Lowgradient Lowflow aortic stenosis with low LV ejection
- Slides: 39
Low-gradient/ Low-flow aortic stenosis with low LV ejection fraction Jean-Luc MONIN, MD, Ph. D. Henri Mondor University Hospital, Créteil, FRANCE
Disclosures related to this presentation: None 2
Low-gradient/ Low-flow AS with low LV ejection fraction DEFINITION: • Valve area < 1. 0 cm² (< 0. 6 cm²/m²) • WITH LV systolic dysfunction (LVEF< 40%) • AND Transaortic MPG < 40 mm Hg ESC/ EACTS Guidelines. Eur Heart J. 2012; 33: 2451 -96 AHA/ACC Guidelines on VHD. Circulation. 2014; 129: e 521 -e 643 3
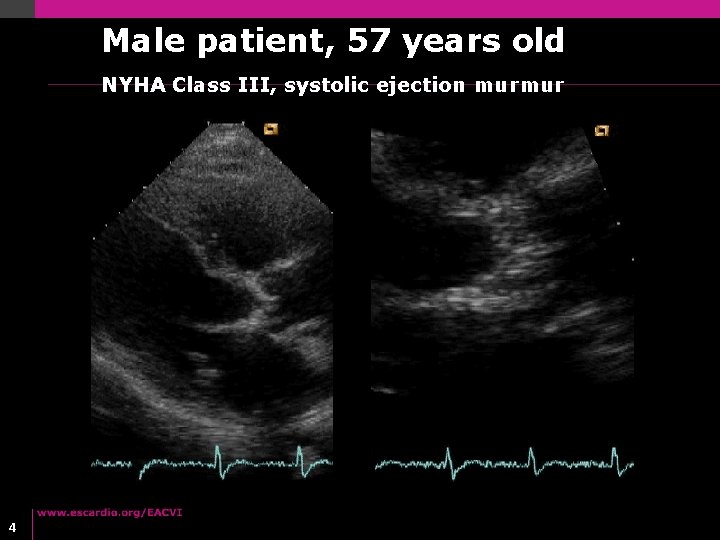
Male patient, 57 years old NYHA Class III, systolic ejection murmur 4
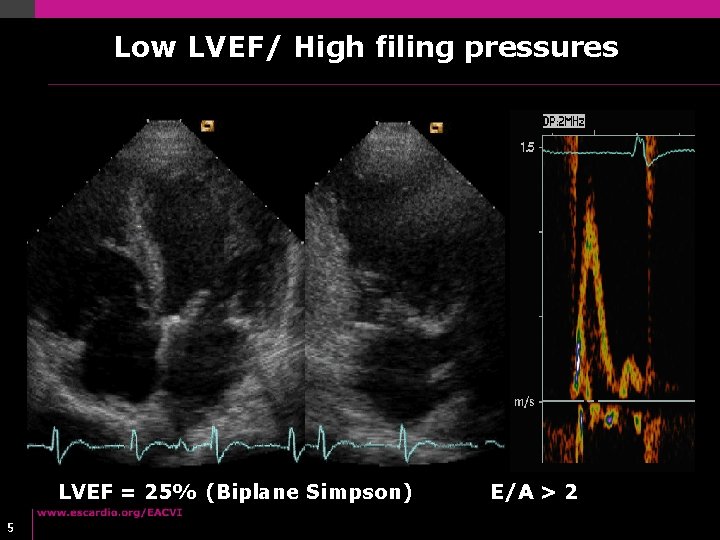
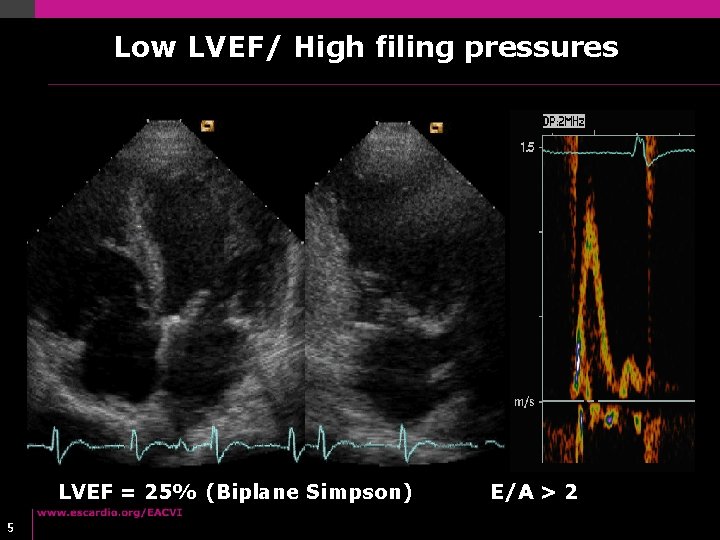
Low LVEF/ High filing pressures LVEF = 25% (Biplane Simpson) 5 E/A > 2
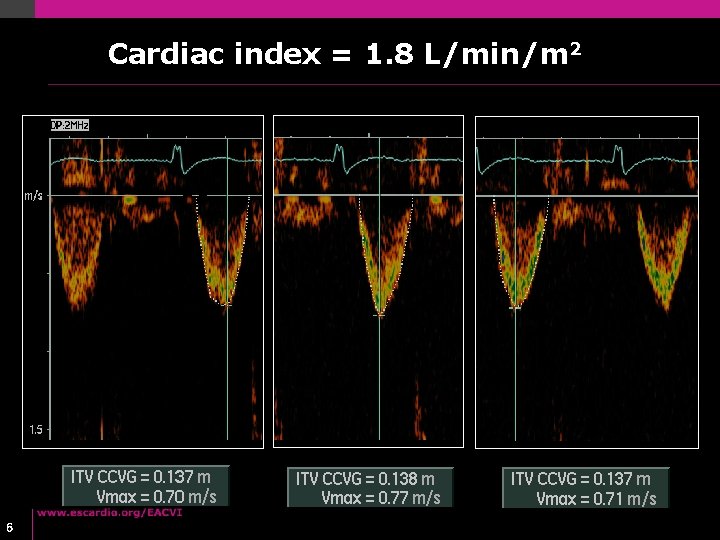
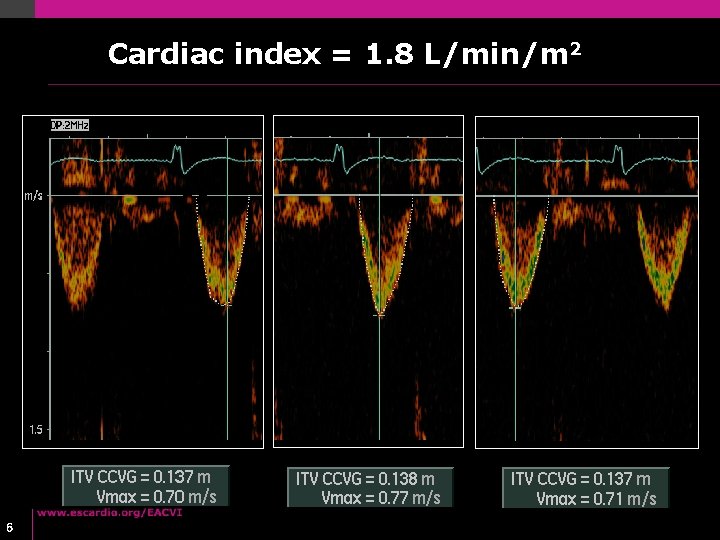
Cardiac index = 1. 8 L/min/m 2 6
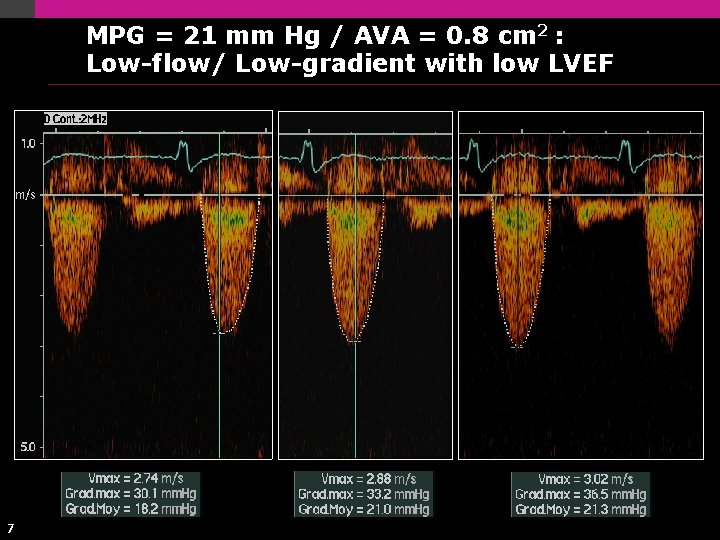
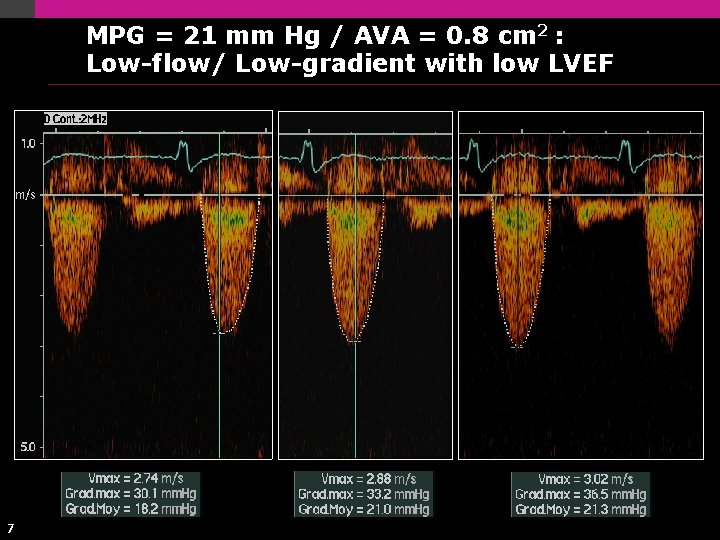
MPG = 21 mm Hg / AVA = 0. 8 cm 2 : Low-flow/ Low-gradient with low LVEF 7
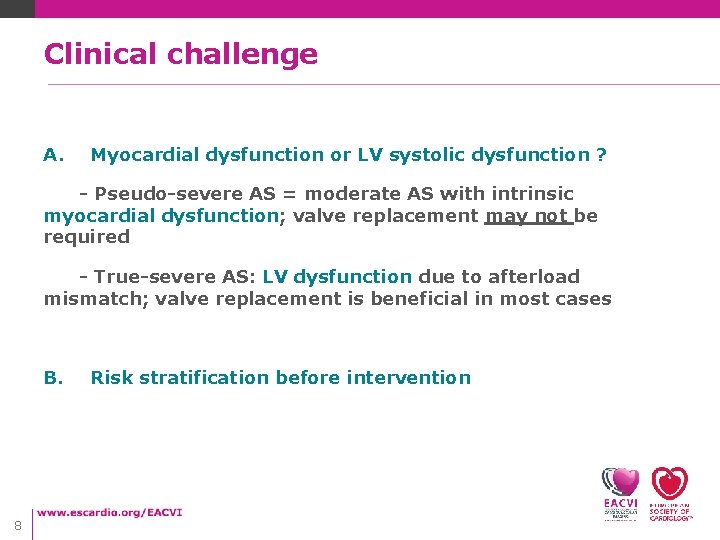
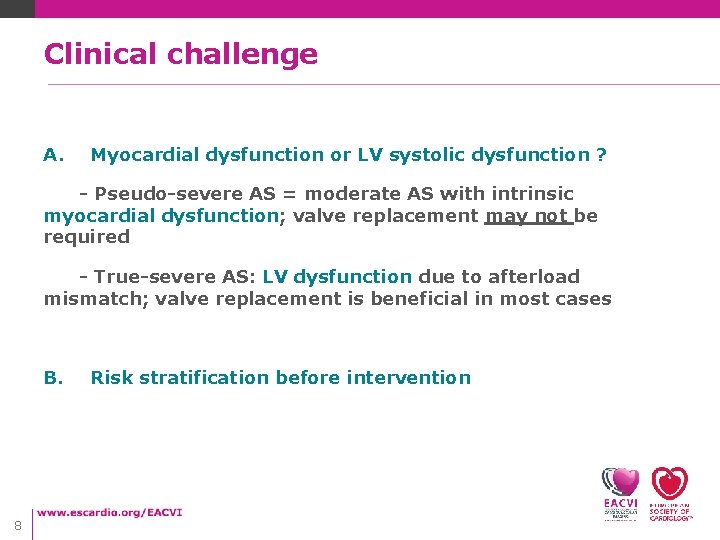
Clinical challenge A. Myocardial dysfunction or LV systolic dysfunction ? - Pseudo-severe AS = moderate AS with intrinsic myocardial dysfunction; valve replacement may not be required - True-severe AS: LV dysfunction due to afterload mismatch; valve replacement is beneficial in most cases B. 8 Risk stratification before intervention
Low-gradient/ Low-flow AS with low LV ejection fraction • How to differentiate True-severe from pseudo-severe AS ? • Outcome implications regarding pseudo-severe AS • Current role of risk stratification 9
Low-gradient/ Low-flow AS with low LV ejection fraction • How to differentiate True-severe from pseudo-severe AS ? • Outcome implications regarding pseudo-severe AS • Current role of risk stratification 10
de. Filippi et al. Am J Cardiol. 1995; 75: 191 -4 11
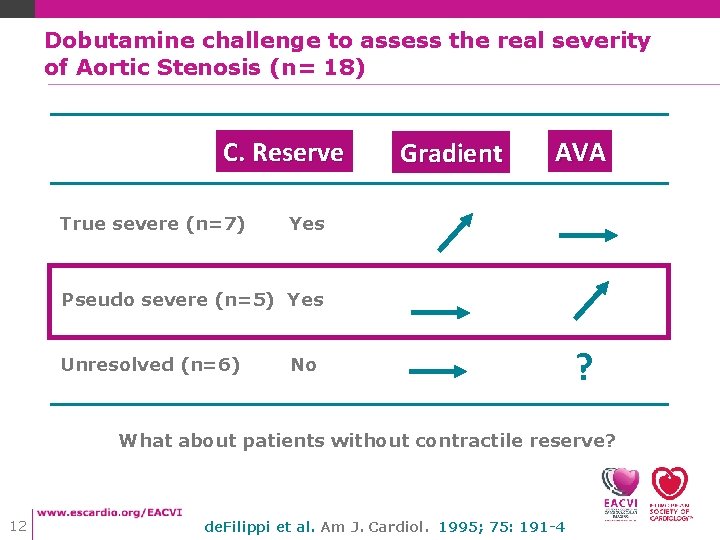
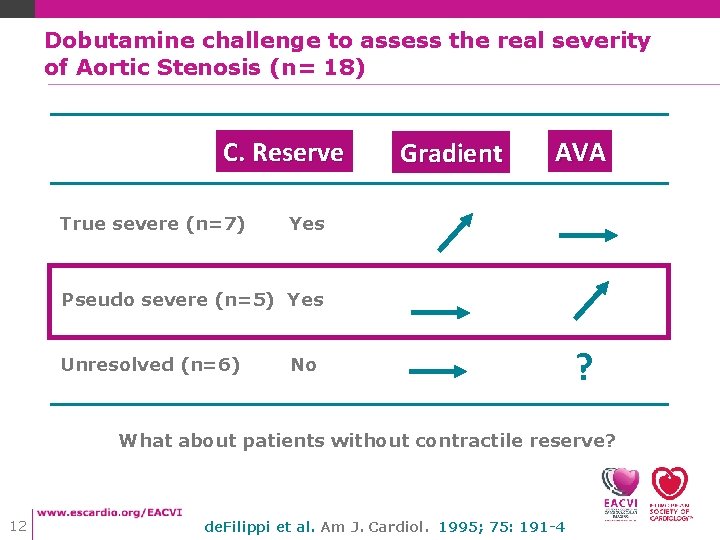
Dobutamine challenge to assess the real severity of Aortic Stenosis (n= 18) C. Reserve True severe (n=7) Gradient AVA Yes Pseudo severe (n=5) Yes Unresolved (n=6) No ? What about patients without contractile reserve? 12 de. Filippi et al. Am J. Cardiol. 1995; 75: 191 -4
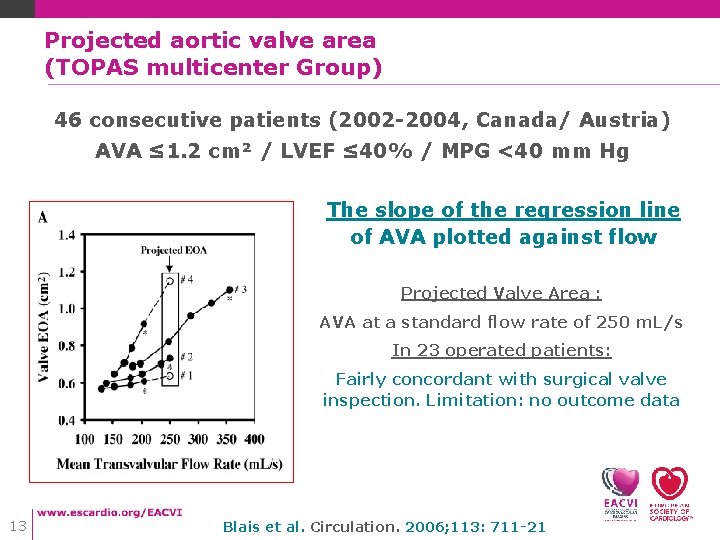
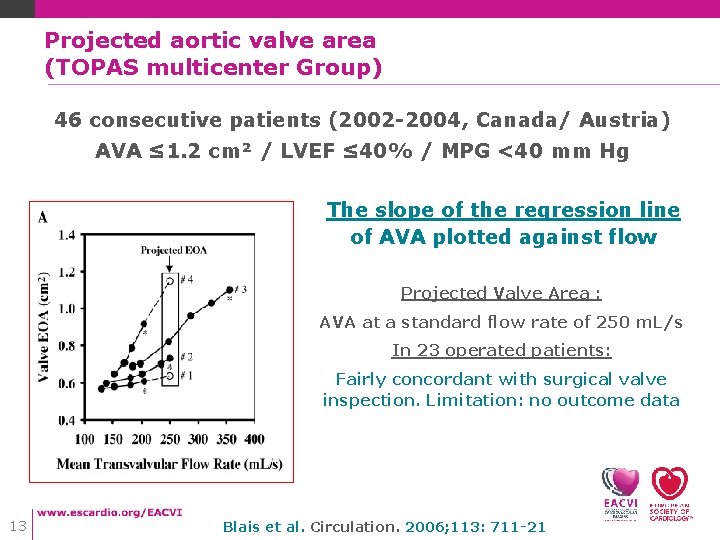
Projected aortic valve area (TOPAS multicenter Group) 46 consecutive patients (2002 -2004, Canada/ Austria) AVA ≤ 1. 2 cm² / LVEF ≤ 40% / MPG <40 mm Hg The slope of the regression line of AVA plotted against flow Projected Valve Area : AVA at a standard flow rate of 250 m. L/s In 23 operated patients: Fairly concordant with surgical valve inspection. Limitation: no outcome data 13 Blais et al. Circulation. 2006; 113: 711 -21
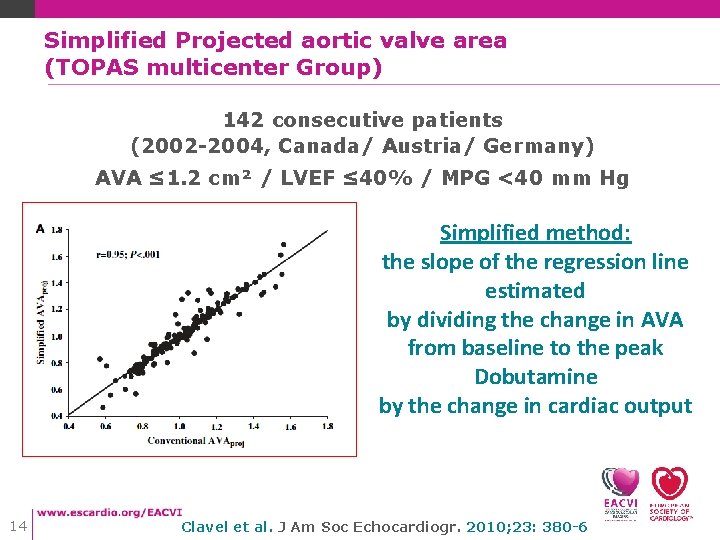
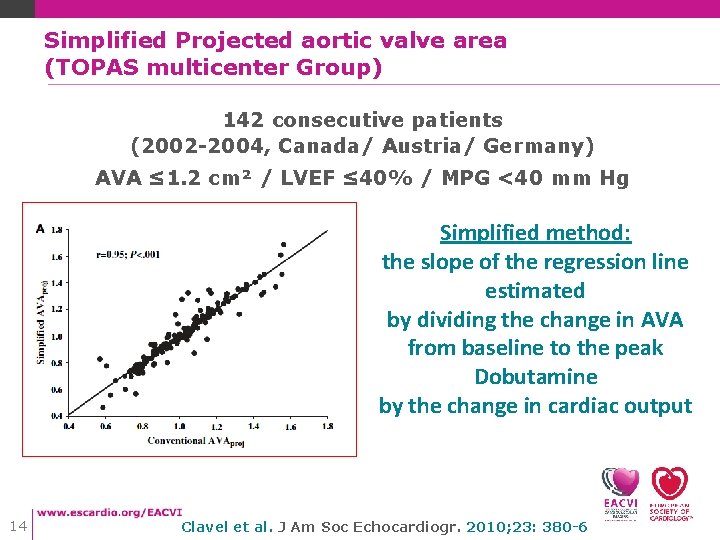
Simplified Projected aortic valve area (TOPAS multicenter Group) 142 consecutive patients (2002 -2004, Canada/ Austria/ Germany) AVA ≤ 1. 2 cm² / LVEF ≤ 40% / MPG <40 mm Hg Simplified method: the slope of the regression line estimated by dividing the change in AVA from baseline to the peak Dobutamine by the change in cardiac output 14 Clavel et al. J Am Soc Echocardiogr. 2010; 23: 380 -6
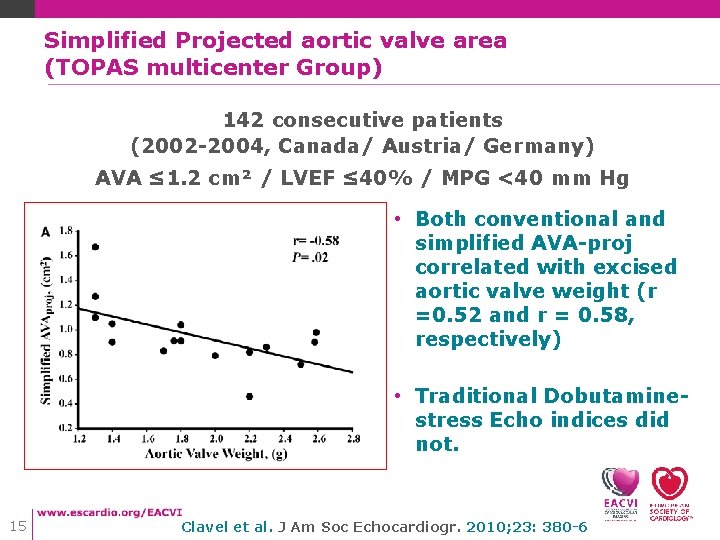
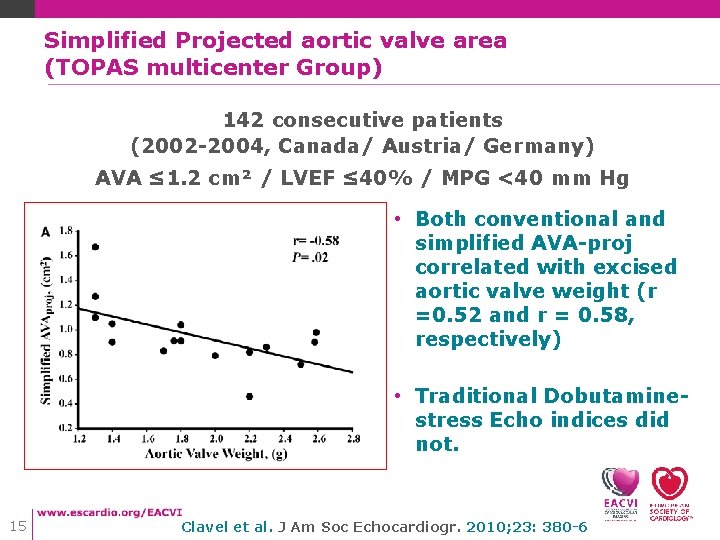
Simplified Projected aortic valve area (TOPAS multicenter Group) 142 consecutive patients (2002 -2004, Canada/ Austria/ Germany) AVA ≤ 1. 2 cm² / LVEF ≤ 40% / MPG <40 mm Hg • Both conventional and simplified AVA-proj correlated with excised aortic valve weight (r =0. 52 and r = 0. 58, respectively) • Traditional Dobutaminestress Echo indices did not. 15 Clavel et al. J Am Soc Echocardiogr. 2010; 23: 380 -6
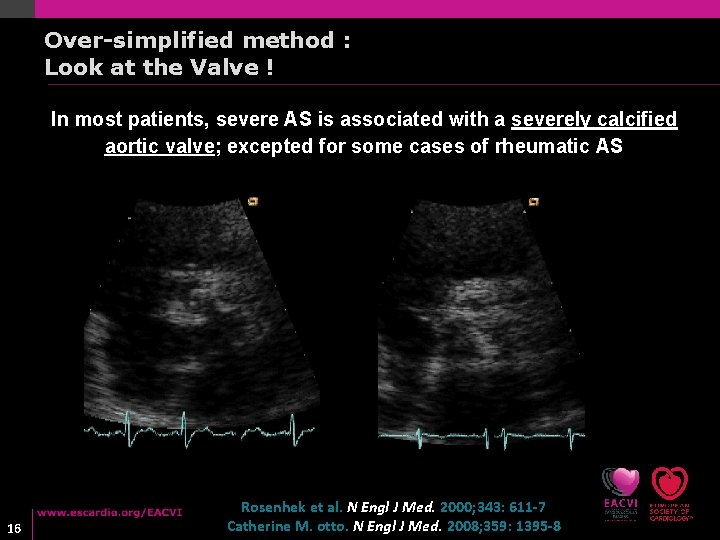
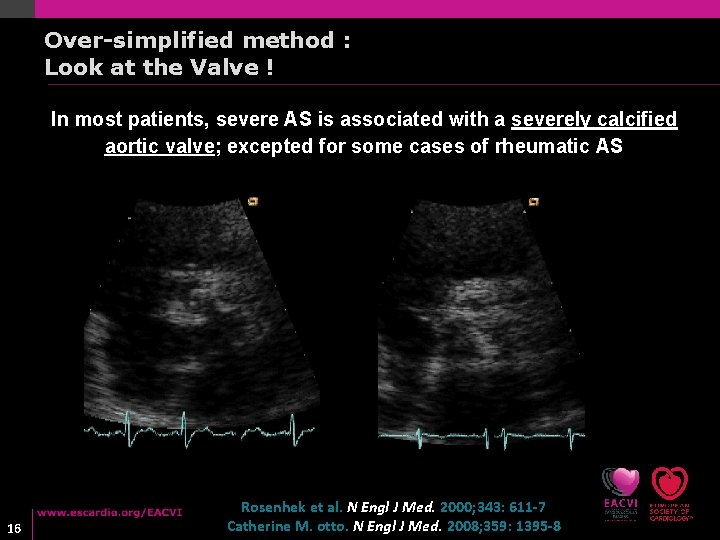
Over-simplified method : Look at the Valve ! In most patients, severe AS is associated with a severely calcified aortic valve; excepted for some cases of rheumatic AS 16 Rosenhek et al. N Engl J Med. 2000; 343: 611 -7 Catherine M. otto. N Engl J Med. 2008; 359: 1395 -8
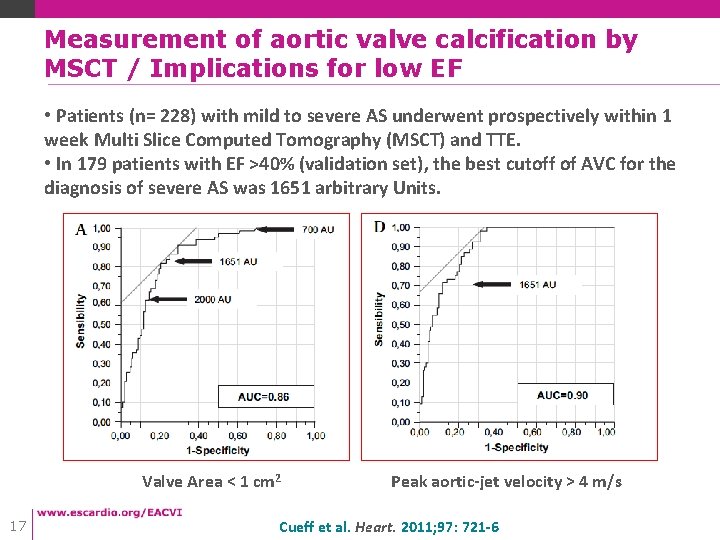
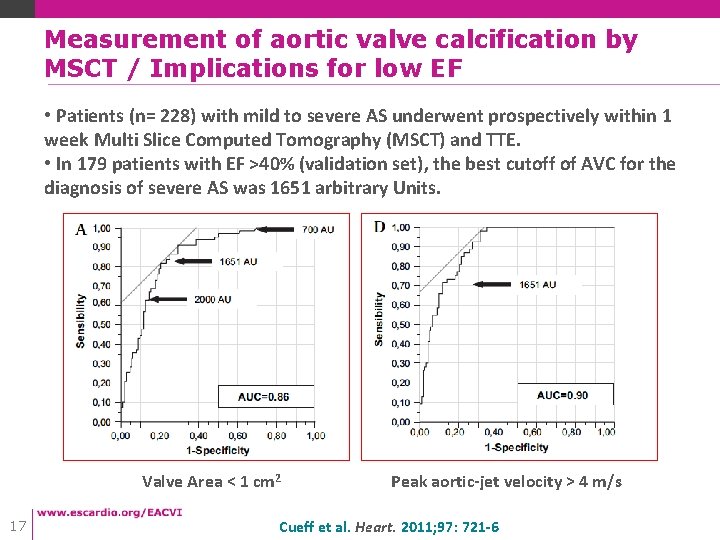
Measurement of aortic valve calcification by MSCT / Implications for low EF • Patients (n= 228) with mild to severe AS underwent prospectively within 1 week Multi Slice Computed Tomography (MSCT) and TTE. • In 179 patients with EF >40% (validation set), the best cutoff of AVC for the diagnosis of severe AS was 1651 arbitrary Units. Valve Area < 1 cm 2 17 Peak aortic-jet velocity > 4 m/s Cueff et al. Heart. 2011; 97: 721 -6
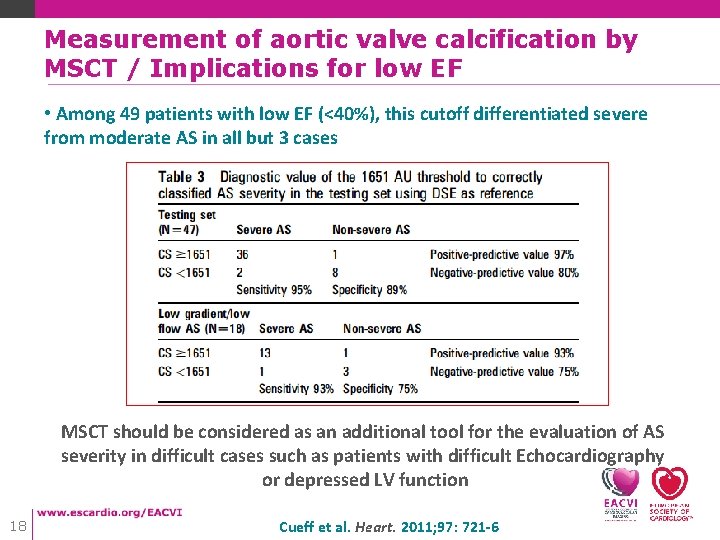
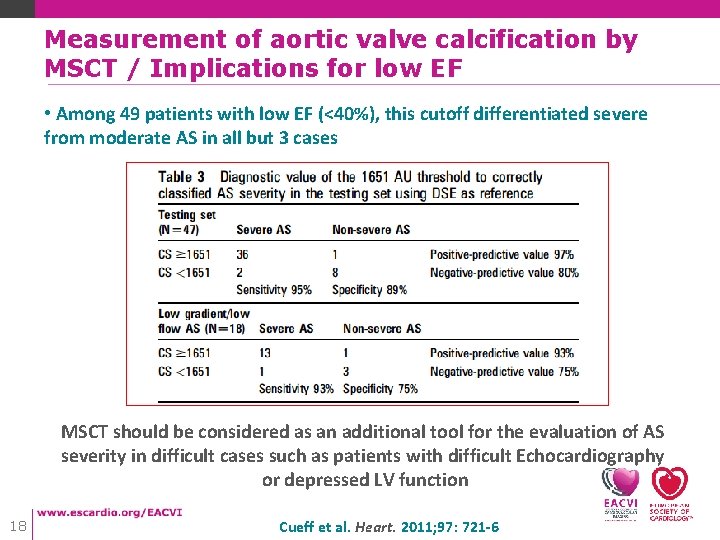
Measurement of aortic valve calcification by MSCT / Implications for low EF • Among 49 patients with low EF (<40%), this cutoff differentiated severe from moderate AS in all but 3 cases MSCT should be considered as an additional tool for the evaluation of AS severity in difficult cases such as patients with difficult Echocardiography or depressed LV function 18 Cueff et al. Heart. 2011; 97: 721 -6
Low-gradient/ Low-flow AS with low LV ejection fraction • How to differentiate True-severe from pseudo-severe AS ? • Outcome implications regarding pseudo-severe AS • Current role of risk stratification 19
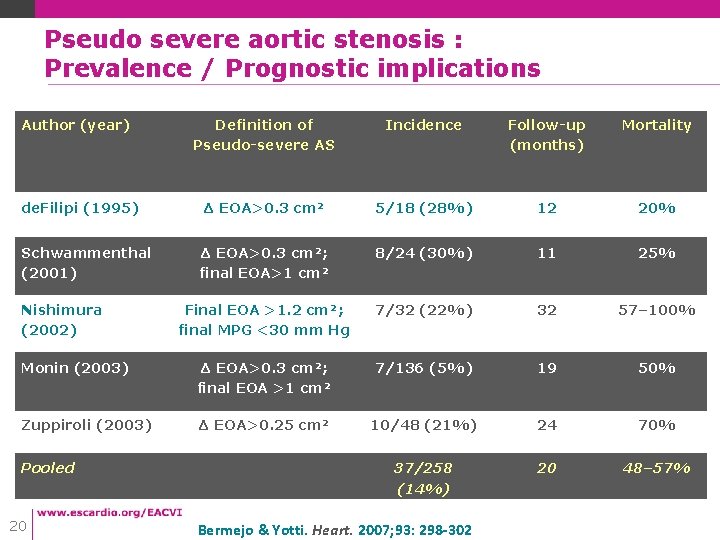
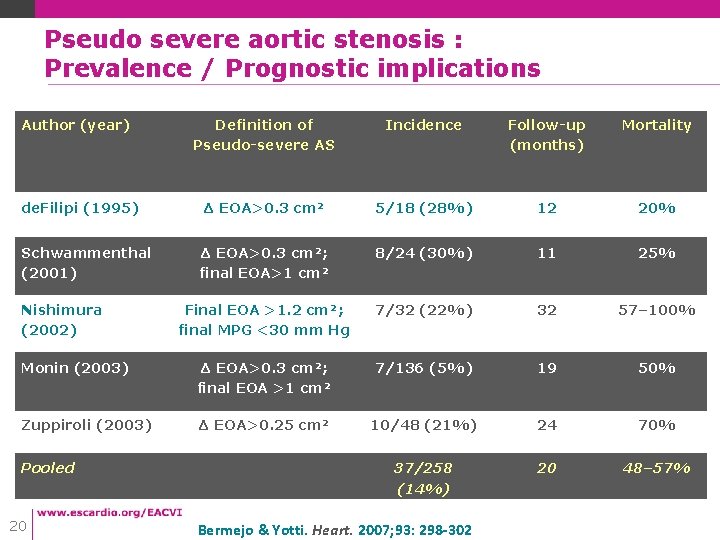
Pseudo severe aortic stenosis : Prevalence / Prognostic implications Author (year) Definition of Pseudo-severe AS Incidence Follow-up (months) Mortality de. Filipi (1995) Δ EOA>0. 3 cm² 5/18 (28%) 12 20% Δ EOA>0. 3 cm²; final EOA>1 cm² 8/24 (30%) 11 25% Final EOA >1. 2 cm²; final MPG <30 mm Hg 7/32 (22%) 32 57– 100% Monin (2003) Δ EOA>0. 3 cm²; final EOA >1 cm² 7/136 (5%) 19 50% Zuppiroli (2003) Δ EOA>0. 25 cm² 10/48 (21%) 24 70% 37/258 (14%) 20 48– 57% Schwammenthal (2001) Nishimura (2002) Pooled 20 Bermejo & Yotti. Heart. 2007; 93: 298 -302
Assessing AS in patients with LV systolic dysfunction: Major issues 1/ Valve calcification ( « Look at the valve » ) 2/ LV contractile reserve: perhaps most important, rather than precise distinction between fixed and pseudo-AS 3/ Pseudo-severe AS: remains to be tested in large groups, against clinical outcome 21 Paul A. Grayburn Circulation. 2006; 113: 604 -606
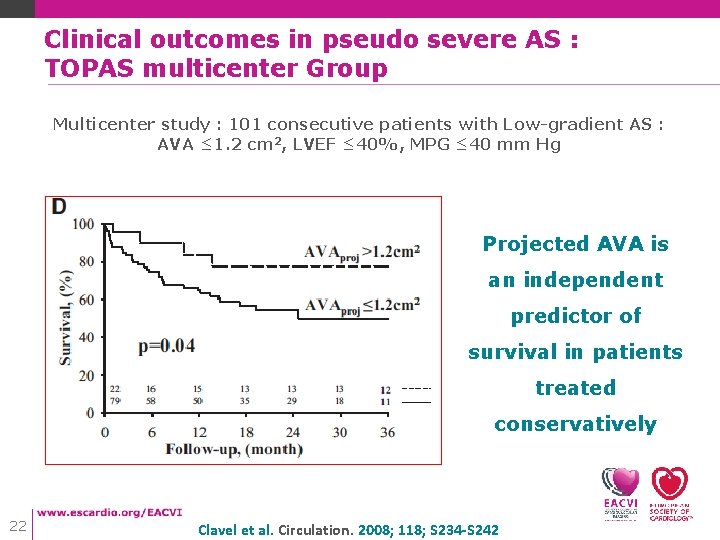
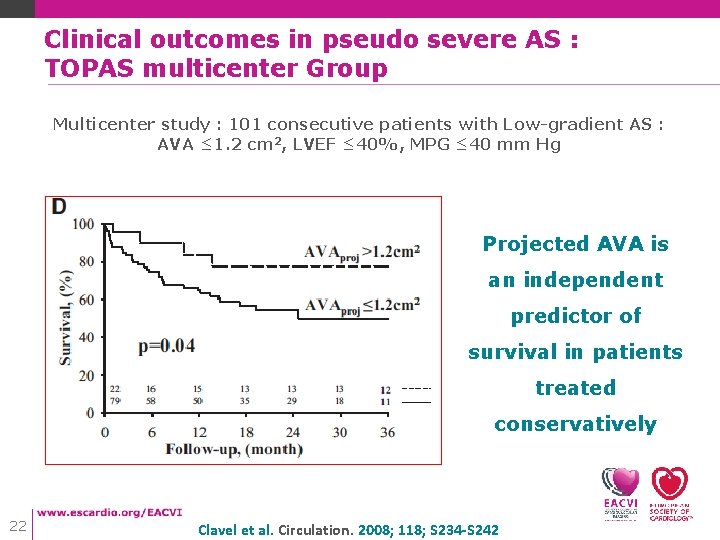
Clinical outcomes in pseudo severe AS : TOPAS multicenter Group Multicenter study : 101 consecutive patients with Low-gradient AS : AVA ≤ 1. 2 cm 2, LVEF ≤ 40%, MPG ≤ 40 mm Hg Projected AVA is an independent predictor of survival in patients treated conservatively 22 Clavel et al. Circulation. 2008; 118; S 234 -S 242
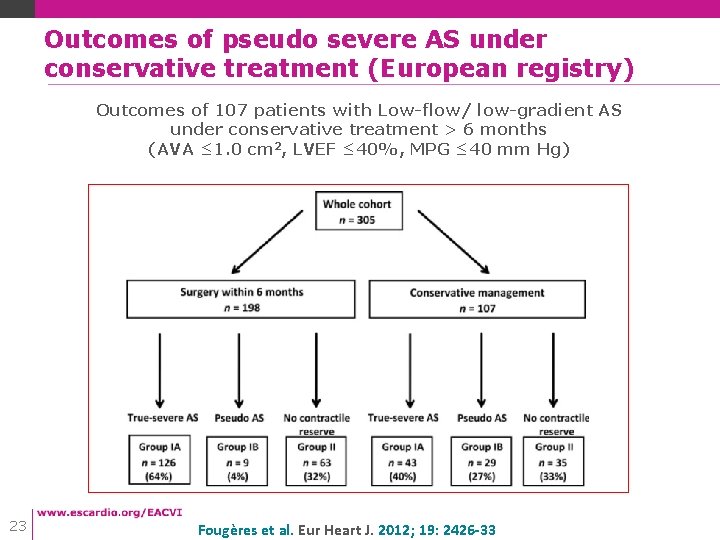
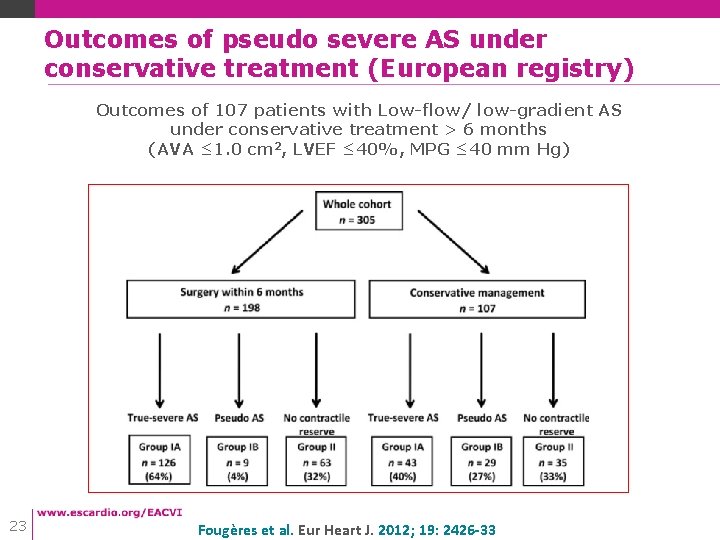
Outcomes of pseudo severe AS under conservative treatment (European registry) Outcomes of 107 patients with Low-flow/ low-gradient AS under conservative treatment > 6 months (AVA ≤ 1. 0 cm 2, LVEF ≤ 40%, MPG ≤ 40 mm Hg) 23 Fougères et al. Eur Heart J. 2012; 19: 2426 -33
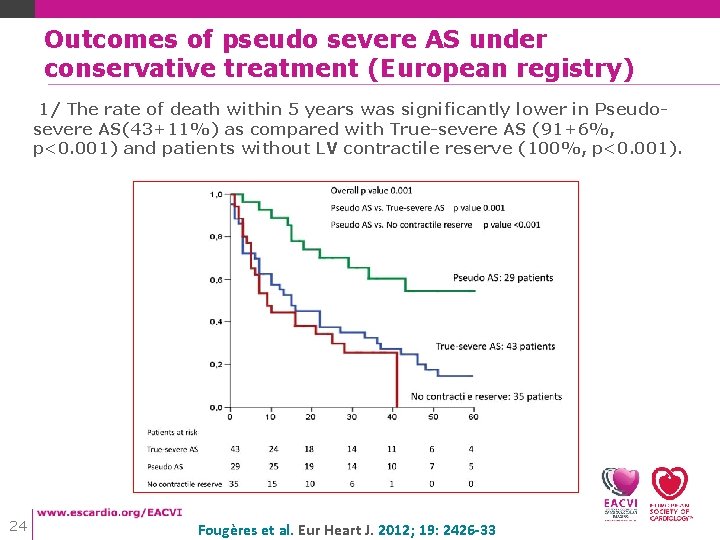
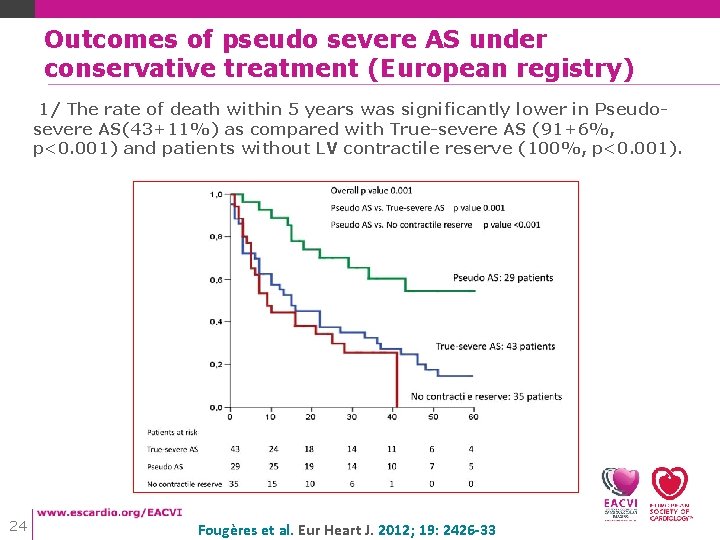
Outcomes of pseudo severe AS under conservative treatment (European registry) 1/ The rate of death within 5 years was significantly lower in Pseudosevere AS(43+11%) as compared with True-severe AS (91+6%, p<0. 001) and patients without LV contractile reserve (100%, p<0. 001). 24 Fougères et al. Eur Heart J. 2012; 19: 2426 -33
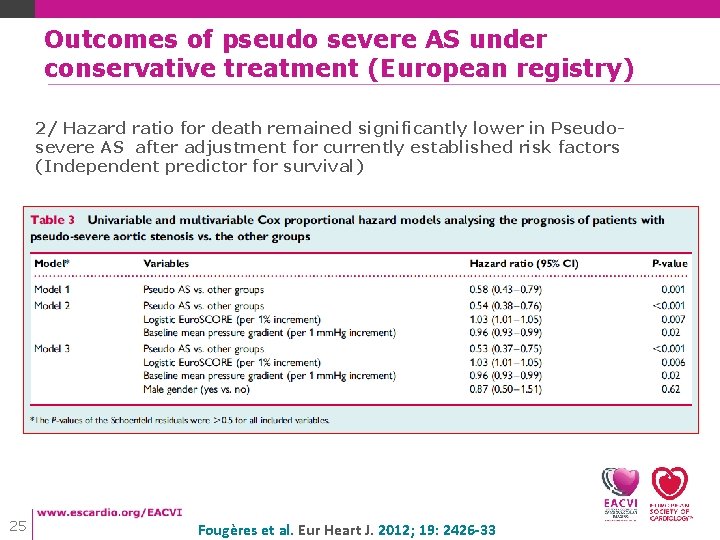
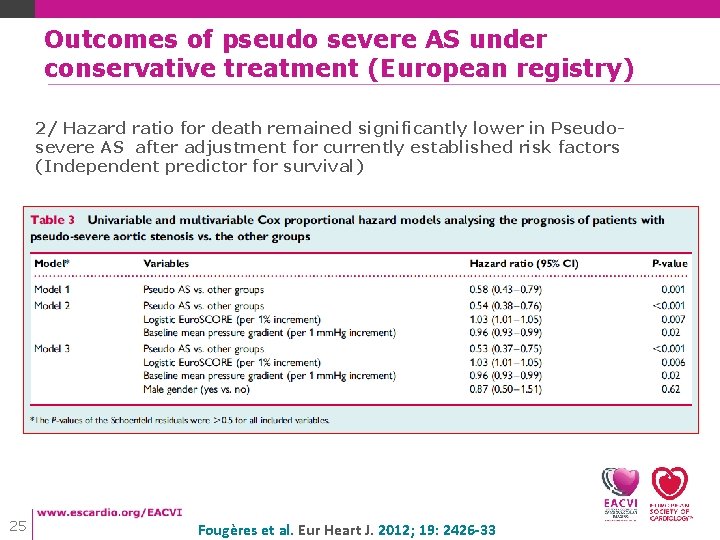
Outcomes of pseudo severe AS under conservative treatment (European registry) 2/ Hazard ratio for death remained significantly lower in Pseudosevere AS after adjustment for currently established risk factors (Independent predictor for survival) 25 Fougères et al. Eur Heart J. 2012; 19: 2426 -33
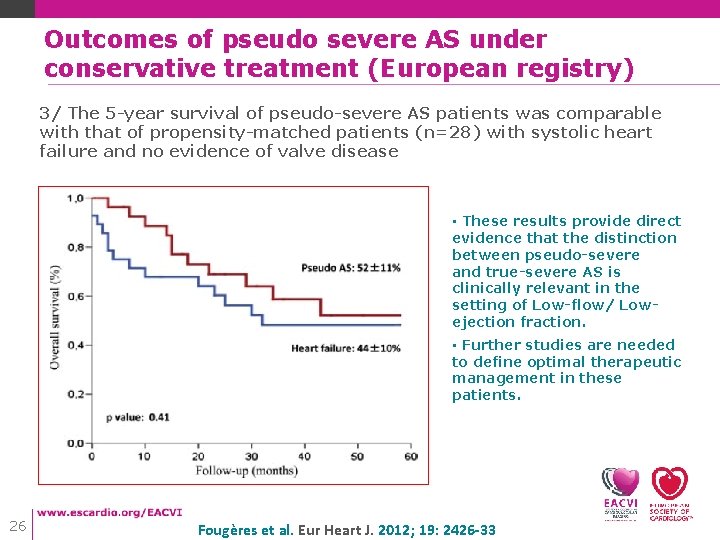
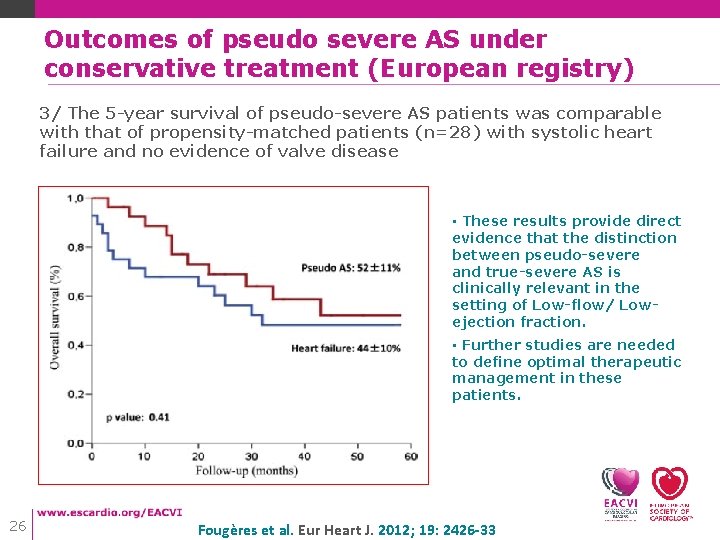
Outcomes of pseudo severe AS under conservative treatment (European registry) 3/ The 5 -year survival of pseudo-severe AS patients was comparable with that of propensity-matched patients (n=28) with systolic heart failure and no evidence of valve disease • These results provide direct evidence that the distinction between pseudo-severe and true-severe AS is clinically relevant in the setting of Low-flow/ Lowejection fraction. • Further studies are needed to define optimal therapeutic management in these patients. 26 Fougères et al. Eur Heart J. 2012; 19: 2426 -33
Low-gradient/ Low-flow AS with low LV ejection fraction • How to differentiate True-severe from pseudo-severe AS ? • Outcome implications regarding pseudo-severe AS • Current role of risk stratification 27
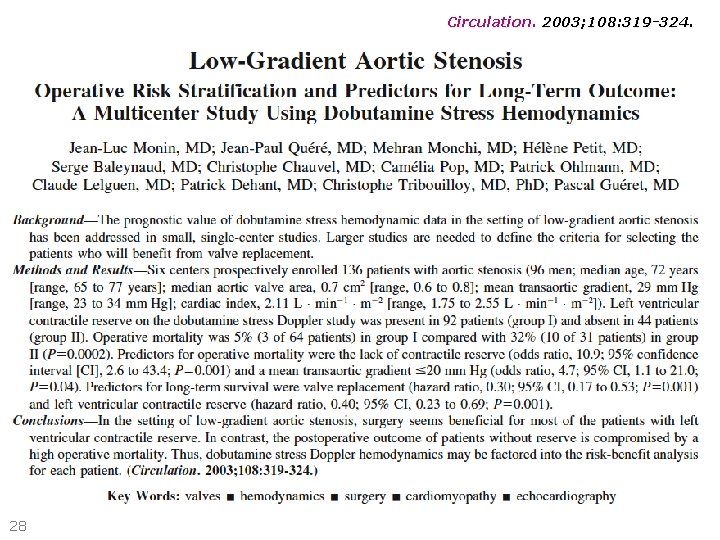
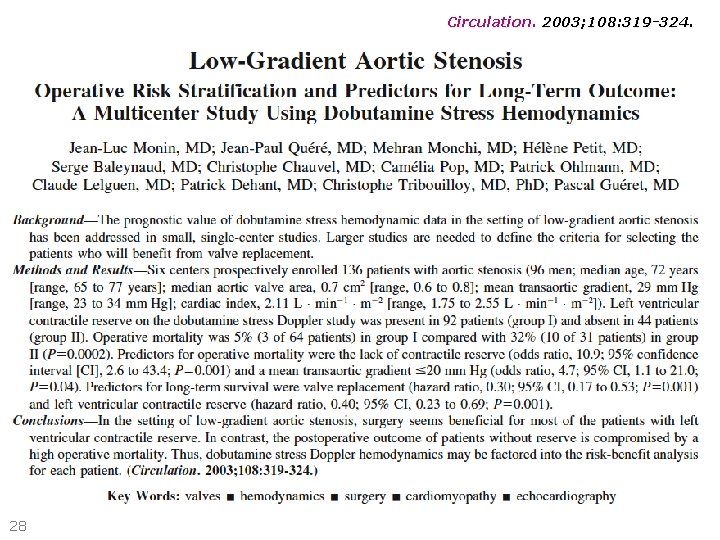
Circulation. 2003; 108: 319 -324. 28
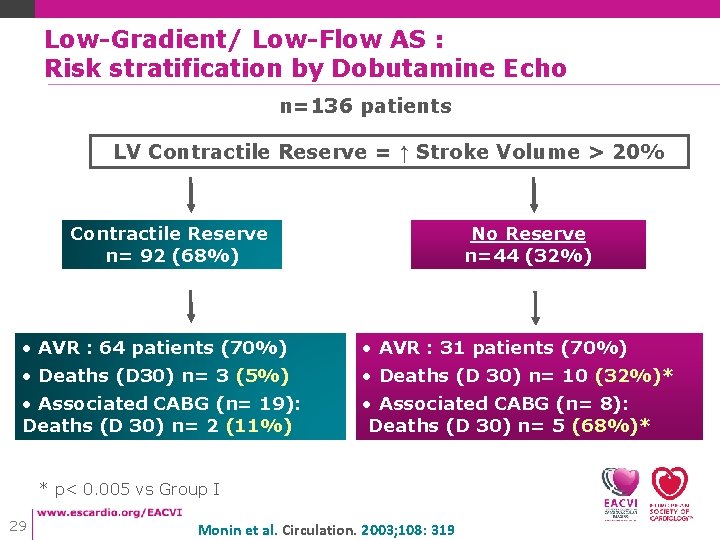
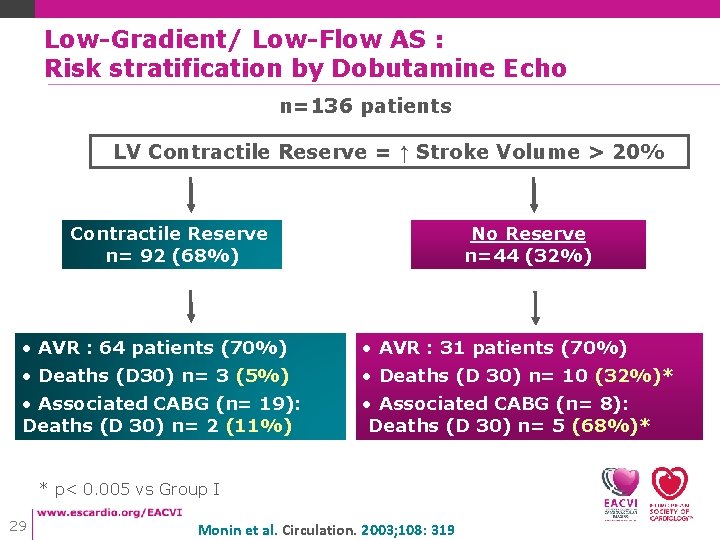
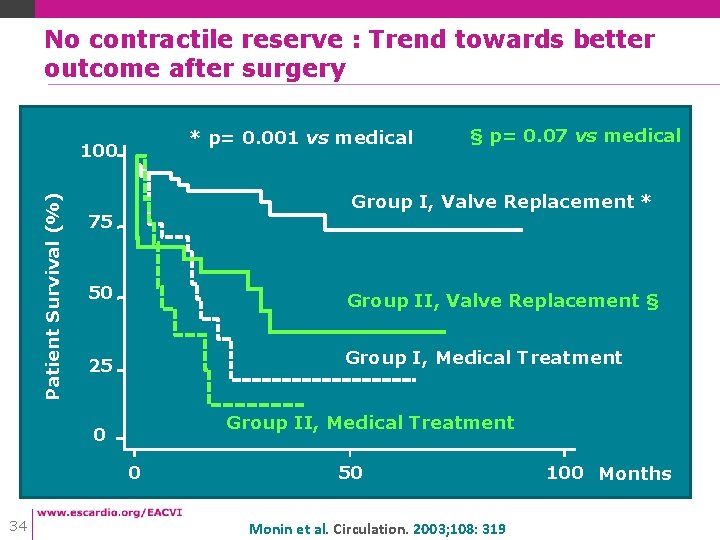
Low-Gradient/ Low-Flow AS : Risk stratification by Dobutamine Echo n=136 patients LV Contractile Reserve = ↑ Stroke Volume > 20% Contractile Reserve n= 92 (68%) No Reserve n=44 (32%) • AVR : 64 patients (70%) • AVR : 31 patients (70%) • Deaths (D 30) n= 3 (5%) • Deaths (D 30) n= 10 (32%)* • Associated CABG (n= 19): Deaths (D 30) n= 2 (11%) • Associated CABG (n= 8): Deaths (D 30) n= 5 (68%)* * p< 0. 005 vs Group I 29 Monin et al. Circulation. 2003; 108: 319
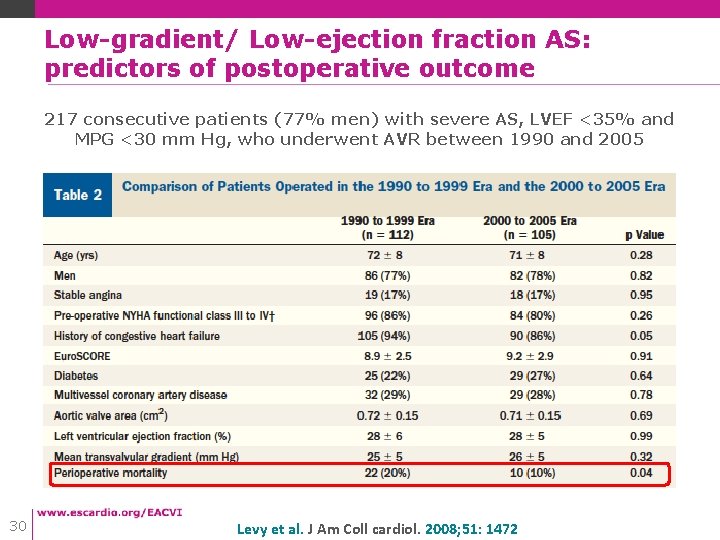
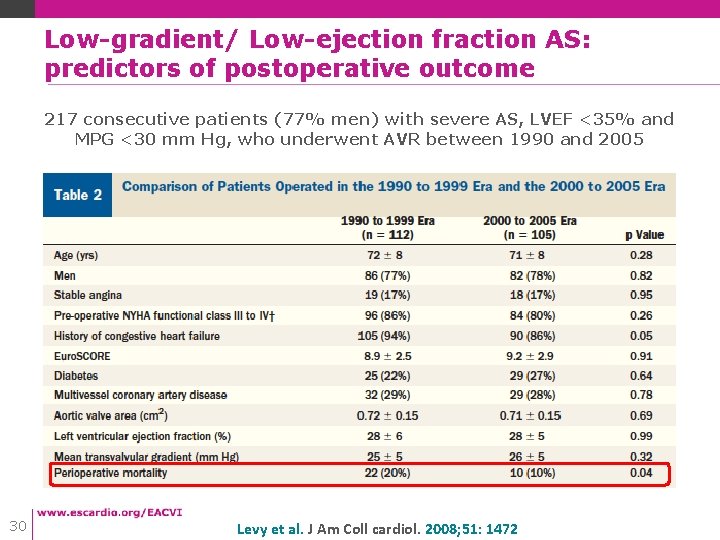
Low-gradient/ Low-ejection fraction AS: predictors of postoperative outcome 217 consecutive patients (77% men) with severe AS, LVEF <35% and MPG <30 mm Hg, who underwent AVR between 1990 and 2005 30 Levy et al. J Am Coll cardiol. 2008; 51: 1472
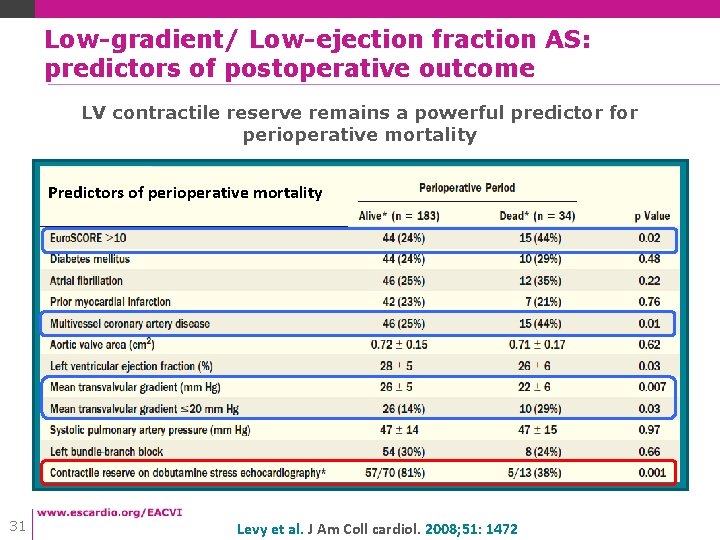
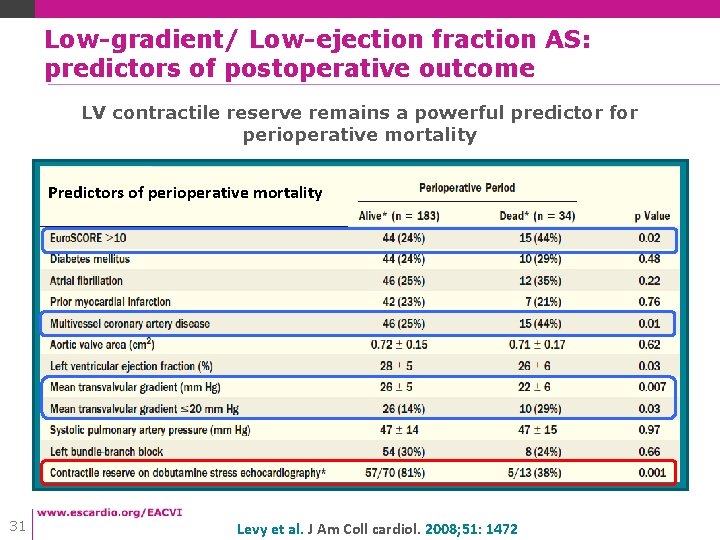
Low-gradient/ Low-ejection fraction AS: predictors of postoperative outcome LV contractile reserve remains a powerful predictor for perioperative mortality Predictors of perioperative mortality 31 Levy et al. J Am Coll cardiol. 2008; 51: 1472
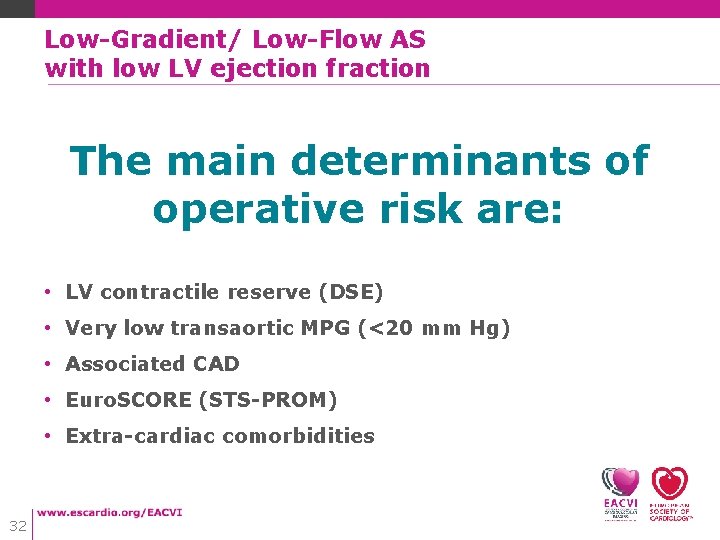
Low-Gradient/ Low-Flow AS with low LV ejection fraction The main determinants of operative risk are: • LV contractile reserve (DSE) • Very low transaortic MPG (<20 mm Hg) • Associated CAD • Euro. SCORE (STS-PROM) • Extra-cardiac comorbidities 32
Low-Gradient/ Low-Flow AS with low LV ejection fraction What if the patient is at very high risk ? 33
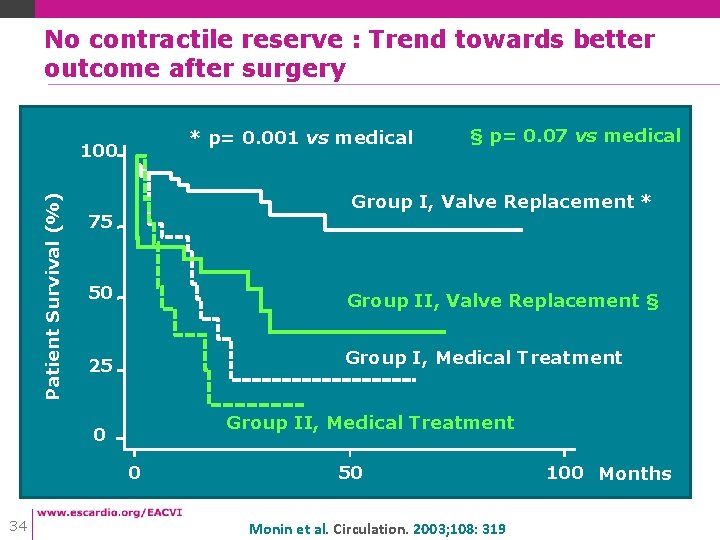
No contractile reserve : Trend towards better outcome after surgery * p= 0. 001 vs medical Patient Survival (%) 100 Group I, Valve Replacement * 75 50 Group II, Valve Replacement § 25 Group I, Medical Treatment Group II, Medical Treatment 0 0 34 § p= 0. 07 vs medical 50 Monin et al. Circulation. 2003; 108: 319 100 Months
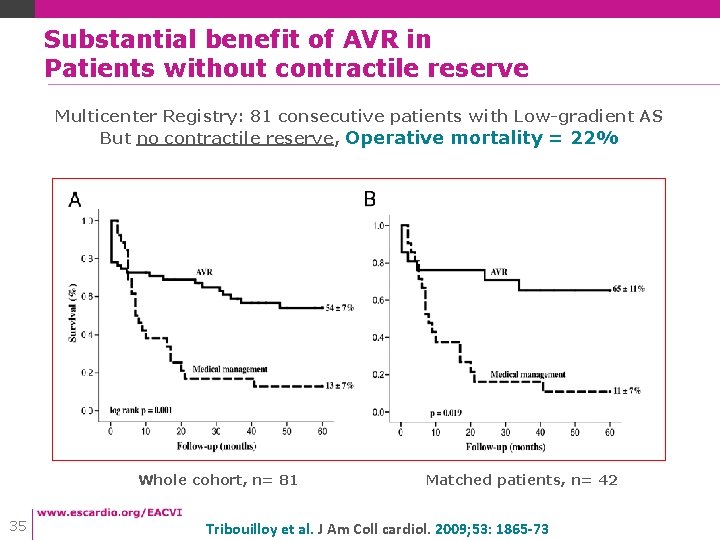
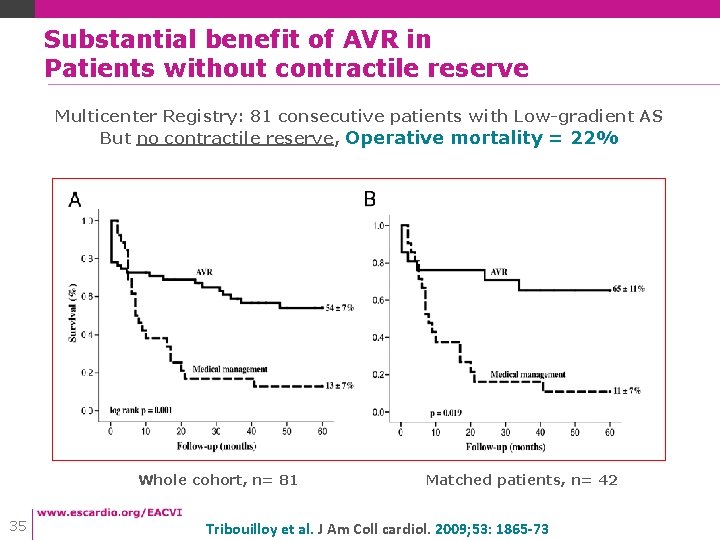
Substantial benefit of AVR in Patients without contractile reserve Multicenter Registry: 81 consecutive patients with Low-gradient AS But no contractile reserve, Operative mortality = 22% Whole cohort, n= 81 35 Matched patients, n= 42 Tribouilloy et al. J Am Coll cardiol. 2009; 53: 1865 -73
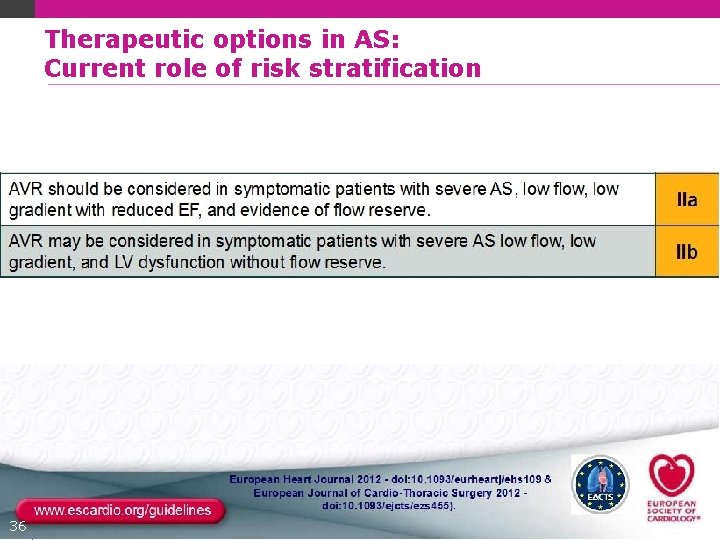
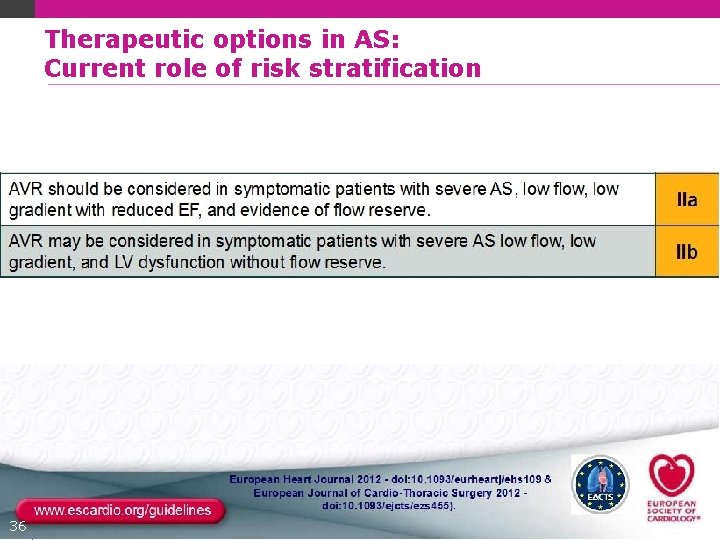
Therapeutic options in AS: Current role of risk stratification 36
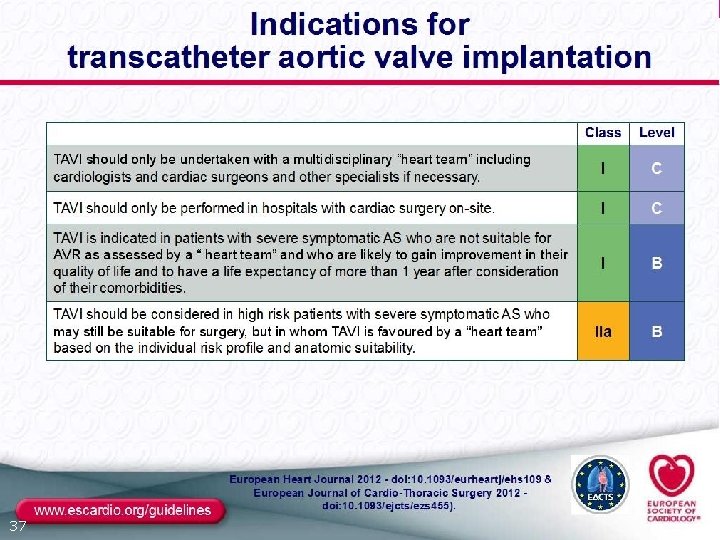
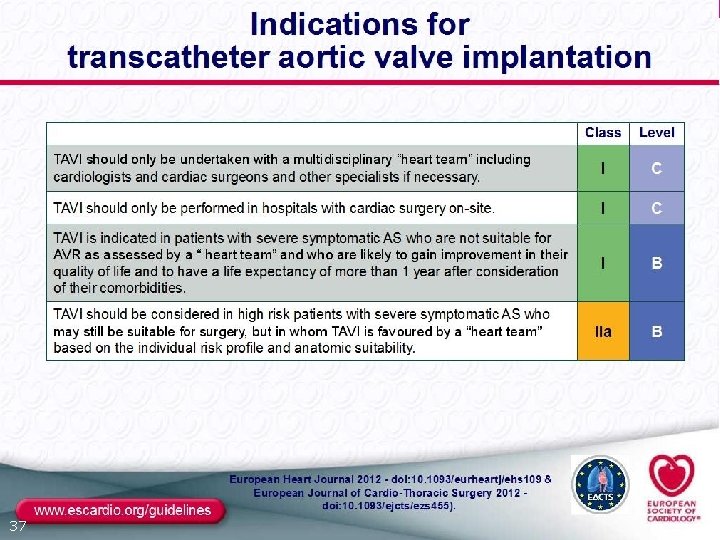
37
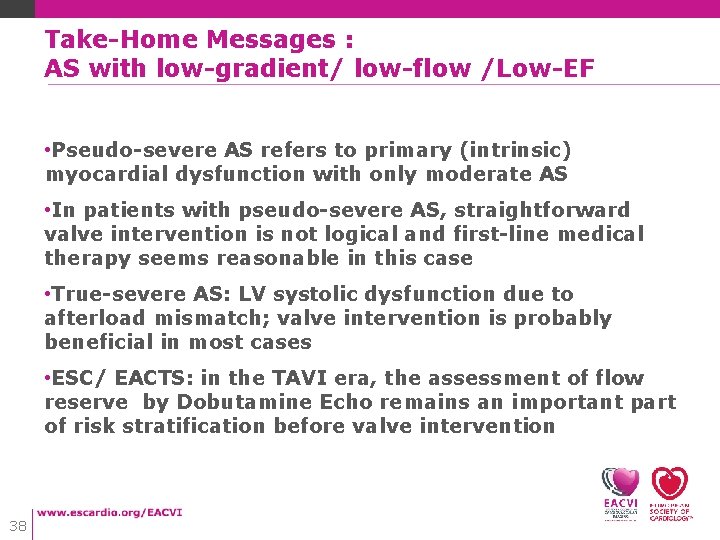
Take-Home Messages : AS with low-gradient/ low-flow /Low-EF • Pseudo-severe AS refers to primary (intrinsic) myocardial dysfunction with only moderate AS • In patients with pseudo-severe AS, straightforward valve intervention is not logical and first-line medical therapy seems reasonable in this case • True-severe AS: LV systolic dysfunction due to afterload mismatch; valve intervention is probably beneficial in most cases • ESC/ EACTS: in the TAVI era, the assessment of flow reserve by Dobutamine Echo remains an important part of risk stratification before valve intervention 38
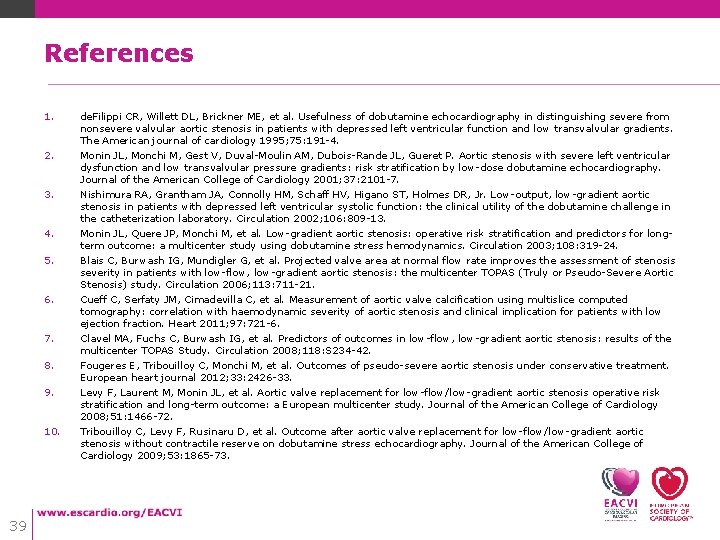
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 39 de. Filippi CR, Willett DL, Brickner ME, et al. Usefulness of dobutamine echocardiography in distinguishing severe from nonsevere valvular aortic stenosis in patients with depressed left ventricular function and low transvalvular gradients. The American journal of cardiology 1995; 75: 191 -4. Monin JL, Monchi M, Gest V, Duval-Moulin AM, Dubois-Rande JL, Gueret P. Aortic stenosis with severe left ventricular dysfunction and low transvalvular pressure gradients: risk stratification by low-dose dobutamine echocardiography. Journal of the American College of Cardiology 2001; 37: 2101 -7. Nishimura RA, Grantham JA, Connolly HM, Schaff HV, Higano ST, Holmes DR, Jr. Low-output, low-gradient aortic stenosis in patients with depressed left ventricular systolic function: the clinical utility of the dobutamine challenge in the catheterization laboratory. Circulation 2002; 106: 809 -13. Monin JL, Quere JP, Monchi M, et al. Low-gradient aortic stenosis: operative risk stratification and predictors for longterm outcome: a multicenter study using dobutamine stress hemodynamics. Circulation 2003; 108: 319 -24. Blais C, Burwash IG, Mundigler G, et al. Projected valve area at normal flow rate improves the assessment of stenosis severity in patients with low-flow, low-gradient aortic stenosis: the multicenter TOPAS (Truly or Pseudo-Severe Aortic Stenosis) study. Circulation 2006; 113: 711 -21. Cueff C, Serfaty JM, Cimadevilla C, et al. Measurement of aortic valve calcification using multislice computed tomography: correlation with haemodynamic severity of aortic stenosis and clinical implication for patients with low ejection fraction. Heart 2011; 97: 721 -6. Clavel MA, Fuchs C, Burwash IG, et al. Predictors of outcomes in low-flow, low-gradient aortic stenosis: results of the multicenter TOPAS Study. Circulation 2008; 118: S 234 -42. Fougeres E, Tribouilloy C, Monchi M, et al. Outcomes of pseudo-severe aortic stenosis under conservative treatment. European heart journal 2012; 33: 2426 -33. Levy F, Laurent M, Monin JL, et al. Aortic valve replacement for low-flow/low-gradient aortic stenosis operative risk stratification and long-term outcome: a European multicenter study. Journal of the American College of Cardiology 2008; 51: 1466 -72. Tribouilloy C, Levy F, Rusinaru D, et al. Outcome after aortic valve replacement for low-flow/low-gradient aortic stenosis without contractile reserve on dobutamine stress echocardiography. Journal of the American College of Cardiology 2009; 53: 1865 -73.