Living Breathing and Teaching the Core Values of
Living, Breathing and Teaching the Core Values of Family Medicine Raj Woolever, MD, FAAFP, Program Director Bethany Picker, MD, Medical Director STFM/AAFP Conference on Practice Improvement December 3, 2011

What are the “Core Values” ? ?

What are the “Core Values” ? � Continuous healing relationships � Whole-person orientation � Comprehensive care � Care delivered in the context of family and community

What are the “Core Values” ? � First contact access �A comprehensive approach � Coordination � Personalization of care
What are the “Core Values” ? “Family physicians are committed to fostering health and integrated health care for the whole person by humanizing medicine and providing sciencebased high-quality care. ”
What Do Family Physicians Value? � � Committed to continuing, comprehensive, compassionate and personal care Concerned with the care of people of all ages Understand that health and disease involve the mind, body and spirit Appreciate the impact of the context of patients’ lives as members of their family and community Martin JC, Avant RF, Bowman MA, et al. The Future of Family Medicine: A collaborative project of the family medicine community. Ann Fam Med. 2004 Mar-April; 2 Suppl 1: S 3 -S 32

What are patients looking for in a provider ? § § § In their insurance plan Convenient location Ability to schedule appointments within a reasonable period of time Good communication skills A reasonable amount of experience in practice Martin JC, Avant RF, Bowman MA, et al. The Future of Family Medicine: A collaborative project of the family medicine community. Ann Fam Med. 2004 Mar-April; 2 Suppl 1: S 3 -S 32
What are patients looking for in a provider ? § In their insurance plan Convenient location Ability to schedule appointments within a reasonable period of time Good communication skills A reasonable amount of experience in practice § A comfortable relationship, above all else § § Martin JC, Avant RF, Bowman MA, et al. The Future of Family Medicine: A collaborative project of the family medicine community. Ann Fam Med. 2004 Mar-April; 2 Suppl 1: S 3 -S 32
What Do Patients Value? � � A deep understanding of the dynamics of the whole person A generative impact on patients’ lives A talent for humanizing the health care experience A natural command of complexity Martin JC, Avant RF, Bowman MA, et al. The Future of Family Medicine: A collaborative project of the family medicine community. Ann Fam Med. 2004 Mar-April; 2 Suppl 1: S 3 -S 32

What are the “Core Values” ? �Safe �Effective �Patient-centered �Timely �Efficient �Equitable
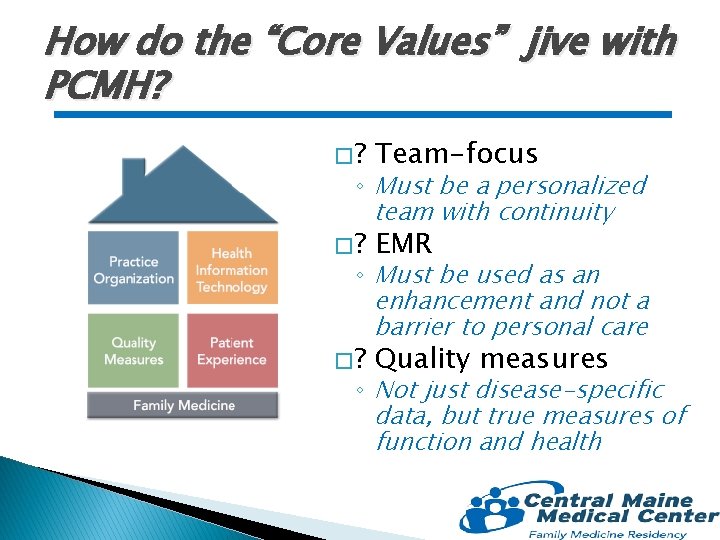
How do the “Core Values” jive with PCMH? �? Team-focus �? EMR �? Quality measures ◦ Must be a personalized team with continuity ◦ Must be used as an enhancement and not a barrier to personal care ◦ Not just disease-specific data, but true measures of function and health

The Power of Connection § § Stange, K; A Science of Connectedness; Ann Fam Med 2009; 7: 387 -395. Fundamental health care § Acute, chronic, proactive Integrated care § Mgmt of multimorbidity Prioritized care § Balancing individual, family, community, system § Iterating btwn biotechnical and biographical Healing & transcendence § Fostering healing § Abiding even when healing cannot be fostered
A Generalist Approach � Ways of being ◦ Readiness for the generalist way � Ways of knowing ◦ Training for the generalist way � Ways of perceiving ◦ Seeing the world in ways that foster integration � Ways of thinking and doing ◦ Prioritized, joined-up action Stange, K; The Generalist Approach; Ann Fam Med 2009; 7: 198 -203.
A Generalist Approach � Not defined by content or specific list of services and procedures
A Generalist Approach � Not defined by content � Not defined by age
A Generalist Approach � Not defined by content � Not defined by age � Not defined by gender
A Generalist Approach � Not defined by content � Not defined by age � Not defined by gender � Not defined by setting in which care is given
It’s all about the process… � We are defined by the process in which we see patients ◦ Patient-physician relationship ◦ Problem definition and prioritization
It’s all about the process… � We are defined by the process in which we see patients ◦ Patient-physician relationship ◦ Problem definition and prioritization � Family physicians use the same process in their approach to all patients
It’s all about the process… � We are the expert in this processoriented discipline ◦ Continuity ◦ Comprehensiveness
It’s all about the process… � We are the expert in this processoriented discipline ◦ Continuity ◦ Comprehensiveness � “Need to find better and more efficient ways of providing personalized care for patients”
It’s all about the process… � We are the expert in this processoriented discipline ◦ Continuity ◦ Comprehensiveness � “Need to find better and more efficient ways of providing personalized care for patients” -1964
Training Residents: the tyranny of the “block schedule” � Schedule dominated by discrete rotations: ◦ Inpatient: � Adult medicine � Pediatrics � Maternity Care � Surgery ◦ Outpatient � Pediatrics � Orthopedics/Sports Medicine � Other “partialist” experiences � “Clinic” schedules often worked around other rotations
The Tyranny of the “Block Schedule” � The timing of experiences drives knowledge and comfort ◦ Predominance of inpatient experiences in the intern year ◦ Relatively little Family Medicine Center experience in the intern year � What does this say about the priorities of training?
Divorce from Reality � Practice patterns of family physicians: ◦ >90% provide outpatient primary care ◦ ~60% provide some inpatient care ◦ ~50% provide some care in the ER ◦ <20% provide obstetrical care
Comfort in Clinic � What makes the clinic experience uncomfortable for many residents?
Comfort in Clinic � What makes the clinic experience uncomfortable for many residents? ◦ ◦ ◦ ◦ Feels more alone Less team work More uncertainty More time pressure “Challenging” patients More difficult to see “results” Takes time to reap rewards
Clinic as the Driver � Improve comfort by making the clinic experience the priority and “driver” � Ensure high quality teaching in the clinic setting � Develop and nurture clinical teams � Improve communication and support � Clarify the evaluation process

Clinic as the Driver � Clinic as priority and driver ◦ Set half day in clinic �Remains constant thru all 3 years of training ◦ With very few exceptions, other rotational experiences must bend around this ◦ Improves ability to plan and prepare ◦ Improves continuity �Improved patient satisfaction �Improved provider satisfaction
Clinic as the Driver � High quality outpatient teaching ◦ Preceptor development to improve teaching skills ◦ Emphasize perspective brought by community preceptors ◦ Implement end-of-day outpatient “rounds” ◦ Addition of the “roamer” �Informal precepting �“Curbside” �How to handle uncertainty
Clinic as the Driver � Invest in clinical teams ◦ Dedicated team meeting times ◦ Team practice improvement projects ◦ Team approach to patient care � Improve communication and support ◦ Huddle ◦ The “roamer”
Clinic as the Driver � Improve the evaluation process ◦ “Daily” eval ◦ Outpatient mentor ◦ Include quality measures: �Monthly dashboard: �Patient satisfaction �Visit numbers �Time to 3 rd next available appointment �Bi-directional continuity
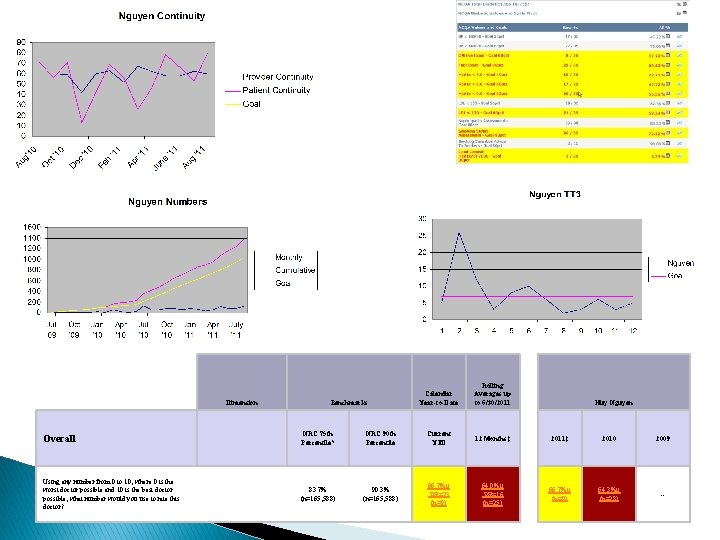
Dimension Benchmarks Calendar Year-to-Date Rolling Averages up to 6/30/2011 Huy Nguyen Overall NRC 75 th Percentile* NRC 90 th Percentile Current YTD 12 Months‡ 2011‡ 2010 2009 Using any number from 0 to 10, where 0 is the worst doctor possible and 10 is the best doctor possible, what number would you use to rate this doctor? 83. 7% (n=165, 588) 90. 3% (n=165, 588) 66. 7%µ PR=23 (n=9) 64. 0%µ PR=16 (n=25) 66. 7%µ (n=9) 64. 3%µ (n=28) --
Finding the Joy � Not just competence, but passion and pleasure � Encourage a fluid inpatient/outpatient experience � Embrace innovation – new approaches keep it fresh

Finding the Joy Not just competence, but passion and pleasure � Encourage a fluid inpatient/outpatient experience � Embrace innovation – new approaches keeps it fresh � � It needs to be learned and experienced to be incorporated in the future
Beware the “Hidden Curriculum” Chuang, A, Nuthalapaty, F, Casey, P; To the point: reviews in medical education-taking control of the hidden curriculum; Am J of Ob. Gyn 2010; Oct: 316. e 1 -316. e 6. “… medical training is also a process of moral enculturation, and that in transmitting normative rules regarding behaviors and emotions to its trainees, the medical learning environment functions as a moral community…”
Beware the “Hidden Curriculum” 3 common medical student criticisms of physicians: § § § Chuang, A, Nuthalapaty, F, Casey, P; To the point: reviews in medical education-taking control of the hidden curriculum; Am J of Ob. Gyn 2010; Oct: 316. e 1 -316. e 6. do not care enough about their patients do not know enough to practice the best medicine do not do enough to maintain the public’s trust
Beware the “Hidden Curriculum” � Establish Chuang, A, Nuthalapaty, F, Casey, P; To the point: reviews in medical education-taking control of the hidden curriculum; Am J of Ob. Gyn 2010; Oct: 316. e 1 -316. e 6. a climate of humanism � Recognize and use seminal events � Role model � Actively engage the learner � Be practical and relevant
Teaching the “Core Values” § § Be a mentor – make sure you are living the core values Provide a clinic environment that supports the core values Enlist patients as part of the teaching team Re-discover and transmit the joy

The “Core Values” of Family Medicine � Questions/Comments
“the Central Maine way…” � Set ◦ ◦ of tools and commitments: Function as part of a team Be engaged and involved Innovate Serve the underserved, especially the rural underserved
- Slides: 41