Lower Limb Amputations Level Selection Arvind Lee Vascular
Lower Limb Amputations – Level Selection Arvind Lee Vascular Fellow Nepean Hospital
Overview • Integral part of any surgical practice. • The global lower extremity amputation study group - wide variations in amputation rates worldwide - similarities in age and sex distribution - very high correlation with diabetes (BJS 2000)
Overview • Australian data – - 2629 diabetes related lower limb amputations per year - 2: 1 male: female ratio - majority in the 65 -79 year age group - Highest incidence in SA and NT (MJA 2000)
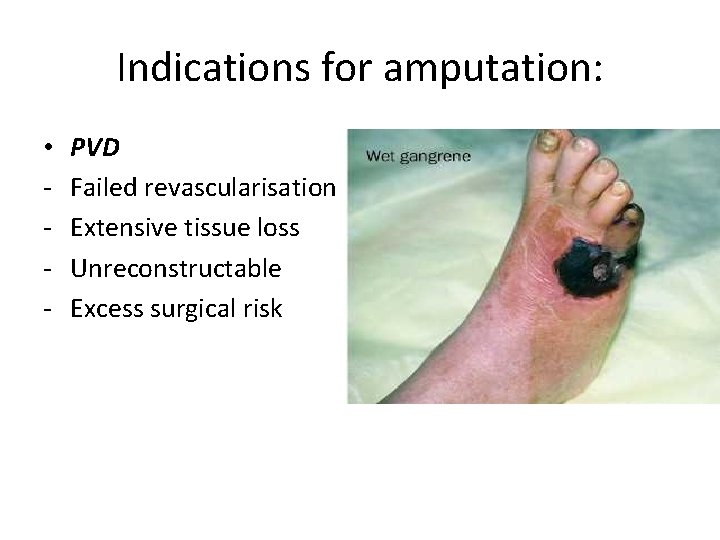
Indications for amputation: • - PVD Failed revascularisation Extensive tissue loss Unreconstructable Excess surgical risk
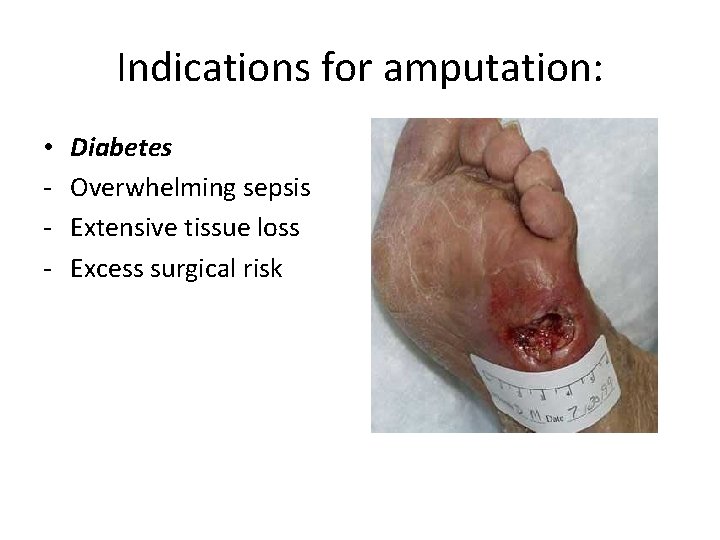
Indications for amputation: • - Diabetes Overwhelming sepsis Extensive tissue loss Excess surgical risk
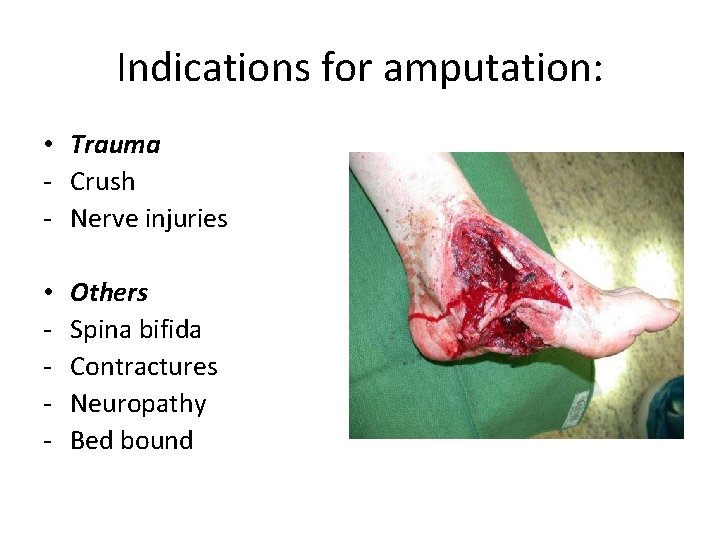
Indications for amputation: • Trauma - Crush - Nerve injuries • - Others Spina bifida Contractures Neuropathy Bed bound
Goals of amputation: • Get rid of all infected, necrotic and painful tissue • Attain successful wound healing • Have an adequate stump for a prosthetic
Attempt limb salvage or primary amputation? • Extent of tissue loss in foot • Anatomy of reconstruction • Associated comorbidities • ESRD with heel gangrene – maybe best treated with primary amputation
Natural history of major amputation: • 10% perioperative mortality • 3 year survival after BKA – 57%; after AKA – 39% • Of 440 major amputations – 75 died in hospital, 113 deemed unsuitable for prosthesis. Of 57% referred for prosthesis – at 3 years follow up a further 54 died, only 1015% were mobile at home. (BJS 1992)
Amputation levels and significance: • Major amputation: above tarso metatarsal joint. • Levels - BKA - Through knee - AKA - Hip disarticulation
Amputation levels and significance: • BKA – maximal rehabilitation potential - 10 -40% increase in energy expenditure - 15 -20% of all BKAs go onto an AKA in 3 years (5% periop mortality) • AKA – less rehab potential - 50 -70% extra energy expenditure - Better rates of healing
Level Selection: • Subjective: - Clinical exam – skin quality, extent of ischemia/ infection - Pulses – presence of a pulse immedietly above the level of amputation – almost 100% chance of healing - “Clinical judgment” alone 80% accurate in predicting healing with BKA and 90% in AKA.
Level Selection: • Wagner et al (J vasc surgery 1988): clinical judgment superior to objective assessments. More distal amputations can be achieved with clinical measures over objective studies. • Clinical judgment is central to amputation level selection.
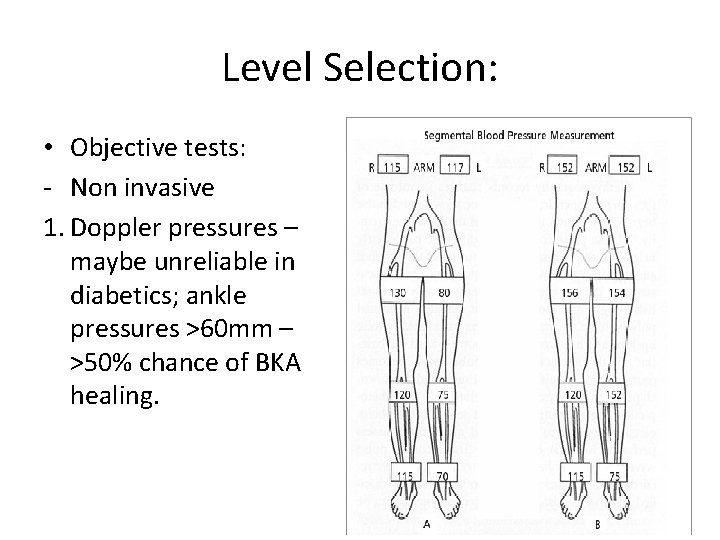
Level Selection: • Objective tests: - Non invasive 1. Doppler pressures – maybe unreliable in diabetics; ankle pressures >60 mm – >50% chance of BKA healing.
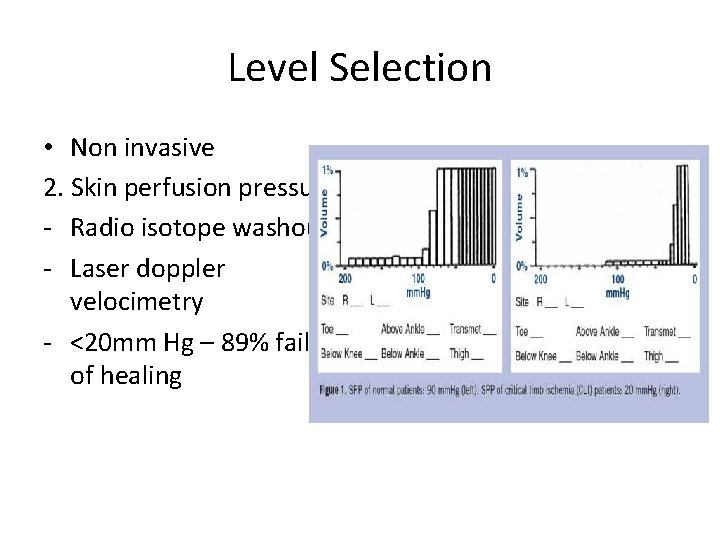
Level Selection • Non invasive 2. Skin perfusion pressures - Radio isotope washout - Laser doppler velocimetry - <20 mm Hg – 89% failure of healing
Level Selection • Non Invasive 3. Transcutaneous oximetry - Tested under local hyperthermia - Correlates with true Pa. O 2 - Threshold value – 30 mm
Level Selection: • Invasive – Angiographic scoring • Poor correlation
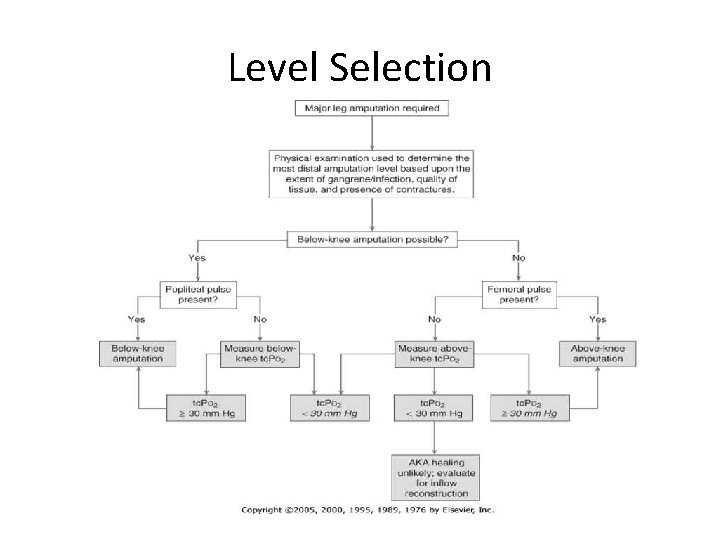
Level Selection
Conclusions: • Amputation is traumatic enough…poor level selection can make it worse. • Clinical judgement central to proper level selection • Patient factors are more important than objective testing
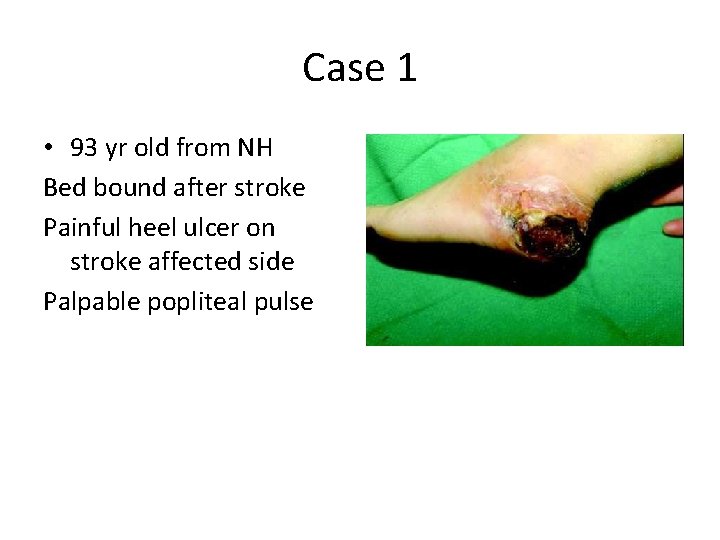
Case 1 • 93 yr old from NH Bed bound after stroke Painful heel ulcer on stroke affected side Palpable popliteal pulse
Case 2 • 68 yr old male CRF on hemodialysis Post surgery for #NOF – bilateral heel ulcers Painful, non healing despite multiple debridements Palpable popliteal pulses
- Slides: 21