Longterm Followup after Vascularized Contralateral Ulnar Nerve Transfer
- Slides: 1
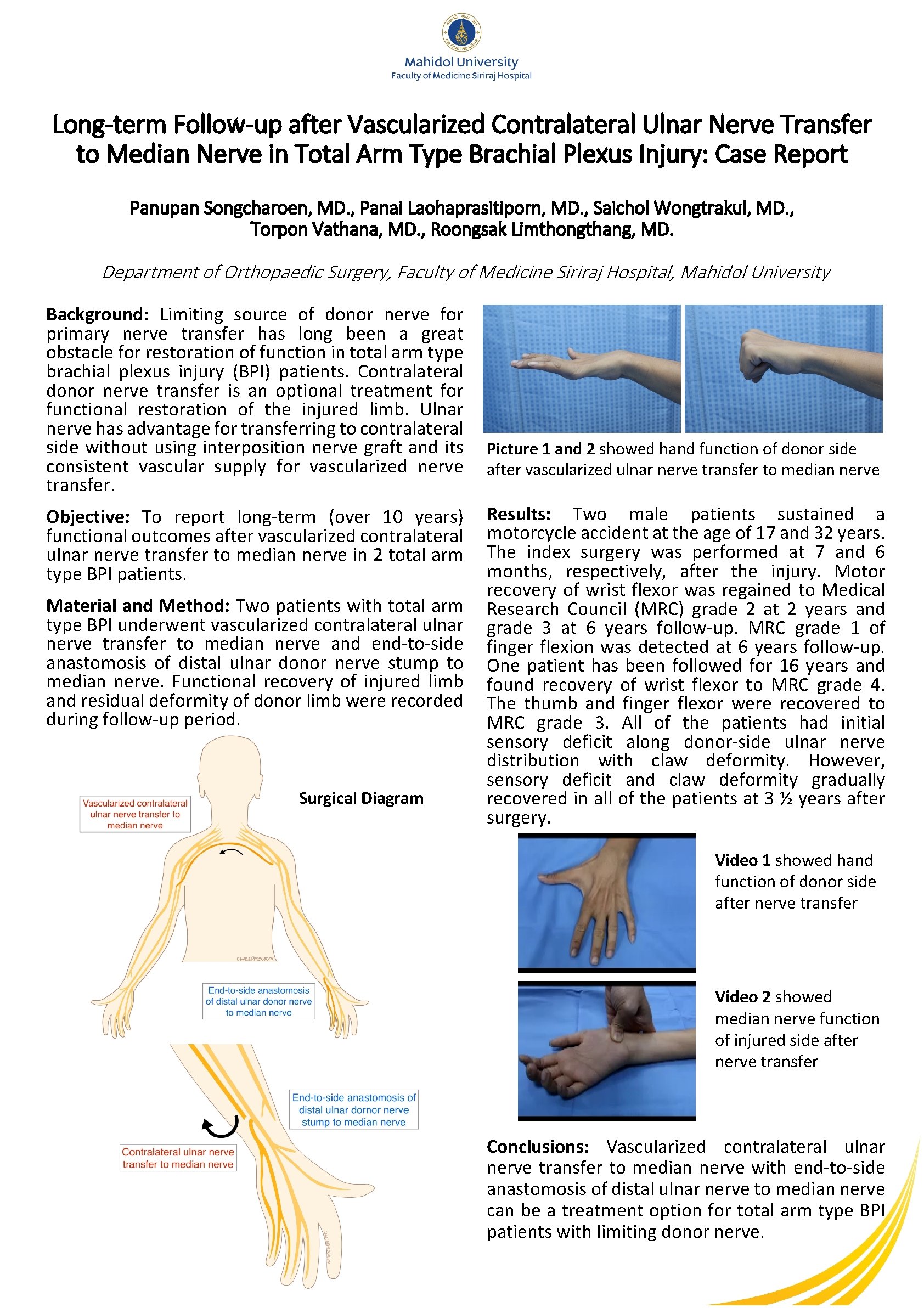
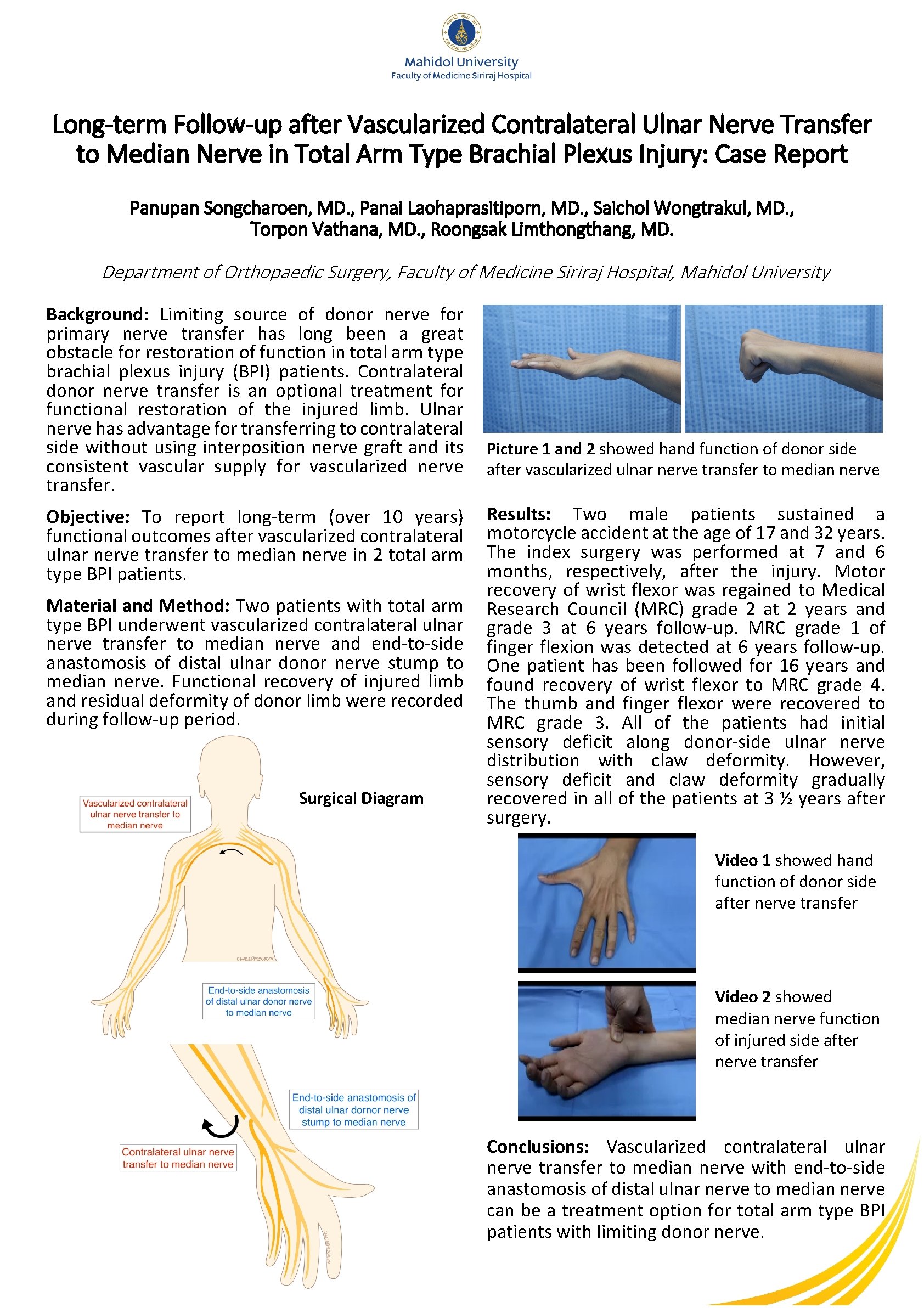
Long-term Follow-up after Vascularized Contralateral Ulnar Nerve Transfer to Median Nerve in Total Arm Type Brachial Plexus Injury: Case Report Panupan Songcharoen, MD. , Panai Laohaprasitiporn, MD. , Saichol Wongtrakul, MD. , Torpon Vathana, MD. , Roongsak Limthongthang, MD. Department of Orthopaedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University Background: Limiting source of donor nerve for primary nerve transfer has long been a great obstacle for restoration of function in total arm type brachial plexus injury (BPI) patients. Contralateral donor nerve transfer is an optional treatment for functional restoration of the injured limb. Ulnar nerve has advantage for transferring to contralateral side without using interposition nerve graft and its consistent vascular supply for vascularized nerve transfer. Objective: To report long-term (over 10 years) functional outcomes after vascularized contralateral ulnar nerve transfer to median nerve in 2 total arm type BPI patients. Material and Method: Two patients with total arm type BPI underwent vascularized contralateral ulnar nerve transfer to median nerve and end-to-side anastomosis of distal ulnar donor nerve stump to median nerve. Functional recovery of injured limb and residual deformity of donor limb were recorded during follow-up period. Surgical Diagram Picture 1 and 2 showed hand function of donor side after vascularized ulnar nerve transfer to median nerve Results: Two male patients sustained a motorcycle accident at the age of 17 and 32 years. The index surgery was performed at 7 and 6 months, respectively, after the injury. Motor recovery of wrist flexor was regained to Medical Research Council (MRC) grade 2 at 2 years and grade 3 at 6 years follow-up. MRC grade 1 of finger flexion was detected at 6 years follow-up. One patient has been followed for 16 years and found recovery of wrist flexor to MRC grade 4. The thumb and finger flexor were recovered to MRC grade 3. All of the patients had initial sensory deficit along donor-side ulnar nerve distribution with claw deformity. However, sensory deficit and claw deformity gradually recovered in all of the patients at 3 ½ years after surgery. Video 1 showed hand function of donor side after nerve transfer Video 2 showed median nerve function of injured side after nerve transfer Conclusions: Vascularized contralateral ulnar nerve transfer to median nerve with end-to-side anastomosis of distal ulnar nerve to median nerve can be a treatment option for total arm type BPI patients with limiting donor nerve.