LONG ACTING REVERSIBLE CONTRACEPTIVES The Basics Objectives Explain
LONG ACTING REVERSIBLE CONTRACEPTIVES The Basics
Objectives • Explain the basic information for history taking and counseling patients on LARCs (IUDs and Implants), including contraindications. • Utilize online resources for patient education and clinician references regarding medical eligibility. • Demonstrate the techniques for insertion and removal of LARC.
Contraceptive users in the US • 61 million US women in childbearing years • ~43 million of them (70%) are at risk of unintended pregnancy • 62% of women of reproductive age currently using some form of contraception • Couples who don’t use contraception have ~85% chance of experiencing pregnancy over the course of a year
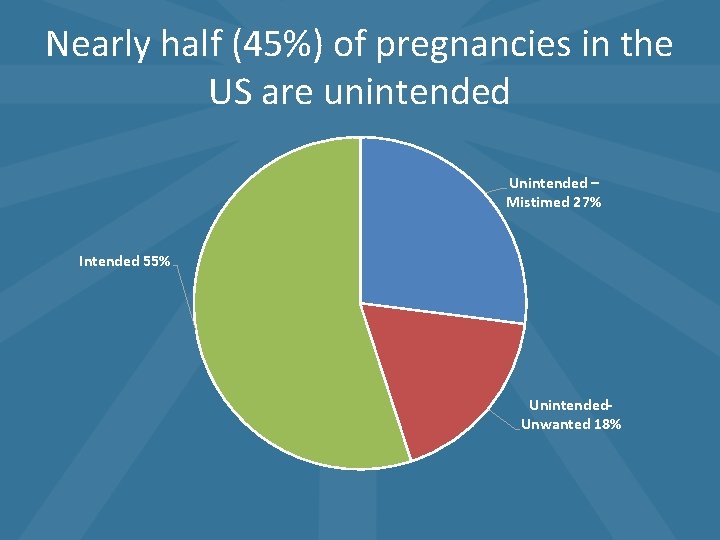
Nearly half (45%) of pregnancies in the US are unintended Unintended – Mistimed 27% Intended 55% Unintended. Unwanted 18%
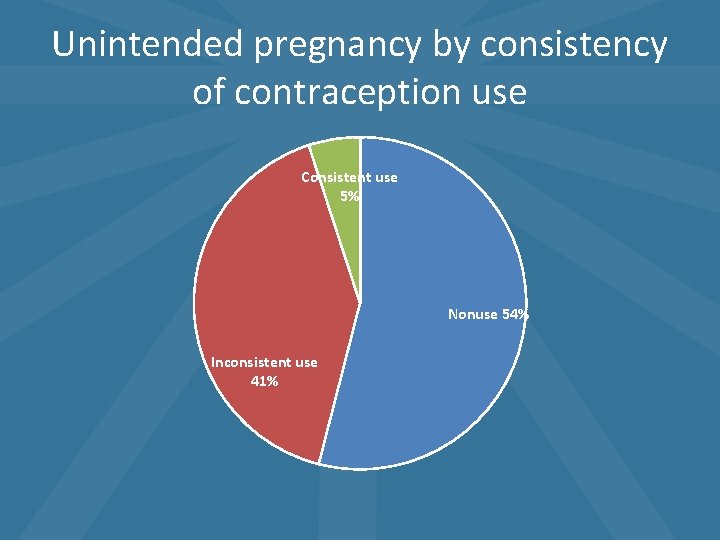
Unintended pregnancy by consistency of contraception use Consistent use 5% Nonuse 54% Inconsistent use 41%
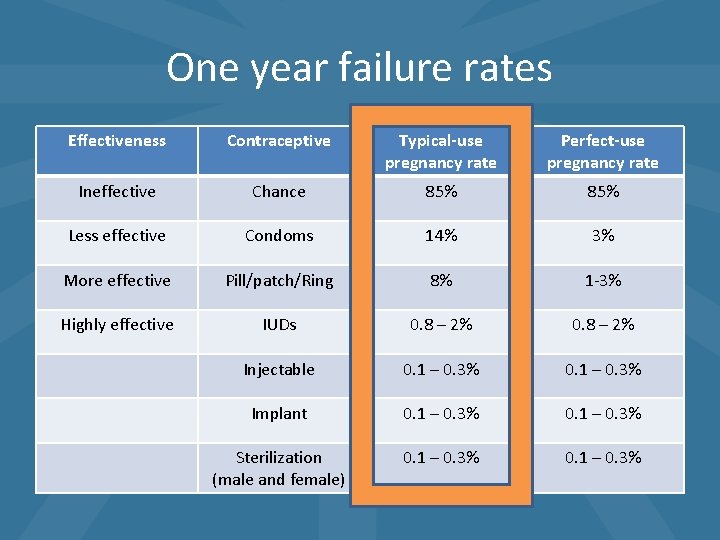
One year failure rates Effectiveness Contraceptive Typical-use pregnancy rate Perfect-use pregnancy rate Ineffective Chance 85% Less effective Condoms 14% 3% More effective Pill/patch/Ring 8% 1 -3% Highly effective IUDs 0. 8 – 2% Injectable 0. 1 – 0. 3% Implant 0. 1 – 0. 3% Sterilization (male and female) 0. 1 – 0. 3%
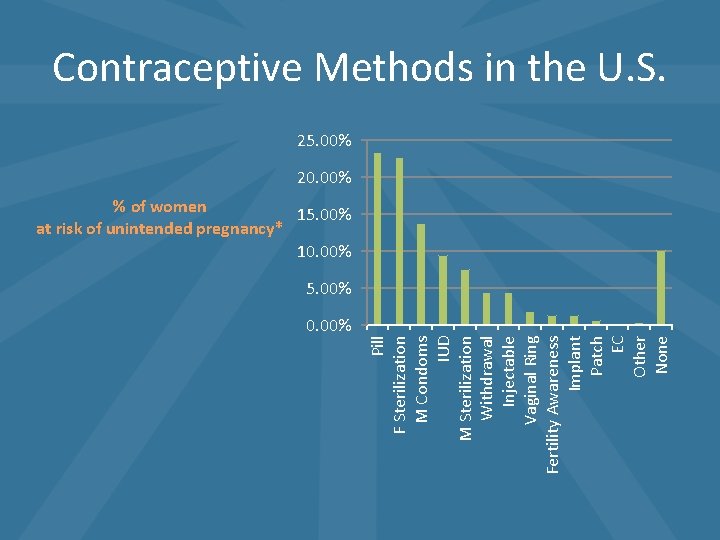
Pill F Sterilization M Condoms IUD M Sterilization Withdrawal Injectable Vaginal Ring Fertility Awareness Implant Patch EC Other None Contraceptive Methods in the U. S. 25. 00% 20. 00% % of women 15. 00% at risk of unintended pregnancy* 10. 00% 5. 00% 0. 00%
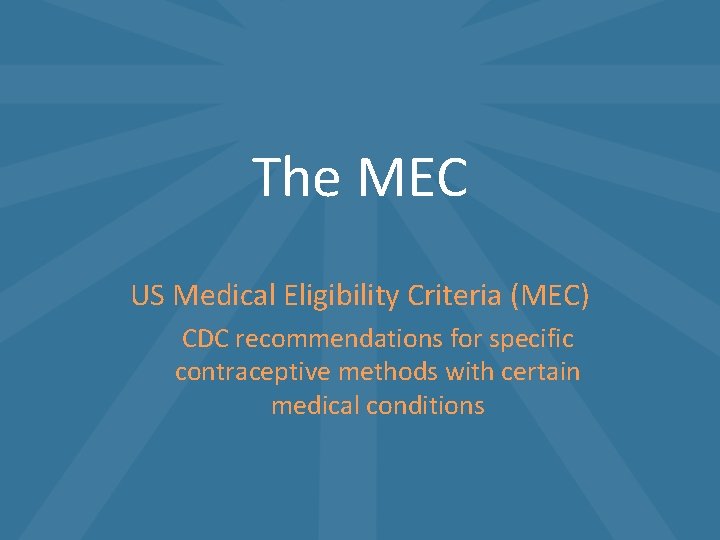
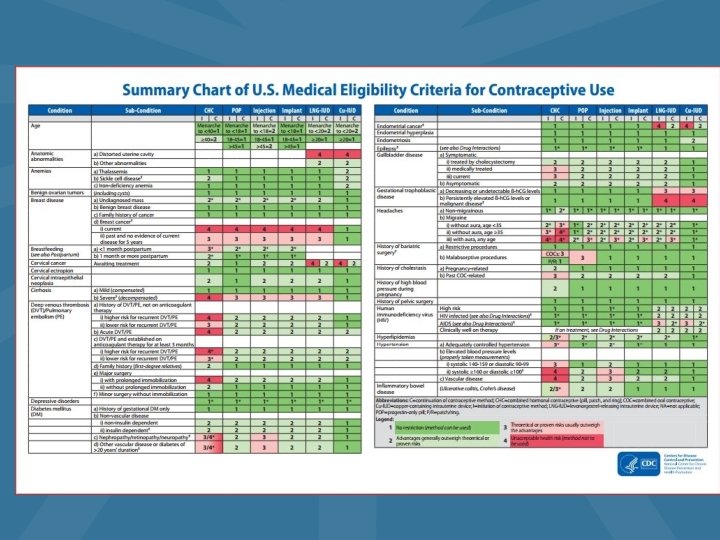
The MEC US Medical Eligibility Criteria (MEC) CDC recommendations for specific contraceptive methods with certain medical conditions
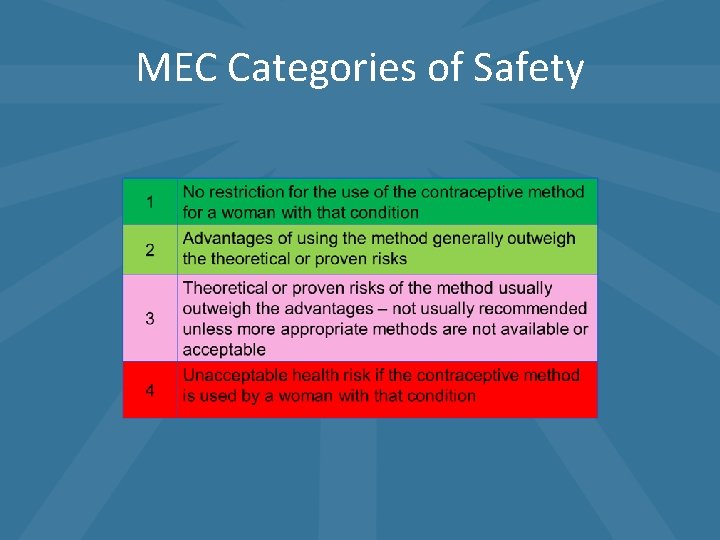
MEC Categories of Safety
There’s an APP for that: - Can be downloaded on i. OS and Android operating systems (https: //www. cdc. gov/mobileapp. html)
Another helpful APP… • Contraceptive Point-of-Care App
Cases In LARC management
Shani • 21 years old • Post-partum 4 weeks • Asking about tubal sterilization because she’s not good with pills
Sterilization by Education • If graduated college, 13% had tubal ligation • If some college, 29% had BTL • If graduated HS, 42% had BTL • If no HS graduation, 55% had BTL
Young women and sterilization • 20% of women selecting sterilization at age 30 years or younger later express regret
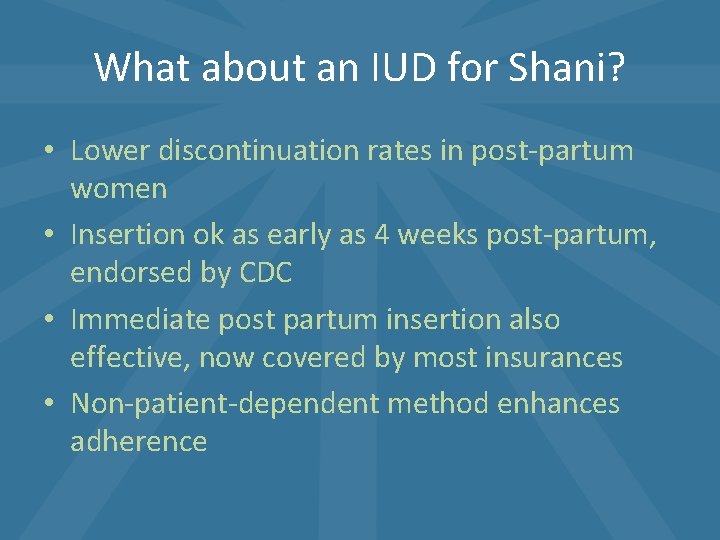
What about an IUD for Shani? • Lower discontinuation rates in post-partum women • Insertion ok as early as 4 weeks post-partum, endorsed by CDC • Immediate post partum insertion also effective, now covered by most insurances • Non-patient-dependent method enhances adherence
Ultimate goal: Patient-Centered • If, after all the information, she still wants sterilization, we need to honor her decision making
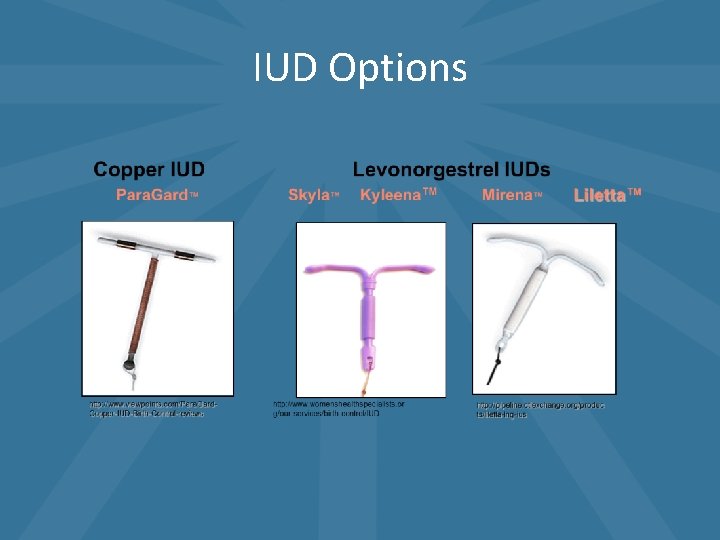
IUD Options
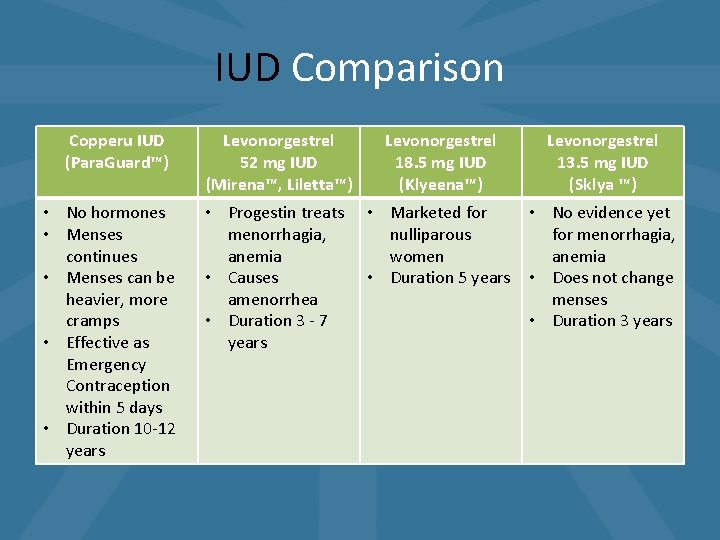
IUD Comparison Copperu IUD (Para. Guard™) • No hormones • Menses continues • Menses can be heavier, more cramps • Effective as Emergency Contraception within 5 days • Duration 10 -12 years Levonorgestrel 52 mg IUD (Mirena™, Liletta™) Levonorgestrel 18. 5 mg IUD (Klyeena™) Levonorgestrel 13. 5 mg IUD (Sklya ™) • Progestin treats menorrhagia, anemia • Causes amenorrhea • Duration 3 - 7 years • Marketed for nulliparous women • Duration 5 years • No evidence yet for menorrhagia, anemia • Does not change menses • Duration 3 years
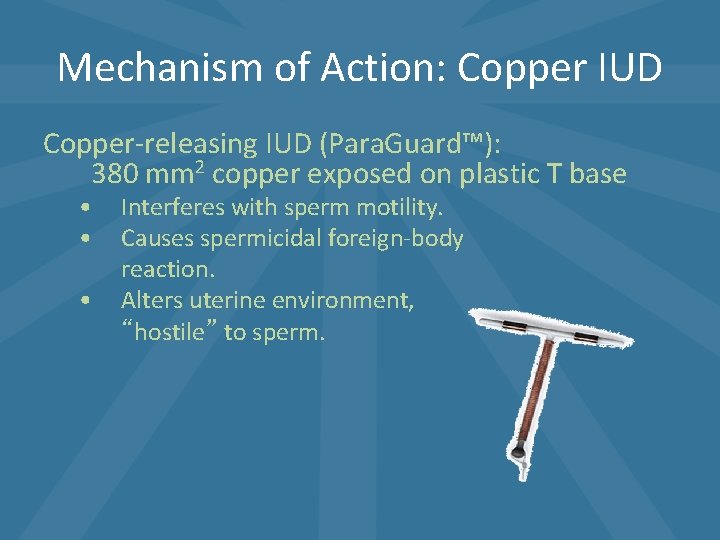
Mechanism of Action: Copper IUD Copper-releasing IUD (Para. Guard™): 380 mm 2 copper exposed on plastic T base • • • Interferes with sperm motility. Causes spermicidal foreign-body reaction. Alters uterine environment, “hostile” to sperm.
Mechanism of Action: Hormonal IUDs • Hormone-releasing IUD levonorgestrel on its arms and stem released at decreasing rate with time • Thickens cervical mucus (acting as a sperm barrier) • Thins uterine lining. • Partial inhibition of ovulation. • Presence of plastic alone may have some efficacy
Maggie • 35 years old • Heavy smoker
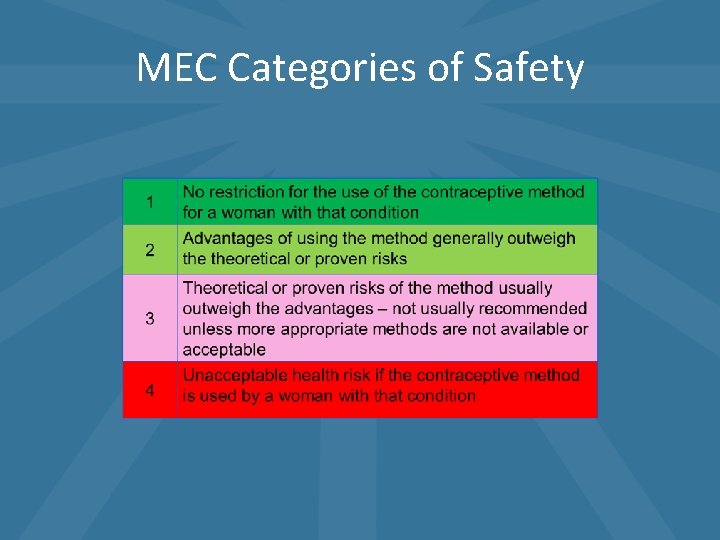
MEC Categories of Safety
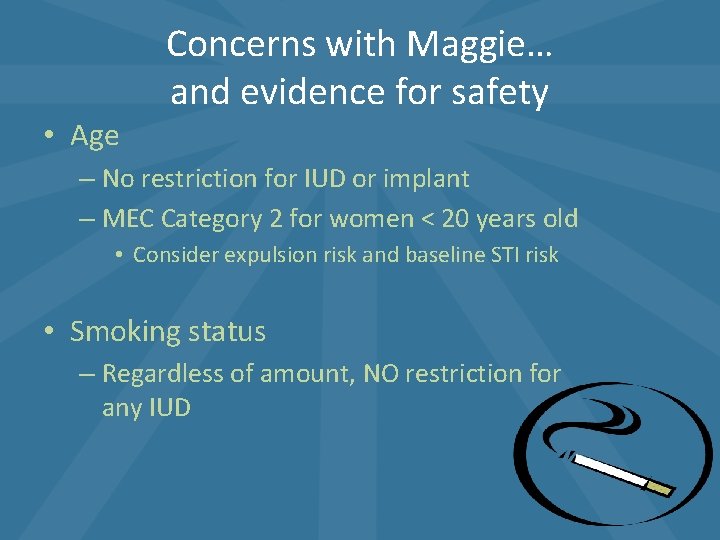
• Age Concerns with Maggie… and evidence for safety – No restriction for IUD or implant – MEC Category 2 for women < 20 years old • Consider expulsion risk and baseline STI risk • Smoking status – Regardless of amount, NO restriction for any IUD
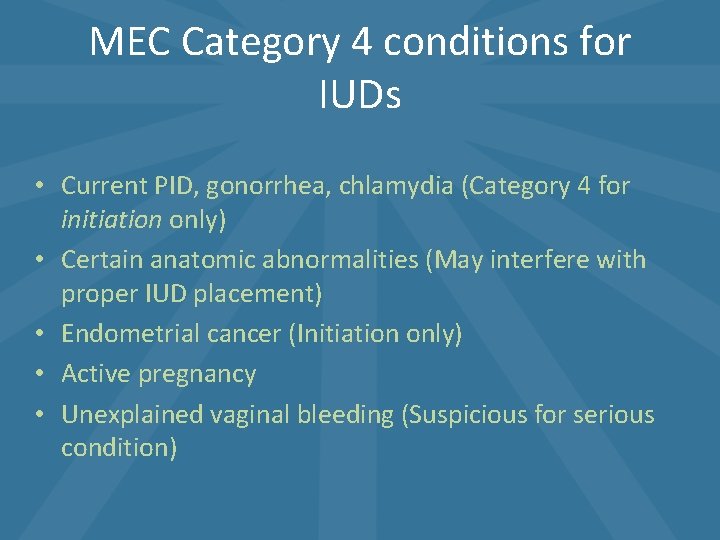
MEC Category 4 conditions for IUDs • Current PID, gonorrhea, chlamydia (Category 4 for initiation only) • Certain anatomic abnormalities (May interfere with proper IUD placement) • Endometrial cancer (Initiation only) • Active pregnancy • Unexplained vaginal bleeding (Suspicious for serious condition)

Krystal • 24 year old • G 2 P 1 • History of chlamydia as a teen
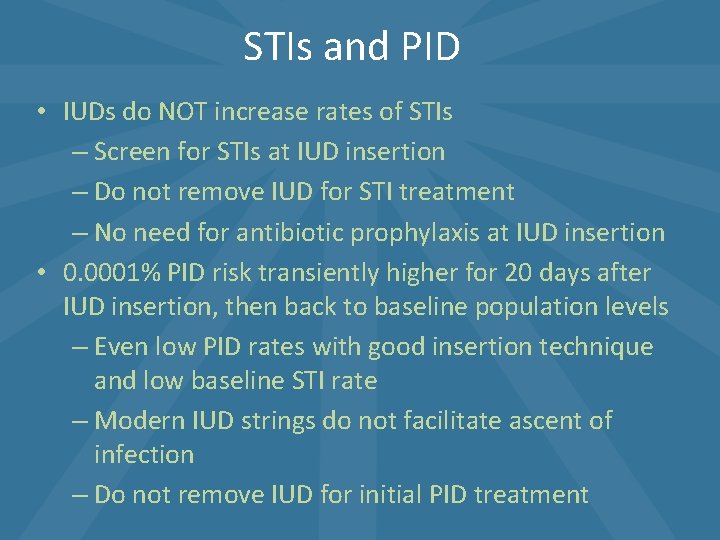
STIs and PID • IUDs do NOT increase rates of STIs – Screen for STIs at IUD insertion – Do not remove IUD for STI treatment – No need for antibiotic prophylaxis at IUD insertion • 0. 0001% PID risk transiently higher for 20 days after IUD insertion, then back to baseline population levels – Even low PID rates with good insertion technique and low baseline STI rate – Modern IUD strings do not facilitate ascent of infection – Do not remove IUD for initial PID treatment
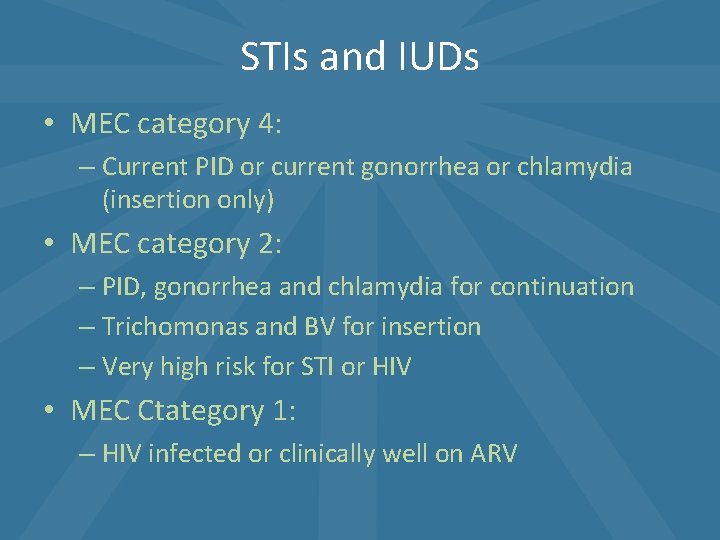
STIs and IUDs • MEC category 4: – Current PID or current gonorrhea or chlamydia (insertion only) • MEC category 2: – PID, gonorrhea and chlamydia for continuation – Trichomonas and BV for insertion – Very high risk for STI or HIV • MEC Ctategory 1: – HIV infected or clinically well on ARV
Kerry • • 18 year old G 1 P 0 DM Type 1 Borderline HTN
Medical Eligibility • Progestin IUD or Implant does not alter glycemic control in patients with DM 1, does not affect blood pressure • Copper IUD is approved for almost all medical conditions: – Cardiovascular disease – Hypertension – Migraines – Smoking – Lipid disorders – Diabetes
Tammy • 35 year old • Heavy periods with anemia
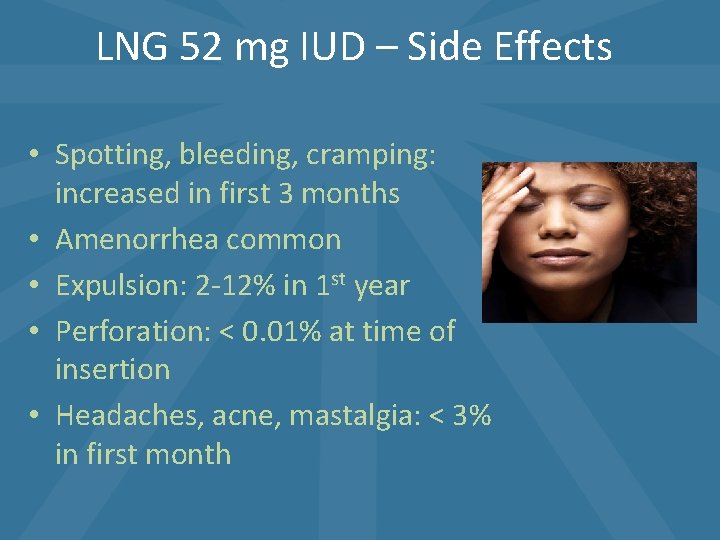
LNG 52 mg IUD – Side Effects • Spotting, bleeding, cramping: increased in first 3 months • Amenorrhea common • Expulsion: 2 -12% in 1 st year • Perforation: < 0. 01% at time of insertion • Headaches, acne, mastalgia: < 3% in first month
LNG 52 mg IUD- Medical Advantages • Cramps and menorrhagia improve • 90% decrease in overall blood loss • Decreases number of invasive treatments for DUB, fibroids • Decreases risk of ectopic pregnancy • May protect against endometrial cancer • Decreases peri-menopausal symptoms
LNG 13. 5 mg • Only 6% have amenorrhea after one year • No evidence that lower dose means less progestin side effects • 50% of failures were ectopic pregnancies
Non-contraceptive benefits of LNG 52 mg IUD • Treatment of menorrhagia – Including in women with uterine fibroids and adenomyosis • Treatment of pain in women with endometriosis • Prevention of endometrial hyperplasia in perimenopausal women using estrogen therapy • Prevention of endometrial proliferation and polyps in breast cancer survivors taking tamoxifen
Myths about IUDs • Must IUDs be inserted during menses? • Can the IUD be used as emergency contraception?
Pamela • Has had an IUD for two years • Positive pregnancy test • You can feel the strings
IUD and Ectopic Risk • Ectopic pregnancy rate is the same in IUD users as in the general population, not higher • Pregnancy rate in IUD users is very low • However, if pregnant with IUD in place, one out of 2 -3 pregnancies in IUD users will be ectopic. URGENT NEED FOR ULTRASOUND TO LOCATE THE PREGNANCY.
Jennifer • 18 years old • Her mother was just diagnosed with a Pulmonary Embolism, she wants something other than pills • Not ok with having a pelvic exam.
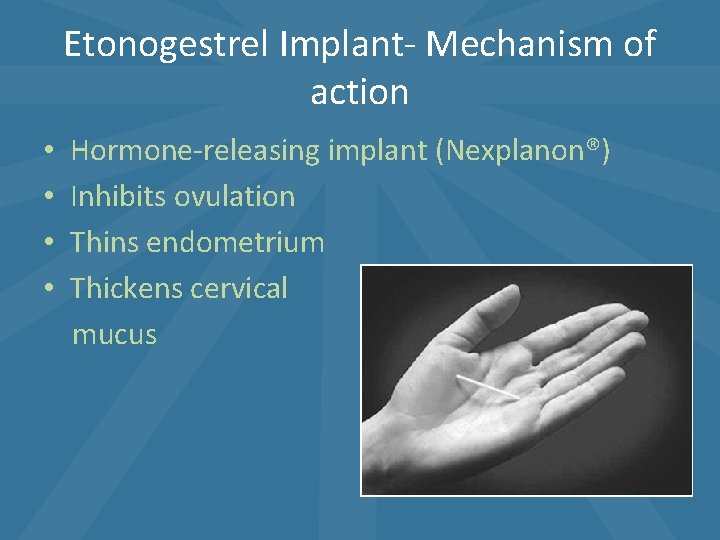
Etonogestrel Implant- Mechanism of action • • Hormone-releasing implant (Nexplanon®) Inhibits ovulation Thins endometrium Thickens cervical mucus
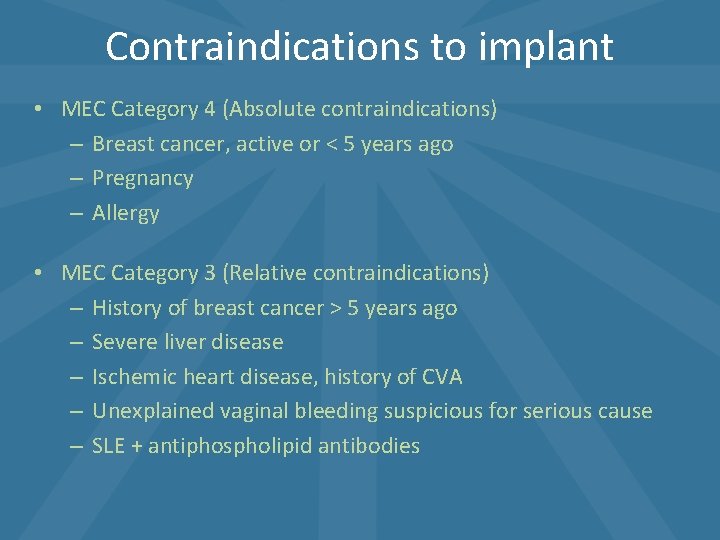
Contraindications to implant • MEC Category 4 (Absolute contraindications) – Breast cancer, active or < 5 years ago – Pregnancy – Allergy • MEC Category 3 (Relative contraindications) – History of breast cancer > 5 years ago – Severe liver disease – Ischemic heart disease, history of CVA – Unexplained vaginal bleeding suspicious for serious cause – SLE + antiphospholipid antibodies
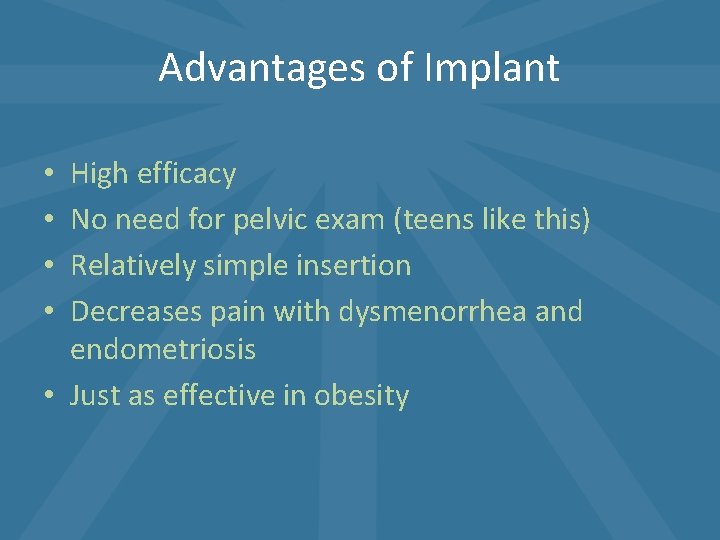
Advantages of Implant High efficacy No need for pelvic exam (teens like this) Relatively simple insertion Decreases pain with dysmenorrhea and endometriosis • Just as effective in obesity • •
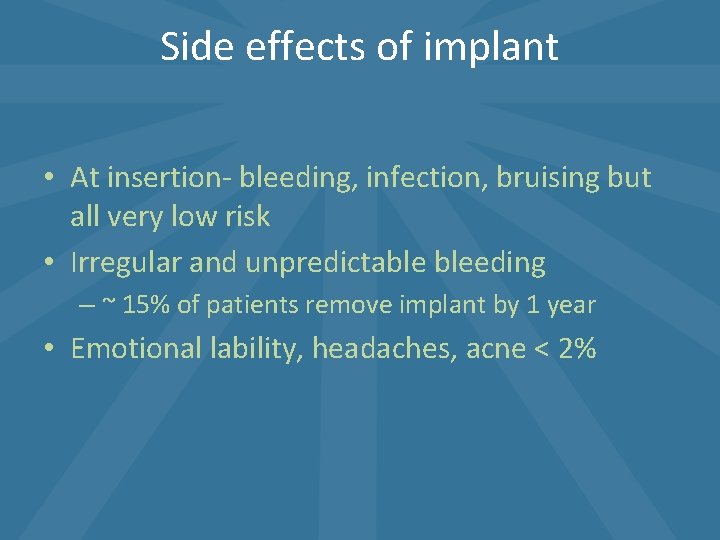
Side effects of implant • At insertion- bleeding, infection, bruising but all very low risk • Irregular and unpredictable bleeding – ~ 15% of patients remove implant by 1 year • Emotional lability, headaches, acne < 2%
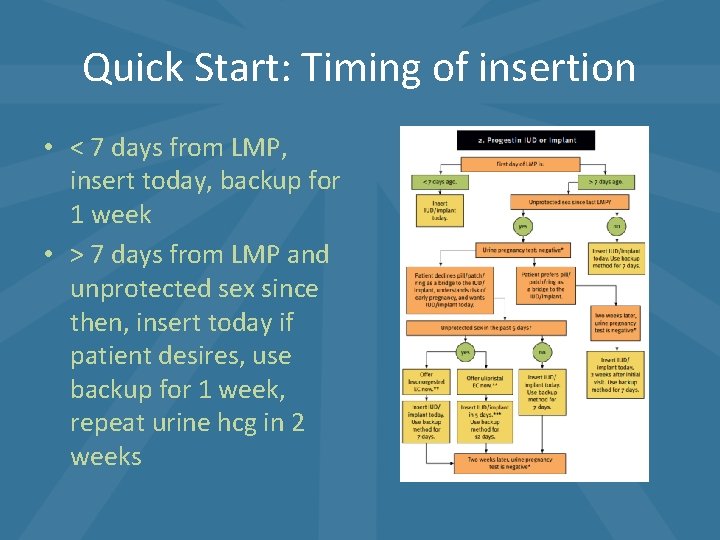
Quick Start: Timing of insertion • < 7 days from LMP, insert today, backup for 1 week • > 7 days from LMP and unprotected sex since then, insert today if patient desires, use backup for 1 week, repeat urine hcg in 2 weeks
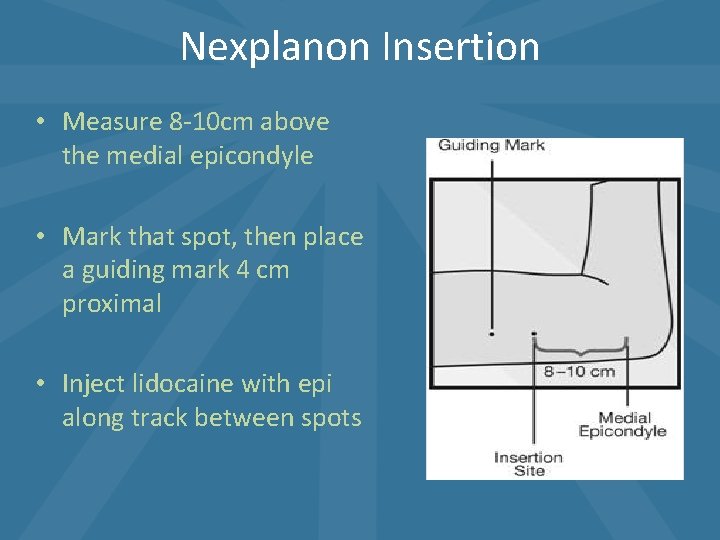
Nexplanon Insertion • Measure 8 -10 cm above the medial epicondyle • Mark that spot, then place a guiding mark 4 cm proximal • Inject lidocaine with epi along track between spots
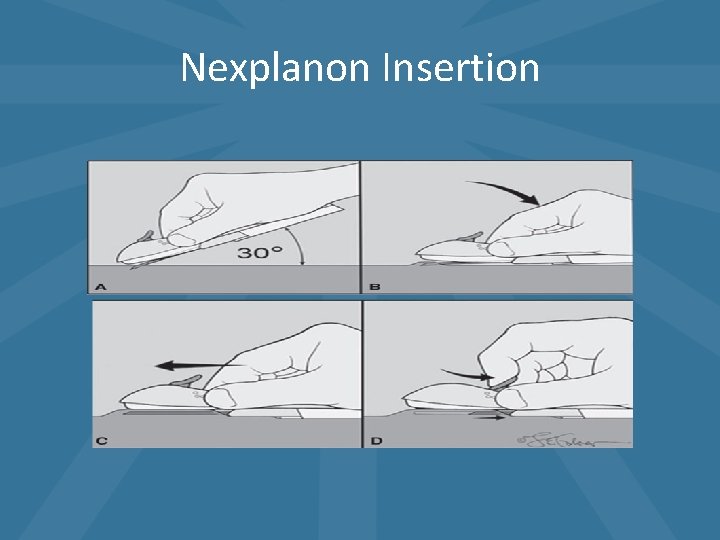
Nexplanon Insertion
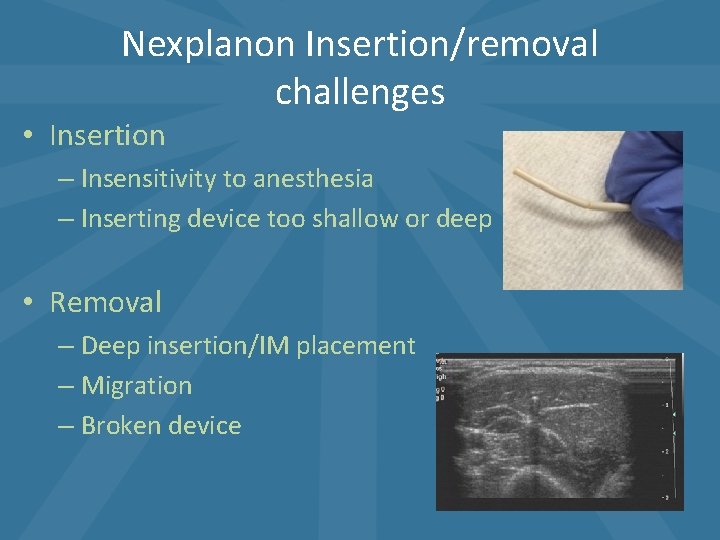
Nexplanon Insertion/removal challenges • Insertion – Insensitivity to anesthesia – Inserting device too shallow or deep • Removal – Deep insertion/IM placement – Migration – Broken device
Troubleshooting IUD issues • Bleeding pattern problems – Short term NSAIDs or OCPs plus time • Pain problems – NSAIDs plus time (check placement, pelvic exam and/or US) • String issues – Leave long (3 -4 cm, can always shorten), cut at right angle, tuck behind cervix.
Challenges with IUD insertion • Discomfort/difficulty with speculum placement • Visualizing the cervix • Extreme uterine position/uterine distortion • Prior c-sections • Tight cervical os • Vasovagal reactions • Perforation
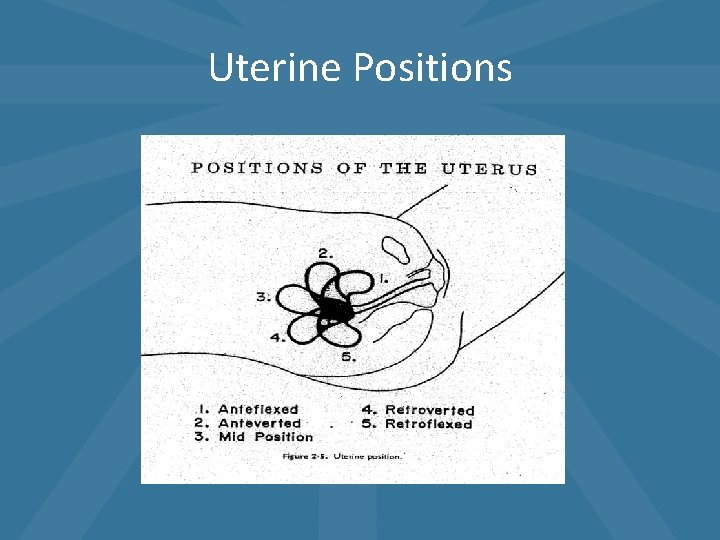
Uterine Positions
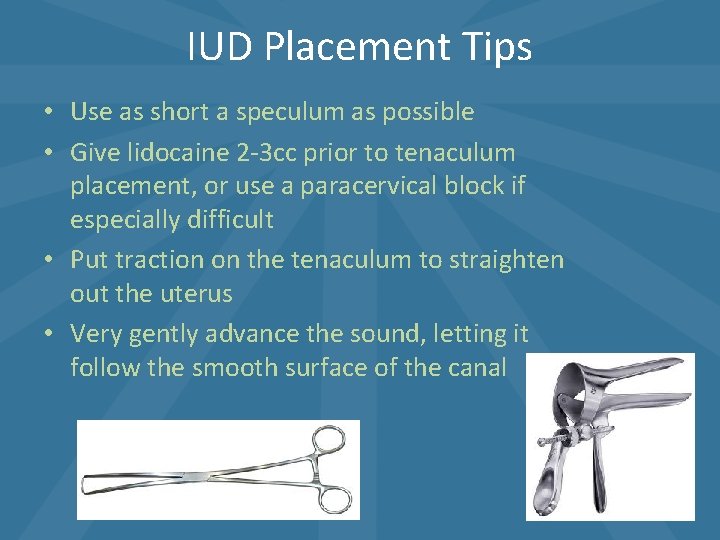
IUD Placement Tips • Use as short a speculum as possible • Give lidocaine 2 -3 cc prior to tenaculum placement, or use a paracervical block if especially difficult • Put traction on the tenaculum to straighten out the uterus • Very gently advance the sound, letting it follow the smooth surface of the canal
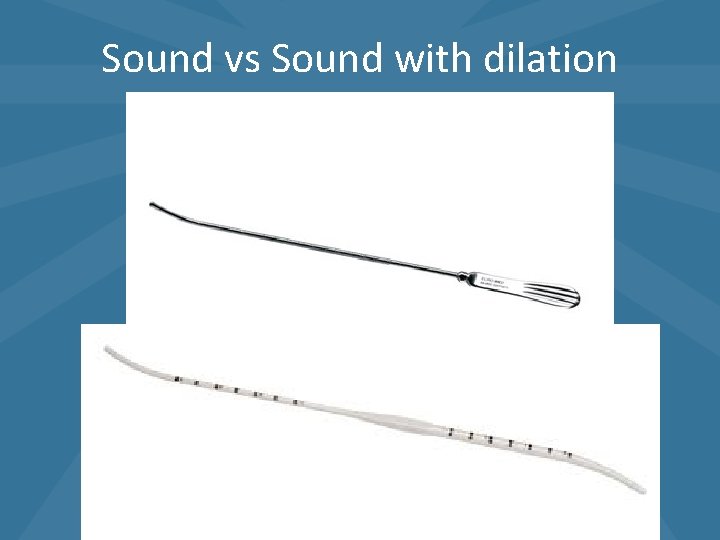
Sound vs Sound with dilation

Os finders
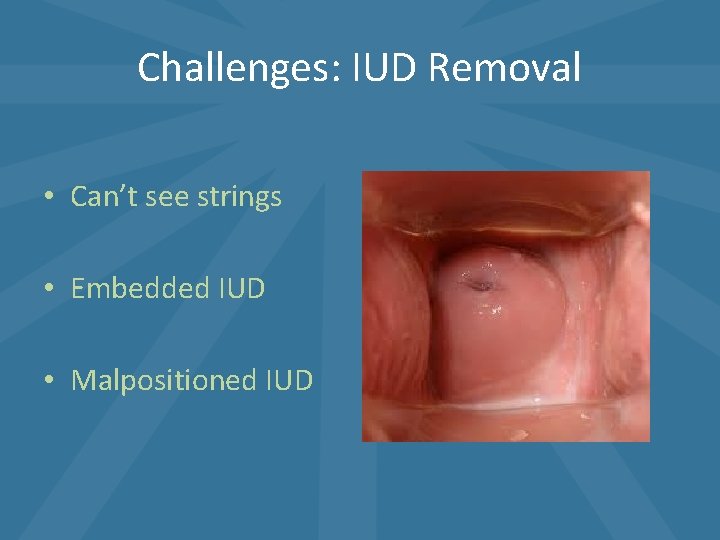
Challenges: IUD Removal • Can’t see strings • Embedded IUD • Malpositioned IUD
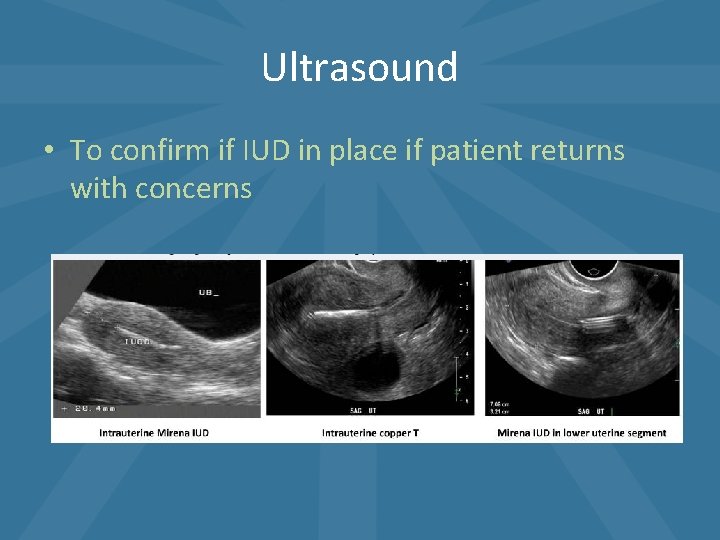
Ultrasound • To confirm if IUD in place if patient returns with concerns
Take Home Messages • You can do this! • LARC is a good option for patients • The risks are minimal • The benefits are enormous

- Slides: 58