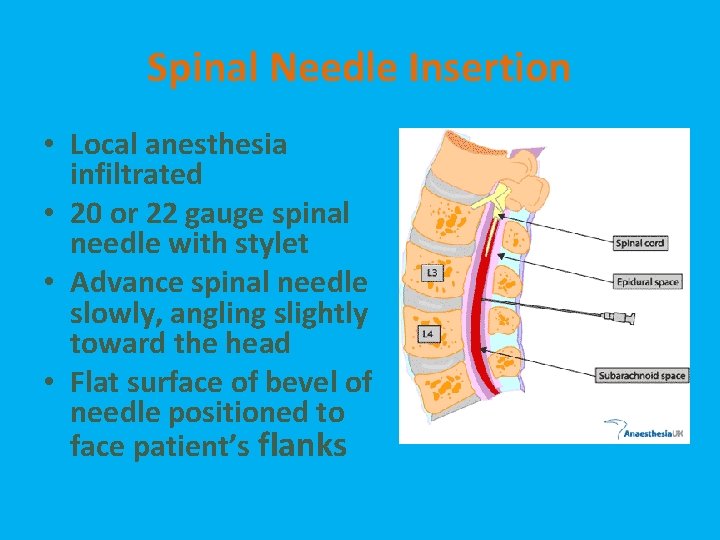
Spinal Needle Insertion • Local anesthesia infiltrated • 20 or 22 gauge spinal needle with stylet • Advance spinal needle slowly, angling slightly toward the head • Flat surface of bevel of needle positioned to face patient’s flanks

Collecting CSF • 4 – tubes • 8 -12 drops, 1 -2 ml. • Cytology more than 4 ml. • Ordering/labeling your CSF samples correctly.
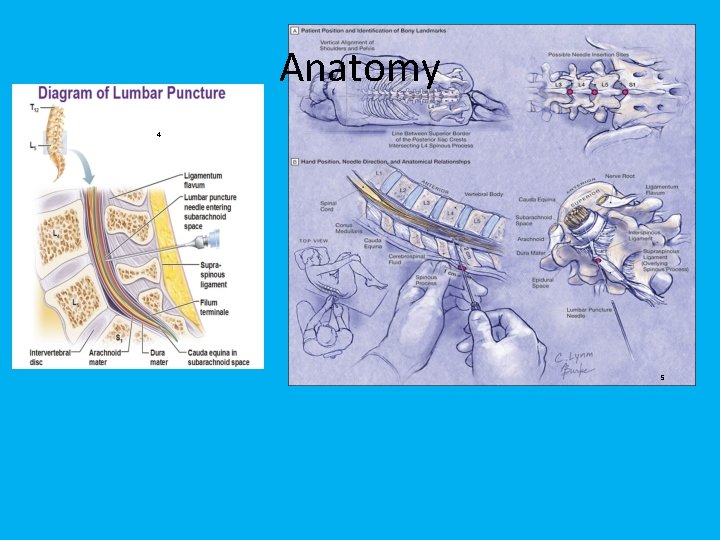
Anatomy 4 5
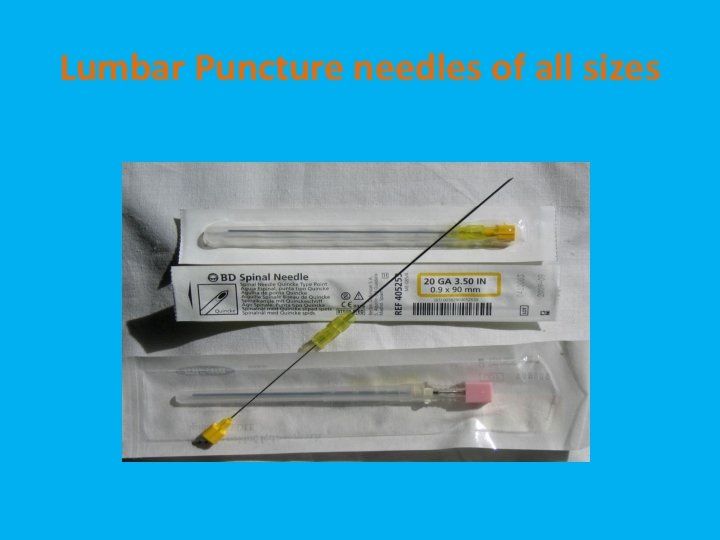
Lumbar Puncture needles of all sizes
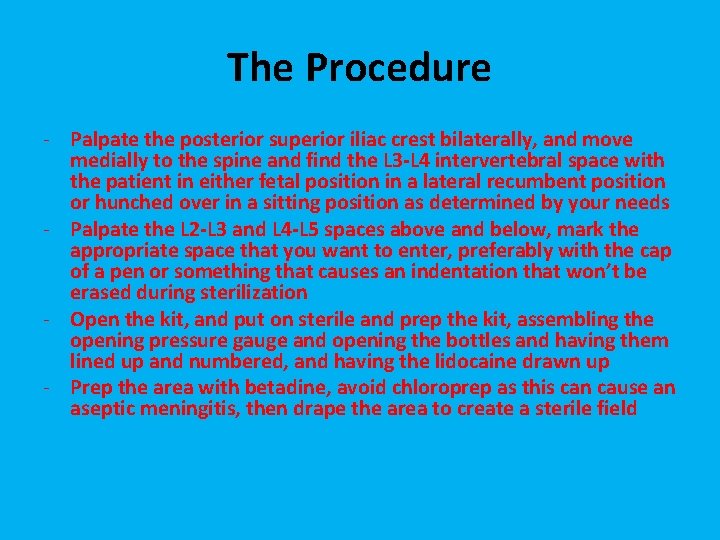
The Procedure - Palpate the posterior superior iliac crest bilaterally, and move medially to the spine and find the L 3 -L 4 intervertebral space with the patient in either fetal position in a lateral recumbent position or hunched over in a sitting position as determined by your needs - Palpate the L 2 -L 3 and L 4 -L 5 spaces above and below, mark the appropriate space that you want to enter, preferably with the cap of a pen or something that causes an indentation that won’t be erased during sterilization - Open the kit, and put on sterile and prep the kit, assembling the opening pressure gauge and opening the bottles and having them lined up and numbered, and having the lidocaine drawn up - Prep the area with betadine, avoid chloroprep as this can cause an aseptic meningitis, then drape the area to create a sterile field
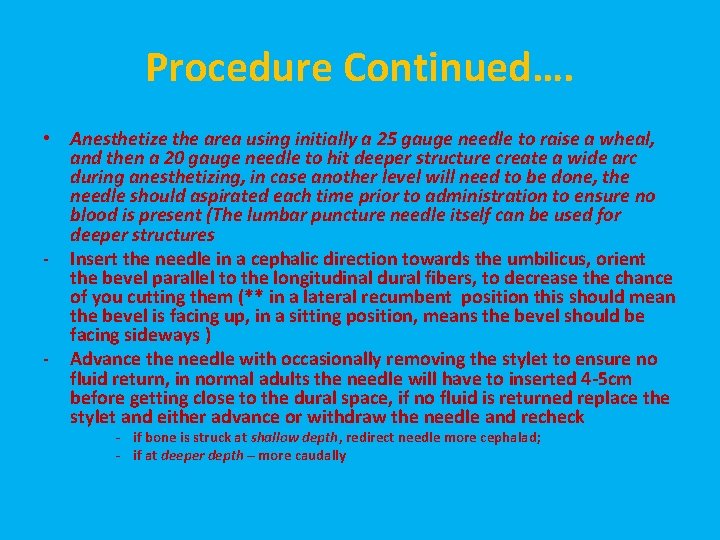
Procedure Continued…. • Anesthetize the area using initially a 25 gauge needle to raise a wheal, and then a 20 gauge needle to hit deeper structure create a wide arc during anesthetizing, in case another level will need to be done, the needle should aspirated each time prior to administration to ensure no blood is present (The lumbar puncture needle itself can be used for deeper structures - Insert the needle in a cephalic direction towards the umbilicus, orient the bevel parallel to the longitudinal dural fibers, to decrease the chance of you cutting them (** in a lateral recumbent position this should mean the bevel is facing up, in a sitting position, means the bevel should be facing sideways ) - Advance the needle with occasionally removing the stylet to ensure no fluid return, in normal adults the needle will have to inserted 4 -5 cm before getting close to the dural space, if no fluid is returned replace the stylet and either advance or withdraw the needle and recheck - if bone is struck at shallow depth, redirect needle more cephalad; - if at deeper depth – more caudally
Complications - Uncal herniation Epidural/perivertebral abscess Paresthesias- temporary or permanent Post lumbar puncture headache Spinal or epidural bleeding Adhesive arachnoiditis Late onset of epidermoid tumours to thecal sac Back pain
CSF analysis - Gram stain: Sensitive in 60 -80% of bacterial meningitis and 40 -60% range in partially treated bacterial meningitis - Cytology: determyning the type & number of cells - Protein - can be adjusted to RBC by decreasing protein concentration by 1 mg/d. L or. 01 g/L for every 1, 000 RBC/mm 3 but both levels have to be drawn from the same tube. - Is the most sensitive indicator of intracranial pathology but not very sensitive. Also, normal levels vary a lot from lab to lab. - Glucose- normally 60% of serum glucose, though in severe hyperglycemia this ratio breaks down as CSF glucose levels do not exceed 300 mg/DL
The End
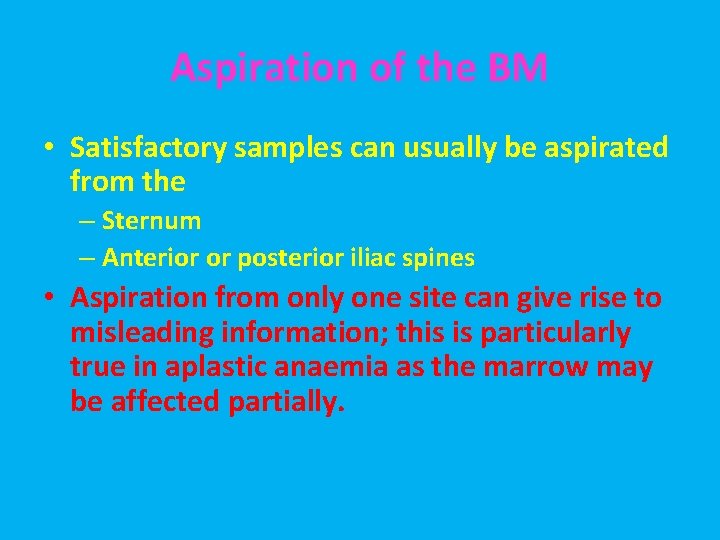
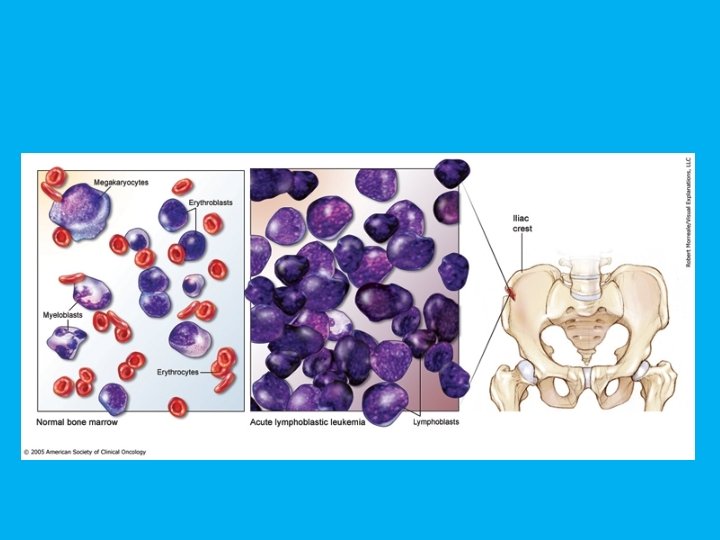
Aspiration of the BM • Satisfactory samples can usually be aspirated from the – Sternum – Anterior or posterior iliac spines • Aspiration from only one site can give rise to misleading information; this is particularly true in aplastic anaemia as the marrow may be affected partially.
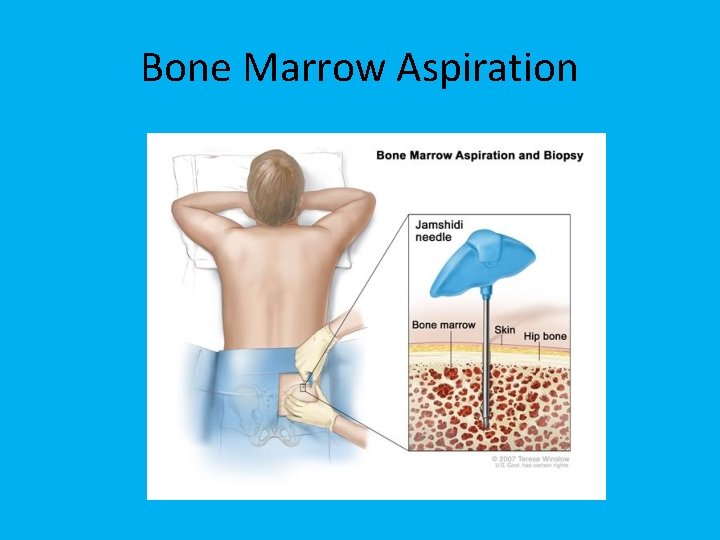
Bone Marrow Aspiration
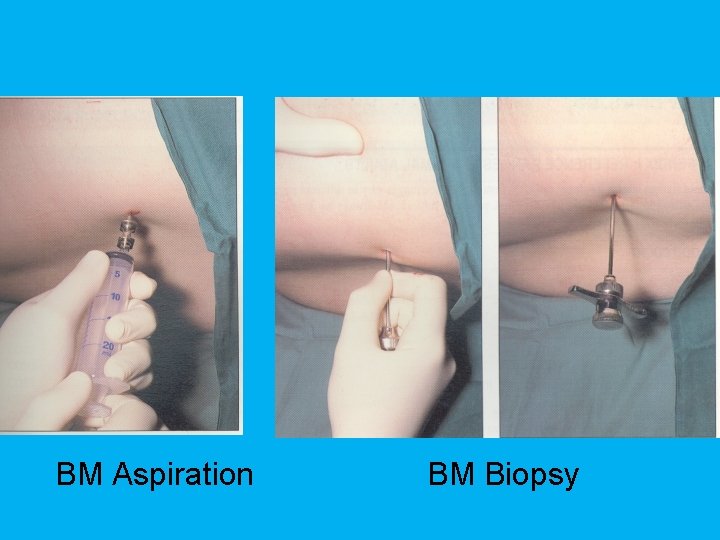
BM Aspiration BM Biopsy
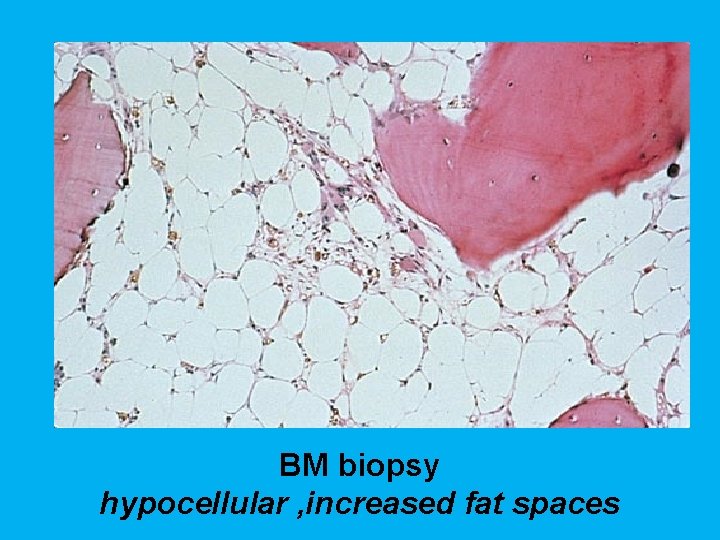
BM biopsy hypocellular , increased fat spaces
• There is little advantage in aspirating more than 0. 3 ml of marrow fluid from a single site for morphological examination as this increases peripheral blood dilution.
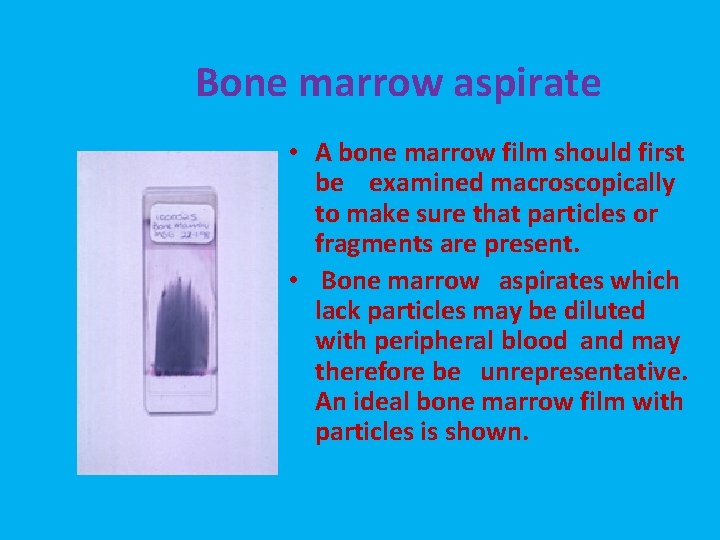
Bone marrow aspirate • A bone marrow film should first be examined macroscopically to make sure that particles or fragments are present. • Bone marrow aspirates which lack particles may be diluted with peripheral blood and may therefore be unrepresentative. An ideal bone marrow film with particles is shown.
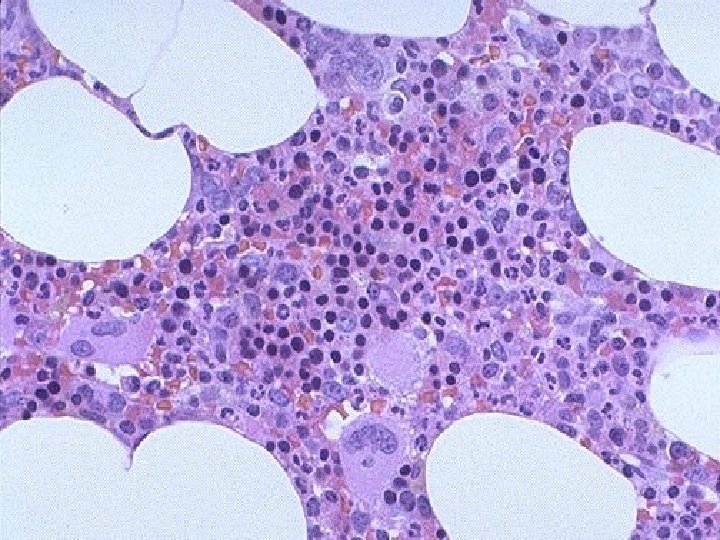
Cells of the bone marrow Erythroid series Myeloid series Megakaryocytic series
Systemic scheme for Examining aspirated BM films • Low power (x 10) – Determine cellularity – Identify megakaryocytes – Look for clumps of abnormal cells – Identify macrophages
Systemic scheme for Examining aspirated BM films • Higher power (x 40, x 100) – Identify all stages of maturation of myeloid and erythroid cells. – Determine the M: E ratio – Perform a differential count – Look for areas of BM necrosis. – Assess the iron content.
• Only after the bone marrow has been carefully assessed on low and medium power should the X 100 oil be used to assess cellular detail.
Points to be considered in BMA reporting • The M: E ratio is the ratio of all granulocytic plus monocytic cells (Myeloid) to all erythroblasts (Erythroid). • For all bone marrow aspirates examined, the report should specify the M: E ratio and the percentage of lymphocytes and plasma cells. • A differential count of at least 200 -300 cells should be performed. • If there is any borderline abnormality, e. g. in the number of blasts, lymphocytes or plasma cells, a 500 cell differential count should be performed.

Thank You

- Slides: 42