Liver diseases Review Outline Hepatology Abnormal LFTs Viral
Liver diseases
Review Outline • • Hepatology – – – – Abnormal LFTs Viral hepatitis (A, B, C) PSC PBC AIH NASH/NAFLD Drugs (Tylenol) Cirrhosis Ascites Metabolic liver diseases (A 1 AT, HH, Wilsons) Gilbert’s Disease Liver masses Pregnancy Pancreatiobiliary – – Pancreatitis – acute and chronic Pancreatitis complications Pancreatic cancer Billiary disease
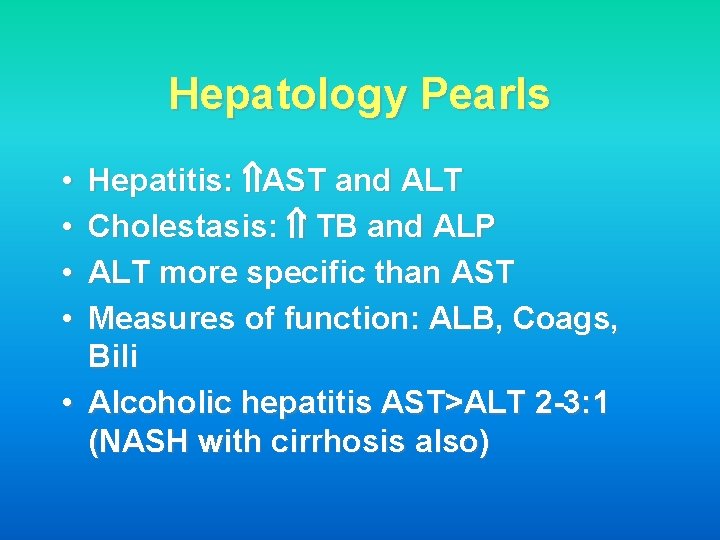
Hepatology Pearls Hepatitis: AST and ALT Cholestasis: TB and ALP ALT more specific than AST Measures of function: ALB, Coags, Bili • Alcoholic hepatitis AST>ALT 2 -3: 1 (NASH with cirrhosis also) • •
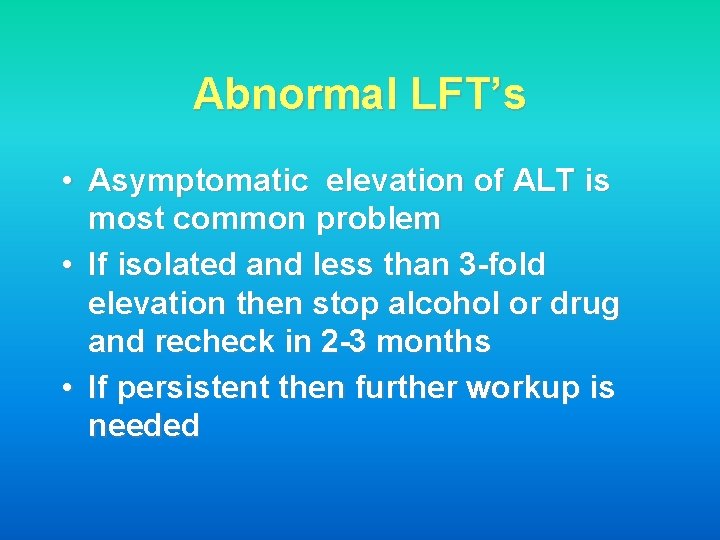
Abnormal LFT’s • Asymptomatic elevation of ALT is most common problem • If isolated and less than 3 -fold elevation then stop alcohol or drug and recheck in 2 -3 months • If persistent then further workup is needed
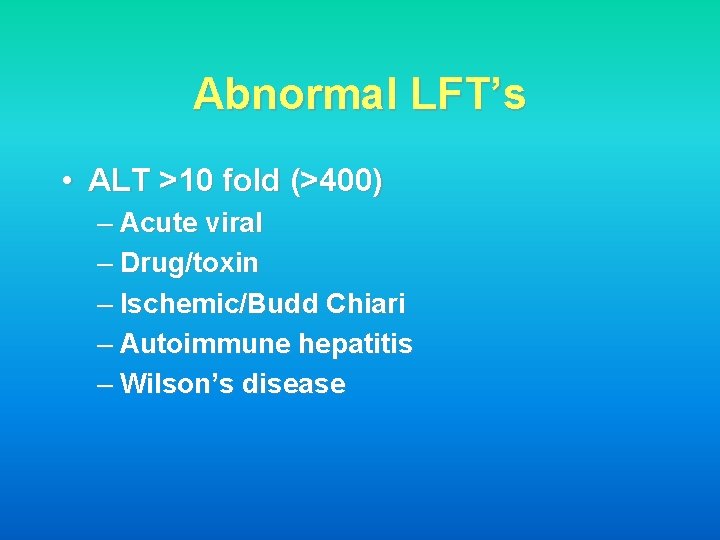
Abnormal LFT’s • ALT >10 fold (>400) – Acute viral – Drug/toxin – Ischemic/Budd Chiari – Autoimmune hepatitis – Wilson’s disease
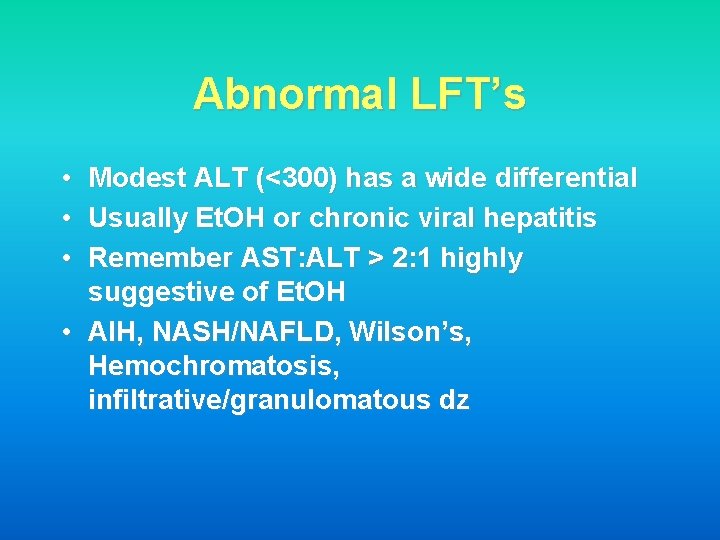
Abnormal LFT’s • • • Modest ALT (<300) has a wide differential Usually Et. OH or chronic viral hepatitis Remember AST: ALT > 2: 1 highly suggestive of Et. OH • AIH, NASH/NAFLD, Wilson’s, Hemochromatosis, infiltrative/granulomatous dz
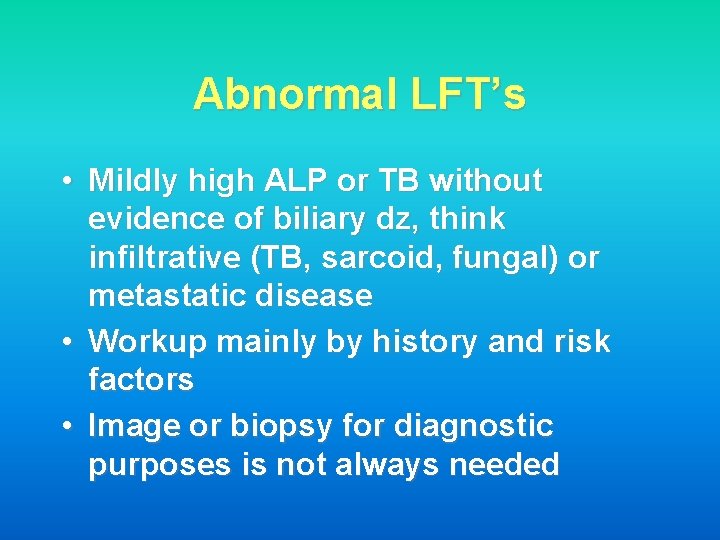
Abnormal LFT’s • Mildly high ALP or TB without evidence of biliary dz, think infiltrative (TB, sarcoid, fungal) or metastatic disease • Workup mainly by history and risk factors • Image or biopsy for diagnostic purposes is not always needed
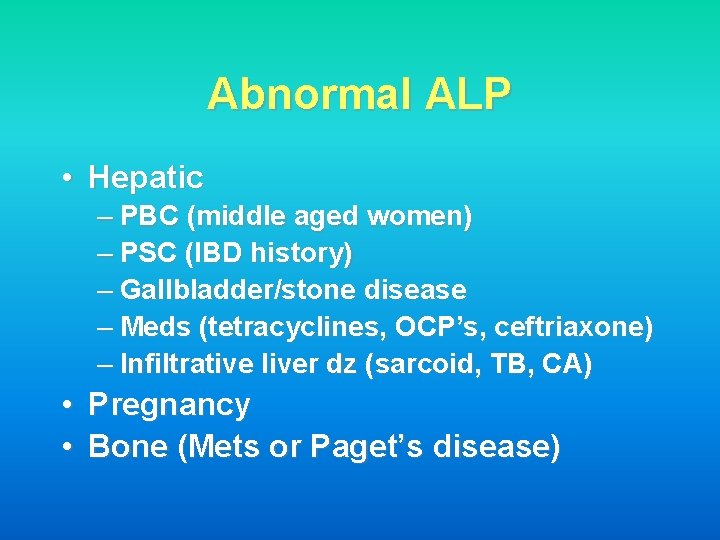
Abnormal ALP • Hepatic – PBC (middle aged women) – PSC (IBD history) – Gallbladder/stone disease – Meds (tetracyclines, OCP’s, ceftriaxone) – Infiltrative liver dz (sarcoid, TB, CA) • Pregnancy • Bone (Mets or Paget’s disease)
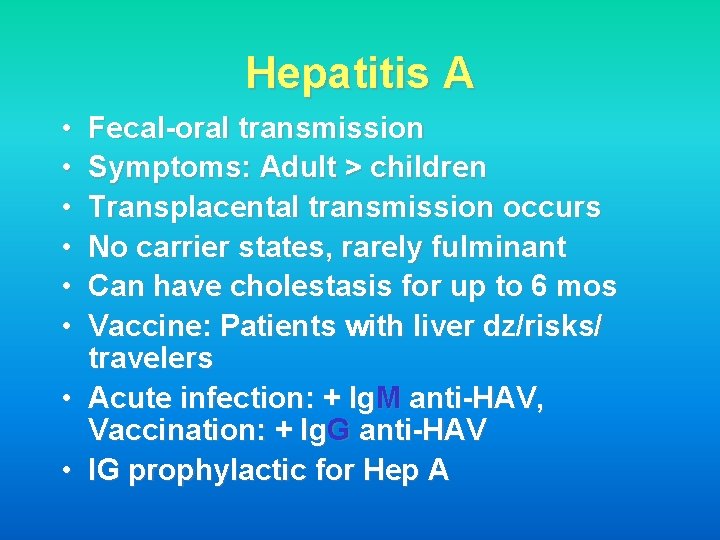
Hepatitis A • • Fecal-oral transmission Symptoms: Adult > children Transplacental transmission occurs No carrier states, rarely fulminant Can have cholestasis for up to 6 mos Vaccine: Patients with liver dz/risks/ travelers Acute infection: + Ig. M anti-HAV, Vaccination: + Ig. G anti-HAV IG prophylactic for Hep A
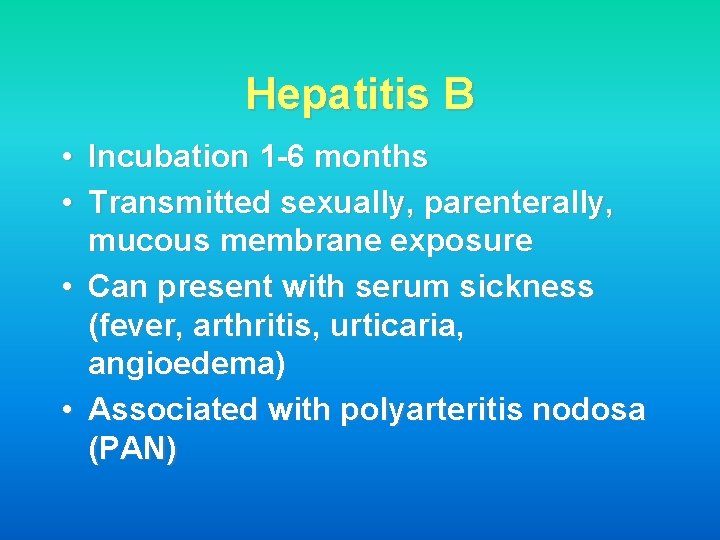
Hepatitis B • Incubation 1 -6 months • Transmitted sexually, parenterally, mucous membrane exposure • Can present with serum sickness (fever, arthritis, urticaria, angioedema) • Associated with polyarteritis nodosa (PAN)
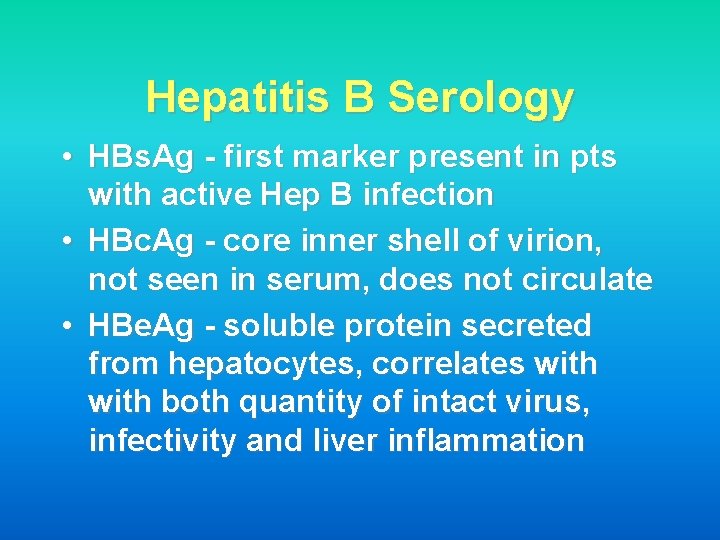
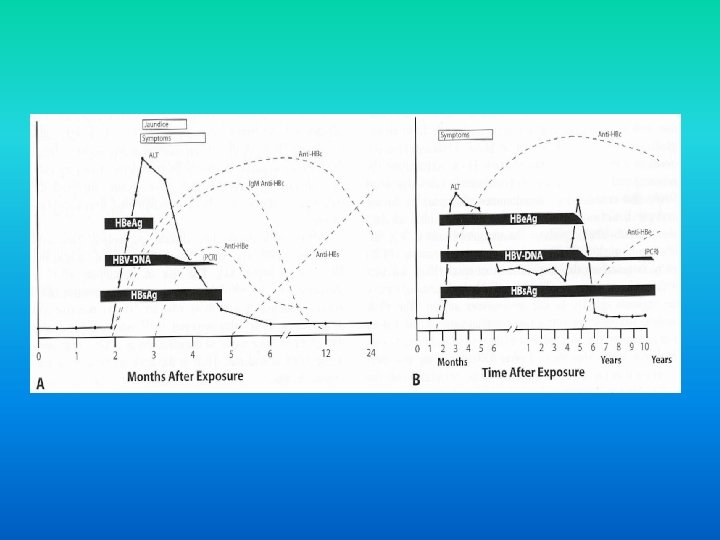
Hepatitis B Serology • HBs. Ag - first marker present in pts with active Hep B infection • HBc. Ag - core inner shell of virion, not seen in serum, does not circulate • HBe. Ag - soluble protein secreted from hepatocytes, correlates with both quantity of intact virus, infectivity and liver inflammation
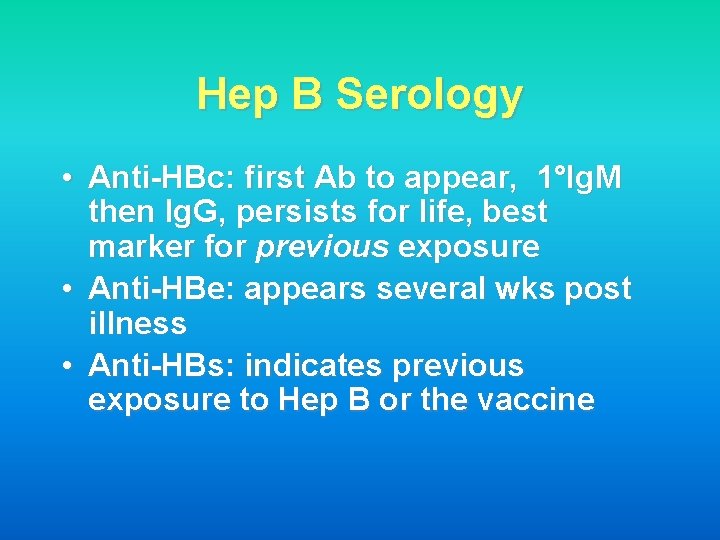
Hep B Serology • Anti-HBc: first Ab to appear, 1°Ig. M then Ig. G, persists for life, best marker for previous exposure • Anti-HBe: appears several wks post illness • Anti-HBs: indicates previous exposure to Hep B or the vaccine
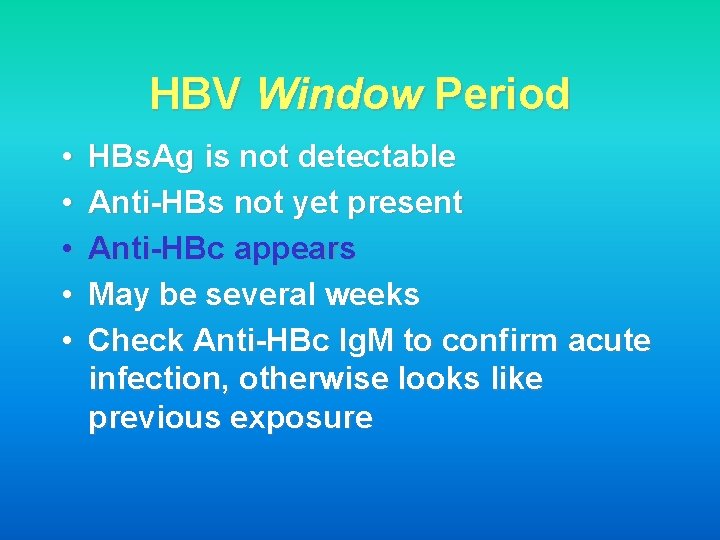
HBV Window Period • • • HBs. Ag is not detectable Anti-HBs not yet present Anti-HBc appears May be several weeks Check Anti-HBc Ig. M to confirm acute infection, otherwise looks like previous exposure
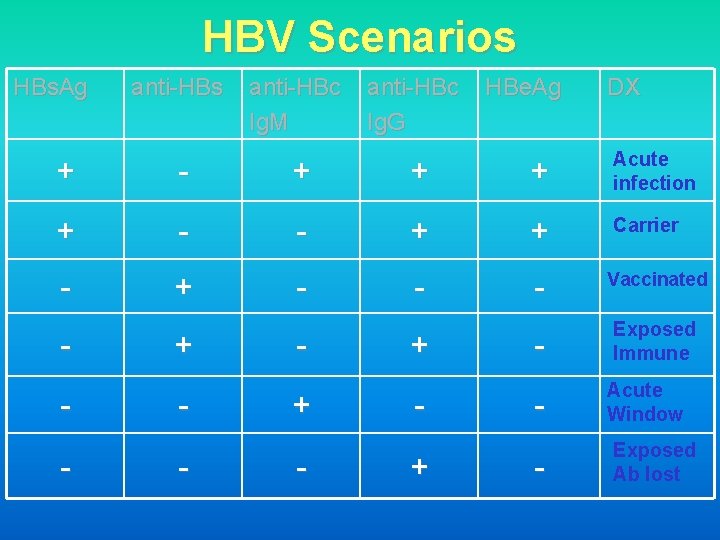
HBV Scenarios HBs. Ag anti-HBs anti-HBc Ig. M anti-HBc Ig. G HBe. Ag DX + - + + + Acute infection + - - + + Carrier - + - - - Vaccinated - Exposed Immune - Acute Window - Exposed Ab lost - + - + +
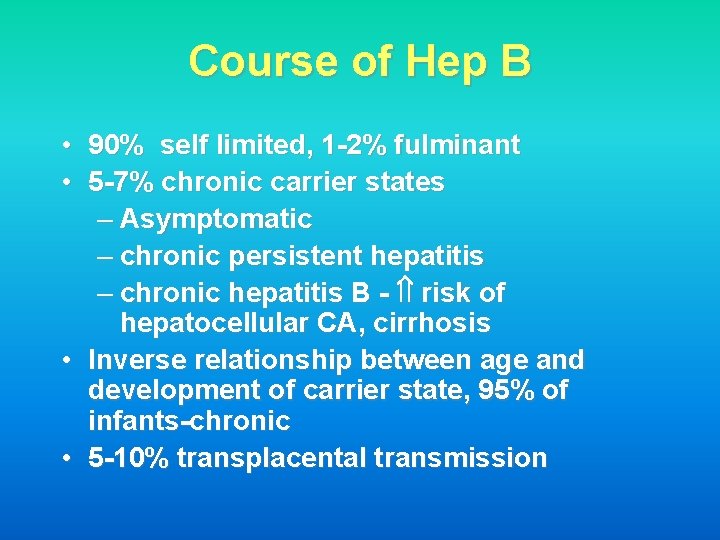
Course of Hep B • 90% self limited, 1 -2% fulminant • 5 -7% chronic carrier states – Asymptomatic – chronic persistent hepatitis – chronic hepatitis B - risk of hepatocellular CA, cirrhosis • Inverse relationship between age and development of carrier state, 95% of infants-chronic • 5 -10% transplacental transmission
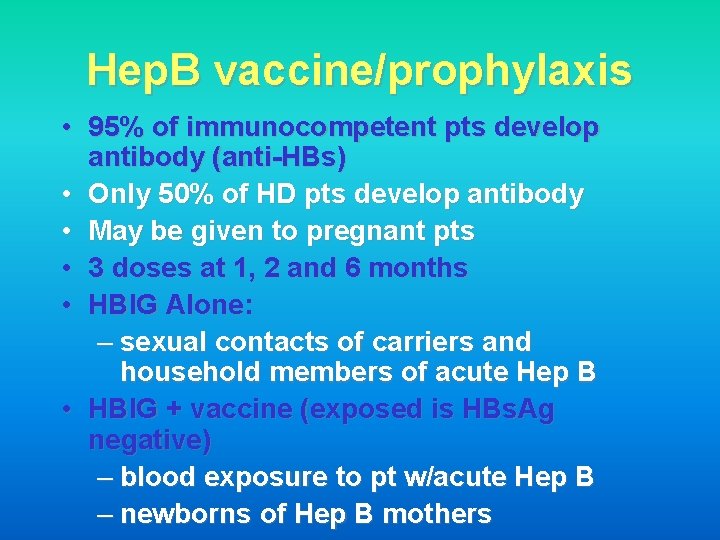
Hep. B vaccine/prophylaxis • 95% of immunocompetent pts develop antibody (anti-HBs) • Only 50% of HD pts develop antibody • May be given to pregnant pts • 3 doses at 1, 2 and 6 months • HBIG Alone: – sexual contacts of carriers and household members of acute Hep B • HBIG + vaccine (exposed is HBs. Ag negative) – blood exposure to pt w/acute Hep B – newborns of Hep B mothers
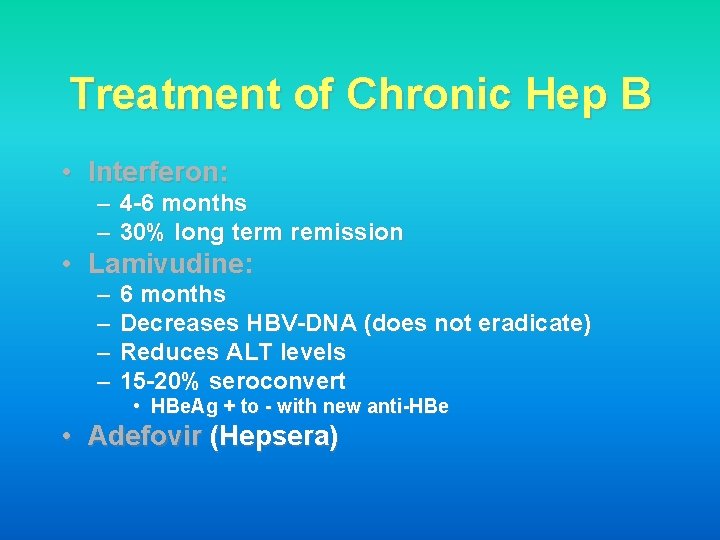
Treatment of Chronic Hep B • Interferon: – 4 -6 months – 30% long term remission • Lamivudine: – – 6 months Decreases HBV-DNA (does not eradicate) Reduces ALT levels 15 -20% seroconvert • HBe. Ag + to - with new anti-HBe • Adefovir (Hepsera)
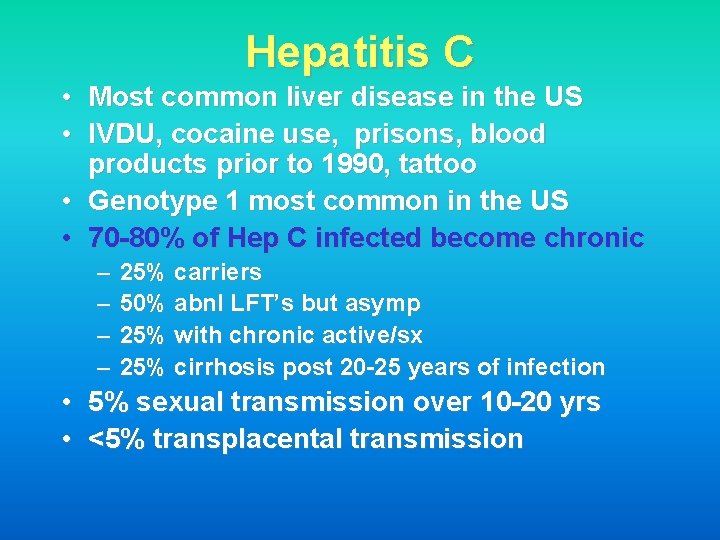
Hepatitis C • Most common liver disease in the US • IVDU, cocaine use, prisons, blood products prior to 1990, tattoo • Genotype 1 most common in the US • 70 -80% of Hep C infected become chronic – – • • 25% carriers 50% abnl LFT’s but asymp 25% with chronic active/sx 25% cirrhosis post 20 -25 years of infection 5% sexual transmission over 10 -20 yrs <5% transplacental transmission
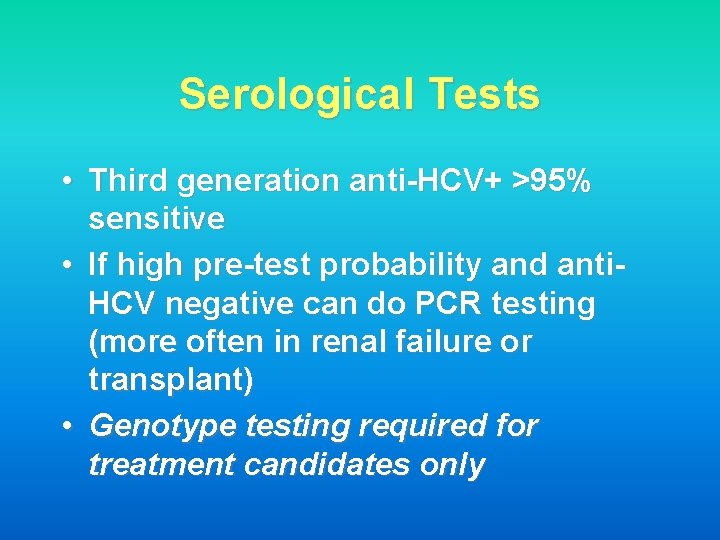
Serological Tests • Third generation anti-HCV+ >95% sensitive • If high pre-test probability and anti. HCV negative can do PCR testing (more often in renal failure or transplant) • Genotype testing required for treatment candidates only
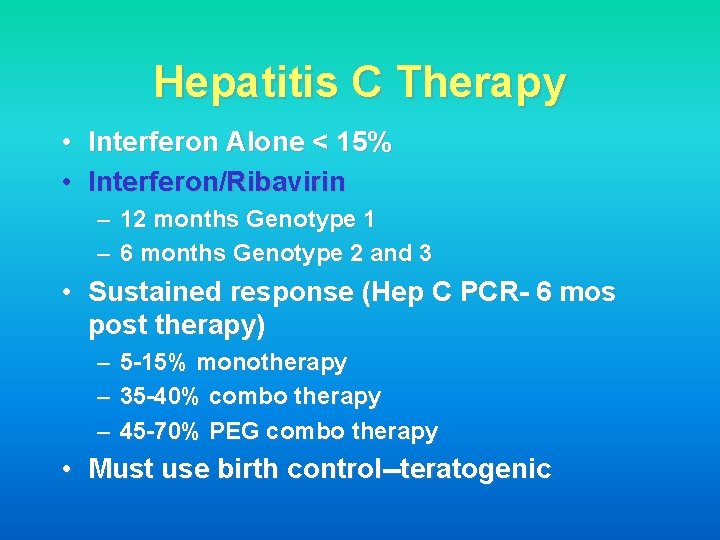
Hepatitis C Therapy • Interferon Alone < 15% • Interferon/Ribavirin – 12 months Genotype 1 – 6 months Genotype 2 and 3 • Sustained response (Hep C PCR- 6 mos post therapy) – 5 -15% monotherapy – 35 -40% combo therapy – 45 -70% PEG combo therapy • Must use birth control--teratogenic
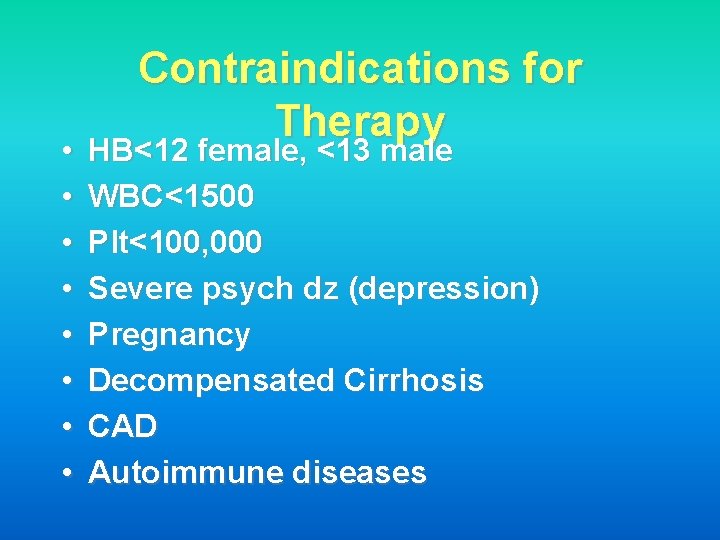
• • Contraindications for Therapy HB<12 female, <13 male WBC<1500 Plt<100, 000 Severe psych dz (depression) Pregnancy Decompensated Cirrhosis CAD Autoimmune diseases
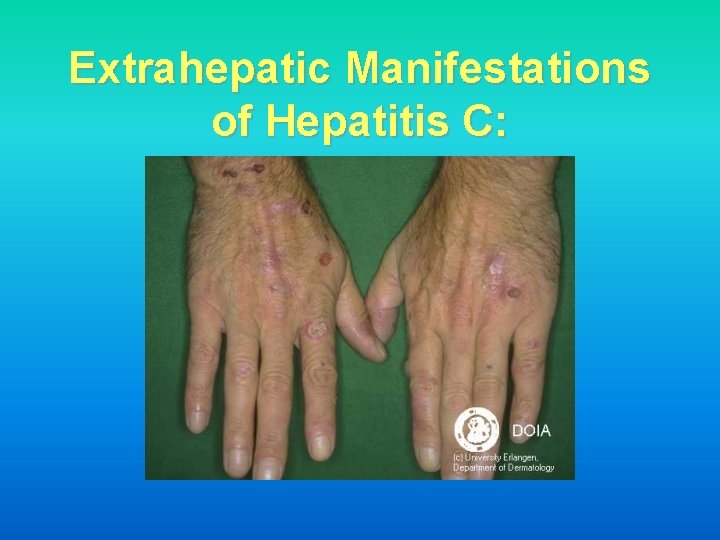
Extrahepatic Manifestations of Hepatitis C:

Extrahepatic Manifestations:

Extrahepatic Manifestations • • Glomerulonephritis/MPGN Cryoglobulins Porphyria cutanea tarda (PCT) Thrombocytopenia – Autoantibody – ITP • • Neuropathy Thyroiditis Sjogren’s Syndrome Inflammatory arthritis
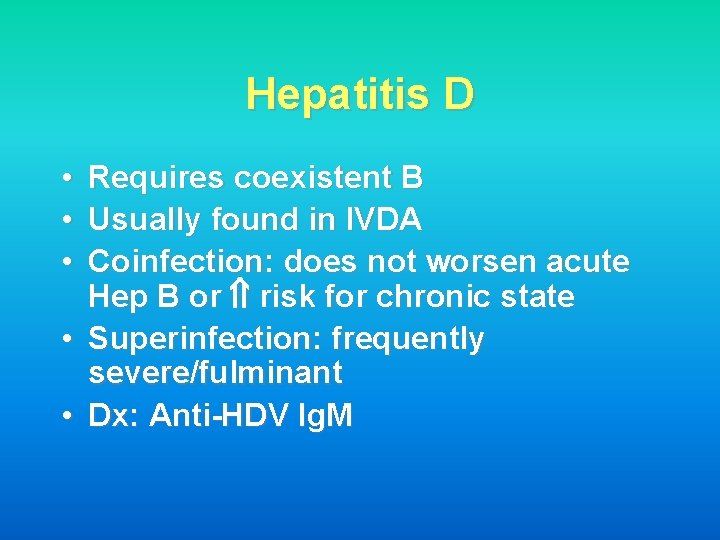
Hepatitis D • • • Requires coexistent B Usually found in IVDA Coinfection: does not worsen acute Hep B or risk for chronic state • Superinfection: frequently severe/fulminant • Dx: Anti-HDV Ig. M
Hepatitis E • • Monsoon flooding Fecal-oral route No chronic forms Fulminant hepatitis in 3 rd trimester of pregnancy
Chronic Hepatitis • By definition, active hepatitis for 6 months or longer • Usually viral but also metabolic and autoimmune
Case • 38 yo woman presents to your office c/o fatigue and pruritis for 6 months. Routine bloodwork reveals normal CBC, TB, AST and ALT. ALP is elevated at 260. • Skin exam shows this:

• • • Primary Biliary Cirrhosis (PBC) Middle-aged woman Elevated alkaline phosphatase Symptom: itching! – Later: jaundice, osteomalacia, osteoporosis Xanthomas/xanthalasmas – hypercholesterolemia with low risk CAD Diagnosis: – antimitochondrial antibody (AMA) – liver bx with granulomas Tx: Ursodeoxycholic acid (Actigall) improves survival; late-liver transplant
Case • 38 yo gentleman with h/o chronic diarrhea and occasional BRBPR who presents to your office with new onset jaundice and fever. • ERCP shows:

Primary Sclerosing Cholangitis (PSC) • Male: female 2: 1 • Intra and Extrahepatic inflammation and sclerosis of the biliary tree • Strong Association (75%) with IBD (Ulcerative colitis) • Cholestatic enzyme pattern (TB and ALP) • Dx: ERCP or cholangiogram • ~15% develop cholangiocarcinoma • Tx: Stenting of dominant strictures, Liver Transplant
Autoimmune Hepatitis • • • Young women insidious hepatitis, elevated AST/ALT assoc with other autoimmune dz – hypothyroid, ITP, Coombs+ anemia • Dx: – Serology: ANA+, Anti-smooth muscle Ab+ (most specific), Elevated quant Ig. G, Anti-LKM – Histology: Plasma cells, interface hepatitis • Tx: Prednisone-rapidly reverses sx and improves survival, add azathioprine for steroid sparing
NASH/NAFLD • Risk Factors: – Obesity or gastric bypass – DM – Hyperlipidemia – TPN, amiodarone • Histology: Steatosis, PMN’s, Necrosis • Tx: Wt Loss (>15%), Exercise, Control of DM, Lipid Lowering Agents
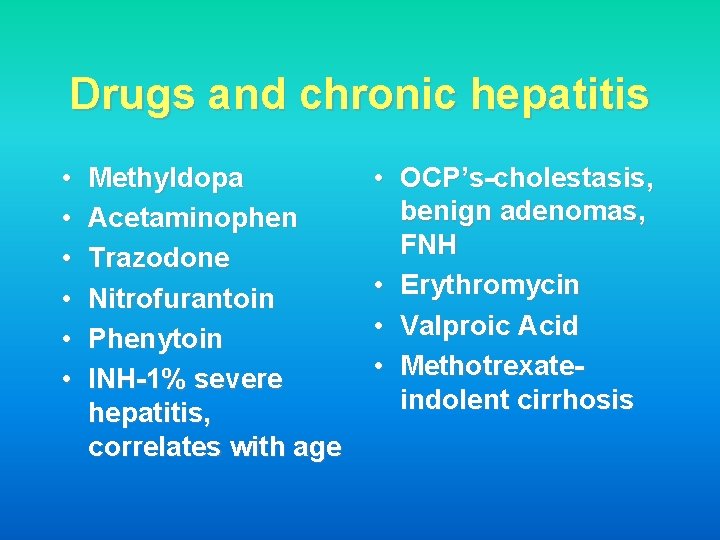
Drugs and chronic hepatitis • • • Methyldopa Acetaminophen Trazodone Nitrofurantoin Phenytoin INH-1% severe hepatitis, correlates with age • OCP’s-cholestasis, benign adenomas, FNH • Erythromycin • Valproic Acid • Methotrexateindolent cirrhosis
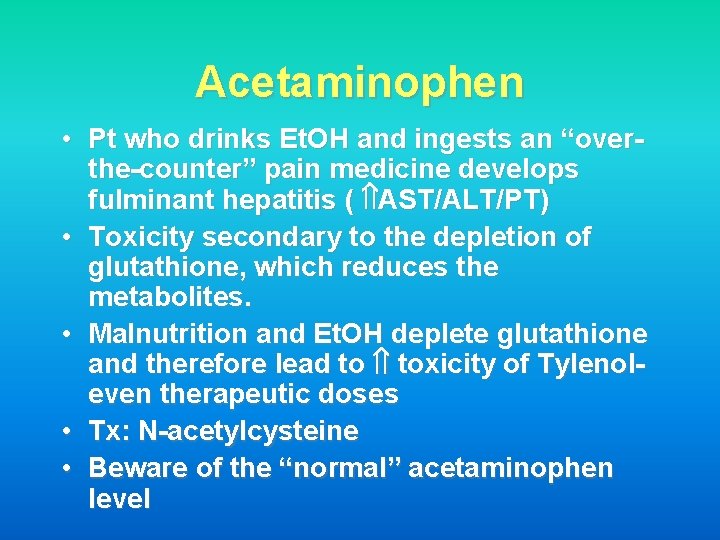
Acetaminophen • Pt who drinks Et. OH and ingests an “overthe-counter” pain medicine develops fulminant hepatitis ( AST/ALT/PT) • Toxicity secondary to the depletion of glutathione, which reduces the metabolites. • Malnutrition and Et. OH deplete glutathione and therefore lead to toxicity of Tylenoleven therapeutic doses • Tx: N-acetylcysteine • Beware of the “normal” acetaminophen level
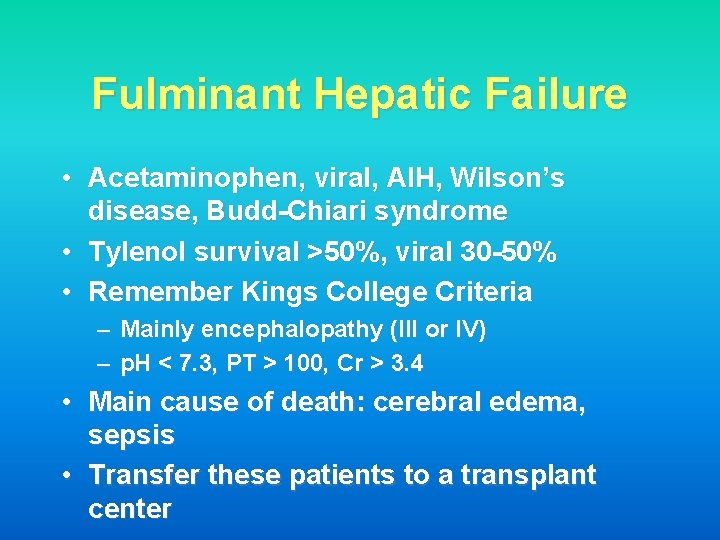
Fulminant Hepatic Failure • Acetaminophen, viral, AIH, Wilson’s disease, Budd-Chiari syndrome • Tylenol survival >50%, viral 30 -50% • Remember Kings College Criteria – Mainly encephalopathy (III or IV) – p. H < 7. 3, PT > 100, Cr > 3. 4 • Main cause of death: cerebral edema, sepsis • Transfer these patients to a transplant center
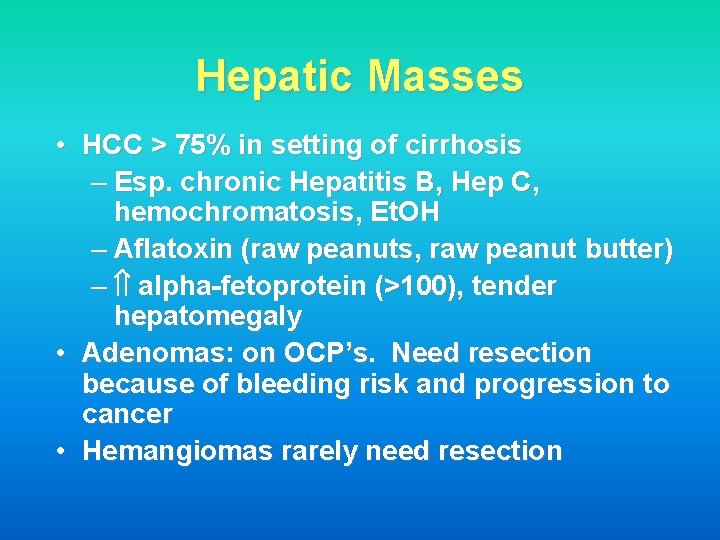
Hepatic Masses • HCC > 75% in setting of cirrhosis – Esp. chronic Hepatitis B, Hep C, hemochromatosis, Et. OH – Aflatoxin (raw peanuts, raw peanut butter) – alpha-fetoprotein (>100), tender hepatomegaly • Adenomas: on OCP’s. Need resection because of bleeding risk and progression to cancer • Hemangiomas rarely need resection
Cirrhosis • Et. OH - most common cause in the U. S. • Esophageal Varices – 1/3 bleed; 1/3 die with bleed – Larger, distal varices bleed – Propranolol rebleeds and may prevent the first bleed – Tx: • Octreotide • Banding or Sclerotherapy • Transjugular intrahepatic portosystemic shunt (TIPS)
Cirrhosis • Encephalopathy – Hyperreflexia and Asterixis – Usually precipitated by infection, bleed, drugs – Tx: Lactulose (acidifies the colonic contents) • Hepatorenal Syndrome – Urinary Na+ < 10, no urine protein – Oliguric Renal Failure – Usually iatrogenic with diuretics/Abx-esp Aminoglycosides
Ascites • Cause: requires peritoneal tap-send for cell count, protein, albumin, cytology • SAAG: Serum albumin-ascitic albumin – >1. 1 Portal Hypertension • Budd-Chiari, RHF, Cirrhosis – <1. 1 Non Portal Hypertensive causes • TB, Nephrotic syndrome, Pancreatitis and Peritoneal carcinomatosis • Chylous Ascites (lymph blockage) – Trauma, Lymphoma, TB and Filiarisis
Ascites • If protein < 1. 0 in cirrhotic ascites then patient is at increased risk for SBP – SBP: • Cloudy fluid, some with fever, abd pain • > 250 PMN’s or >400 total WBC’s • E. coli, Strep, Klebsiella • Treat with cefotaxime • Albumin (1. 5 g/kg, then 1. 0 g/kg on day 3) • Tx: Na+( 2 gm) and water restriction (2 L) – Spironolactone + loop diuretic – Refractory: TIPS
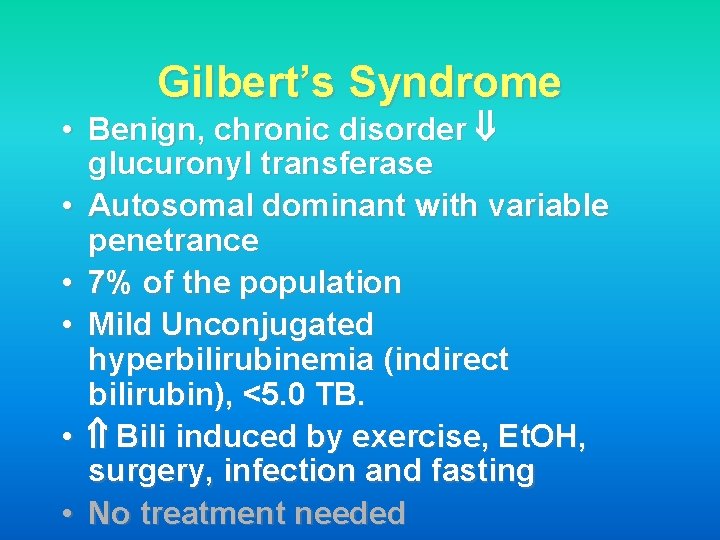
Gilbert’s Syndrome • Benign, chronic disorder glucuronyl transferase • Autosomal dominant with variable penetrance • 7% of the population • Mild Unconjugated hyperbilirubinemia (indirect bilirubin), <5. 0 TB. • Bili induced by exercise, Et. OH, surgery, infection and fasting • No treatment needed
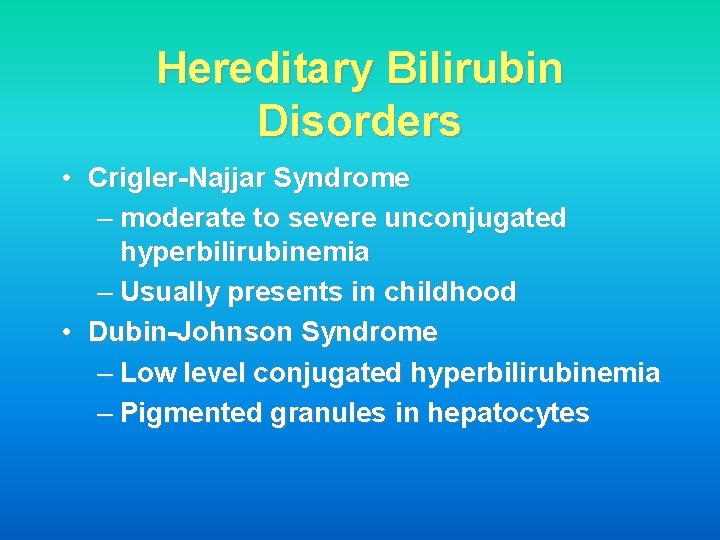
Hereditary Bilirubin Disorders • Crigler-Najjar Syndrome – moderate to severe unconjugated hyperbilirubinemia – Usually presents in childhood • Dubin-Johnson Syndrome – Low level conjugated hyperbilirubinemia – Pigmented granules in hepatocytes
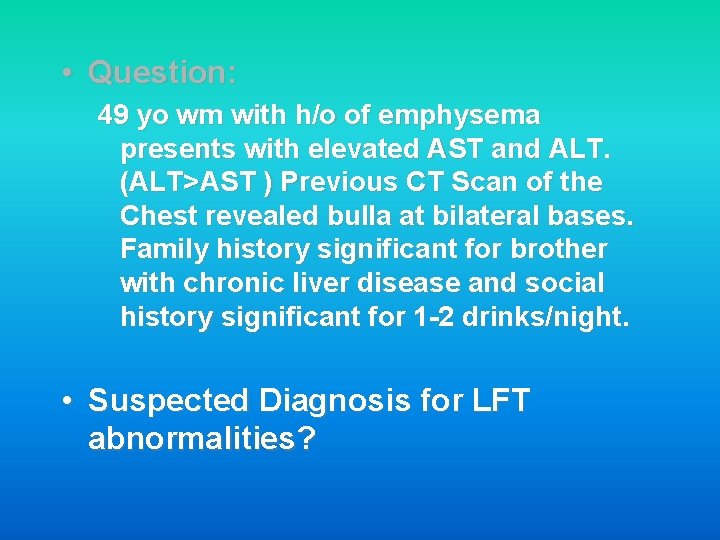
• Question: 49 yo wm with h/o of emphysema presents with elevated AST and ALT. (ALT>AST ) Previous CT Scan of the Chest revealed bulla at bilateral bases. Family history significant for brother with chronic liver disease and social history significant for 1 -2 drinks/night. • Suspected Diagnosis for LFT abnormalities?
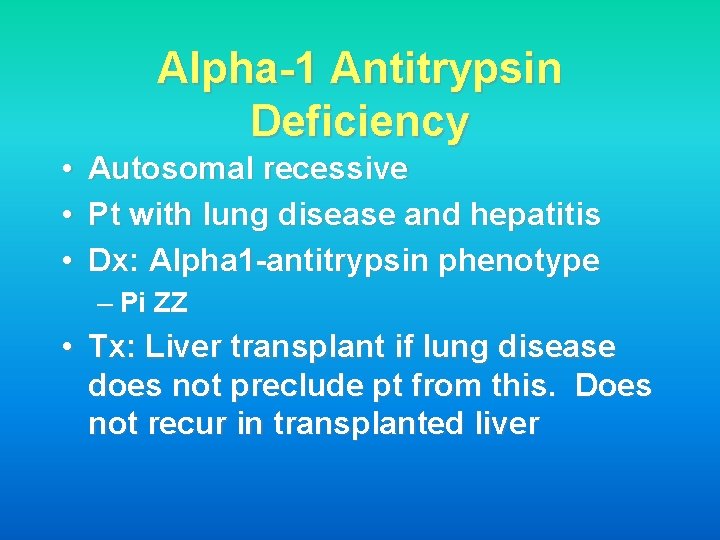
Alpha-1 Antitrypsin Deficiency • • • Autosomal recessive Pt with lung disease and hepatitis Dx: Alpha 1 -antitrypsin phenotype – Pi ZZ • Tx: Liver transplant if lung disease does not preclude pt from this. Does not recur in transplanted liver
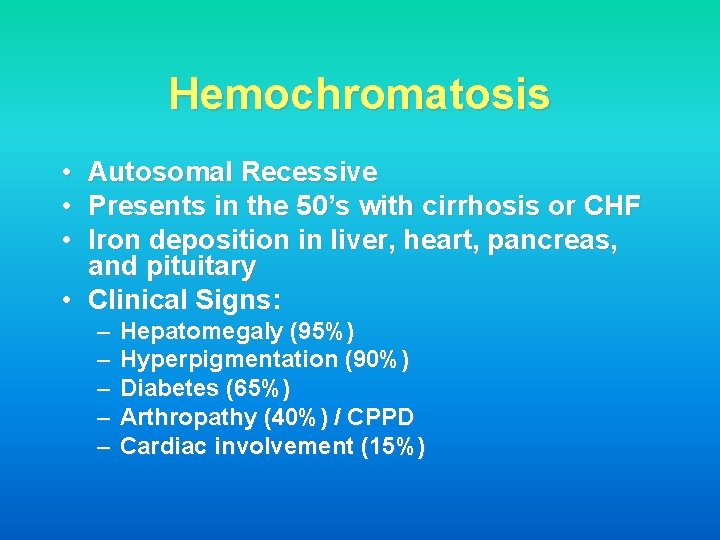
Hemochromatosis • • • Autosomal Recessive Presents in the 50’s with cirrhosis or CHF Iron deposition in liver, heart, pancreas, and pituitary • Clinical Signs: – – – Hepatomegaly (95%) Hyperpigmentation (90%) Diabetes (65%) Arthropathy (40%) / CPPD Cardiac involvement (15%)
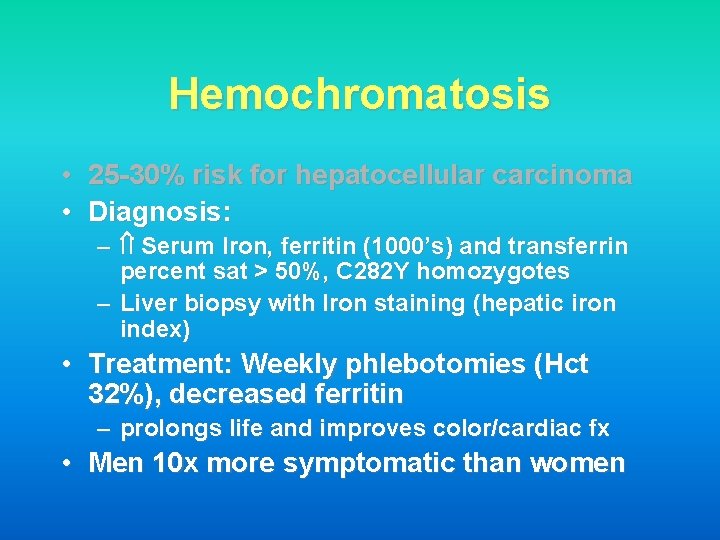
Hemochromatosis • 25 -30% risk for hepatocellular carcinoma • Diagnosis: – Serum Iron, ferritin (1000’s) and transferrin percent sat > 50%, C 282 Y homozygotes – Liver biopsy with Iron staining (hepatic iron index) • Treatment: Weekly phlebotomies (Hct 32%), decreased ferritin – prolongs life and improves color/cardiac fx • Men 10 x more symptomatic than women
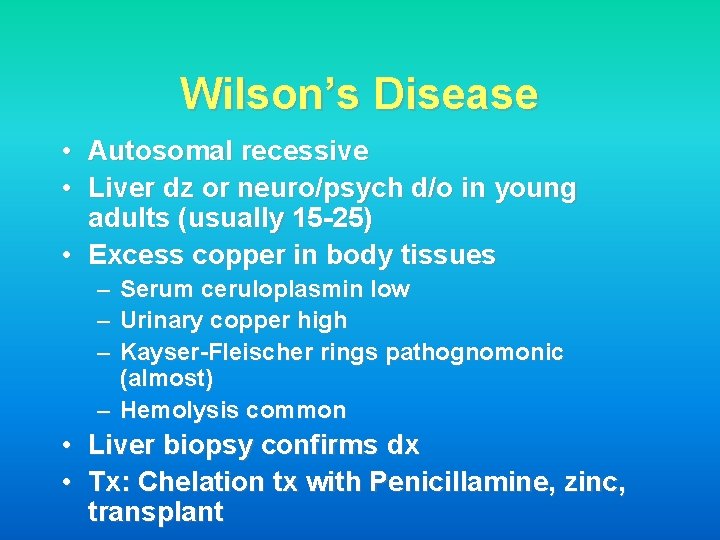
Wilson’s Disease • Autosomal recessive • Liver dz or neuro/psych d/o in young adults (usually 15 -25) • Excess copper in body tissues – Serum ceruloplasmin low – Urinary copper high – Kayser-Fleischer rings pathognomonic (almost) – Hemolysis common • Liver biopsy confirms dx • Tx: Chelation tx with Penicillamine, zinc, transplant
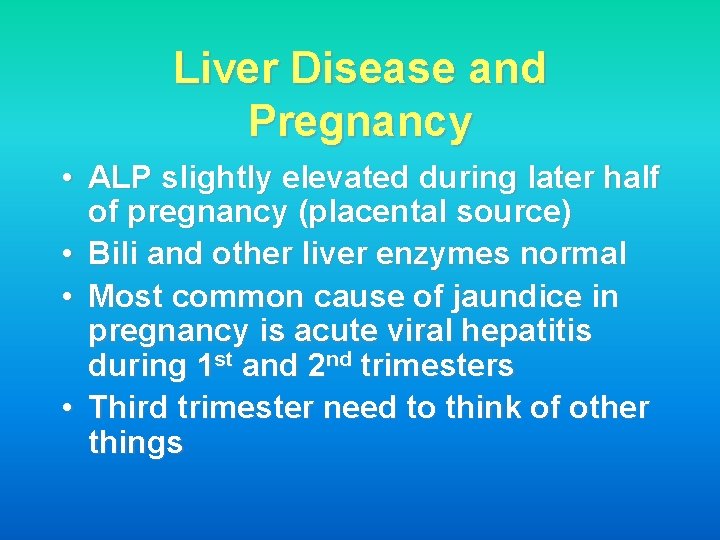
Liver Disease and Pregnancy • ALP slightly elevated during later half of pregnancy (placental source) • Bili and other liver enzymes normal • Most common cause of jaundice in pregnancy is acute viral hepatitis during 1 st and 2 nd trimesters • Third trimester need to think of other things
Acute Fatty Liver of Pregnancy • Very serious, present with fulminant failure • Microvesicular fat deposition • Third trimester • RUQ U/S shows fatty liver • Encephalopathy, hypoglycemia, preeclampsia, DIC and renal failure • Delivery
HELLP Syndrome • Hemolysis, Elevated LFT’s, Low Platelets • Third trimester • Difficult to distinguish from AFLP with DIC clinically • Severe abdominal pain and hypotension may be hepatic hematoma • Delivery
Liver transplant • Treatment for most end-stage liver disease, confined liver cancer, and fulminant failure not responding to supportive measures • Need to consider in all decompensated cirrhotics--encephalopathy, ascites, SBP, variceal bleeding, albumin <2. 5 • Also indicated for intractable pruritis, such as in PBC • Contraindicated in Active Et. OH or drug use, Metastatic CA, severe lung or cardiac disease +/- HIV infection
- Slides: 55