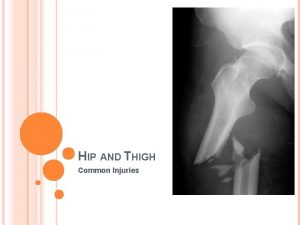
Lower Extremity Trauma Lower Extremity Trauma Hip Fractures















- Slides: 126
Lower Extremity Trauma
Lower Extremity Trauma Hip Fractures / Dislocations Femur Fractures Patella Fractures Knee Dislocations Tibia Fractures Ankle Fractures Foot Fracture
Hip Fractures n Hip Dislocations n Femoral Head Fractures n Femoral Neck Fractures n Intertrochanteric Fractures n Subtrochanteric Fractures
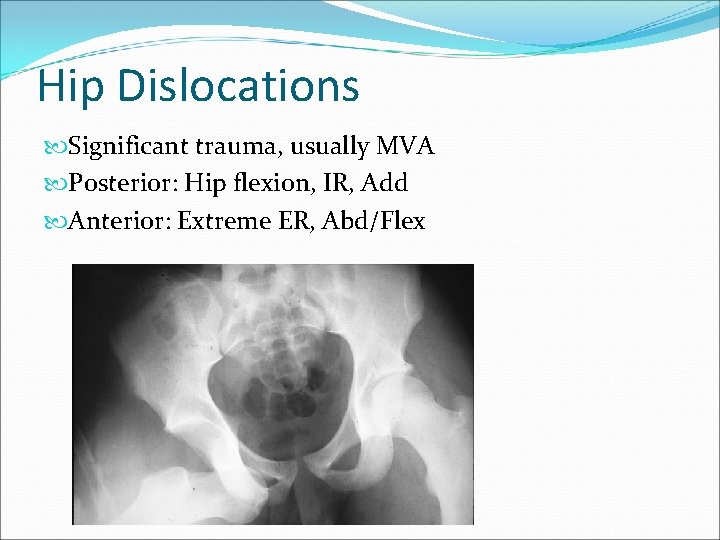
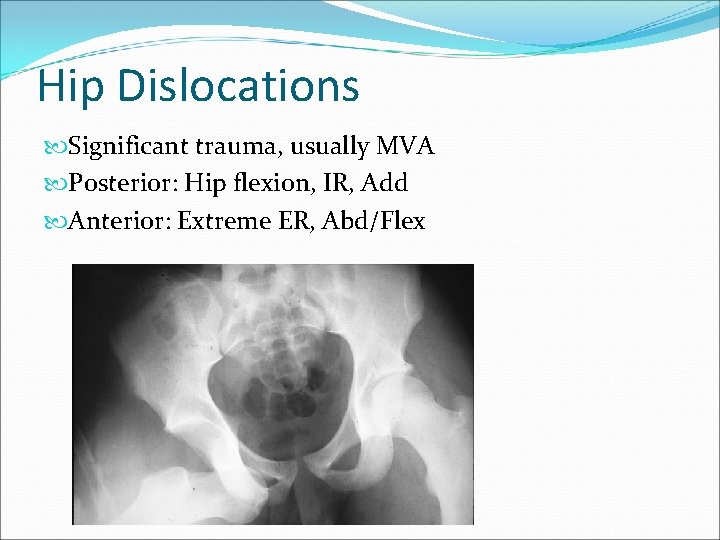
Hip Dislocations Significant trauma, usually MVA Posterior: Hip flexion, IR, Add Anterior: Extreme ER, Abd/Flex
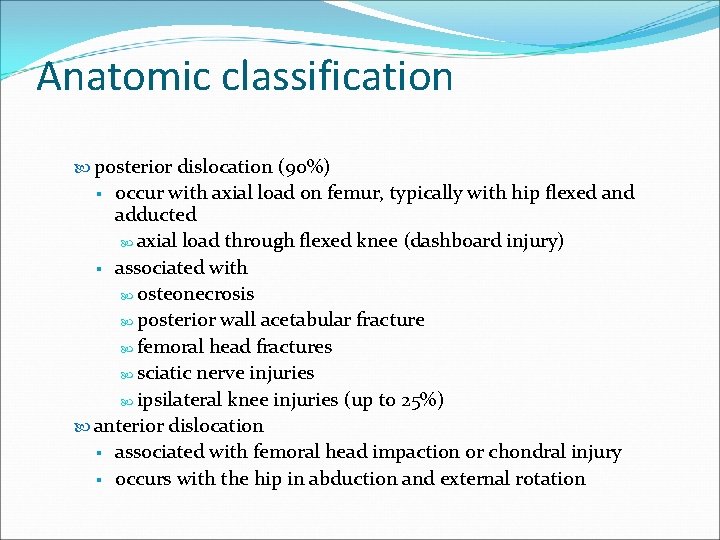
Anatomic classification posterior dislocation (90%) occur with axial load on femur, typically with hip flexed and adducted axial load through flexed knee (dashboard injury) § associated with osteonecrosis posterior wall acetabular fracture femoral head fractures sciatic nerve injuries ipsilateral knee injuries (up to 25%) anterior dislocation § associated with femoral head impaction or chondral injury § occurs with the hip in abduction and external rotation §
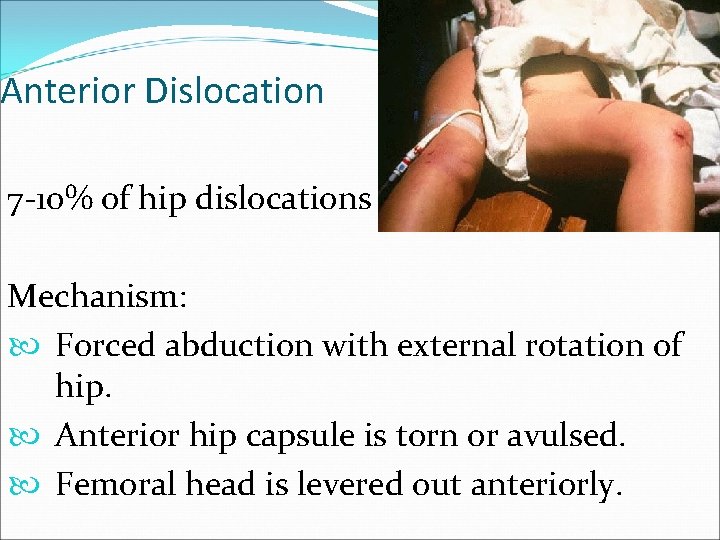
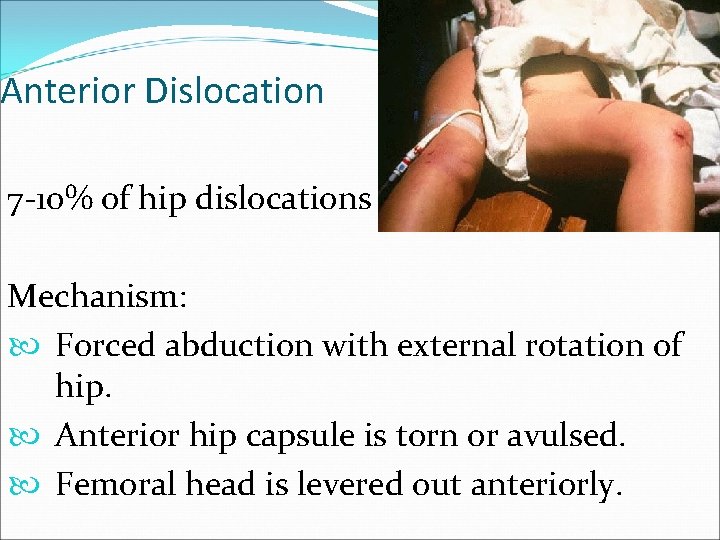
Anterior Dislocation 7 -10% of hip dislocations Mechanism: Forced abduction with external rotation of hip. Anterior hip capsule is torn or avulsed. Femoral head is levered out anteriorly.
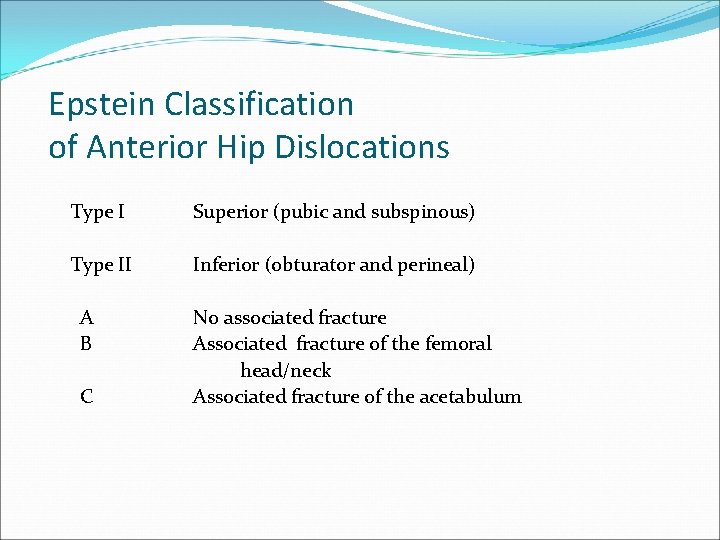
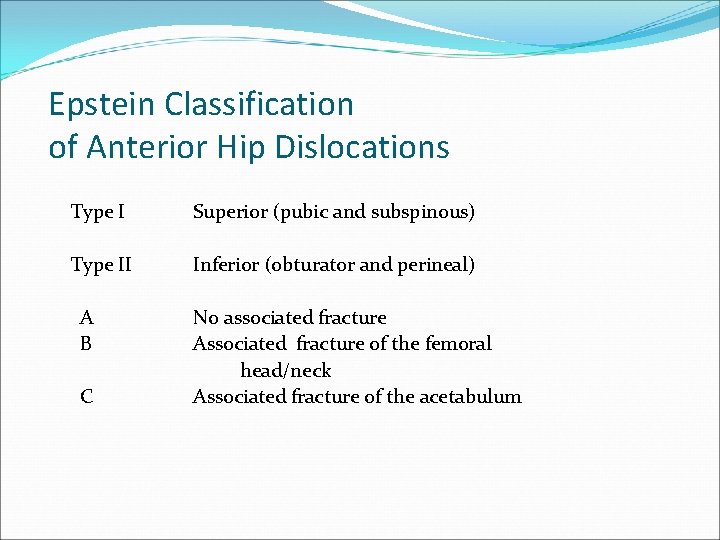
Epstein Classification of Anterior Hip Dislocations Type I Superior (pubic and subspinous) Type II Inferior (obturator and perineal) A No associated fracture B Associated fracture of the femoral head/neck C Associated fracture of the acetabulum
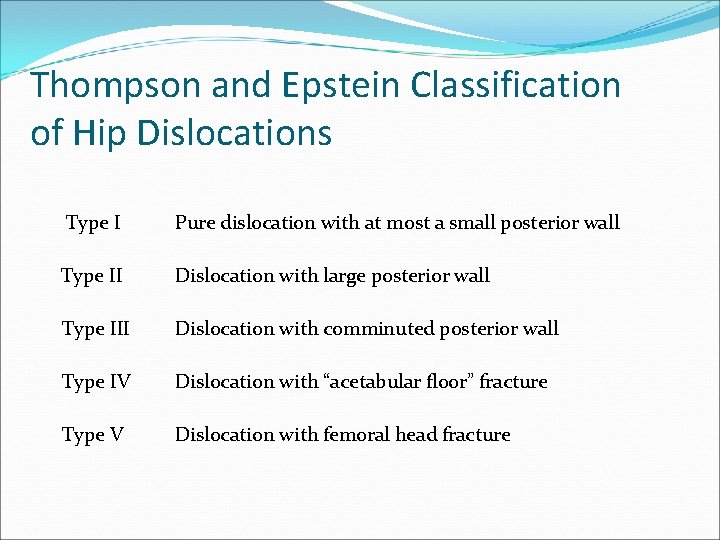
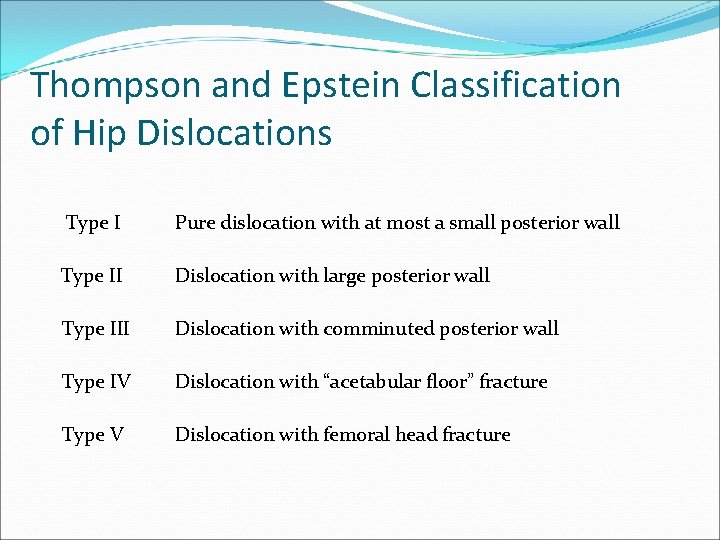
Thompson and Epstein Classification of Hip Dislocations Type II Pure dislocation with at most a small posterior wall Dislocation with large posterior wall Type III Dislocation with comminuted posterior wall Type IV Dislocation with “acetabular floor” fracture Type V Dislocation with femoral head fracture
Hip Dislocations Emergent Treatment: Closed Reduction Dislocated hip is an emergency Goal is to reduce risk of AVN and DJD Allows restoration of flow through occluded or compressed vessels Literature supports decreased AVN with earlier reduction Requires proper anesthesia Requires “team” (i. e. more than one person)
Hip Dislocations Emergent Treatment: Closed Reduction General anesthesia with muscle relaxation facilitates reduction, but is not necessary Conscious sedation is acceptable Attempts at reduction with inadequate analgesia/ sedation will cause unnecessary pain, cause muscle spasm, and make subsequent attempts at reduction more difficult
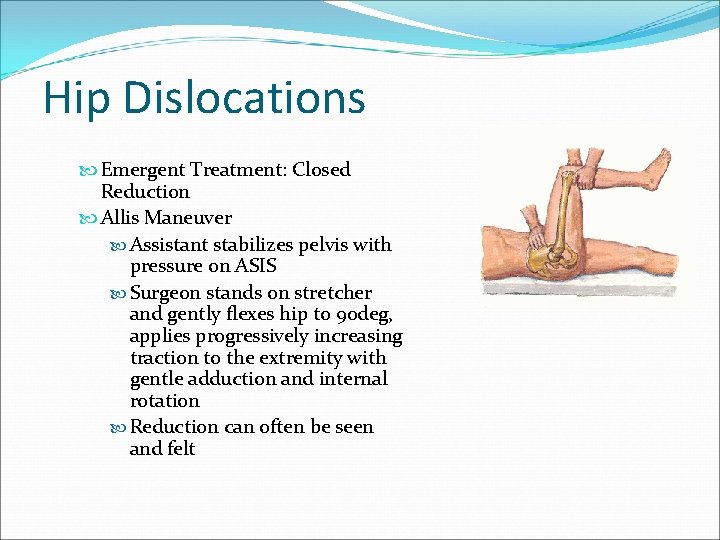
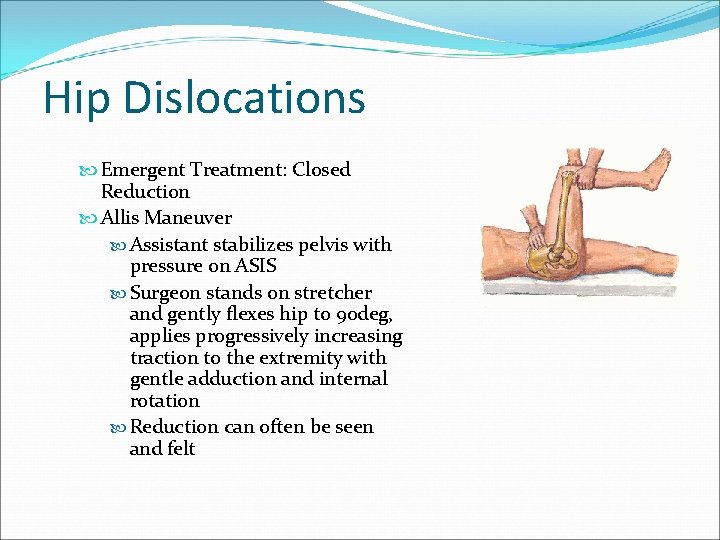
Hip Dislocations Emergent Treatment: Closed Reduction Allis Maneuver Assistant stabilizes pelvis with pressure on ASIS Surgeon stands on stretcher and gently flexes hip to 90 deg, applies progressively increasing traction to the extremity with gentle adduction and internal rotation Reduction can often be seen and felt Insert hip Reduction Picture
Hip Dislocations Following Closed Reduction Check stability of hip to 90 deg flexion Repeat AP pelvis Judet views of pelvis (if acetabulum fx) CT scan with thin cuts through acetabulum R/O bony fragments within hip joint (indication for emergent OR trip to remove incarcerated fragment of bone)
Hip Dislocations Following Closed Reduction No flexion > 60 deg (Hip Precautions) Early mobilization with P. W. B. for 4 -6 weeks MRI at 3 months (follow risk of AVN)
Complications n Post-traumatic arthritis up to 20% for simple dislocation, markedly increased for complex dislocation n Femoral head osteonecrosis 5 -40% incidence Increased risk with increased time to reduction n Sciatic nerve injury 8 -20% incidence associated with longer time to reduction n Recurrent dislocations less than 2%
Femoral Head Fractures Concurrent with hip dislocation due to shear injury
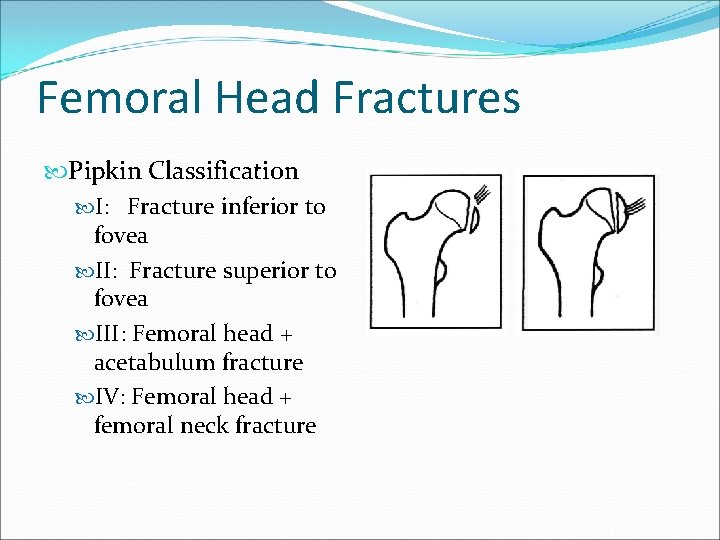
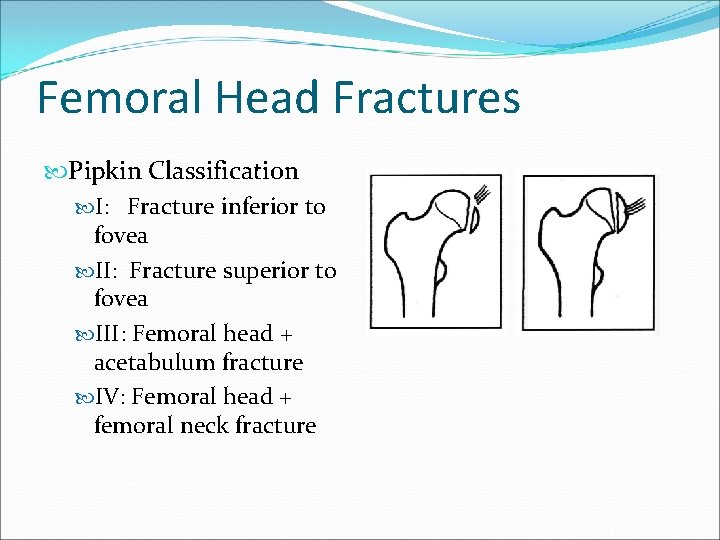
Femoral Head Fractures Pipkin Classification I: Fracture inferior to fovea II: Fracture superior to fovea III: Femoral head + acetabulum fracture IV: Femoral head + femoral neck fracture
Femoral Head Fractures Treatment Options Type I Nonoperative: non-displaced ORIF if displaced Type II: ORIF Type III: ORIF of both fractures Type IV: ORIF vs. hemiarthroplasty
Epidemiology 250, 000 Hip fractures annually Expected to double by 2050 At risk populations Elderly: poor balance & vision, osteoporosis, inactivity, medications, malnutrition Young: high energy trauma
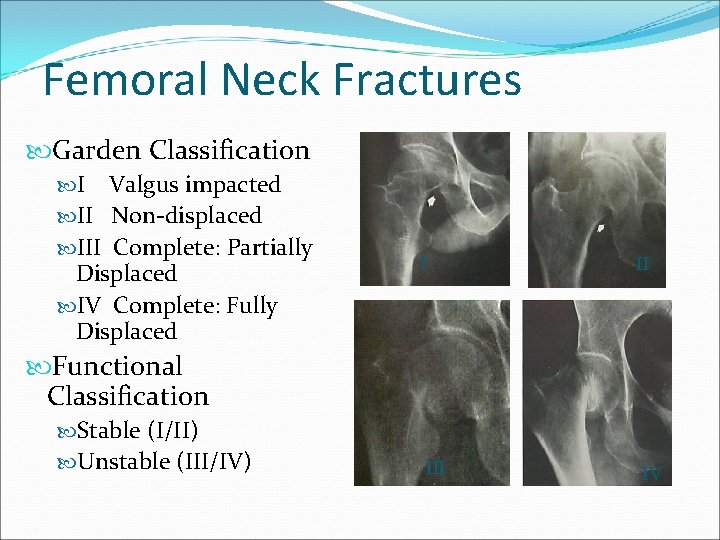
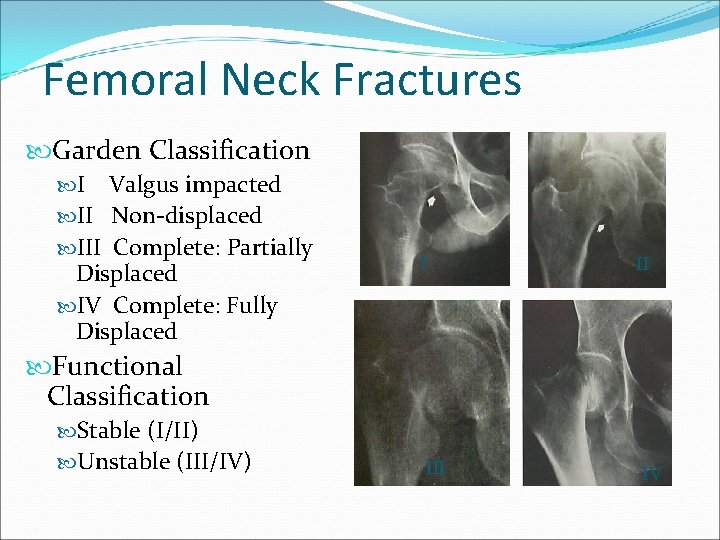
Femoral Neck Fractures Garden Classification I Valgus impacted II Non-displaced III Complete: Partially Displaced IV Complete: Fully Displaced I II IV Functional Classification Stable (I/II) Unstable (III/IV)
Femoral Neck Fractures Treatment Options Operative ORIF Hemiarthroplasty (Endoprosthesis) Total Hip Replacement
Femoral Neck Fractures Young Patients Urgent ORIF (<6 hrs) Elderly Patients ORIF possible (higher risk AVN, non-union, and failure of fixation) Hemiarthroplasty Total Hip Replacement

Hemi ORIF THR
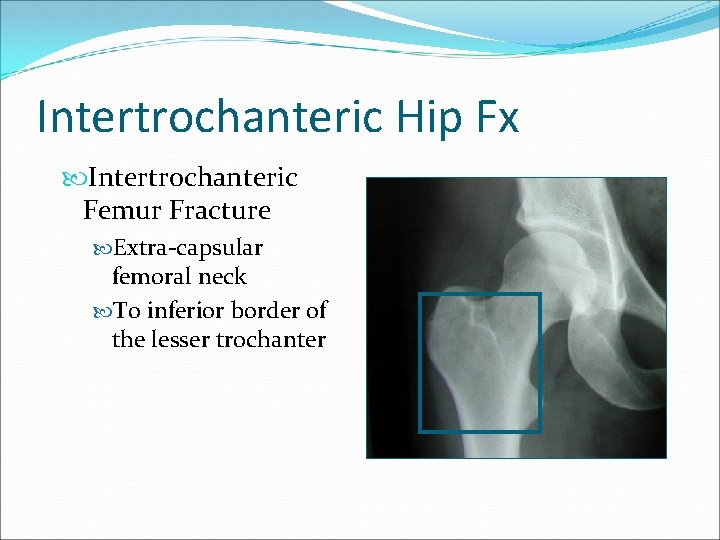
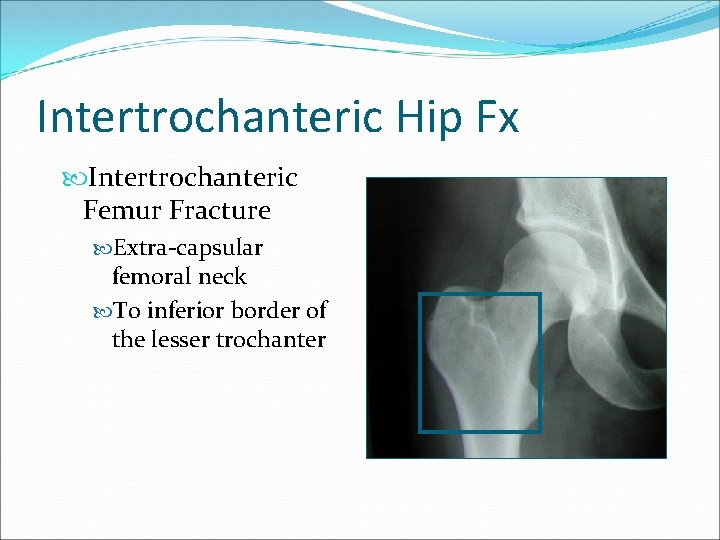
Intertrochanteric Hip Fx Intertrochanteric Femur Fracture Extra-capsular femoral neck To inferior border of the lesser trochanter
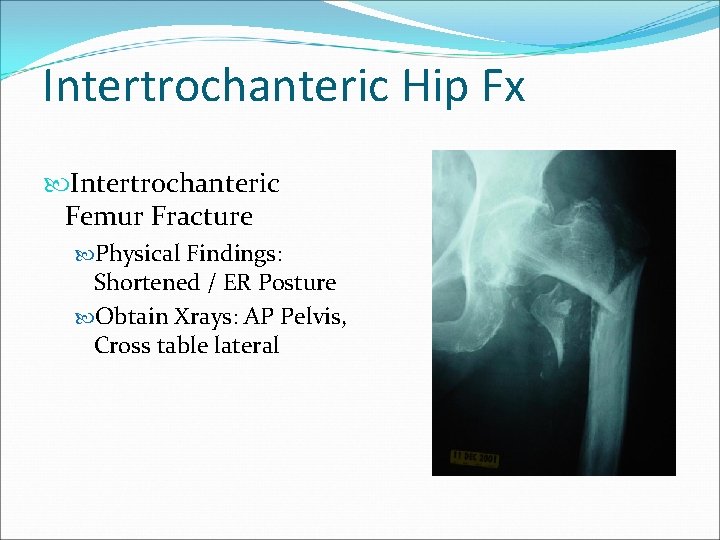
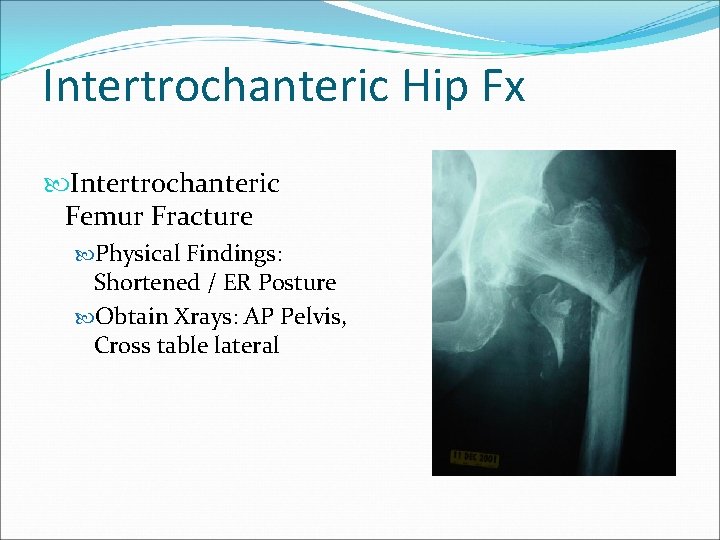
Intertrochanteric Hip Fx Intertrochanteric Femur Fracture Physical Findings: Shortened / ER Posture Obtain Xrays: AP Pelvis, Cross table lateral
Intertrochanteric Hip Fx Classification # of parts: Head/Neck, GT, LT, Shaft Stable Resists medial & compressive Loads after fixation Unstable Collapses into varus or shaft medializes despite anatomic reduction with fixation Reverse Obliquity
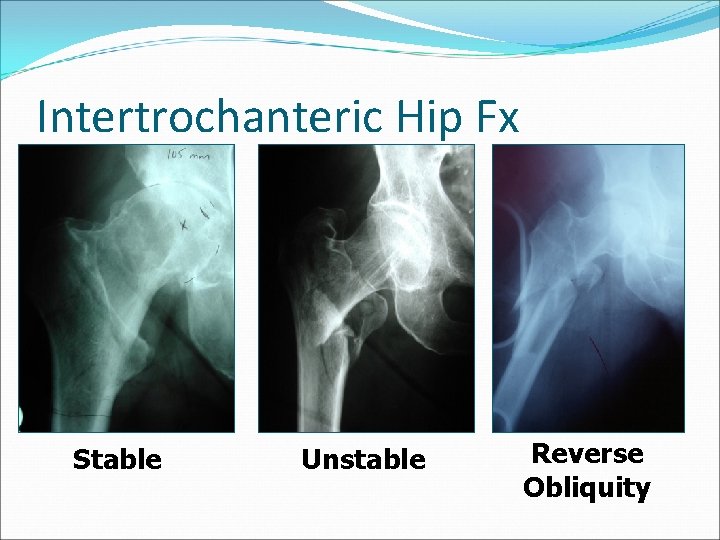
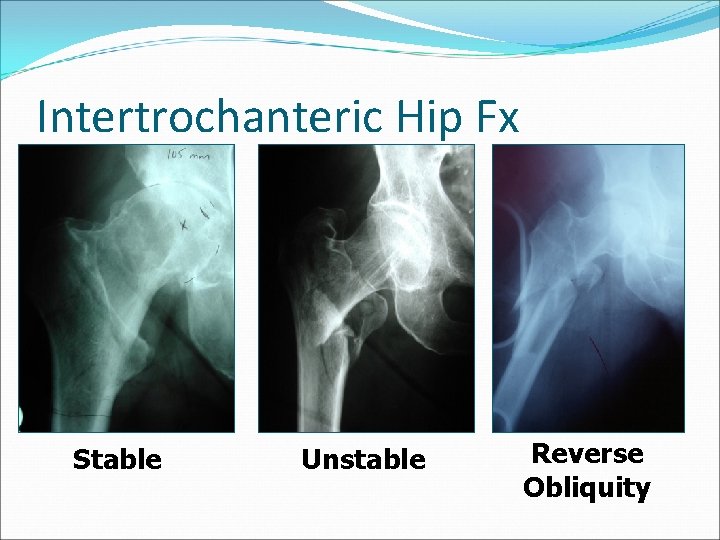
Intertrochanteric Hip Fx Stable Unstable Reverse Obliquity
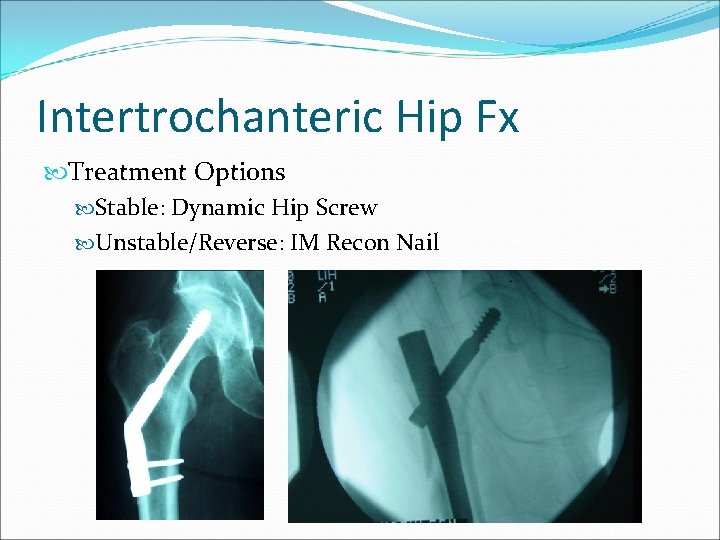
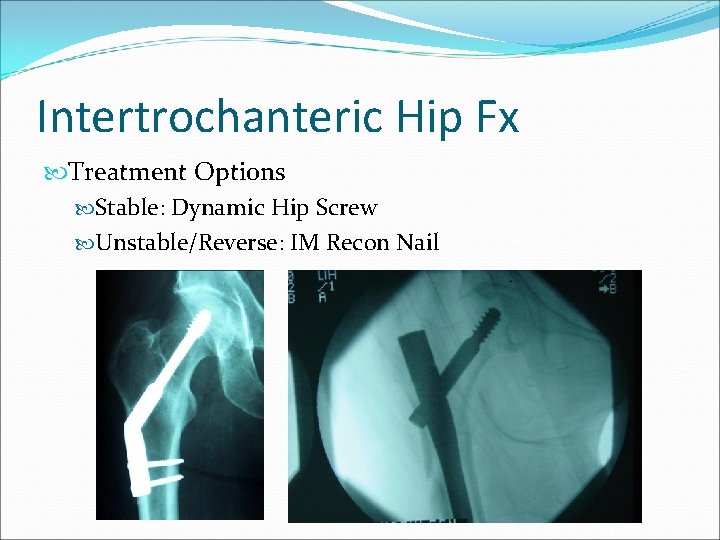
Intertrochanteric Hip Fx Treatment Options Stable: Dynamic Hip Screw Unstable/Reverse: IM Recon Nail
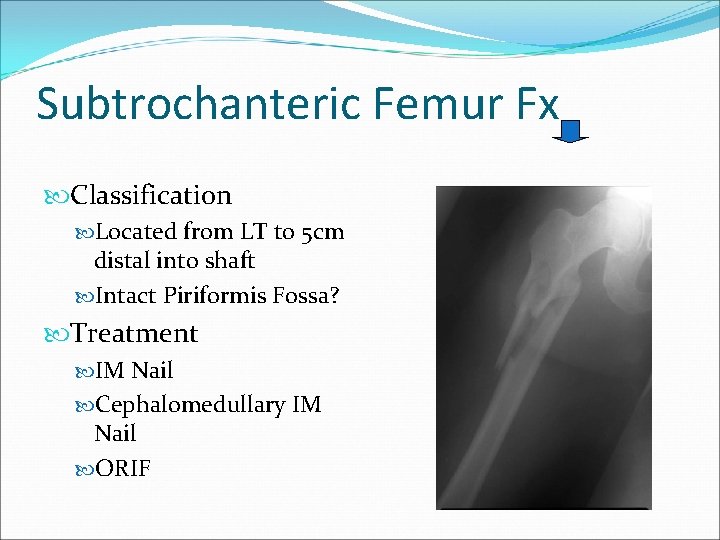
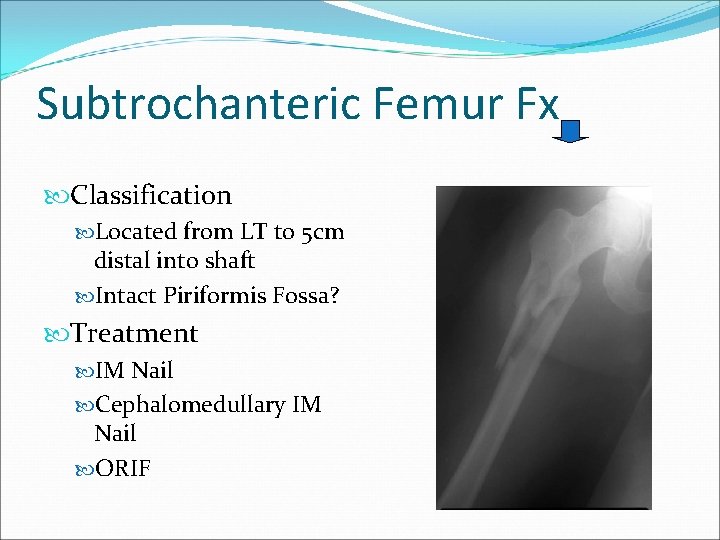
Subtrochanteric Femur Fx Classification Located from LT to 5 cm distal into shaft Intact Piriformis Fossa? Treatment IM Nail Cephalomedullary IM Nail ORIF
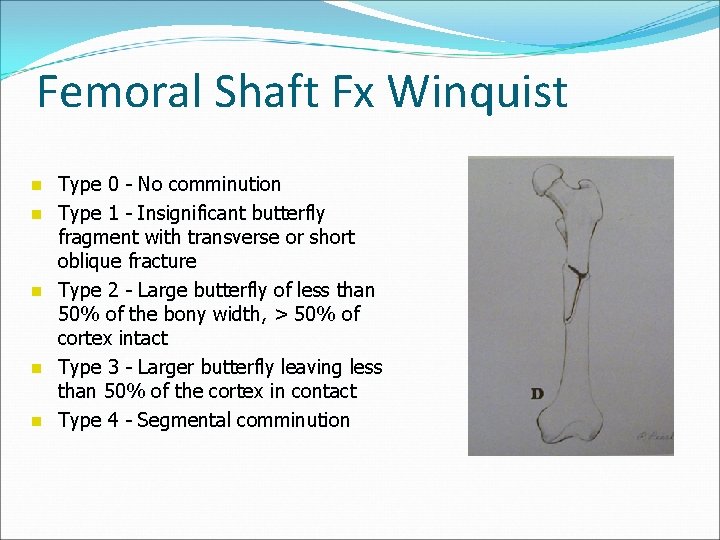
Femoral Shaft Fx Winquist n n n Type 0 - No comminution Type 1 - Insignificant butterfly fragment with transverse or short oblique fracture Type 2 - Large butterfly of less than 50% of the bony width, > 50% of cortex intact Type 3 - Larger butterfly leaving less than 50% of the cortex in contact Type 4 - Segmental comminution
Femoral Shaft Fx Treatment Options IM Nail with locking screws ORIF with plate/screw construct External fixation Consider traction pin if prolonged delay to surgery
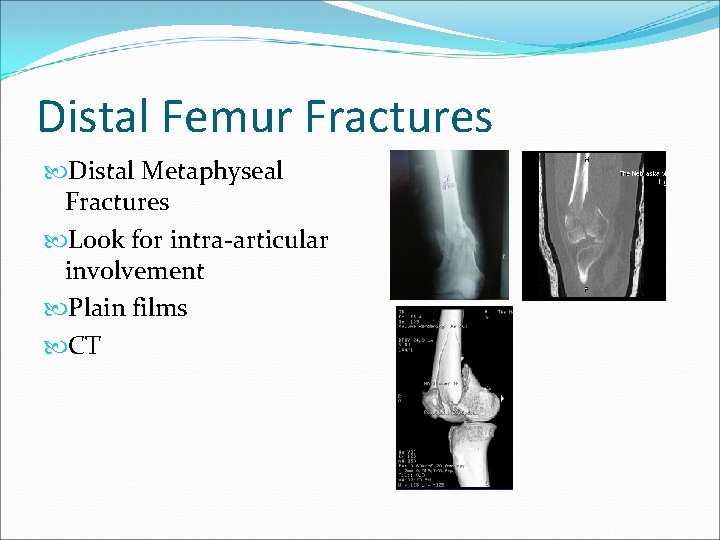
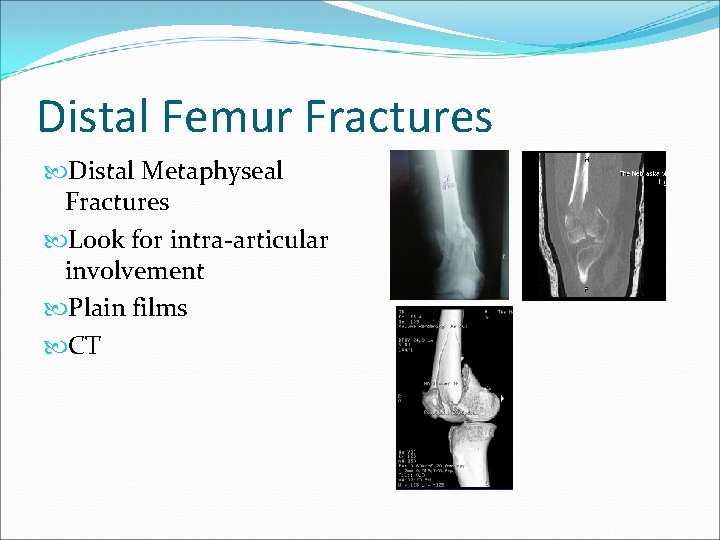
Distal Femur Fractures Distal Metaphyseal Fractures Look for intra-articular involvement Plain films CT
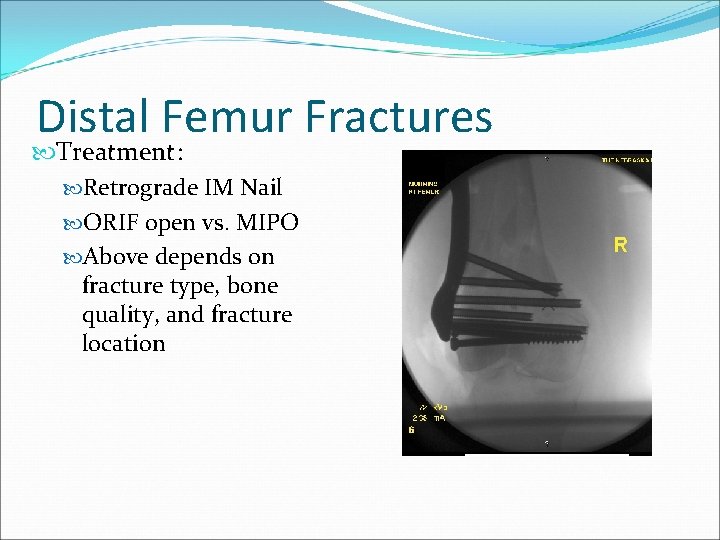
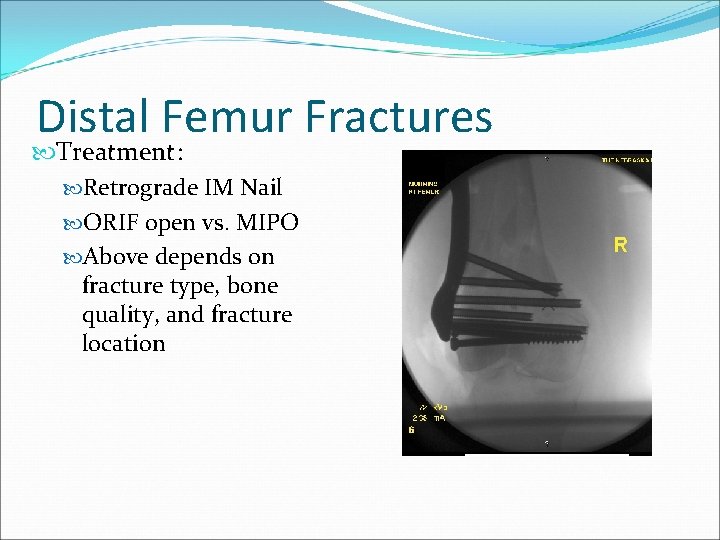
Distal Femur Fractures Treatment: Retrograde IM Nail ORIF open vs. MIPO Above depends on fracture type, bone quality, and fracture location
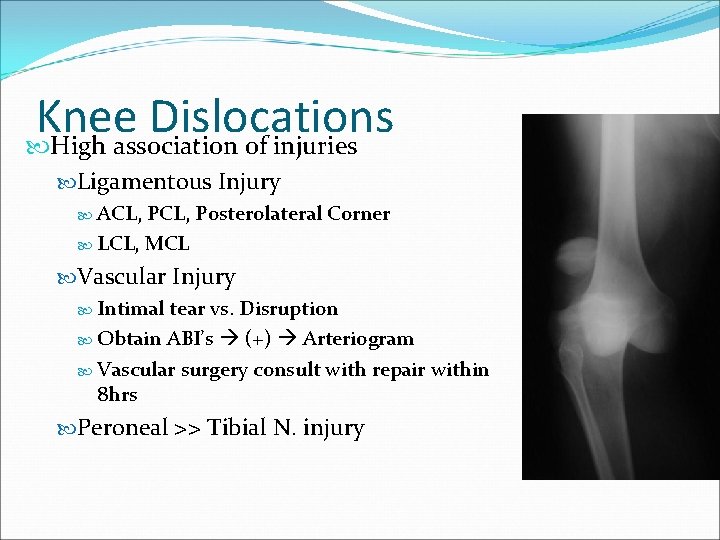
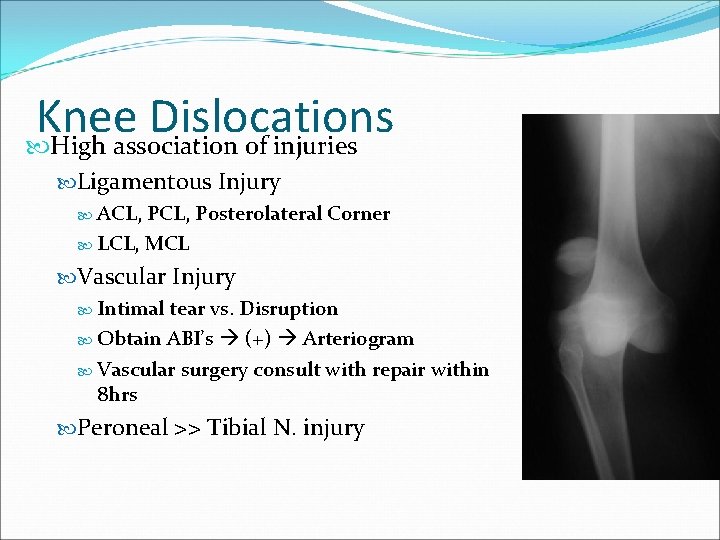
Knee Dislocations High association of injuries Ligamentous Injury ACL, Posterolateral Corner LCL, MCL Vascular Injury Intimal tear vs. Disruption Obtain ABI’s (+) Arteriogram Vascular surgery consult with repair within 8 hrs Peroneal >> Tibial N. injury
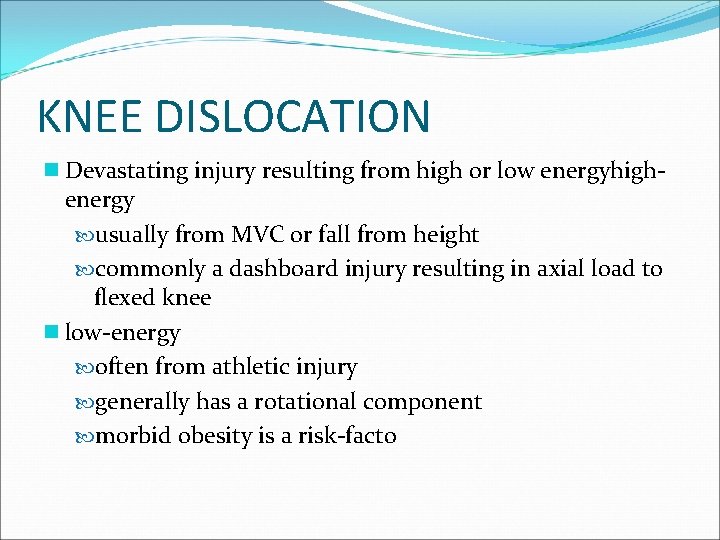
KNEE DISLOCATION n Devastating injury resulting from high or low energyhighenergy usually from MVC or fall from height commonly a dashboard injury resulting in axial load to flexed knee n low-energy often from athletic injury generally has a rotational component morbid obesity is a risk-facto
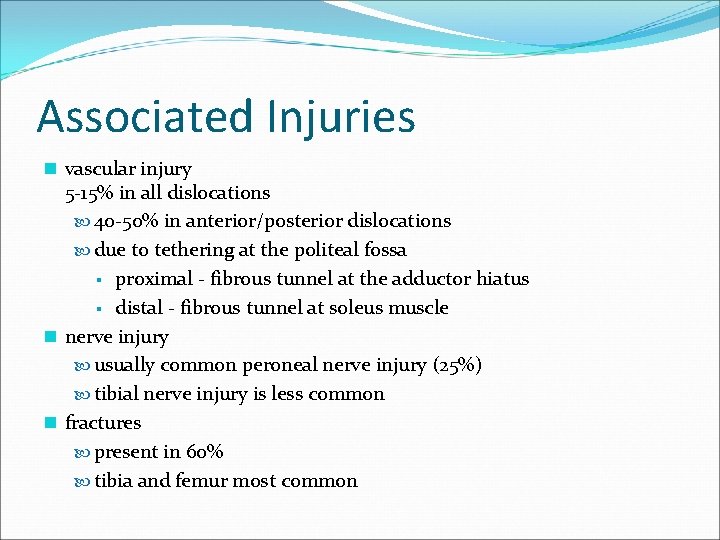
Associated Injuries n vascular injury 5 -15% in all dislocations 40 -50% in anterior/posterior dislocations due to tethering at the politeal fossa § proximal - fibrous tunnel at the adductor hiatus § distal - fibrous tunnel at soleus muscle n nerve injury usually common peroneal nerve injury (25%) tibial nerve injury is less common n fractures present in 60% tibia and femur most common
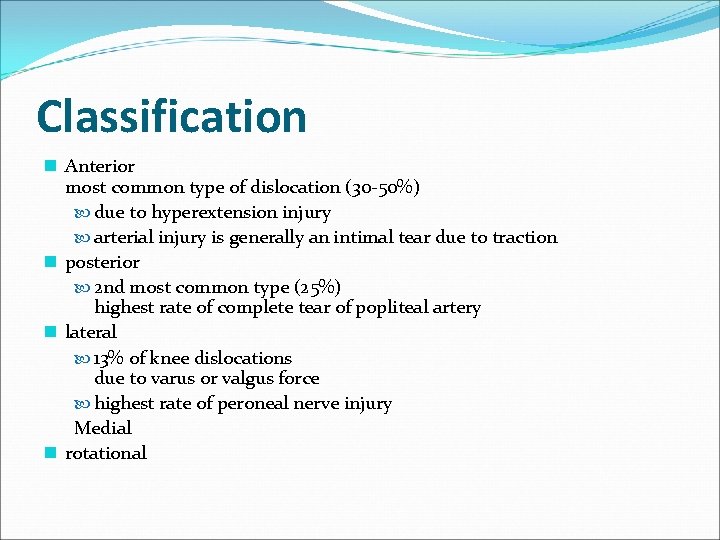
Classification n Anterior most common type of dislocation (30 -50%) due to hyperextension injury arterial injury is generally an intimal tear due to traction n posterior 2 nd most common type (25%) highest rate of complete tear of popliteal artery n lateral 13% of knee dislocations due to varus or valgus force highest rate of peroneal nerve injury Medial n rotational
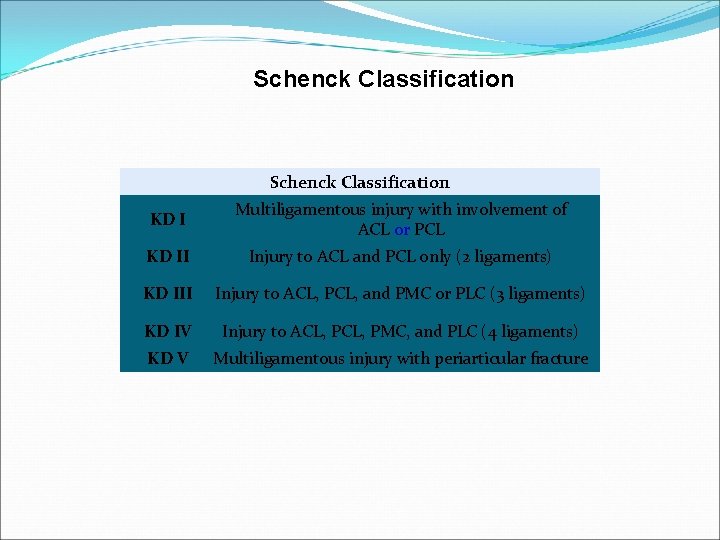
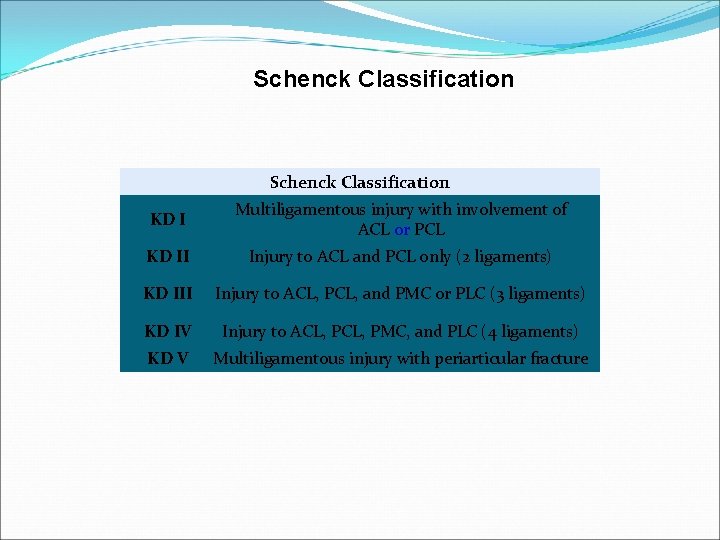
Schenck Classification KD I Multiligamentous injury with involvement of ACL or PCL KD II Injury to ACL and PCL only (2 ligaments) KD III Injury to ACL, PCL, and PMC or PLC (3 ligaments) KD IV Injury to ACL, PMC, and PLC (4 ligaments) KD V Multiligamentous injury with periarticular fracture
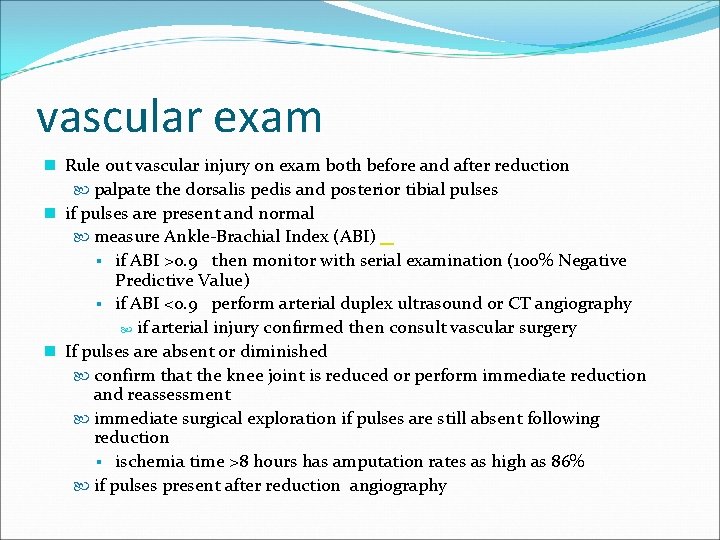
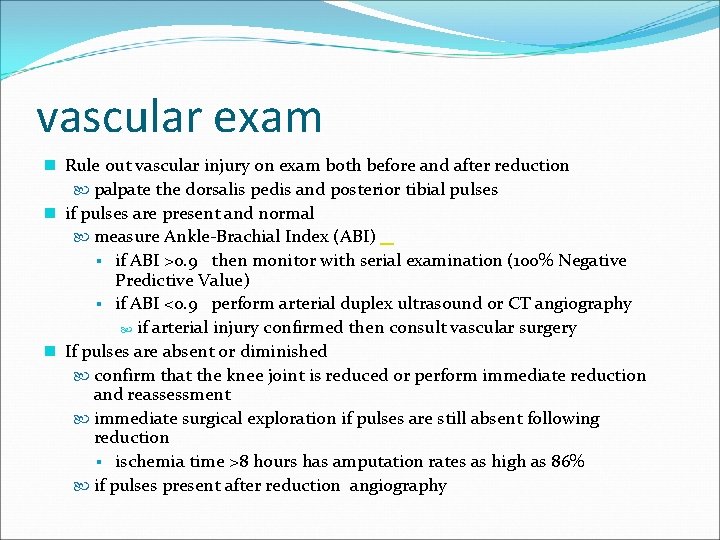
vascular exam n Rule out vascular injury on exam both before and after reduction palpate the dorsalis pedis and posterior tibial pulses n if pulses are present and normal measure Ankle-Brachial Index (ABI) § if ABI >0. 9 then monitor with serial examination (100% Negative Predictive Value) § if ABI <0. 9 perform arterial duplex ultrasound or CT angiography if arterial injury confirmed then consult vascular surgery n If pulses are absent or diminished confirm that the knee joint is reduced or perform immediate reduction and reassessment immediate surgical exploration if pulses are still absent following reduction § ischemia time >8 hours has amputation rates as high as 86% if pulses present after reduction angiography
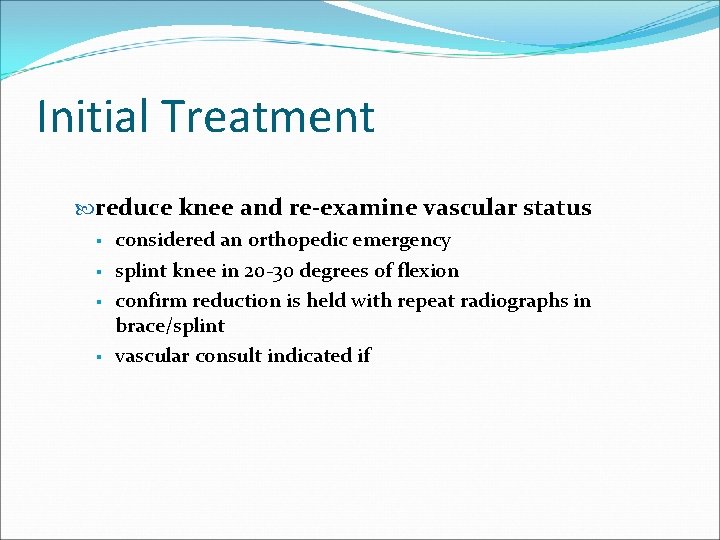
Initial Treatment reduce knee and re-examine vascular status § considered an orthopedic emergency § splint knee in 20 -30 degrees of flexion § confirm reduction is held with repeat radiographs in brace/splint § vascular consult indicated if
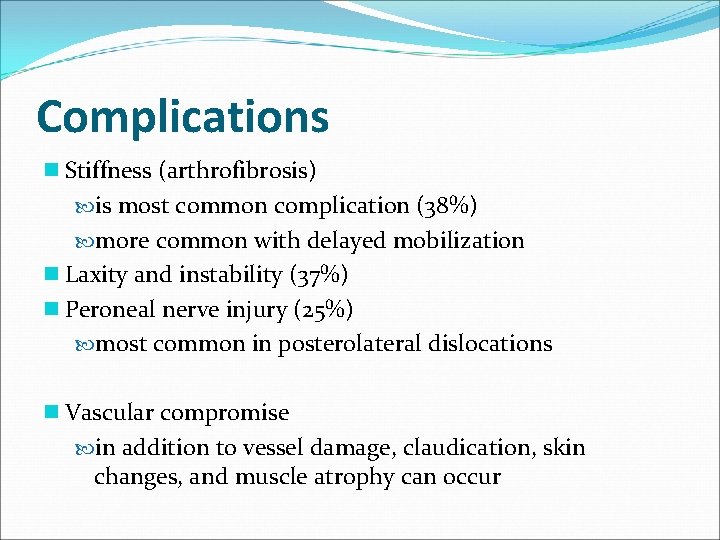
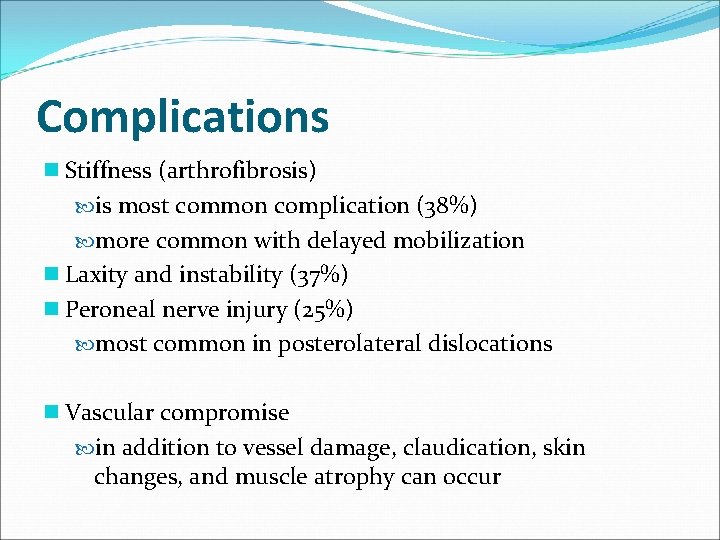
Complications n Stiffness (arthrofibrosis) is most common complication (38%) more common with delayed mobilization n Laxity and instability (37%) n Peroneal nerve injury (25%) most common in posterolateral dislocations n Vascular compromise in addition to vessel damage, claudication, skin changes, and muscle atrophy can occur
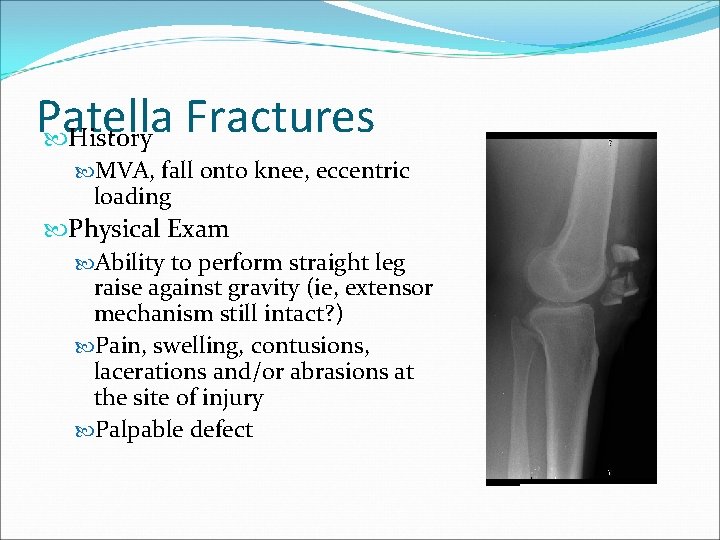
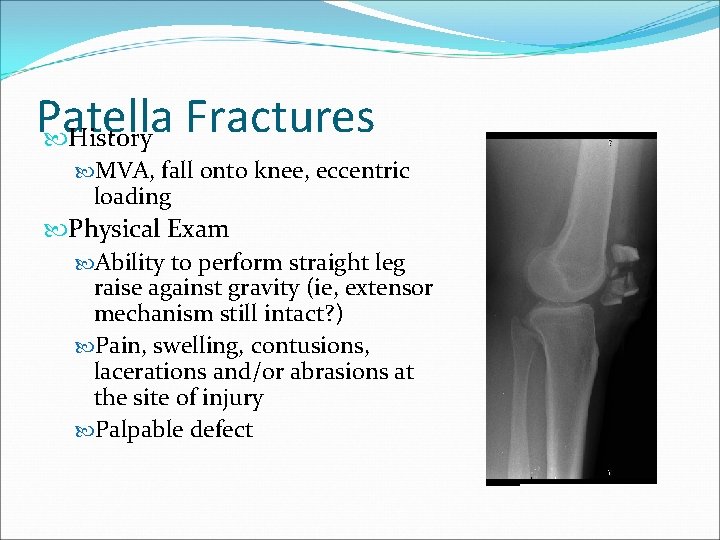
Patella Fractures History MVA, fall onto knee, eccentric loading Physical Exam Ability to perform straight leg raise against gravity (ie, extensor mechanism still intact? ) Pain, swelling, contusions, lacerations and/or abrasions at the site of injury Palpable defect
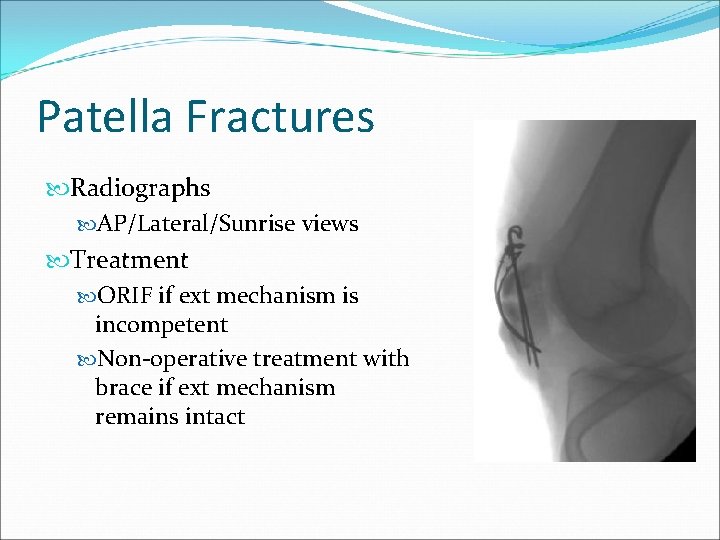
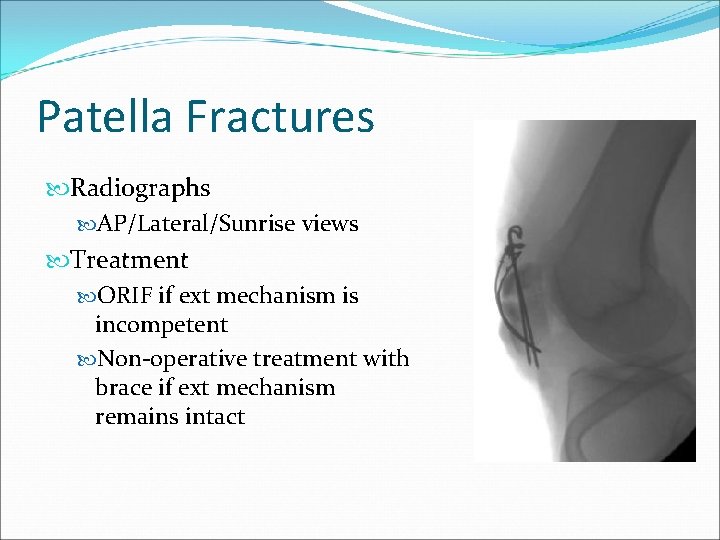
Patella Fractures Radiographs AP/Lateral/Sunrise views Treatment ORIF if ext mechanism is incompetent Non-operative treatment with brace if ext mechanism remains intact

Tibia Fractures Proximal Tibia Fractures (Tibial Plateau) Tibial Shaft Fractures Distal Tibia Fractures (Tibial Pilon/Plafond)
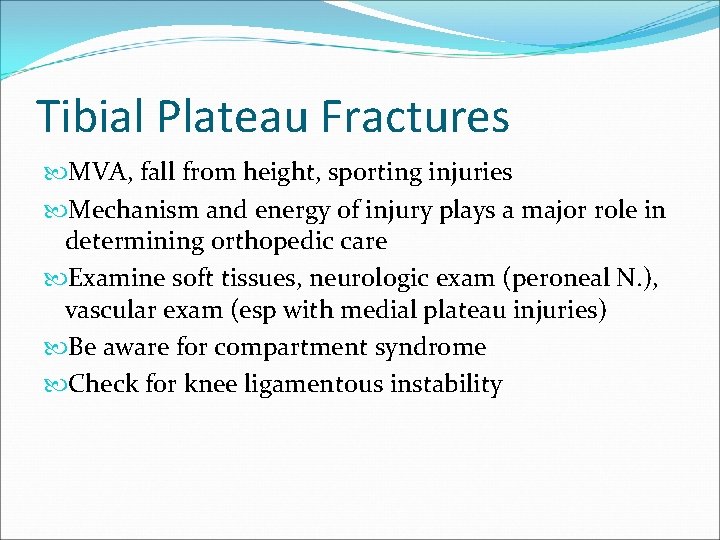
Tibial Plateau Fractures MVA, fall from height, sporting injuries Mechanism and energy of injury plays a major role in determining orthopedic care Examine soft tissues, neurologic exam (peroneal N. ), vascular exam (esp with medial plateau injuries) Be aware for compartment syndrome Check for knee ligamentous instability
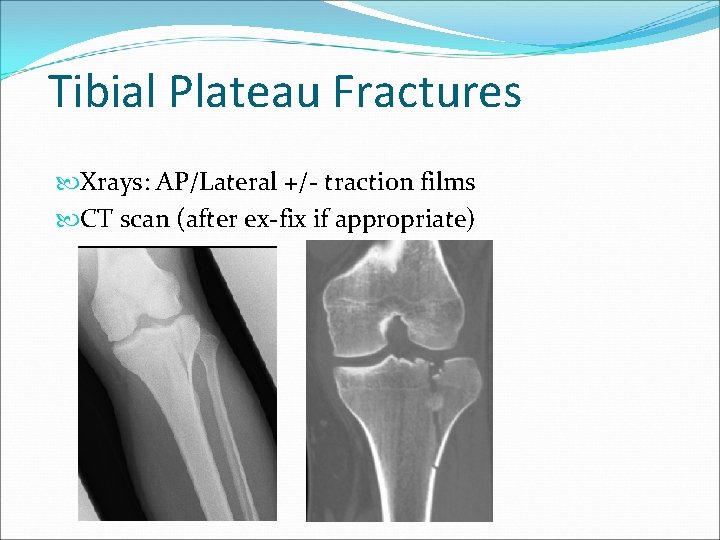
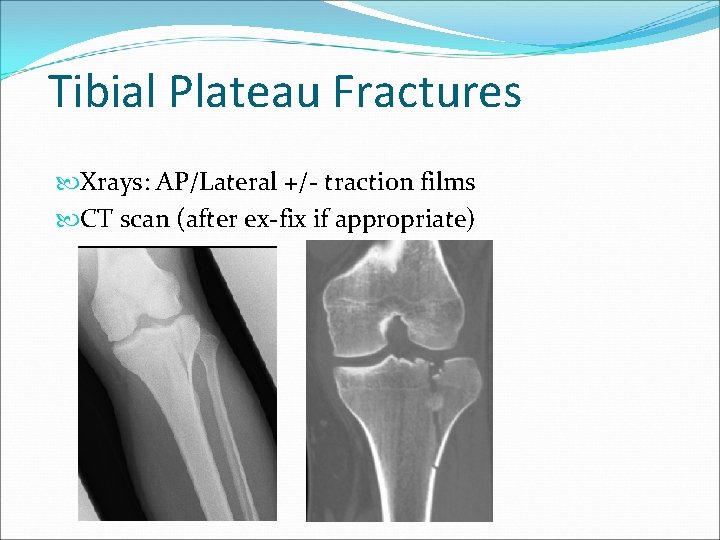
Tibial Plateau Fractures Xrays: AP/Lateral +/- traction films CT scan (after ex-fix if appropriate)
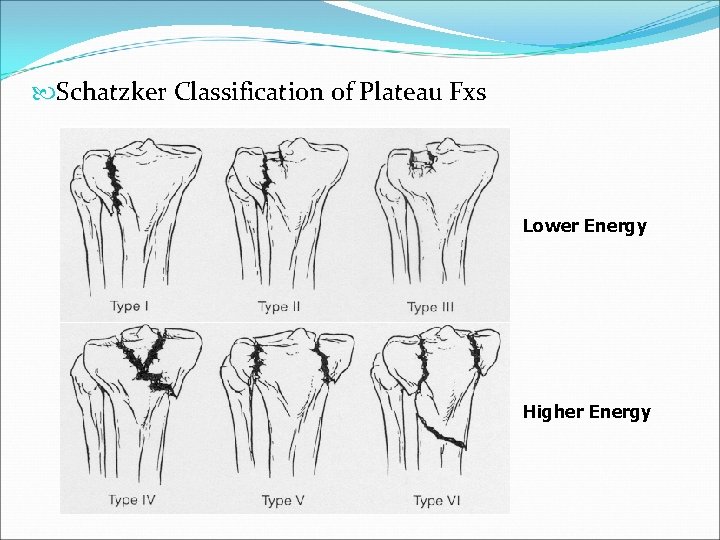
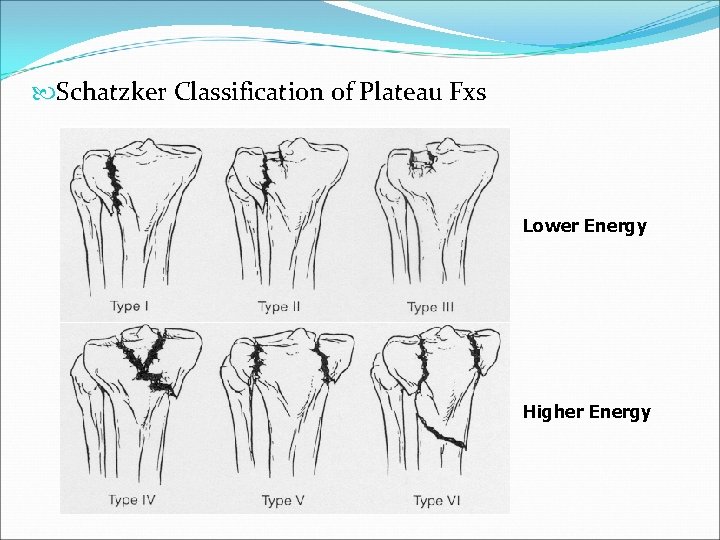
Schatzker Classification of Plateau Fxs Lower Energy Higher Energy
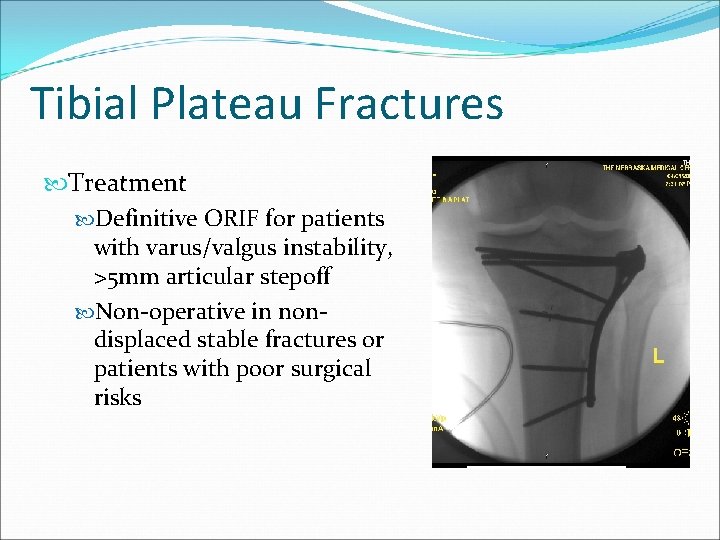
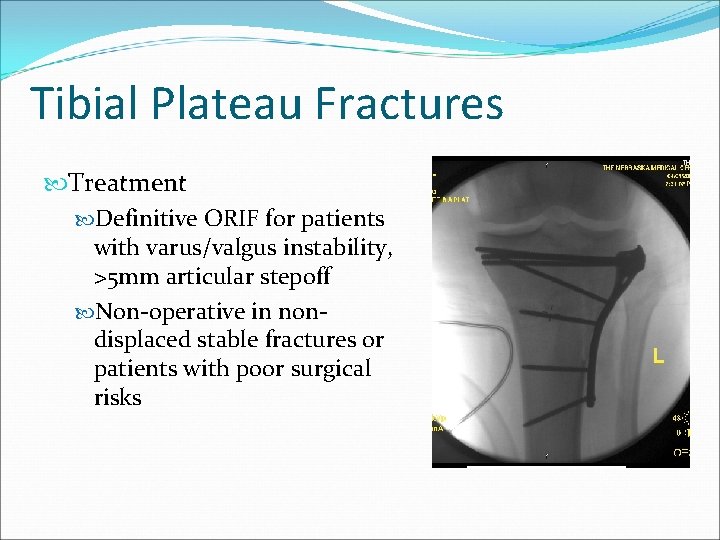
Tibial Plateau Fractures Treatment Definitive ORIF for patients with varus/valgus instability, >5 mm articular stepoff Non-operative in nondisplaced stable fractures or patients with poor surgical risks
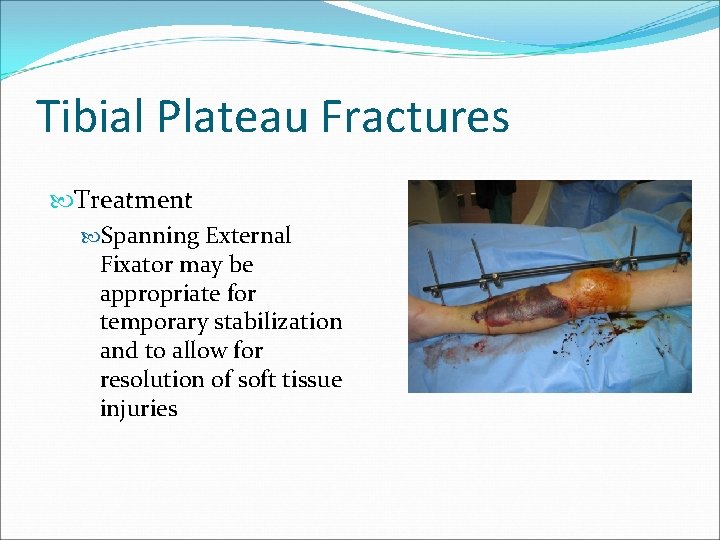
Tibial Plateau Fractures Treatment Spanning External Fixator may be appropriate for temporary stabilization and to allow for resolution of soft tissue injuries Insert blister Pics of ex-fix here
Tibial Shaft Fractures Mechanism of Injury Can occur in lower energy, torsion type injury (e. g. , skiing) More common with higher energy direct force (e. g. , car bumper) Open fractures of the tibia are more common than in any other long bone
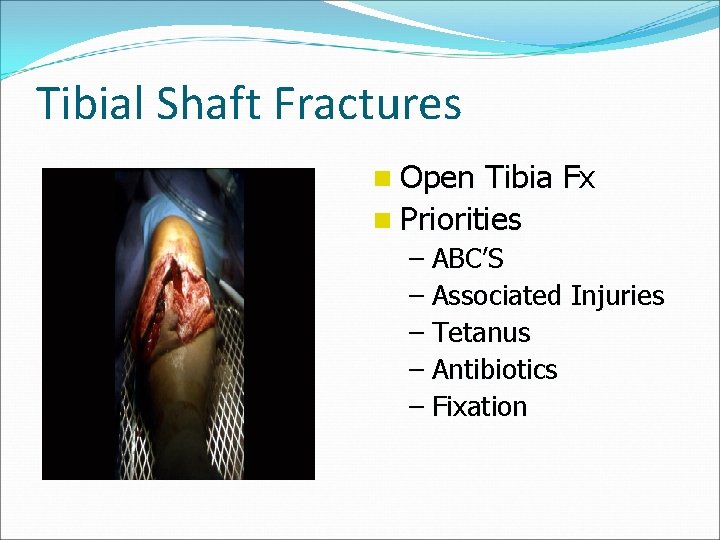
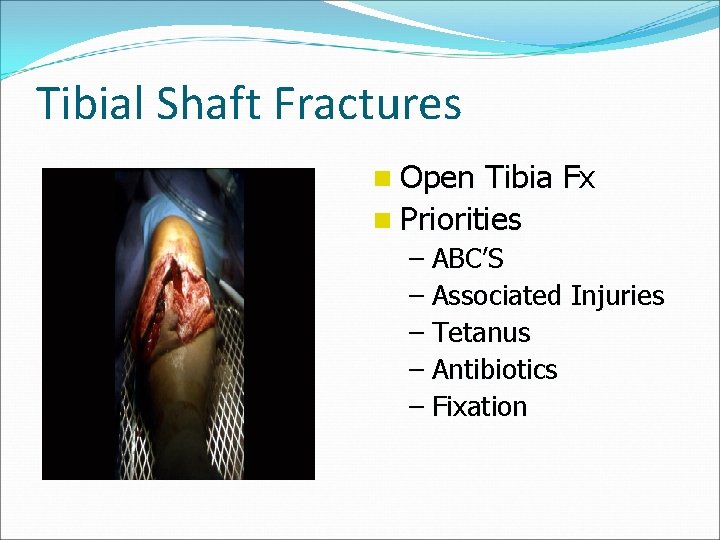
Tibial Shaft Fractures n Open Tibia Fx n Priorities – ABC’S – Associated Injuries – Tetanus – Antibiotics – Fixation
Tibial Shaft Fractures Gustilo and Anderson Classification of Open Fx Grade 1 <1 cm, minimal muscle contusion, usually inside out mechanism Grade 2 1 -10 cm, extensive soft tissue damage Grade 3 3 a: >10 cm, adequate bone coverage 3 b: >10 cm, periosteal stripping requiring flap advancement or free flap 3 c: vascular injury requiring repair

Tibial Shaft Fractures Management of Open Fx Soft Tissues ER: initial evaluation wound covered with sterile dressing and leg splinted, tetanus prophylaxis and appropriate antibiotics OR: Thorough I&D undertaken within 6 hours with serial debridements as warranted followed by definitive soft tissue cover

Tibial Shaft Fractures n Definitive Soft Tissue Coverage – Proximal third tibia fractures can be covered with gastrocnemius rotation flap – Middle third tibia fractures can be covered with soleus rotation flap – Distal third fractures usually require free flap for coverage
Tibial Shaft Fractures Treatment Options IM Nail ORIF with Plates External Fixation Cast or Cast-Brace
Tibial Shaft Fractures Advantages of IM nailing Lower non-union rate Smaller incisions Earlier weightbearing and function Single surgery
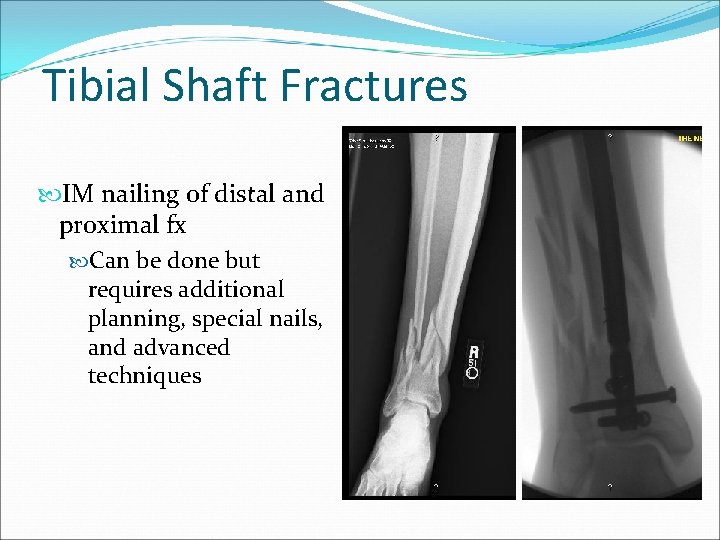
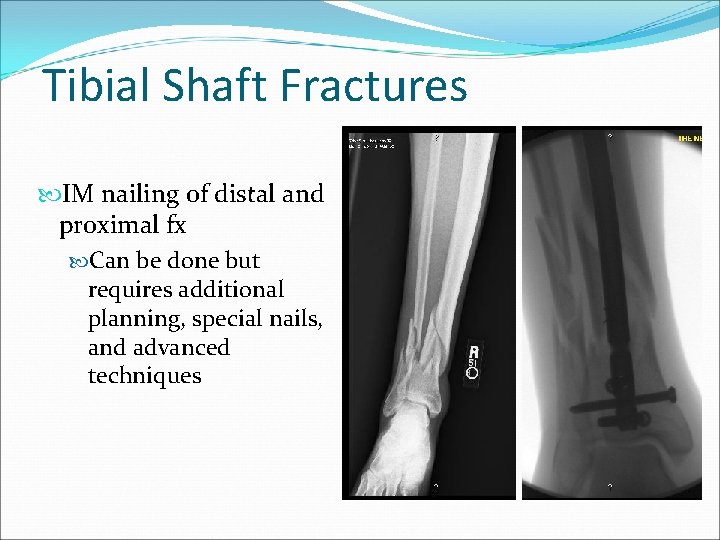
Tibial Shaft Fractures IM nailing of distal and proximal fx Can be done but requires additional planning, special nails, and advanced techniques
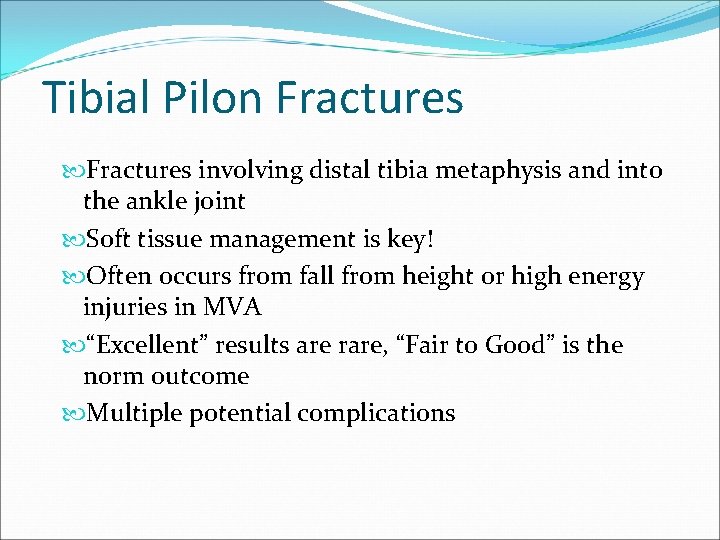
Tibial Pilon Fractures involving distal tibia metaphysis and into the ankle joint Soft tissue management is key! Often occurs from fall from height or high energy injuries in MVA “Excellent” results are rare, “Fair to Good” is the norm outcome Multiple potential complications
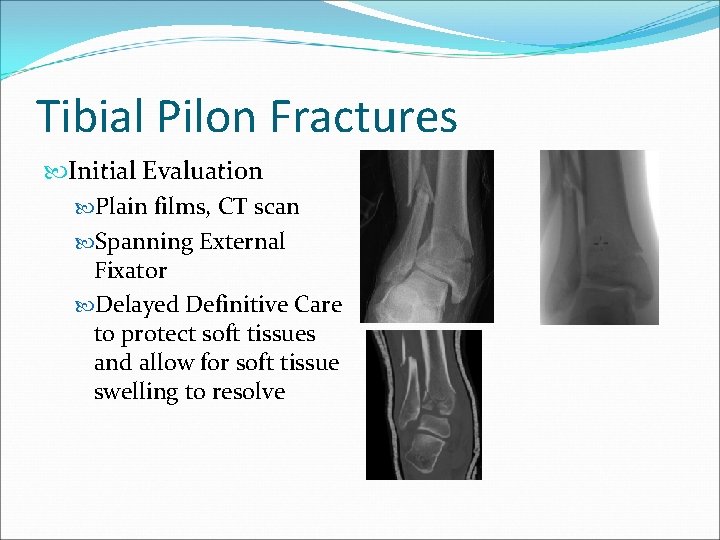
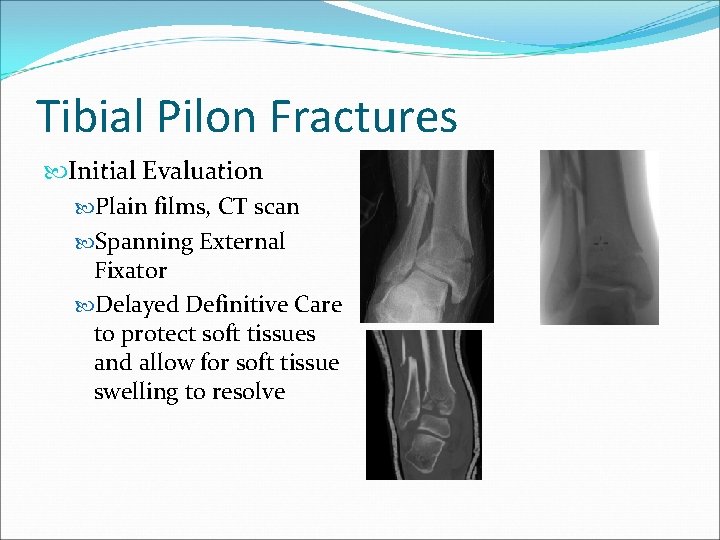
Tibial Pilon Fractures Initial Evaluation Plain films, CT scan Spanning External Fixator Delayed Definitive Care to protect soft tissues and allow for soft tissue swelling to resolve
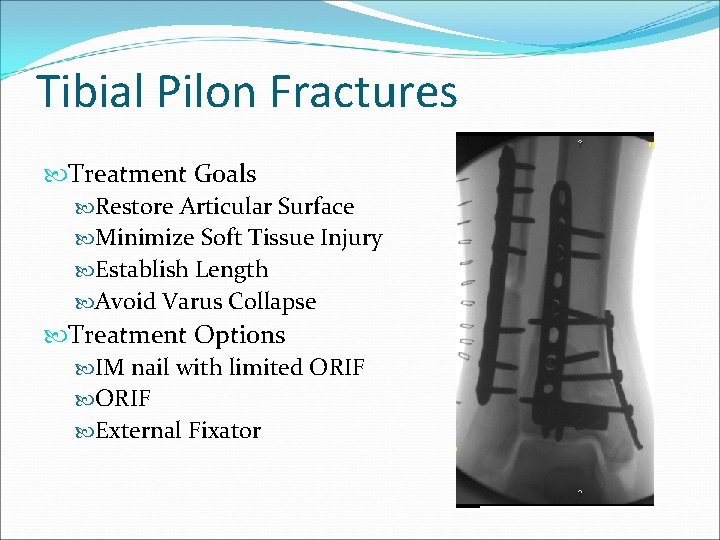
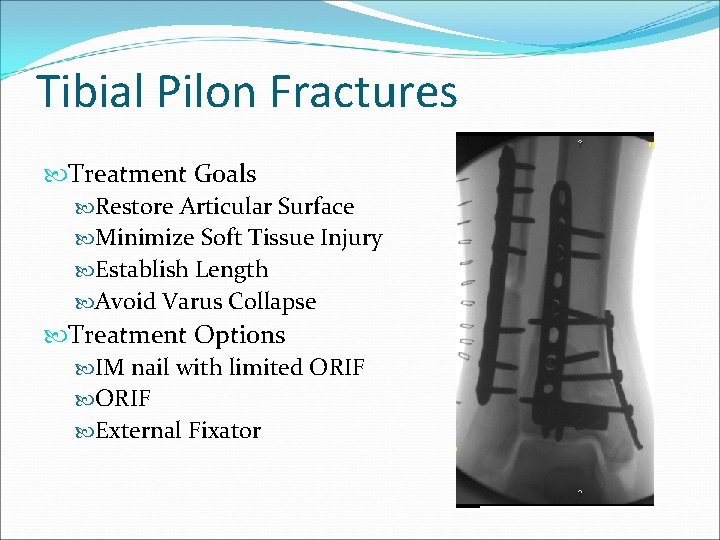
Tibial Pilon Fractures Treatment Goals Restore Articular Surface Minimize Soft Tissue Injury Establish Length Avoid Varus Collapse Treatment Options IM nail with limited ORIF External Fixator
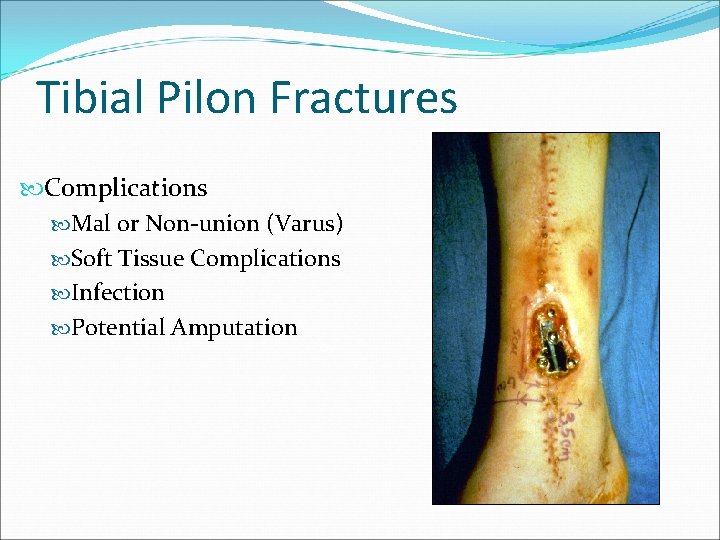
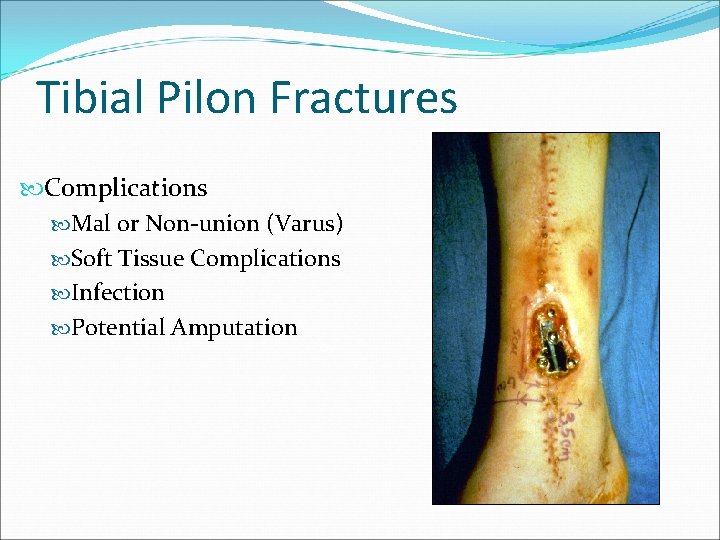
Tibial Pilon Fractures Complications Mal or Non-union (Varus) Soft Tissue Complications Infection Potential Amputation
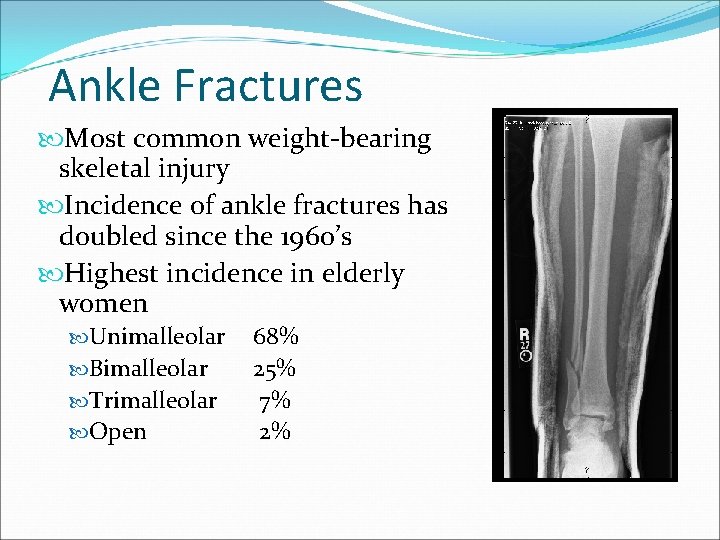
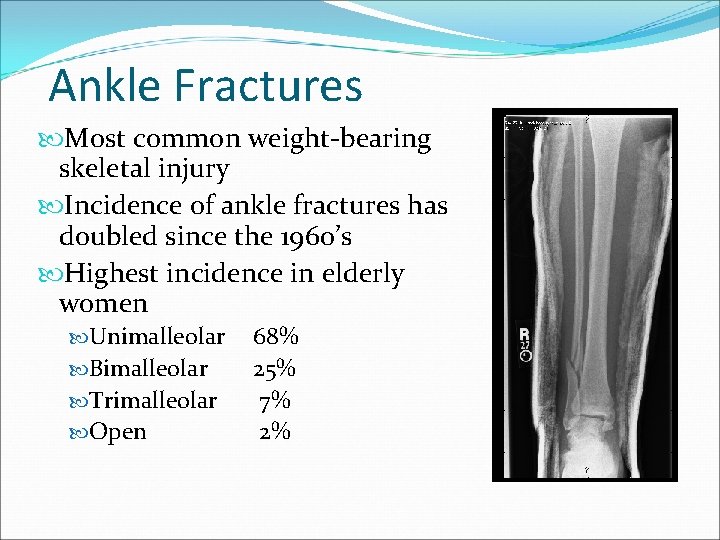
Ankle Fractures Most common weight-bearing skeletal injury Incidence of ankle fractures has doubled since the 1960’s Highest incidence in elderly women Unimalleolar Bimalleolar Trimalleolar Open 68% 25% 7% 2%
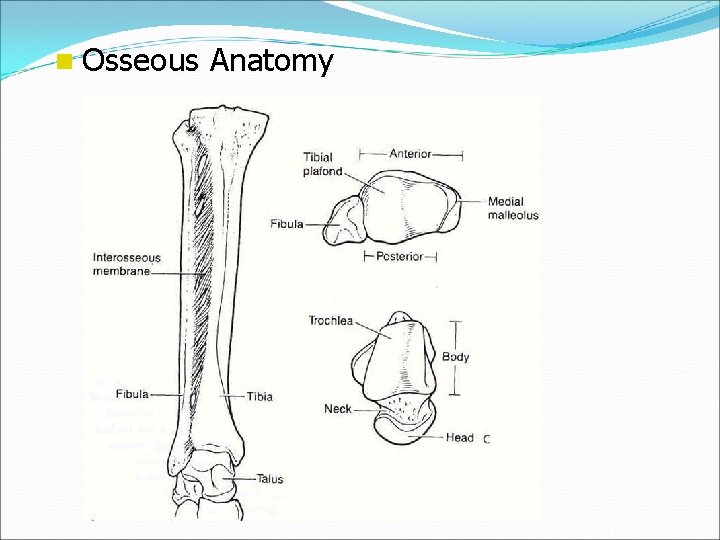
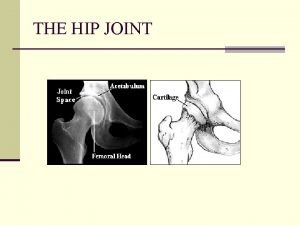
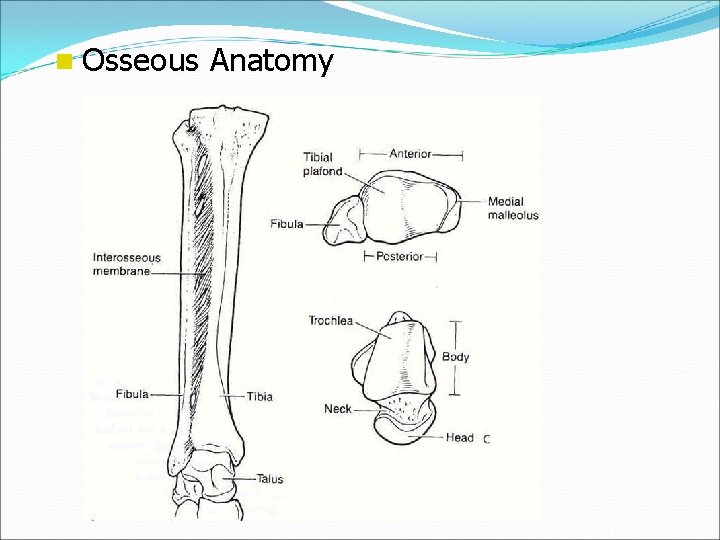
n Osseous Anatomy
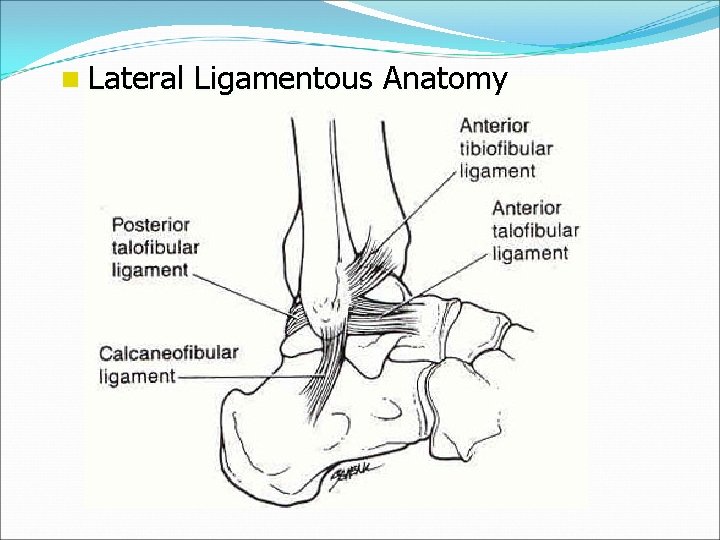
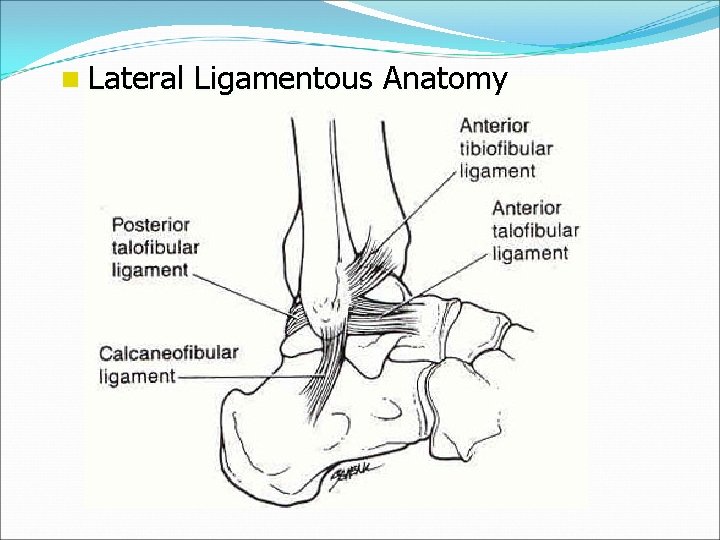
n Lateral Ligamentous Anatomy
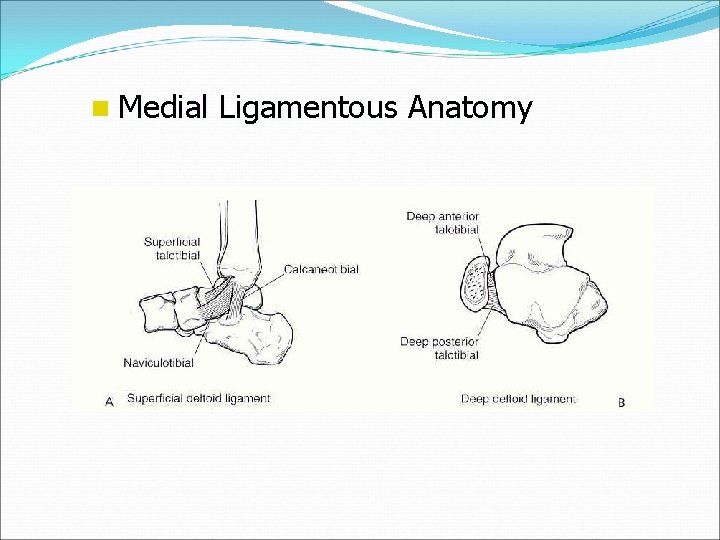
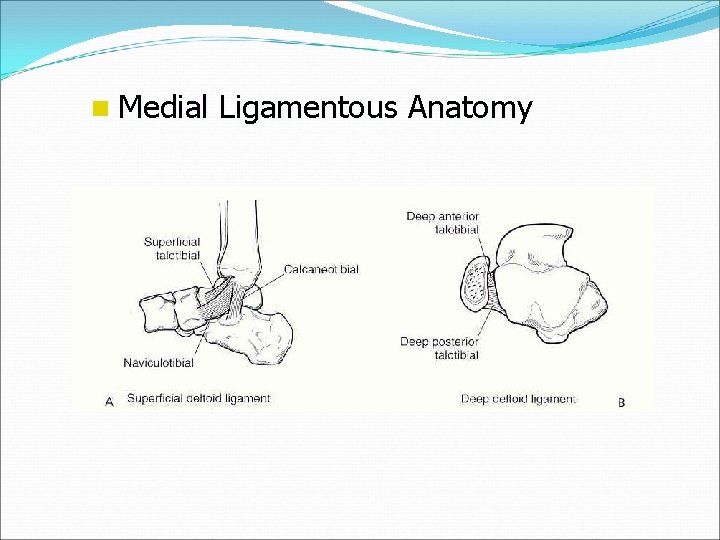
n Medial Ligamentous Anatomy
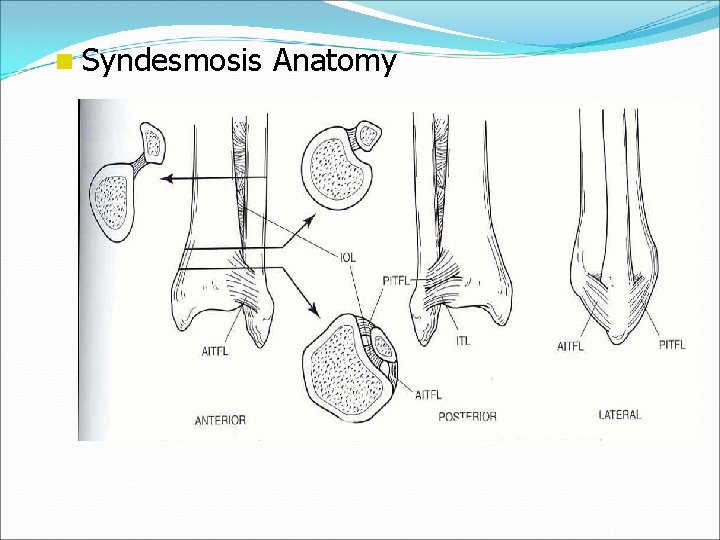
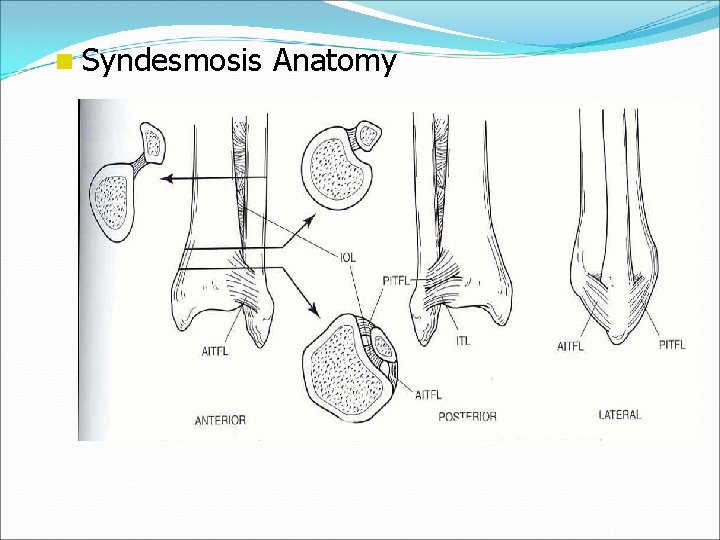
n Syndesmosis Anatomy
Ankle Fractures History Mechanism of injury Time elapsed since the injury Soft-tissue injury Has the patient ambulated on the ankle? Patient’s age / bone quality Associated injuries Comorbidities (DM, smoking)
Ankle Fractures Physical Exam Neurovascular exam Note obvious deformities Pain over the medial or lateral malleoli Palpation of ligaments about the ankle Palpation of proximal fibula, lateral process of talus, base of 5 th MT Examine the hindfoot and forefoot
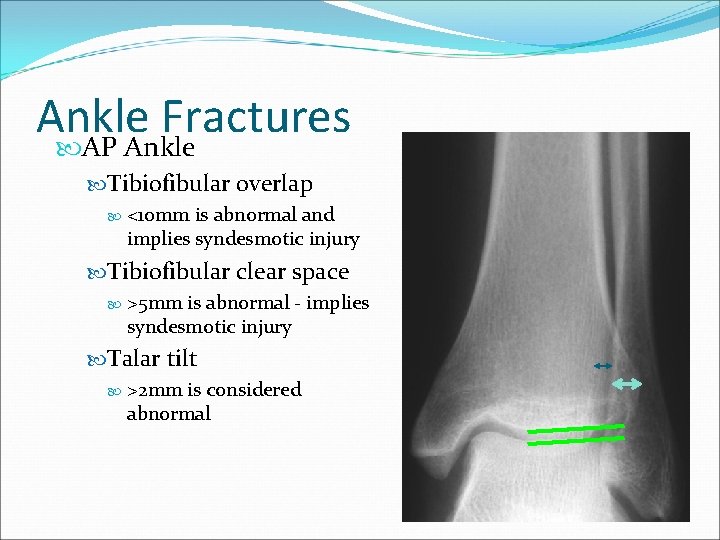
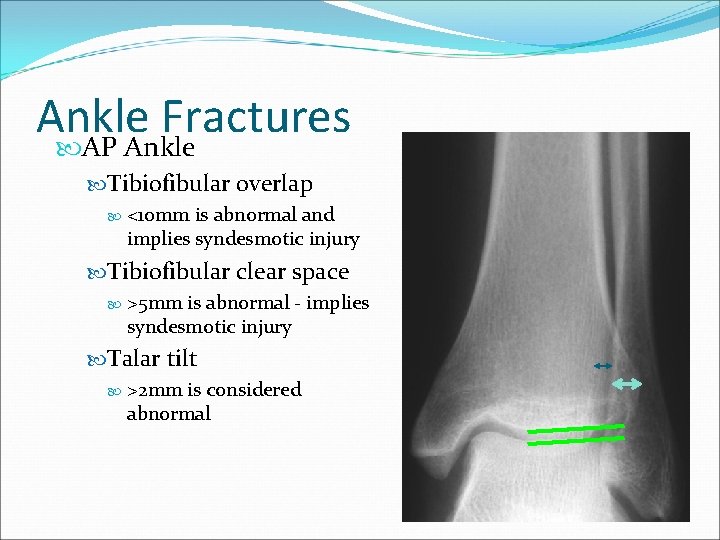
Ankle Fractures AP Ankle Tibiofibular overlap <10 mm is abnormal and implies syndesmotic injury Tibiofibular clear space >5 mm is abnormal - implies syndesmotic injury Talar tilt >2 mm is considered abnormal
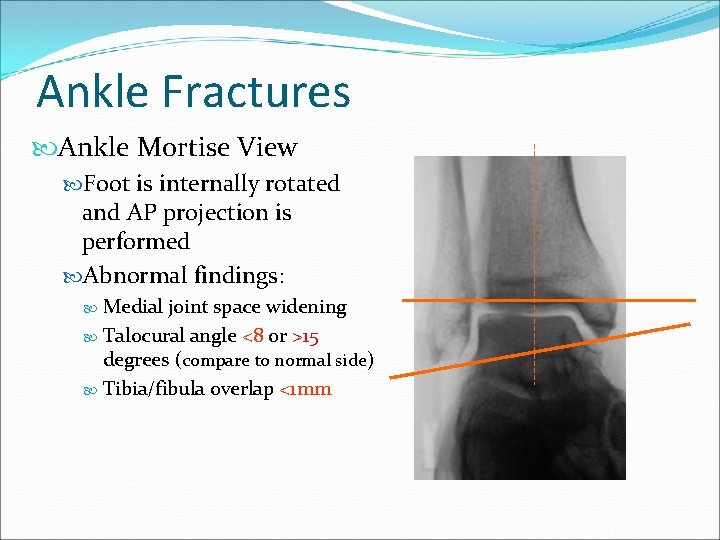
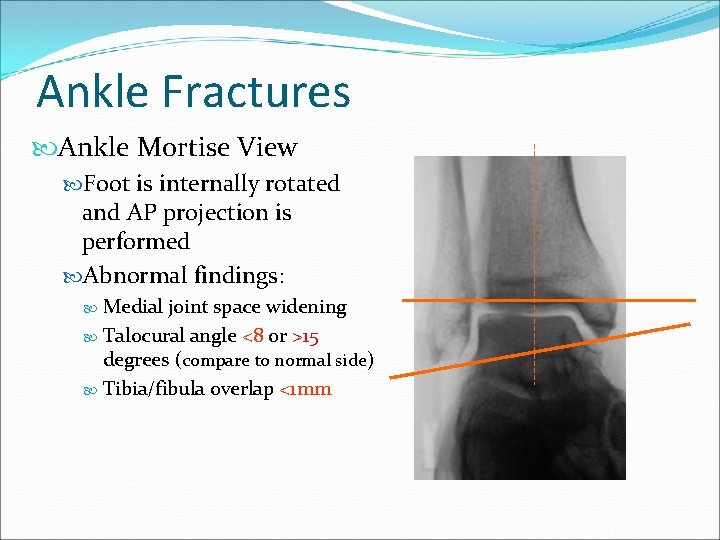
Ankle Fractures Ankle Mortise View Foot is internally rotated and AP projection is performed Abnormal findings: Medial joint space widening Talocural angle <8 or >15 degrees (compare to normal side) Tibia/fibula overlap <1 mm
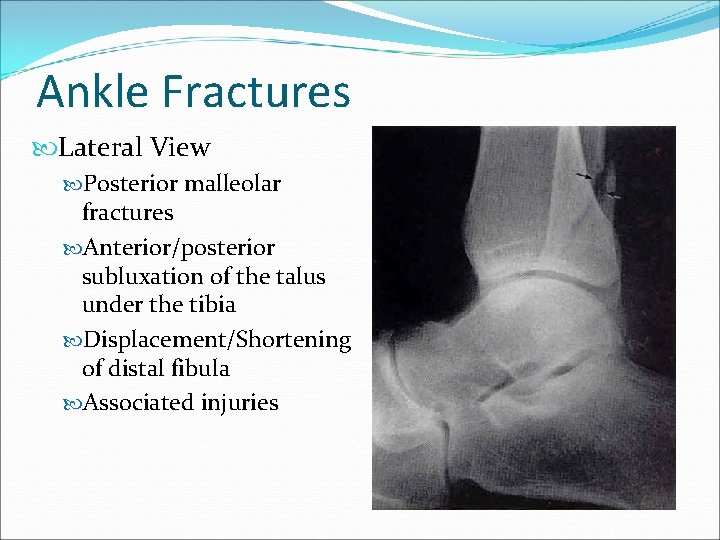
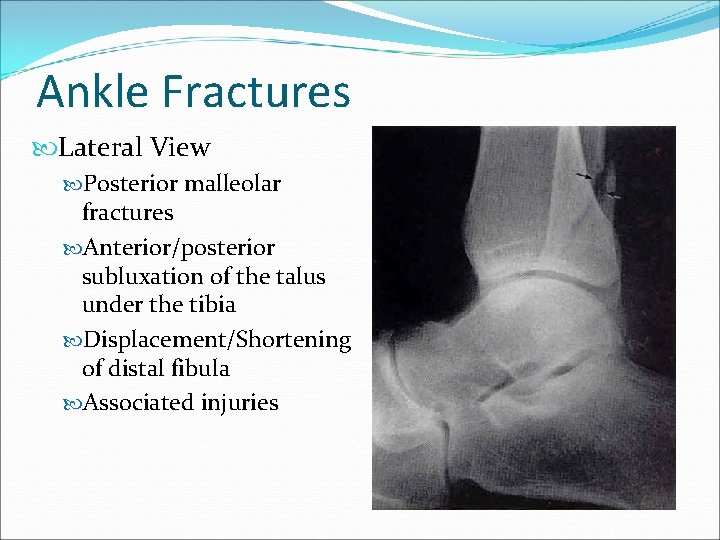
Ankle Fractures Lateral View Posterior malleolar fractures Anterior/posterior subluxation of the talus under the tibia Displacement/Shortening of distal fibula Associated injuries
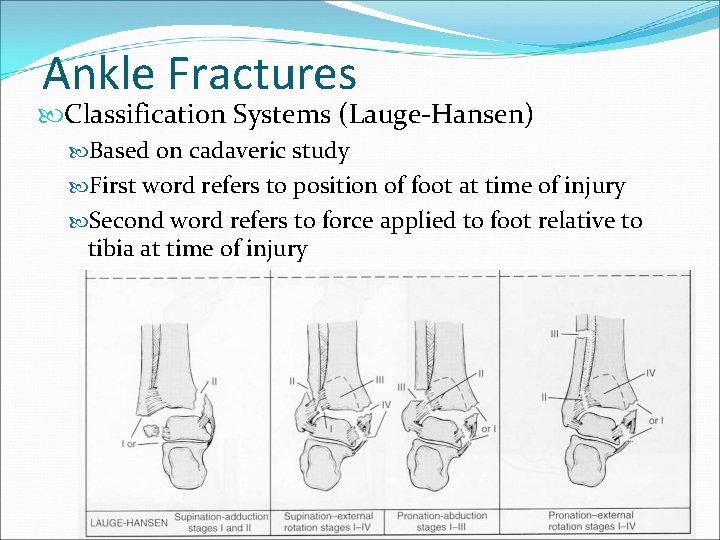
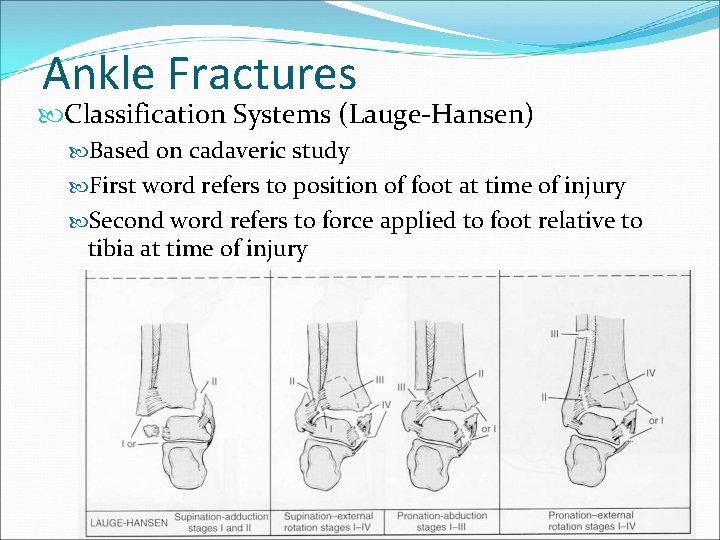
Ankle Fractures Classification Systems (Lauge-Hansen) Based on cadaveric study First word refers to position of foot at time of injury Second word refers to force applied to foot relative to tibia at time of injury
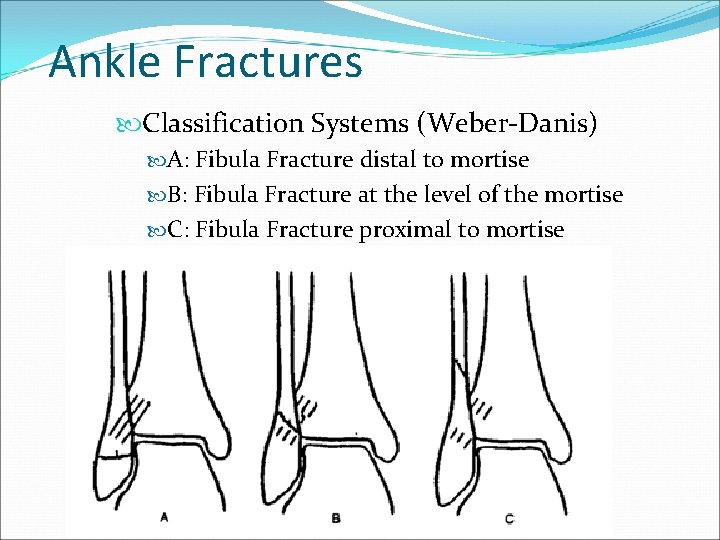
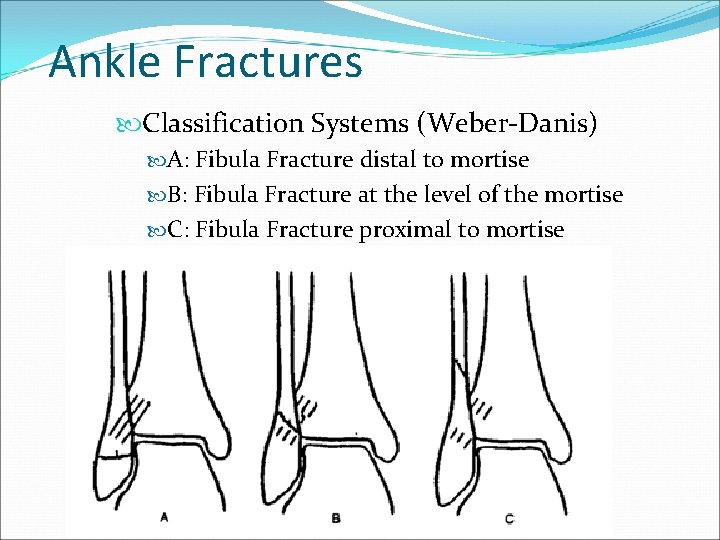
Ankle Fractures Classification Systems (Weber-Danis) A: Fibula Fracture distal to mortise B: Fibula Fracture at the level of the mortise C: Fibula Fracture proximal to mortise
Ankle Fractures Initial Management Closed reduction (conscious sedation may be necessary) Splint Delayed fixation until soft tissues stable Pain control Monitor for possible compartment syndrome in high energy injuries
Ankle Fractures n Indications for non-operative care: – Nondisplaced fracture with intact syndesmosis and stable mortise – Less than 3 mm displacement of the isolated fibula fracture with no medial injury – Patient whose overall condition is unstable and would not tolerate an operative procedure n Management: – WBAT in short leg cast or CAM boot for 4 -6 weeks – Repeat x-ray at 7– 10 days to r/o interval displacement
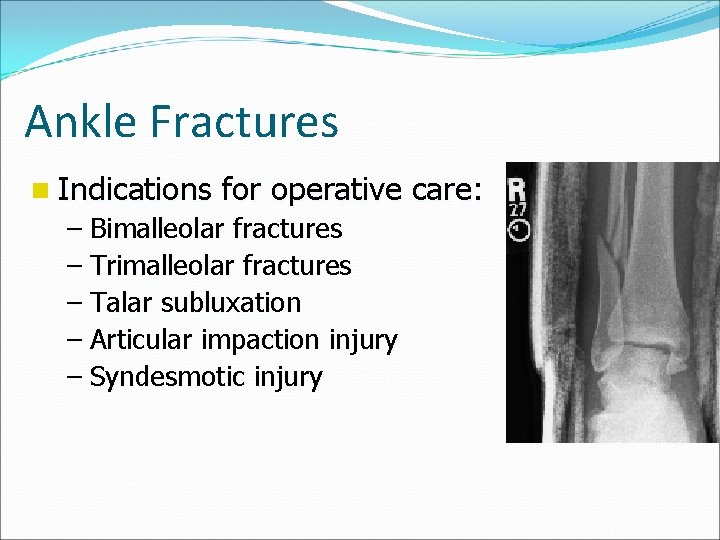
Ankle Fractures n Indications for operative care: – Bimalleolar fractures – Trimalleolar fractures – Talar subluxation – Articular impaction injury – Syndesmotic injury
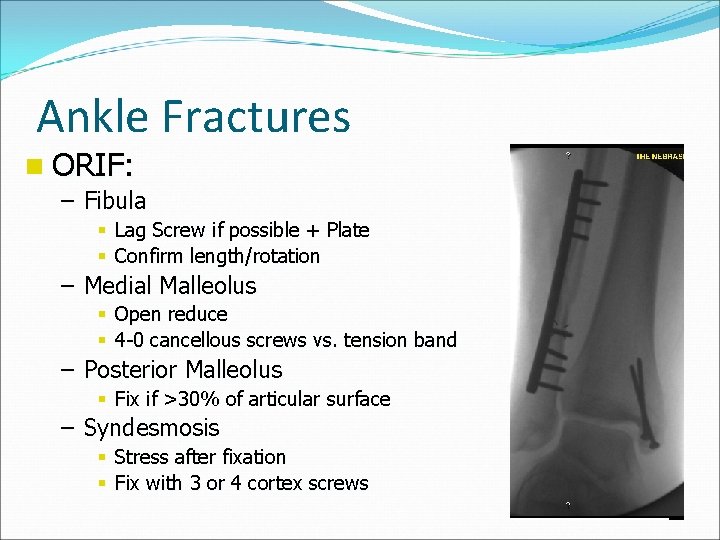
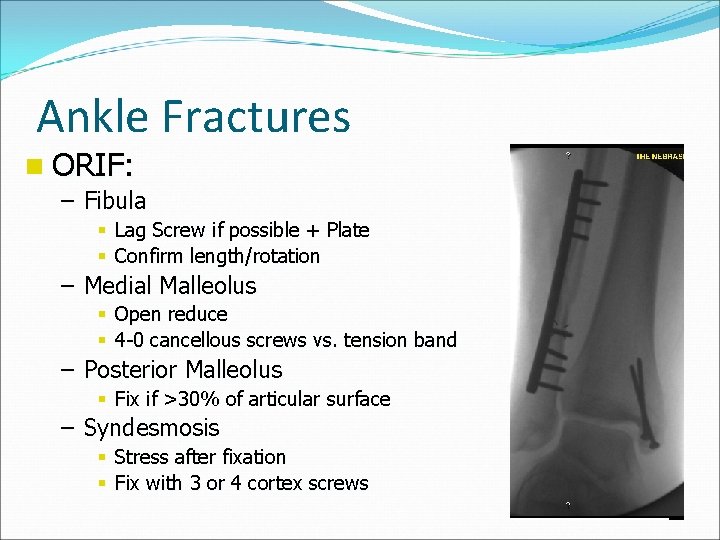
Ankle Fractures n ORIF: – Fibula § Lag Screw if possible + Plate § Confirm length/rotation – Medial Malleolus § Open reduce § 4 -0 cancellous screws vs. tension band – Posterior Malleolus § Fix if >30% of articular surface – Syndesmosis § Stress after fixation § Fix with 3 or 4 cortex screws
Hindfoot Fractures: Talus Calcaneus

Talar fractures: Rare Poor blood supply high incidence of AVN Can be major or minor
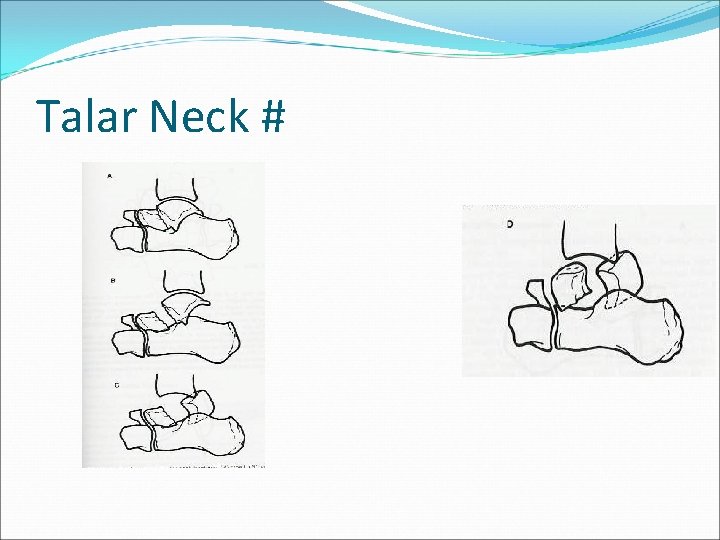
Major Talar fractures: Neck, head, body (& lat process) Talar neck fractures = 50% Hawkins type 1= non displaced + no joint inv. Type II = displaced with subluxation or dislocation of the subtalar joint BUT ankle joint is OK Type III = Type II +dislocation of ankle joint Type IV = Type III + talar head dislocation
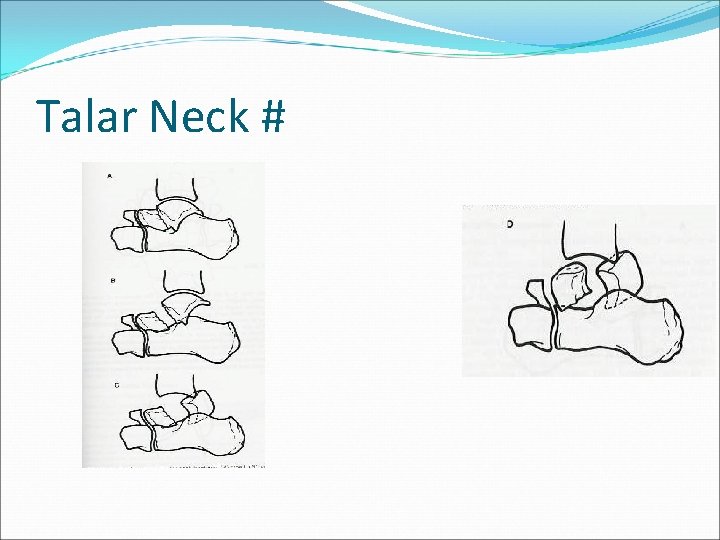
Talar Neck #
R calcaneus x-ray:

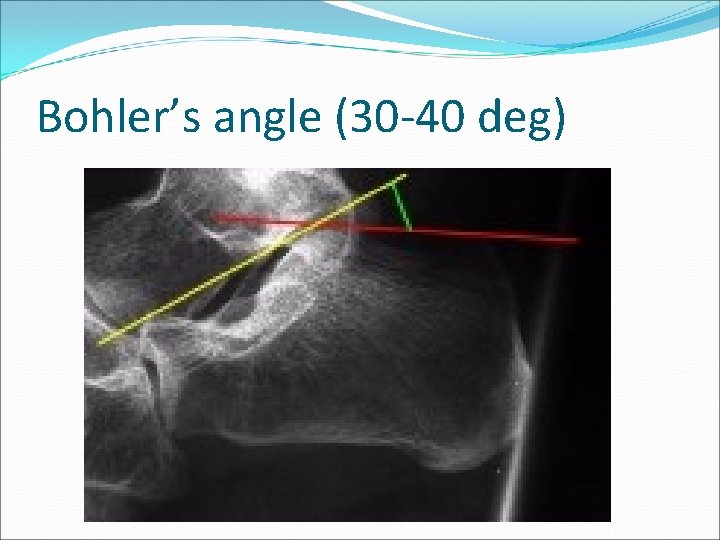
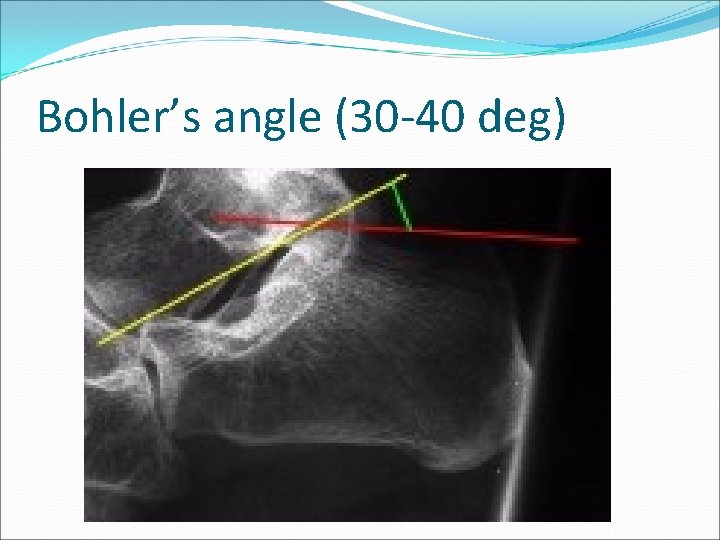
Bohler’s angle (30 -40 deg)
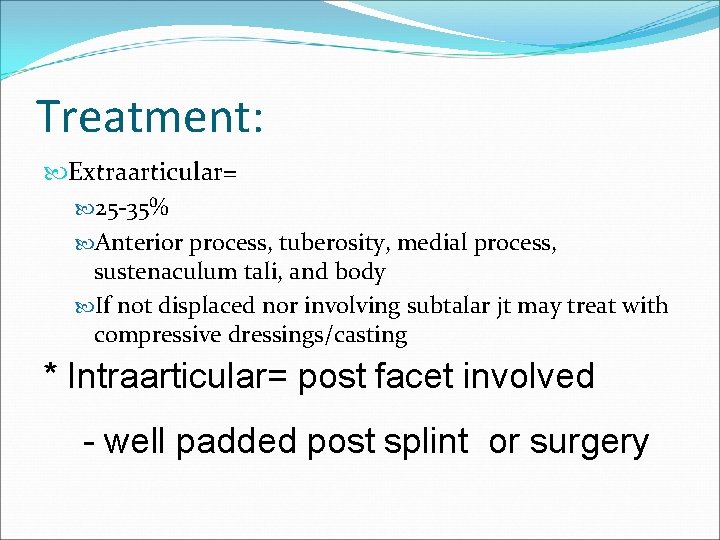
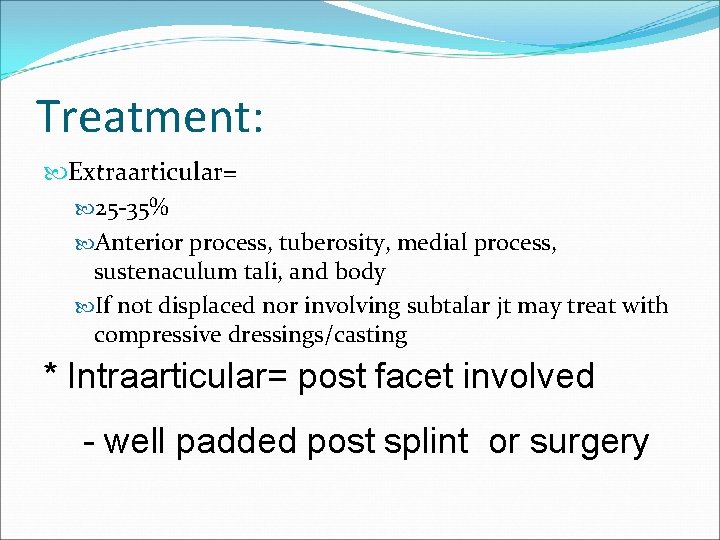
Treatment: Extraarticular= 25 -35% Anterior process, tuberosity, medial process, sustenaculum tali, and body If not displaced nor involving subtalar jt may treat with compressive dressings/casting * Intraarticular= post facet involved - well padded post splint or surgery
Calcaneal fractures: More than 50% are associated with other extremity or spinal fractures
Midfoot Fractures: Navicular Cuboid Lisfranc

Navicular fractures: -Most common midfoot fracture but still rare -treatment= non-displaced=short-leg walking cast x 6 wks displaced : surgery
Cuboid Fractures: Treat as per navicular fractures r/o Lisfranc injury
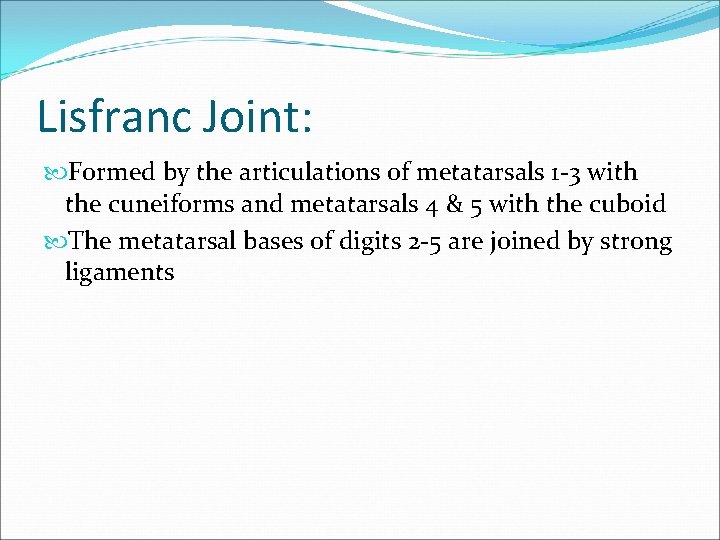
Lisfranc Joint: Formed by the articulations of metatarsals 1 -3 with the cuneiforms and metatarsals 4 & 5 with the cuboid The metatarsal bases of digits 2 -5 are joined by strong ligaments
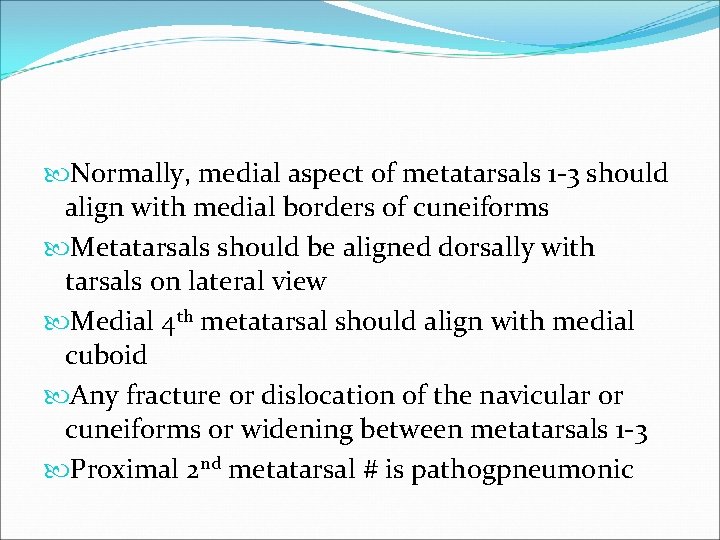
Normally, medial aspect of metatarsals 1 -3 should align with medial borders of cuneiforms Metatarsals should be aligned dorsally with tarsals on lateral view Medial 4 th metatarsal should align with medial cuboid Any fracture or dislocation of the navicular or cuneiforms or widening between metatarsals 1 -3 Proximal 2 nd metatarsal # is pathogpneumonic

Normal Lisfranc joint
Treatment: May try closed reduction with traction but post reduction displacement of >2 mm or tarso-metatarsal angle> 15 degrees requires surgery
Forefoot fractures: Metatarsal Phalangeal
Treatment: Nondisplaced or min displaced fractures of metatarsal 2 -4 stiff shoe, casting, or fracture brace. Non displaced 1 st metatarsal NWB BK walking cast Displaced 1 st or 5 th metatarsal Attempt closed reduction if >3 mm displacement or 10 degrees angulation
Treatment cont. Metatarsal base # r/o LF injury Jones Fracture=5 th metatarsal base fracture. Tx=non displaced NWB BK cast x 6 -8 wks = displaced surgery

Jones #
Dislocations of the Upper Limb
Dislocation of the Shoulder Mostly Anterior > 95 % of dislocations Posterior Dislocation occurs < 5 % True Inferior dislocation (luxatio erecta) occurs < 1% Habitual Non traumatic dislocation may present as Multi directional dislocation due to generalized ligamentous laxity and is Painless
Mechanism of anterior shoulder dislocation Usually Indirect fall on Abducted and extended shoulder May be direct when there is a blow on the shoulder from behind
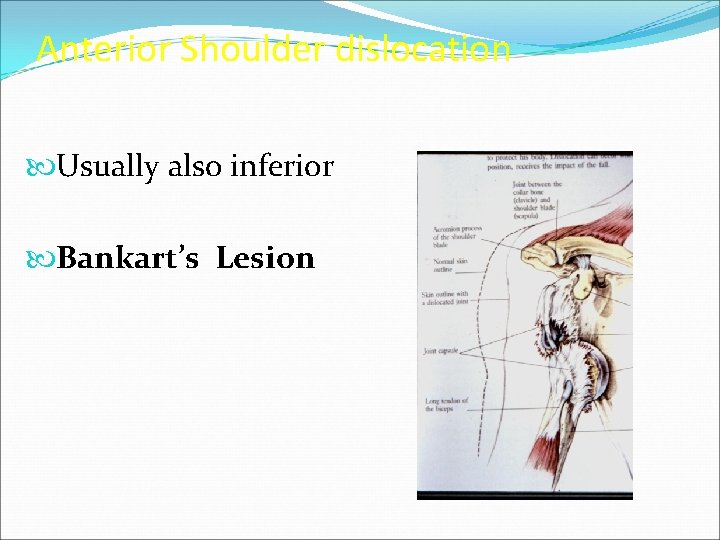
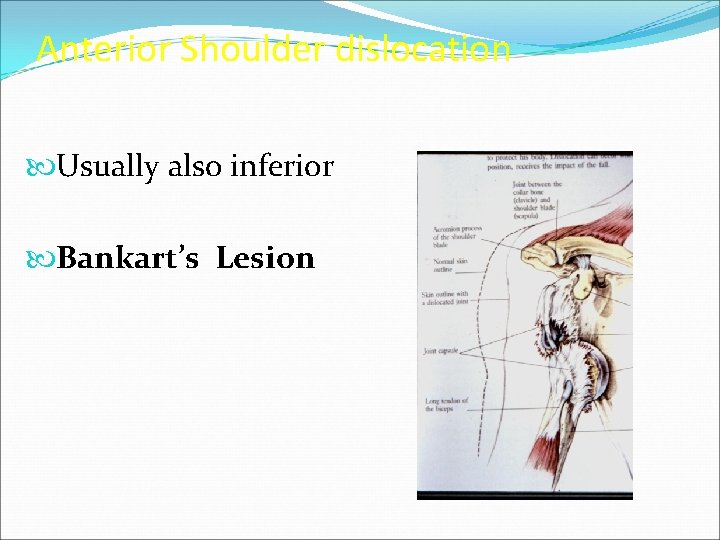
Anterior Shoulder dislocation Usually also inferior Bankart’s Lesion
Clinical Picture Patient is in pain Holds the injured limb with other hand close to the trunk The shoulder is abducted and the elbow is kept flexed There is loss of the normal contour of the shoulder
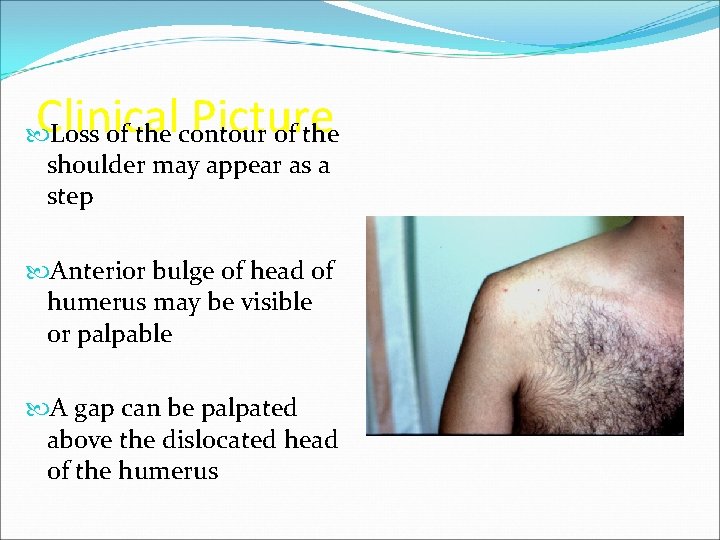
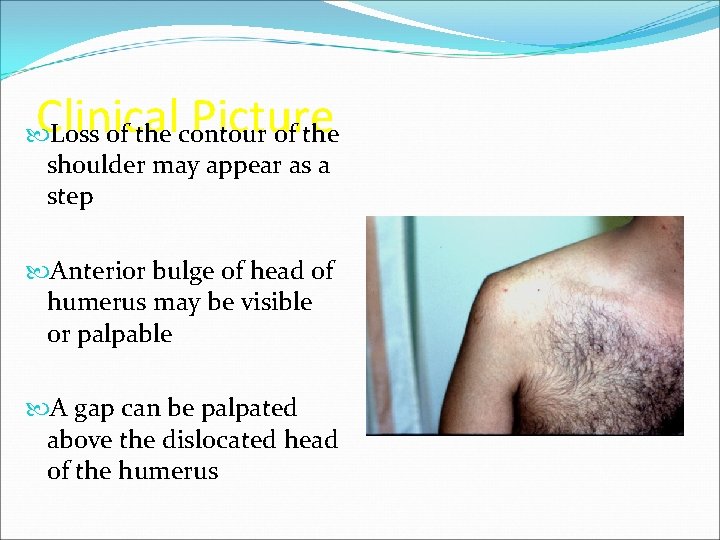
Clinical Picture Loss of the contour of the shoulder may appear as a step Anterior bulge of head of humerus may be visible or palpable A gap can be palpated above the dislocated head of the humerus

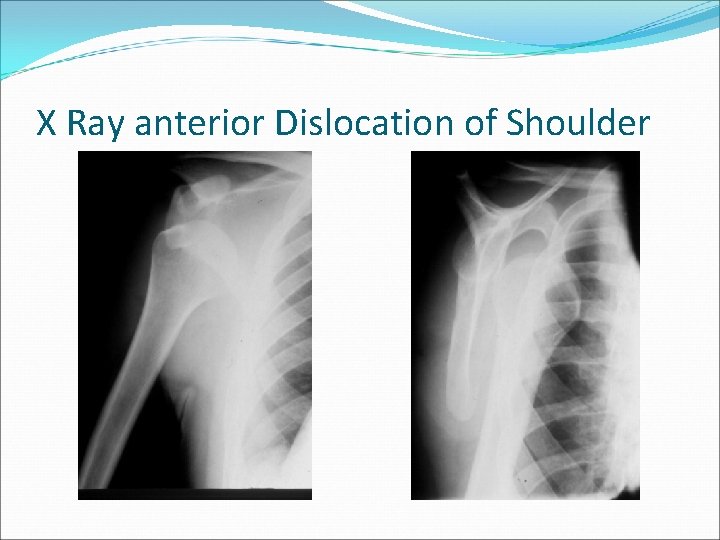
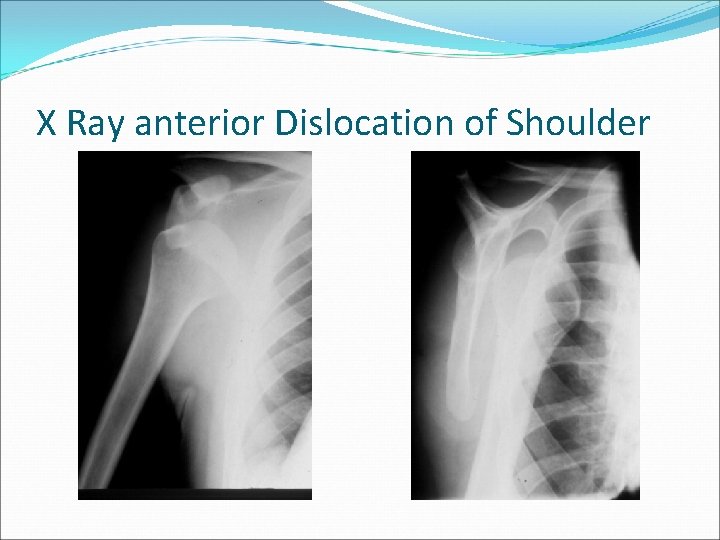
X Ray anterior Dislocation of Shoulder
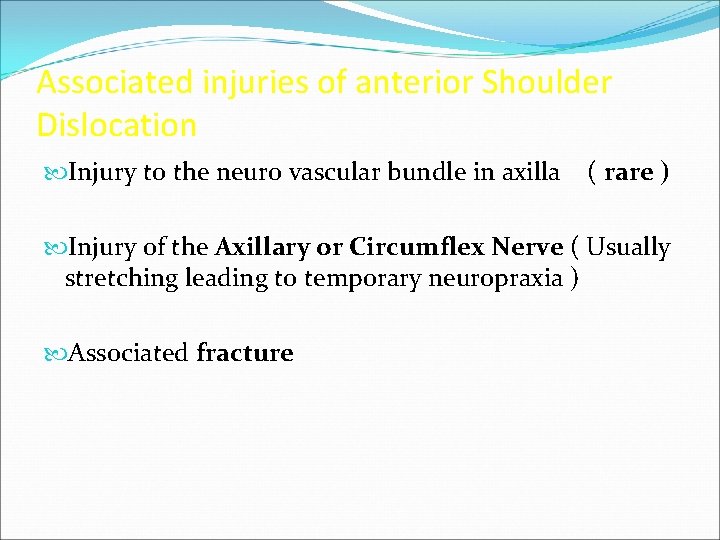
Associated injuries of anterior Shoulder Dislocation Injury to the neuro vascular bundle in axilla ( rare ) Injury of the Axillary or Circumflex Nerve ( Usually stretching leading to temporary neuropraxia ) Associated fracture
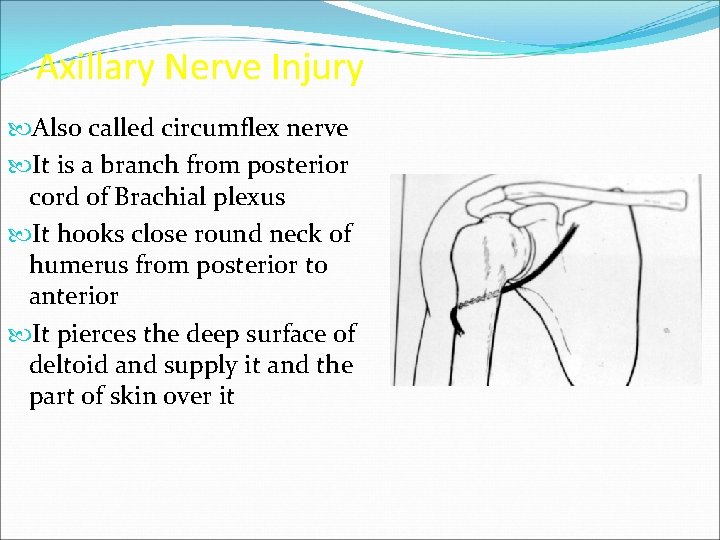
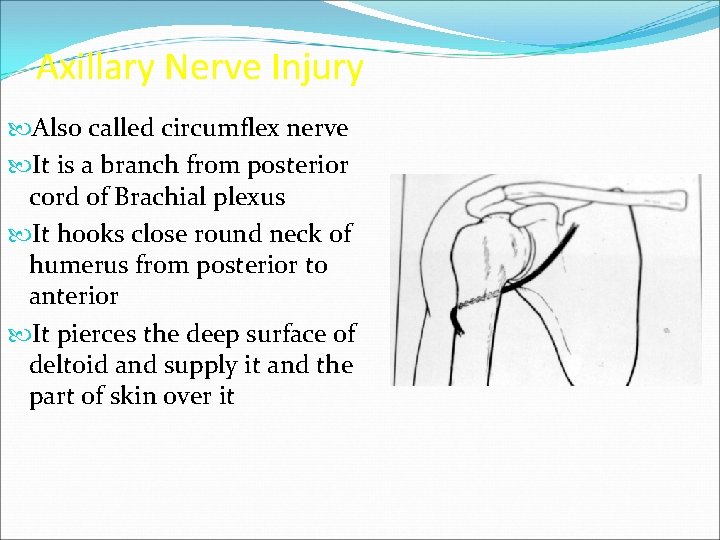
Axillary Nerve Injury Also called circumflex nerve It is a branch from posterior cord of Brachial plexus It hooks close round neck of humerus from posterior to anterior It pierces the deep surface of deltoid and supply it and the part of skin over it

Axillary nerve injury
Management of Anterior Shoulder Dislocation Is an Emergency It should be reduced in less than 24 hours or there may be Avascular Necrosis of head of humerus Following reduction the shoulder should be immobilised strapped to the trunk for 3 -4 weeks and rested in a collar and cuff
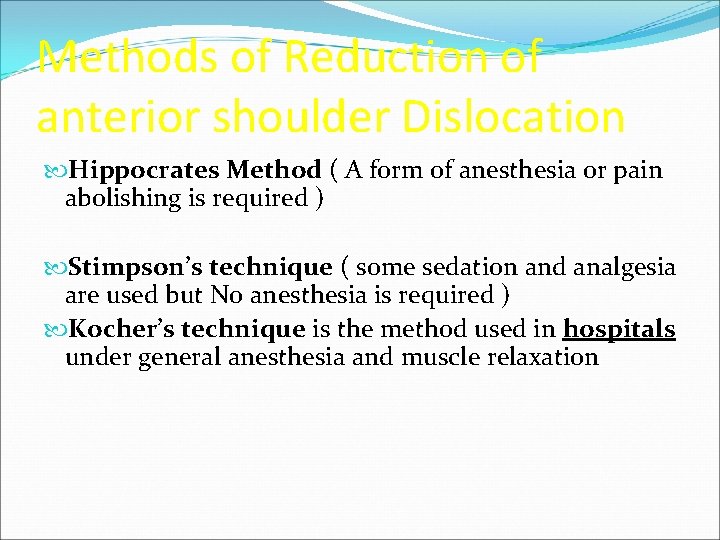
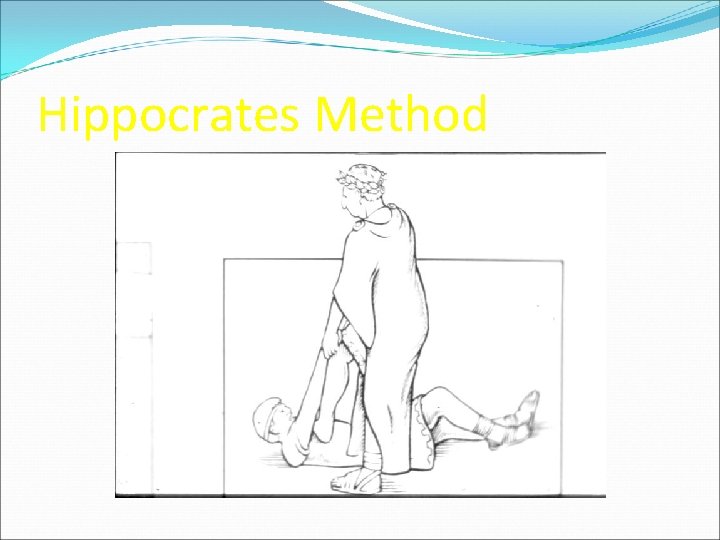
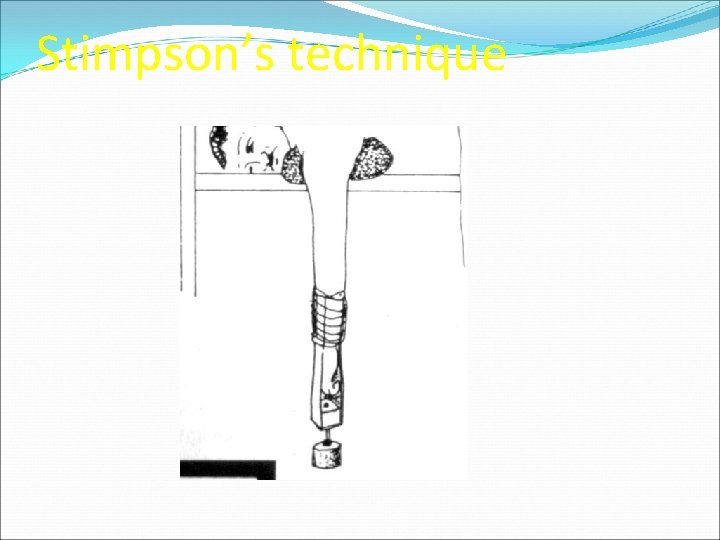
Methods of Reduction of anterior shoulder Dislocation Hippocrates Method ( A form of anesthesia or pain abolishing is required ) Stimpson’s technique ( some sedation and analgesia are used but No anesthesia is required ) Kocher’s technique is the method used in hospitals under general anesthesia and muscle relaxation
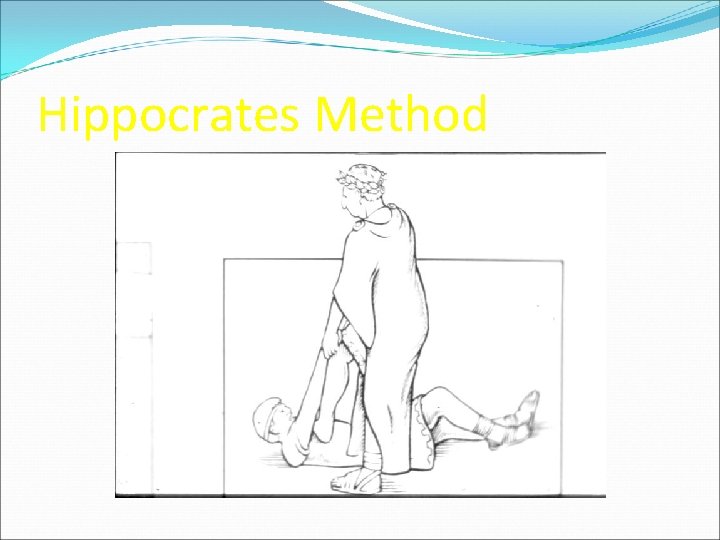
Hippocrates Method
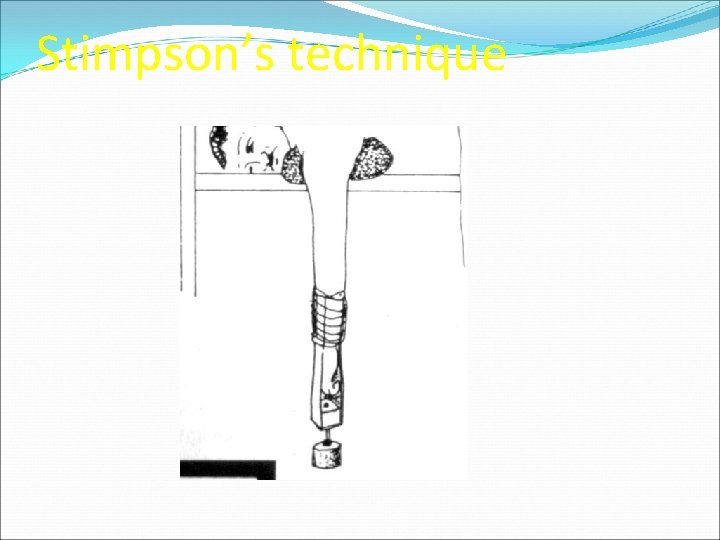
Stimpson’s technique

Kocher’s Technique
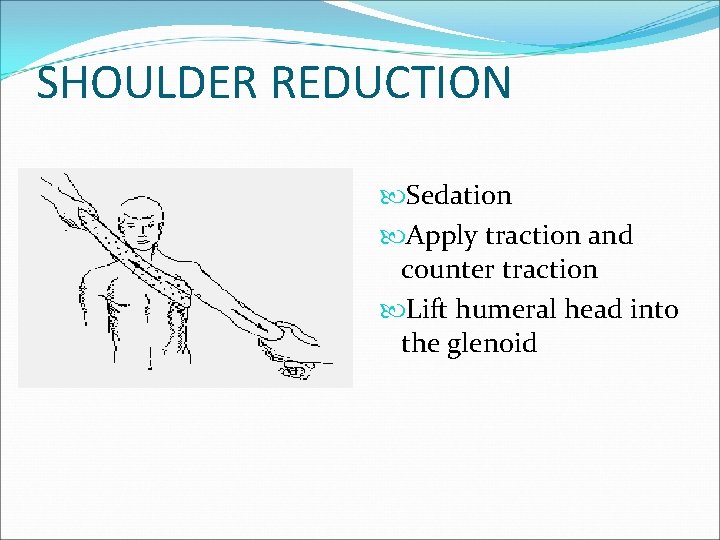
SHOULDER REDUCTION Sedation Apply traction and counter traction Lift humeral head into the glenoid
Complications of anterior Shoulder Dislocation : Early Neuro vascular injury ( rare ) Axillary nerve injury Associated Fracture of neck of humerus or greater or lesser tuberosities
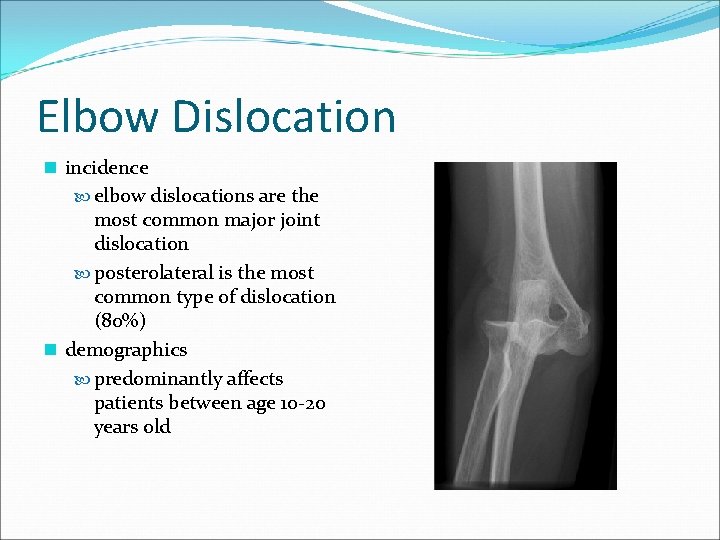
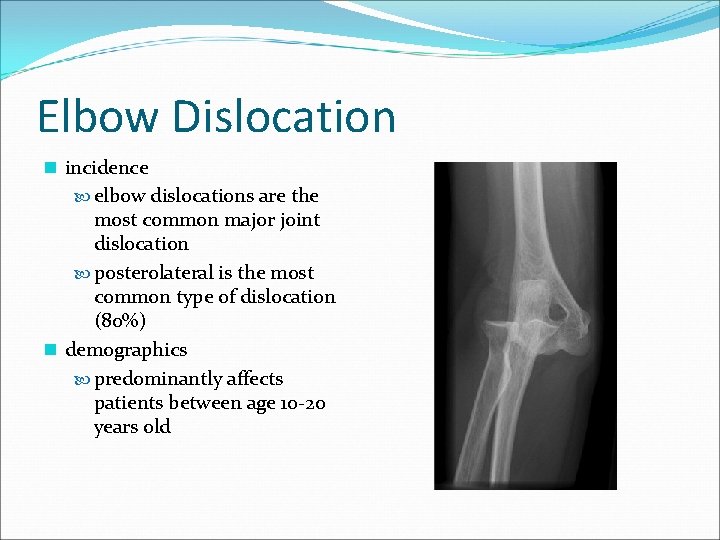
Elbow Dislocation n incidence elbow dislocations are the most common major joint dislocation posterolateral is the most common type of dislocation (80%) n demographics predominantly affects patients between age 10 -20 years old
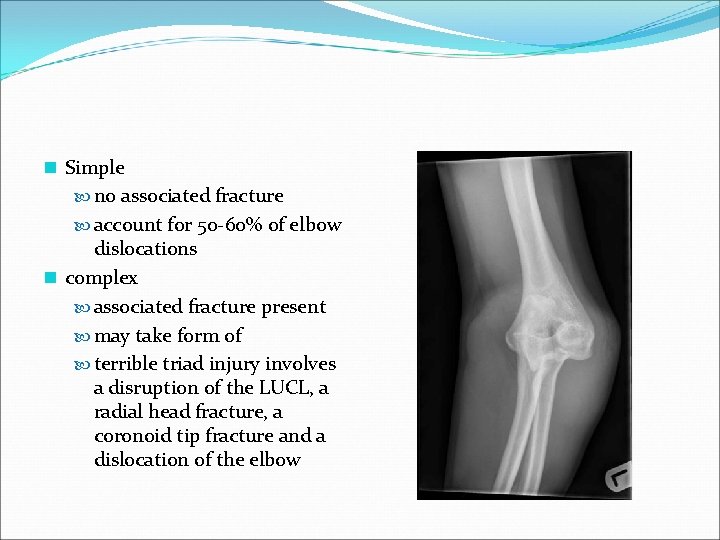
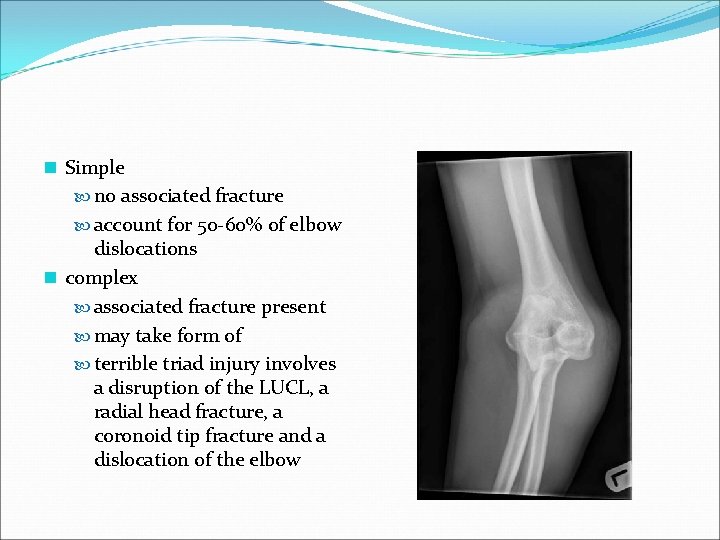
n Simple no associated fracture account for 50 -60% of elbow dislocations n complex associated fracture present may take form of terrible triad injury involves a disruption of the LUCL, a radial head fracture, a coronoid tip fracture and a dislocation of the elbow

Fracture dislocation
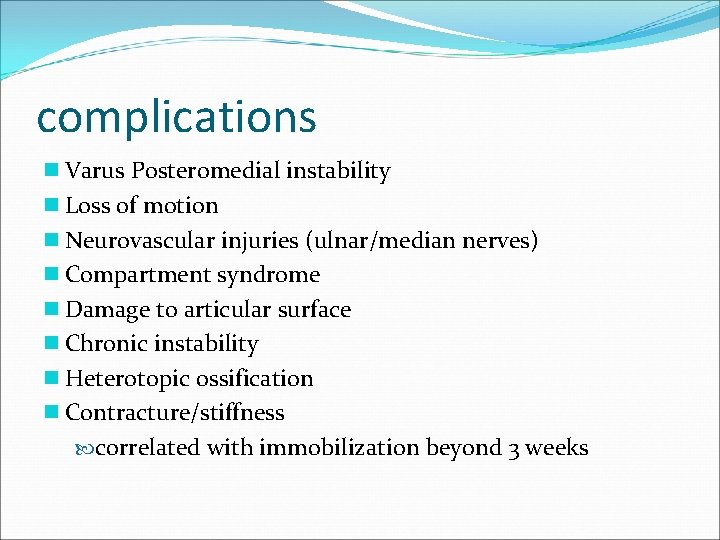
complications n Varus Posteromedial instability n Loss of motion n Neurovascular injuries (ulnar/median nerves) n Compartment syndrome n Damage to articular surface n Chronic instability n Heterotopic ossification n Contracture/stiffness correlated with immobilization beyond 3 weeks
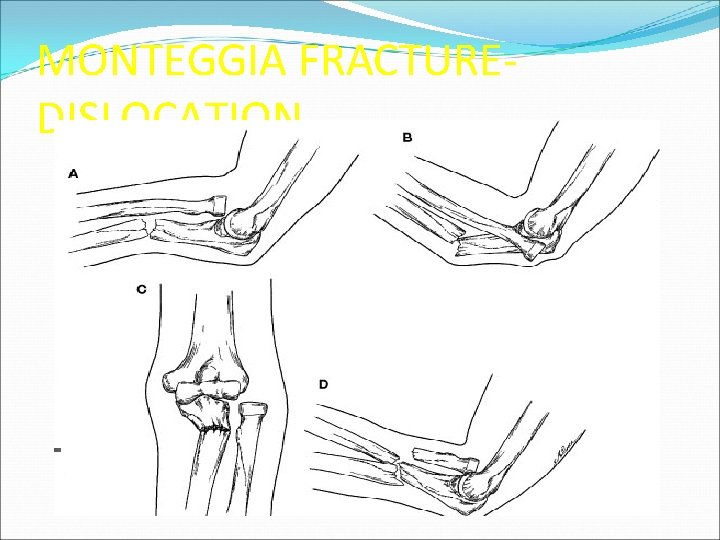
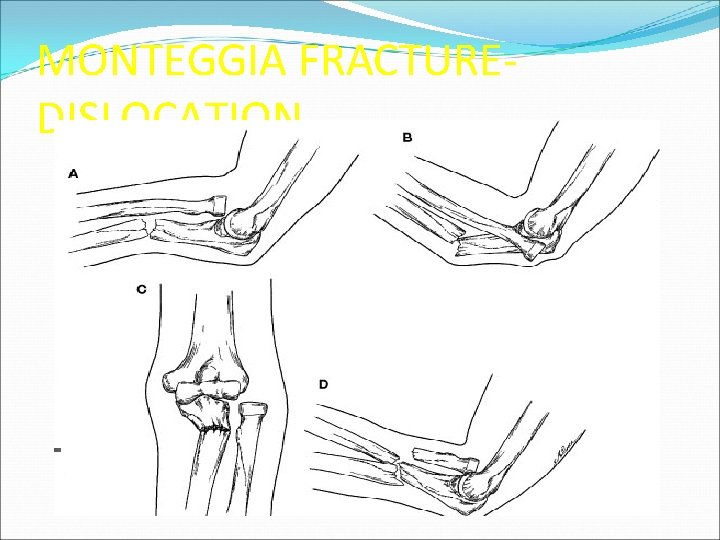
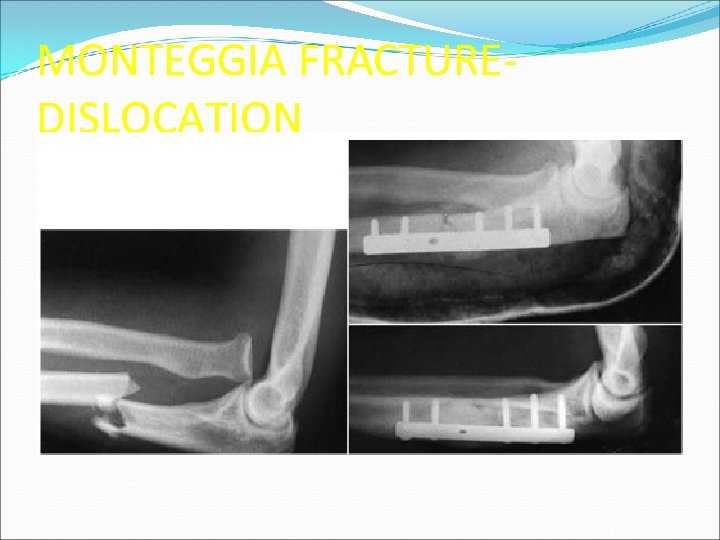
MONTEGGIA FRACTUREDISLOCATION
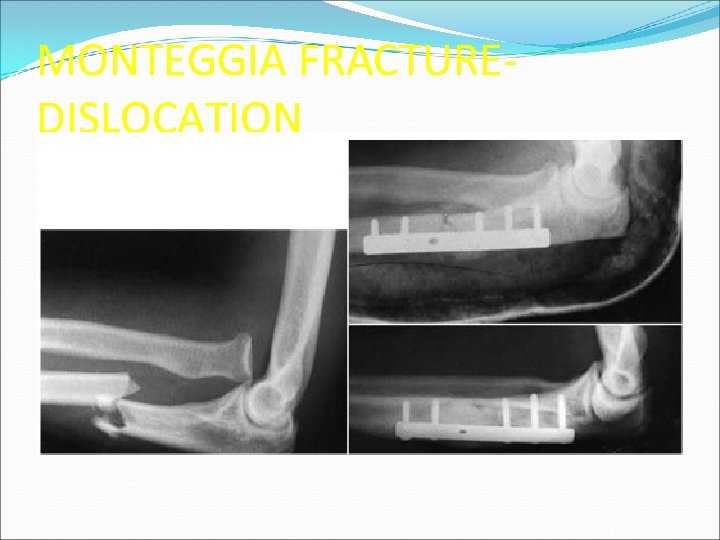
MONTEGGIA FRACTUREDISLOCATION

GALEAZZI FRACTUREDISLOCATION

 Popliteal pulse
Popliteal pulse Skeletal system
Skeletal system Diagonal patterns pnf
Diagonal patterns pnf Posterior tibial artery pulse
Posterior tibial artery pulse Left lower extremity
Left lower extremity Posterior tibial pulse
Posterior tibial pulse Lower extremity muscles
Lower extremity muscles Spasticity definition
Spasticity definition Hip hop hip to the hippity
Hip hop hip to the hippity Hip hop hip to the hippity
Hip hop hip to the hippity Olecranon bursitis irving
Olecranon bursitis irving Bobine d andrieu
Bobine d andrieu Types of fractures with pictures
Types of fractures with pictures Arc antérieur du bassin
Arc antérieur du bassin Fracture supracondylienne coude classification
Fracture supracondylienne coude classification Acetabular fractures
Acetabular fractures Daniel tibia
Daniel tibia Radial and concentric fractures
Radial and concentric fractures Types of fractures with pictures
Types of fractures with pictures Parts of a chest tube
Parts of a chest tube Types of glass fractures
Types of glass fractures Weber classification
Weber classification Dr sukhpal singh
Dr sukhpal singh Radial lines glass
Radial lines glass Tubular shaft of a long bone
Tubular shaft of a long bone Primary bone vs secondary bone
Primary bone vs secondary bone Non union types
Non union types Open fracture treatment
Open fracture treatment Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Acetabular fractures
Acetabular fractures Panfacial fractures sequencing
Panfacial fractures sequencing Moving and lifting of the patient
Moving and lifting of the patient Elbow restraints for pediatrics
Elbow restraints for pediatrics Orrin franko
Orrin franko Upper limb dermatome distribution
Upper limb dermatome distribution Maggie knott pnf
Maggie knott pnf Purple wristband meaning hospital
Purple wristband meaning hospital Open chain and closed chain kinematics
Open chain and closed chain kinematics Biomechanics of upper extremity
Biomechanics of upper extremity Superficial vein of upper limb
Superficial vein of upper limb Ischiopubic
Ischiopubic Hip hop presentation
Hip hop presentation L2 hip flexion
L2 hip flexion Hip hop prezentace
Hip hop prezentace Army hip pocket scholarship
Army hip pocket scholarship Gummy bear directional and regional terms practice
Gummy bear directional and regional terms practice Copyright
Copyright Hip bone
Hip bone Hip international
Hip international Hip joint labelled
Hip joint labelled Hip fracture x rays
Hip fracture x rays Hip hop history timeline
Hip hop history timeline Parallel chord truss flat roof
Parallel chord truss flat roof Os elementos constitutivos da dança
Os elementos constitutivos da dança Hip joint ppt
Hip joint ppt Hip internal rotation goniometry
Hip internal rotation goniometry Protocolo sctp
Protocolo sctp Coxa plana
Coxa plana Elbow flexion test
Elbow flexion test Bilateral hip disarticulation
Bilateral hip disarticulation Acsm body fat chart
Acsm body fat chart Fibular head
Fibular head Kool rock steady death
Kool rock steady death Cappagh hospital day ward
Cappagh hospital day ward Site:slidetodoc.com
Site:slidetodoc.com Gable roof plan
Gable roof plan Ball and socket joint
Ball and socket joint Parts of a trouser
Parts of a trouser Hipennial
Hipennial Hands up hands down hands on hips sit down
Hands up hands down hands on hips sit down Reggae referat
Reggae referat Hip club
Hip club Thigh contusion
Thigh contusion Eksternal rotasi hip
Eksternal rotasi hip Distinguished toastmaster
Distinguished toastmaster Acetabulum hip
Acetabulum hip Spinal reflexology chart
Spinal reflexology chart Waist to hip ratio
Waist to hip ratio Hip hi
Hip hi Nelaton's line test
Nelaton's line test Hip hop publications
Hip hop publications Osteokinematics of hip joint
Osteokinematics of hip joint Shakespeare flocabulary answers
Shakespeare flocabulary answers Seahawks tackling drills
Seahawks tackling drills Squat pelvic tilt
Squat pelvic tilt Hilton's law
Hilton's law Sole medical term
Sole medical term Agiab
Agiab Occupational therapy hip replacement interventions
Occupational therapy hip replacement interventions Galeazzi sign
Galeazzi sign X-ray hip joint
X-ray hip joint Medial rotation of hip muscles
Medial rotation of hip muscles Closed packed position of hip
Closed packed position of hip Hip hop subkultur
Hip hop subkultur Example of roof plan
Example of roof plan Chapter 17 the thigh hip groin and pelvis
Chapter 17 the thigh hip groin and pelvis Von rosen splint
Von rosen splint Piston test for hip dislocation
Piston test for hip dislocation Hip tiles
Hip tiles Supratrochanteric
Supratrochanteric Skiffy hip
Skiffy hip Hip surgery
Hip surgery Knee goniometry
Knee goniometry Hip dysplasia alpha angle
Hip dysplasia alpha angle Evans jensen classification
Evans jensen classification Hip hughes christianity
Hip hughes christianity Infrahyoid
Infrahyoid Dysplacia
Dysplacia Piston test for hip dislocation
Piston test for hip dislocation Hip fracture care clinical care standard
Hip fracture care clinical care standard Pots fracture
Pots fracture How to treat bursitis in the hip
How to treat bursitis in the hip Bo jackson hip dislocation
Bo jackson hip dislocation Curiosidades hip hop
Curiosidades hip hop Nerves in the hip
Nerves in the hip Hip hop php
Hip hop php Characteristics of rap
Characteristics of rap 99 p
99 p Nelaton triangle
Nelaton triangle Taskforce uk hip hop
Taskforce uk hip hop Hip implant materials
Hip implant materials Open basket weave taping purpose
Open basket weave taping purpose Glutal fold
Glutal fold Hip international limited
Hip international limited Psoas sign
Psoas sign Bryant traction
Bryant traction Pelvic internal rotation
Pelvic internal rotation