Lower Gastrointestinal Tract KNH 411 Lactose and low









- Slides: 39
Lower Gastrointestinal Tract KNH 411

Lactose and low residue

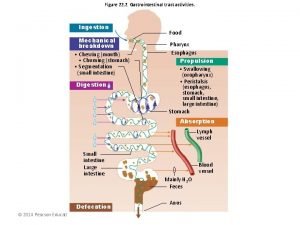
Stimulate acids Insulin release Between meals looking at motility © 2007 Thomson - Wadsworth

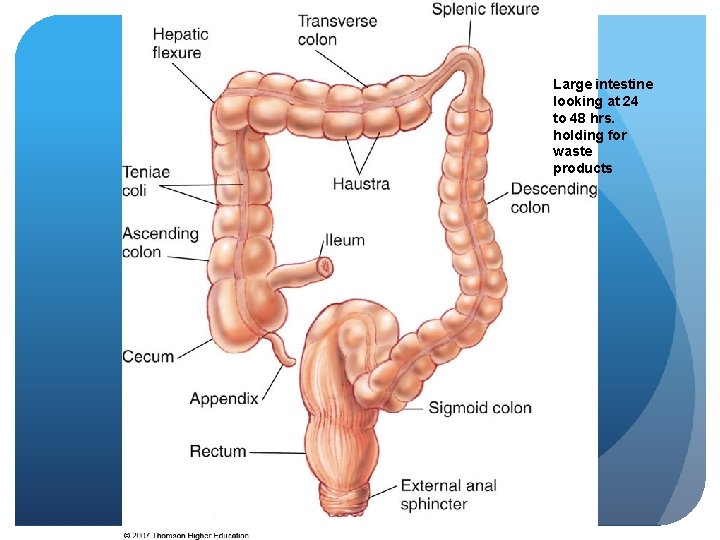
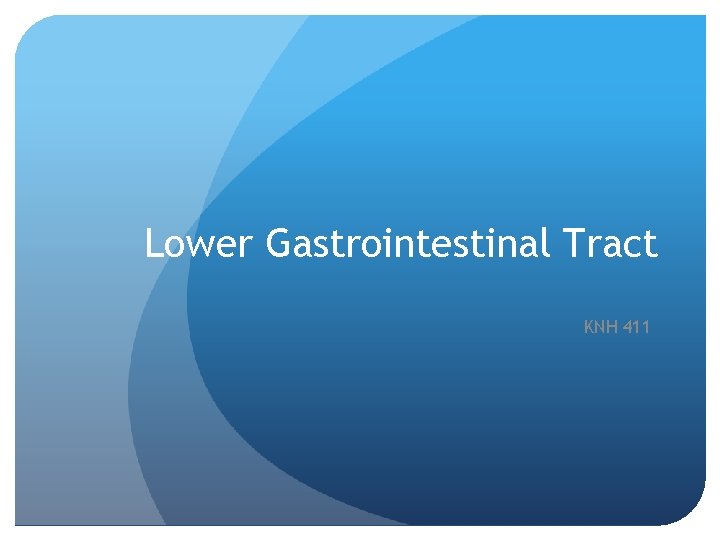
Large intestine looking at 24 to 48 hrs. holding for waste products
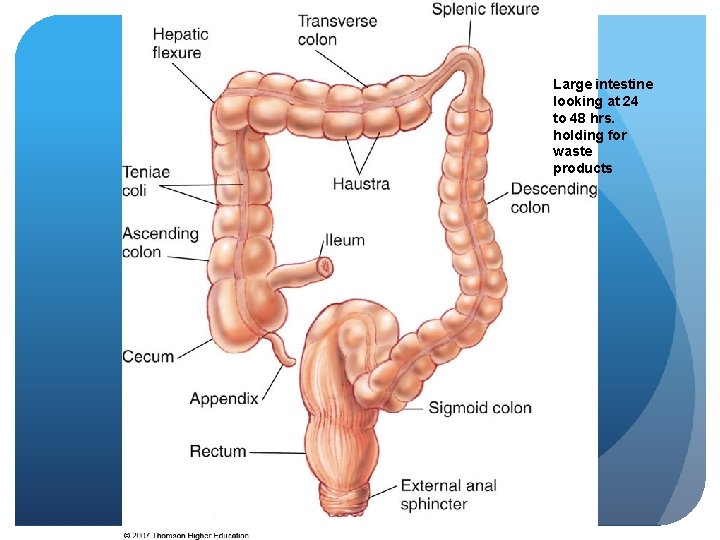
Pathophysiology: Lower GI Tract Malabsorption - maldigestion of fat, CHO, Protein # 1 concern- diarrhea and constipation Decreased villious height, enzyme production Decreased transit time With surgery can alter GI might need rest, decreased use in pancreas or liver
Pathophysiology: Lower GI Tract Malabsorption - fat Steatorrhea – fat travels undigested to large intestine and diarrhea Fat-soluble vitamins malabsorbed- ADE and K Potential for excess oxalate- kidney stones Abdominal pain, cramping, diarrhea Dg; fecal fat test or D-xylose absorption test, or small bowel x-ray
Pathophysiology: Lower GI Tract Malabsorption - Fat – Nutrition Restrict fat 25 -50 g/day Use of MCT supplements w/ infants Pancreatic enzymes- aid w/ malabsorption (chromes) Take before meals
Pathophysiology: Lower GI Tract Malabsorption - CHO Lactose malabsorption Increased gas, abdominal cramping, diarrhea Restrict milk and dairy products Products such as Lactaid can be rec. Celiac’s, Type 2 Diabetics & blood is swimming in sugar and water - concern with gastroperisis dumping syndrome - alcoholic malabsorption of CHO and PRO
Pathophysiology: Lower GI Tract Malabsorption - protein Protein-losing enteropathy- excessive protein loss albumin 21 day ½ life Reduced serum protein Peripheral edema cells cannot hold in water, fluid overload, low onconic pressure pre-albumin has 2 day ½ life which is useful for short term (ICU)
Pathophysiology: Lower GI Tract Malabsorption - Nutrition Therapy Results in weight loss Low vitamins and minerals, chronic PEM Treat underlying disease/ nutrient being malabsorbed
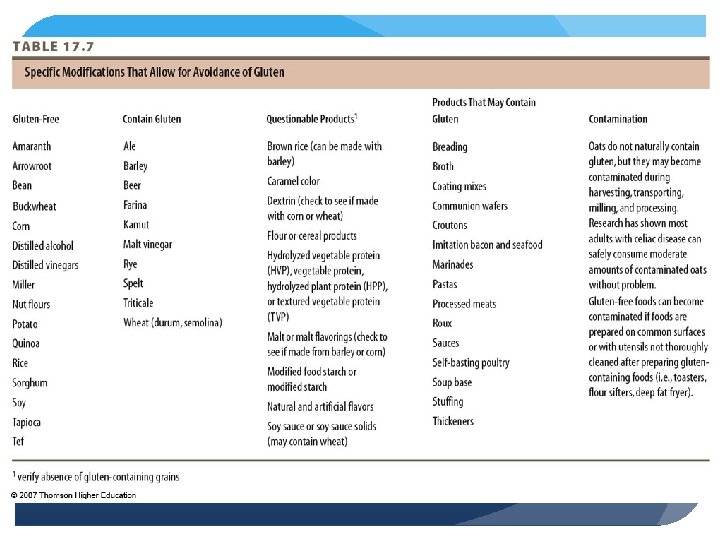
Pathophysiology: Lower GI Tract Celiac disease Damage to lower GI Genetic and autoimmune Occurs when alpha-gliadin from wheat, rye, malt, barley are eaten, can include oats Infiltration of WBC, production of Ig. A antibodies

Pathophysiology: Lower GI Tract Celiac disease - pathophysiology Damage to villi reduce height and flatten Decreased enzyme function Maldigestion and malabsorption Occurs with other autoimmune disorders type 1 diabetes, rheumatoid arthritis, dermatitis

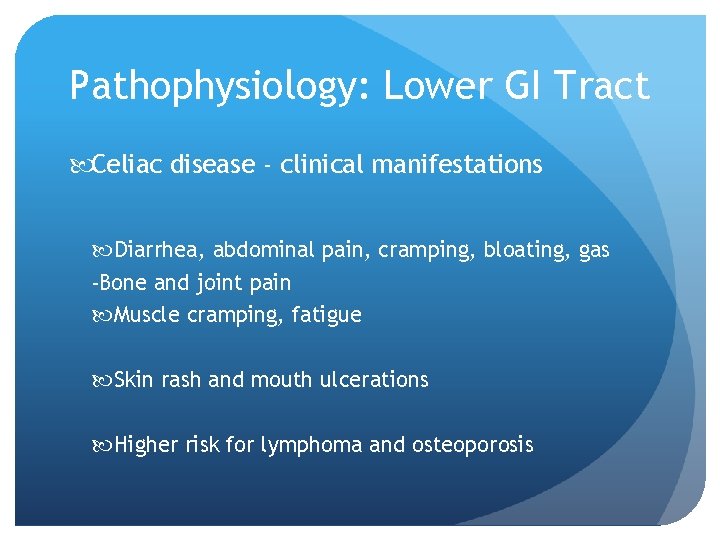
Pathophysiology: Lower GI Tract Celiac disease - clinical manifestations Diarrhea, abdominal pain, cramping, bloating, gas -Bone and joint pain Muscle cramping, fatigue Skin rash and mouth ulcerations Higher risk for lymphoma and osteoporosis
Pathophysiology: Lower GI Tract Celiac Disease - Diagnosis/Treatment/Prognosis Biopsy of small intestinal mucosa Reversal of symptoms following gluten-free diet Refractory CD; d/t coexisting disease
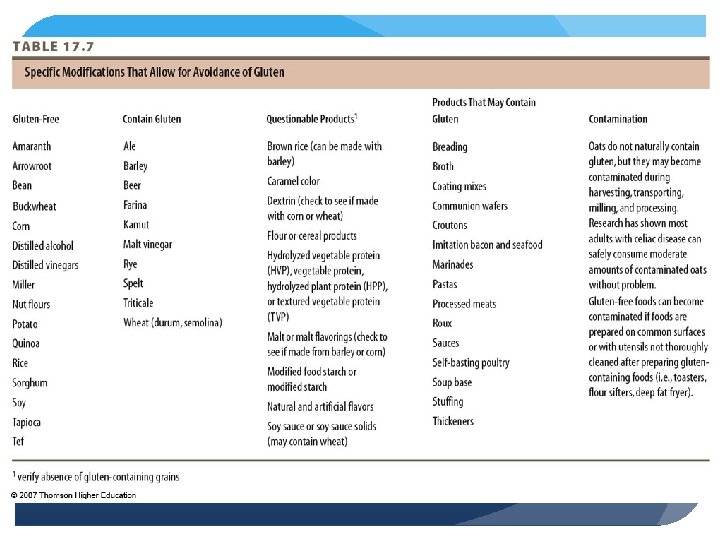
Pathophysiology: Lower GI Tract Celiac Disease - Nutrition Intervention Low-residue, low-fat, lactose-free, gluten-free diet No more than 45 to 55 g/day Identify hidden sources of gluten Specialty products max. allowance of oats ½ cup per day
Pathophysiology: Lower GI Tract Irritable Bowel Syndrome (IBS) - Most common Pain relieved with defecation Onset associated with change in frequency of stool Onset associated with change in form of stool Eliminate “red flag” symptoms
Pathophysiology: Lower GI Tract IBS Most common GI complaint -pain w/ defecation, women most common Etiology unknown Increased serotonin, inflammatory response, abnormal motility, pain Any emotional trauma can trigger
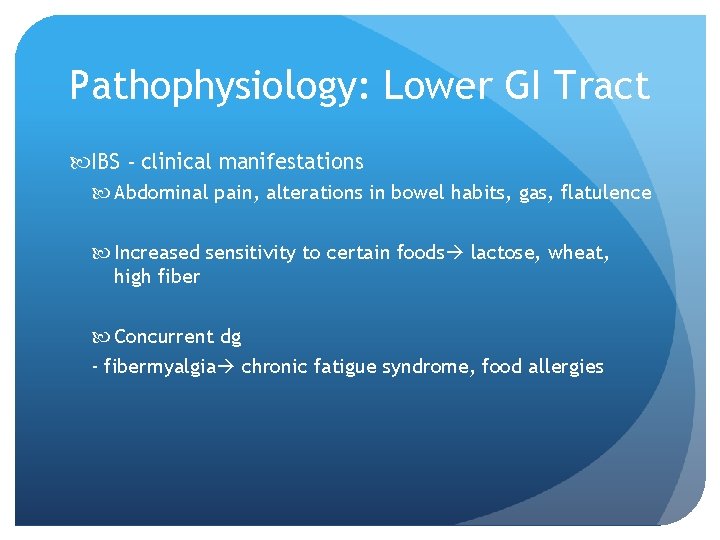
Pathophysiology: Lower GI Tract IBS - clinical manifestations Abdominal pain, alterations in bowel habits, gas, flatulence Increased sensitivity to certain foods lactose, wheat, high fiber Concurrent dg - fibermyalgia chronic fatigue syndrome, food allergies
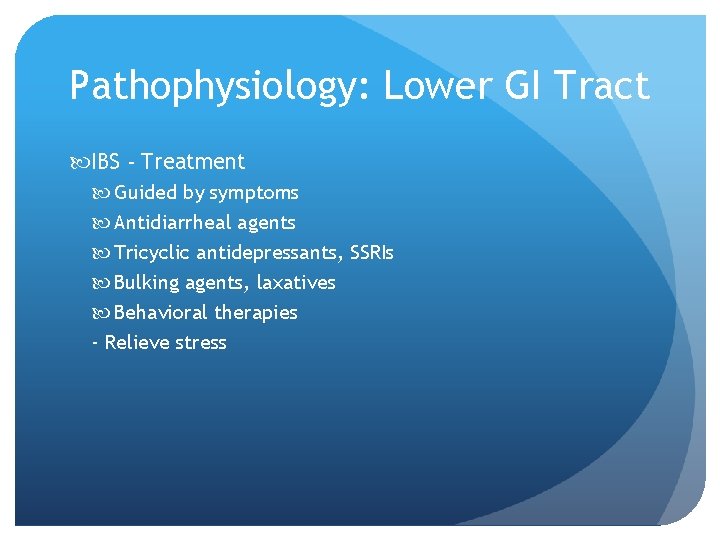
Pathophysiology: Lower GI Tract IBS - Treatment Guided by symptoms Antidiarrheal agents Tricyclic antidepressants, SSRIs Bulking agents, laxatives Behavioral therapies - Relieve stress

Pathophysiology: Lower GI Tract IBS - Nutrition Therapy Can lead to nutrient deficiency, underweight - Due to constant pain and depression Decrease anxiety, issues with trying to normalize dietary patterns
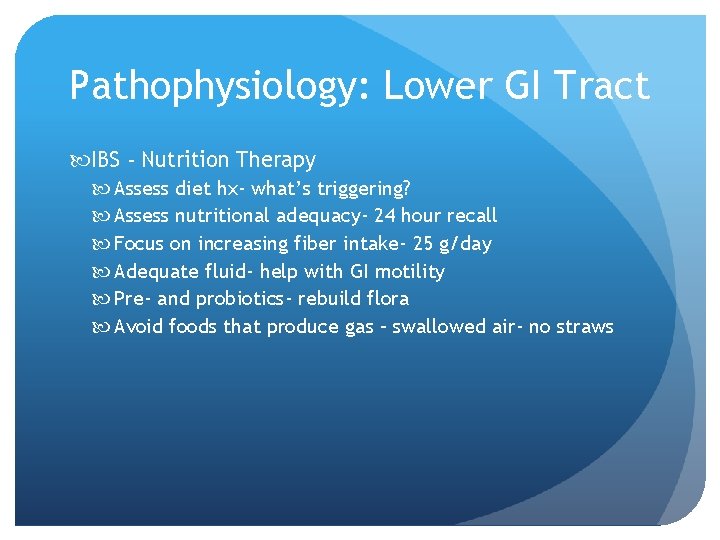
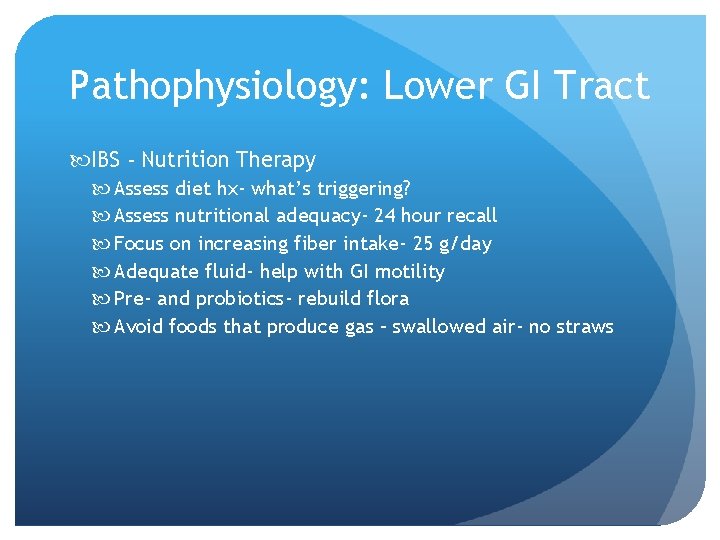
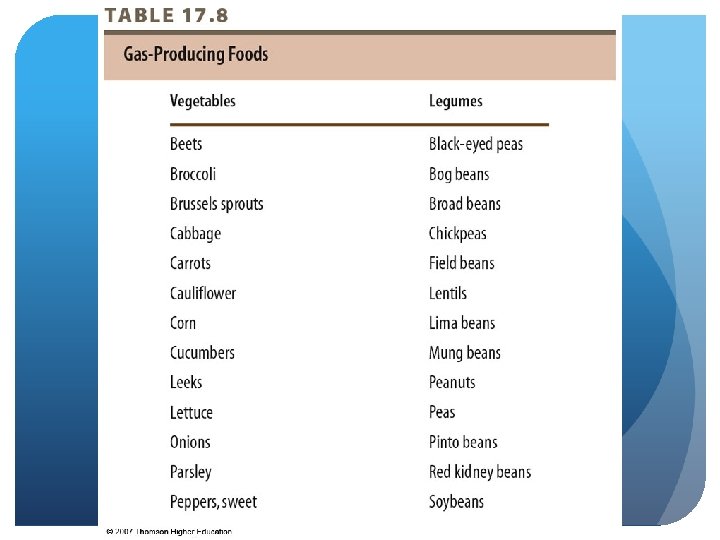
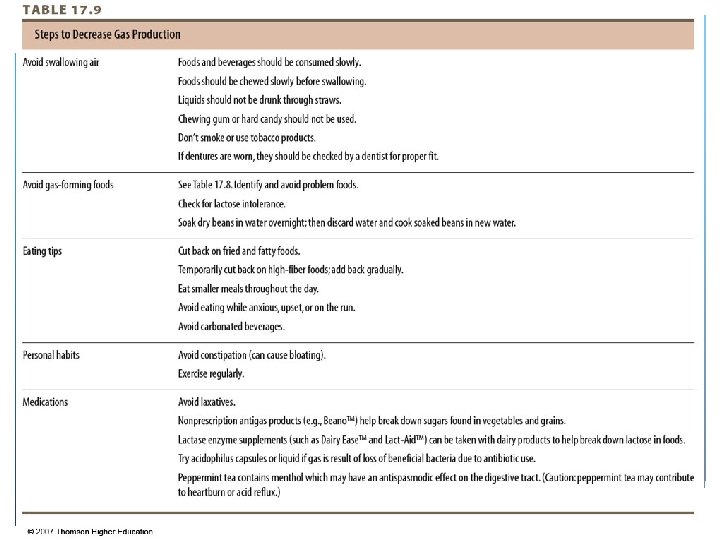
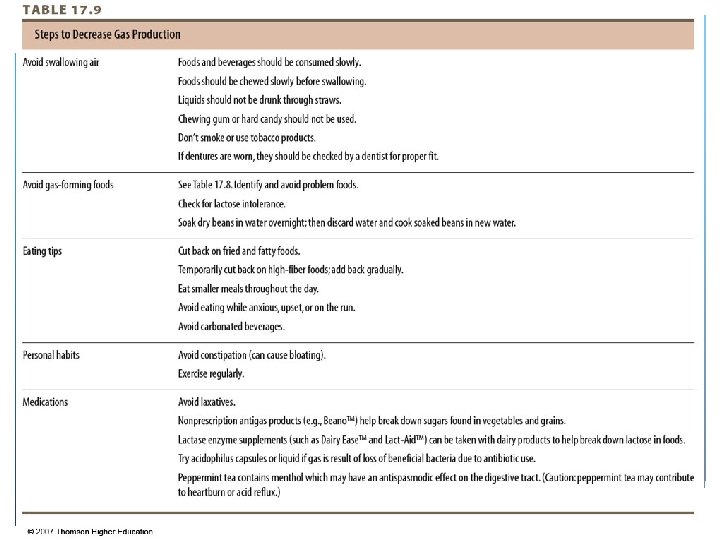
Pathophysiology: Lower GI Tract IBS - Nutrition Therapy Assess diet hx- what’s triggering? Assess nutritional adequacy- 24 hour recall Focus on increasing fiber intake- 25 g/day Adequate fluid- help with GI motility Pre- and probiotics- rebuild flora Avoid foods that produce gas – swallowed air- no straws

© 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth

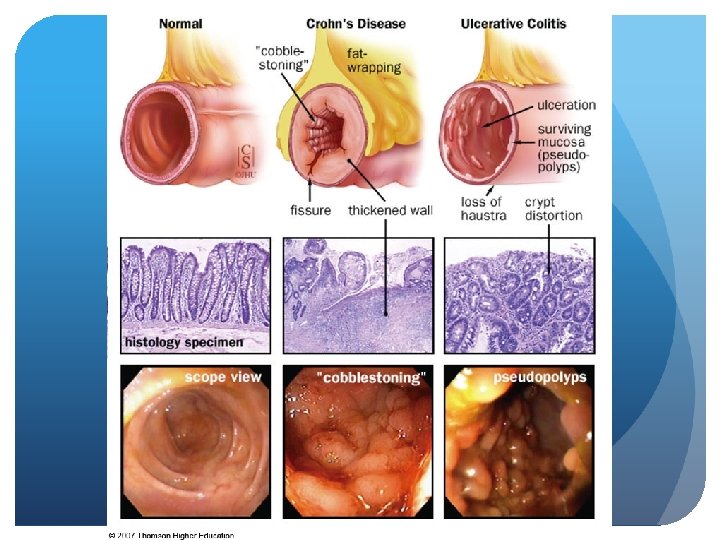
Pathophysiology: Lower GI Tract IBD - Nutrition Therapy Malnutrition May need to increase kcal, protein, micronutrients low Key: iron, zinc, magnesium, electrolytes (K, Na, Cl)
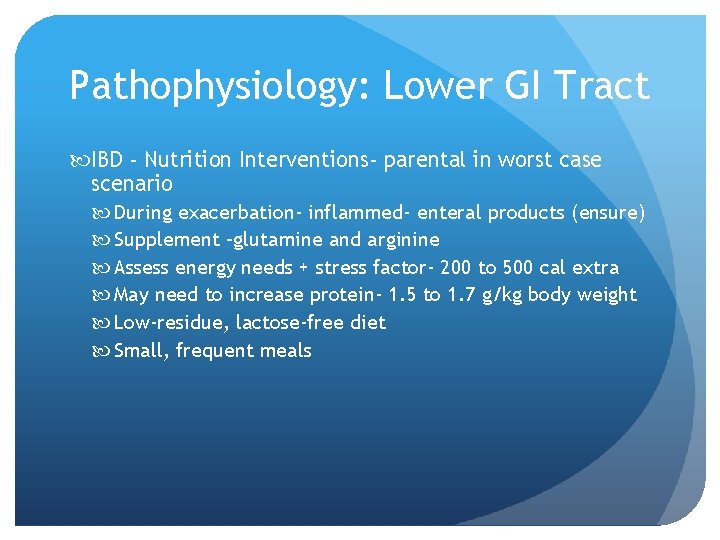
Pathophysiology: Lower GI Tract IBD - Nutrition Interventions- parental in worst case scenario During exacerbation- inflammed- enteral products (ensure) Supplement –glutamine and arginine Assess energy needs + stress factor- 200 to 500 cal extra May need to increase protein- 1. 5 to 1. 7 g/kg body weight Low-residue, lactose-free diet Small, frequent meals
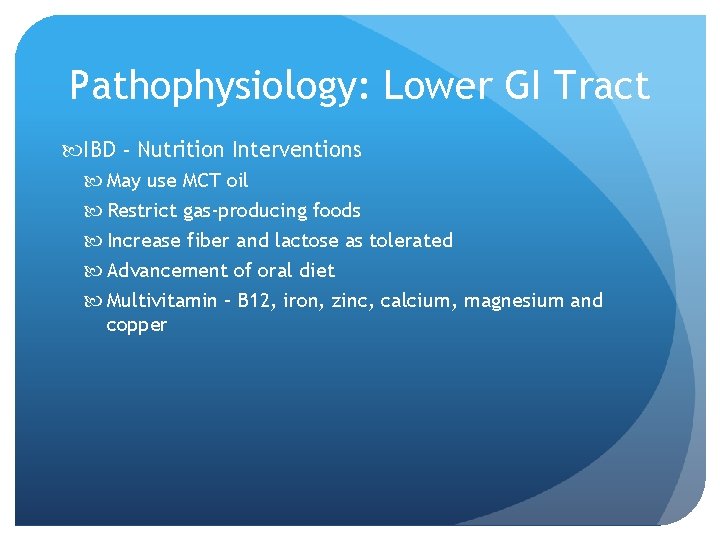
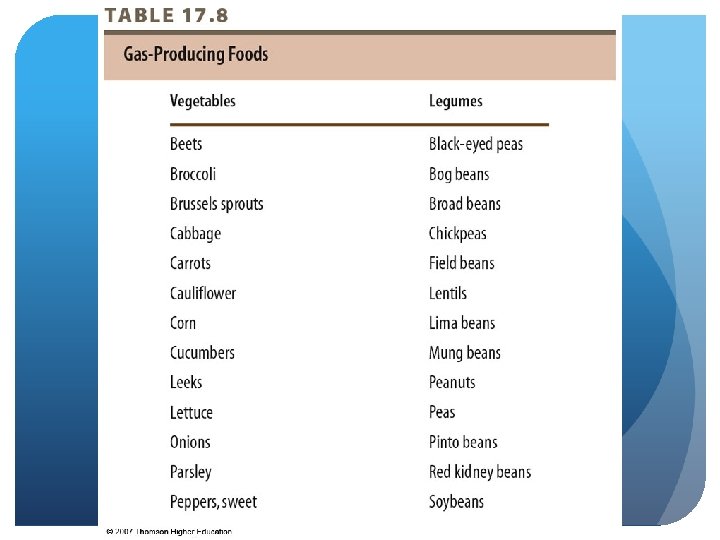
Pathophysiology: Lower GI Tract IBD - Nutrition Interventions May use MCT oil Restrict gas-producing foods Increase fiber and lactose as tolerated Advancement of oral diet Multivitamin – B 12, iron, zinc, calcium, magnesium and copper
Pathophysiology: Lower GI Tract IBD - Nutrition Interventions During remission/rehabilitation Maximize energy & protein Weight gain and physical activity Food sources of antioxidants, Omega-3 s Pro- and prebiotics
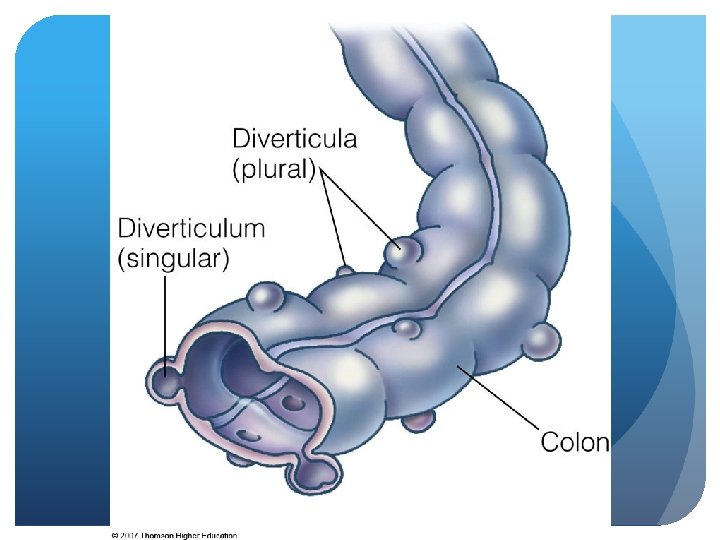
Pathophysiology: Lower GI Tract Diverticulosis/diverticulitis – abnormal presence of outpockets or pouches on surface of SI or colon/inflammation of these Low fiber intake Increases inflammatory response Other risks - strong history of cigarettes, obesity, sedentary lifestyle, caffeine
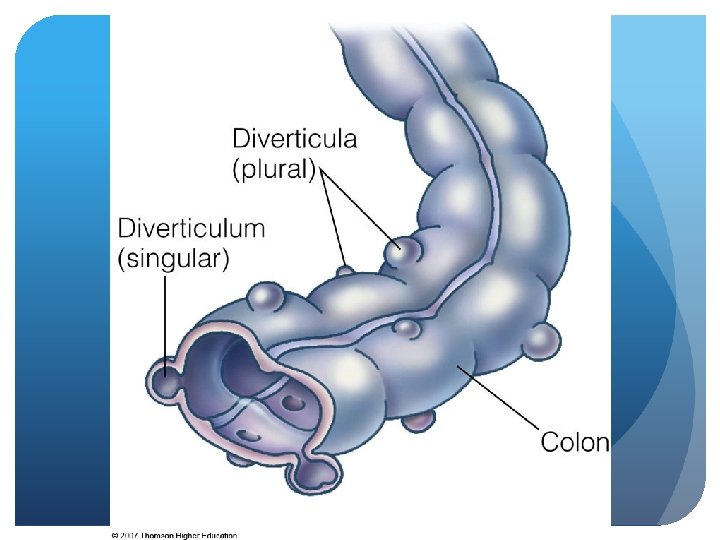
Pathophysiology: Lower GI Tract Diverticulosis/diverticulitis – pathophysiology Fecal matter trapped Development of pouches Diverticulitis Food stuff Bleeding abscess, obstruction, fistula, perforation

Pathophysiology: Lower GI Tract Diverticulosis/-itis – Treatment/ Nutrition Therapy Specific focus on fiber Pro- and prebiotic supplementation Acute Antibiotics - Nothing by mouth, clear liquids, food liquids, reg. diet
Pathophysiology: Lower GI Tract Diverticulosis/-itis – Nutrition Therapy -osis Avoid nuts, seeds, hulls Fiber supplement- add 6 to 10 g total to current rec. for fiber -itis Bowel rest Avoid nuts, seeds, fibrous vegetables - May not be as concerned
 Gastrointestinal tract
Gastrointestinal tract Chemotrypsinogen
Chemotrypsinogen Gastrointestinal tract
Gastrointestinal tract Human alimentary canal diagram class 10
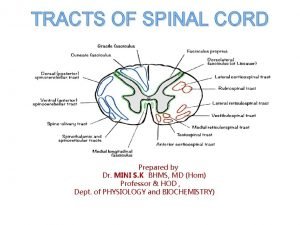
Human alimentary canal diagram class 10 Extrapyramidal tract names
Extrapyramidal tract names Anterior spinothalamic tract
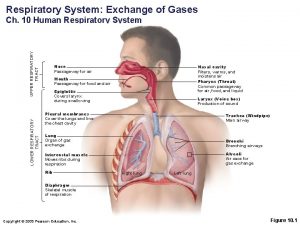
Anterior spinothalamic tract Upper and lower respiratory tract
Upper and lower respiratory tract Respiratory system maintain homeostasis
Respiratory system maintain homeostasis Knh
Knh Knh
Knh Lower respiratory tract
Lower respiratory tract Pneumonia classification
Pneumonia classification Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Reflective style of communication
Reflective style of communication Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Gastrointestinal hormones
Gastrointestinal hormones Dr sigit djuniawan
Dr sigit djuniawan Sinal de lichtenberg medicina legal
Sinal de lichtenberg medicina legal Pankreatik polipeptid
Pankreatik polipeptid Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Focused physical assessment
Focused physical assessment Cloaca
Cloaca Motilidad gastrointestinal
Motilidad gastrointestinal Dumping syndrome signs
Dumping syndrome signs Qual a função do sistema digestório
Qual a função do sistema digestório Identifique
Identifique Gastrointestinal disease
Gastrointestinal disease Sublingual ilaç uygulaması
Sublingual ilaç uygulaması Intestinal villus
Intestinal villus Gastrointestinal
Gastrointestinal Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Hirschsprung disease nursing management
Hirschsprung disease nursing management Nursing management of gastrointestinal disorders
Nursing management of gastrointestinal disorders Mid low high
Mid low high Low accuracy low precision
Low accuracy low precision Low voltage = low hazard
Low voltage = low hazard Structure of sucrose maltose and lactose
Structure of sucrose maltose and lactose Lactose test strips
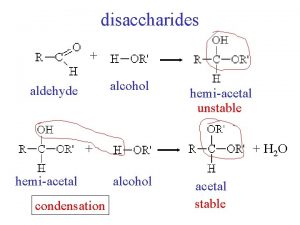
Lactose test strips Does lactose have a hemiacetal group
Does lactose have a hemiacetal group