Liver Cirrhosis Assist Prof Mona Arafa Tropical Medicine





- Slides: 45

Liver Cirrhosis Assist. Prof. Mona Arafa Tropical Medicine Department

Objectives 1. Understand the basic mechanisms of Liver cirrhosis 2. Recognize the classic presentations of Liver cirrhosis and its complications 3. Get an idea about the management of these complications
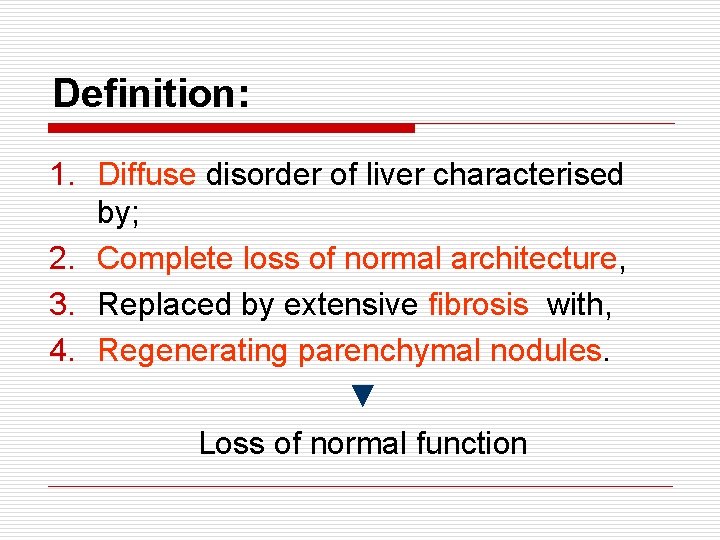
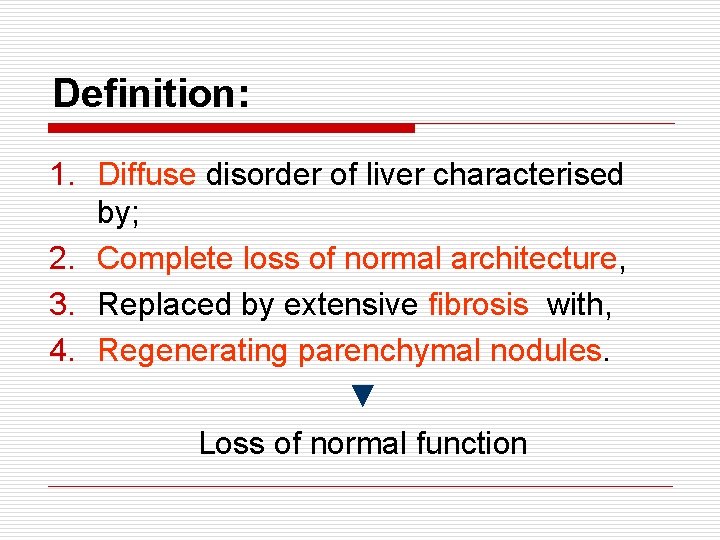
Definition: 1. Diffuse disorder of liver characterised by; 2. Complete loss of normal architecture, 3. Replaced by extensive fibrosis with, 4. Regenerating parenchymal nodules. ▼ Loss of normal function
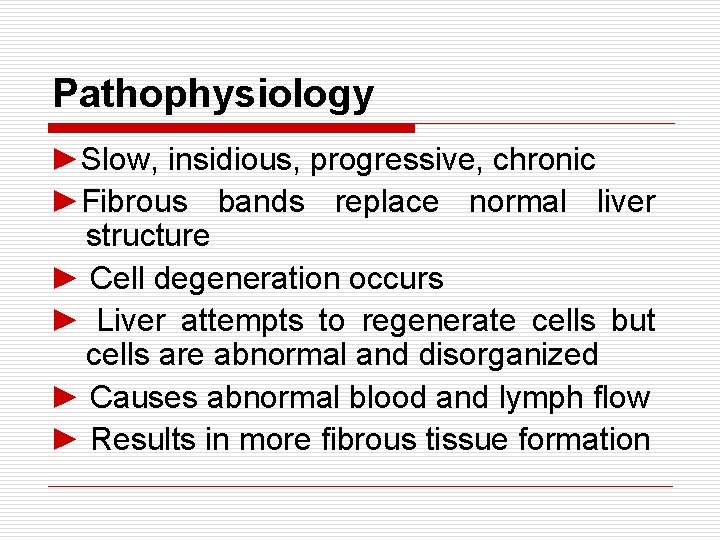
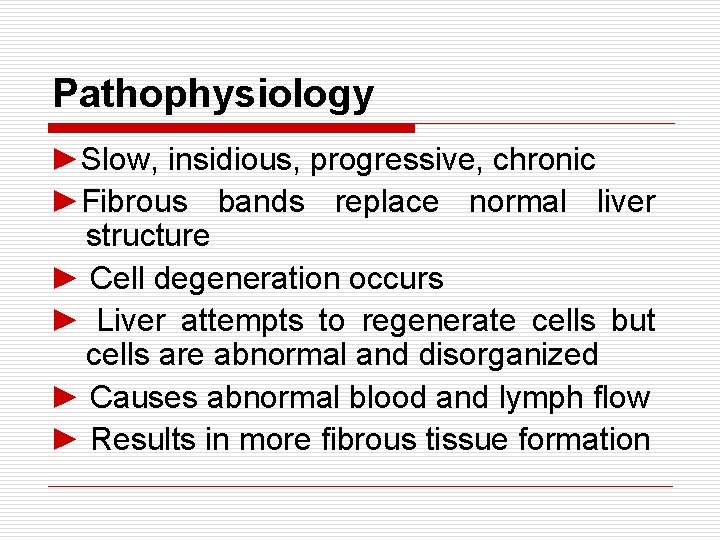
Pathophysiology ►Slow, insidious, progressive, chronic ►Fibrous bands replace normal liver structure ► Cell degeneration occurs ► Liver attempts to regenerate cells but cells are abnormal and disorganized ► Causes abnormal blood and lymph flow ► Results in more fibrous tissue formation
Normal Liver
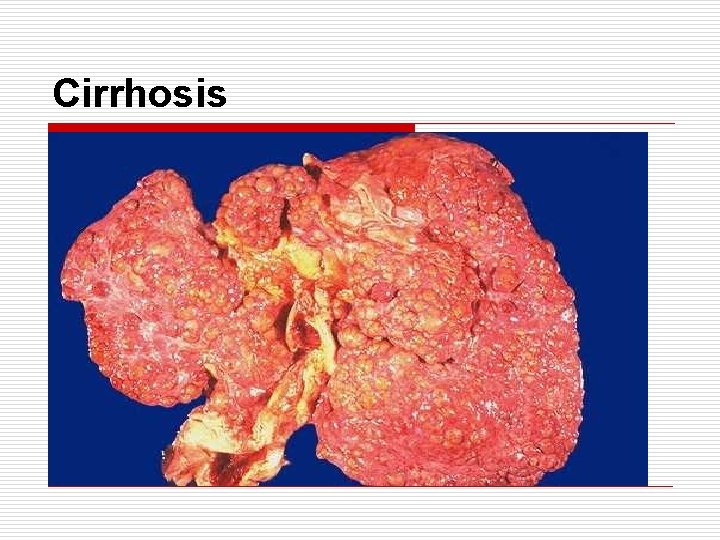
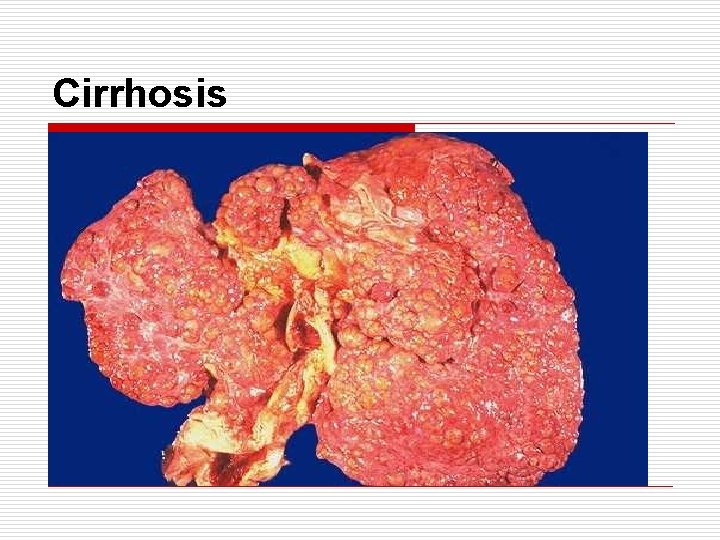
Cirrhosis
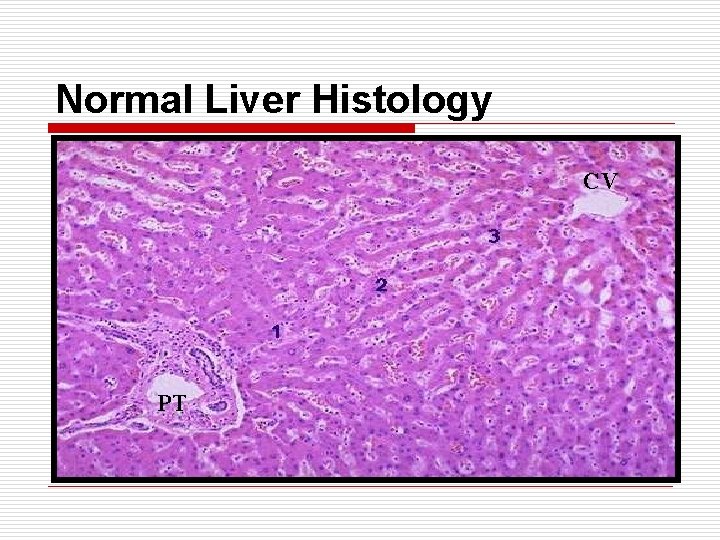
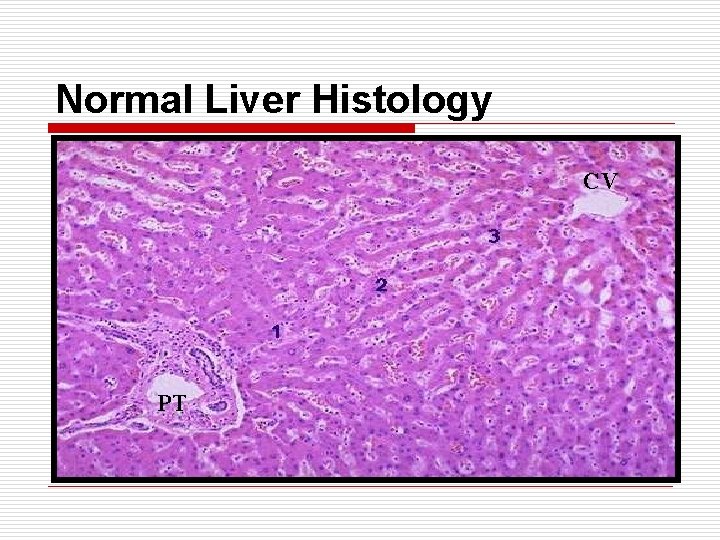
Normal Liver Histology CV PT

Cirrhosis Fibrosis Regenerating Nodule
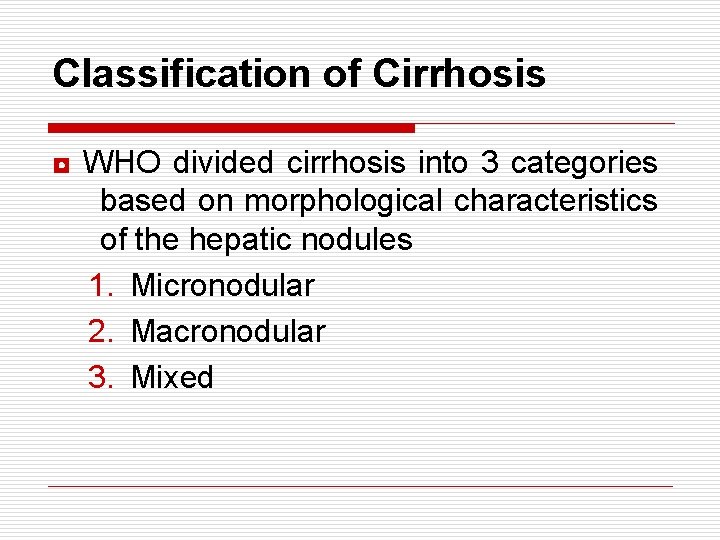
Classification of Cirrhosis ◘ WHO divided cirrhosis into 3 categories based on morphological characteristics of the hepatic nodules 1. Micronodular 2. Macronodular 3. Mixed
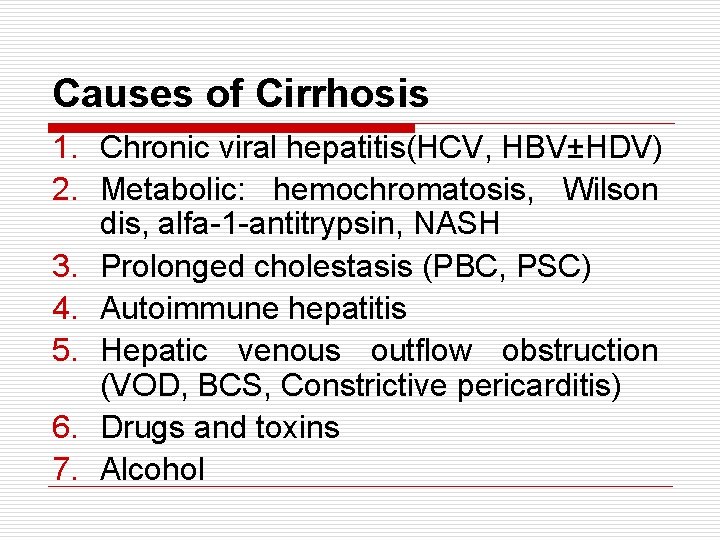
Causes of Cirrhosis 1. Chronic viral hepatitis(HCV, HBV±HDV) 2. Metabolic: hemochromatosis, Wilson dis, alfa-1 -antitrypsin, NASH 3. Prolonged cholestasis (PBC, PSC) 4. Autoimmune hepatitis 5. Hepatic venous outflow obstruction (VOD, BCS, Constrictive pericarditis) 6. Drugs and toxins 7. Alcohol
Clinical Presentation o Stigmata of chronic liver disease. o Abnormal LFTs and CBC. o Radiographic abnormalities. o Complication of cirrhosis. o Cirrhotic appearance of the liver at laparotomy or laparoscopy.
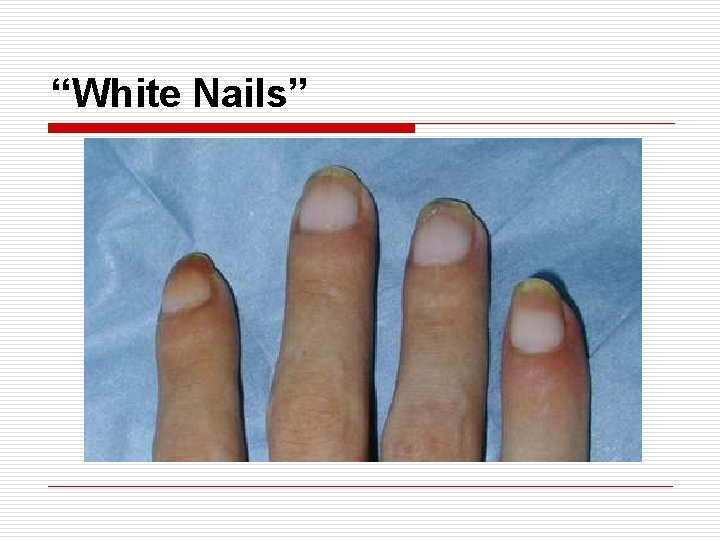
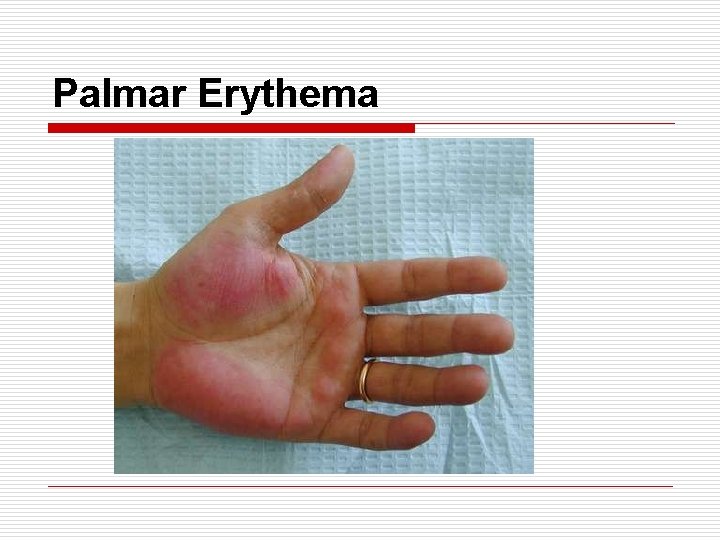
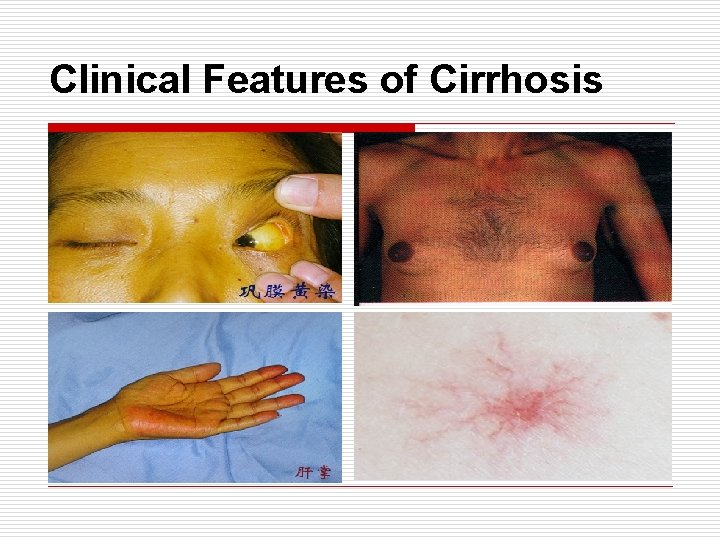
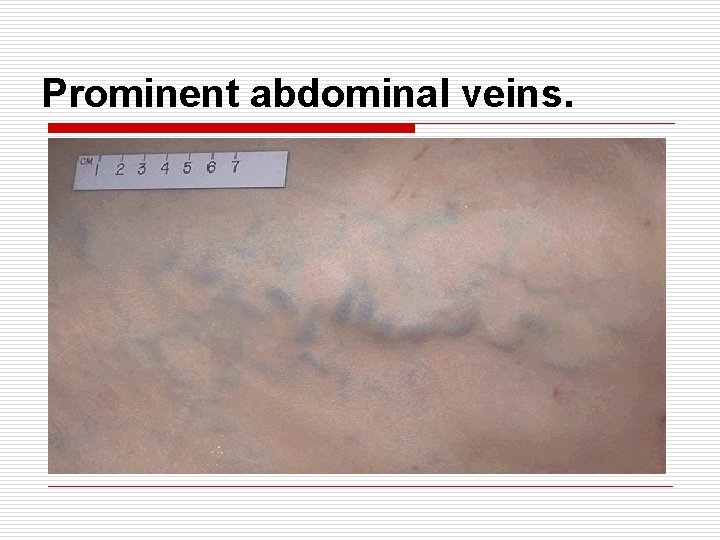
Clinical Features *Fatigue, anorexia, malaise. *Weight loss & muscle wasting. *Jaundice & dark urine. *Parotid enlargement & diarrhea. *Anemia, leucopenia, thrombocytopenia. *Bleeding gum, epistaxis, ecchymosis. *Spider angioma, palmar erythema, white nails, dilated veins.
Clinical Features Cont. *Gynecomastia, change in body hair patterns. *Amenorrhea, loss of libido, testicular atrophy, impotence. *Swelling of LL and abdomen. *Dyspnea & hypoxia. *Increased susceptibility to infections.
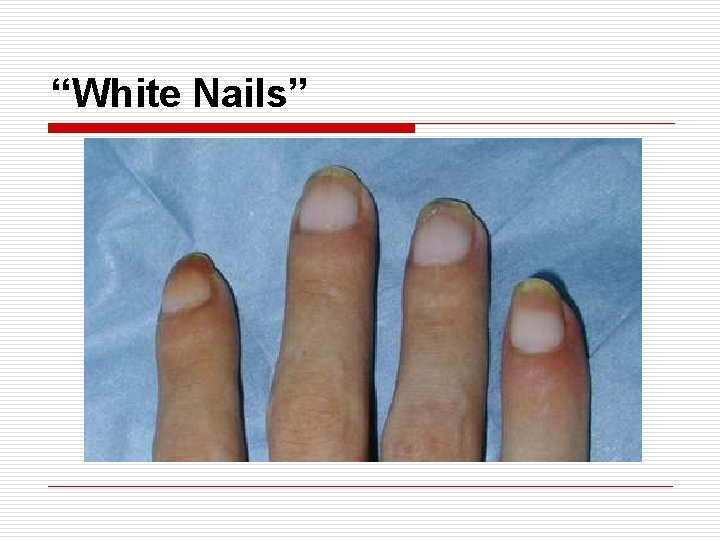
“White Nails”
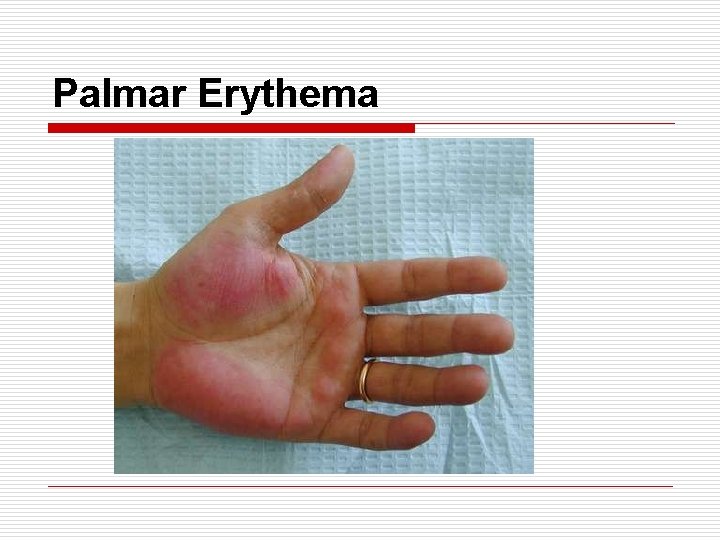
Palmar Erythema
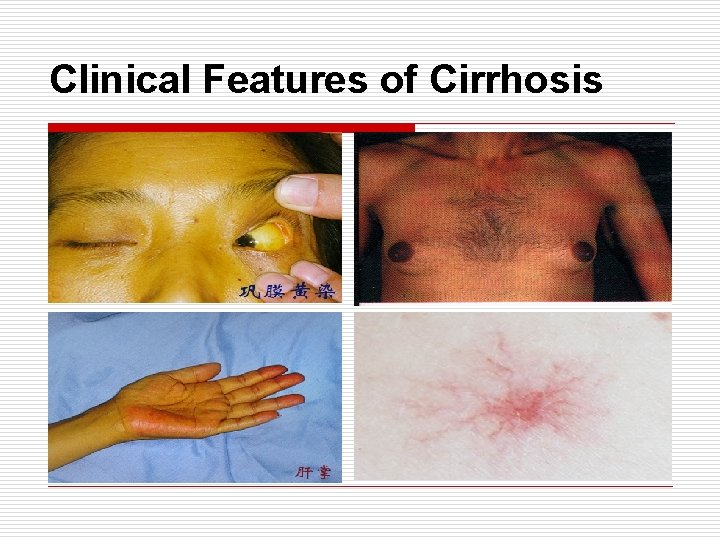
Clinical Features of Cirrhosis
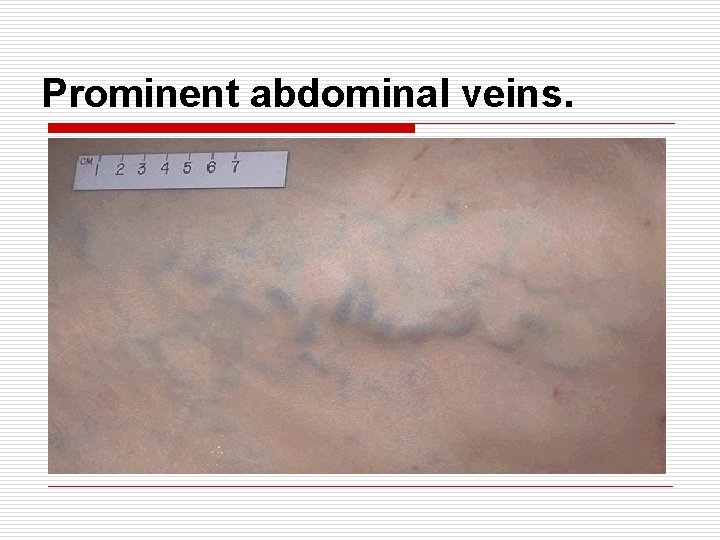
Prominent abdominal veins.
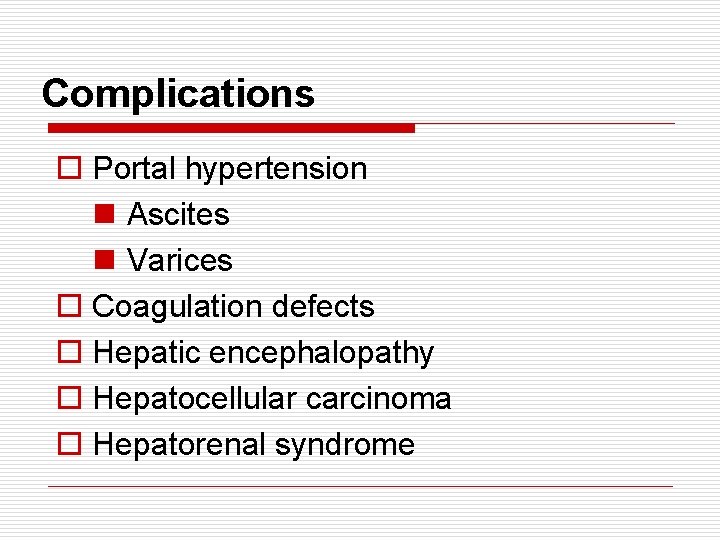
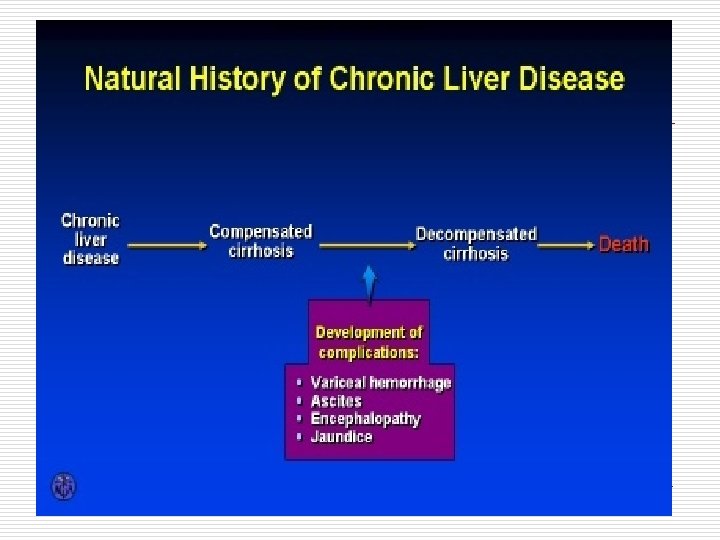
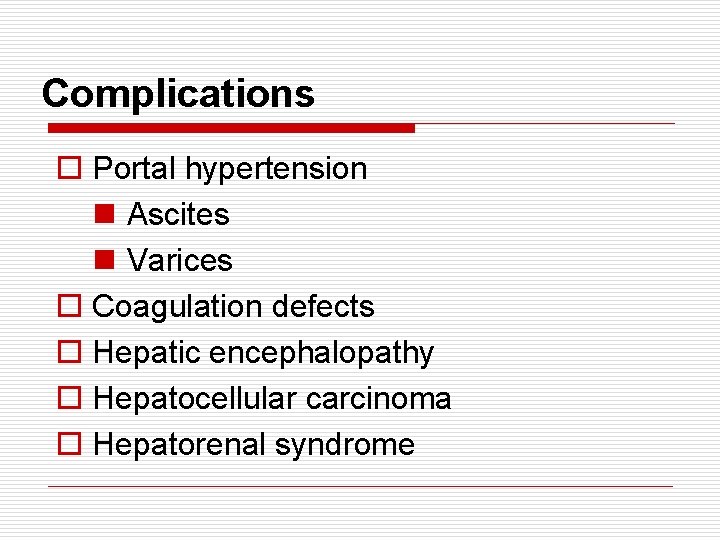
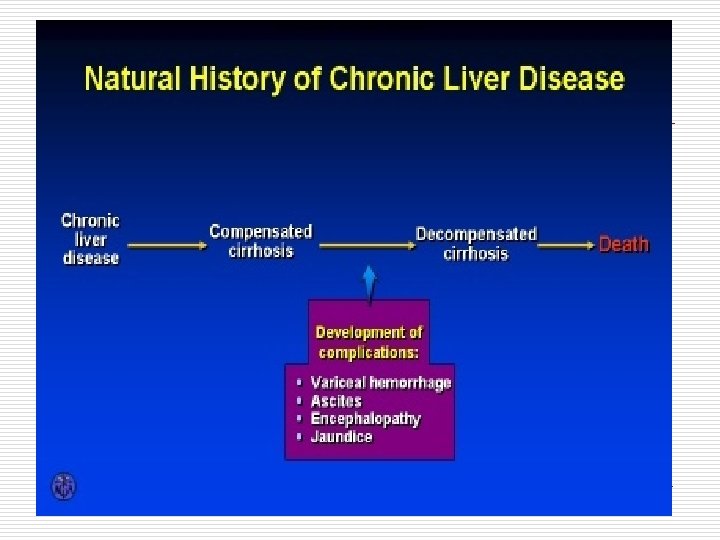
Complications o Portal hypertension n Ascites n Varices o Coagulation defects o Hepatic encephalopathy o Hepatocellular carcinoma o Hepatorenal syndrome
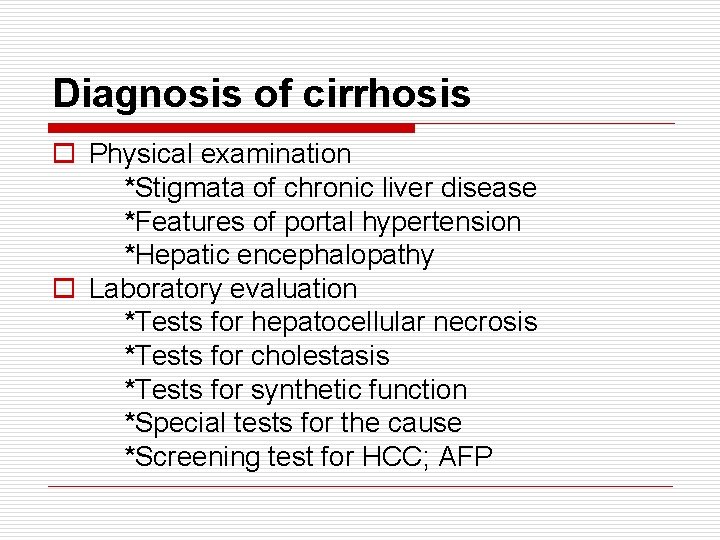
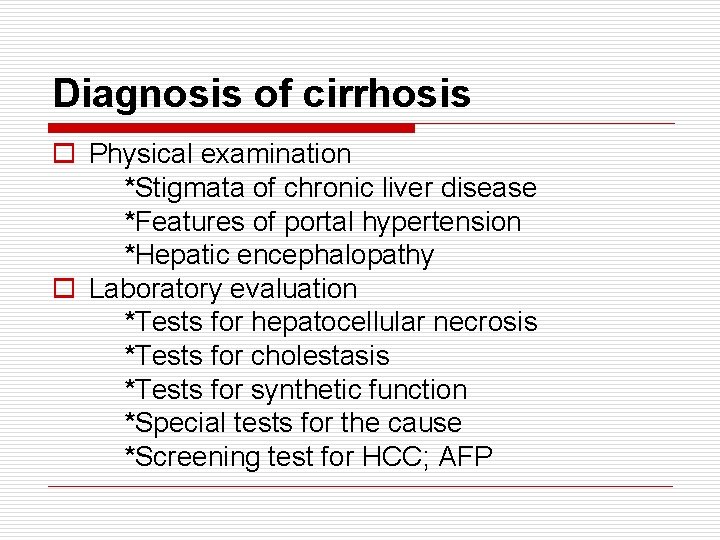
Diagnosis of cirrhosis o Physical examination *Stigmata of chronic liver disease *Features of portal hypertension *Hepatic encephalopathy o Laboratory evaluation *Tests for hepatocellular necrosis *Tests for cholestasis *Tests for synthetic function *Special tests for the cause *Screening test for HCC; AFP
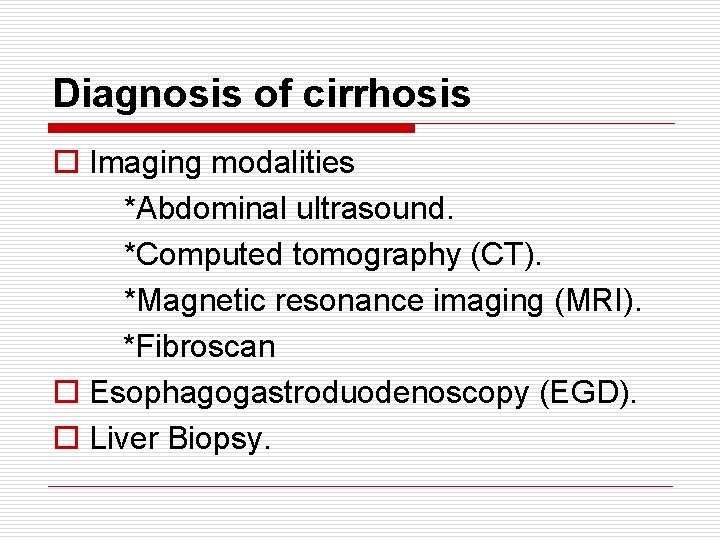
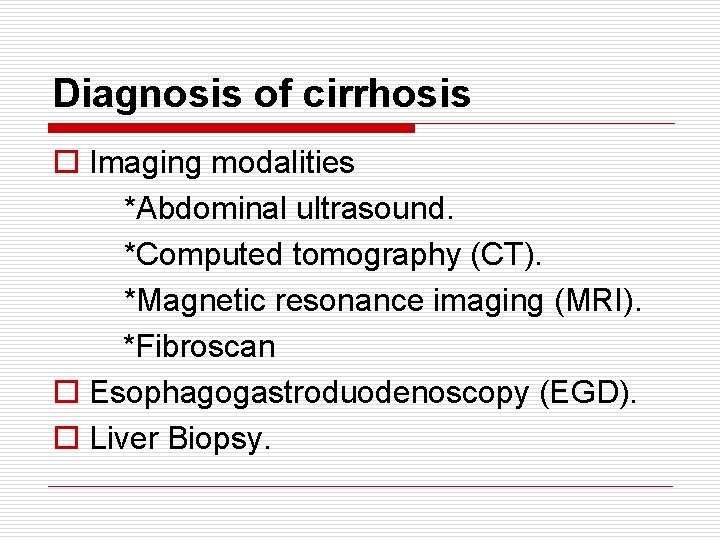
Diagnosis of cirrhosis o Imaging modalities *Abdominal ultrasound. *Computed tomography (CT). *Magnetic resonance imaging (MRI). *Fibroscan o Esophagogastroduodenoscopy (EGD). o Liver Biopsy.
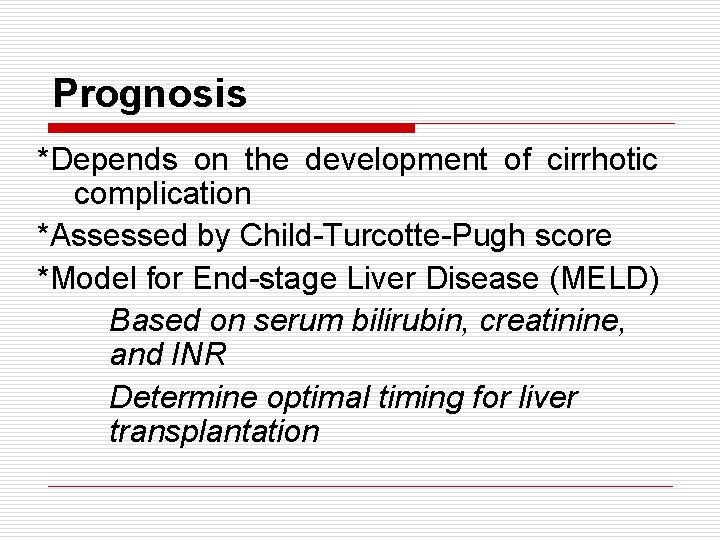
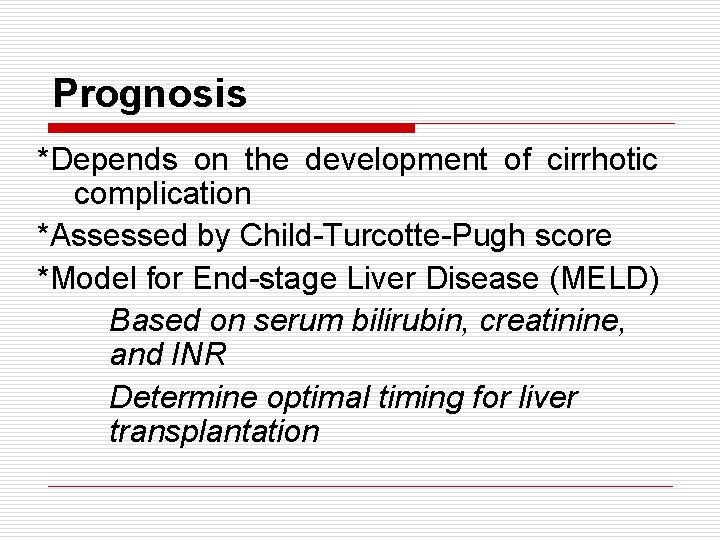
Prognosis *Depends on the development of cirrhotic complication *Assessed by Child-Turcotte-Pugh score *Model for End-stage Liver Disease (MELD) Based on serum bilirubin, creatinine, and INR Determine optimal timing for liver transplantation
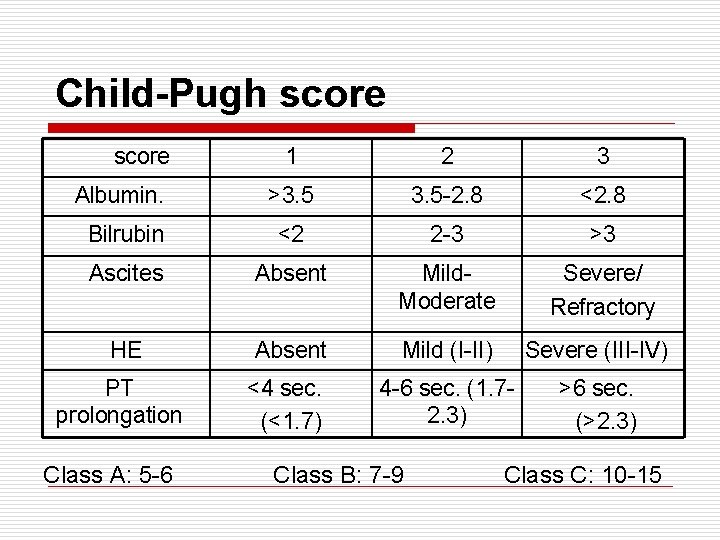
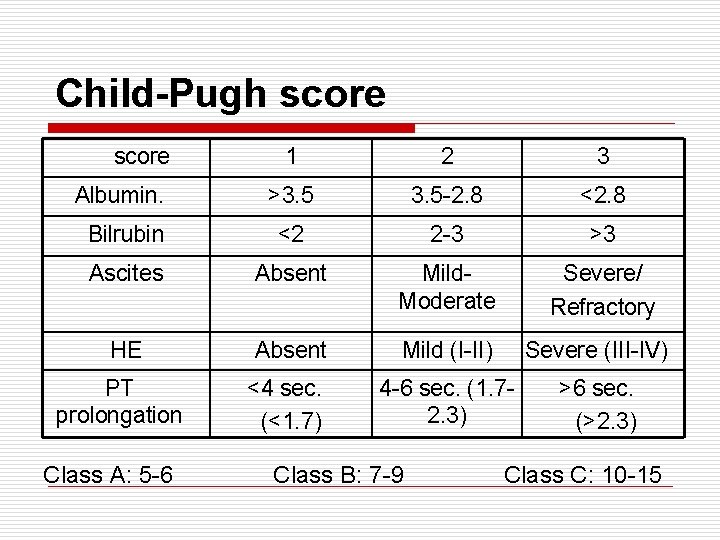
Child-Pugh score 1 2 3 Albumin. >3. 5 -2. 8 <2. 8 Bilrubin <2 2 -3 >3 Ascites Absent Mild. Moderate Severe/ Refractory HE Absent Mild (I-II) Severe (III-IV) PT prolongation <4 sec. (<1. 7) 4 -6 sec. (1. 72. 3) >6 sec. (>2. 3) Class A: 5 -6 Class B: 7 -9 Class C: 10 -15
Management o Specific treatment *Antiviral in HBV-cirrhosis *Corticosteroids in AIH *Phlebotomy in hemochromatosis o Treatment of complications o Screening for HCC o Liver transplantation
Portal hypertension Definition : Increase in hepatic sinusoidal pressure to ≥ 6 mm Hg. N. B : Portal pressure must be at least 10 mm Hg for gastroesophegeal varices to develop and at least 12 mm Hg for varicees to bleed.
Portal hypertension is classified as : prehepatic , hepatic and post hepatic. Prehpatic causes include : *Splenic vien thrombosis *Portal vein thrombosis (associated with hpercoagulable states and with malignancy )
Intrahepatic causes : Presinusoidal : eg. Schistosomiasis Sinusoidal : eg. Cirrhosis Post sinusoidal : eg. VOD
Post hepatic causes : *Chronic right sided heart failure *TR Obstructing lesions of hepatic viens and I. V. C (Budd-chiari syndrome )
Management of complications Varices o May be esophageal, gastric, colo-rectal o Diagnosis *History : Hematemesis, melena *Physical examination *Ultrasound abdomen *Endoscopy
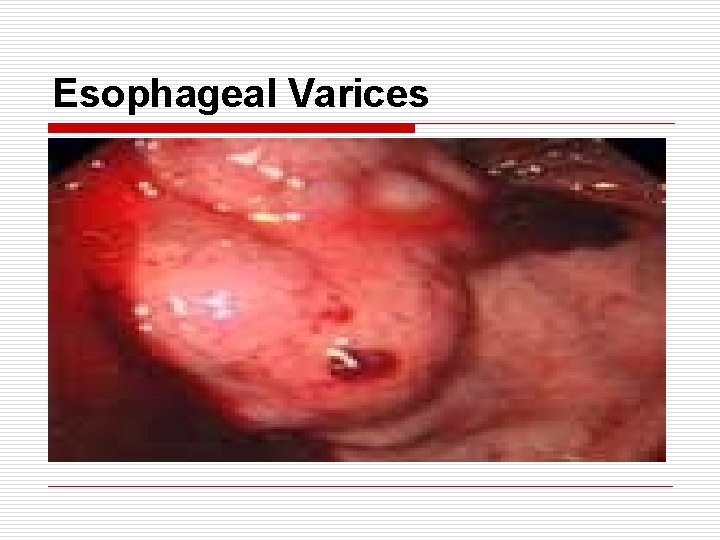
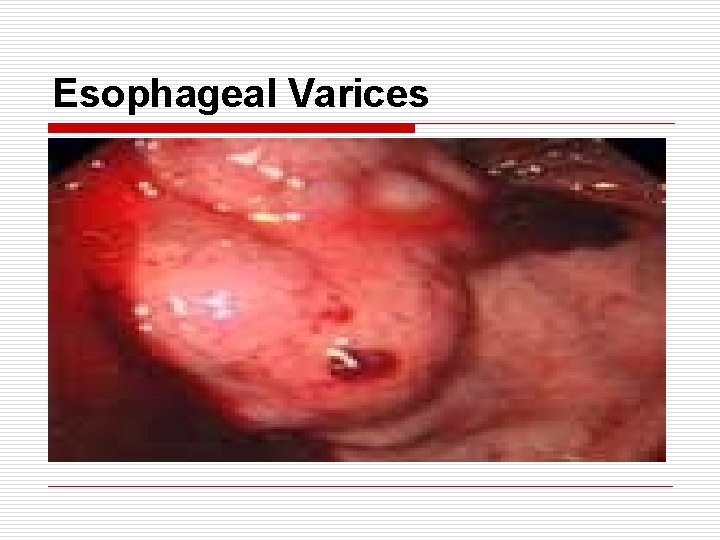
Esophageal Varices
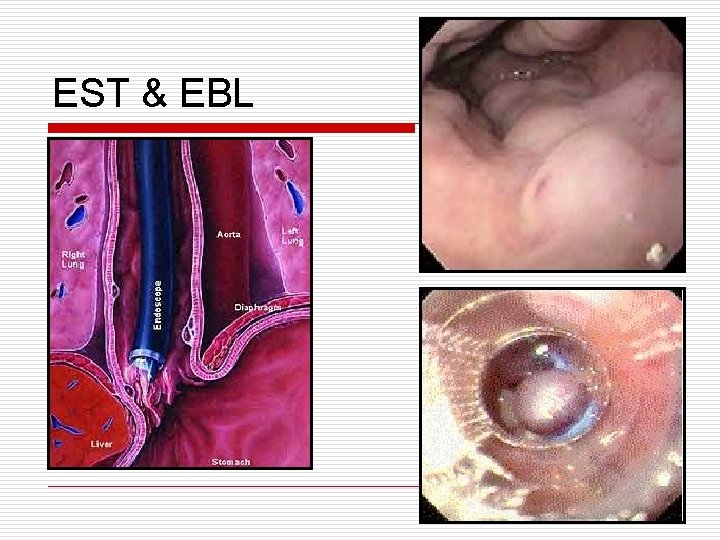
Management of complications Varices o Management *ABC *Two IV Lines *Blood group *Resuscitation (fluid, blood, FFP) *IV vasoconstrictors (Octreotide) *Endoscopic therapy (EST, EBL) *Shunting (surgical, TIPS)
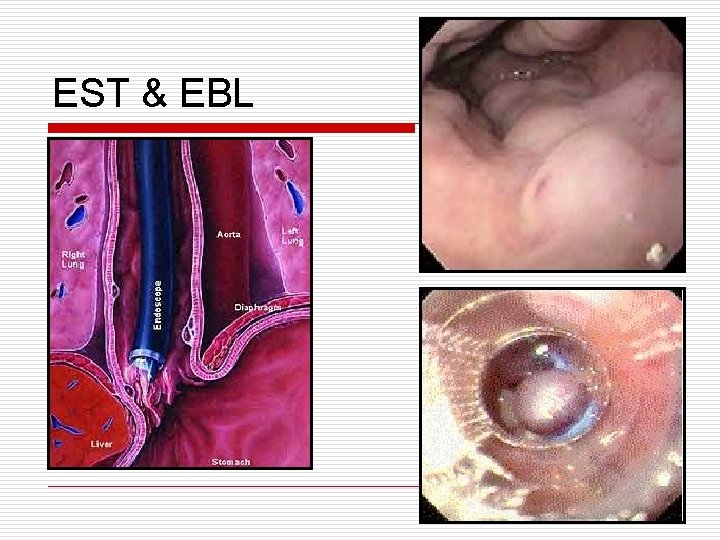
EST & EBL
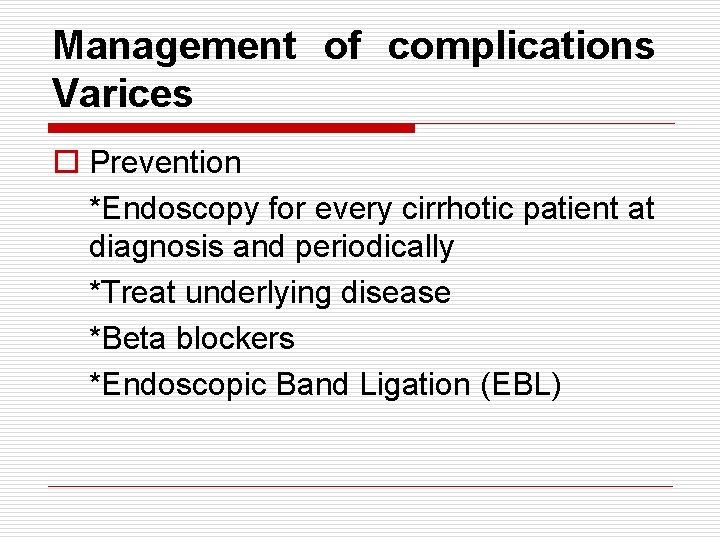
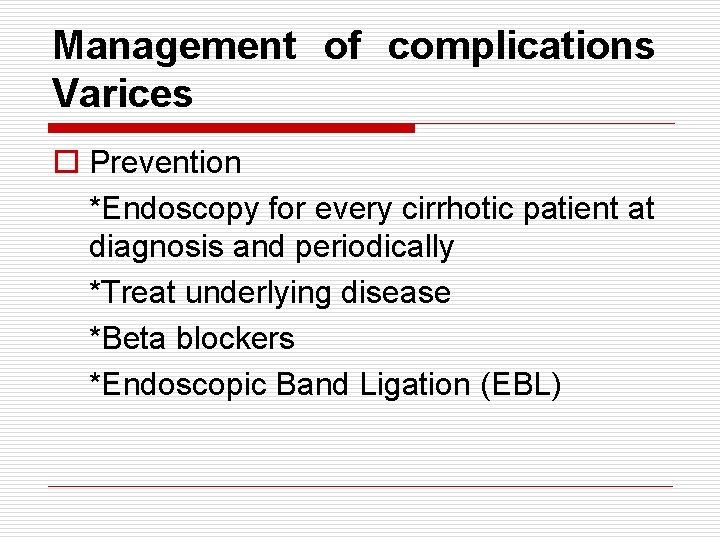
Management of complications Varices o Prevention *Endoscopy for every cirrhotic patient at diagnosis and periodically *Treat underlying disease *Beta blockers *Endoscopic Band Ligation (EBL)

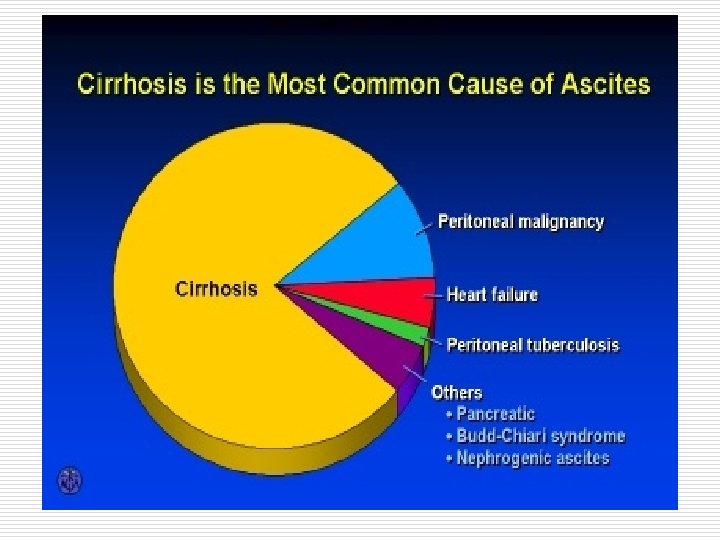
Ascites
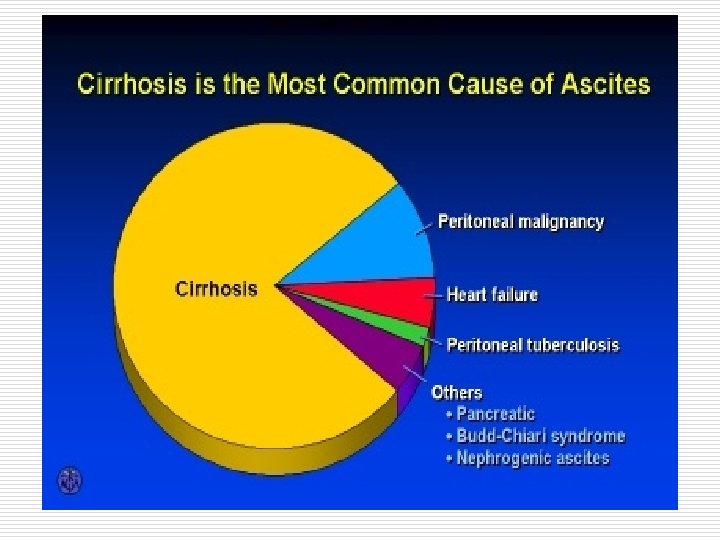
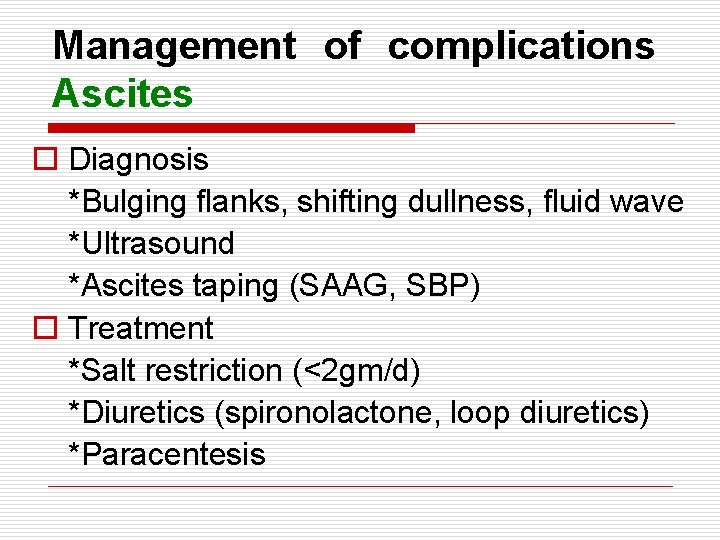
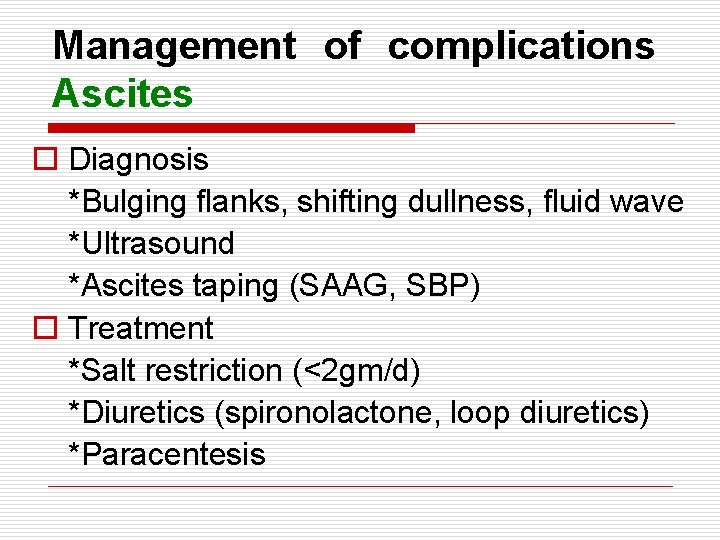
Management of complications Ascites o Diagnosis *Bulging flanks, shifting dullness, fluid wave *Ultrasound *Ascites taping (SAAG, SBP) o Treatment *Salt restriction (<2 gm/d) *Diuretics (spironolactone, loop diuretics) *Paracentesis

Paracentesis
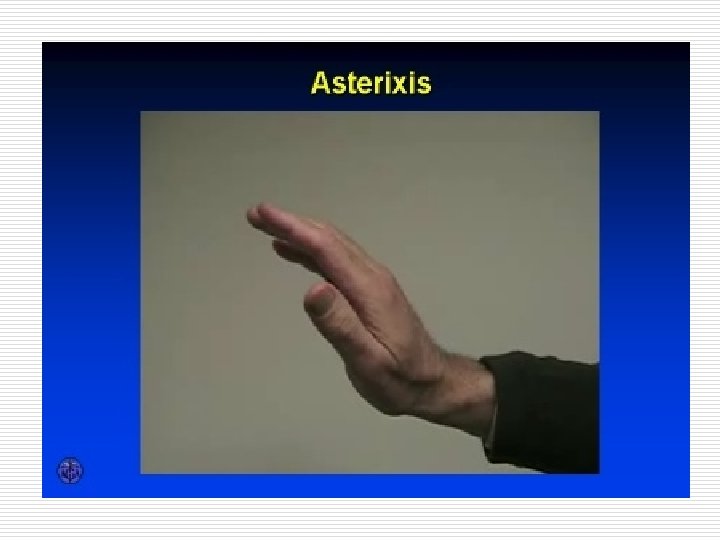
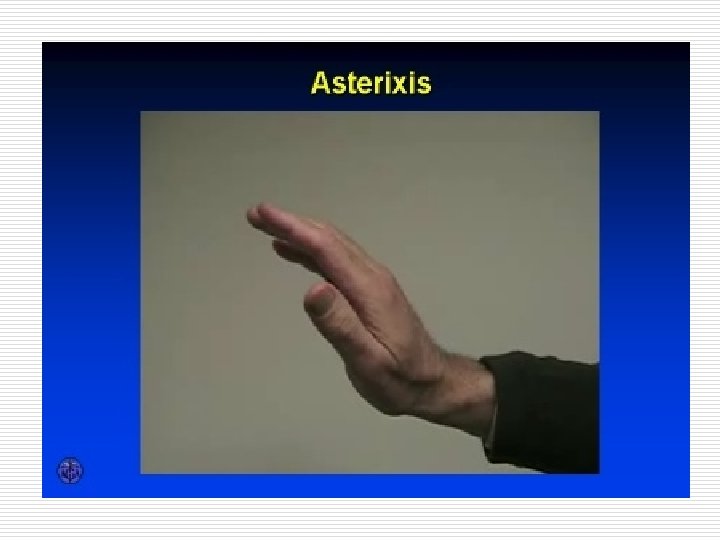
Hepatic encephalopathy o Neuropsychiatric abnormalities secondary to liver disease
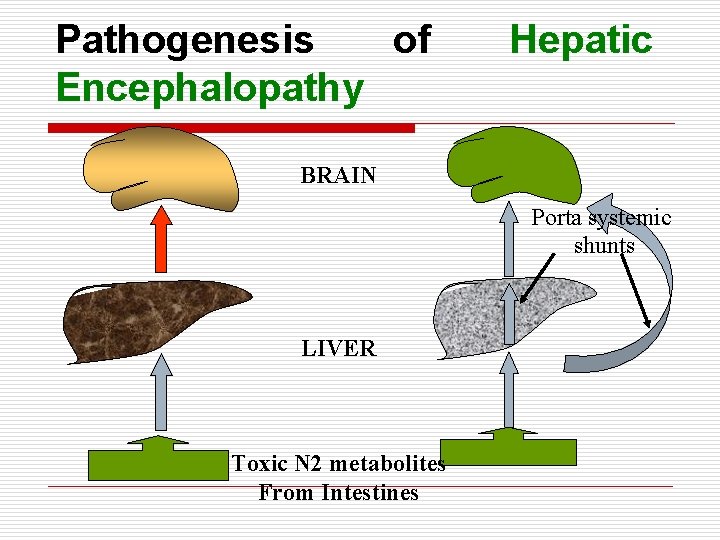
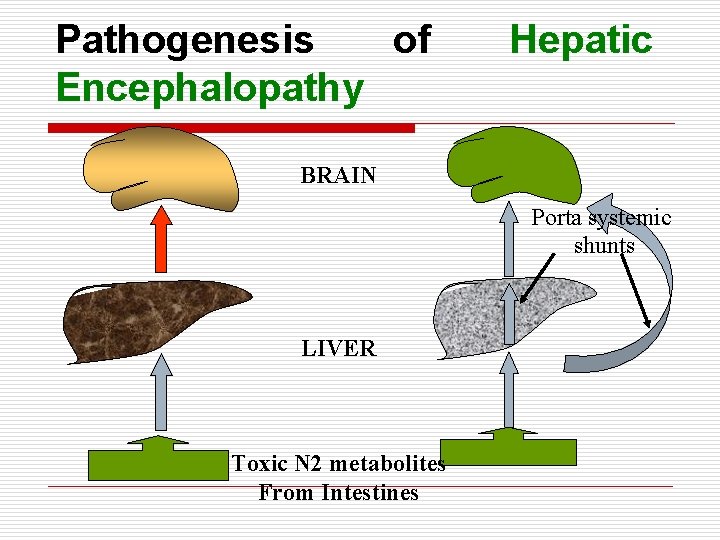
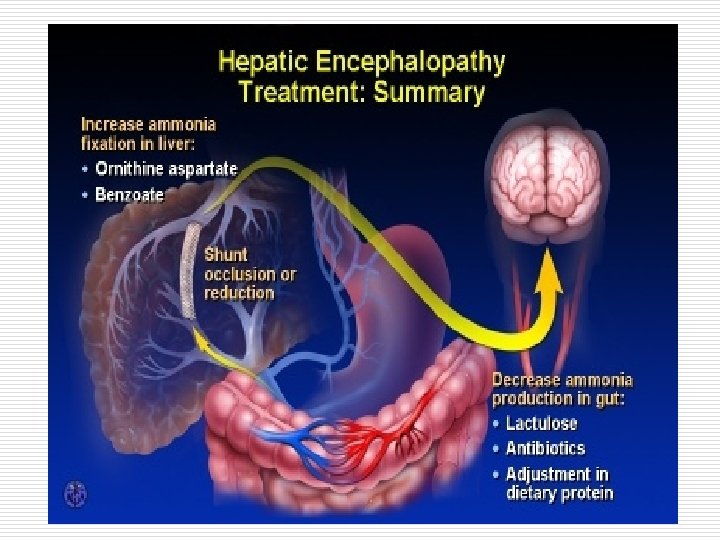
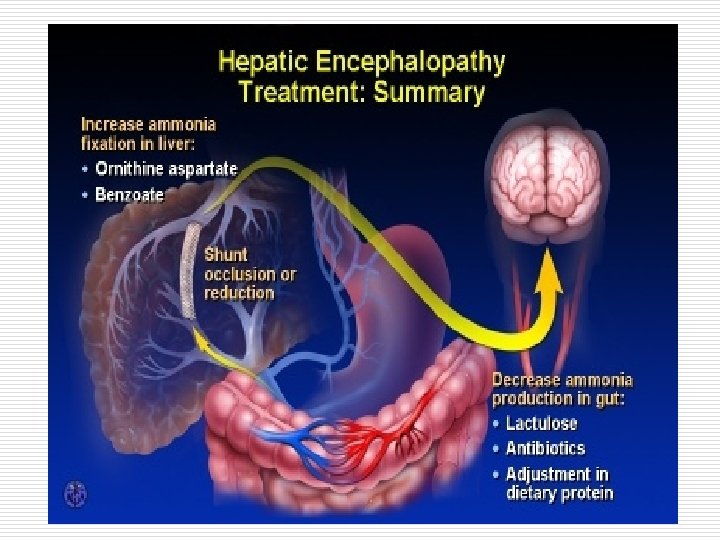
Pathogenesis of Encephalopathy Hepatic BRAIN Porta systemic shunts LIVER Toxic N 2 metabolites From Intestines
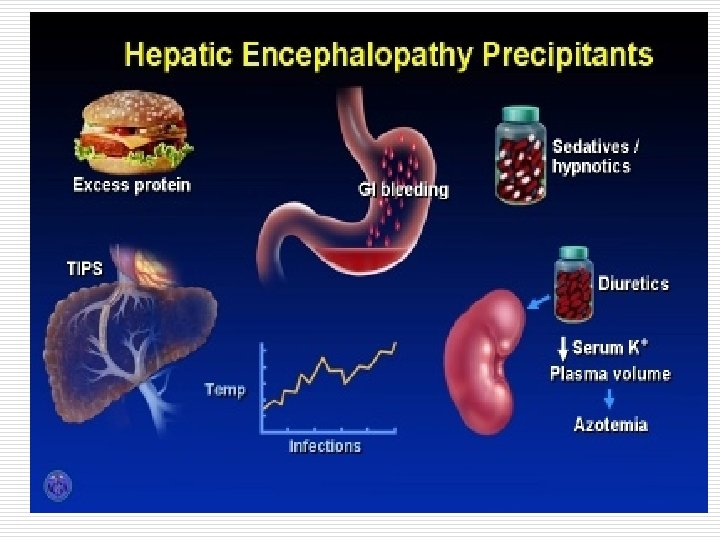
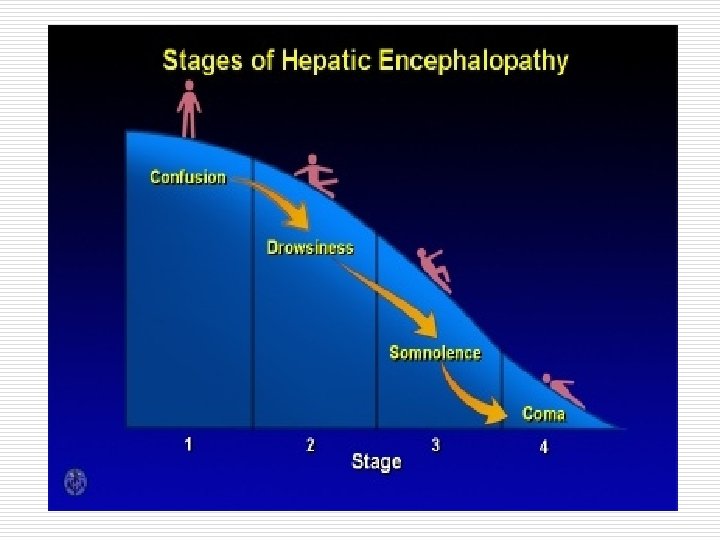
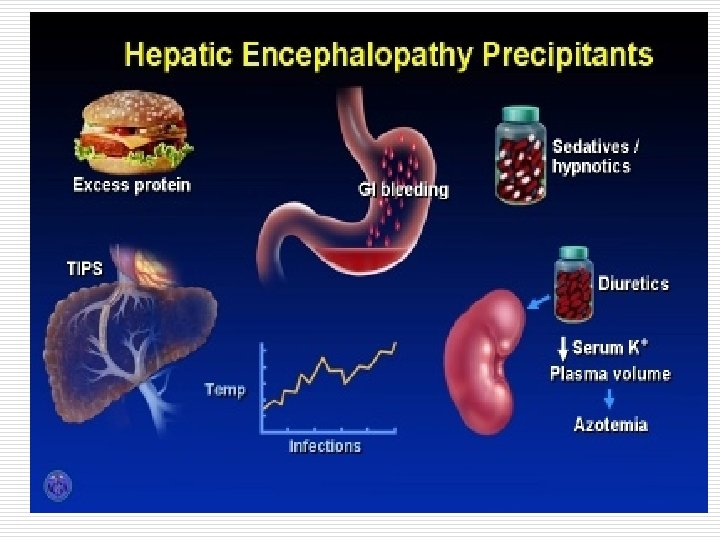
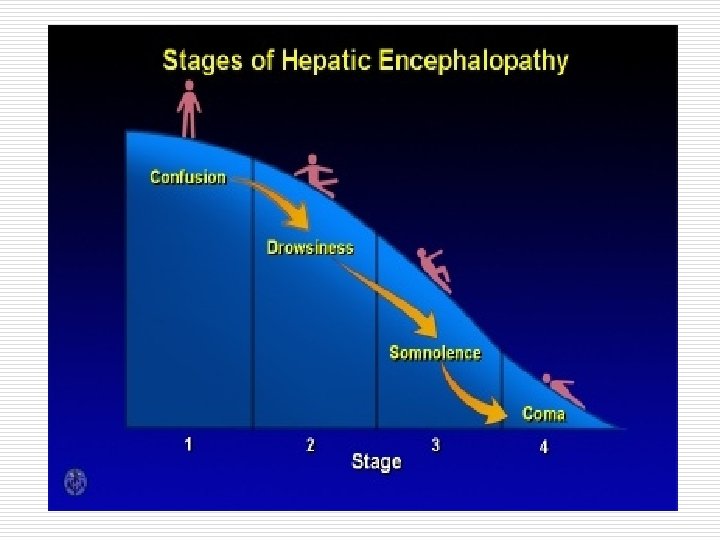
Management of complications Hepatic encephalopathy o Treatment *Identify and treat precipitating factor *Low protein diet *L-ornithine L-aspartate *Antibiotics (Neomycin, metronidazole, rifaximin) *Lactulose *Enemas *Transplantation
Thank You