LOWER FEMALE GENITAL TRACT INFECTIONS Defence Mechanism Against


- Slides: 42
LOWER FEMALE GENITAL TRACT INFECTIONS
Defence Mechanism Against Ascent of Infection (Natural Barrier) l Vulva: ¡ ¡ l Vagina: ¡ ¡ l l Apocrine glands: modified sweat glands → fungicidal acid Apposition of labia closes introitus Apposition of anterior and posterior walls Stratified squamous epithelium resistant to infection Vaginal acidity Flora: the G+ve Doderlein’s bacilli splits glycogen into lactic acid Cervix: closed by bacteriolytic cervical mucus Uterus: Periodic endometrial shedding during menstruation eliminates any infection
Variations in The Efficacy of Defence Mechanism l With Age: During childhood and after the menopause Estrogen deficiency → glycogen and Doderlein bacilli → absent vaginal acidity. ¡ Endometrium poorly developed or atrophic and does not undergo cyclic shedding. ¡ l With menstruation: ¡ ¡ Absent cervical mucus plug Lowered vaginal acidity by alkaline menstruation.
Variations in The Efficacy of Defence Mechanism l During the puerperium: Uterus, cervix & vagina widely opened ¡ Vaginal acidity neutralized by alkaline lochia ¡ Raw placental site ¡ Lacerations ¡ Low general resistance ¡
VAGINITIS PRIMARY VAGINITIS l During childhood: Vulvovaginitis of children l During the reproductive period: ¡ ¡ ¡ l Trichomonas infection Monilia infection Bacterial vaginosis Puerperal infection Others; Gonococcal, T. B. syphilis, bilharziasis Post menopausal: Senile vaginitis
VAGINITIS SECONDARY VAGINITIS l Spread from ¡ Urinary conditions: Vesico-vaginal fistula ¡ Rectal conditions: Recto-vaginal fistula and complete perineal tear l Mechanical irritation (pessary or tampon) l Chemical irritation (drugs and douches)
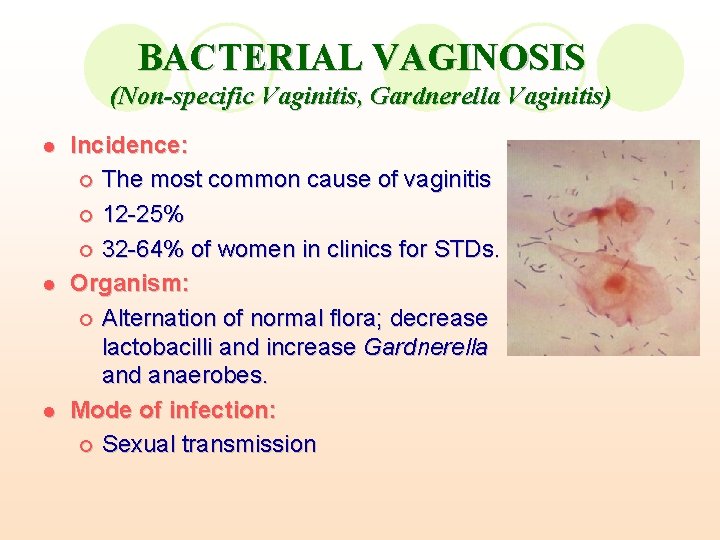
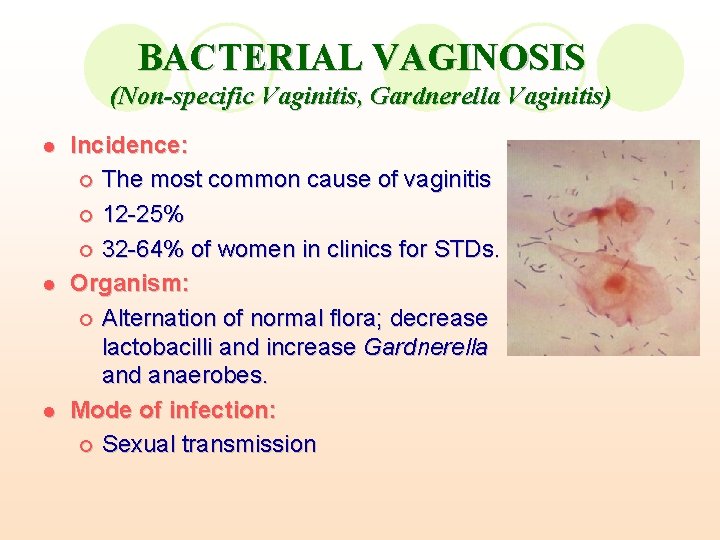
BACTERIAL VAGINOSIS (Non-specific Vaginitis, Gardnerella Vaginitis) l l l Incidence: ¡ The most common cause of vaginitis ¡ 12 -25% ¡ 32 -64% of women in clinics for STDs. Organism: ¡ Alternation of normal flora; decrease lactobacilli and increase Gardnerella and anaerobes. Mode of infection: ¡ Sexual transmission
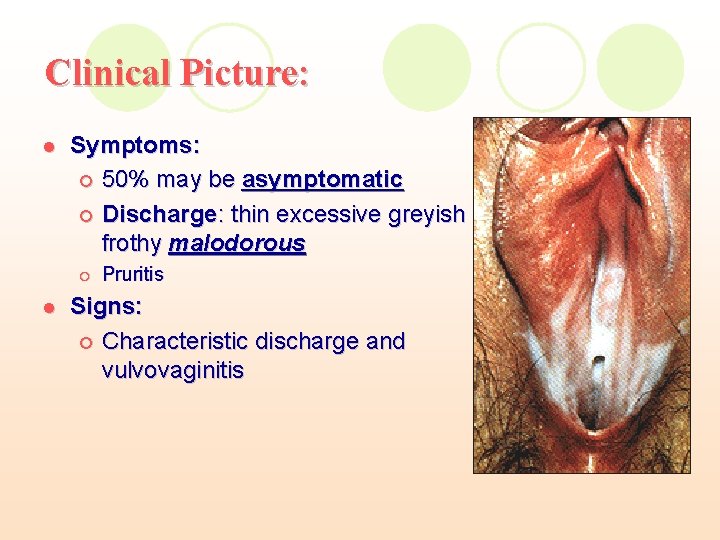
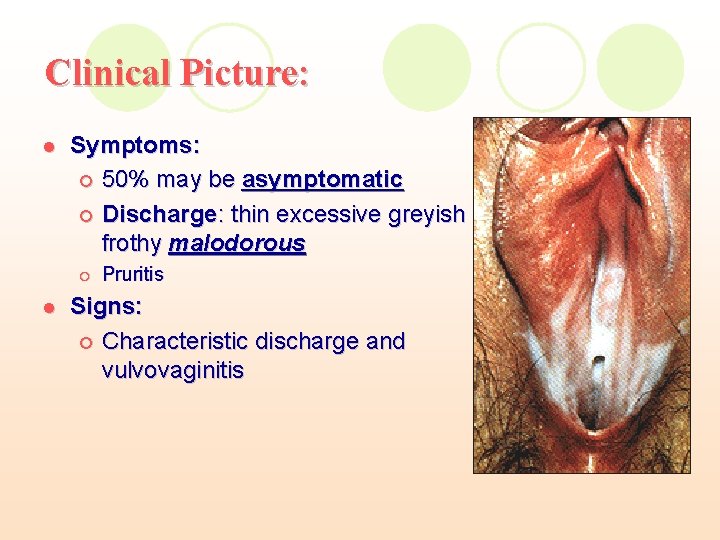
Clinical Picture: l Symptoms: ¡ 50% may be asymptomatic ¡ Discharge: thin excessive greyish frothy malodorous ¡ l Pruritis Signs: ¡ Characteristic discharge and vulvovaginitis
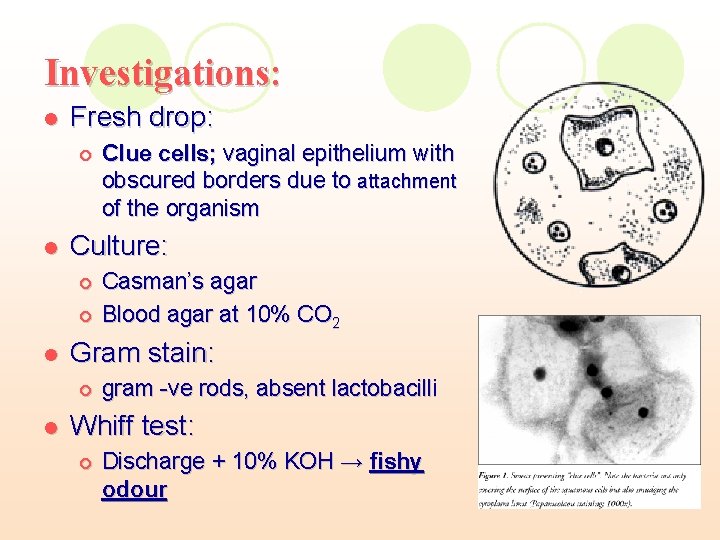
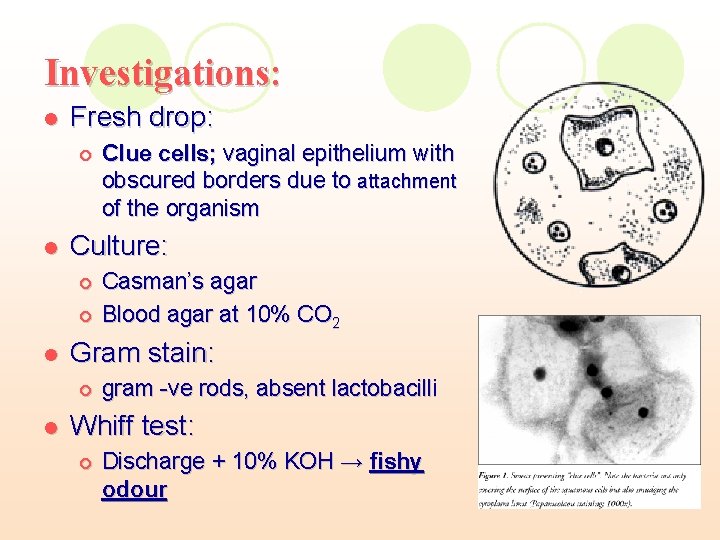
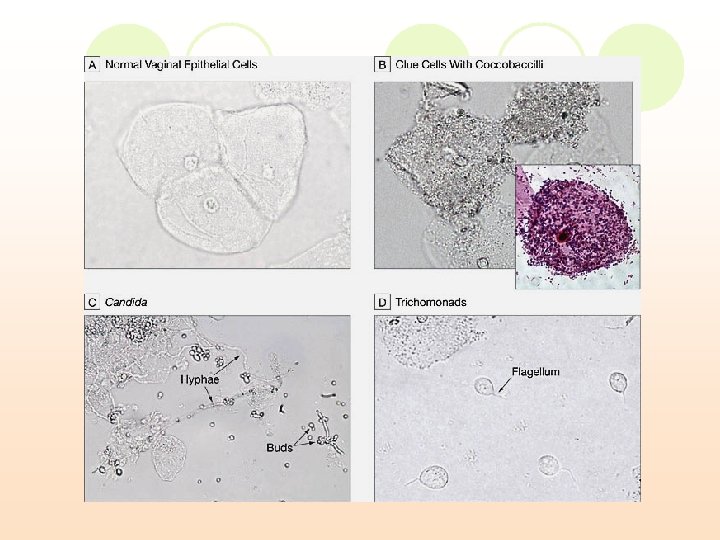
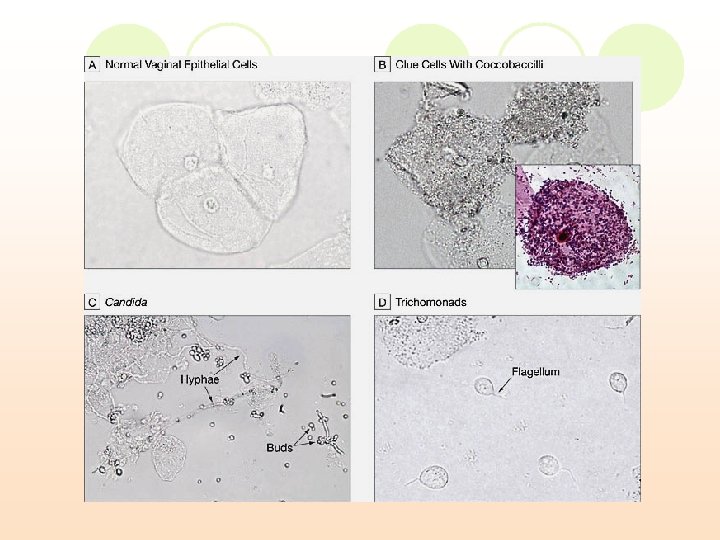
Investigations: l Fresh drop: ¡ l Culture: ¡ ¡ l Casman’s agar Blood agar at 10% CO 2 Gram stain: ¡ l Clue cells; vaginal epithelium with obscured borders due to attachment of the organism gram -ve rods, absent lactobacilli Whiff test: ¡ Discharge + 10% KOH → fishy odour
Diagnosis: l Amsel’s ¡ ¡ l l criteria: (3 of the following criteria) Thin homogeneous discharge on examination. p. H of discharge > 4. 5. Whiff test: vaginal discharge + 10% KOH → "aminelike" or "fishy" odor. Clue cells on microscopy, Gram-stained vaginal smear Culture of vaginal secretions has no place in the diagnosis of BV.
Treatment: A) Intravaginal preparations; Clindamycin cream 2% at bed time for 7 days Metronidazole once daily for 5 days l B) Oral regimens: Metronidazole as a single 2 gm dose Clindamycin 300 mg twice daily for 7 days l C) Sexual partner should be treated if infection is recurrent l D) During pregnancy; Clindamycin may be used throughout pregnancy Metronidazole may be used after the first trimester l
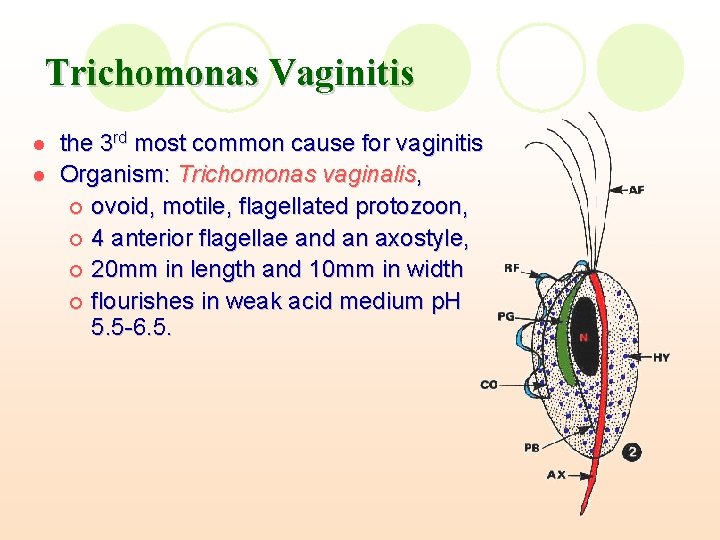
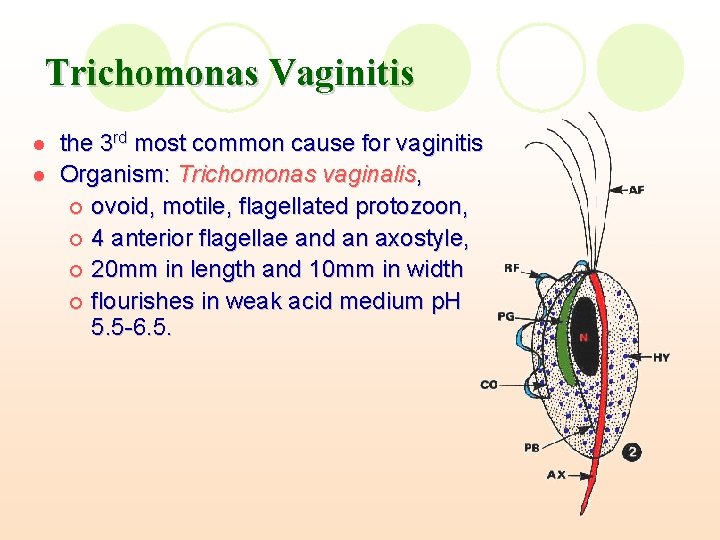
Trichomonas Vaginitis l l the 3 rd most common cause for vaginitis Organism: Trichomonas vaginalis, ¡ ovoid, motile, flagellated protozoon, ¡ 4 anterior flagellae and an axostyle, ¡ 20 mm in length and 10 mm in width ¡ flourishes in weak acid medium p. H 5. 5 -6. 5.
Trichomonas Vaginitis l Sites of infection: ¡ l Vagina, urethra, Skene’s tubules, bladder and cervix Mode of infection: Sexual intercourse ¡ Contaminated towels and instruments ¡
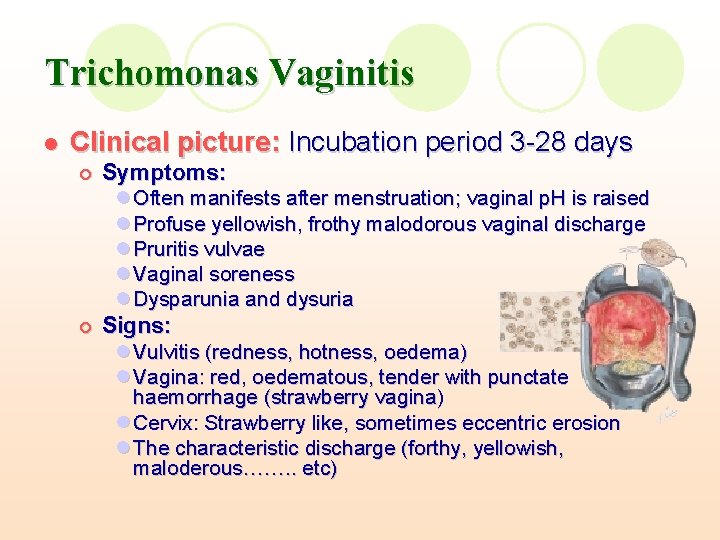
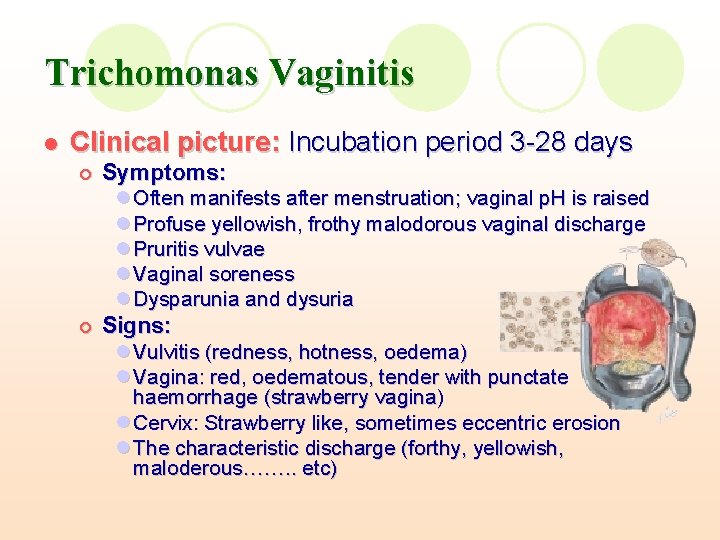
Trichomonas Vaginitis l Clinical picture: Incubation period 3 -28 days ¡ Symptoms: l Often manifests after menstruation; vaginal p. H is raised l Profuse yellowish, frothy malodorous vaginal discharge l Pruritis vulvae l Vaginal soreness l Dysparunia and dysuria ¡ Signs: l Vulvitis (redness, hotness, oedema) l Vagina: red, oedematous, tender with punctate haemorrhage (strawberry vagina) l Cervix: Strawberry like, sometimes eccentric erosion l The characteristic discharge (forthy, yellowish, maloderous……. . etc)
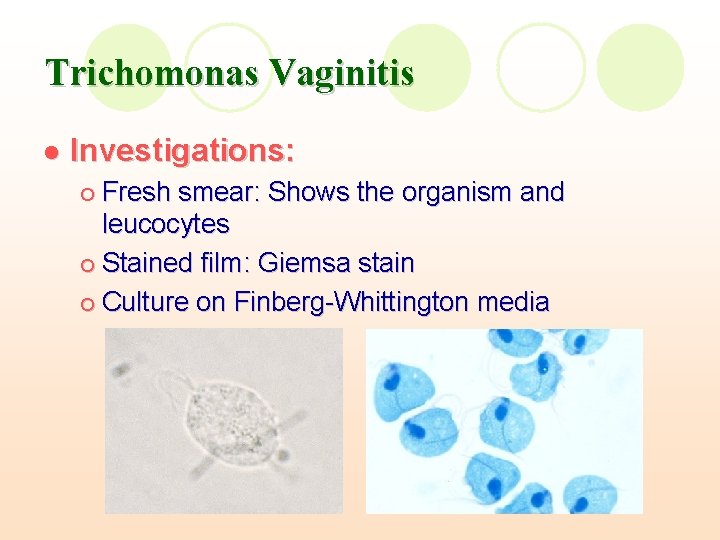
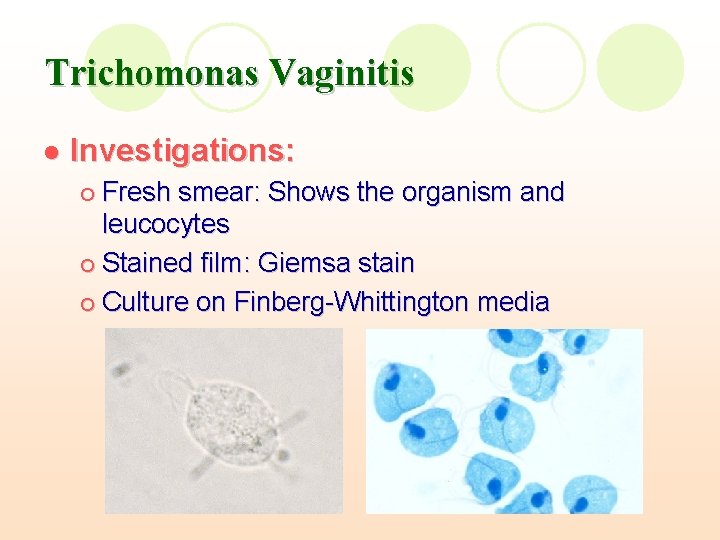
Trichomonas Vaginitis l Investigations: Fresh smear: Shows the organism and leucocytes ¡ Stained film: Giemsa stain ¡ Culture on Finberg-Whittington media ¡
Trichomonas Vaginitis l Treatment: ¡ Metronidazole tablets (Flagyl): l 500 mg/12 h for 10 days OR l 2 gm single dose ¡ Protozole and Tinedazole: l 2 gm single dose Clotrimazole, vaginal pessaries used during pregnancy and lactation in stead of metronidazole. ¡ The husband should be treated at the same time ¡
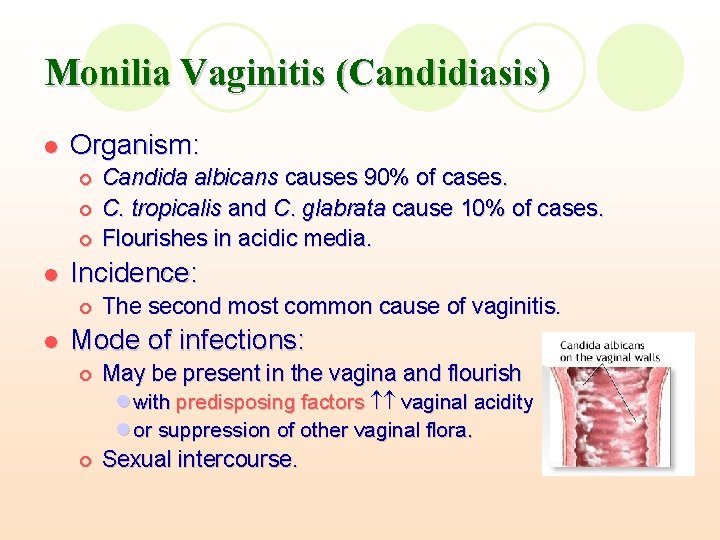
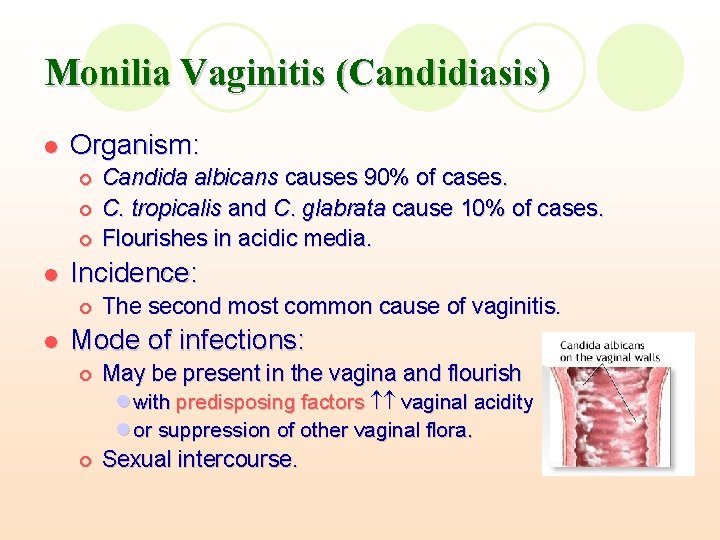
Monilia Vaginitis (Candidiasis) l Organism: ¡ ¡ ¡ l Incidence: ¡ l Candida albicans causes 90% of cases. C. tropicalis and C. glabrata cause 10% of cases. Flourishes in acidic media. The second most common cause of vaginitis. Mode of infections: ¡ May be present in the vagina and flourish l with predisposing factors vaginal acidity l or suppression of other vaginal flora. ¡ Sexual intercourse.
Predisposing factors: l l l l Antibiotics → the lactobacilli that Candida growth Oral contraceptives → glycogen Pregnancy high oestrogen level → glycogen Steroids and immunosuppressives lower immunity Male partner infection Diabetes → glycogen deposition and low immunity Lack of proper hygiene
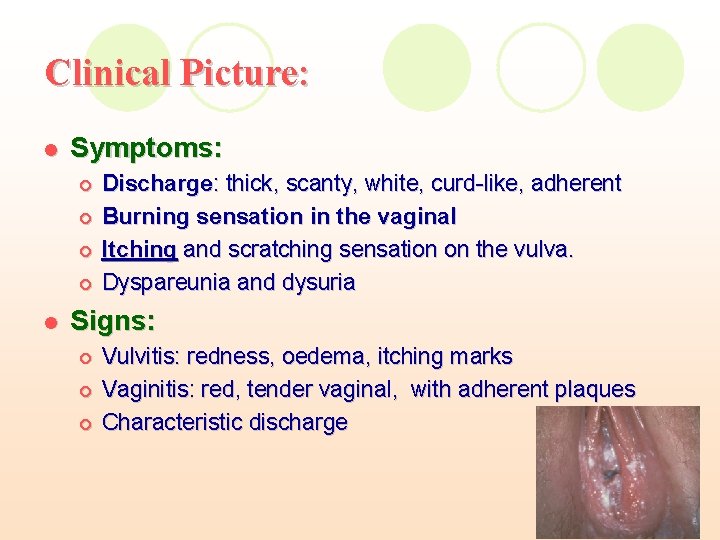
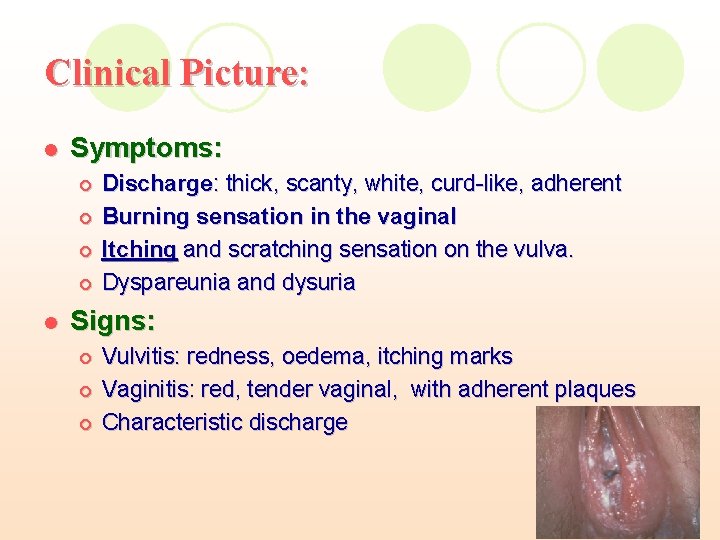
Clinical Picture: l Symptoms: ¡ ¡ l Discharge: thick, scanty, white, curd-like, adherent Burning sensation in the vaginal Itching and scratching sensation on the vulva. Dyspareunia and dysuria Signs: ¡ ¡ ¡ Vulvitis: redness, oedema, itching marks Vaginitis: red, tender vaginal, with adherent plaques Characteristic discharge
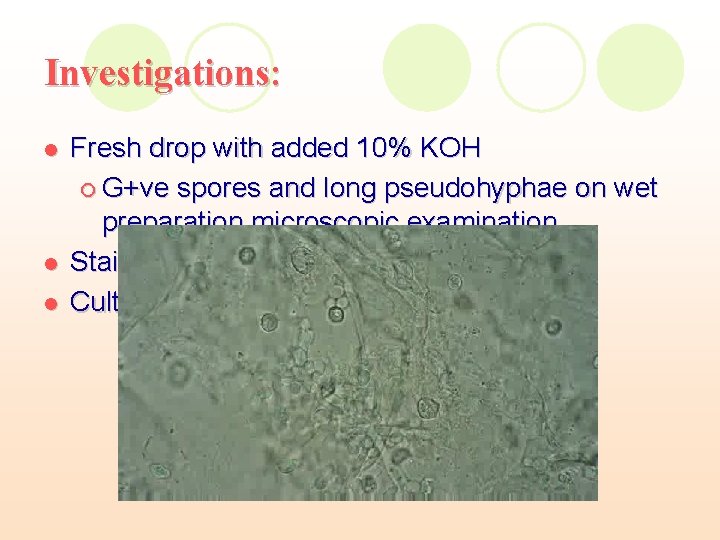
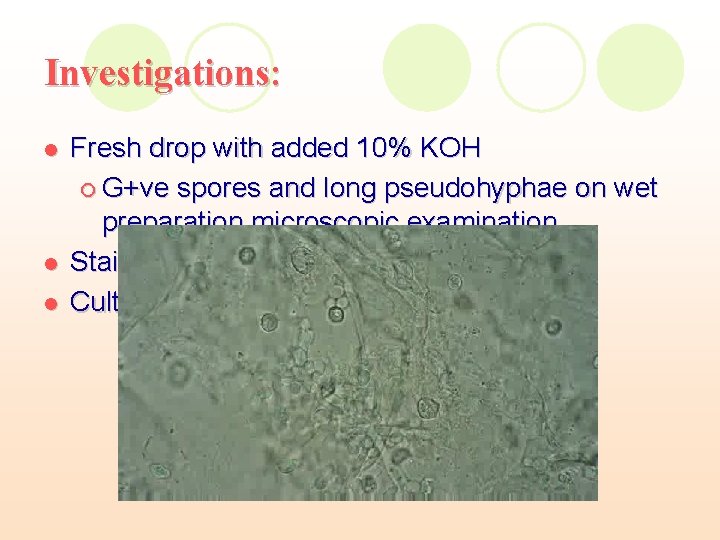
Investigations: l l l Fresh drop with added 10% KOH ¡ G+ve spores and long pseudohyphae on wet preparation microscopic examination. Stained film with methylene blue Culture of Feinberg-Whittington media

Treatment: ¡ Oral antifungal treatment Fluconazole; Single oral dose 150 mg, for treatment of uncomplicated cases Ketoconazole; 200 mg twice a day for 5 days, for recurrent cases. Treatment can be repeated on special schedules along a period of 3 -6 months, for chronic cases. ¡ l l Vaginal Antifungal preparations l Vaginal suppositories or intravaginal creams with special applicator available as either a single dose, a 3 -day course, or a 7 -day course l Agents include clotrimazole, miconazole, and tioconazole preparations

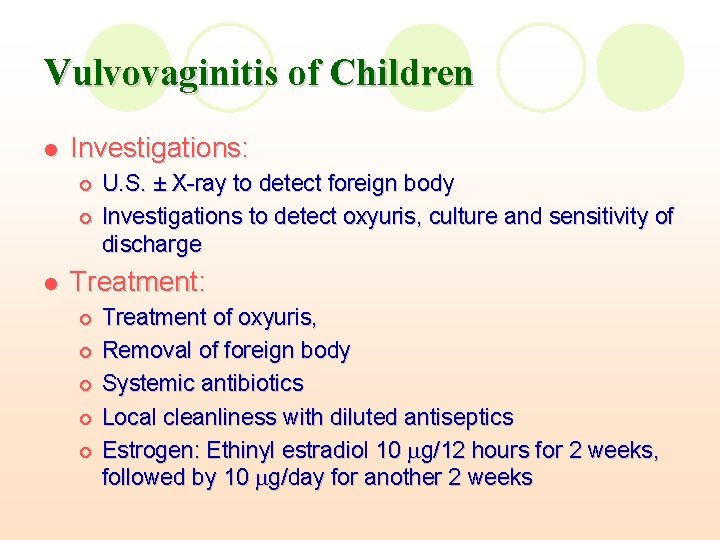
Vulvovaginitis of Children l Microorganism: ¡ l Predisposing factors: ¡ ¡ ¡ l l E. coli, Strept, Staph, gonococci, Candida, Trichomonas Foreign body (oxyuris) Decreased vaginal acidity Poor hygiene Mode of infection: Infected towels Clinical picture: ¡ Symptoms: l Purulent, sometimes bloody, vaginal discharge, l Itching, pain, sometimes dysuria ¡ Signs: l Foul discharge, vulvitis, vaginitis
Vulvovaginitis of Children l Investigations: ¡ ¡ l U. S. ± X-ray to detect foreign body Investigations to detect oxyuris, culture and sensitivity of discharge Treatment: ¡ ¡ ¡ Treatment of oxyuris, Removal of foreign body Systemic antibiotics Local cleanliness with diluted antiseptics Estrogen: Ethinyl estradiol 10 g/12 hours for 2 weeks, followed by 10 g/day for another 2 weeks
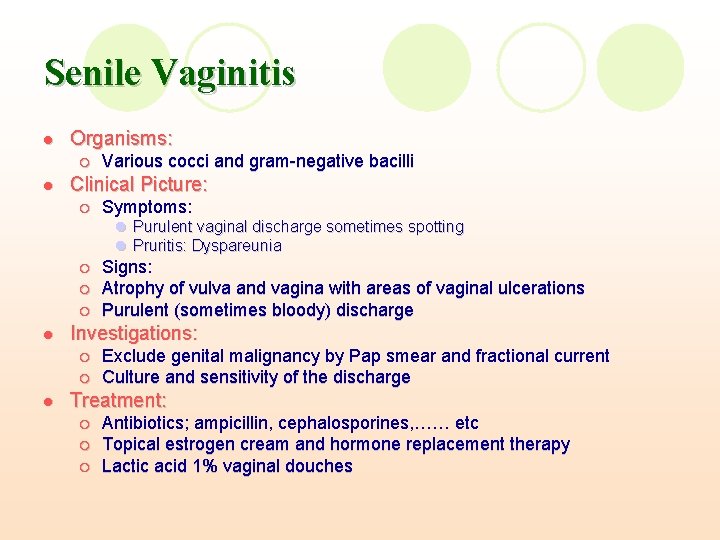
Senile Vaginitis l Organisms: ¡ l Various cocci and gram-negative bacilli Clinical Picture: ¡ Symptoms: l Purulent vaginal discharge sometimes spotting l Pruritis: Dyspareunia ¡ ¡ ¡ l Investigations: ¡ ¡ l Signs: Atrophy of vulva and vagina with areas of vaginal ulcerations Purulent (sometimes bloody) discharge Exclude genital malignancy by Pap smear and fractional current Culture and sensitivity of the discharge Treatment: ¡ ¡ ¡ Antibiotics; ampicillin, cephalosporines, …… etc Topical estrogen cream and hormone replacement therapy Lactic acid 1% vaginal douches
Acute Cervicitis Acute inflammation of the endocervical glands and underlying tissues. l Cause: l Gonococcal ¡ Chlamydial ¡ Puerperal ¡ Post-abortive ¡ Post-operative infection, after instrumentation or cervical dilatations, cauterization or trachelorraphy (i. e. repair of a lacerated cervix) ¡
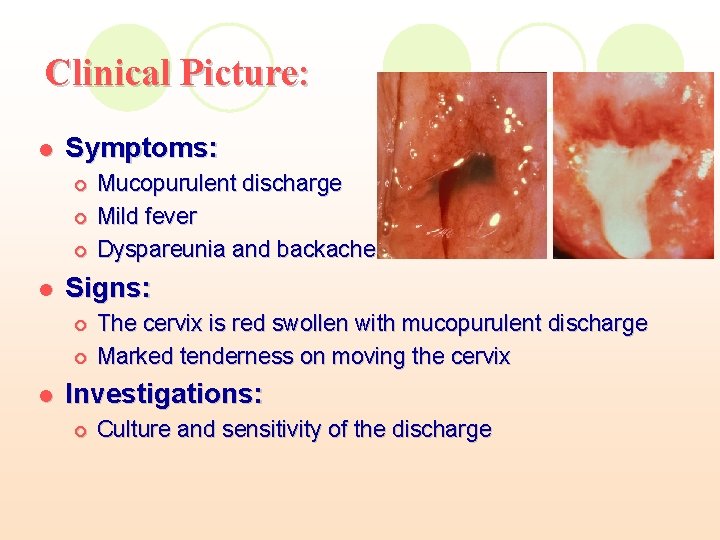
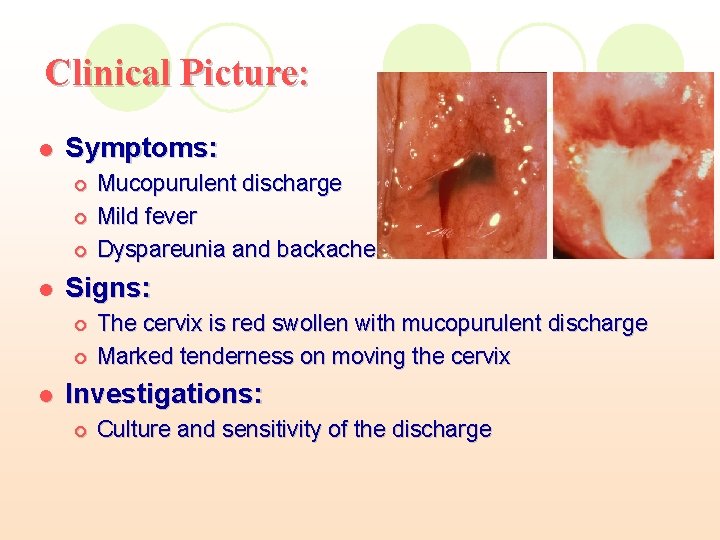
Clinical Picture: l Symptoms: ¡ ¡ ¡ l Signs: ¡ ¡ l Mucopurulent discharge Mild fever Dyspareunia and backache The cervix is red swollen with mucopurulent discharge Marked tenderness on moving the cervix Investigations: ¡ Culture and sensitivity of the discharge
Acute Cervicitis l l Treatment: ¡ Antibiotics , according to organism (broad spectrum) Complications: ¡ Commonly turns chronic infection due to the racemose nature of the cervical glands ¡ Secondary vaginitis ¡ Spread to: lupper genital tract lparametrium lurinary tract
Chronic Cervicitis CLINICAL PICTURE: l Symptoms ¡ Mucopurulent discharge ¡ Congestive dysmenorrhea and menorrhagia (pelvic congestion) ¡ Backache (spread of infection along the uterosacral ligament) ¡ Contact bleeding (cervical erosion) ¡ Dyspareunia (parametritis) ¡ Infertility (hostile cervical discharge) ¡ Frequency of micturition (cystitis) ¡ Manifestations of septic focus
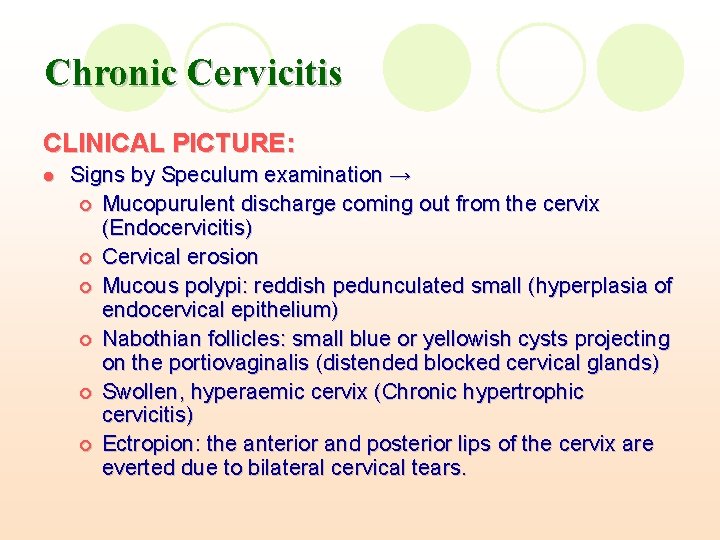
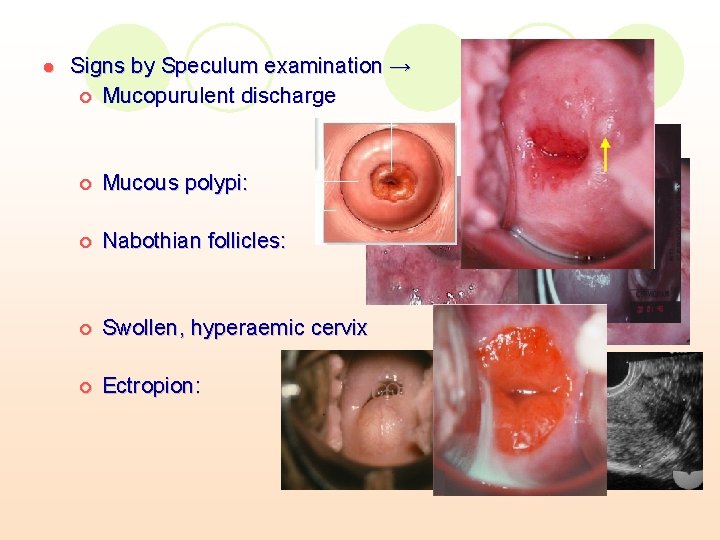
Chronic Cervicitis CLINICAL PICTURE: l Signs by Speculum examination → ¡ Mucopurulent discharge coming out from the cervix (Endocervicitis) ¡ Cervical erosion ¡ Mucous polypi: reddish pedunculated small (hyperplasia of endocervical epithelium) ¡ Nabothian follicles: small blue or yellowish cysts projecting on the portiovaginalis (distended blocked cervical glands) ¡ Swollen, hyperaemic cervix (Chronic hypertrophic cervicitis) ¡ Ectropion: the anterior and posterior lips of the cervix are everted due to bilateral cervical tears.
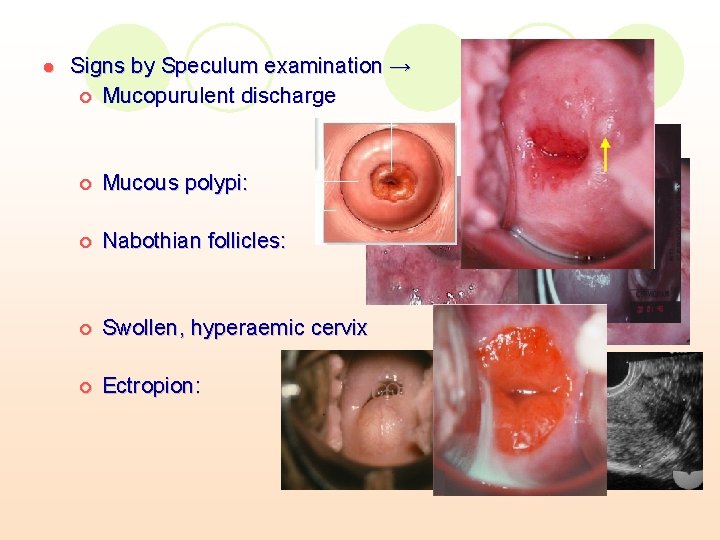
l Signs by Speculum examination → ¡ Mucopurulent discharge ¡ Mucous polypi: ¡ Nabothian follicles: ¡ Swollen, hyperaemic cervix ¡ Ectropion:
Chronic Cervicitis l Investigations: Exclusion of malignancy ¡ Culture and sensitivity of the discharge. ¡ l Treatment: Oral or vaginal Antibiotics ¡ Cervical Cauterization ¡ Trachelorraphy: to treat cervical tears ¡ Conization in suspicious lesions ¡
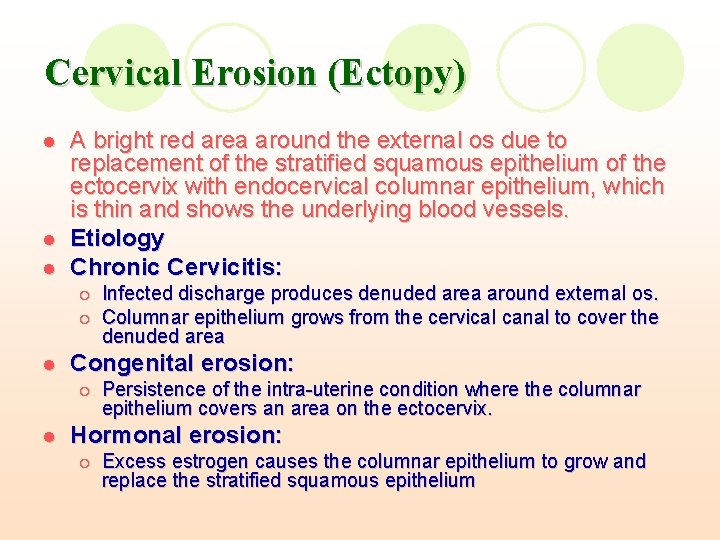
Cervical Erosion (Ectopy) l l l A bright red area around the external os due to replacement of the stratified squamous epithelium of the ectocervix with endocervical columnar epithelium, which is thin and shows the underlying blood vessels. Etiology Chronic Cervicitis: ¡ ¡ l Congenital erosion: ¡ l Infected discharge produces denuded area around external os. Columnar epithelium grows from the cervical canal to cover the denuded area Persistence of the intra-uterine condition where the columnar epithelium covers an area on the ectocervix. Hormonal erosion: ¡ Excess estrogen causes the columnar epithelium to grow and replace the stratified squamous epithelium
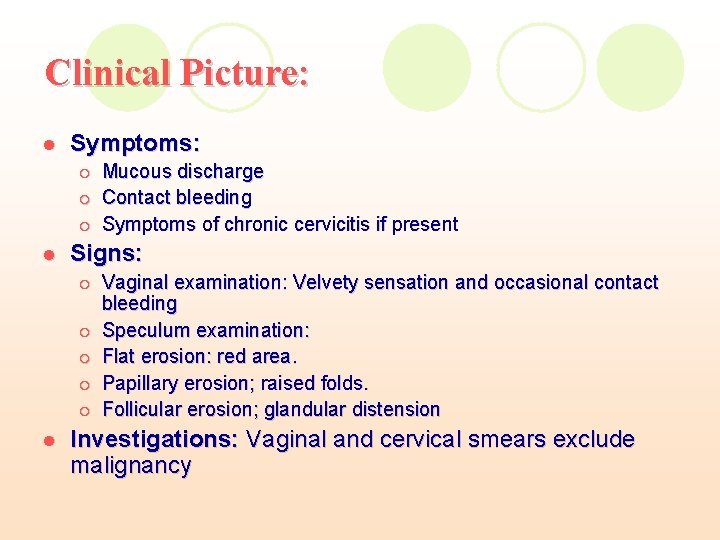
Clinical Picture: l Symptoms: ¡ ¡ ¡ l Signs: ¡ ¡ ¡ l Mucous discharge Contact bleeding Symptoms of chronic cervicitis if present Vaginal examination: Velvety sensation and occasional contact bleeding Speculum examination: Flat erosion: red area. Papillary erosion; raised folds. Follicular erosion; glandular distension Investigations: Vaginal and cervical smears exclude malignancy
Treatment: Hormonal erosion: NO ttt except if the case persists for more than three months. l Antibiotics to treat associated infection. l Cauterisation: l The main line of treatment ¡ It opens and drains the infected glands and coagulates the superficial epithelium over the erosion ¡
Methods Of Cauterisation Electrocautery l Cryocautery (freezing) l Laser Cauterisation l Endcoagulation: Semm’s coagulator l Chemical Cautery l
Electrocautery l l l No anaesthesia Cervix is exposed and cleaned by sodium carbonate Using a red-hot electrode, 3 linear burns are made on the anterior and posterior lips of the cervix extending from the internal as to the edge of the erosion. ¡ l l The depth of cauterisation is 2 mm. Vaginal discharge will increase for 10 days Squamous epithelium takes 4 -6 weeks to cover the cauterised area.
Electrocautery Complications: l Secondary haemorrhage: Due to sloughing ¡ About the 10 th day ¡ Treated by packing, antibiotics ¡ Ascending infection and parametritis l Cervical stenosis l
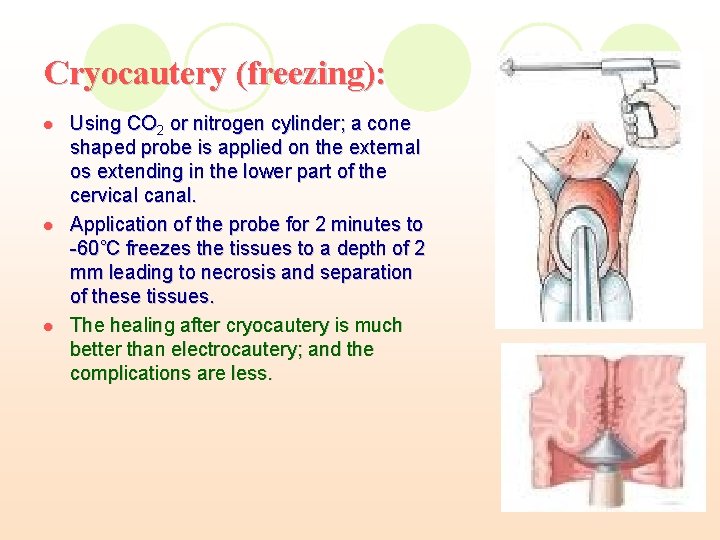
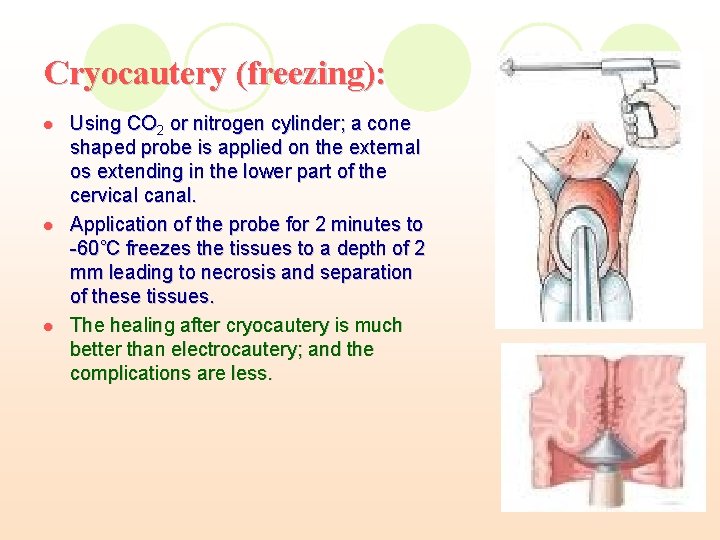
Cryocautery (freezing): l l l Using CO 2 or nitrogen cylinder; a cone shaped probe is applied on the external os extending in the lower part of the cervical canal. Application of the probe for 2 minutes to -60˚C freezes the tissues to a depth of 2 mm leading to necrosis and separation of these tissues. The healing after cryocautery is much better than electrocautery; and the complications are less.
Laser Cauterization Controlled destruction of the superficial thin layer of tissues by vaporization of cells. l It gives excellent results but the instrument is expensive and requires training. l
Endcoagulation: Semm’s coagulator l The probe is heated to 100°C causing coagulation without excessive necrosis the results are excellent but the instrument is expensive.
Chemical Cautery: Using silver nitrate 20% (after protecting the vagina with Ferguson speculum). l It is an old method but can be used for mild residual lesions l