Liver cirrhosis Usama Ahmed Arafa MD Ass Professor















- Slides: 42
Liver cirrhosis Usama Ahmed Arafa, MD Ass. Professor of Internal Medicine

Definition
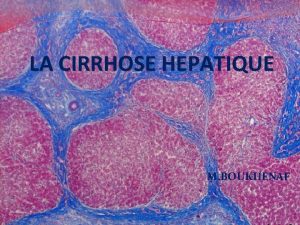
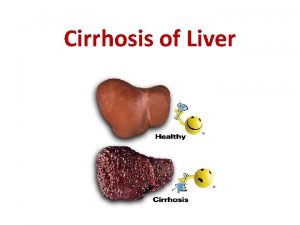
Liver cirrhosis is characterized by: 1 - Hepatocellular necrosis 2 - Hepatic fibrosis 3 - Regeneration nodules 4 - Loss of architecture
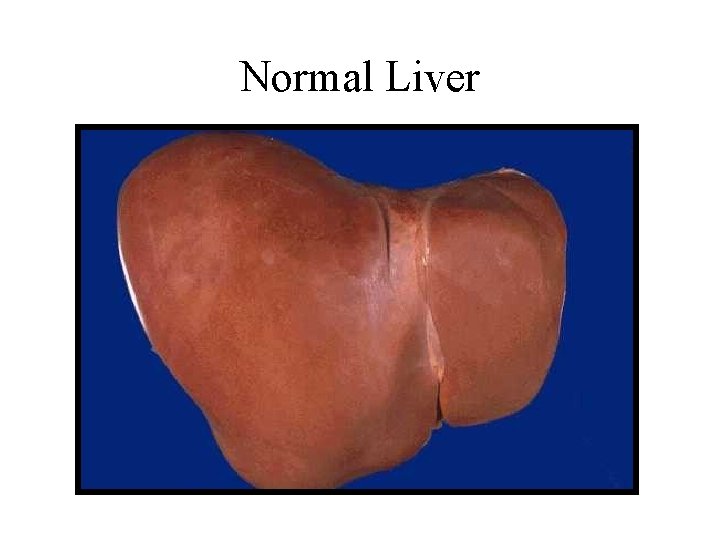
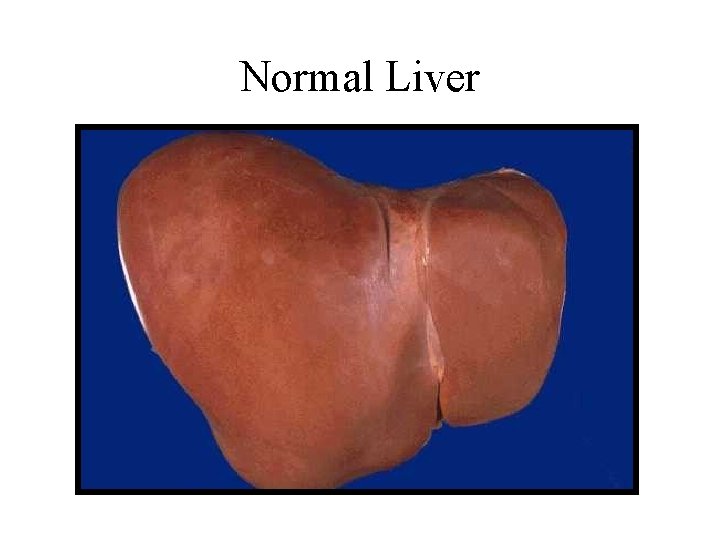
Normal Liver
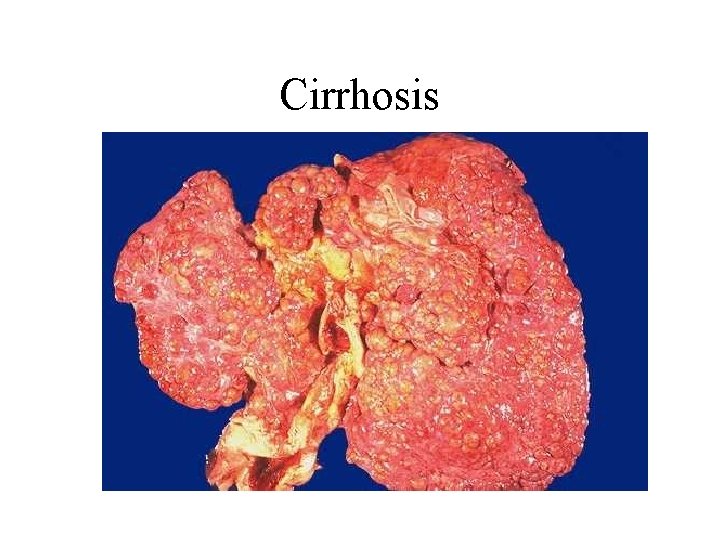
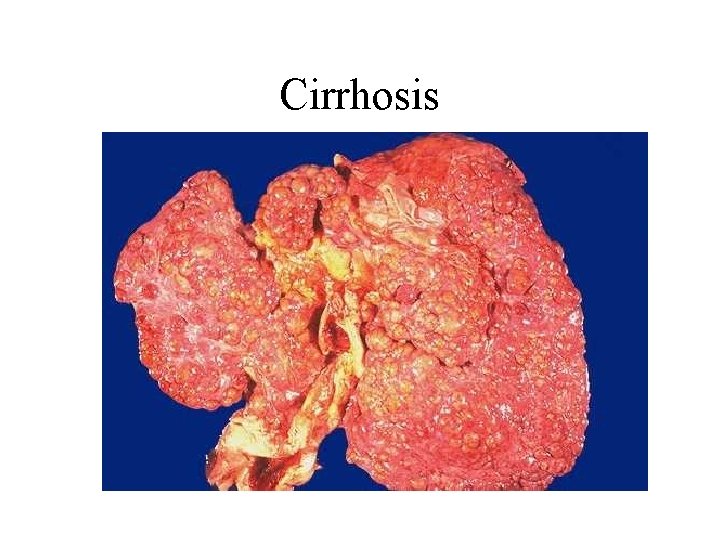
Cirrhosis

Normal Liver Histology CV PT
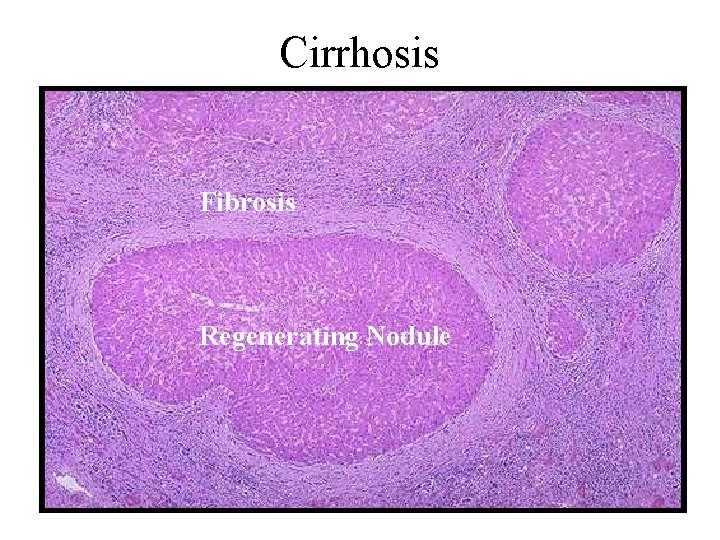
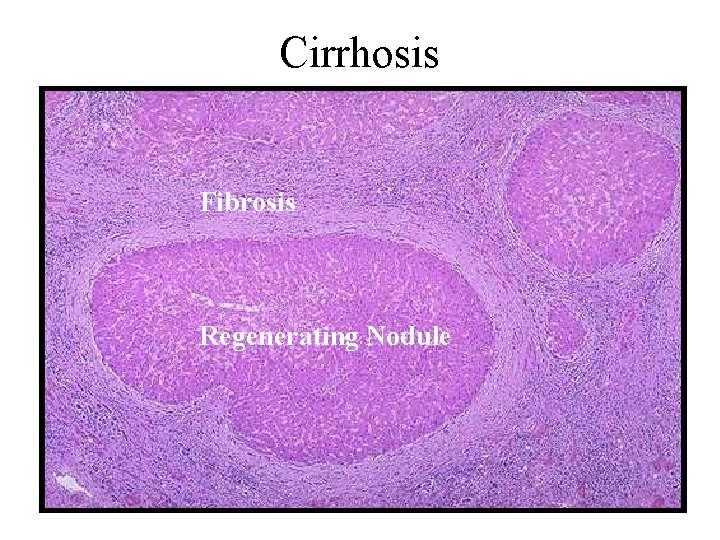
Cirrhosis Fibrosis Regenerating Nodule

Etiology
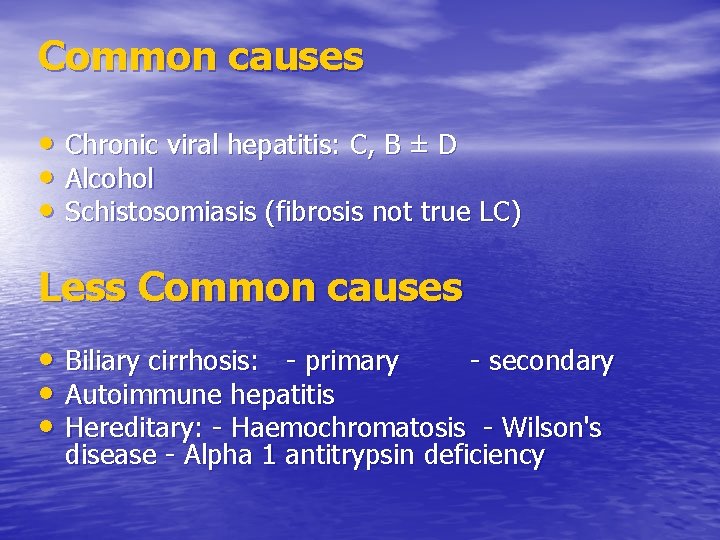
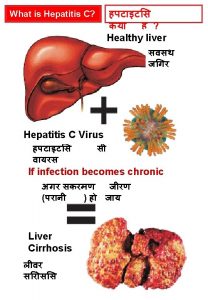
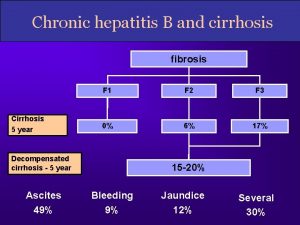
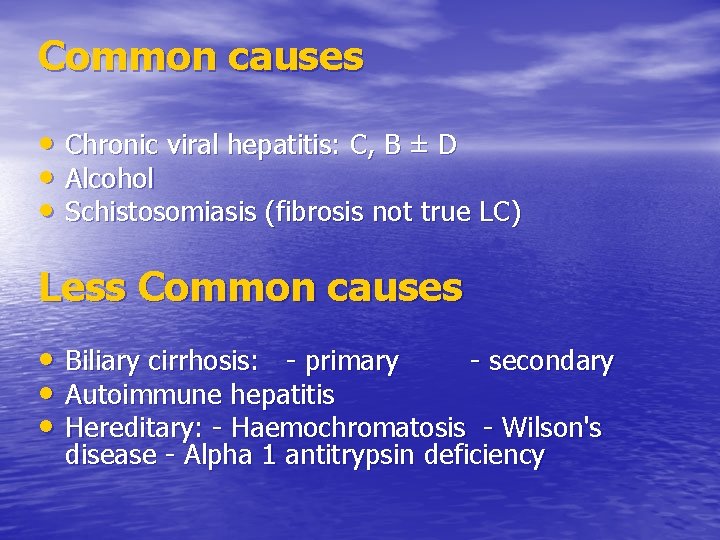
Common causes • Chronic viral hepatitis: C, B ± D • Alcohol • Schistosomiasis (fibrosis not true LC) Less Common causes • Biliary cirrhosis: - primary - secondary • Autoimmune hepatitis • Hereditary: - Haemochromatosis - Wilson's disease - Alpha 1 antitrypsin deficiency

• Drugs (e. g. methotrexate) • Cystic fibrosis • Non-alcoholic fatty liver disease (NAFLD) • Glycogen storage disease • Veno-occlusive disease • Hepatic venous congestion • Budd-Chiari syndrome • Idiopathic (cryptogenic)

Pathogenesis
• Chronic injury to the liver results in inflammation, necrosis and, eventually, fibrosis. • Fibrosis is initiated by activation of the stellate cells.
• In the space of Disse, the normal matrix is replaced by collagen. Subendothelial fibrosis leads to loss of the endothelial fenestrations, and this impairs liver function. • There is accumulating evidence that liver fibrosis is reversible.

• Pathogenesis of fibrosis
Pathological Types
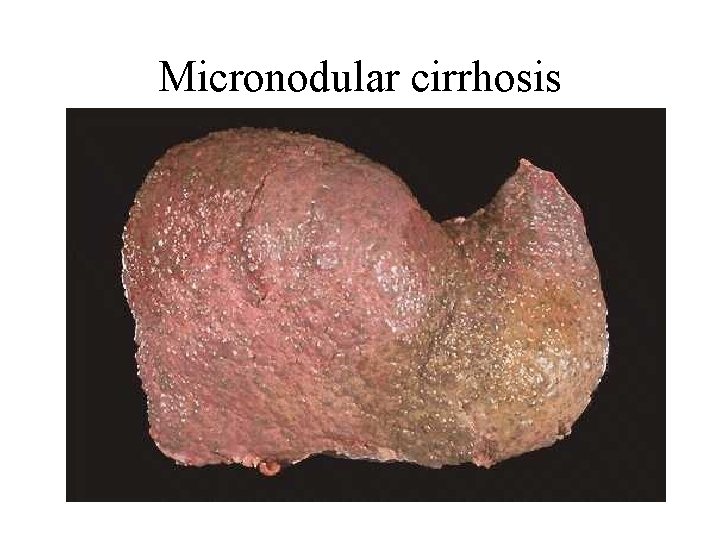
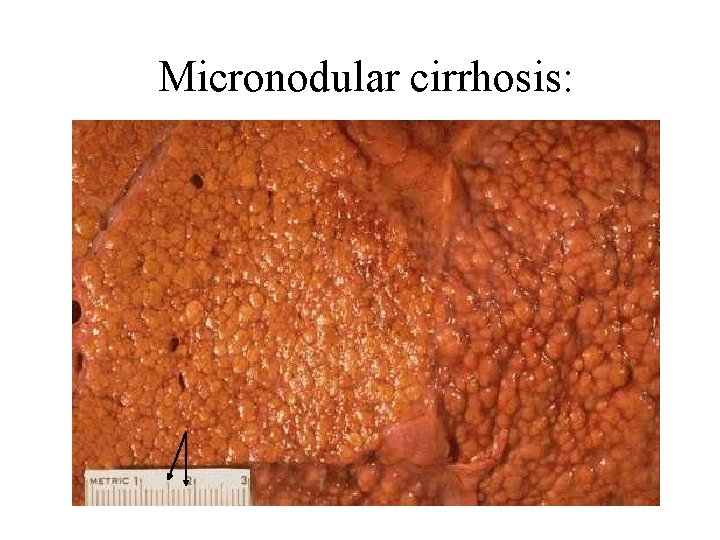
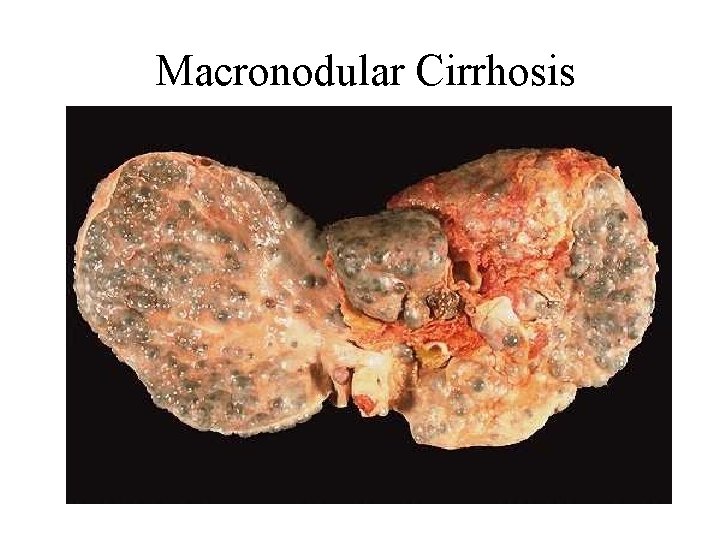
Micronodular cirrhosis: Regenerating nodules are usually less than 3 mm in size. This type is often caused by alcoholic or biliary cirrhosis. Macronodular cirrhosis: The nodules are of variable size and normal acini may be seen within the larger nodules. This type is often seen following previous hepatitis. A mixed picture: with small and large nodules is sometimes seen.
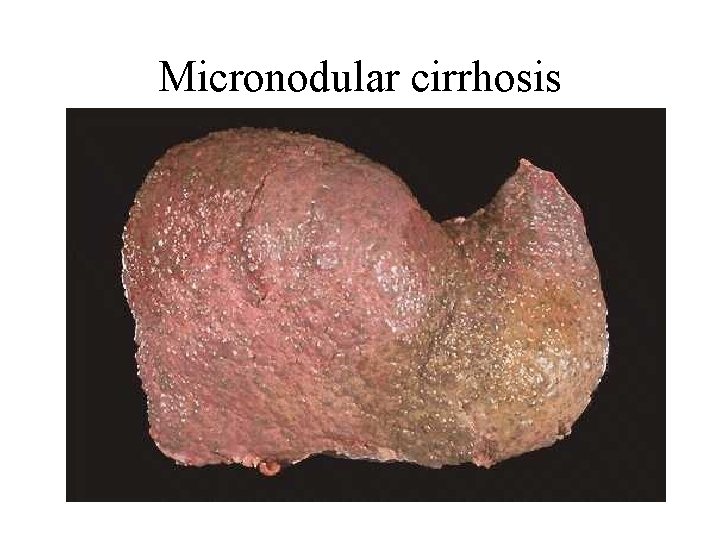
Micronodular cirrhosis
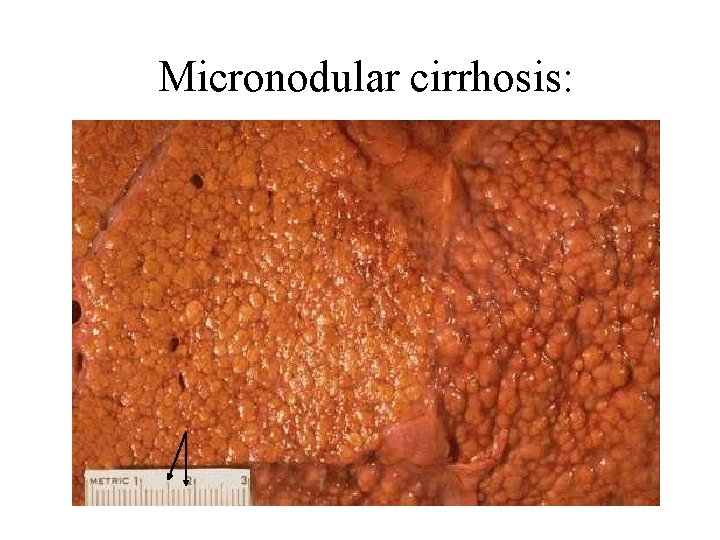
Micronodular cirrhosis:
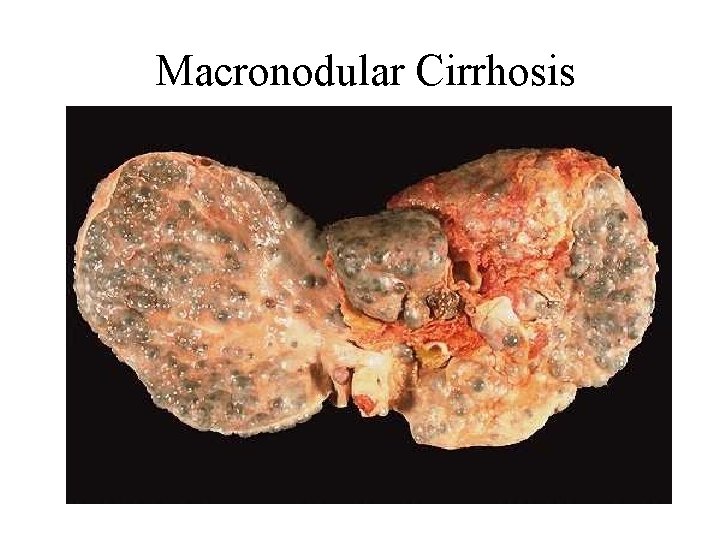
Macronodular Cirrhosis

Symptoms and Signs

A- General manifestations • Wasting • Parotid enlargement • Hyperkinetic circulation • Increased susceptibility to infection

B- Skin manifestations • Spider nevi • Palmar erythema • Leuconychia • Dupuytren’s contractures • Xanthomas • Alternation of body hair distribution

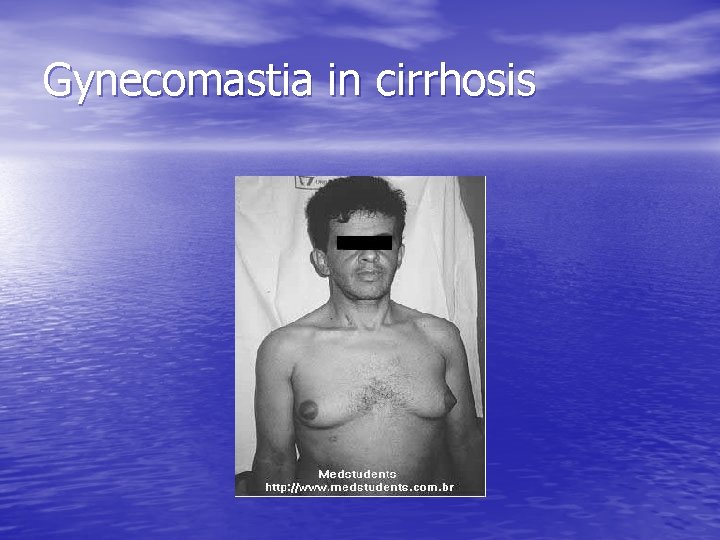
C- Endocrinal manifestations • Gynecomastia • Testicular atrophy • Amenorrhea in females
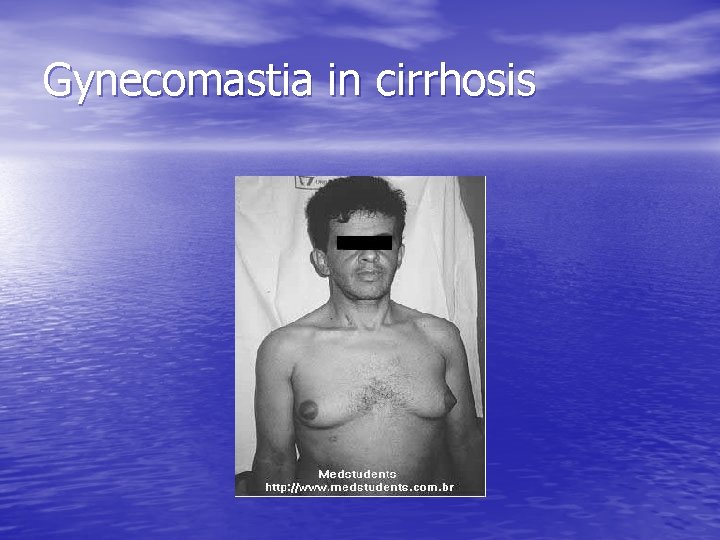
Gynecomastia in cirrhosis

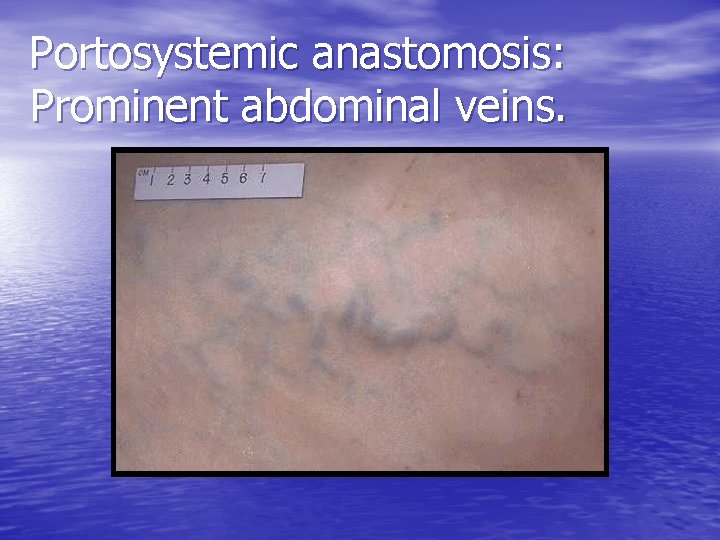
D- Abdominal manifestations • Hepatomegaly then shrinkage later • Splenomegaly • Prominent abdominal veins • Peptic ulcer disease • Chronic pancreatitis • Steatorrhea
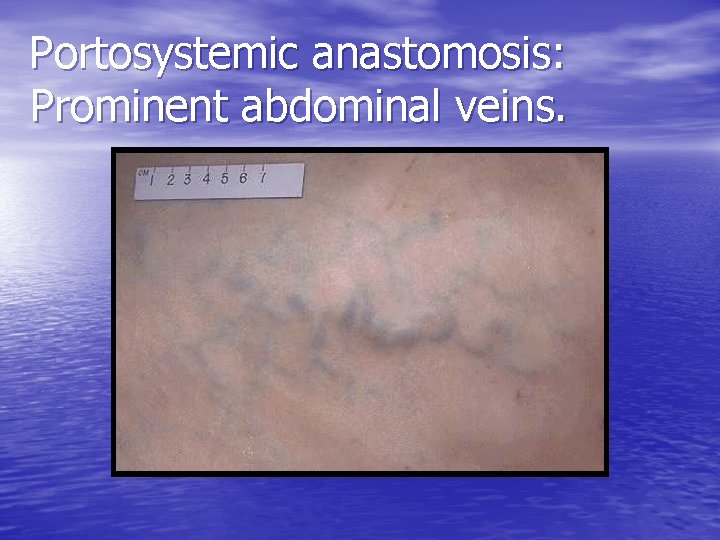
Portosystemic anastomosis: Prominent abdominal veins.
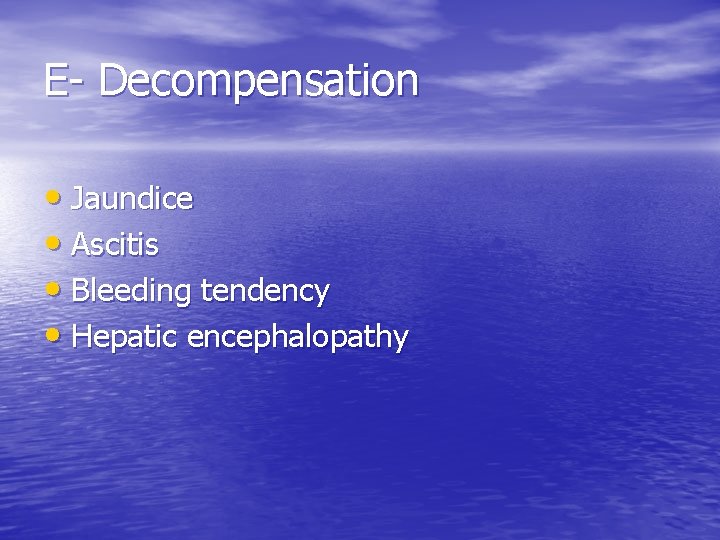
E- Decompensation • Jaundice • Ascitis • Bleeding tendency • Hepatic encephalopathy
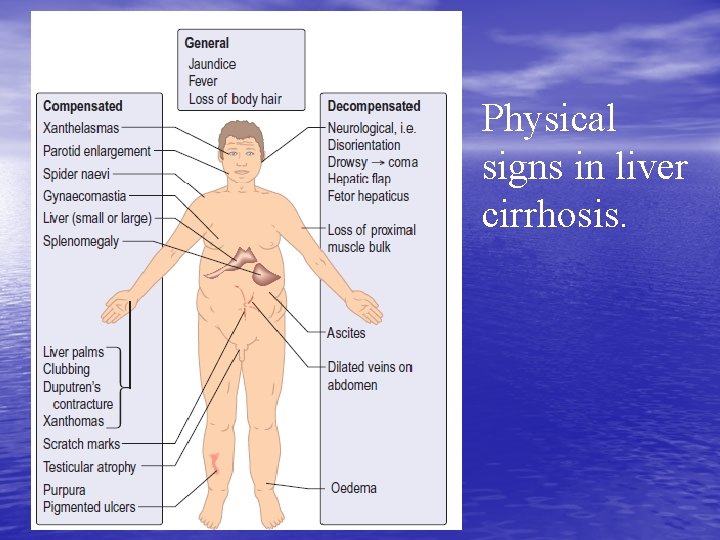
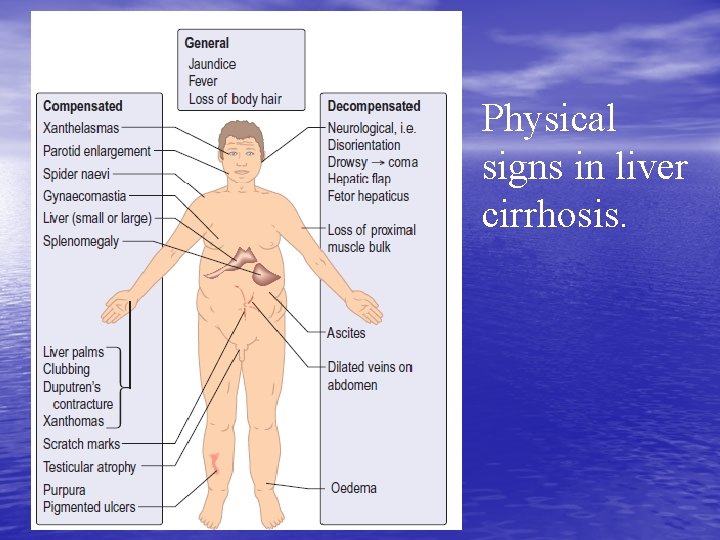
Physical signs in liver cirrhosis.

Investigations
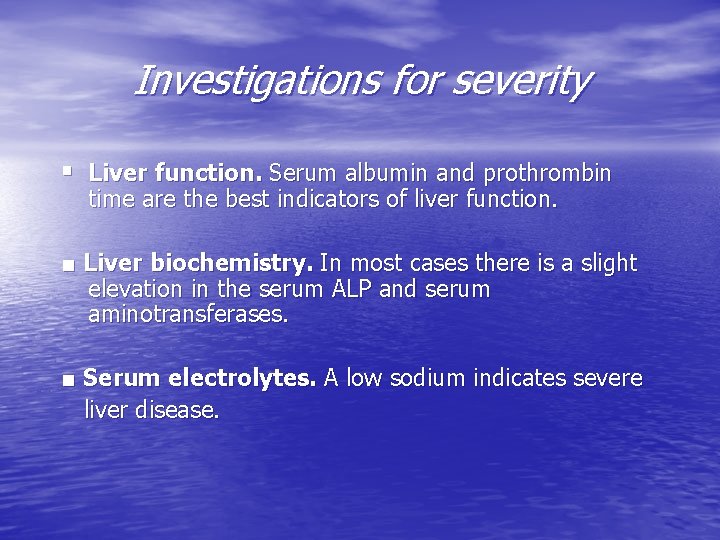
Investigations for severity § Liver function. Serum albumin and prothrombin time are the best indicators of liver function. ■ Liver biochemistry. In most cases there is a slight elevation in the serum ALP and serum aminotransferases. ■ Serum electrolytes. A low sodium indicates severe liver disease.
Investigations for the etiology • • • Viral markers Serum autoantibodies Iron indices and ferritin Copper, ceruloplasmin Alpha 1 antitrypsin (Serum copper and alpha 1 antitrypsin should always be measured in young cirrhotics)
Others • Ultrasound examination. • CT scan. • MRI scan. • Endoscopy. • Liver biopsy.

Management

► Management is that of complications. ► Patients should have 6 -monthly ultrasound and serum AFP to detect the development of a hepatocellular carcinoma as early as possible. ► There is no treatment that will arrest or reverse the cirrhotic changes although progression may be halted by correcting the underlying cause.
► Patients with compensated cirrhosis should lead a normal life. ► The only dietary restriction is to reduce salt intake. ► Aspirin and NSAIDs should be avoided. ► Alcohol should be avoided.
LIVER TRANSPLANTATION ► This is an established treatment for a number of liver diseases. ► Shortage of donors is a major problem in all developed countries.
Course and Prognosis
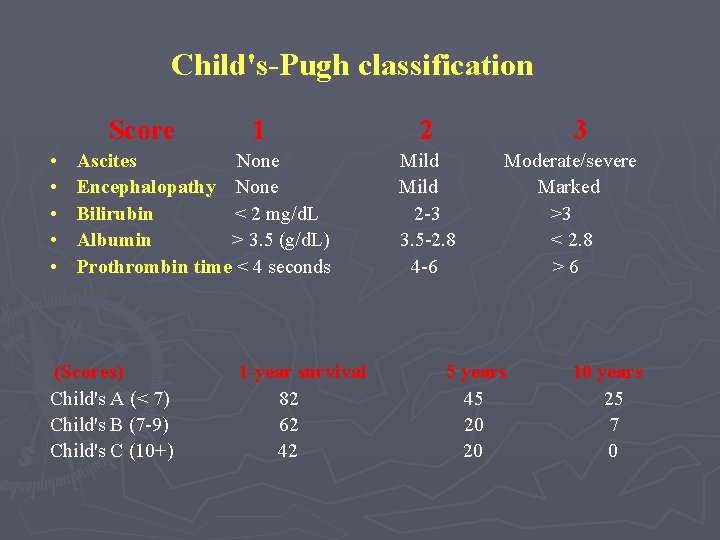
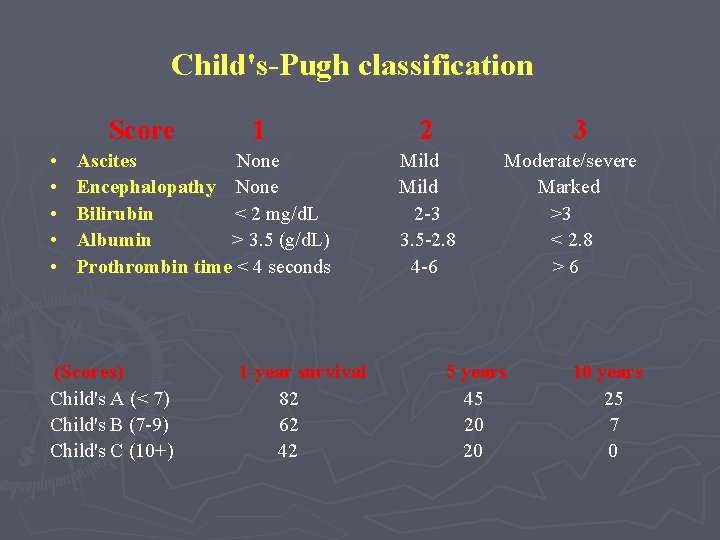
Child's-Pugh classification Score • • • 1 Ascites None Encephalopathy None Bilirubin < 2 mg/d. L Albumin > 3. 5 (g/d. L) Prothrombin time < 4 seconds (Scores) Child's A (< 7) Child's B (7 -9) Child's C (10+) 1 -year survival 82 62 42 2 3 Mild 2 -3 3. 5 -2. 8 4 -6 Moderate/severe Marked >3 < 2. 8 >6 5 years 45 20 20 10 years 25 7 0
COMPLICATIONS AND EFFECTS OF CIRRHOSIS
► Portal hypertension and gastrointestinal haemorrhage ► Ascites ► Portosystemic encephalopathy ► Renal failure (hepatorenal syndrome) ► Hepatopulmonary syndrome ► Hepatocellular carcinoma ► Bacteraemias, infections ► Malnutrition
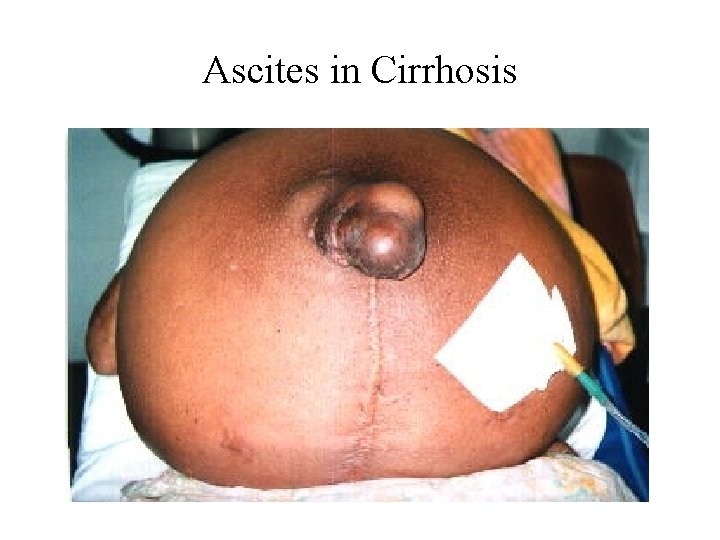
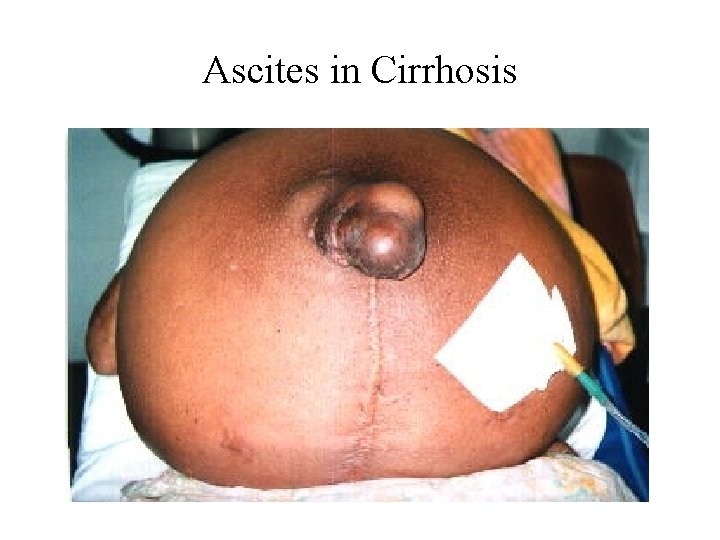
Ascites in Cirrhosis

Hepatocellular Carcinoma
 Mitochondrial swelling
Mitochondrial swelling Stages of cirrhosis
Stages of cirrhosis Liver cirrhosis stages
Liver cirrhosis stages Kelsey conrad
Kelsey conrad Complication of liver cirrhosis
Complication of liver cirrhosis Primary biliary cholangitis skin
Primary biliary cholangitis skin Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis What is hepatocirrhosis
What is hepatocirrhosis Pathophysiology of cirrhosis of liver
Pathophysiology of cirrhosis of liver Complication of liver cirrhosis
Complication of liver cirrhosis Mahmoud arafa
Mahmoud arafa Ahmed muhudiin ahmed
Ahmed muhudiin ahmed Dr usama ahmad
Dr usama ahmad Ali ahmed is a mathematics professor who tries to involve
Ali ahmed is a mathematics professor who tries to involve Promotion from associate professor to professor
Promotion from associate professor to professor Terlipressin
Terlipressin Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Nor udca
Nor udca Diet hepatic encephalopathy
Diet hepatic encephalopathy Easl 2018 decompensated cirrhosis
Easl 2018 decompensated cirrhosis Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Mild hepatic steatosis
Mild hepatic steatosis Primary biliary cirrhosis
Primary biliary cirrhosis Cirrhosis
Cirrhosis What is cirrhosis
What is cirrhosis Cirrhosis care near woodland
Cirrhosis care near woodland Pokemon my ass rom hack
Pokemon my ass rom hack Ass
Ass Angela fogarolli
Angela fogarolli Valbona berisha fakulteti i edukimit
Valbona berisha fakulteti i edukimit Neptune ass
Neptune ass Oracin
Oracin Brazilian ass slave
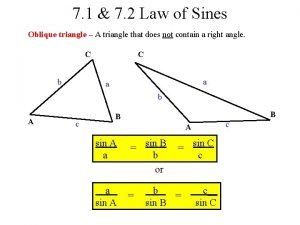
Brazilian ass slave Oblique triangle
Oblique triangle Heba ass
Heba ass Hana ass
Hana ass Hermana ass
Hermana ass Ass ana
Ass ana Big asd fans
Big asd fans Sead dizdarevic profesor
Sead dizdarevic profesor Ass salud
Ass salud