Liver Diseases Function of the liver 1 Production





- Slides: 41
Liver Diseases
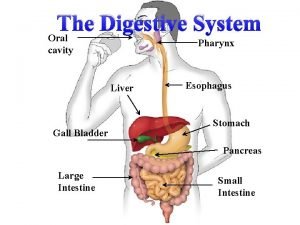
Function of the liver
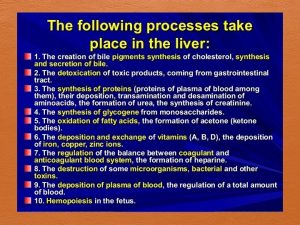
1. Production of bile, which helps break down fats in the small intestine during digestion 2. Production of certain proteins for blood plasma( albumin) 3. Production of cholesterol and special proteins to help carry fats through the body 4. Conversion of excess glucose into glycogen for storage 5. Regulation of blood levels of amino acids, which form the building blocks of proteins
6. Processing of hemoglobin for use of its iron content (The liver stores iron. ) 7. Conversion of poisonous ammonia to urea (Urea is one of the end products of protein metabolism that is excreted in the urine. ) 8. Clearing the blood of drugs and other poisonous substances 9. Regulating blood clotting

Fatty Liver( hepatic steatosis) Fatty Liver : An accumulation of fat in the liver tissue
• Ordinary , the liver triglycerides are packaged into VLDL and exported to the blood stream. • The exact cause of fatty liver is unknown. • Fatty liver represents an imbalance between the amount of fat synthesized in the liver or picked up from the blood and the amount exported to the blood via VLDL
Fatty liver is common to many conditions: 1. Alcoholic liver disease 2. Exposure to drugs and toxic metals 3. Accompanies obesity, diabetes mellitus, kwashiorkor and Marasmus 4. Long-term total parenteral nutrition
Consequences fatty liver • In many individuals , fatty liver causes no harm. • But in other cases it may accompanied by : 1. Liver enlargement ( hepatomegaly) 2. Liver inflammation 3. Fatigue 4. Liver damage 5. Liver failure 6. Liver cancer
Consequences fatty liver • Abnormal elevation liver enzyme levels ALT( alanine aminotransferase) and AST ( aspartate aminotransferase) • Increased triglycerides • Elevated cholesterol levels • Elevated blood glucose levels
Treatment Fatty Liver Elimination of factors that cause it üAlcohol abuse üDrug treatment • Weight reduction – no rapid – may accelerate progression of liver disease • Physical activity • Reduction of blood lipid levels • Medications to improve insulin sensitivity
Insulin resistance promotes fat accumulation in the liver by : 1. Stimulating fatty acid synthesis 2. Inhabiting fatty acid oxidation 3. Blokking VLDL secretion into the blood stream.
Hepatitis : Inflammation of the liver Acute Hepatitis : lasts less than six months Chronic Hepatitis: lasts six months or longer
Causes of Hepatitis 1. Infection with specific viruses, which are designated by the letters A, B, C, D, and E. 2. Contact with infected persons 3. Ingesting contaminated food or water 4. Excessive alcohol intake 5. Exposure to certain drugs and toxic chemicals
Viral hepatitis Hepatitis A ( HAV) : • spread via fecal – oral route , is due to the contamination of foods with fecal materials. • It usually resolves within a few months and dose not cause chronic illness or permananent liver damage.
Hepatitis B ( HAB) : • Is transmitted by infected blood or needles Hepatitis C ( HAC) : Is transmitted by blood contact. • Both can cause cirrhosis and liver cancer.
Symptoms of Hepatitis • • • Fatigue Nausea Anorexia Pain in the liver area Fever Headache Muscle pain Skin rashes Elevated serum levels of ALT & AST Jaundice
Jaundice Results when liver dysfunction impairs the metabolism of bilirubin, a breakdown of hemoglobin that is normally eliminated in bile. Accumulation of bilirubin in the bloodstream leads to yellow discoloration of tissues.
Treatment of Hepatitis • Bed rest • Appropriate diet • Avoid substances that may aggravate the liver – alcohol and drugs or dietary supplements that cause liver toxicity • Hepatitis A usually resolves without use of medications • Antiviral agents – hepatitis B, hepatitis C

Medical Nutrition Therapy of Hepatitis • Nutrition care varies according to patients symptoms and nutrition status • If malnourished : a diet adequate in protein (1. 0 – 1. 2 g/kg) and energy • Small, frequent meals
Medical Nutrition Therapy: • If fluid retention – avoid high-sodium foods • Low-fat diet (<30% kcalories) if steatorrhea present • Fluid and electrolyte replacement for persistent vomiting • Liquid supplements may improve nutrient intake

Cirrhosis
Cirrhosis : • End-stage condition that results from long-term liver disease in which gradually destroys liver tissue. extensive scarring replaces healthy liver tissue causing impairment liver function and liver failure
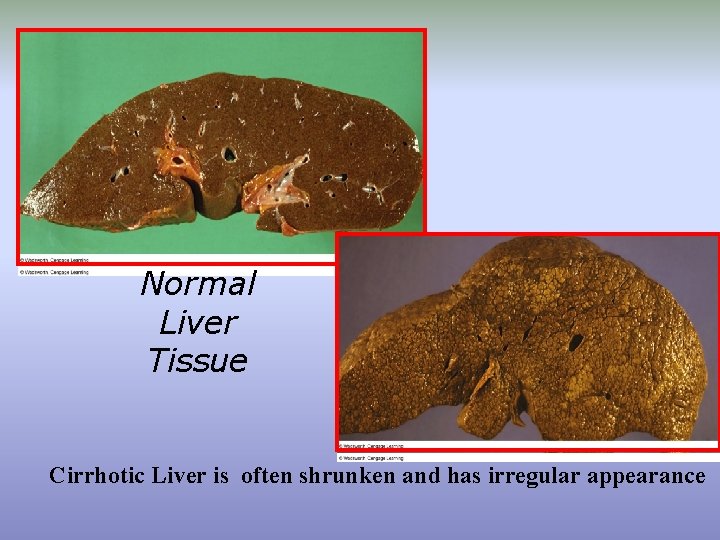
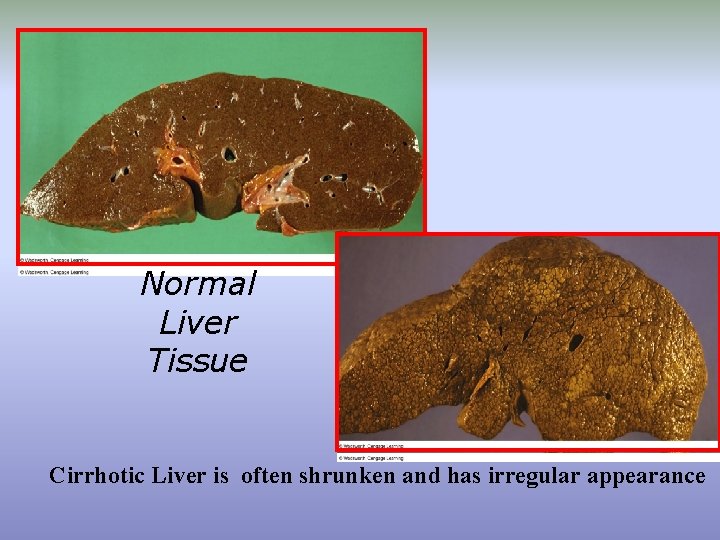
Normal Liver Tissue Cirrhotic Liver is often shrunken and has irregular appearance

Consequences of cirrhosis 1. Initial disease: mild or asymptomatic, fatigue, weakness, anorexia, weight loss 2. Later disease: decline in liver function, anemia, impaired blood clotting, increased susceptibility to infection, jaundice, fat malabsorption 3. Advanced disease: disruption of kidney & lung function , altered liver enzymes, bilirubin levels, lowered albumin levels, extended clotting times and elevated blood ammonia levels
Cirrhosis - Consequences 1. Portal hypertension: resistance to blood flow in liver causes a rise in pressure within the portal vein
Cirrhosis - Consequences 2. esophageal varices : dilated vessels develop throughout the gastrointestinal tract that become enlarged and engorged. it may rupture and cause sever bleeding
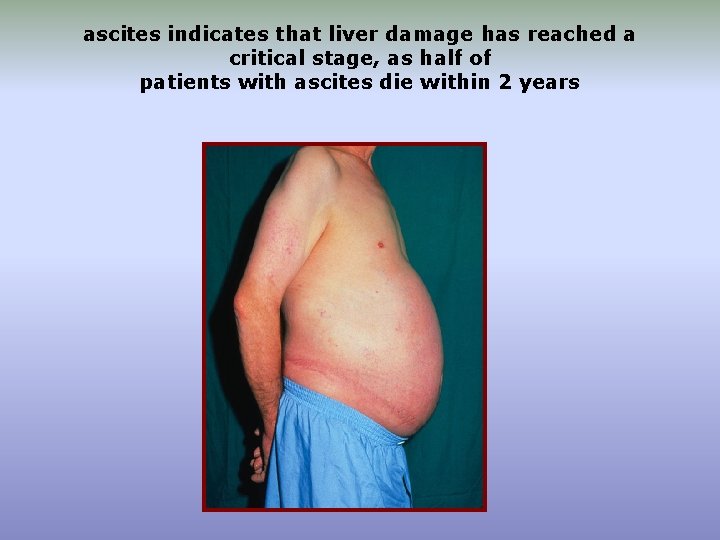
Cirrhosis - Consequences 3. Ascites : abnormal accumulation of fluid in the abdominal cavity caused by: ü Portal hypertension forces fluids to leak from the blood into abdominal cavity ü Water retention due to altered kidney function ü Reduced albumin synthesis by the diseased liver which helps to retain the fluid in blood vessels.

Ascites can cause üAbdominal discomfort and early satiety leading to malnutrition üBody weight is difficult to interpret
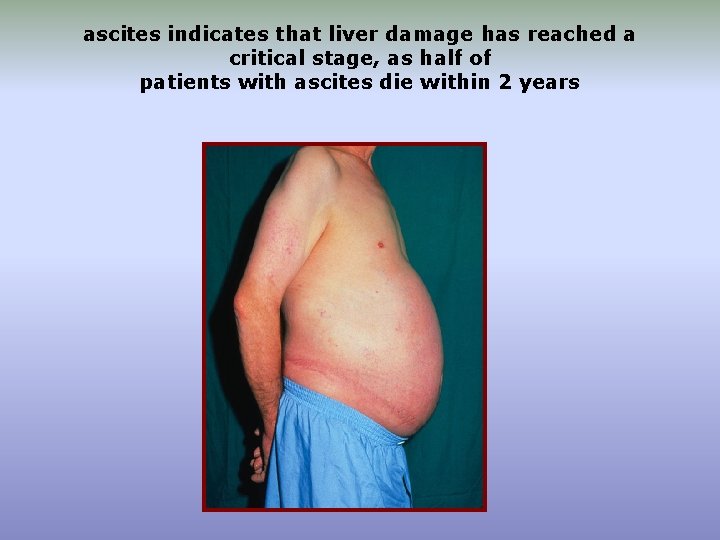
ascites indicates that liver damage has reached a critical stage, as half of patients with ascites die within 2 years
Cirrhosis - Consequences 4. Hepatic encephalopathy: disorder characterized by abnormal neurological functioning Caused by elevated ammonia levels Including changes in: personality, mental abilities, motor functions. At worst , hepatic coma may develop.
5. Elevated blood ammonia levels: ü Much of body free ammonia is produced by bacterial action on unabsorbed dietary protein in the colon ü Normally, the liver extracts ammonia from portal blood and converts it to urea, most of which is excreted by the kidneys ü In advanced liver disease, reaches the brain tissue – producing neurological symptoms called hepatic encephalopathy
Cirrhosis - Consequences 6 - Malnutrition and wasting ü Most patients with cirrhosis are at high risk of developing protein-energy malnutrition (PEM) caused by combination of several factors: ü Consume less food due to reduced appetite, fatigue, or gastrointestinal symptoms (ascites – early satiety) ü taste changes ü Diet has lack of taste due to limited sodium intake ü Fat malabsorption – steatorrhea ü Catabolism, inadequate protein synthesis, reduce nutrient storage
Medical nutrition therapy of Cirrhosis
• MNT is customized to each patients need 1 -Energy • Calculate resting metabolic rate (RMR) and multiply by stress factor 1. 2 initially • Nutrient malabsorption, recent weight loss, and infection increase energy needs • RMR calculations are based on desirable weight or estimated dry weight (weight without ascites) • A value for dry weight can be obtained after diuretic therapy or after a medical procedure that directly removes excess abdominal fluid. • Four to six feedings daily
Cirrhosis - MNT 2 -Protein • Protein recommendations 0. 8 – 1. 2 grams per kg body weight (desirable weight or dry weight) • Protein restriction may worsen malnutrition and wasting • Patients with hepatic encephalopthy should avoid excessive protein consumption and their protein intake should be modest in quantity and spread throughout the day. • Protein restriction is not helpful because it can worsen malnutrition
Cirrhosis - MNT 3 - Carbohydrate • Carbohydrate provides a good portion of energy need. • Many patients with cirrhosis are insulin resistant and require medicines or insulin to manage hyperglycemia • Patients with diabetes – consume mostly complex carbohydrates at regular intervals
Cirrhosis - MNT 4 - Fat • Patients with fat malabsorption – restricted to less than 30 % of total kcalories or as necessary to control steatorrhea • If steatorrhea present, fat intake is restricted, medium-chain triglycerides (MCT) can be used to provide energy but supplementation with essential fatty acids is necessary. • Severe steatorrhea – warrants supplementation of fat-soluble vitamins, calcium, magnesium, and zinc
Cirrhosis - MNT 5 - Sodium and fluid • If ascites present – restrict sodium to no more than 2000 mg/day • if unpalatable may allow more liberal sodium intake & depend on diuretics to mobilize fluid • Diuretic therapy
Cirrhosis - MNT 5 - Sodium and fluid • Patients who are non-responsive to sodium restriction and diuretic therapy fluids may be removed by surgical puncture • Monitor potassium intake if on potassiumwasting diuretic • If ascites present – restrict sodium to no more than 2000 mg/day • Fluid restriction serum sodium <128 meq/L – 1, 200 -1, 500 m. L/day serum sodium < 125 meq/L – 1, 000 -1, 200 m. L/day
Cirrhosis - MNT 6 - Vitamins and minerals • Vitamin and mineral deficiencies can be a result of the illness, complications of disease, or alcoholism • Multivitamin supplementation is recommended • If steatorrhea occurs, fat-soluble nutrients provided in water-soluble forms • If esophageal varices – liquid form may be preferred
7 - Enteral and parenteral nutrition support ü may be used in patients who are unable to consume enough food. • Enteral standard formulas – energy-dense, moderate-protein, low-electrolyte may be necessary for patients with ascites or fluid restriction. • Tube feeding may be warranted if varices present so use narrow, flexible tube • Parenteral nutrition may be needed if obstruction, gastrointestinal bleeding or uncontrollable vomiting
 Pre production post production
Pre production post production Test for gilbert syndrome
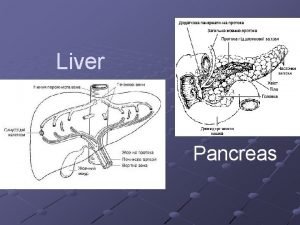
Test for gilbert syndrome Liver and pancreas function
Liver and pancreas function L
L Synthetic function of liver
Synthetic function of liver Physiolocial
Physiolocial Function of liver physiology
Function of liver physiology What is the primary function of the liver
What is the primary function of the liver Normal lft
Normal lft Liver profile
Liver profile Pylonephrite
Pylonephrite Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
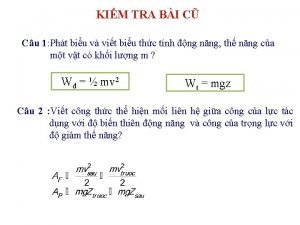
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
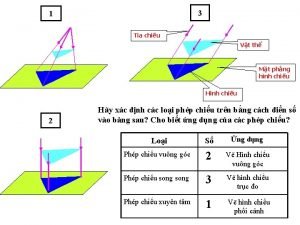
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là