Liver pathology CIRRHOSIS Ivana Mari Mentor A mega



- Slides: 18
Liver pathology: CIRRHOSIS Ivana Marić Mentor: A. Žmegač Horvat
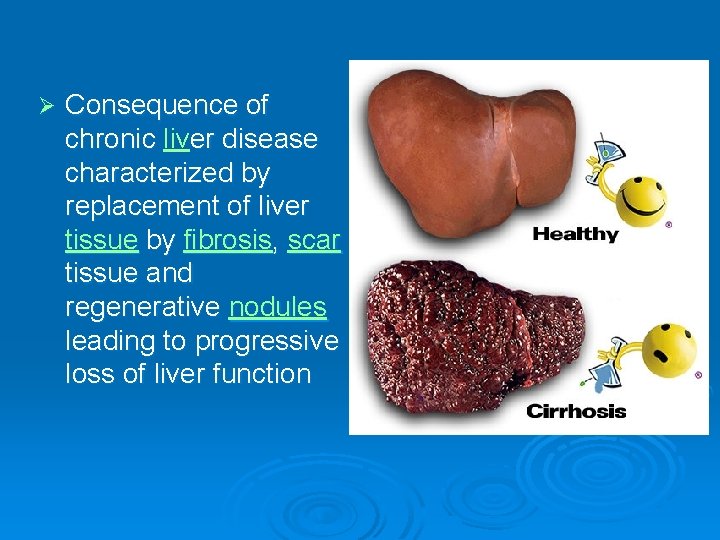
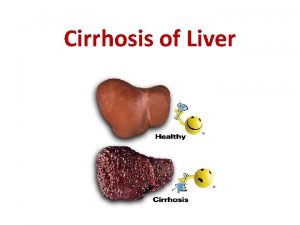
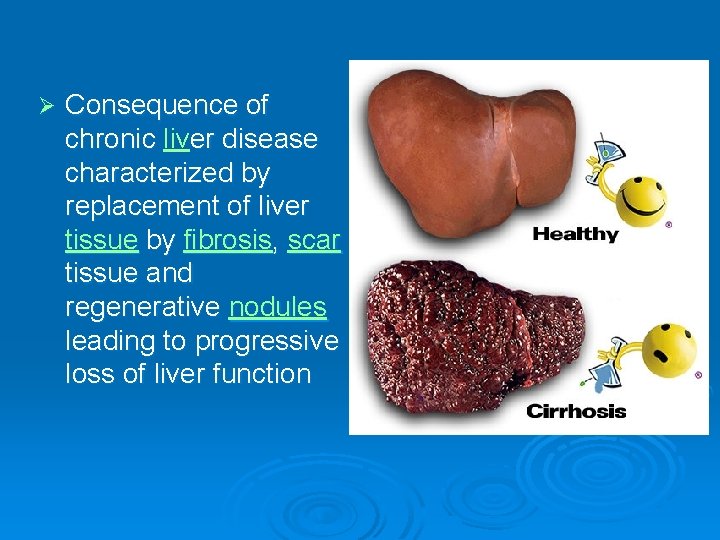
Ø Consequence of chronic liver disease characterized by replacement of liver tissue by fibrosis, scar tissue and regenerative nodules leading to progressive loss of liver function
Aetiology Ø Ø Alcohol Chronic hepatitis B Chronic hepatitis C Other: Haemochromatosis Non-alcoholic fatty liver disease Primary biliary cirrhosis Sclerosing cholangitis Autoimmune hepatitis Cystic fibrosis. . .
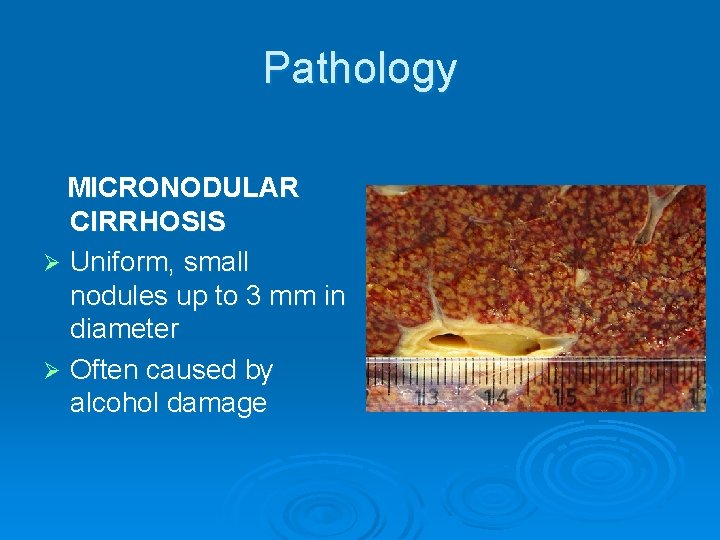
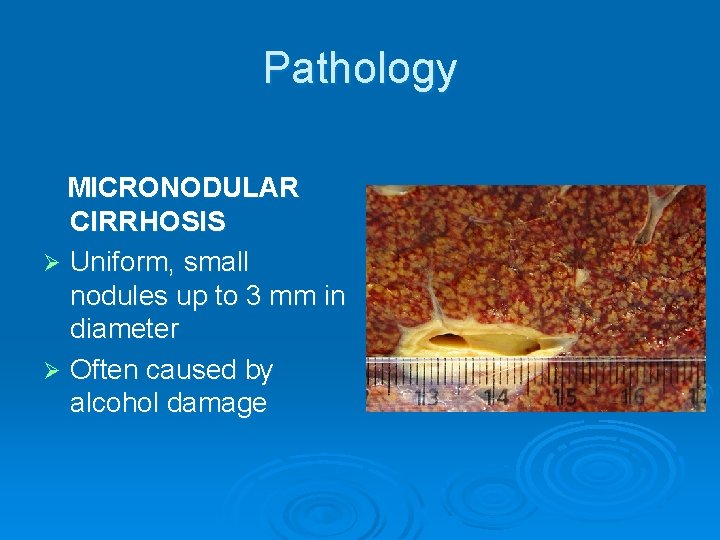
Pathology MICRONODULAR CIRRHOSIS Ø Uniform, small nodules up to 3 mm in diameter Ø Often caused by alcohol damage
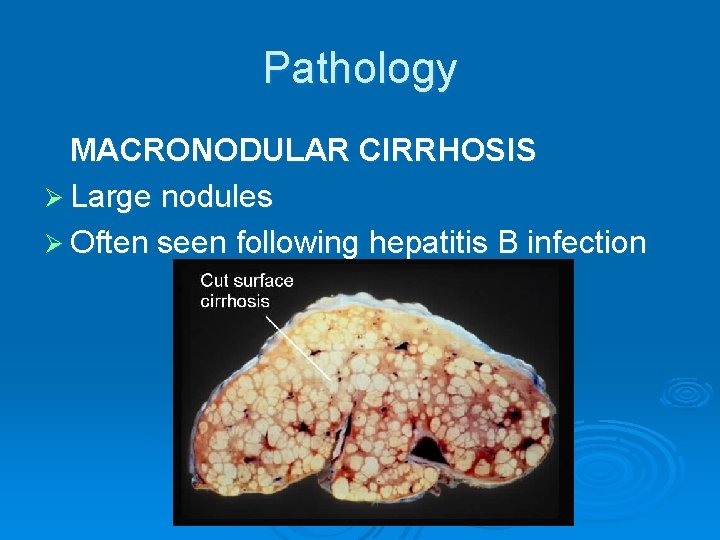
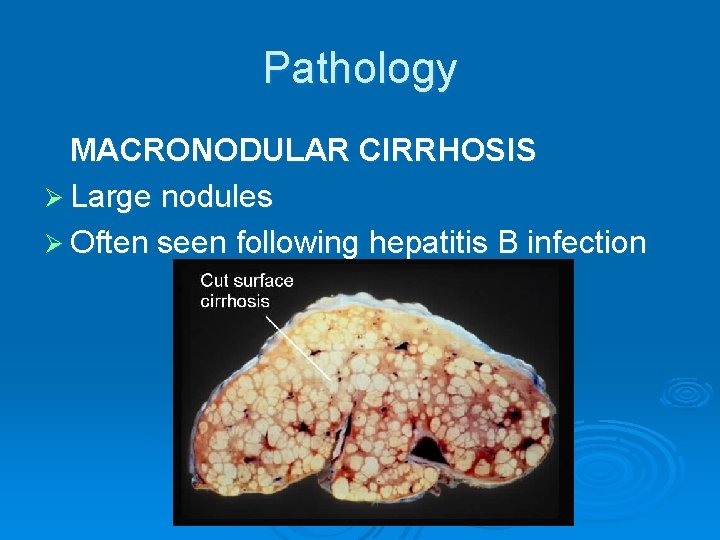
Pathology MACRONODULAR CIRRHOSIS Ø Large nodules Ø Often seen following hepatitis B infection
Ø Cirrhosis with complicatons of encephalopathy, ascites or variceal haemorrhage – DECOMPENSATED CIRRHOSIS Ø Cirrhosis without any of these complications – COMPENSATED CIRRHOSIS
Signs and symptoms Ø Jaundice Ø Fatigue Ø Weakness Ø Loss of appetite Ø Itching Ø Easy bruising
Investigations Ø Liver biochemistry (usually slight elevation of serum alkaline phosphatase and aminotransferase) Ø Liver function - serum albumin and prothrombin Ø Serum electrolytes Ø Serum alpha-fetoprotein Ø Endoscopy

Investigations Ø Ultrasound Ø CT
Management Ø Irreversible disease, frequently progresses Ø Correcting the underlying cause (abstinence from alcohol) Ø Screening for hepatocellular carcinoma Ø Liver transplantation Ø 5 -year survival rate approximately 50%
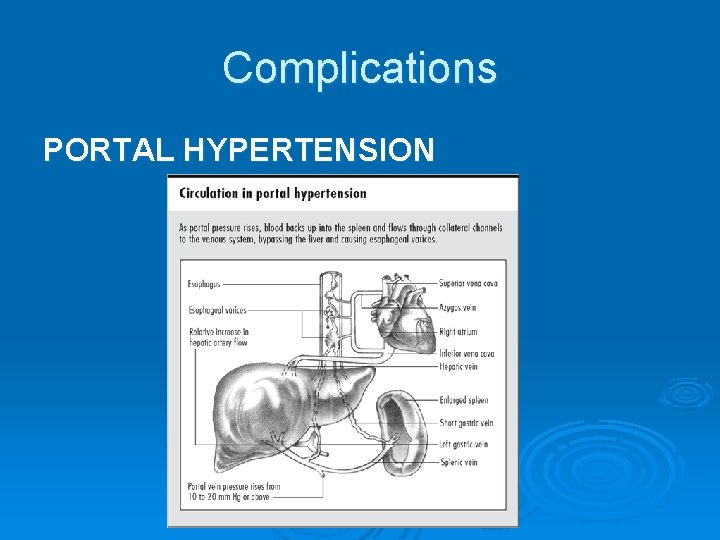
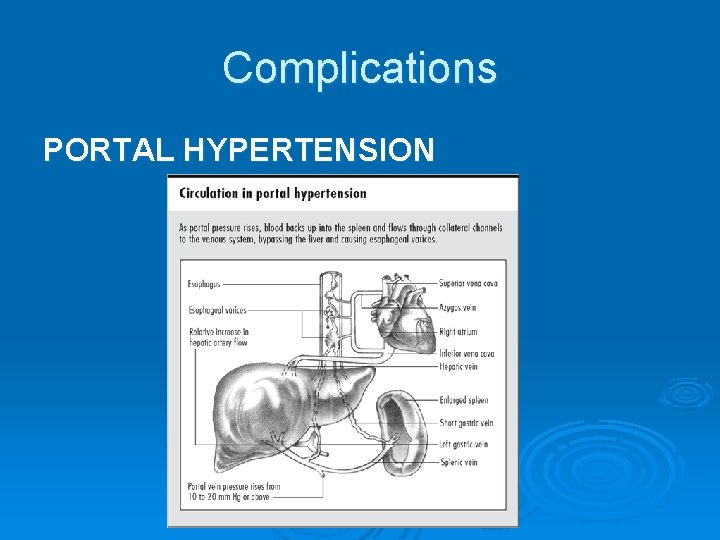
Complications PORTAL HYPERTENSION
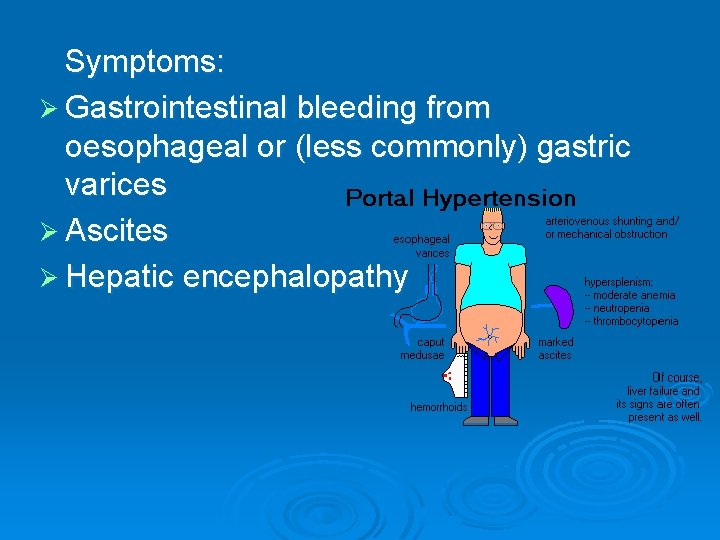
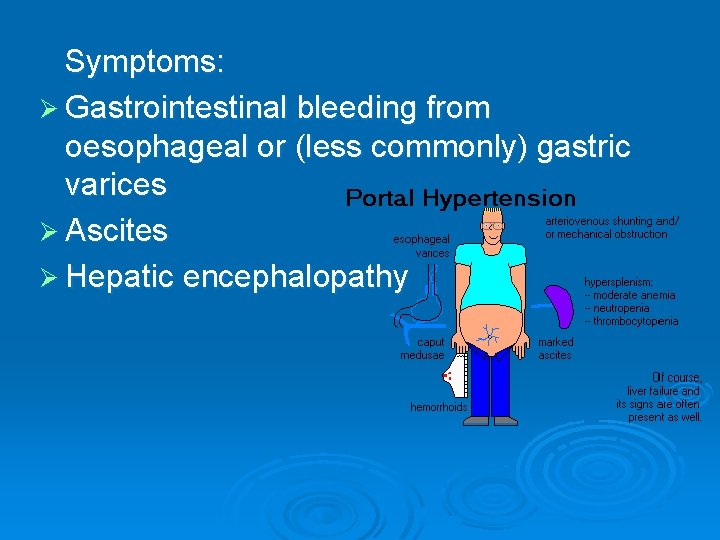
Symptoms: Ø Gastrointestinal bleeding from oesophageal or (less commonly) gastric varices Ø Ascites Ø Hepatic encephalopathy
VARICEAL HAEMORRHAGE 30% of patients with varices bleed from them often massive bleeding; 50% mortality Ø Therapy: endoscopic therapy: sclerotherapy variceal band ligation pharmacological treatment balloon tamponade TIPS surgery Ø

ASCITES Presence of fluid in the peritoneal cavity Ø Therapy: diuretics paracentesis Ø
PORTOSYSTEMIC ENCEPHALOPATHY Ø Toxic substances (ammonia) bypass the liver via collaterals and gain access to the brain Ø Symptoms: lethargy mild confusion anorexia reversal of sleep pattern disorientation coma
HEPATORENAL SYNDROME Ø Development of acute renal failure in patients with advanced liver disease Ø Splanchnic vasodilatation - fall in systemic vascular resistance, vasoconstriction of renal circulation, reduced renal perfusion Ø Oliguria, rising serum creatinine, low urine sodium

Ø http: //www. youtube. com/watch? v=pm. BBT 4 ve. CRc
References: Ø www. wikipedia. com Ø Kumar&Clark: Clinical medicine
 Una frase completa
Una frase completa Types of cirrhosis
Types of cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Councilman bodies
Councilman bodies Nursing management of chronic liver disease
Nursing management of chronic liver disease S.terre hepatic
S.terre hepatic Pes statement for cirrhosis
Pes statement for cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Primary biliary cholangitis skin
Primary biliary cholangitis skin Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Why does liver disease cause splenomegaly
Why does liver disease cause splenomegaly Hepatocirrhosis
Hepatocirrhosis Ivana mari
Ivana mari Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Gastrointestinalis
Gastrointestinalis Alcoholic liver disease
Alcoholic liver disease What is cirrhosis
What is cirrhosis Cirrhosis care near woodland
Cirrhosis care near woodland Terlipressin
Terlipressin