LOWER LIMB EDEMA A systemic approach By PBL

LOWER LIMB EDEMA (A systemic approach) By PBL 20 Tutor : DR ALIAA ELSAWY
OBJECTIVES
üDefinition of edema üAnatomy and pathophysiology of edema üClassification of edema ØBilateral edema ØUnilateral pitting edema ØUnilateral non-pitting edema üInitial assessment and diagnosis of edema üLymphatic filariasis
DEFINITION OF EDEMA
• abnormal infiltration and excess accumulation of large fluid volume in the circulatory system or in tissues between the body's cells (interstitial spaces).

ANATOMY & PATHOPHYSIOLOGY OF EDEMA
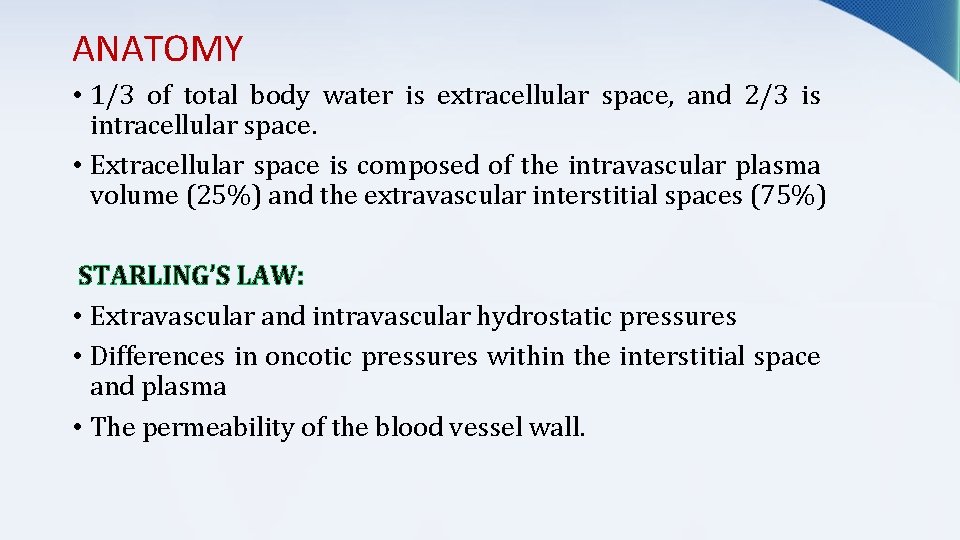
ANATOMY • 1/3 of total body water is extracellular space, and 2/3 is intracellular space. • Extracellular space is composed of the intravascular plasma volume (25%) and the extravascular interstitial spaces (75%) STARLING’S LAW: • Extravascular and intravascular hydrostatic pressures • Differences in oncotic pressures within the interstitial space and plasma • The permeability of the blood vessel wall.
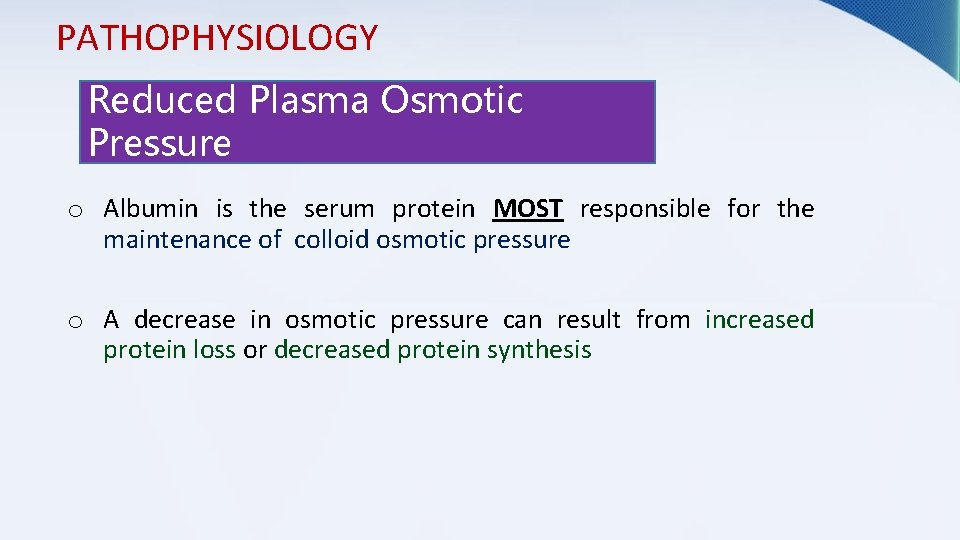
PATHOPHYSIOLOGY Reduced Plasma Osmotic Pressure o Albumin is the serum protein MOST responsible for the maintenance of colloid osmotic pressure o A decrease in osmotic pressure can result from increased protein loss or decreased protein synthesis

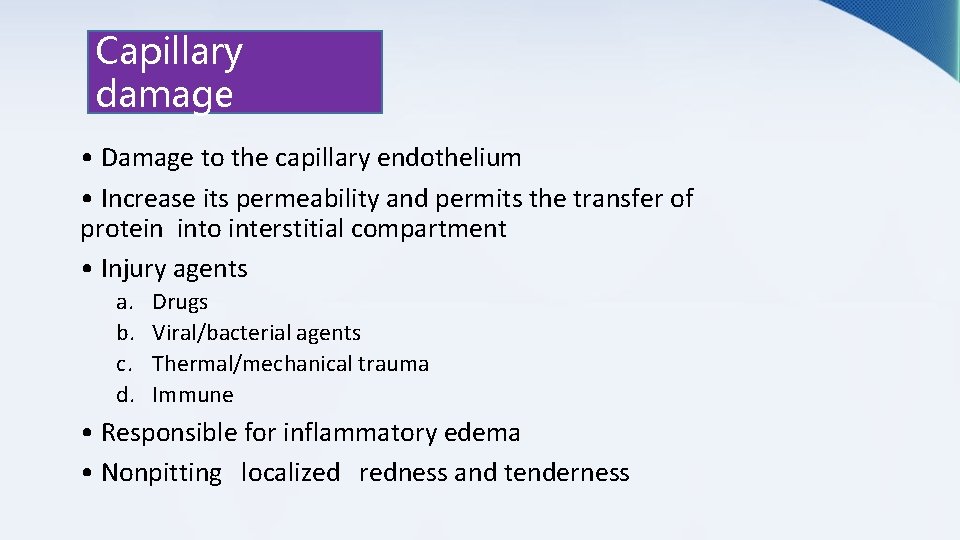
Capillary damage • Damage to the capillary endothelium • Increase its permeability and permits the transfer of protein into interstitial compartment • Injury agents a. b. c. d. Drugs Viral/bacterial agents Thermal/mechanical trauma Immune • Responsible for inflammatory edema • Nonpitting localized redness and tenderness
CLASSIFICATION OF EDEMA
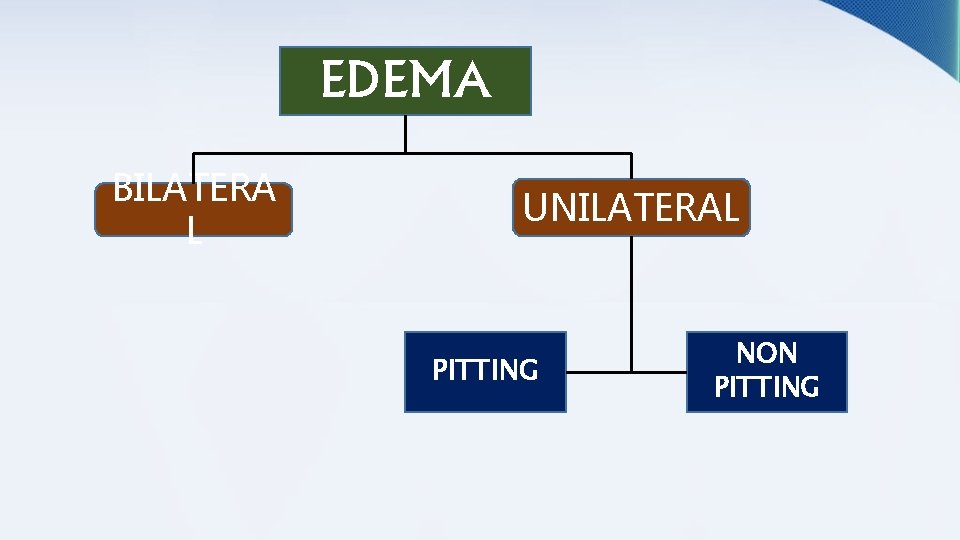
EDEMA BILATERA L UNILATERAL PITTING NON PITTING

BILATERAL EDEMA -Due to systemic disease 1. 2. 3. 4. 5. 6. 7. 8. Heart failure Kidney disease Liver failure Myxedema Malnutrition and malabsorption Hereditary angioedema Drug induced Idiopathic

UNILATERAL PITTING EDEMA • Varicose vein • Thrombophlebitis of the deep veins UNILATERAL NON PITTING EDEMA • lymphedema • hyperthyroidism

INITIAL ASSESSMENT & DIAGNOSIS OF EDEMA
INITIAL ASSESSMENT • History Taking and Physical Examination - Vitals signs - CVS examination - Abdominal examination - Local (limb) examination
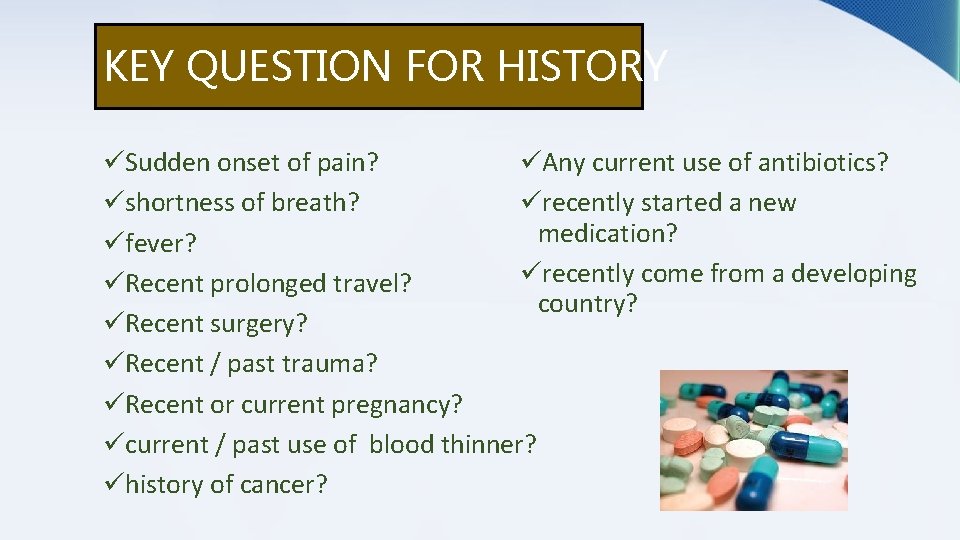
KEY QUESTION FOR HISTORY üSudden onset of pain? üAny current use of antibiotics? üshortness of breath? ürecently started a new medication? üfever? ürecently come from a developing üRecent prolonged travel? country? üRecent surgery? üRecent / past trauma? üRecent or current pregnancy? ücurrent / past use of blood thinner? ühistory of cancer?

PHYSICAL EXAMINATION Vitals signs • fever cellulitis, abscess, osteomyelitis, septic joint. not reliable in elderly DVT/PE could have fever in 14% • RR > 20/min / HR > 100 bpm HF, liver failure, cor pulmonale, renal failure, fever, dehydration, pain, PE • HTN + edematous, pregnant patient preeclampsia
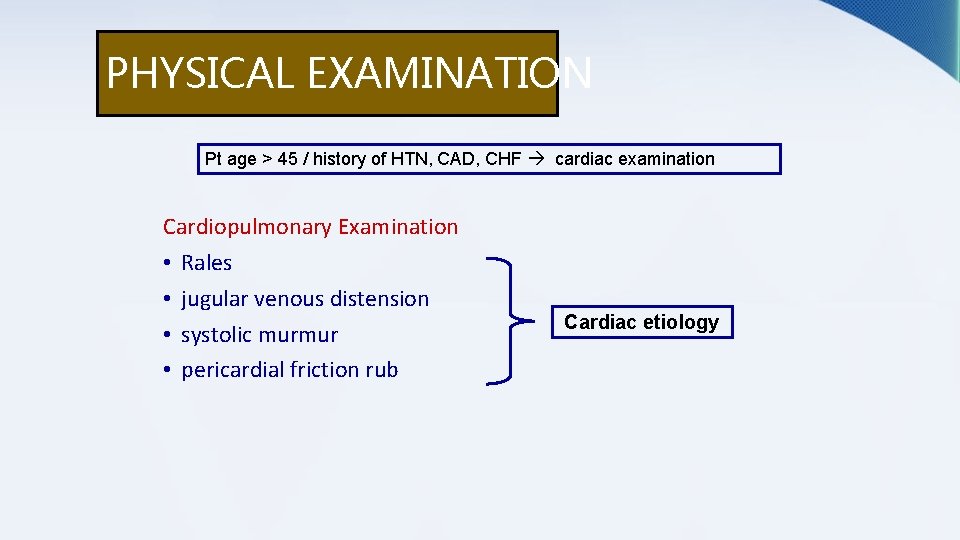
PHYSICAL EXAMINATION Pt age > 45 / history of HTN, CAD, CHF cardiac examination Cardiopulmonary Examination • Rales • jugular venous distension • systolic murmur • pericardial friction rub Cardiac etiology

PHYSICAL EXAMINATION Pt with hx of chronic alcohol use, cirrhosis, hepatitis abdominal exam Abdominal Examination • Shifting dullness • fluid wave • spiderangiomas • Jaundice • Palpable abdominal • & pelvic masses Liver disease external venous or lymphatic compression ovarian / prostate cancer
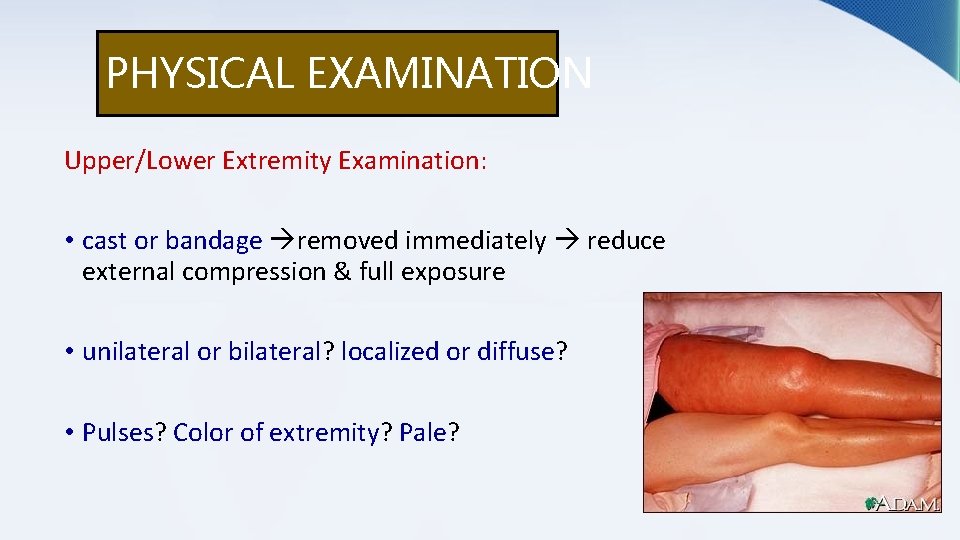
PHYSICAL EXAMINATION Upper/Lower Extremity Examination: • cast or bandage removed immediately reduce external compression & full exposure • unilateral or bilateral? localized or diffuse? • Pulses? Color of extremity? Pale?
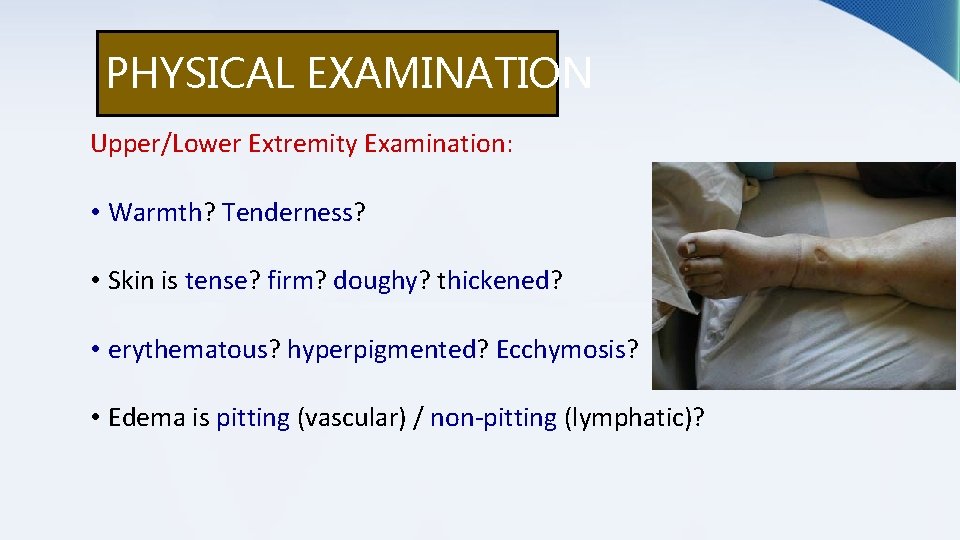
PHYSICAL EXAMINATION Upper/Lower Extremity Examination: • Warmth? Tenderness? • Skin is tense? firm? doughy? thickened? • erythematous? hyperpigmented? Ecchymosis? • Edema is pitting (vascular) / non-pitting (lymphatic)?

DIAGNOSTIC STUDIES Laboratory Testing Radiographic Studies
LABORATORY TESTING • CBC • Chemistry • D-dimer • Blood & tissue culture • Acute Phase Reactants (ESR, CRP, PCT)

RADIOGRAPHIC STUDIES • X-ray • US • CT & MRI • Venography

X-ray

Ultra sound lower extremity Doppler U/S • DVT • Baker cyst • Popliteal artery aneurysms • vascular masses

Venography A, B) Direct signs of a fresh DVT, intraluminal contrast defects, in the popliteal vein and leg vein (arrows). C) lndirect sign of extensive thrombosis of leg veins; no filling of posterior tibial or peroneal veins, massive collateral circulation via superficial veins.

LYMPHATIC FILARIASIS
-Infection by 2 Nematodes: 1. Wuchereria bancrofti 2. Brugia malayi • Transmitted by the bite of infected mosquito. • All the parasites have similar life cycle. • Adults seen in lymphatic vessels. • Microfilaria (pre-larva) seen in peripheral blood during night.
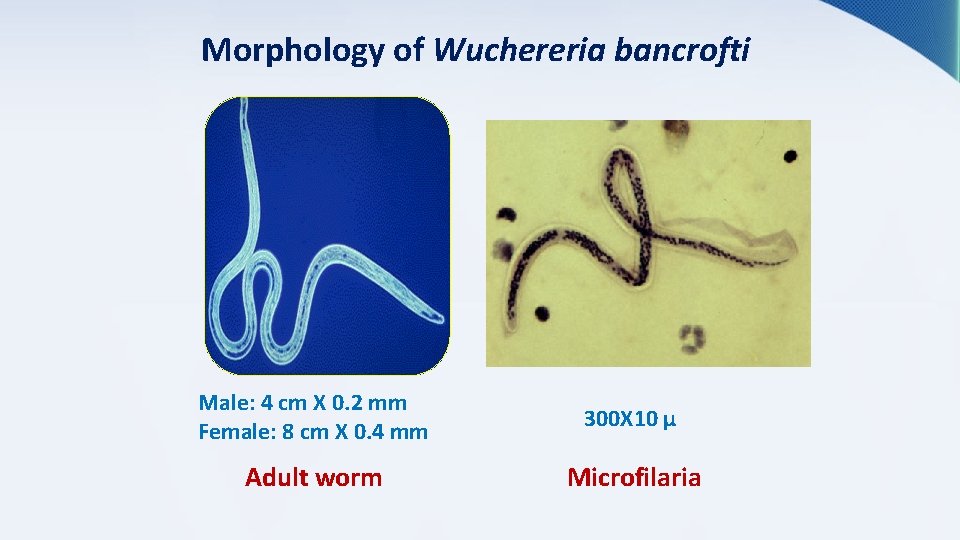
Morphology of Wuchereria bancrofti Male: 4 cm X 0. 2 mm Female: 8 cm X 0. 4 mm 300 X 10 µ Adult worm Microfilaria

Life Cycle
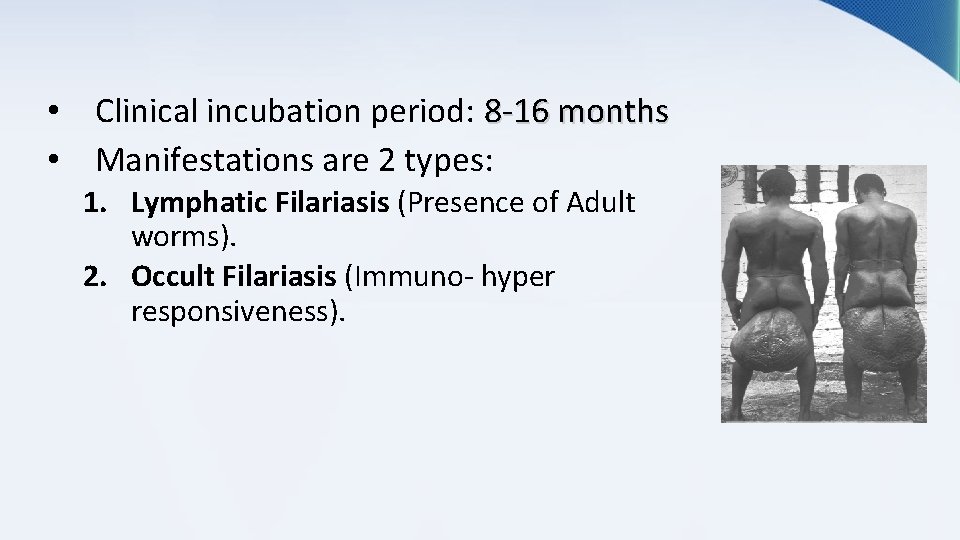
• Clinical incubation period: 8 -16 months • Manifestations are 2 types: 1. Lymphatic Filariasis (Presence of Adult worms). 2. Occult Filariasis (Immuno- hyper responsiveness).
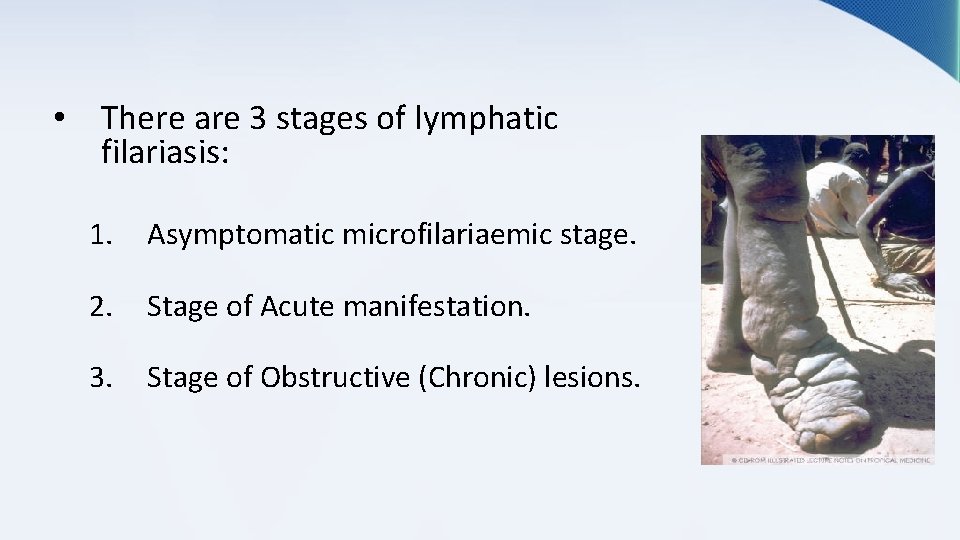
• There are 3 stages of lymphatic filariasis: 1. Asymptomatic microfilariaemic stage. 2. Stage of Acute manifestation. 3. Stage of Obstructive (Chronic) lesions.
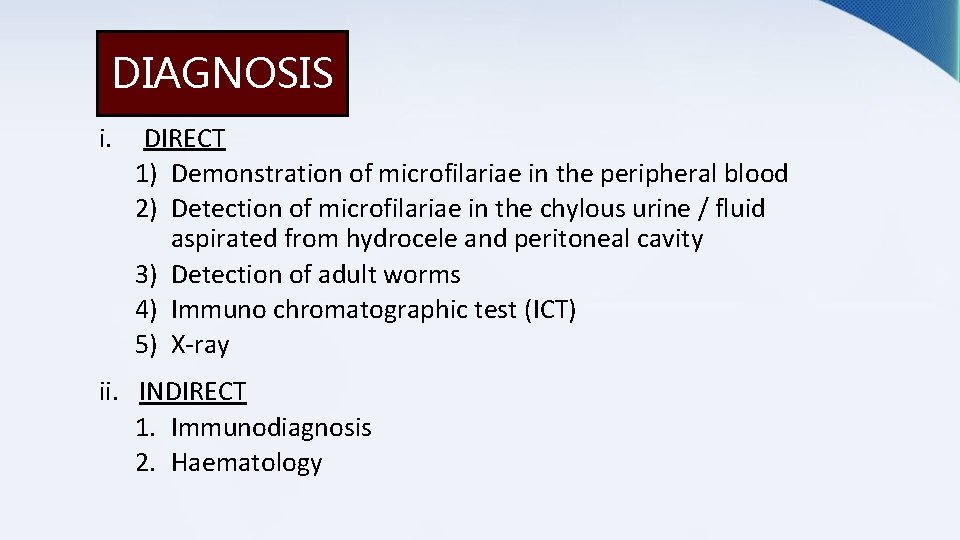
DIAGNOSIS i. DIRECT 1) Demonstration of microfilariae in the peripheral blood 2) Detection of microfilariae in the chylous urine / fluid aspirated from hydrocele and peritoneal cavity 3) Detection of adult worms 4) Immuno chromatographic test (ICT) 5) X-ray ii. INDIRECT 1. Immunodiagnosis 2. Haematology
TREATMENT 1. Chemotherapy a. Diethyl carbamazine citrate b. Ivermectin c. Albendazole 2. Surgical a. Hydrocele excision b. Scrotal elip removal c. Lymphoedema –excision of redundant tissue

SAMEH HUSSAIN AMAN HAFIY ROWA BELLA AMIRA PUTRI AISYAH HANIS NATASHA

- Slides: 38