LPNC Unit Four Rationale for Intravenous Therapy What




- Slides: 96
LPN-C Unit Four Rationale for Intravenous Therapy
What is the Purpose of Intravenous Therapy? Maintenance ◦ Water ◦ Glucose ◦ Protein ◦ Vitamins ◦ Electrolytes ◦ p. H Restoration of previous losses Replacement of present losses Administration of medication
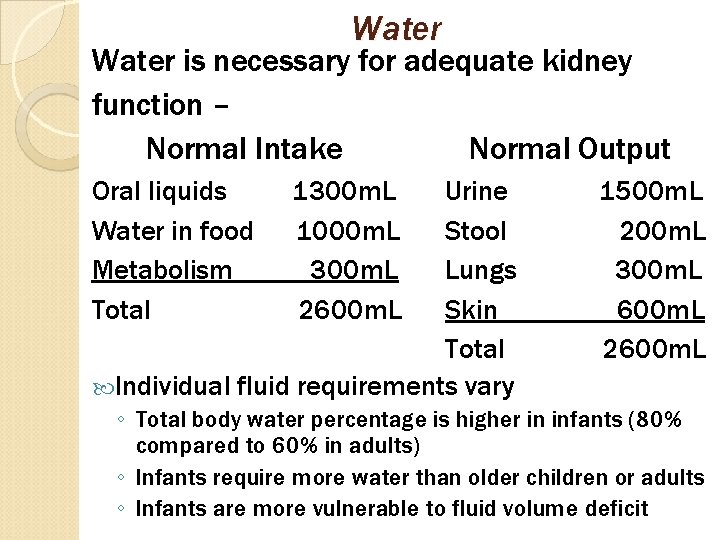
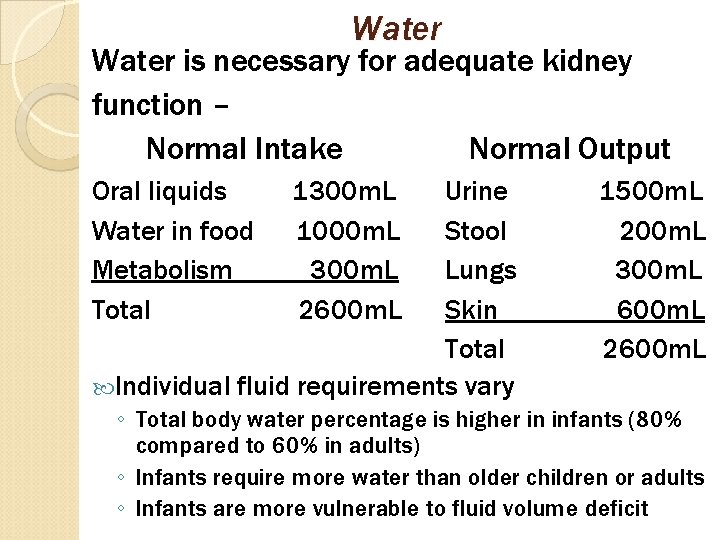
Water is necessary for adequate kidney function – Normal Intake Normal Output Oral liquids Water in food Metabolism Total 1300 m. L 1000 m. L 300 m. L 2600 m. L Urine Stool Lungs Skin Total Individual fluid requirements vary 1500 m. L 200 m. L 300 m. L 600 m. L 2600 m. L ◦ Total body water percentage is higher in infants (80% compared to 60% in adults) ◦ Infants require more water than older children or adults ◦ Infants are more vulnerable to fluid volume deficit
Glucose Converted to glycogen by the liver Has 4 main uses in parenteral therapy ◦ Improves hepatic function ◦ Supplies the necessary calories for energy ◦ Spares body protein ◦ Minimizes ketosis Approximately 100 – 150 g of glucose is needed daily to minimize protein catabolism 1 liter of 5% dextrose in water supplies 50 g of glucose Dextrose in water is available in 2. 5%, 10%, 20%, and 30%
Glucose (cont’d) Dextrose concentrations higher than 10% must be given through a central vein ◦ The exception is 50% dextrose slow IV push at a rate of 3 m. L/min through a peripheral vein for emergency treatment of hypoglycemia Protein Amino acids are the building blocks of the body ◦ Tissue growth and repair ◦ Wound healing Available in concentrations of 3. 5 – 15% Used in TPN centrally and peripherally
Daily Protein (cont’d) requirements = 1 g protein/kg body weight ◦ Amount increases as stress to the body increases Gluconeogenesis = conversion of protein to glucose to meet energy requirements ◦ Occurs during starvation, stress, or infection ◦ Uses large amount of energy ◦ Body will use protein for energy if there are inadequate glucose stores
Vitamins B and C are most frequently used ◦ Vitamin B is needed for the metabolism of carbohydrates and maintenance of GI function ◦ Vitamin C promotes wound healing Electrolytes Correction of electrolyte imbalances is important in preventing serious complications Important in parenteral therapy ◦ Potassium, sodium, chloride, magnesium, phosphorus, calcium, bicarbonate
Electrolytes (cont’d) Potassium ◦ Adequate replacement therapy = 20 m. Eq/L ◦ Patients who need potassium replacement – Stress from tissue injury Wound infection Gastric or bowel surgery Prolonged gastric suction ◦ Assess renal function prior to potassium replacement Excreted through the urine Intoxication can occur rapidly and with no symptoms ◦ Slow rate of infusion no more than 20 m. Eq/L per hour via peripheral line no more than 40 m. Eq/L per hour via central line ◦ Never give potassium via IV push ◦ Always use a cardiac monitor with K+ infusion
Electrolytes (cont’d) Potassium (cont’d) -- ◦ Infiltration of potassium is extremely irritating to the tissue Can cause necrosis Imperative to use extravasation protocol In the case of infiltration, discontinue the infusion, apply cool compresses, and elevate the extremity by 4 inches p. H Most IV solutions are acidic ◦ Allows for longer shelf life ◦ The more acidic a solution, the more irritating to the vein
Parenteral Nutrition Peripheral venous delivery of parenteral nutrition (PPN) ◦ Glucose concentration is not to exceed 10% ◦ Usually utilized for 3 – 7 days ◦ Assess for metabolic abnormalities Hyperglycemia Most common metabolic abnormality in PPN Rapid administration of fluid Increased levels of stress hormones Hypoglycemia can occur if infusion is discontinued abruptly Hypokalemia Insulin-related shift of potassium from the extracellular compartment to the intracellular compartment
Fluid Balance in Infants and Children More vulnerable to fluid volume deficit Kidneys are immature up to 2 years of age ◦ Cannot conserve or excrete water or sodium in response to imbalances as efficiently as adults Body surface area in infants is larger than in adults per size ◦ Lose more fluid through the skin Infants have a higher metabolism rate which requires more water per size ◦ Produce more heat than adults ◦ Larger amount of metabolic waste to secrete Less stable regulatory responses to fluid imbalances
Fluid Balance/Infants/Children (cont’d) Fevers are higher and last longer in acute illness ◦ Increases fluid loss Symptoms of fluid imbalance ◦ Decreased appetite ◦ Less active ◦ More irritable ◦ Flaccid appearance ◦ Diarrhea, vomiting ◦ Decrease in voiding Nursing assessment ◦ Assess concentration of urine
Fluid Balance/Infants/Children (cont’d) Nursing assessment (cont’d) -- ◦ Weigh diapers ◦ Monitor for diarrhea Common cause of isotonic dehydration Proportionate loss of water and electrolytes Formula containing an inappropriately high amount of solute can cause diarrhea that leads to hypertonic dehydration Greater loss of water than electrolytes ◦ Monitor for weight changes Record weight before onset of illness Physician’s records Parent/family/caregiver report Weight loss resulting from fluid volume deficit is more rapid than with loss of body mass
Fluid Balance/Infants/Children (cont’d) Nursing assessment (cont’d) – ◦ Monitor vital signs Blood pressure is not always reliable because elasticity of the blood vessels in children keeps blood pressure stable initially Tissue turgor ◦ Skin remains slightly raised for a few seconds with fluid volume deficit ◦ Skin turgor begins to decrease after 3 -5% body weight is lost as fluid ◦ Obese infants/children have deceptive skin turgor Normal in appearance in spite of fluid volume deficit
Fluid Balance in the Elderly At risk for fluid volume deficit due to normal aging changes ◦ 6% reduction of total body water ◦ Decrease in ratio of intracellular fluid to ECF ◦ Loss of 30 -50% glomeruli by the age of 70 Decrease in glomerular filtration rate Decreased ability to concentrate urine Decreased secretion of aldosterone Decrease in the response of the distal tubule to ADH ◦ Decrease in glucose tolerance ◦ Decreased sensation of thirst ◦ Decreased skin elasticity Poor indication of turgor ◦ Atrophy of the sweat glands
Fluid Balance in the Elderly (cont’d) Normal aging changes (cont’d) -- ◦ Diminished capillary bed Less effective cooling of body temperature ◦ Decreased cardiac output Increased risk for orthostatic hypotension Increased risk for falls ◦ Decreased elasticity of arteries ◦ Immediately assess fluid status with any changes in mental status Typical assessment findings ◦ Dehydration frequently seen ◦ Normal body temperature lower (97°F) ◦ Mucus membranes less moist ◦ Positional changes in blood pressure common
Fluid Balance in the Elderly (cont’d) Typical assessment findings (cont’d) – ◦ Most accurate assessment of skin turgor is over the sternum Special problems in the elderly ◦ Hypernatremia Common problem in LTC facilities Immobility Unable to express thirst ◦ Reduced motility of GI tract Laxative dependency ◦ Heat stroke Elderly more susceptible Decreased efficacy of sweat glands Normal temperature decreases with age Temperature of 99°F would be high for the body
Fluid Balance in the Elderly (cont’d) Special problems (cont’d) -- ◦ Radiocontrast agents (IVP) High in sodium Difficulty excreting due to ↓ glomerular filtration rate ◦ Preoperative concerns Administration of adequate IV fluids before surgery Improves renal blood flow and renal function Minimum urine output should be 50 m. L/hour High risk for hypothermia in the operating room Cool fluids, cool environment, etc. ◦ Diminished respiratory function interferes with elimination of carbon dioxide Leads to respiratory acidosis Achieve maximum ventilation through suction, turning, activity
Fluid Balance in the Elderly (cont’d) Special problems (cont’d) -◦ Preparation for diagnostic tests Bowel cleansing NPO status Diet and Lifestyle Factors Affecting Fluid Balance Difficulty chewing or swallowing ◦ Inadequate food/fluid intake Malnutrition/starvation ◦ Low protein intake; altered fluid volume status Excessive alcohol consumption ◦ Liver damage leading to fluid/electrolyte imbalance

Environmental Factors & Fluid Balance Vigorous exercise increases metabolism, ventilation, sweating ◦ Increases fluid demand ◦ Potential lack of fluid intake Heat injuries ◦ Exposure to hot, humid environments increases sweat production to as much as 2 L/hour ◦ Body fluid weight loss >7% is associated with failure of body cooling mechanisms Medications Altering Fluid Balance Diuretics = excessive fluid loss Chemotherapy = nausea/vomiting, poor oral intake
Fluid Needs for Those with Acute Illness Surgery can result in blood and fluid loss Gastroenteritis causes nausea/vomiting and diarrhea Nasogastric suctioning leads to fluid and electrolyte losses Brain injury from stroke, trauma, or tumor ◦ Causes cerebral edema, which may put pressure on the hypothalamus and/or pituitary ◦ Alters ADH SIADH Diabetes insipidus Excessive or inadequate ADH production/release Burns
Factors Burns affecting fluid loss -- ◦ Surface area The larger the burn, the greater the fluid loss ◦ Extent, depth, and cause of the burn ◦ Age of the client ◦ Pre-existing medical conditions Diagnostic findings – ◦ WBC reflects immune function ◦ Hgb/HCT increases due to fluid loss ◦ Glucose increases due to stress response ◦ Sodium decreases (trapped in third spaces) ◦ Potassium increases due to tissue destruction
Third Burns (cont’d) space fluid shifts -- ◦ Phase I → plasma to interstitial space Occurs rapidly (before the end of the 1 st hour) Plasma leaks out through damaged capillaries at the burn area Edema forms Hypovolemia occurs (may lead to acute tubular necrosis) Decreased renal perfusion Low urine output Hyperkalemia Fluid accumulation phase occurs during the first 36 to 48 hours Capillaries have recovered by the end of this time
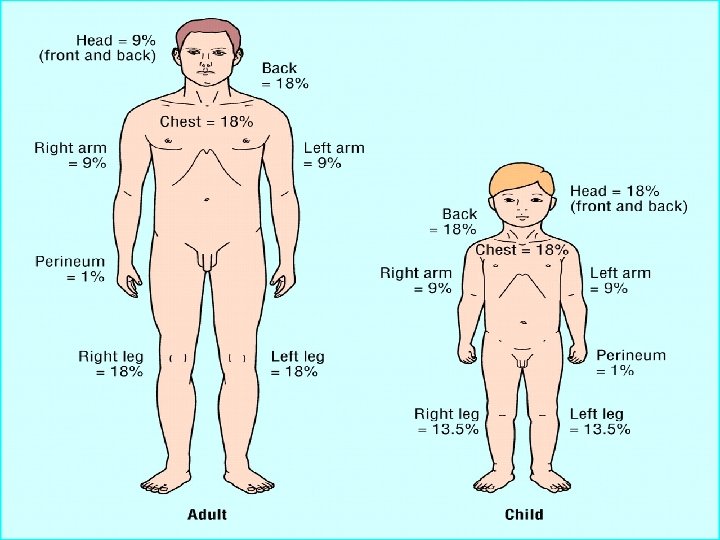
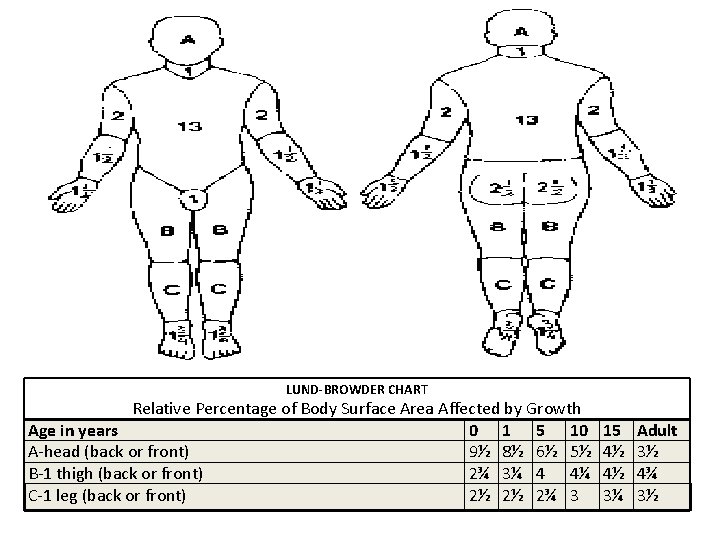
Third Burns (cont’d) space fluid shifts (cont’d) -- ◦ Phase II → fluid remobilization Begins approximately 48 hours after burn occurs Edema at burn site resolving Hypervolemia due to fluid shifting back into the intravascular compartment Metabolic acidosis due to accumulation of acids released from the injured tissue Respiratory acidosis due to inhalation injury that interferes with gas exchange Nursing assessment – ◦ Rule of Nines ◦ Lund-Browder Chart
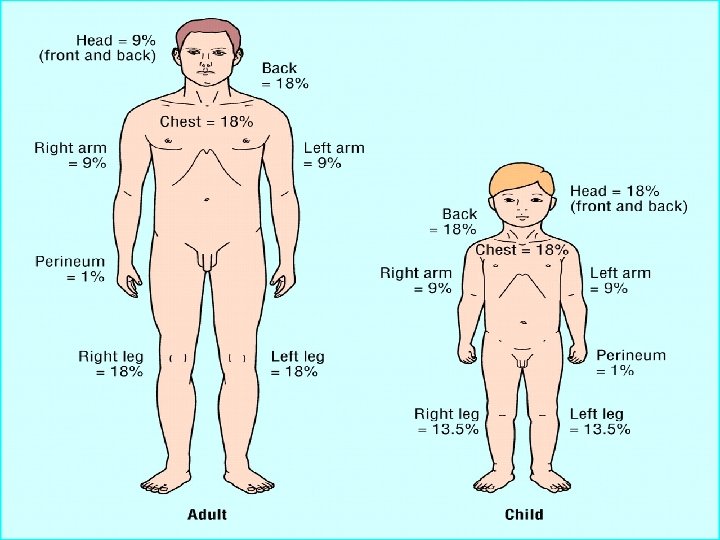
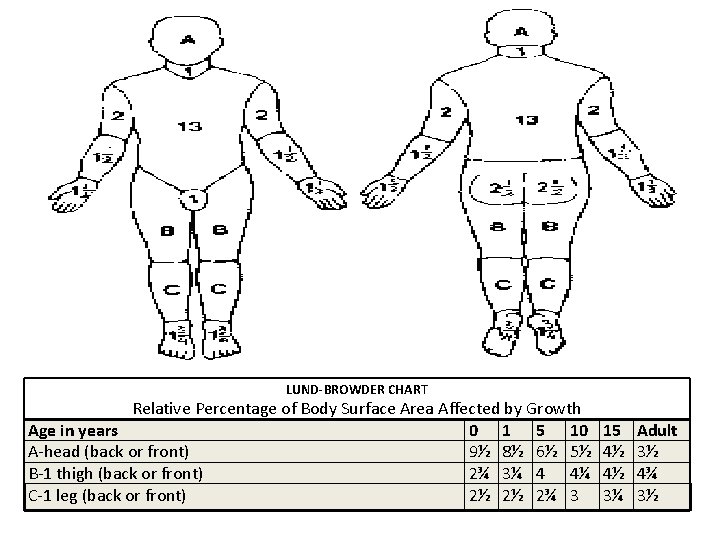
LUND-BROWDER CHART Relative Percentage of Body Surface Area Affected by Growth Age in years 0 1 5 10 A-head (back or front) 9½ 8½ 6½ 5½ B-1 thigh (back or front) 2¾ 3¼ 4 4¼ C-1 leg (back or front) 2½ 2½ 2¾ 3 15 4½ 4½ 3¼ Adult 3½ 4¾ 3½
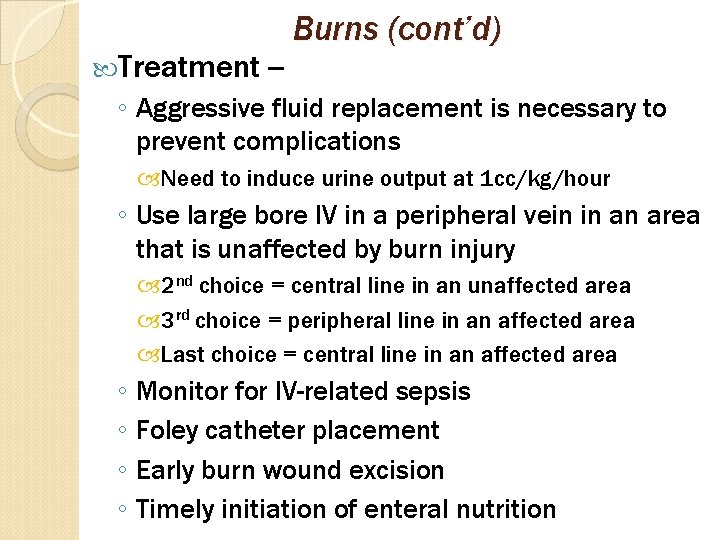
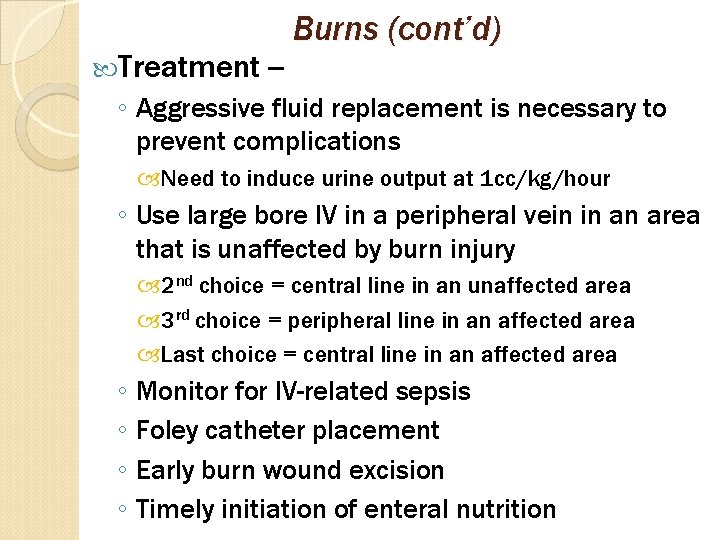
Treatment -- Burns (cont’d) ◦ Aggressive fluid replacement is necessary to prevent complications Need to induce urine output at 1 cc/kg/hour ◦ Use large bore IV in a peripheral vein in an area that is unaffected by burn injury 2 nd choice = central line in an unaffected area 3 rd choice = peripheral line in an affected area Last choice = central line in an affected area ◦ Monitor for IV-related sepsis ◦ Foley catheter placement ◦ Early burn wound excision ◦ Timely initiation of enteral nutrition
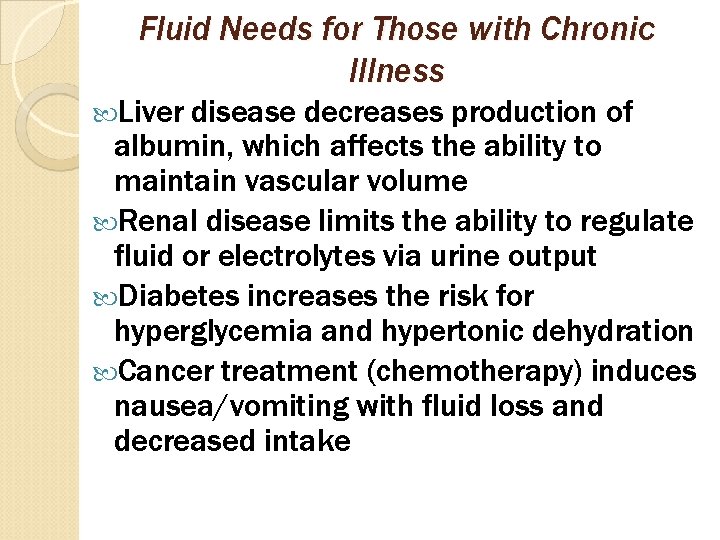
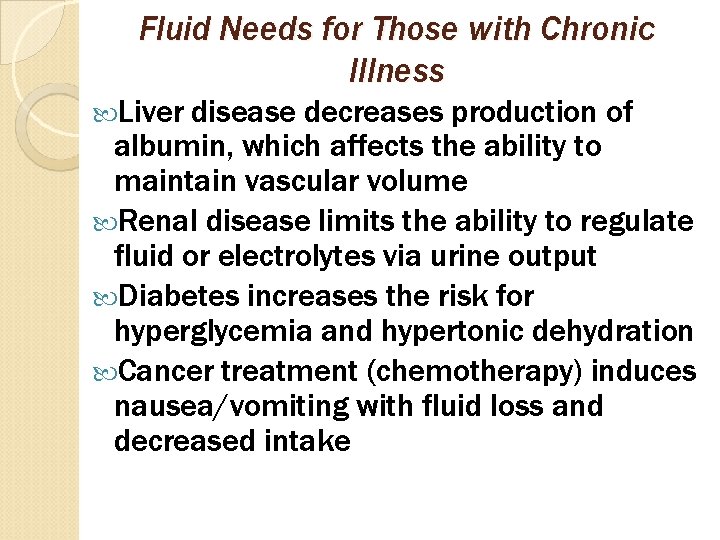
Fluid Needs for Those with Chronic Illness Liver disease decreases production of albumin, which affects the ability to maintain vascular volume Renal disease limits the ability to regulate fluid or electrolytes via urine output Diabetes increases the risk for hyperglycemia and hypertonic dehydration Cancer treatment (chemotherapy) induces nausea/vomiting with fluid loss and decreased intake
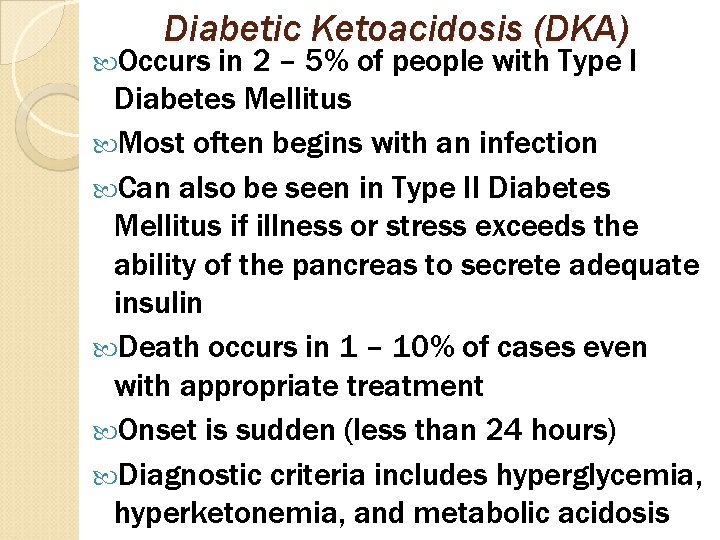
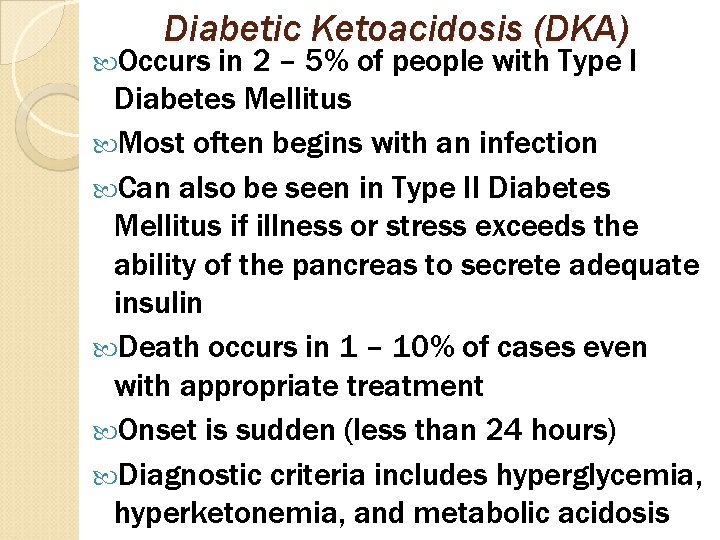
Diabetic Ketoacidosis (DKA) Occurs in 2 – 5% of people with Type I Diabetes Mellitus Most often begins with an infection Can also be seen in Type II Diabetes Mellitus if illness or stress exceeds the ability of the pancreas to secrete adequate insulin Death occurs in 1 – 10% of cases even with appropriate treatment Onset is sudden (less than 24 hours) Diagnostic criteria includes hyperglycemia, hyperketonemia, and metabolic acidosis
DKA (cont’d) Pathophysiology - Body is unable to utilize carbohydrates ◦ Not enough insulin to transport glucose into the cells ◦ Body resorts to utilizing fats for energy Results in ketones in the blood and urine ◦ Leads to acidosis Etiology – Inadequate medication/insulin Infection Change in diet, exercise Other stressors
DKA (cont’d) Clinical manifestations - Rapid, weak pulse Kussmaul’s respirations “Fruity” breath Nausea/vomiting, abdominal pain Dehydration Polyuria, polydipsia Normal/low temperature in the presence of infection Weight loss Dry skin Sunken eyes, soft eyeballs Lethargy, coma
DKA (cont’d) Lab findings – Serum glucose = >300 mg/d. L Serum ketones = positive Urine ketones = positive Serum p. H = <7. 35 Serum HCO 3 = <15 m. Eq/L Serum potassium = ↑ with acidosis, ↓ with dehydration BUN = >20 mg/d. L due to dehydration Creatinine + >1. 5 mg/d. L due to dehydration
DKA (cont’d) Emergency management – Establish a patent airway Administer oxygen and Na. HCO 3 if ↓ p. H Place IV with large bore catheter Administer NS per IV ◦ 1 L/hour for first 2 -3 hours to stabilize blood pressure and ensure adequate urine output IV fluid changed to D 5 ½ NS when serum glucose reaches 250 mg/d. L Urine output will decrease as osmotic diuresis effect of hyperglycemia is reduced Careful monitoring of potassium level
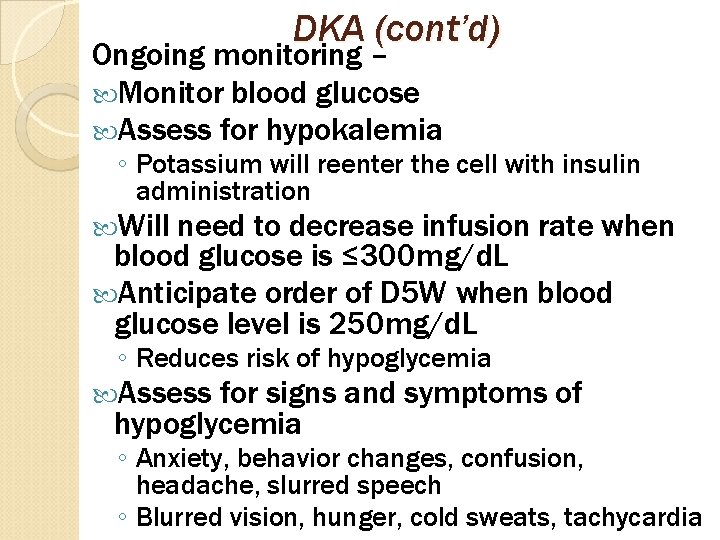
DKA (cont’d) Ongoing monitoring – Monitor blood glucose Assess for hypokalemia ◦ Potassium will reenter the cell with insulin administration Will need to decrease infusion rate when blood glucose is ≤ 300 mg/d. L Anticipate order of D 5 W when blood glucose level is 250 mg/d. L ◦ Reduces risk of hypoglycemia Assess for signs and symptoms of hypoglycemia ◦ Anxiety, behavior changes, confusion, headache, slurred speech ◦ Blurred vision, hunger, cold sweats, tachycardia
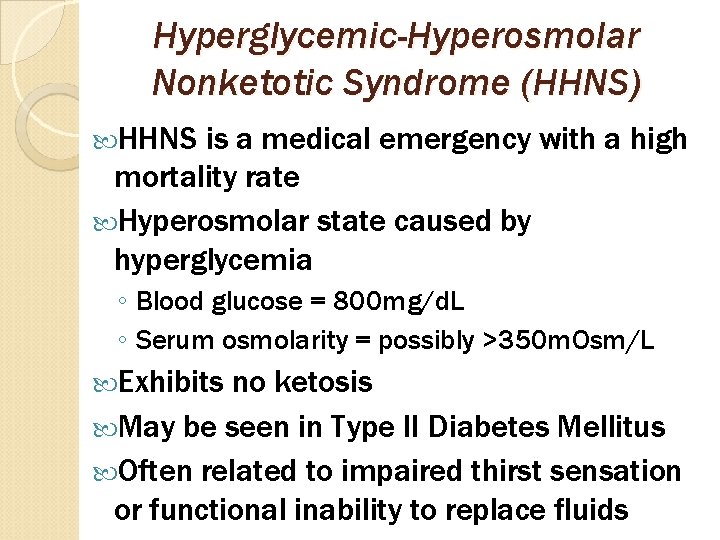
Hyperglycemic-Hyperosmolar Nonketotic Syndrome (HHNS) HHNS is a medical emergency with a high mortality rate Hyperosmolar state caused by hyperglycemia ◦ Blood glucose = 800 mg/d. L ◦ Serum osmolarity = possibly >350 m. Osm/L Exhibits no ketosis May be seen in Type II Diabetes Mellitus Often related to impaired thirst sensation or functional inability to replace fluids
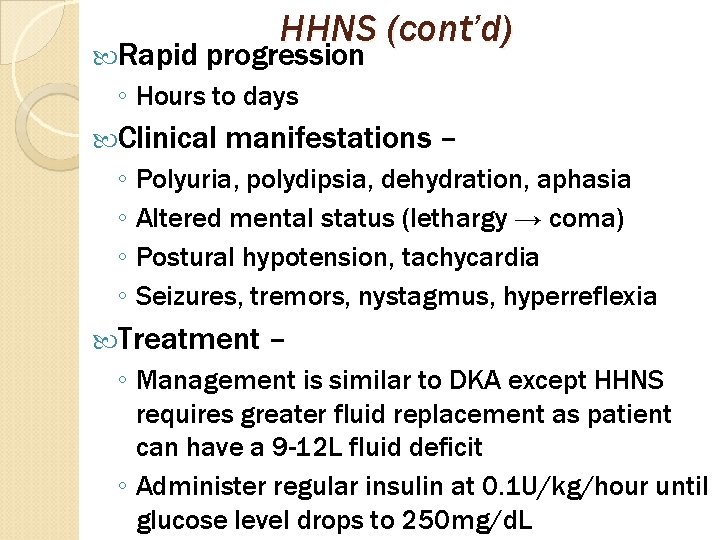
Rapid HHNS (cont’d) progression ◦ Hours to days Clinical manifestations – ◦ Polyuria, polydipsia, dehydration, aphasia ◦ Altered mental status (lethargy → coma) ◦ Postural hypotension, tachycardia ◦ Seizures, tremors, nystagmus, hyperreflexia Treatment – ◦ Management is similar to DKA except HHNS requires greater fluid replacement as patient can have a 9 -12 L fluid deficit ◦ Administer regular insulin at 0. 1 U/kg/hour until glucose level drops to 250 mg/d. L
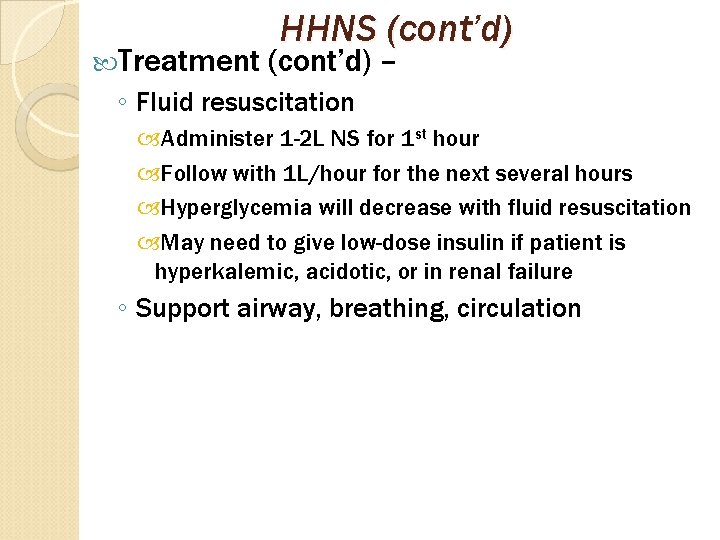
Treatment HHNS (cont’d) – ◦ Fluid resuscitation Administer 1 -2 L NS for 1 st hour Follow with 1 L/hour for the next several hours Hyperglycemia will decrease with fluid resuscitation May need to give low-dose insulin if patient is hyperkalemic, acidotic, or in renal failure ◦ Support airway, breathing, circulation
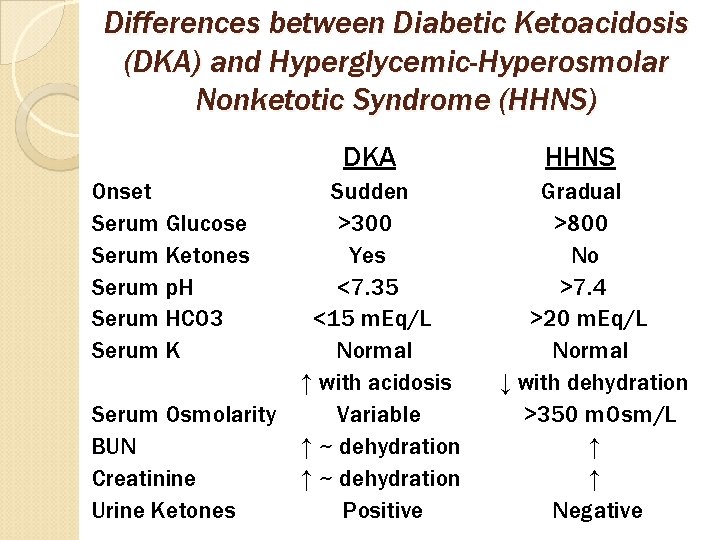
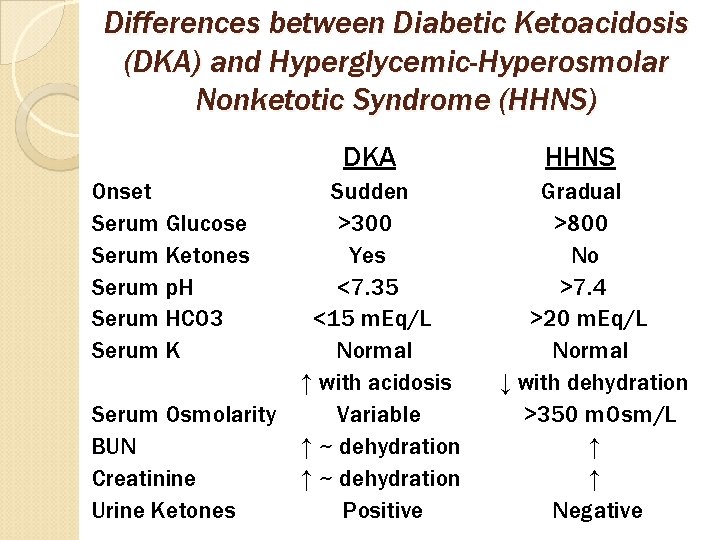
Differences between Diabetic Ketoacidosis (DKA) and Hyperglycemic-Hyperosmolar Nonketotic Syndrome (HHNS) DKA Onset Serum Glucose Serum Ketones Serum p. H Serum HCO 3 Serum K Serum Osmolarity BUN Creatinine Urine Ketones Sudden >300 Yes <7. 35 <15 m. Eq/L Normal ↑ with acidosis Variable ↑ ~ dehydration Positive HHNS Gradual >800 No >7. 4 >20 m. Eq/L Normal ↓ with dehydration >350 m. Osm/L ↑ ↑ Negative
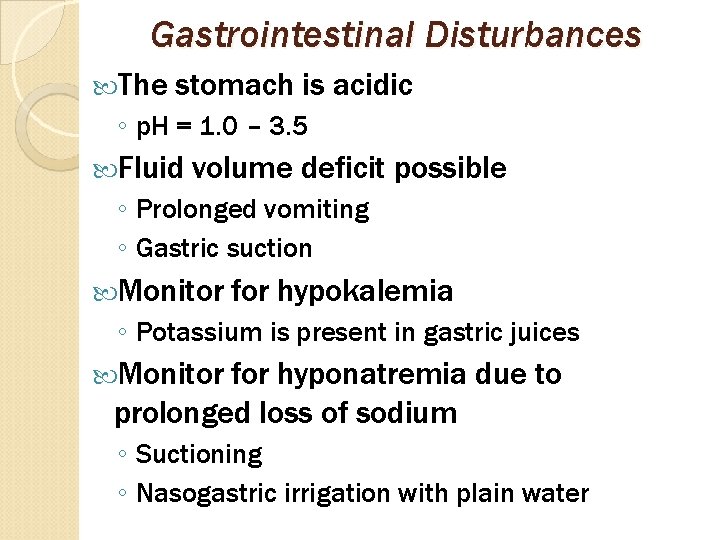
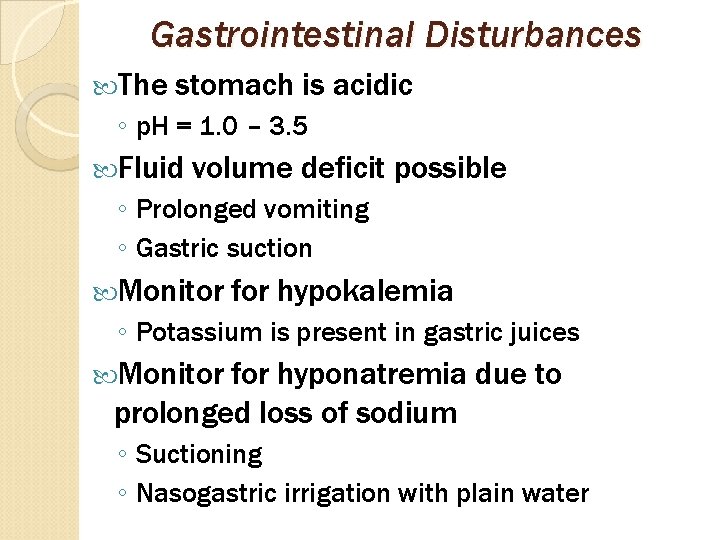
Gastrointestinal Disturbances The stomach is acidic ◦ p. H = 1. 0 – 3. 5 Fluid volume deficit possible ◦ Prolonged vomiting ◦ Gastric suction Monitor for hypokalemia ◦ Potassium is present in gastric juices Monitor for hyponatremia due to prolonged loss of sodium ◦ Suctioning ◦ Nasogastric irrigation with plain water
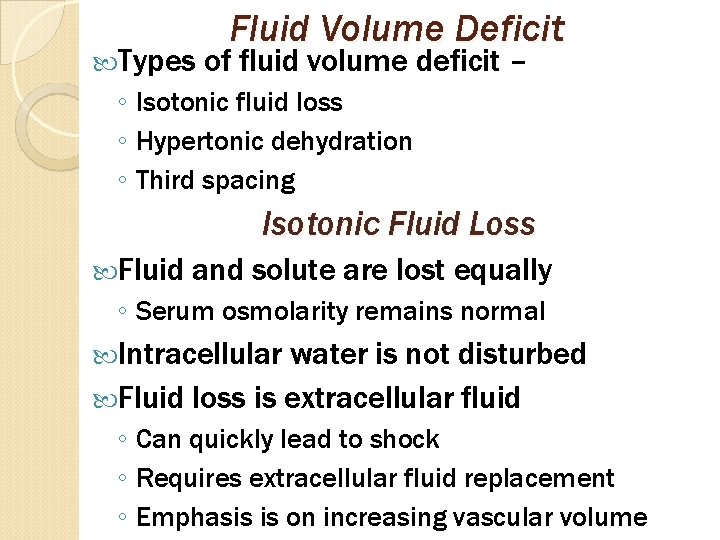
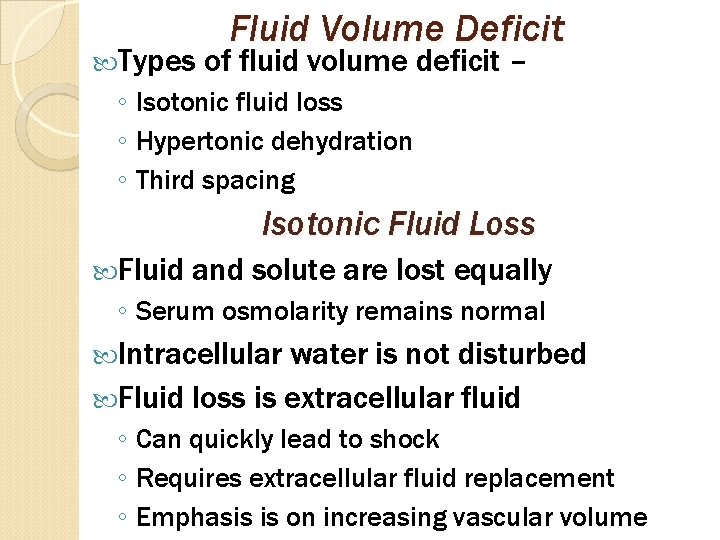
Types Fluid Volume Deficit of fluid volume deficit – ◦ Isotonic fluid loss ◦ Hypertonic dehydration ◦ Third spacing Isotonic Fluid Loss Fluid and solute are lost equally ◦ Serum osmolarity remains normal Intracellular water is not disturbed Fluid loss is extracellular fluid ◦ Can quickly lead to shock ◦ Requires extracellular fluid replacement ◦ Emphasis is on increasing vascular volume
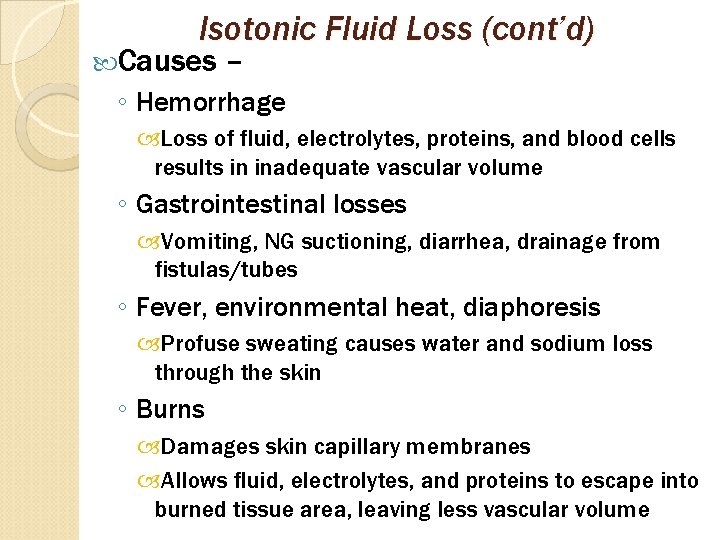
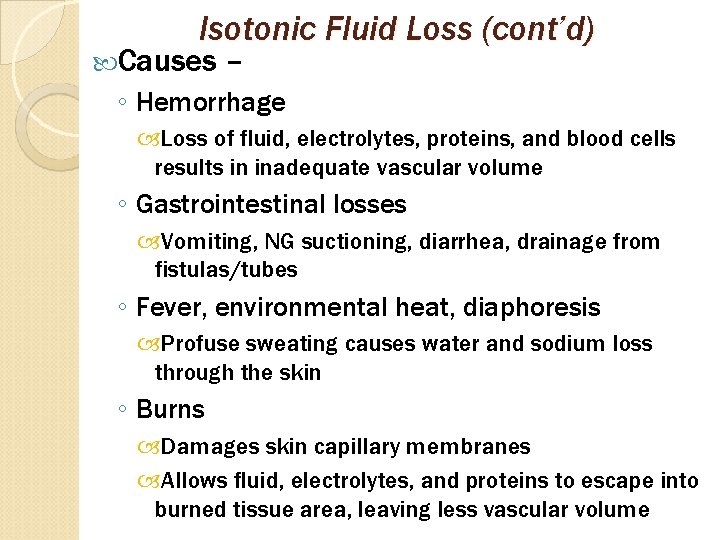
Isotonic Fluid Loss (cont’d) Causes – ◦ Hemorrhage Loss of fluid, electrolytes, proteins, and blood cells results in inadequate vascular volume ◦ Gastrointestinal losses Vomiting, NG suctioning, diarrhea, drainage from fistulas/tubes ◦ Fever, environmental heat, diaphoresis Profuse sweating causes water and sodium loss through the skin ◦ Burns Damages skin capillary membranes Allows fluid, electrolytes, and proteins to escape into burned tissue area, leaving less vascular volume
Isotonic Fluid Loss (cont’d) Causes (cont’d) – ◦ Diuretics can cause excessive loss of fluid and electrolytes ◦ Third spacing Fluid moves from the vascular space into extracellular spaces Treatment – ◦ Expand extracellular volume with isotonic IV fluids Increases circulating blood volume Restores renal perfusion ◦ Provide blood transfusion for hypovolemia caused by hemorrhage
Isotonic Fluid Loss (cont’d) Treatment (cont’d) – ◦ Administer 1– 2 L bolus of isotonic fluid for adults Infuse in 30 minutes or less ◦ Administer up to an additional 2– 3 L Improves urine output, blood pressure, heart rate, and mental status ◦ Infuse 20– 30 m. L/kg bolus of isotonic fluid for infants/young children to improve urine output, heart rate, respiratory rate, and mental status
Hypertonic Dehydration More water is lost than solute ◦ Creates a solute excess Primarily sodium ◦ Results in fluid volume deficit Solute water can also be gained in excess of ◦ Creates a similar imbalance ◦ Most common with sodium or glucose Serum osmolarity becomes elevated ◦ Results in hypertonic extracellular fluid ◦ Pulls fluids into the vessels from the cells by osmosis ◦ Causes cells to shrink and become dehydrated
Hypertonic Dehydration (cont’d) Causes – Inadequate fluid intake ◦ Inability to respond to thirst ◦ May occur due to age (infants or the elderly), immobility, nausea, anorexia, dysphagia, or being NPO without fluid replacement Severe or prolonged isotonic fluid losses ◦ Extracellular fluid becomes hypertonic and draws water from the cells Compensatory mechanisms become exhausted Conservation of water via the kidneys depleted Results in cellular dehydration ◦ May occur with nausea/vomiting, diarrhea Loss of more water than solute
Hypertonic Dehydration (cont’d) Causes (cont’d) – Watery diarrhea ◦ Loss of more water than electrolytes Diabetes insipidus ◦ Leads to massive, uncontrolled diuresis of dilute urine As much as 30 L/day Can quickly lead to shock and death ◦ Usually caused by a brain injury Damages/puts pressure on the hypothalamus or pituitary gland ◦ Need to administer parenteral vasopressin ◦ In a fluid volume deficit related to diabetes insipidus, urine will be pale, dilute, and high in volume
Hypertonic Dehydration (cont’d) Causes (cont’d) – Increased solute intake ◦ Excessive salt, sugar, or protein intake without a proportional intake of water ◦ Increases plasma osmolarity ◦ Water is pulled from the cells, leading to cellular dehydration ◦ Results in osmotic diuresis, which makes cellular dehydration worse Dangerous for patients with heart or kidney problems Conditions that lead to hypertonic dehydration – Highly concentrated enteral or parenteral feedings
Hypertonic Dehydration (cont’d) Conditions that lead to hypertonic dehydration (cont’d) – Improperly prepared infant formulas that are too concentrated Hyperglycemia and/or diabetic ketoacidosis ◦ Excessive glucose and ketones in the blood Increased sodium ingestion ◦ Ingestion of excessive amounts of seawater ◦ Taking salt water tablets Excessive use of osmotic diuretics
Hypertonic Dehydration (cont’d) Clinical manifestations – Thirst ◦ Early sign of dehydration ◦ Unreliable in the elderly and the very young Concentrated urine ◦ Dark in color ◦ High specific gravity (normal is 1. 010 – 1. 030) Low urine volume ◦ Normal output for adults is 30 m. L/hour Dry mucus membranes ◦ When assessing mucus membranes, remember that environmental conditions can also cause dry lips
Hypertonic Dehydration (cont’d) Clinical manifestations (cont’d) – Dry skin ◦ Decreased turgor ◦ Decreased elasticity ◦ Tenting Tissues stick together from interstitial fluid loss Unreliable in the elderly due to decreased elastin Test on sternum, forehead, inner thigh, top of hip instead of arms and legs Check infant skin over abdomen or inner thighs Dry tongue with longitudinal furrows Decreased tearing with dry conjunctiva Sunken eyes
Hypertonic Dehydration (cont’d) Clinical manifestations (cont’d) – Sunken or depressed fontanel in infants less than 1 year Flat neck veins and poor peripheral vein filling ◦ Jugular veins are nondistended even with the head of bed at <45 degrees ◦ When the hand is placed lower than the heart, the hand veins normally distend in 3 – 5 seconds Tachypnea

Hypertonic Dehydration (cont’d) Clinical manifestations (cont’d) – Low grade fever ◦ May be higher in severe dehydration Mental status changes ◦ Often the first sign noticed in the elderly ◦ Irritability, restlessness ◦ Drowsiness, lethargy ◦ Confusion Decreased cardiac output ◦ Tachycardia (early sign in infants) ◦ Weak, thready pulse ◦ Cool extremities with delayed capillary refill
Hypertonic Dehydration (cont’d) Clinical manifestations (cont’d) – Postural hypotension when rising from lying to standing position ◦ Pulse increased by greater than 10 -15 bpm ◦ Fall in systolic blood pressure by greater than 10 -15 mm. Hg ◦ The greater the fall in blood pressure or rise in heart rate, the greater the fluid volume deficit ◦ Weakness, dizziness, light-headedness, syncope Frank hypotension ◦ Exists even when lying down ◦ Late sign in infants and young children
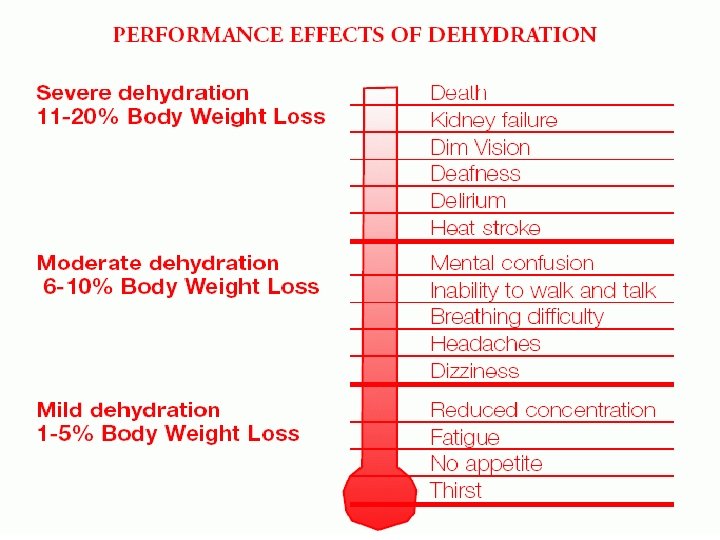
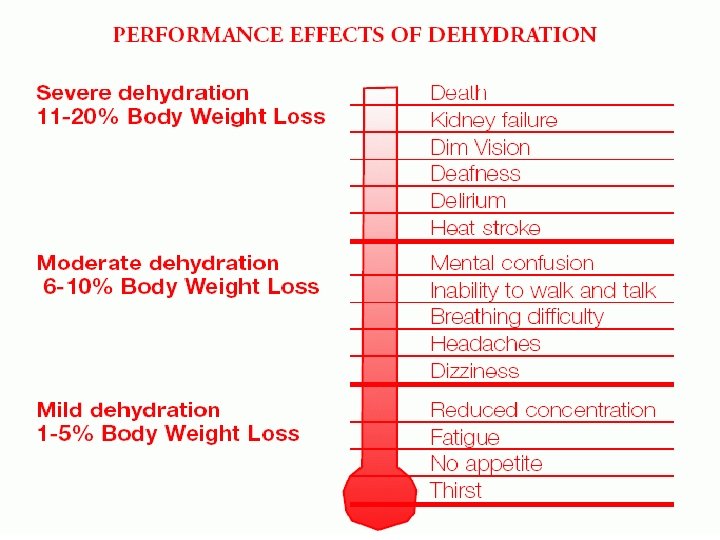
Hypertonic Dehydration (cont’d) Clinical manifestations (cont’d) – Acute weight loss ◦ 2% body weight loss Mild fluid deficit (thirst) 1 – 2 L fluid loss in an adult ◦ 5% body weight loss Moderate fluid deficit Signs and symptoms of dehydration appear 3 – 5 L fluid loss in an adult ◦ 8% body weight loss Severe fluid deficit Frank hypotension 5 – 10 L fluid loss in an adult ◦ >15% body weight loss Fatal >10 L fluid loss in an adult
Hypertonic Dehydration (cont’d) Parenteral therapy – Hypovolemia and impending shock ◦ Isotonic fluids administered for adequate circulation and renal perfusion ◦ Hypotonic solutions administered to correct cellular dehydration Given slowly to prevent cerebral edema due to sensitivity of brain cells to hypotonicity Hypervolemia ◦ Resulting from excessive sodium intake ◦ Administer a diuretic with hypotonic fluid to provide free water to cells while preventing vascular volume overload
Hypertonic Dehydration (cont’d) Nursing interventions - Monitor vital signs for changes in heart rate, blood pressure, and respiratory rate Assess mental status ◦ Lack of improvement (or worsening) could indicate the infusion of hypotonic fluids is too rapid Monitor urine output and concentration Monitor IV rate ◦ Watch for fluid volume overload Monitor I&O Monitor weight daily
Hypertonic Dehydration (cont’d) Lab findings – Hemoconcentration ◦ Plasma becomes concentrated to the red blood cells and urea particles ◦ BUN would be high High urine specific gravity (>1. 030) ◦ Kidneys conserve water while continuing to excrete solute ◦ In cases of diabetes insipidus, specific gravity would be low (<1. 010) Increased plasma concentration ◦ Elevated serum osmolality (>300 m. Osm/kg) ◦ Elevated serum potassium (>150 m. Eq/L) ◦ Elevated serum glucose (>120 mg/d. L)
Third Spacing spaces are extracellular body spaces where fluid can accumulate This accumulated fluid is useless to the body ◦ Unavailable for use as reserve fluid ◦ Unable to transport nutrients Common locations for third space fluid to accumulate – ◦ Tissue spaces (edema) ◦ Abdomen (ascites) ◦ Pleural spaces (pleural effusion) ◦ Pericardial space (pericardial effusion)
Third Spacing (cont’d) Causes – Injury or inflammation ◦ Increased capillary permeability allows fluid, electrolytes, and proteins to leak from the vessels Massive trauma Crush injuries Burns Sepsis Cancer Intestinal obstruction Abdominal surgery
Third Spacing (cont’d) Causes (cont’d) – Malnutrition or liver dysfunction ◦ Prevents liver from producing albumin, which lowers capillary oncotic pressure Starvation Cirrhosis Chronic alcoholism High vascular hydrostatic pressure ◦ Pushes abnormal volumes of fluid from the vessels Heart failure Renal failure Other vascular fluid overload
Third Spacing (cont’d) Treatment – Osmotic diuretics are used to mobilize some of the fluid back into the blood vessels for elimination by the kidneys
Types Fluid Volume Excess of fluid volume excess – ◦ Isotonic fluid excess Hypervolemia Edema ◦ Hypotonic fluid excess Water intoxication Risk factors that predispose individuals to fluid volume excess -◦ Individuals of certain age Elderly (due to ↓ heart and kidney function) Children < age 2 (due to immature kidneys) Children ages 2 – 12 years (due to unstable regulatory responses)
Risk Fluid Volume Excess (cont’d) factors (cont’d) – ◦ Acute illness Stimulates the stress response, which releases cortisol, ADH, and aldosterone → promotes water and sodium retention ◦ Chronic illness Cardiovascular disease causes sodium and water retention Reduces the pumping strength of the heart Reduces blood flow to the kidneys Renal disease leads to abnormal retention of water, sodium, and potassium ◦ Medications Long-term glucocorticoid therapy Drugs that act to retain sodium and fluids
Risk Fluid Volume Excess (cont’d) factors (cont’d) – ◦ Patients receiving IV fluids Lab findings – Decreased hematocrit and BUN due to hemodilution ◦ Returns to normal once excess fluid is removed Serum osmolarity is low Serum sodium is very low Chest x-ray may show pleural effusion Low PO 2 and PCO 2 Decreased p. H due to respiratory acidosis (results from pulmonary edema)
Fluid Volume Excess (cont’d) Clinical manifestations – ◦ Peripheral edema Legs, ankles, feet, and hands in ambulatory individuals Sacrum and back in bedridden clients ◦ Edema in the legs and feet Indicates local obstruction of veins Edematous skin is often tight and shiny due to decreased circulation in swollen tissue ◦ Puffiness in the face and around the eyes (periorbital edema) Associated with heart or kidney problems ◦ Tense or bulging fontanels in children less than 1 year of age
Fluid Volume Excess (cont’d) Clinical manifestations (cont’d) – ◦ Pitting edema ◦ High central venous pressure Distended neck veins when HOB is elevated Delayed hand vein emptying when hand is raised above the heart for 3 – 5 seconds ◦ Venous congestion Hepatomegaly Splenomegaly ◦ Decreased urine output if cardiac or renal function is impaired ◦ Weight gain of 3 lbs over 2 – 5 days ◦ Full/bounding pulse, warm extremities
Fluid Volume Excess (cont’d) Treatment – ◦ Restrict fluid intake to 1, 000 – 1, 500 m. L/day ◦ Maintain sodium restriction ◦ Maintain IV access ◦ Administer diuretics ◦ Increase protein intake to increase capillary oncotic pressure to pull fluid out of the tissues ◦ Monitor respiratory status ◦ Monitor venous engorgement ◦ Monitor I&O, daily weight ◦ Assess for edema ◦ Assess neurologic status ◦ Monitor labs (BUN, HCT, sodium, ABGs, K+)
Isotonic Fluid Excess Hypervolemia = gain of fluid and solute (sodium) in proportional amounts ◦ Overall gain in the extracellular fluid without a change in serum osmolarity Edema = excess tissue (interstitial) fluid throughout the body or specific to a body tissue or organ Causes -◦ Renal failure Decreased excretion of water and sodium ◦ Rapid infusion of isotonic fluid Exceeds the ability to compensate by the heart and kidneys
Isotonic Fluid Excess (cont’d) Causes (cont’d) – ◦ Heart failure Venous congestion Decreased renal blood flow leading to decreased renal excretion of fluid and sodium ◦ High corticosteroid levels, which results in sodium and water retention Therapy Stress response ◦ High aldosterone levels, which results in sodium and water retention Stress response Adrenal dysfunction
Gain Hypotonic Fluid Excess of more fluid than solute (sodium) ◦ Creates fluid volume excess ◦ Results in a deficit of sodium ◦ Serum osmolarity decreases Causes hypotonic extracellular fluid that gets pulled into the cells Cells swell, and cerebral edema occurs Causes – ◦ Frequent use of plain water enemas ◦ Multiple nasogastric tube or bladder irrigations with plain water ◦ Infusing hypotonic solutions too rapidly ◦ Use of improperly prepared infant formula
Hypotonic Fluid Excess (cont’d) Causes (cont’d) – ◦ Increased release of ADH SIADH causes the kidneys to retain large amounts of water without retaining sodium Creates hypotonic extracellular fluid, which is drawn into the cells Highly concentrated urine with low urine volume Stress Surgery, anesthesia Opioid analgesics, pain Tumors of the lung or brain ◦ Psychogenic polydipsia Compulsive drinking of excessive amounts of water associated with psychiatric disorders (i. e. some types of schizophrenia)

Hypotonic Fluid Excess (cont’d) Causes (cont’d) – ◦ Severe or prolonged isotonic fluid volume excess Compensated by increased urine output Clients with heart failure, renal failure, and diabetes are sensitive to excess fluid administration Capillary Fluid Movement Hydrostatic pressure = the pushing force of a fluid against the walls of the space it occupies ◦ Generated by the heart’s pumping action ◦ Varies within the vascular system
Capillary Fluid Movement (cont’d) Oncotic pressure = the pulling force exerted by colloids in a solution ◦ Albumin is a pulling force for water Maintains normal serum oncotic pressure Maintains adequate vascular fluid volume Causes of low capillary oncotic pressure -◦ Injury or inflammation (trauma, burns, sepsis) Increases capillary permeability Allows fluids and proteins to leak from the vessels ◦ Malnutrition or liver dysfunction (starvation, cirrhosis, chronic alcoholism) Prevents liver from producing albumin ↓ capillary oncotic pressure; fluid remains in vessels
Capillary Fluid Movement (cont’d) Starling’s Law ◦ Filtration = movement of fluid into or out of the capillary, determined by the pushing and pulling forces ◦ At the arterial end of the capillary, capillary hydrostatic pressure exceeds capillary oncotic pressure Fluid movement is from the capillary into the tissue Carries nutrients to the tissues ◦ At the venous end of the capillary, capillary hydrostatic pressure is less than capillary oncotic pressure Fluid movement is into the capillary from the tissue Carries wastes away from the tissues
Edema = soft tissue swelling due to expansion of the interstitial volume ◦ Can be localized or generalized ◦ Fluid moves from the capillaries into the interstitial space and back again, carrying wastes with it Increased capillary hydrostatic pressure ◦ Forces more fluid out of the arterial end of the capillary ◦ Draws less fluid back into the venous end of the capillary ◦ Results in edema as fluid accumulates in the tissues
Decreased Edema (cont’d) capillary oncotic pressure ◦ Disrupts normal movement of fluid into and out of the capillaries ◦ Weaker pulling pressure allows more fluid to be pushed out of the arterial end of the capillary ◦ Unable to draw adequate amount of fluid back into the venous end of the capillary ◦ Results in edema Causes ◦ Hypertension ◦ Hypervolemia, lymphedema ◦ Renal failure
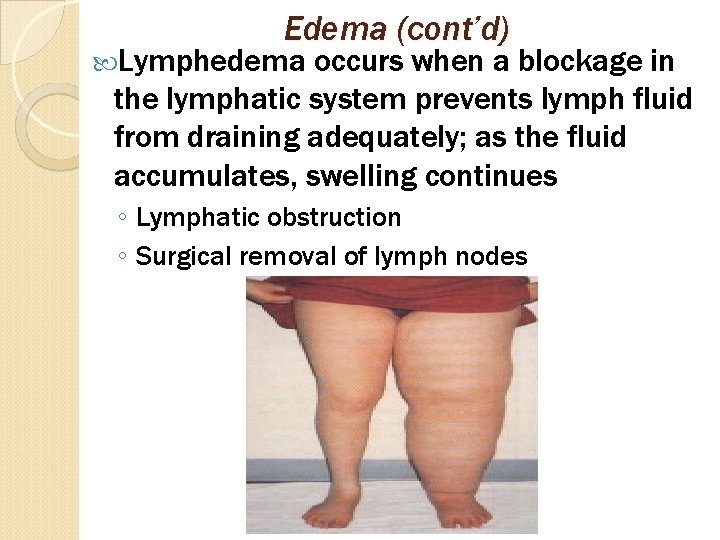
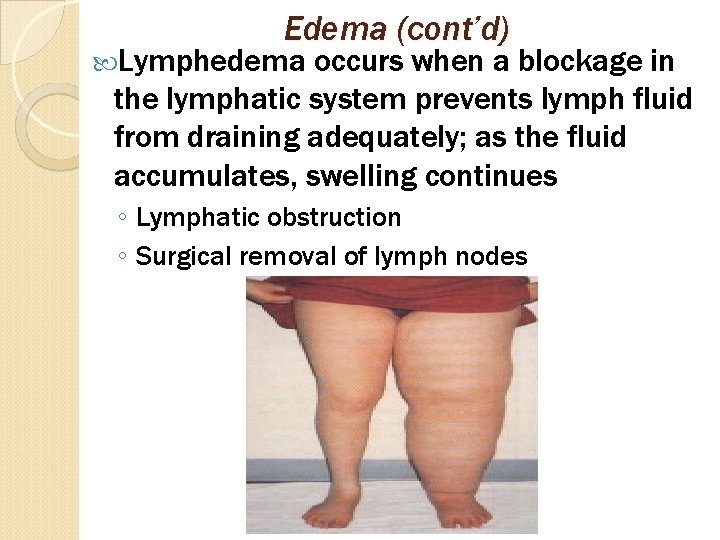
Edema (cont’d) Lymphedema occurs when a blockage in the lymphatic system prevents lymph fluid from draining adequately; as the fluid accumulates, swelling continues ◦ Lymphatic obstruction ◦ Surgical removal of lymph nodes
Renal Edema (cont’d) failure causes decreased renal perfusion leading to excess aldosterone in the blood ◦ Causes water retention that elevates the blood pressure ◦ Increases hydrostatic pressure within the capillaries, which forces more fluid into the tissues ◦ Results in edema
Congestive Heart Failure (CHF) Inability of the heart to pump enough blood to meet the metabolic needs of the tissues of the body Associated with hypertension, myocardial infarction (MI), valvular disease Left ventricular failure seen with pulmonary edema Right ventricular failure seen with edema in the lower extremities Failure tends to occur in both ventricles, so client will present with both peripheral and pulmonary edema
Fluid CHF (cont’d) and electrolyte imbalances seen with CHF – ◦ Fluid volume excess Decreased renal blood flow associated with decreased cardiac output ◦ Hyponatremia ADH causes greater retention of water, diluting serum sodium level ◦ Hypokalemia Caused by diuretics, vomiting, and diarrhea ◦ Respiratory acidosis Pulmonary congestion interferes with carbon dioxide elimination from the lungs ◦ Metabolic acidosis Anoxic tissue releases lactic acid
Fluid CHF (cont’d) and electrolyte imbalances (cont’d) -- ◦ Edema Shift of intravascular fluid into interstitial tissue due to increase in hydrostatic pressure from excessive venous blood volume Signs and symptoms – ◦ Fatigue due to decreased cardiac output ◦ Dyspnea Cardiac output is inadequate to provide for body’s oxygen requirements Paroxysmal nocturnal dyspnea occurs when client is in a recumbent position because edema fluid from the extremities returns to the bloodstream, increasing cardiac preload ◦ Decreased urine output due to secretion of aldosterone and ADH
Signs CHF (cont’d) and symptoms (cont’d) – ◦ Cough ◦ Tachycardia ◦ Peripheral edema ◦ Pulmonary edema Increased pulmonary venous pressure forces serum and blood cells in the alveoli Severe dyspnea, coughing, pink frothy sputum ◦ Distention of the peripheral veins from elevated venous pressure Visible in the hands, face, and neck ◦ Orthopnea Increased interstitial edema increases the work of breathing Upright position fosters air exchange
Signs CHF (cont’d) and symptoms (cont’d) – ◦ Nocturia Oxygen demand reduced at night, decreasing renal constriction and increasing glomerular filtration rate ◦ Cardiomegaly Hypertrophy of the myocardium that helps to maintain stroke volume Nursing interventions – ◦ Lessen cardiac preload and afterload Give diuretics per IV ◦ Administer ACE inhibitors (arterial vasodilators) ◦ Restrict fluids ◦ Monitor I&O
Pulmonary Edema Pulmonary edema is a medical emergency ◦ Place patient in high Fowler’s position ◦ Administer oxygen ◦ Administer IV morphine Reduces preload through peripheral dilation Reduces afterload through decreased blood pressure Reduces anxiety Signs and symptoms – ◦ Tachypnea, dyspnea, labored breathing, cough, moist rales, decreased oxygen saturation ◦ Third spacing as fluids are forced out of the vessels and into spaces that normally do not contain much fluid (ascites, pleural effusion) ◦ Acute, rapid weight gain
Basic Classifications of Infusates Crystalloids 2. Colloids 3. Hydrating solutions 4. Hypertonic-hyperosmolar preparations 5. Blood or blood components Crystalloids - Capable of crystallization Forms a solution Can diffuse through membranes Includes electrolyte solutions that may be isotonic, hypotonic, and hypertonic 1.
Classifications of Infusates (cont’d) Colloids – Cannot form a solution (does not dissolve) Cloudy in appearance Raises osmotic pressure Plasma or volume expander Types of colloids -◦ Albumin ◦ Dextran ◦ Plasmanate ◦ Hetastarch ◦ Artificial blood substitute
Classifications of Infusates (cont’d) Hydrating Solutions (cont’d) – Supplements calorie intake Supplies nutrients Provides free water ◦ Maintenance ◦ Rehydration Promotes effective renal output Frequently used hydrating solutions ◦ Dextrose 2½% in 0. 45% saline ◦ Dextrose 5% in water (D 5 W) ◦ Dextrose 5% in 0. 45% saline ◦ Dextrose 5% in 0. 2% saline ◦ Sodium chloride 0. 45%

Classifications of Infusates (cont’d) Hydrating Solutions (cont’d) – Electrolytes in IV solutions are measured in m. Eq/L Milliequivalents measure how many chemically active ions are present in a solution Sodium chloride contains 154 m. Eq/L of sodium and 154 m. Eq/L of chloride, which equals 308 m. Osm/L 0. 45% Na. Cl (1/2 strength saline) has 77 m. Eq/L of sodium and 77 m. Eq/L of chloride, which equals 154 m. Osm/L
Classifications of Infusates (cont’d) Dextrose Solutions – Manufactured as a percentage of the concentration in water or sodium chloride Expressed as the number of grams of solute per 100 m. L of solvent 5% dextrose in water solution contains 5 g of dextrose in 100 m. L of water
Isotonic Infusions D 5 W ◦ Osmolarity = 252. 52 m. Osm/L ◦ Best solution for hydration Isotonic in bag Hypotonic once dextrose metabolized ◦ Does not contain electrolytes ◦ Not given to patient with increased intracranial pressure ◦ ADH secretion is increased as a stress response to surgery Use cautiously in early post-operative period to prevent water intoxication ◦ Hypokalemia can occur due to cellular use of glucose Potassium shifts from the extracellular fluid to the intracellular fluid
D 5 W Isotonic Infusions (cont’d) -- ◦ Use cautiously in patients with signs of fluid overload and congestive heart failure Dehydration with rapid infusion due to osmotic diuresis ◦ May alter insulin/oral hypoglycemic needs in diabetics Contraindicated in diabetic coma ◦ Should not be used in patients with allergies to corn and corn products ◦ Medication incompatibilities – Ampicillin Diazepam Erythromycin Fat emulsions Phenytoin sodium Procainamide Sodium bicarbonate Warfarin sodium Whole blood Vitamin B 12
0. 9% Isotonic Infusions (cont’d) normal saline (NS) ◦ Osmolarity = 308 m. Osm/L ◦ Only infusate compatible with a blood infusion ◦ Maintains patency of heparin locks ◦ Used as a diluent for medications ◦ Replaces extracellular fluid losses by expanding intravascular space ◦ Corrects hyponatremia ◦ Used to treat hypovolemia ◦ Can cause intravascular overload Monitor I&O ◦ Can cause hypokalemia Saline promotes potassium excretion
Isotonic Infusions (cont’d) NS (cont’d) – ◦ Can cause hypernatremia Sodium may be retained in intraoperative and early post-operative situations Excessive sodium retention when used with glucocorticoids Contraindicated in patients with edema and sodium retention ◦ Does not provide free water or calories ◦ Used with caution in certain patients Decreased renal function Altered circulatory function Elderly
Isotonic Infusions (cont’d) NS (cont’d) – ◦ Medication incompatibilities – Amphotericin B (antifungal) Chlordiazepoxide HCl (Librium) Diazepam Fat emulsions Levarterenol (norepinephrine) Mannitol Methylprednisolone sodium succinate (Solu-Medrol) Phenytoin sodium
IV Fluid Reminders The body is in a state of homeostasis when the serum osmolarity is the same as other body fluids ◦ Approximately 280 – 300 m. Osm/L To change the osmolarity, glucose and/or electrolytes must be added to the solvent ◦ Increases the total number of particles in the solution ◦ Increases osmotic pressure